Submitted:
23 March 2025
Posted:
24 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Scale Development
2.2. Delphi Expert Consultation
2.3. Expert Evaluation and Data Analysis
2.4. Participant Recruitment
2.5. Reliability and Validity Testing
2.6. Statistical Analysis
3. Results
3.1. Expert Panel
3.1.1. Expert Demographics
3.1.2. Expert Correlation Coefficients
3.2. Delphi Results
3.4. Statistical Analysis Results
3.4.1. Analysis of Pharmacists' Demographic Data on Psychological Contract, Job Burnout, and Attitudes and Behaviors Toward Patient Medication Adherence Management
3.4.2. Correlation Between Pharmacists' Psychological Contract, Job Burnout, and Attitudes and Behaviors Toward Patient Medication Adherence Management
3.4.3. Regression Analysis of Pharmacists' Attitudes and Behaviors Toward Patient Medication Adherence Management
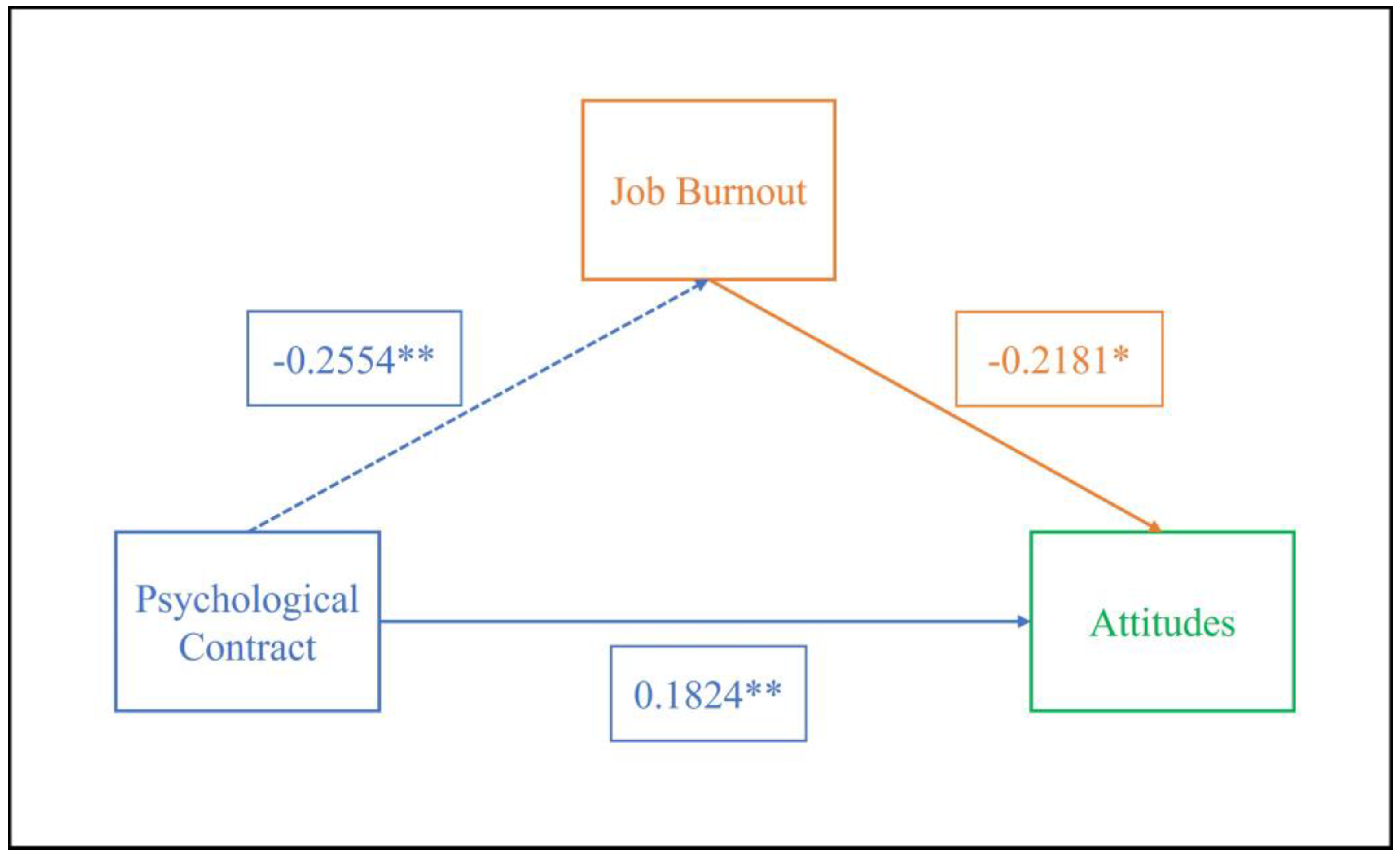
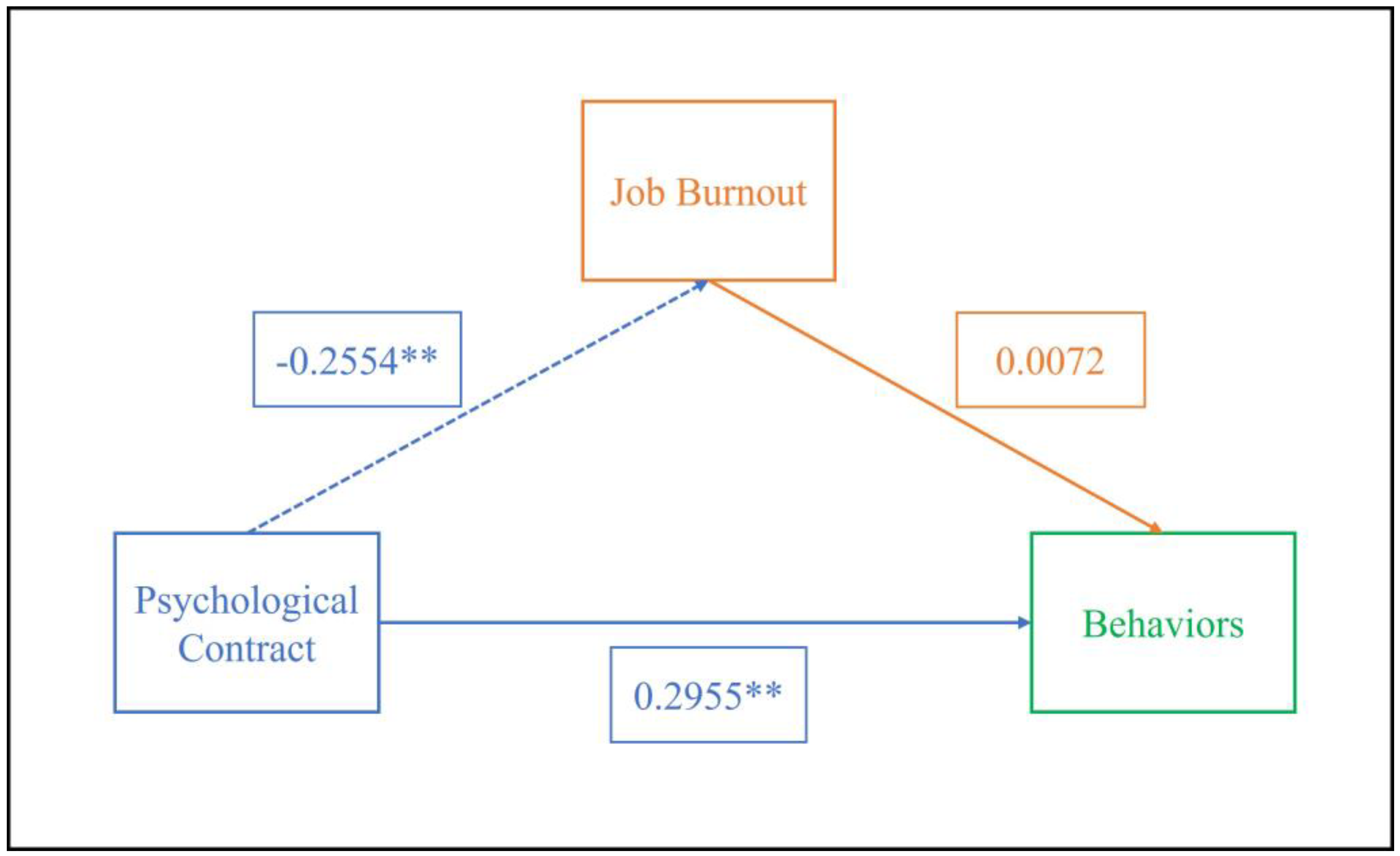
3.4.4. Mediating Effect of Job Burnout
| Model | Type of effect | Effect | standard error | t/Z | P | Boot CI Upper Limit | Boot CI lower limit | Proportion of effect |
|---|---|---|---|---|---|---|---|---|
| Attitudes | Total | 0.1914 | 0.0585 | 3.2713 | 0.0013 | 0.0759 | 0.3068 | 100.00% |
| Direct | 0.1466 | 0.0592 | 2.4753 | 0.0143 | 0.0297 | 0.2635 | 76.59% | |
| Professional burnout | 0.0448 | 0.0203 | 0.0113 | 0.0899 | 23.51% | |||
| Behaviors | Total | 0.4858 | 0.1185 | 4.0992 | 0.0001 | 0.2519 | 0.7197 | 100.00% |
| Direct | 0.4888 | 0.1229 | 3.9769 | 0.0001 | 0.2463 | 0.7314 | 100.62% | |
| Professional burnout | -0.0003 | 0.0381 | -0.0823 | 0.0724 | -0.62% |
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Ethical Approval
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Cr | Authority Coefficient |
| Cs | Coefficient of Familiarity |
| Ca | Coefficient of Judgment Basis |
| CV | Coefficient of Variation |
| KMO | Kaiser-Meyer-Olkin |
References
- Osterberg, L.; Blaschke, T. Adherence to medication. The New England journal of medicine 2005, 353(5), 487–97. [Google Scholar] [CrossRef] [PubMed]
- Baryakova, T. H.; Pogostin, B. H.; Langer, R.; McHugh, K. J., Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nature reviews. Drug discovery 2023, 22 (5), 387-409. [CrossRef]
- Ammous, O.; Kampo, R.; Wollsching-Strobel, M.; Zimmermann, M.; Andreas, S.; Friede, T.; Kroppen, D.; Stanzel, S.; Salem, S.; Windisch, W.; Mathes, T., Adherence-enhancing interventions for pharmacological and oxygen therapy in patients with COPD: a systematic review and component network meta-analyses. European respiratory review: an official journal of the European Respiratory Society 2024, 33 (173). [CrossRef]
- Chisholm-Burns, M. A.; Kim Lee, J.; Spivey, C. A.; Slack, M.; Herrier, R. N.; Hall-Lipsy, E.; Graff Zivin, J.; Abraham, I.; Palmer, J.; Martin, J. R.; Kramer, S. S.; Wunz, T., US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Medical care 2010, 48 (10), 923-33. Medical care. [CrossRef]
- Glover, L. H.; Skelley, J. W.; Cimino, L. H.; Berry, R. B., Impact of a pharmacist-driven COPD clinic on outcomes related to COPD in a federally qualified health center. J Am Pharm Assoc (2003) 2024, 64 (2), 512-516. [CrossRef]
- Wu, M.; Xu, X.; Zhao, R.; Bai, X.; Zhu, B.; Zhao, Z., Effect of Pharmacist-Led Interventions on Medication Adherence and Glycemic Control in Type 2 Diabetic Patients: A Study from the Chinese Population. Patient Prefer Adherence 2023, 17, 119-129. [CrossRef]
