Submitted:
07 April 2025
Posted:
07 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
Eating Disorder Symptoms and Multiple Sclerosis
The Role of Neuroticism in Eating Disorders in Individuals with Multiple Sclerosis
The Mediating Role of Self-Esteem and Body Dissatisfaction
The Present Study
2. Materials and Methods
Participants and Procedure
Materials
Sociodemographic and Clinical Characteristics
Psychological Variables
Statistical Analyses
Data Inspection
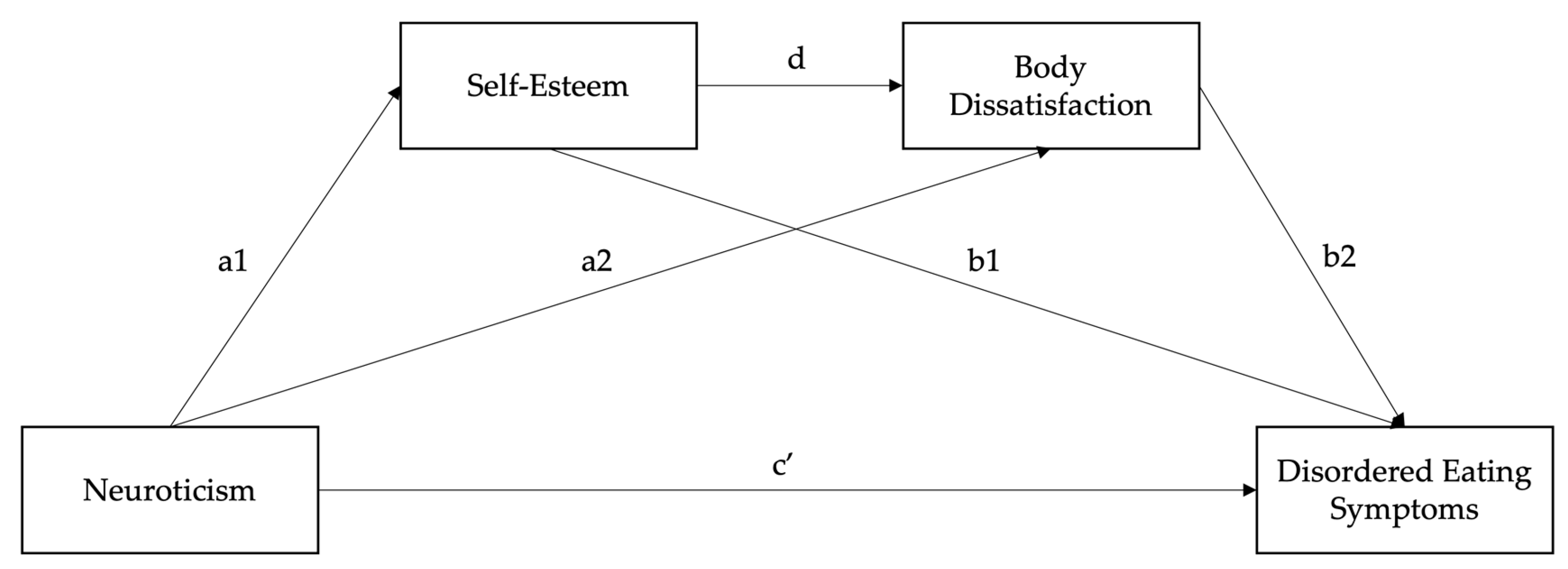
Serial Mediation Model
3. Results
Sample Characteristics
Descriptive Statistics and Correlations
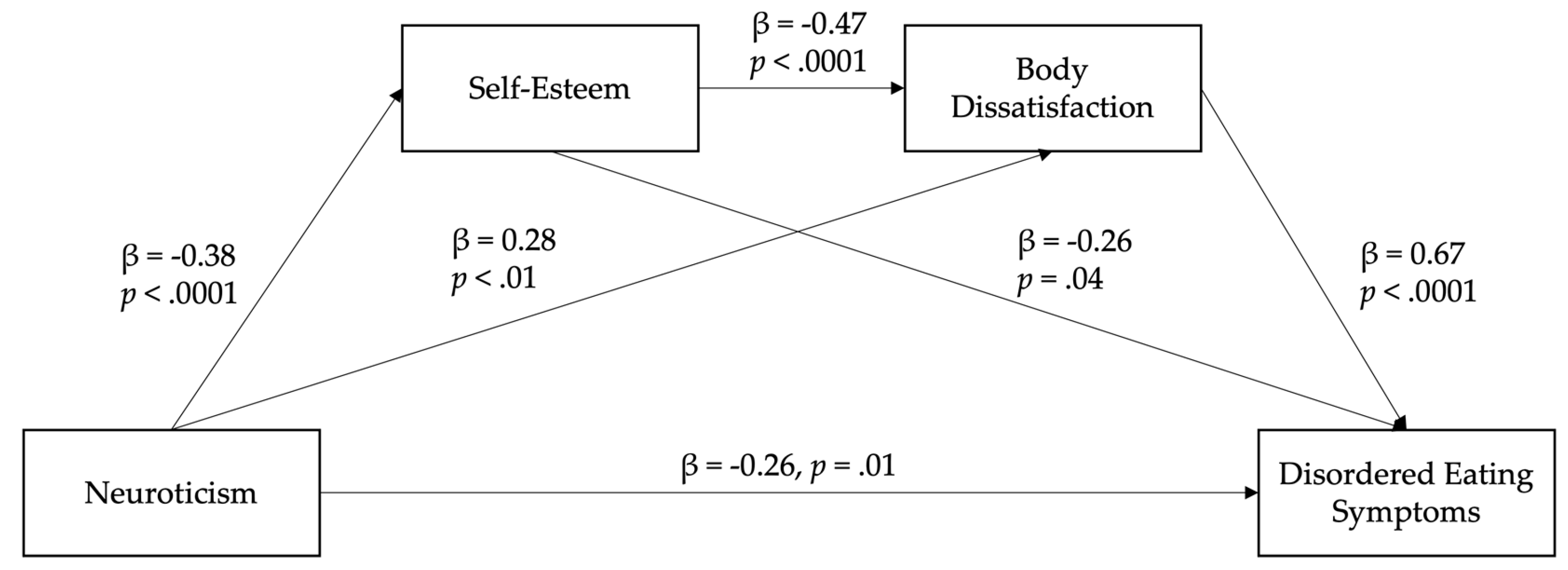
Serial Mediation Model
4. Discussion
Clinical Implications
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MS | Multiple sclerosis |
| ED | Eating disorder |
| DE | Disordered eating |
| BFI | Big Five Inventory |
| RSES | Rosenberg Self-esteem Scale |
| BSQ | Body Shape Questionnaire |
| EAT-26 | Eating Attitudes Test |
Appendix A
| Model pathway | β | SE | z | p | LL 95% CI | UL 95% CI |
| Neuroticism → Self-esteem (a1) | -0.42 (-0.46) | 0.06 | -7.17 | < .001 | -0.54 | -0.31 |
| Neuroticism → Body dissatisfaction (a2) | 0.23 (0.15) | 0.12 | 1.98 | .048 | 0.00 | 0.45 |
| Self-esteem → ED symptoms (b1) | -0.27 (-0.14) | 0.13 | -2.00 | .046 | -0.53 | -0.01 |
| Body dissatisfaction → ED symptoms (b2) | 0.68 (0.59) | 0.08 | 9.05 | < .001 | 0.53 | 0.82 |
