1. Introduction and Clinical Significance
Spinal hemangiomas are rare vascular lesions characterized by dilated, thin-walled capillaries prone to hemorrhage. Venous hypertension is a proposed mechanism for the development of secondary AVFs. In this case, the presence of a hemangioma may have contributed to venous congestion, potentially leading to the formation of the SDAVF.
These lesions can lead to significant neurological morbidity, with clinical presentations ranging from asymptomatic cases to severe neurological deficits such as pain, sensory disturbances, motor weakness, and bladder or bowel dysfunction [
1]. While spinal hemangiomas are typically benign, their potential for hemorrhage and mass effect on the spinal cord necessitates accurate diagnosis and timely intervention [
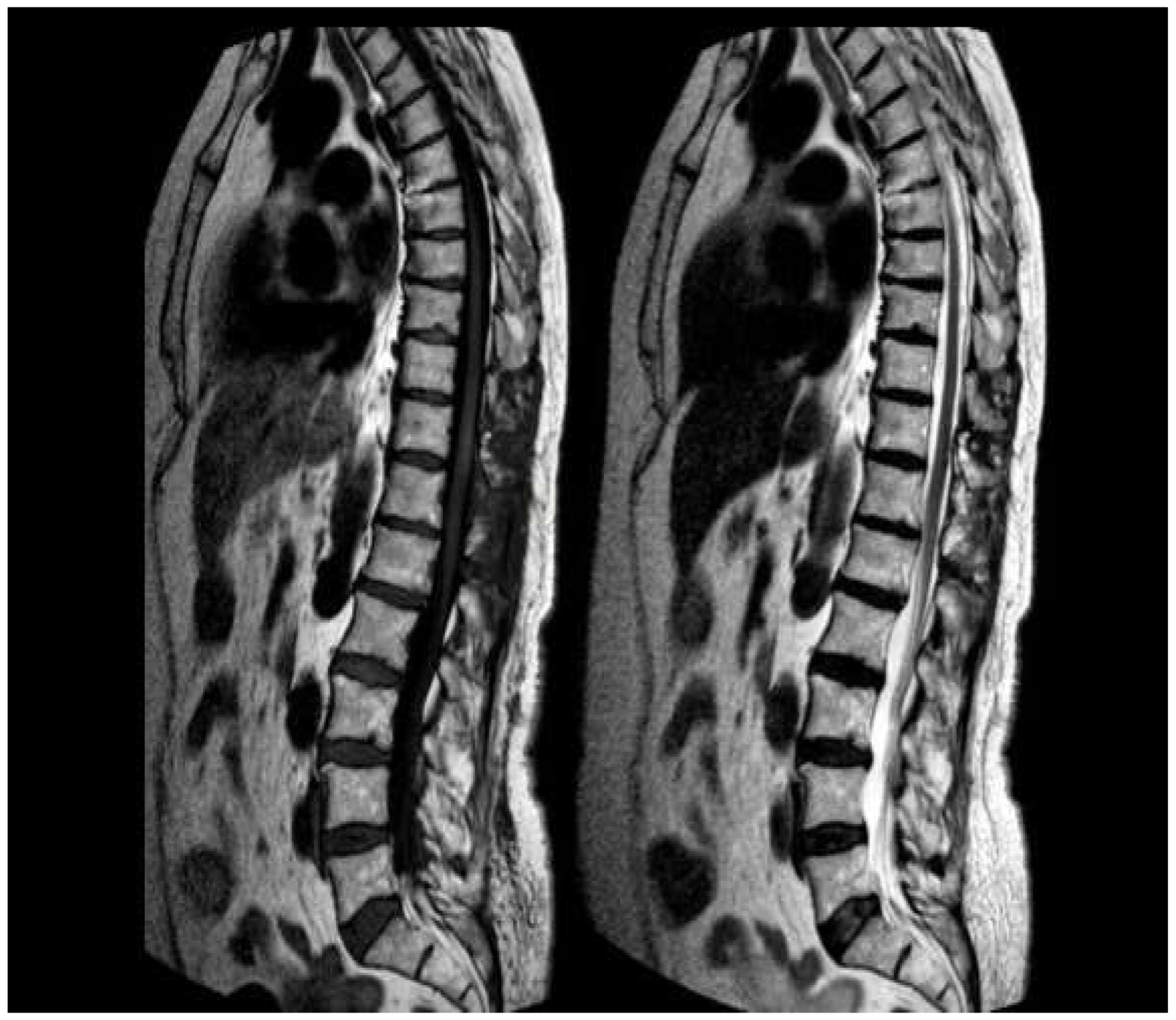
2]. Magnetic resonance imaging (MRI) has become the cornerstone of diagnostic evaluation, revealing characteristic features such as a "popcorn" appearance, mixed T1 and T2 signal intensities, and a low-signal rim on T2-weighted images [
3]. However, the role of additional imaging modalities, such as spinal angiography, in identifying associated vascular anomalies or concurrent pathologies remains an area of ongoing investigation [
4].