- Rousseau, D. M., New hire perceptions of their own and their employer’s obligations: A study of psychological contracts. Journal of Organizational Behavior 1990, 11 (5), 389-400. [CrossRef]
- Rodwell, J.; Johnson, D. The state of the psychological contract, justice and engagement drive nurses' performance behaviors. International journal of environmental research and public health, 2022; 19, 20. [Google Scholar] [CrossRef]
- Yu, J., Impacts of psychological contract fulfillment on work attitudes and behaviors during the COVID-19 pandemic: Mediating role of perceived organizational support. Curr Psychol 2022, 1-10. [CrossRef]
- Zhang, T. A study on the relationship between psychological contract of pharmacists in medical institutions and attitudes and behaviors of pharmaceutical services: a case study of Zunyi City [master's thesis]. Guizhou Province: Zunyi Medical University. (2019).
- Hu, L.; Chen, C.; Zhu, J.; Zhang, Y.; Chen, Y.; Jia, Y., Relationship Between Psychological Contract Violation and Physicians' Destructive and Constructive Behaviors in Tertiary Public Hospitals: An Empirical Evidence in Beijing. J Multidiscip Healthc 2023, 16, 997-1010. [CrossRef]
- Collins, A.; Beauregard, A., The effect of breaches of the psychological contract on the job satisfaction and wellbeing of doctors in Ireland: A quantitative study. Hum Resour Health 2020, 18 (1), 89. [CrossRef]
- Yu, Y.; Chen, Z.; Zhao, Y.; Wang, Y.; Zhang, R.; Zhou, X., Medical service quality, psychological contract, and patient loyalty: An empirical study among patients in China. Medicine 2020, 99 (48), e21079. [CrossRef]
- Zhang, T.; Yin, C.; Geng, Y.; Zhou, Y.; Sun, S.; Tang, F., Development and validation of psychological contract scale for hospital pharmacists. J Multidiscip Healthc 2020, 13, 1433-1442. [CrossRef]
- Dai, F.; Wei, K.; Chen, Y.; Ju, M., Construction of an index system for qualitative evaluation of undergraduate nursing students innovative ability: A Delphi study. J Clin Nurs 2019, 28 (23-24), 4379-4388. [CrossRef]
- Hu, Q.; Qin, Z.; Zhan, M.; Wu, B.; Chen, Z.; Xu, T., Development of a trigger tool for the detection of adverse drug events in Chinese geriatric inpatients using the Delphi method. Int J Clin Pharm 2019, 41 (5), 1174-1183. [CrossRef]
- de Goumoëns, V.; Lefrançois, L. E.; Forestier, A.; Grandjean, C.; Balice-Bourgois, C.; Quillet-Cotting, J.; Thévoz, A. L.; Ramelet, A. S., Bachelor nursing competencies to care for children in hospital and home settings: A Delphi study. Nurse education today 2025, 145, 106487. [CrossRef]
- Robinson, K. R.; Leighton, P.; Logan, P.; Gordon, A. L.; Anthony, K.; Harwood, R. H.; Gladman, J. R.; Masud, T., Developing the principles of chair based exercise for older people: a modified Delphi study. BMC geriatrics 2014, 14, 65. [CrossRef]
- Wells, C.; Kolt, G. S.; Marshall, P.; Bialocerkowski, A., The definition and application of Pilates exercise to treat people with chronic low back pain: a Delphi survey of Australian physical therapists. Physical therapy 2014, 94 (6), 792-805. [CrossRef]
- Teo, V.; Weinman, J.; Yap, K. Z., A cultural adaptation and validation study of the Intentional Nonadherence Scale (INAS) among people with type 2 diabetes in Singapore. Journal of psychosomatic research 2025, 188, 111969. [CrossRef]