| Self-esteem → Body dissatisfaction (d) | -0.44 (-0.27) | 0.13 | -3.36 | .001 | -0.70 | -0.18 |
| Total model effect | 0.16 (0.09) | 0.13 | 1.29 | .198 | -0.09 | 0.41 |
| Direct effect (c’) | -0.23 (-0.13) | 0.12 | -2.00 | .045 | -0.45 | -0.00 |
| Total indirect effect | 0.39 (0.23) | 0.10 | 4.12 | < .001 | 0.21 | 0.58 |
| Neuroticism → Self-esteem → ED symptoms (ind1) | 0.11 (0.07) | 0.06 | 1.92 | .054 | 0.00 | 0.23 |
| Neuroticism → Body dissatisfaction → ED symptoms (ind2) | 0.15 (0.09) | 0.08 | 1.94 | .053 | 0.00 | 0.32 |
| Neuroticism → Self-esteem → Body dissatisfaction → ED symptoms (ind3) | 0.13 (0.07) | 0.04 | 2.89 | .053 | 0.05 | 0.22 |
| Pairwise comparisons of indirect effects | ||||||
| Ind1 – Ind2 | -0.04 (-0.03) | 0.10 | -0.42 | .673 | -0.25 | 0.16 |
| Ind1 – Ind3 | -0.01 (-0.01) | 0.07 | -0.19 | .851 | -0.16 | 0.13 |
| Ind2 – Ind3 | 0.03 (0.02) | 0.10 | 0.28 | .777 | -0.18 | 0.23 |
References
- Ward, M.; Goldman, M.D. Epidemiology and pathophysiology of multiple sclerosis. Continuum (Minneap Minn) 2022, 28, 988–1005. [Google Scholar] [CrossRef] [PubMed]
- Stevens, S.D.; Thompson, N.R.; Sullivan, A.B. Prevalence and correlates of body image dissatisfaction in patients with multiple sclerosis. Int J MS Care 2019, 21, 207–213. [Google Scholar] [CrossRef]
- Glasofer, D.R.; Attia, E.; Pike, K.M. Eating disorders. In Psychopathology: From science to clinical practice, Castonguay, L.G., Oltmanns, T.F., Eds.; The Guilford Press: 2013; pp. 198-240.