The co-occurrence of spinal hemangiomas with other vascular malformations, such as arteriovenous malformations (AVMs) or dural arteriovenous fistulas (dAVFs), is exceptionally rare: this case report presents an elderly woman with a spinal intradural hemangioma and a concurrent spinal dural arteriovenous fistula, a rare and diagnostically challenging combination. By reviewing the current literature on spinal hemangiomas and concurrent vascular malformations, we aim to highlight the unique aspects of these rare conditions, the diagnostic challenges they pose, and the importance of advanced imaging techniques in ensuring accurate diagnosis and effective treatment. The case underscores the risk of insufficient care if concurrent lesions are overlooked and emphasizes the need for a high index of suspicion in patients with complex spinal vascular pathologies.
2. Case Presentation
A 76-year-old woman presented with a six-month history of progressive dorsolumbar pain. Neurological examination revealed significant pain but preserved lower limb strength; bladder dysfunction was present and worsening overtime. Magnetic resonance imaging (MRI) of the thoracic spine revealed an expansive lesion at the D11 vertebral level [
Figure 1]. Neurosurgical evaluation indicated the need for surgical resection. The patient’s medical history included long QT syndrome, osteoporosis, and bilateral carpal tunnel syndrome.
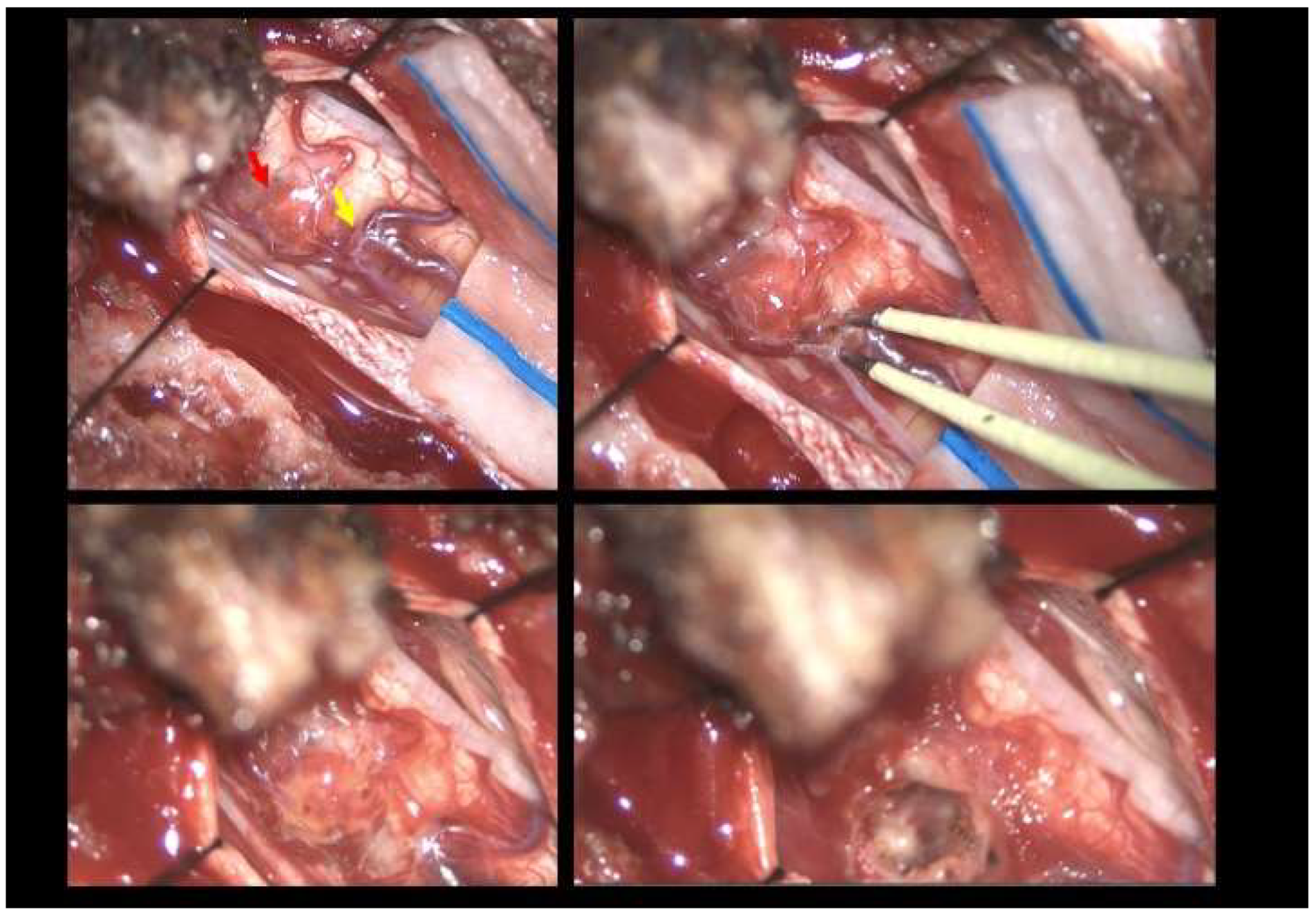
The patient underwent a laminotomy and microsurgical resection of the lesion. Intraoperatively, a vascular malformation resembling a dural arteriovenous fistula (SDAVF) was observed and sealed using bipolar cautery and scissor separation [
Figure 2]. Histopathological examination confirmed the diagnosis of hemangioma, with immunohistochemical staining positive for ERG and CD34.