- Wu, S. F., Rapid screening of psychological well-being of patients with chronic illness: Reliability and validity test on WHO-5 and PHQ-9 scales. Depression Research and Treatment 2014, 2014, 239490. [CrossRef]
- Dawson, L. A., What factors affect adherence to medicines? Archives of disease in childhood. Education and practice edition 2019, 104 (1), 49-52. [CrossRef]
- Ahn, H.; Byun, B. K.; Lee, T. H.; Kang, D. W.; Park, S. K., Effects of pharmacist-led home visit services and factors influencing medication adherence improvement. PloS one 2024, 19 (11), e0314204. [CrossRef]
- Listed, N.A. Adherence strategies. Improve bedside manner, affect patient adherence. Communication makes a difference. AIDS Alert 2005, 20, 57–59. [Google Scholar]
- de Oliveira, D. R.; Shoemaker, S. J., Achieving patient centeredness in pharmacy practice: openness and the pharmacist's natural attitude. J Am Pharm Assoc (2003) 2006, 46 (1), 56-64; quiz 64-6. [CrossRef]
- Feng, Y.; Zhang, Z.; Zeng, X.; Liu, Y., The influence of internship satisfaction and the psychological contract on the career identity behavior of fresh graduates. Front Psychol 2023, 14, 1294799. [CrossRef]
- Sui, M.; Yu, Z.; Zhou, M., The impact of psychological contract, physical and mental health on burnout in grassroots civil servants: Evidence from China. Psychology research and behavior management 2023, 16, 3461-3476. [CrossRef]
- Mu, X.; Yin, C.; He, X.; Li, H.; Gong, Y.; Wei, W.; Zhang, Y.; Tang, F., Correlation between patients' medication adherence and their psychological contract with hospital pharmacists. Patient Prefer Adherence 2020, 14, 1605-1613. [CrossRef]
- Gu, Y.; Mu, X.; Zhang, Y.; Tang, Y.; Zhang, T.; Tang, F., The Effect of Patients' Psychological Contract with Pharmacists on Medication Adherence: A Qualitative Study. Patient Prefer Adherence 2023, 17, 547-555. [CrossRef]
| The basis for expert review | Expert Scoring Judgment Coefficient | ||
|---|---|---|---|
| large | middle | little | |
| Practical experience | 0.5 | 0.4 | 0.3 |
| Theoretical analysis | 0.3 | 0.2 | 0.1 |
| Relevant literature | 0.1 | 0.1 | 0.1 |
| Personal intuition | 0.1 | 0.1 | 0..1 |
| Group | Basic Information | Number | Percentage |
|---|---|---|---|
| Gender | Male | 7 | 44% |
| Female | 9 | 56% | |
| Age | 30-39 | 5 | 31% |
| 40-49 | 7 | 44% | |
| 50-59 | 3 | 19% | |
| 60 and above | 1 | 6% | |
| Years of Experience | Less than 10 years | 0 | 0% |
| 10-20 years | 9 | 56% | |
| More than 20 years | 7 | 44% | |
| Education | Doctorate | 4 | 25% |
| Master's | 8 | 50% | |
| Bachelor's | 4 | 25% | |
| Professional Title | Senior Title | 9 | 56% |
| Associate Senior Title | 7 | 44% | |
| Research Field | Pharmacy | 1 | 6% |
| Clinical Pharmacy | 10 | 64% | |
| Hospital Pharmacy | 1 | 6% | |
| Pharmaceutical Management | 2 | 12.% | |
| Other | 2 | 12% | |
| Hospital Level | Grade III, Class A | 15 | 94% |
| Grade III, Class B | 1 | 6% |
| Indicator | First Round | |
|---|---|---|
| Expert Activity Index | Questionnaire Recovery Rate | 100% |
| Effective Recovery Rate | 100% | |
| Opinion Proposal Rate | 38.0% | |
| Expert Authority Coefficient | Cs | 0.70 |
| Ca | 0.90 | |
| Cr | 0.83 | |
| Expert Opinion Coordination Level | χ2 | 101.151 |
| CV | 0.08~0.60 | |
| W | 0.198** |