- Crone, C.; Fochtmann, L.J.; Attia, E.; Boland, R.; Escobar, J.; Fornari, V.; Golden, N.; Guarda, A.; Jackson-Triche, M.; Manzo, L.; et al. The american psychiatric association practice guideline for the treatment of patients with eating disorders. Am J Psychiatry 2023, 180, 167–171. [Google Scholar] [CrossRef]
- Cassin, S.E.; von Ranson, K.M. Personality and eating disorders: A decade in review. Clin Psychol Rev 2005, 25, 895–916. [Google Scholar] [CrossRef] [PubMed]
- Farstad, S.M.; McGeown, L.M.; von Ranson, K.M. Eating disorders and personality, 2004–2016: A systematic review and meta-analysis. Clinical Psychology Review 2016, 46, 91–105. [Google Scholar] [CrossRef]
- Gilmartin, T.; Gurvich, C.; Sharp, G. The relationship between disordered eating behaviour and the five factor model personality dimensions: A systematic review. J Clin Psychol 2022, 78, 1657–1670. [Google Scholar] [CrossRef]
- Miller, J.L.; Schmidt, L.A.; Vaillancourt, T.; McDougall, P.; Laliberte, M. Neuroticism and introversion: A risky combination for disordered eating among a non-clinical sample of undergraduate women. Eat Behav 2006, 7, 69–78. [Google Scholar] [CrossRef]
- Allen, M.S.; Robson, D.A. Personality and body dissatisfaction: An updated systematic review with meta-analysis. Body Image 2020, 33, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Taylor, R.; Carvalho, C. Body dissatisfaction assessed by the photographic figure rating scale is associated with sociocultural, personality, and media influences. Scand J Psychol 2011, 52, 57–63. [Google Scholar] [CrossRef]
- Clague, C.A.; Prnjak, K.; Mitchison, D. "I don't want them to judge me": Separating out the role of fear of negative evaluation, neuroticism, and low self-esteem in eating disorders. Eat Behav 2023, 49, 101708. [Google Scholar] [CrossRef]
- Jones, H.; McIntosh, V.V.W.; Britt, E.; Carter, J.D.; Jordan, J.; Bulik, C.M. The effect of temperament and character on body dissatisfaction in women with bulimia nervosa: The role of low self-esteem and depression. Eur Eat Disord Rev 2022, 30, 388–400. [Google Scholar] [CrossRef] [PubMed]
- Skorek, M.; Song, A.V.; Dunham, Y. Self-esteem as a mediator between personality traits and body esteem: Path analyses across gender and race/ethnicity. PLoS One 2014, 9, e112086. [Google Scholar] [CrossRef] [PubMed]
- MacNeill, L.P.; Best, L.A.; Davis, L.L. The role of personality in body image dissatisfaction and disordered eating: Discrepancies between men and women. J Eat Disord 2017, 5, 44. [Google Scholar] [CrossRef]
- Cervera, S.; Lahortiga, F.; Martinez-Gonzalez, M.A.; Gual, P.; de Irala-Estevez, J.; Alonso, Y. Neuroticism and low self-esteem as risk factors for incident eating disorders in a prospective cohort study. Int J Eat Disord 2003, 33, 271–280. [Google Scholar] [CrossRef]
- Krauss, S.; Dapp, L.C.; Orth, U. The link between low self-esteem and eating disorders: A meta-analysis of longitudinal studies. Clinical Psychological Science 2023, 11, 1141–1158. [Google Scholar] [CrossRef]
- Qian, J.; Wu, Y.; Liu, F.; Zhu, Y.; Jin, H.; Zhang, H.; Wan, Y.; Li, C.; Yu, D. An update on the prevalence of eating disorders in the general population: A systematic review and meta-analysis. Eat Weight Disord 2022, 27, 415–428. [Google Scholar] [CrossRef]
- Galmiche, M.; Dechelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of eating disorders over the 2000-2018 period: A systematic literature review. Am J Clin Nutr 2019, 109, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Leon, L.; Clemente, D.; Heredia, C.; Abasolo, L. Self-esteem, self-concept, and body image of young people with rheumatic and musculoskeletal diseases: A systematic literature review. Semin Arthritis Rheum 2024, 68, 152486. [Google Scholar] [CrossRef]
- Bahrami, M.; Mohamadirizi, M.; Mohamadirizi, S.; Hosseini, S.A. Evaluation of body image in cancer patients and its association with clinical variables. J Educ Health Promot 2017, 6, 81. [Google Scholar] [CrossRef]