Postoperatively, the patient exhibited mild lower limb weakness (MRC 4), persistent paresthesia and hypoesthesia in the left leg, and significant postvoid residual volumes requiring intermittent catheterization. A rehabilitation consultation recommended an extensive homebased rehabilitation program; the patient fully recovered with no neurological deficits after 2 months [
Figure 3].
Surgical Technique
The patient was positioned prone, and a midline incision was performed, followed by bilateral muscle dissection and laminotomy at D11-D12 using a Piezoelectric osteotome (Mectron s.p.a – Italy) [
Figure 4]. Under the operating microscope, a dural opening was made, exposing the lesion, which appeared as an exophytic protrusion from the surface of the left posterior spinal cord, surrounded by a vascular malformation with multiple arteriovenous fistulas on the pial surface [
Figure 2]. Coagulation and disconnection of the fistulas were performed first. An incision was made around the lesion, which exhibited a firm consistency. Due to the inability to remove the pathological tissue without traction, an ultrasonic aspirator was used for resection. Meticulous hemostasis was achieved. The dura mater was sutured, and the laminae were repositioned using plates and screws. Standard wound closure was performed.
3. Discussion
The co-occurrence of spinal hemangiomas with other vascular malformations, such as arteriovenous malformations (AVMs) or dural arteriovenous fistulas (dAVFs), is exceptionally rare, with only one documented case reported in the literature [
5]. This rarity poses significant diagnostic and therapeutic challenges, as the presence of concurrent lesions may complicate clinical presentation, imaging interpretation, and treatment planning. Spinal AVMs and dAVFs are abnormal vascular connections that can lead to venous hypertension, spinal cord ischemia, or hemorrhage, often presenting with progressive neurological deficits [
6]. The distinct clinical presentations and pathophysiological mechanisms of these lesions underscore the importance of a comprehensive diagnostic approach, particularly in cases where concurrent pathologies may be initially overlooked on imaging.
The diagnostic evaluation of spinal vascular malformations relies heavily on advanced imaging techniques. MRI, with its superior soft tissue contrast, is the primary screening tool, while spinal angiography remains the gold standard for definitive characterization of vascular anatomy and lesion type; in this case, the concurrent presence of a hemangioma and SDAVF posed a diagnostic challenge, necessitating a multimodal imaging approach.
[
7]. However, the identification of concurrent lesions, such as hemangiomas with AVMs or dAVFs, requires a high index of suspicion and meticulous imaging analysis. The coexistence of spinal hemangiomas and vascular malformations is exceedingly rare, with only one documented case in the literature. Spinal hemangiomas are typically benign, incidental findings, while spinal vascular malformations, such as SDAVFs and AVMs, can lead to significant neurological deficits if left untreated.
The single documented case of concurrent intradural AVM and sacral dAVF, reported by Hsu et al. (2002), highlights the diagnostic complexities and the risk of insufficient care if these lesions are neglected [
5]. In this case, the initial imaging findings were subtle, and the concurrent dAVF was only identified through detailed angiographic evaluation, underscoring the importance of thorough diagnostic workups in patients with spinal vascular lesions.
Treatment strategies for spinal hemangiomas and concurrent vascular malformations are primarily guided by the patient's clinical presentation and the lesion's characteristics. Surgical resection remains the mainstay of treatment for spinal hemangiomas and vascular malformations: is generally recommended for symptomatic cases, particularly those with evidence of hemorrhage or progressive neurological decline [
8]. Microsurgical techniques, including laminectomy and posterior approaches, have been shown to yield favorable outcomes, with studies reporting neurological improvement in 41-80% of patients [
9]. In cases of concurrent lesions, both lesions may need to be addressed surgically in the same operation to achieve optimal outcomes (5). Conservative management, including observation and serial imaging, is typically reserved for asymptomatic or non-hemorrhagic lesions, although the long-term outcomes of this approach remain less well-defined [
8]
In this case we preferred performing a laminotomy to preserve stability and the Piezoelectric osteotome to maximize safe bone removal minimizing the risk of soft tissue damaging and dural tear [
10,
11].