| Subscale | Key Indicators | Mean | Full Score Frequency | CV | Expert Comments |
|---|---|---|---|---|---|
| Pharmacist's attitude towards participating in patient medication adherence management | #1. Participating in patient medication adherence management is a requirement of pharmacists' professional ethics. | 4.63 | 62.50% | 0.10 | Modified to "professional ethics" to "responsibility" |
| 2. Participating in patient medication adherence management is not necessarily part of pharmacists' responsibilities. | 4.19 | 43.75% | 0.24 | ||
| #3. Pharmacists play a leading role in improving patient medication adherence. | 4.31 | 31.25% | 0.11 | Modified to "Pharmacists should play a leading role in patient medication adherence management." | |
| 4. Pharmacists' management of patient medication adherence plays a crucial role in treatment outcomes. | 4.38 | 43.75% | 0.14 | ||
| 5. Participating in medication adherence management is one way for pharmacists to achieve self-worth. | 4.56 | 68.75% | 0.15 | ||
| 6. Pharmacists should regularly assess patients' medication adherence. | 4.69 | 75.00% | 0.12 | ||
| 7. Pharmacists should regularly educate patients on medication adherence. | 4.81 | 81.25% | 0.08 | ||
| 8. Pharmacists should actively research and use various tools and methods to improve patient medication adherence. | 4.63 | 68.75% | 0.13 | ||
| *9. Whether patients adhere to medication is their own choice and is the responsibility of the patient or prescribing physician, not the pharmacist. | 2.75 | 25.00% | 0.60 | Delete, as it duplicates other items. | |
| The behaviors of pharmacists in participating in patient medication adherence management | 1. Establish patient health records, document medication information, and implement personalized adherence management. | 4.69 | 75.00% | 0.12 | |
| #2. Monitor patients' medication adherence through methods such as pill counting and blood drug concentration monitoring. | 4.44 | 50.00% | 0.14 | Modified to "Monitoring patient medication adherence through inquiry or monitoring methods (such as pill count, blood drug concentration monitoring, and clinical indicator testing, etc.)" | |
| #3. Assess the psychological and pathological factors in patients that may affect medication adherence. | 4.63 | 62.50% | 0.10 | Modified to “Assess psychological and pathophysiological factors (such as advanced age, memory decline, and decreased mobility) and social factors (such as previous treatment failures, medication accessibility, and financial burden related to medication use) that may affect the patient's medication adherence.” | |
| #4. Regularly inquire about objective factors that may affect patients' adherence to prescribed medications (such as side effects of the medication, financial burden related to medication use, complexity of the medication regimen, etc.). | 4.69 | 75.00% | 0.12 | Remove "financial burden related to medication use" | |
| #5. Verify the medication usage of patients with chronic diseases, especially the use of medication devices. | 4.56 | 56.35% | 0.11 | Modified to “Check the mastery of medication usage methods among patients with chronic diseases and implement necessary educational measures as needed.” | |
| 6. Assess the patient's medication adherence using compliance evaluation scales (such as MMAS, TAI, etc.) based on the patient's specific conditions. | 4.63 | 62.50% | 0.10 | ||