- Troncone, A.; Cascella, C.; Chianese, A.; Zanfardino, A.; Piscopo, A.; Borriello, A.; Casaburo, F.; Del Giudice, E.M.; Iafusco, D. Body image problems and disordered eating behaviors in italian adolescents with and without type 1 diabetes: An examination with a gender-specific body image measure. Front Psychol 2020, 11, 556520. [Google Scholar] [CrossRef]
- Gascoyne, C.R.; Simpson, S., Jr.; Chen, J.; van der Mei, I.; Marck, C.H. Modifiable factors associated with depression and anxiety in multiple sclerosis. Acta Neurol Scand 2019, 140, 204–211. [Google Scholar] [CrossRef]
- Mikula, P.; Timkova, V.; Fedicova, M.; Szilasiova, J.; Nagyova, I. Self-management, self-esteem and their associations with psychological well-being in people with multiple sclerosis. Mult Scler Relat Disord 2021, 53, 103069. [Google Scholar] [CrossRef] [PubMed]
- Kiropoulos, L.A.; Kilpatrick, T.; Holmes, A.; Threader, J. A pilot randomized controlled trial of a tailored cognitive behavioural therapy based intervention for depressive symptoms in those newly diagnosed with multiple sclerosis. BMC Psychiatry 2016, 16, 435. [Google Scholar] [CrossRef]
- Reininghaus, E.; Reininghaus, B.; Fitz, W.; Hecht, K.; Bonelli, R.M. Sexual behavior, body image, and partnership in chronic illness: A comparison of huntington's disease and multiple sclerosis. J Nerv Ment Dis 2012, 200, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Bailey, K.A.; Dagenais, M.; Gammage, K.L. Is a picture worth a thousand words? Using photo-elicitation to study body image in middle-to-older age women with and without multiple sclerosis. Qual Health Res 2021, 31, 1542–1554. [Google Scholar] [CrossRef]
- Pfaffenberger, N.; Gutweniger, S.; Kopp, M.; Seeber, B.; Sturz, K.; Berger, T.; Gunther, V. Impaired body image in patients with multiple sclerosis. Acta Neurol Scand 2011, 124, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Matusik, E.; Durmala, J.; Ksciuk, B.; Matusik, P. Body composition in multiple sclerosis patients and its relationship to the disability level, disease duration and glucocorticoid therapy. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Taul-Madsen, L.; Connolly, L.; Dennett, R.; Freeman, J.; Dalgas, U.; Hvid, L.G. Is aerobic or resistance training the most effective exercise modality for improving lower extremity physical function and perceived fatigue in people with multiple sclerosis? A systematic review and meta-analysis. Arch Phys Med Rehabil 2021, 102, 2032–2048. [Google Scholar] [CrossRef]
- Jagannath, V.A.; Filippini, G.; Di Pietrantonj, C.; Asokan, G.V.; Robak, E.W.; Whamond, L.; Robinson, S.A. Vitamin d for the management of multiple sclerosis. Cochrane Database Syst Rev 2018, 9, CD008422. [Google Scholar] [CrossRef]
- Parks, N.E.; Jackson-Tarlton, C.S.; Vacchi, L.; Merdad, R.; Johnston, B.C. Dietary interventions for multiple sclerosis-related outcomes. Cochrane Database Syst Rev 2020, 5, CD004192. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T. The neo personality inventory: Using the five-factor modei in counseling. Journal of Counseling & Development 2011, 69, 367–372. [Google Scholar] [CrossRef]
- Roy, S.; Drake, A.S.; Eizaguirre, M.B.; Zivadinov, R.; Weinstock-Guttman, B.; Chapman, B.P.; Benedict, R.H. Trait neuroticism, extraversion, and conscientiousness in multiple sclerosis: Link to cognitive impairment? Mult Scler 2018, 24, 205–213. [Google Scholar] [CrossRef]
- Maggio, M.G.; Cuzzola, M.F.; Latella, D.; Impellizzeri, F.; Todaro, A.; Rao, G.; Manuli, A.; Calabro, R.S. How personality traits affect functional outcomes in patients with multiple sclerosis: A scoping review on a poorly understood topic. Mult Scler Relat Disord 2020, 46, 102560. [Google Scholar] [CrossRef] [PubMed]
- Thomson, W. Depression, neuroticism, and the discrepancy between actual and ideal self-perception. Personality and Individual Differences 2016, 88, 219–224. [Google Scholar] [CrossRef]
- Uliaszek, A.A.; Zinbarg, R.E.; Mineka, S.; Craske, M.G.; Sutton, J.M.; Griffith, J.W.; Rose, R.; Waters, A.; Hammen, C. The role of neuroticism and extraversion in the stress-anxiety and stress-depression relationships. Anxiety Stress Coping 2010, 23, 363–381. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive behaviour therapy for eating disorders: A "transdiagnostic" theory and treatment. Behav Res Ther 2003, 41, 509–528. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.; Rieger, E.; Byrne, D. A longitudinal investigation of the mediating role of self-esteem and body importance in the relationship between stress and body dissatisfaction in adolescent females and males. Body Image 2013, 10, 544–551. [Google Scholar] [CrossRef]