4. Conclusions
This case underscores the importance of thorough clinical and surgical attention in patients presenting with spinal hemangiomas and progressive neurological symptoms. A multimodal approach, combining microsurgical resection and postoperative rehabilitation, is crucial for optimizing clinical outcomes. The rare coexistence of a spinal hemangioma and SDAVF highlights the need for careful microscopic assessment in such cases in order to avoid missing additional pathology that may contribute to the clinical outcome.
Author Contributions
conceptualization, S.V. and A.I.; methodology, M.L., S.V. R.T.; formal analysis, A.M.,A.I, M.V., E.G.; data curation, M.L, A.I, R.T, S.V.; writing—original draft preparation, S.V, A.I, E.G, .; writing—review and editing, A.I, E.G., R.B, A.M.; visualization, , S.V, R.T; supervision,M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived being the procedure part of the routine care.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
data is unavailable due to privacy and ethical restrictions.
Acknowledgments
We would like to thank Stefano Bruni M.D., Department of Neuroradiology, and Edoardo Barboni, MD Department of Neurointensive care.
Conflicts of Interest
The authors declare no conflicts of interest
Abbreviations
The following abbreviations were used in this manuscript:
| SDAVF |
Spinal dural arteriovenous fistula |
| AVF |
Arteriovenous fistula |
| AVM |
Arteriovenous malformation |
| MRI |
Magnetic resonance imaging |
| DSA |
Digital subtraction angiography |
References
- Bostroem A, Thron A, Hans FJ, Krings T. Spinal vascular malformations--typical and atypical findings. Zentralbl Neurochir. 2007 Nov;68(4):205–13.
- Canavero S, Pagni CA, Duca S, Bradac GB. Spinal intramedullary cavernous angiomas: a literature meta-analysis. Surg Neurol. 1994 May;41(5):381–8.
- Sun I, Pamir MN. Spinal Cavernomas: Outcome of Surgically Treated 10 Patients. Front Neurol [Internet]. 2017 Dec 20 [cited 2025 Mar 23];8. Available from: https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2017.00672/full. [CrossRef]
- Binkert CA, Kollias SS, Valavanis A. Spinal cord vascular disease: characterization with fast three-dimensional contrast-enhanced MR angiography. AJNR Am J Neuroradiol. 1999;20(10):1785–93.
- Hsu Sw, Hsu SW, SW Hsu, Georges Rodesch, Rodesch G, Luo Cb, et al. Concomitant Conus Medullaris Arteriovenous Malformation and Sacral Dural Arteriovenous Fistula of the Filum Terminale. Interv Neuroradiol. 2002 Mar 30;8(1):47–53.
- Koch C. Spinal dural arteriovenous fistula. Curr Opin Neurol. 2006 Feb;19(1):69–75.
- Talenti G, Vitale G, Cester G, Della Puppa A, Faggin R, Causin F. Rare association between spinal dural arteriovenous fistulas and dysraphisms: Report of two cases and review of the literature with a focus on pitfalls in diagnosis and treatment. Interv Neuroradiol. 2017 Oct 1;23(5):458–64. [CrossRef]
- Fotakopoulos G, Kivelev J, Andrade-Barazarte H, Tjahjadi M, Goehre F, Hernesniemi J. Outcome in Patients with Spinal Cavernomas Presenting with Symptoms Due to Mass Effect and/or Hemorrhage: Conservative versus Surgical Management: Meta-analysis of Direct Comparison of Approach-Related Complications. World Neurosurg. 2021 Aug;152:6–18. [CrossRef]
- Steiger HJ, Turowski B, Hänggi D. Prognostic factors for the outcome of surgical and conservative treatment of symptomatic spinal cord cavernous malformations: a review of a series of 20 patients. Neurosurg Focus. 2010 Sep;29(3):E13. [CrossRef]
- Iacoangeli A, Alsagheir M, Aiudi D, Gladi M, Di Rienzo A, Esposito DP, Diab M, Naas H, Eldellaa A, Gigante A, Iacoangeli M, Alshafai NS, Luzardo G. Microendoscopic Tailored Spine Decompression as a Less-Invasive, Stability-Preserving Surgical Option to Instrumented Correction in Complex Spine Deformities: A Preliminary Multicenter Experience. World Neurosurg. 2024 Jun;186:e142-e150. Epub 2024 Mar 22. [CrossRef] [PubMed]
- Franzini A, Legnani F, Beretta E, Prada F, DiMeco F, Visintini S, Franzini A. Piezoelectric Surgery for Dorsal Spine. World Neurosurg. 2018 Jun;114:58-62. Epub 2018 Mar 10. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).