| #7. Conduct medication adherence education activities through patient education lectures and community outreach. | 4.50 | 56.25% | 0.14 | Modified to "Conduct medication adherence education activities through patient education lectures, community outreach, and playing medication education videos." | |
| #8. Correct the patient's misconception of stopping medication as soon as their condition shows slight improvement. | 4.75 | 75.00% | 0.09 | Modified to "correct the perception and behavior of patients discontinuing medication on their own, emphasizing the importance of regular medical visits and the dangers of arbitrarily stopping medication." | |
| #9. Implement standardized communication regarding medication therapy, covering the nature of the disease, medication options, treatment expectations, and more. | 4.50 | 56.25% | 0.14 | Modified to "Standardize communication regarding medication therapy, covering the nature of the disease, medication options, treatment expectations, safety, and cost-effectiveness." | |
| #10. Promote medication adherence-related communication among patients. | 3.75 | 31.25% | 0.35 | Modify to "Regularly organize group discussions among patients to exchange experiences on overcoming medication barriers and coping with drug side effects." | |
| 11. The pharmacist regularly communicates with the patient and their family members or caregivers to ensure that the patient is supervised in taking their medication according to the prescribed regimen. | 4.63 | 62.50% | 0.10 | ||
| #12. Collaborate with the medical team to provide feedback on patient adherence and offer recommendations for medication selection. | 4.69 | 68.75% | 0.10 | Change"offer recommendations for medication selection." to "provide recommendations for adjustments to drug treatment plans." | |
| 13. Provide patients with health consultations and guidance related to rational medication use, including diet, exercise, and stress management, and offer personalized professional services for special patient groups. | 4.38 | 43.75% | 0.14 | ||
| #14. During the patient consultation process, clarify and verify the medication instructions. | 4.44 | 56.25% | 0.16 | Modify to “During the medication guidance process, promptly correct any inappropriate medication behaviors of the patient, demonstrate the correct method, and ensure that they understand and master the proper way to take the medication.” | |
| *15. Make clear notes on the medications taken by patients who are forgetful or elderly. | 4.69 | 68.75% | 0.10 | Delete, as it duplicates other items. | |
| 16. Encourage patients to develop self-medication monitoring and cultivate awareness of self-adherence management. | 4.69 | 75.00% | 0.12 | ||
| 17. Using the Health Belief Model to enhance patients' perception of their susceptibility to illness and the severity of the disease. | 4.38 | 43.75% | 0.14 | ||
| 18. Plan, monitor, and evaluate the medication regimen, and establish a treatment plan that is tailored to the patient’s preferences. | 4.38 | 43.75% | 0.14 | ||
| #19. Use medication cards or instructional leaflets to remind and guide patients to take their medications correctly. | 4.38 | 43.75% | 0.14 | Modify to "Use drug cards or medication instruction leaflets to remind and guide patients to take their medications correctly, and make clear notes on the medications taken by forgetful or elderly patients." | |