- Brechan, I.; Kvalem, I.L. Relationship between body dissatisfaction and disordered eating: Mediating role of self-esteem and depression. Eat Behav 2015, 17, 49–58. [Google Scholar] [CrossRef]
- Cruz-Saez, S.; Pascual, A.; Wlodarczyk, A.; Echeburua, E. The effect of body dissatisfaction on disordered eating: The mediating role of self-esteem and negative affect in male and female adolescents. J Health Psychol 2020, 25, 1098–1108. [Google Scholar] [CrossRef]
- McCabe, M.P. Mood and self-esteem of persons with multiple sclerosis following an exacerbation. J Psychosom Res 2005, 59, 161–166. [Google Scholar] [CrossRef]
- Mikula, P.; Nagyova, I.; Krokavcova, M.; Vitkova, M.; Rosenberger, J.; Szilasiova, J.; Gdovinova, Z.; Stewart, R.E.; Groothoff, J.W.; van Dijk, J.P. Self-esteem, social participation, and quality of life in patients with multiple sclerosis. J Health Psychol 2017, 22, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, M.; Salmen, A.; Barin, L.; Puhan, M.A.; Calabrese, P.; Kamm, C.P.; Gobbi, C.; Kuhle, J.; Manjaly, Z.M.; Ajdacic-Gross, V.; et al. Development and validation of the self-reported disability status scale (srdss) to estimate edss-categories. Mult Scler Relat Disord 2020, 42, 102148. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (edss). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef]
- John, O.P.; Srivastava, S. The big-five trait taxonomy: History, measurement, and theoretical perspectives. In Handbook of personality: Theory and research; Guilford Press: New York, 1999; Volume 2, pp. 102–138. [Google Scholar]
- Costa Mastrascusa, R.; de Oliveira Fenili Antunes, M.L.; de Albuquerque, N.S.; Virissimo, S.L.; Foletto Moura, M.; Vieira Marques Motta, B.; de Lara Machado, W.; Moret-Tatay, C.; Quarti Irigaray, T. Evaluating the complete (44-item), short (20-item) and ultra-short (10-item) versions of the big five inventory (bfi) in the brazilian population. Sci Rep 2023, 13, 7372. [Google Scholar] [CrossRef]
- Rosenberg, M. Rosenberg self-esteem scale (rses). Available online: https://www.apa.org/obesity-guideline/rosenberg-self-esteem.pdf (accessed on 3 January).
- Cooper, P.; Taylor, M.; Cooper, Z.; Fairburn, C.G. The development and validation of the body shape questionnaire. Int J Eat Disord 1987, 6, 485–494. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychol Med 1982, 12, 871–878. [Google Scholar] [CrossRef]
- Papini, N.M.; Jung, M.; Cook, A.; Lopez, N.V.; Ptomey, L.T.; Herrmann, S.D.; Kang, M. Psychometric properties of the 26-item eating attitudes test (eat-26): An application of rasch analysis. J Eat Disord 2022, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A language and environment for statistical computing. 2024.
- Schoemann, A.M.; Moore, E.W.G.; Yagiz, G. How and why to follow best practices for testing mediation models with missing data. Int J Psychol 2025, 60, e13257. [Google Scholar] [CrossRef]
- Austin, P.C.; White, I.R.; Lee, D.S.; van Buuren, S. Missing data in clinical research: A tutorial on multiple imputation. Can J Cardiol 2021, 37, 1322–1331. [Google Scholar] [CrossRef]
- Buuren, S.v.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in r. J Stat Softw 2011, 45. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple imputation for nonresponse in surveys; John Wiley & Sons, Inc.: 1987.
- Rosseel, Y. Lavaan: An r package for structural equation modeling. J Stat Softw 2012, 48. [Google Scholar] [CrossRef]
- Jorgensen, T. Lavaan.Mi: Fit structural equation models to multiply imputed data. Available online: https://CRAN.R-project.org/package=lavaan.
- Jorgensen, T.; Pornprasertmanit, S.; Schoemann, A.M.; Rosseel, Y. Semtools: Useful tools for structural equation modeling. Available online: https://CRAN.R-project.org/package=semTools (accessed on 15 March).
- Rohde, P.; Stice, E.; Shaw, H.; Gau, J.M.; Ohls, O.C. Age effects in eating disorder baseline risk factors and prevention intervention effects. Int J Eat Disord 2017, 50, 1273–1280. [Google Scholar] [CrossRef]
- Lo Buono, V.; Bonanno, L.; Corallo, F.; Cardile, D.; D'Aleo, G.; Rifici, C.; Sessa, E.; Quartarone, A.; De Cola, M.C. The relationship between body image, disability and mental health in patients with multiple sclerosis. J Clin Med 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Sim, M.; Kim, S.Y.; Suh, Y. Sample size requirements for simple and complex mediation models. Educ Psychol Meas 2022, 82, 76–106. [Google Scholar] [CrossRef]
- Claes, L.; Vandereycken, W.; Luyten, P.; Soenens, B.; Pieters, G.; Vertommen, H. Personality prototypes in eating disorders based on the big five model. J Pers Disord 2006, 20, 401–416. [Google Scholar] [CrossRef]
- Clarke, E.; Kiropoulos, L.A. Mediating the relationship between neuroticism and depressive, anxiety and eating disorder symptoms: The role of intolerance of uncertainty and cognitive flexibility. Journal of Affective Disorders Reports 2021, 4. [Google Scholar] [CrossRef]
- Dingemans, A.; Danner, U.; Parks, M. Emotion regulation in binge eating disorder: A review. Nutrients 2017, 9. [Google Scholar] [CrossRef]
- Mattingley, S.; Youssef, G.J.; Manning, V.; Graeme, L.; Hall, K. Distress tolerance across substance use, eating, and borderline personality disorders: A meta-analysis. J Affect Disord 2022, 300, 492–504. [Google Scholar] [CrossRef]
- Friedman, H.S. Long-term relations of personality and health: Dynamisms, mechanisms, tropisms. J Pers 2000, 68, 1089–1107. [Google Scholar] [CrossRef]
- Friedman, H.S. Neuroticism and health as individuals age. Personal Disord 2019, 10, 25–32. [Google Scholar] [CrossRef]
- Weston, S.J.; Jackson, J.J. The role of vigilance in the relationship between neuroticism and health: A registered report. J Res Pers 2018, 73, 27–34. [Google Scholar] [CrossRef]
- Graham, E.K.; Weston, S.J.; Turiano, N.A.; Aschwanden, D.; Booth, T.; Harrison, F.; James, B.D.; Lewis, N.A.; Makkar, S.R.; Mueller, S.; et al. Is healthy neuroticism associated with health behaviors? A coordinated integrative data analysis. Collabra Psychol 2020, 6. [Google Scholar] [CrossRef]
- Weston, S.J.; Jackson, J.J. Identification of the healthy neurotic: Personality traits predict smoking after disease onset. Journal of Research in Personality 2015, 54, 61–69. [Google Scholar] [CrossRef]
- Turiano, N.A.; Whiteman, S.D.; Hampson, S.E.; Roberts, B.W.; Mroczek, D.K. Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. J Res Pers 2012, 46, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Turiano, N.A.; Mroczek, D.K.; Moynihan, J.; Chapman, B.P. Big 5 personality traits and interleukin-6: Evidence for "healthy neuroticism" in a us population sample. Brain Behav Immun 2013, 28, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Stieger, M.; Robinson, S.A.; Bisson, A.N.; Lachman, M.E. The relationship of personality and behavior change in a physical activity intervention: The role of conscientiousness and healthy neuroticism. Pers Individ Dif 2020, 166. [Google Scholar] [CrossRef]
- Arend, I.; Yuen, K. Association between healthy neuroticism and eating behavior as revealed by the nki rockland sample. Sci Rep 2025, 15, 5858. [Google Scholar] [CrossRef]
- Morgan, J.F.; Reid, F.; Lacey, J.H. The scoff questionnaire: A new screening tool for eating disorders. West J Med 2000, 172, 164–165. [Google Scholar] [CrossRef]
- Tesar, N.; Baumhackl, U.; Kopp, M.; Gunther, V. Effects of psychological group therapy in patients with multiple sclerosis. Acta Neurol Scand 2003, 107, 394–399. [Google Scholar] [CrossRef]