| #20. Guide patients to use self-service medical devices (such as blood pressure monitors and glucometers) properly to promote adherence to prescribed medication regimens. | 4.31 | 31.25% | 0.11 | Modify to“Guide patients in the correct use of self-service medical devices (such as blood pressure monitors and glucometers) and instruct them on how to respond to abnormal monitoring results.” | |
| 21. Promote the use of smart pill boxes for patients who are eligible (features include real-time reminders and real-time synchronization of medication records, etc.). | 4.13 | 37.50% | 0.19 | ||
| #22. Patients are regularly reminded of medication use and drug replenishment through various communication means, including phone calls, text messages, pharmaceutical service platforms, QQ, WeChat, and others. | 4.38 | 56.25% | 0.18 | Modify to “Regularly remind patients of medication use, replenish medications, and provide professional answers to medication-related questions through communication means such as telephone, text messages, pharmaceutical service platforms, QQ, and WeChat.” | |
| *23. Research or use of artificial intelligence (AI) in managing patients' medication. | 3.69 | 12.50% | 0.25 | Delete, as it duplicates other items. | |
| #24. Keep abreast of the latest information and developments in first-line medications both domestically and internationally, and actively utilize new theories, knowledge, and technologies in the field of pharmaceutical and medical sciences to guide patients in the rational use of medications. | 4.50 | 56.25% | 0.14 | Modify to “Keep abreast of the latest information and development trends of first-line medications both domestically and internationally, and actively utilize new theories, knowledge, and technologies in the field of pharmaceutical medicine to guide rational medication use in clinical practice and for patients.” | |
| Add new entry:7. Verify the medication information of transferred patients, coordinate the medication plans, and ensure the continuity of medical care; 8. Regularly assess the patient's acceptance and implementation of personalized medication guidance or adherence reminders; 15. Based on the patient's feedback on drug efficacy or adverse reactions, promptly optimize medication guidance and intervention measures. | |||||
| Basic situation | Pharmacist (%) | |
|---|---|---|
| Gender | Male | 69 (38.3%) |
| Female | 111 (61.7%) | |
| Age | 20-29 | 61 (33.9%) |
| 30-39 | 83 (46.1%) | |
| 40-49 | 21 (11.7%) | |
| 50-59 | 15 (8.3%) | |
| 60+ | 0 (0%) | |
| Marital Status | Single | 52 (28.9%) |
| Married | 127 (70.6%) | |
| Divorced/Widowed | 1 (0.5%) | |
| Highest Education | Diploma | 12 (6.7%) |
| Bachelor's | 119 (66.1%) | |
| Master's | 46 (25.6%) | |
| Doctorate | 3 (1.6%) | |
| Years of Work Experience | 1-5 | 67 (37.2%) |
| 6-10 | 39 (21.7%) | |
| 11-15 | 41 (22.8%) | |
| 16-20 | 10 (5.5%) | |
| 21-25 | 8 (4.4%) | |
| 26-30 | 2 (1.1%) | |
| 30+ | 13 (7.3%) | |
| Title | No Title | 23 (12.8%) |
| Junior Pharmacist | 6 (3.3%) | |
| Pharmacist | 57 (31.7%) | |
| Senior Pharmacist | 79 (43.9%) | |
| Deputy Chief Pharmacist | 14 (7.8%) | |
| Chief Pharmacist | 1 (0.5%) | |
| Employment Type | Full-Time | 92 (51.1%) |