- Paolucci, T.; de Sire, A.; Agostini, F.; Bernetti, A.; Salome, A.; Altieri, M.; Di Piero, V.; Ammendolia, A.; Mangone, M.; Paoloni, M. Efficacy of interoceptive and embodied rehabilitative training protocol in patients with mild multiple sclerosis: A randomized controlled trial. Front Neurol 2022, 13, 1095180. [Google Scholar] [CrossRef]
- McCormack, D.; O'Keeffe, D.F.; Seery, C.; Eccles, D.F. The association between body image and psychological outcomes in multiple sclerosis. A systematic review. Mult Scler Relat Disord 2025, 93, 106226. [Google Scholar] [CrossRef]
- Bogosian, A.; Hughes, A.; Norton, S.; Silber, E.; Moss-Morris, R. Potential treatment mechanisms in a mindfulness-based intervention for people with progressive multiple sclerosis. Br J Health Psychol 2016, 21, 859–880. [Google Scholar] [CrossRef] [PubMed]
- Simpson, R.; Mair, F.S.; Mercer, S.W. Mindfulness-based stress reduction for people with multiple sclerosis - a feasibility randomised controlled trial. BMC Neurol 2017, 17, 94. [Google Scholar] [CrossRef]
- Hocaloski, S.; Elliott, S.; Brotto, L.A.; Breckon, E.; McBride, K. A mindfulness psychoeducational group intervention targeting sexual adjustment for women with multiple sclerosis and spinal cord injury: A pilot study. Sexuality and Disability 2016, 34, 183–198. [Google Scholar] [CrossRef]
- Wills, O.; Probst, Y.; Haartsen, J.; McMahon, A.T. The role of multidisciplinary ms care teams in supporting lifestyle behaviour changes to optimise brain health among people living with ms: A qualitative exploration of clinician perspectives. Health Expect 2024, 27, e14042. [Google Scholar] [CrossRef]
- Saul, A.; Taylor, B.V.; Blizzard, L.; Simpson-Yap, S.; Oddy, W.H.; Probst, Y.C.; Black, L.J.; Ponsonby, A.L.; Broadley, S.A.; Lechner-Scott, J.; et al. Associations between diet quality and depression, anxiety, and fatigue in multiple sclerosis. Mult Scler Relat Disord 2022, 63, 103910. [Google Scholar] [CrossRef] [PubMed]
- Hanna, M.; Strober, L.B. Anxiety and depression in multiple sclerosis (ms): Antecedents, consequences, and differential impact on well-being and quality of life. Mult Scler Relat Disord 2020, 44, 102261. [Google Scholar] [CrossRef]
- Hamaker, E.L.; Kuiper, R.M.; Grasman, R.P. A critique of the cross-lagged panel model. Psychol Methods 2015, 20, 102–116. [Google Scholar] [CrossRef]
| Demographic | N (%) |
| Gender | |
| Male | 55 (20.0%) |
| Female | 218 (79.3%) |
| Non-binary | 2 (< 1.0%) |
| Ethnicity | |
| Anglo-Celtic | 211 (76.7%) |
| Asian (Eastern, Southern, Southeastern) | 8 (2.9%) |
| Indigenous Australian and/or Torres Strait Islander | 12 (4.4%) |
| Hispanic or Latin American | 4 (1.5%) |
| Middle Eastern | 3 (1.1%) |
| African American | 22 (8.0%) |
| Other | 15 (5.5%) |
| Country of current residence | |
| Australia | 145 (52.7%) |
| New Zealand | 6 (2.2%) |
| UK | 14 (5.1%) |
| USA | 88 (32.0%) |
| Other | 22 (8.0%) |
| Highest level of education | |
| Postgraduate | 51 (18.6%) |
| Bachelor’s degree | 76 (27.6%) |
| Year 12 (high school) or equivalent | 38 (13.8%) |
| Diploma or certificate level | 103 (37.5%) |
| Below high school | 7 (2.6%) |
| Relationship status | |
| Married | 173 (62.9%) |
| Partnered/De facto | 13 (4.7%) |
| Single/Never married | 38 (13.8%) |
| Divorced/Widowed/Separated | 51 (18.6%) |
| Employment status | |
| Full-time | 110 (40.0%) |
| Part-time/Casual | 73 (26.6%) |
| Unemployed | 92 (33.5%) |
| MS type | |
| Relapsing-remitting | 185 (68.3%) |
| Progressive (primary or secondary) | 80 (29.1%) |