| Contract | 68 (37.8%) | |
| Part-Time | 20 (11.1%) | |
| Position | Inpatient Pharmacist | 38 (21.1%) |
| Outpatient Pharmacist | 70 (38.9%) | |
| Intravenous Therapy Pharmacist | 4 (2.2%) | |
| Clinical Pharmacist | 35 (19.4%) | |
| Other | 33 (18.4%) | |
| Income Level | 0~2000 | 12 (6.7%) |
| 2000~4000 | 43 (23.9%) | |
| 4000~6000 | 72 (40.0%) | |
| 6000+ | 53 (29.4%) | |
| Hospital Level | Tertiary General Hospital | 135 (75.0%) |
| Tertiary specialized hospital | 27 (15.0%) | |
| Secondary General Hospital | 16 (8.9%) | |
| Secondary Specialist Hospital | 2 (1.1%) | |
| Primary General Hospital | 0 (0%) |
| Number of Items | Cronbach’s α | |
|---|---|---|
| Attitudes | 8 | 0.796 |
| Behaviors | 25 | 0.986 |
| Attitudes | Behaviors | ||
|---|---|---|---|
| KMO Sample Measure | 0.899 | 0.963 | |
| Bartlett's Test of Sphericity Significance | Approximate Chi-Square | 1002.900 | 6275.223 |
| Degree of freedom | 28 | 300 | |
| Significance probability | 0.000 | 0.000 | |
| Group | Psychological contract | Job burnout | Attitudes | Behaviors | |
|---|---|---|---|---|---|
| Gender | ①Male | 4.89±0.737 | 2.90±0.940 | 4.11±0.441 | 3.51±1.052 |
| ②Female | 4.79±0.632 | 2.85±0.782 | 4.06±0.598 | 3.12±1.132 | |
| F | 0.949 | 0.157 | 0.263 | 5.254 | |
| P | 0.331 | 0.693 | 0.609 | 0.023 | |
| Age | ①20-29 | 4.88±0.719 | 2.81±0.856 | 4.07±0.583 | 3.48±1.165 |
| ②30-39 | 4.80±0.667 | 2.88±0.838 | 4.11±0.517 | 3.11±1.078 | |
| ③40-49 | 4.71±0.654 | 3.19±0.915 | 3.91±0.573 | 3.43±0.947 | |
| ④50-59 | 4.99±0.566 | 2.62±0.645 | 4.20±0.448 | 3.05±1.256 | |
| F | 0.671 | 1.574 | 1.021 | 1.606 | |
| P | 0.571 | 0.197 | 0.385 | 0.190 | |
| LSD/G-H | —— | ③>④* | —— | —— | |
| Marital Status | ①Single | 4.76±0.712 | 2.76±0.886 | 4.04±0.550 | 3.37±1.119 |
| ②Married | 4.86±0.662 | 2.90±0.186 | 4.10±0.541 | 3.22±1.118 | |
| ③Divorced/Widowed | 5.00±0.000 | 4.55±0.000 | 3.75±0.000 | 4.00±0.000 | |
| F | 0.380 | 2.505 | 0.452 | 0.574 | |
| P | 0.684 | 0.085 | 0.637 | 0.564 | |
| Highest Education | ①Diploma | 5.18±0.423 | 2.71±0.798 | 3.94±0.499 | 3.46±1.214 |
| ②Bachelor's | 4.82±0.688 | 2.92±0.879 | 4.05±0.526 | 3.21±1.121 | |
| ③Master's | 4.77±0.758 | 2.78±0.789 | 4.19±0.593 | 3.33±1.106 | |
| ④Doctorate | 4.79±1.068 | 2.70±0.335 | 4.21±0.402 | 3.80±0.771 | |
| F | 1.249 | 0.504 | 1.096 | 0.493 | |
| P | 0.294 | 0.680 | 0.352 | 0.687 | |
| Years of Work Experience | ①1-5 | 4.85±0.716 | 2.79±0.788 | 4.05±0.541 | 3.33±1.150 |
| ②6-10 | 4.78±0.641 | 2.90±0.791 | 4.20±0.562 | 3.08±1.088 | |
| ③11-15 | 4.85±0.625 | 2.86±0.878 | 4.05±0.567 | 3.39±1.003 | |
| ④16-20 | 4.80±0.850 | 2.81±1.078 | 4.11±0.582 | 3.40±1.408 | |
| ⑤21-25 | 4.79±0.799 | 3.80±1.053 | 3.78±0.499 | 3.61±1.158 | |
| ⑥26-30 | 3.91±0.265 | 2.84±0.996 | 3.69±0.442 | 1.68±0.849 | |
| ⑦30+ | 5.00±0.510 | 2.71±0.645 | 4.20±0.352 | 3.01±1.279 | |
| F | 0.807 | 1.862 | 1.089 | 1.260 | |
| P | 0.565 | 0.090 | 0.371 | 0.279 | |
| Title | ①No Title | 5.07±0.638 | 2.67±0.783 | 4.20±0.529 | 3.42±1.155 |
| ②Junior Pharmacist | 5.10±0.709 | 2.42±0.789 | 4.04±0.557 | 3.19±1.198 | |
| ③Pharmacist | 4.91±0.685 | 2.83±0.948 | 4.11±0.523 | 3.43±1.226 | |
| ④Senior Pharmacist | 4.65±0.673 | 2.93±0.716 | 4.05±0.567 | 3.13±1.007 | |
| ⑤Deputy Chief Pharmacist | 4.98±0.503 | 3.25±1.074 | 3.96±0.532 | 3.10±1.187 | |
| ⑥Chief Pharmacist | 5.30±0.000 | 1.86±0.000 | 4.25±0.000 | 4.04±0.000 | |
| F | 2.304 | —— | 0.488 | 0.744 | |
| H | —— | 6.117 | —— | —— | |
| P | 0.047 | 0.289 | 0.785 | 0.592 | |
| ①Full-Time | 4.78±0.663 | 2.97±0.845 | 4.09±0.583 | 3.32±1.072 | |
| Employment Type | ②Contract | 4.92±0.655 | 2.74±0.880 | 4.09±0.520 | 3.23±1.206 |
| ③Part-Time | 4.78±0.788 | 2.83±0.671 | 4.01±0.422 | 3.12±1.019 | |
| F | 0.878 | 1.432 | 0.210 | 0.314 | |
| P | 0.417 | 0.242 | 0.811 | 0.731 | |
| Position | ①Inpatient Pharmacist | 5.00±0.711 | 2.68±0.981 | 4.15±0.480 | 3.34±1.230 |
| ②Outpatient Pharmacist | 4.80±0.626 | 2.97±0.838 | 3.98±0.547 | 3.19±1.177 | |
| ③Intravenous Therapy Pharmacist | 5.37±0.919 | 2.57±0.494 | 3.91±0.449 | 3.35±1.247 | |
| ④Clinical Pharmacist | 4.62±0.612 | 2.93±0.807 | 4.17±0.561 | 3.36±0.867 | |
| ⑤Other | 4.88±0.721 | 2.86±0.746 | 4.16±0.574 | 3.24±1.123 | |
| F | 0.172 | 0.456 | 0.330 | 0.939 | |
| P | 0.070 | 0.463 | 0.269 | 0.942 | |
| Income Level | ①0-2000 | 5.26±0.842 | 2.58±1.361 | 4.30±0.428 | 3.99±1.282 |
| ②2000-4000 | 4.82±0.778 | 2.87±0.884 | 4.00±0.616 | 3.64±1.018 | |
| ③4000-6000 | 4.74±0.625 | 2.89±0.657 | 4.07±0.520 | 3.06±1.089 | |
| ④6000+ | 4.87±0.581 | 2.91±0.904 | 4.10±0.528 | 3.08±1.071 | |
| F | 0.199 | 0.882 | 0.295 | 0.008 | |
| P | 0.090 | 0.660 | 0.394 | 0.003 | |
| LSD/G-H | —— | —— | —— | ②>③# ②>④# |
|
| Hospital Level | ①Tertiary General Hospital | 4.85±0.695 | 2.84±0.833 | 4.05±0.565 | 3.34±1.028 |
| ②Tertiary specialized hospital | 4.84±0.657 | 3.23±0.916 | 4.25±0.480 | 3.31±1.406 | |
| ③Secondary General Hospital | 4.65±0.564 | 2.58±0.688 | 4.06±0.421 | 2.64±1.196 | |
| ④Secondary Specialist Hospital | 5.11±0.053 | 2.52±0.675 | 3.75±0.000 | 2.60±0.566 | |
| F | 0.001 | 0.244 | —— | 0.225 | |
| P | 0.671 | 0.064 | 0.293 | 0.094 | |
| LSD/G-H | ①<④# ③<④# |
—— | ①>④# ②>④# ③>④# |
—— |
| Project | Psychological Contract | Professional burnout | Attitudes | Behaviors |
|---|---|---|---|---|
| Psychological Contract | 1 | |||
| Professional burnout | -0.272** | 1 | ||
| Attitudes | 0.221** | -0.265** | 1 | |
| Behaviors | 0.297** | -0.088 | 0.271** | 1 |
| Model | Non-standardized coefficient | standardized coefficient | t | P | VIF | ||
|---|---|---|---|---|---|---|---|
| B | standard error | β | |||||
| Attitudes | constant | 3.774 | 0.349 | 10.820 | 0.000 | ||
| Psychological Contract | 0.147 | 0.059 | 0.182 | 2.475 | 0.014 | 1.070 | |
| Professional burnout | -0.140 | 0.047 | -0.218 | -2.959 | 0.004 | 1.070 | |
| R2FP | 0.101 9.961 0.000 |
||||||
| Behaviors | constant | 0.878 | 0.724 | 1.213 | 0.227 | ||
| Psychological Contract | 0.489 | 0.123 | 0.296 | 3.977 | 0.000 | 1.070 | |
| Professional burnout | 0.009 | 0.098 | 0.007 | 0.097 | 0.923 | 1.070 | |
| R2FP | 0.086 8.360 0.000 |
||||||
| The regression equation | The overall fit index | The significance of regression coefficients | ||||
|---|---|---|---|---|---|---|
| result variable | Predictor | R | R2 | F | β | t |
| Professional burnout | Psychological Contract | 0.2554 | 0.0652 | 12.4204 | -0.2554 | -3.5243** |
| Attitudes | Psychological Contract | 0.3181 | 0.1012 | 9.9608 | 0.1824 | 2.4753* |
| Professional burnout | -0.2181 | -2.9588** | ||||
| Behaviors | Psychological Contract | 0.2938 | 0.0863 | 8.3597 | 0.2955 | 3.9769** |
| Professional burnout | 0.0072 | 0.0966 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