| Other/Not sure | 10 (3.6%) |
| MS relapses in the past 12 months | |
| None | 129 (46.9%) |
| 1 to 3 | 119 (43.3%) |
| More than 3 | 27 (9.8%) |
| Current MS relapse at the time of survey | |
| Yes | 75 (27.3%) |
| No | 200 (72.7%) |
| Current disease-modifying treatment/s | |
| Yes | 185 (67.3%) |
| No | 90 (32.7%) |
| Level of ambulation | |
| SRDSS < 3.5 | 117 (42.5%) |
| SRDSS 4 to 6.5 | 94 (34.2%) |
| SRDSS > 7 | 18 (6.6%) |
| Missing | 46 (16.7%) |
| Diagnosis | N (% sample) |
| Depressive disorder diagnosis | |
| Total | 147 (53.5%) |
| Current | 104 (37.8%) |
| Recovered/lifetime | 43 (15.6%) |
| Anxiety disorder diagnosis | |
| Total | 130 (47.3%) |
| Current | 114 (41.5%) |
| Recovered/lifetime | 16 (5.8%) |
| Eating disorder diagnosis | |
| Total | 58 (21.1%) |
| Current | 39 (14.2%) |
| Recovered/lifetime | 19 (6.9%) |
| Depressive disorder typea | |
| Major depressive disorder (incl. post-natal depression) | 52 (18.9%) |
| Persistent depressive disorder | 42 (10.4%) |
| Premenstrual dysphoric disorder | 7 (1.7%) |
| Not sure/other | 55 (13.6%) |
| Anxiety disorder typea | |
| Generalised anxiety disorder (GAD) | 73 (26.6%) |
| Panic disorder | 16 (5.8%) |
| Agoraphobia | 3 (1.1%) |
| Specific phobia | 7 (2.6%) |
| Social anxiety disorder | 33 (12.0%) |
| Health/illness anxiety | 7 (2.6%) |
| Separation anxiety disorder | 13 (4.7%) |
| Not sure/other | 10 (3.6%) |
| Eating disorder typea | |
| Anorexia nervosa (restricting and binge/purging) | 34 (12.4%) |
| Bulimia nervosa (purging and non-purging) | 26 (9.5%) |
| Binge eating disorder | 4 (1.5%) |
| Currently taking antidepressant or anti-anxiety medication | |
| Yes | 132 (48.0%) |
| No | 143 (52.0%) |
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 1.Neuroticism (BFI) | 24.87 | 6.56 | – | ||||||
| 2.Self-esteem (RSES) | 13.87 | 5.69 | -0.50** | – | |||||
| 3.Body dissatisfaction (BSQ) | 24.73 | 9.55 | 0.37** | -0.43** | – | ||||
| 4.DE symptoms (EAT-26) | 13.86 | 11.22 | 0.14* | -0.37** | 0.57** | – | |||
| 5.Age (years) | 43.03 | 12.88 | -0.18** | 0.40** | -0.23** | -0.36** | – | ||
| 6.BMI | 29.13 | 11.38 | 0.00 | -0.13 | 0.19** | -0.06 | -0.01 | – | |
| 7.Ambulation level (SRDSS) | - | - | -0.09 | 0.03 | 0.01 | -0.09 | 0.25** | 0.02 | – |
| Model pathway | β | SE | t | p | LL 95% CI | UL 95% CI |
| Neuroticism → Self-esteem (a1) | -0.38 (-0.44) | 0.05 | -7.88 | < .001 | -0.01 | 0.20 |
| Neuroticism → Body dissatisfaction (a2) | 0.28 (0.19) | 0.10 | 2.83 | .005 | 0.09 | 0.47 |
| Self-esteem → DE symptoms (b1) | -0.26 (-0.13) | 0.13 | -2.06 | .039 | -0.46 | -0.05 |
| Body dissatisfaction → DE symptoms (b2) | 0.67 (0.57) | 0.07 | 9.76 | < .001 | 0.53 | 0.80 |
| Self-esteem → Body dissatisfaction (d) | -0.47 (-0.27) | 0.12 | -3.90 | < .001 | -0.70 | -0.23 |
| Total model effect | 0.15 (0.09) | 0.11 | 1.36 | .173 | -0.07 | 0.37 |
| Direct effect (c’) | -0.26 (-0.15) | 0.10 | -2.49 | .013 | -0.46 | -0.05 |
| Total indirect effect | 0.40 (0.22) | 0.08 | 5.06 | < .001 | 0.25 | 0.57 |
| Neuroticism → Self-esteem → DE symptoms (Ind1) | 0.10 (0.06) | 0.05 | 1.98 | .048 | 0.01 | 0.20 |
| Neuroticism → Body dissatisfaction → DE symptoms (Ind2) | 0.18 (0.11) | 0.07 | 2.74 | .006 | 0.06 | 0.33 |
| Neuroticism → Self-esteem → Body dissatisfaction → DE symptoms (Ind3) | 0.12 (0.07) | 0.04 | 2.99 | .003 | 0.05 | 0.20 |
| Pairwise comparisons of indirect effects | ||||||
| Ind1 – Ind2 | -0.09 (-0.05) | 0.09 | -0.98 | .326 | -0.26 | 0.09 |
| Ind1 – Ind3 | -0.02 (-0.01) | 0.06 | -0.29 | .774 | -0.15 | 0.11 |
| Ind2 – Ind3 | 0.07 (0.04) | 0.09 | 0.77 | .440 | -0.10 | 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





