Submitted:
22 April 2025
Posted:
22 April 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Protocol Architecture
- Core Protocol Layer: DICOM extension with JWT and watermarking
- Middleware Layer: Smart contract execution and authentication workflows
- Application Layer: Dashboard, researcher portal, and patient interface
2.2. Blockchain Logging Mechanism
- User identity (via DID)
- Purpose of export
- Timestamp
- Patient anonymized ID
- Export destination and access policy
2.3. Anonymization Workflow
- Images are processed with the following steps:
- Metadata sanitization
- Facial structure blurring (if applicable)
- Private tag embedding of JWT
- Optional overlay logo placement
2.4. Authentication Stack
- Step 1: Password/SSO (OpenID Connect)
- Step 2: e-signature (certificate + PIN)
- Step 3: Biometric or mobile-based MFA (WebAuthn)
3. Results (Simulated)
3.1. Simulated Use Case: Academic Conference Export
- Researcher uploads a request for export
- System prompts purpose and executes MFA
- Image is anonymized, signed, and watermarked
- Export is logged to blockchain and receipt issued
3.2. Performance Estimate (Benchmark on test server)
- Export process time: <4.2s/image (with full stack)
- Blockchain write latency: <300ms
- JWT extraction success rate: 100% on conformant viewers
4. Discussion
4.1. Related International Initiatives
- Off-chain storage for image data
- Blockchain-based access control ledgers
- Token-based authentication through image metadata
- Clear JWT integration for traceability
- Enhanced interoperability with existing DICOM systems
- Web3.0-native features such as Decentralized Identity (DID) and Smart Contracts
4.2. Reconsidering On-Premise vs. Cloud in the Web3.0 Era
- Token-gated access: Without possession of a valid cryptographic token, intercepted image data is unusable.
- Immutable audit logs: Unauthorized data access or exfiltration is automatically recorded and provable.
- Encryption at rest and in transit: Even in cases of interception, meaningful data is protected by strong cryptographic safeguards.
5. Author's Perspective
6. Future Directions
6.1. Feature Extraction Platform for AI Research
- Allow researchers to extract features from medical images without moving or accessing the raw image data
- Implement federated learning approaches where AI models train across distributed datasets while the data remains at its source
- Apply differential privacy techniques to add statistical noise that protects individual privacy while preserving population-level insights
- Create standardized feature catalogs that researchers can search without compromising patient identities
6.2. Advanced Data Governance and Patient Sovereignty
- Dynamic consent management where patients can modify their data sharing preferences over time
- Granular permission controls that distinguish between clinical use, research, commercial applications, and educational purposes
- Token-based incentive systems that reward patients for contributing their anonymized data to research
- Self-sovereign identity integration allowing patients to control their medical identity across healthcare systems
6.3. Cross-Domain Applications
- Financial sector: Secure document handling with verifiable audit trails
- Public administration: Tamper-proof recording of official document access
- Manufacturing: Tracking intellectual property and design documents
- Legal services: Chain of custody for evidence and confidential documentation
6.4. Data Marketplace and Research Collaboration Platform
- Metadata catalogs allowing researchers to discover relevant datasets while preserving privacy
- Smart contract-based data use agreements automatically enforcing terms and conditions
- Attribution and citation tracking ensuring proper credit for data contributions
- Cross-institutional collaboration frameworks with automated regulatory compliance
6.5. Integration with Emerging Technologies
- Zero-knowledge proofs: Enabling verification of data properties without revealing the data itself
- Multi-party computation: Allowing analysis across multiple datasets without exposing the underlying data
- Homomorphic encryption: Performing computations on encrypted data without decryption
- Quantum-resistant cryptography: Ensuring long-term security as quantum computing advances
6.6. Standardization and Global Adoption
- Formal specification submissions to standards bodies like DICOM Committee, HL7, ISO, or W3C
- Reference implementations demonstrating interoperability across vendor systems
- Conformance testing frameworks to verify implementations
- Educational programs for implementation and adoption
6.7. Implementation Roadmap and Scaling Strategy
- Reference Implementation: A baseline implementation in Rust for the core protocol layer, prioritizing security and performance
- Proof of Concept: Small-scale deployment in a controlled environment (e.g., single department within a research hospital)
- Developer Documentation: Initial API documentation and implementation guidelines
- Test Suite: Comprehensive security and conformance testing framework
- Multi-Site Pilot: Implementation across 3-5 partner institutions with varied use cases (research, clinical, educational)
- Interoperability Testing: Integration with at least two major PACS vendors and standalone DICOM viewers
- Performance Benchmarking: Stress testing with realistic volumes (10,000+ images per day) to identify scalability bottlenecks
- Security Audit: Independent third-party security validation and penetration testing
- User Experience Refinement: Iterative improvement based on clinician and researcher feedback
- SDK Development: Software development kits for multiple languages (JavaScript, Python, Java, Swift)
- Plugin Architecture: Extensibility framework allowing third-party developers to add capability modules
- Integration APIs: Standardized APIs for EMR, PACS, VNA, and cloud storage systems
- Community Building: Open-source reference implementations and developer community engagement
- Adoption Incentives: Programs to encourage institutional adoption (e.g., compliance certification, implementation grants)
- Regional Scaling: Country or region-wide implementations, targeting healthcare systems with centralized governance first
- Regulatory Alignment: Formal recognition by healthcare regulatory bodies as a compliant security approach
- Standards Submission: Submission to formal standards bodies (DICOM Committee, ISO, W3C)
- Global Interoperability: Cross-border exchange protocols and international governance frameworks
- Training and Certification: Professional certification programs for implementation specialists
- Blockchain Scalability: As transaction volume grows, the architecture must adapt without performance degradation, potentially through sharding, sidechains, or optimized consensus mechanisms
- Computational Overhead: Multi-factor authentication and JWT processing must maintain performance at scale, requiring edge computing approaches for latency-sensitive environments
- Storage Optimization: While blockchain stores only metadata, the audit log will grow continuously, requiring efficient pruning and archiving strategies
- Network Effects: Value increases as more institutions participate, creating a positive feedback loop once critical mass is achieved
- Legacy Integration: Complete replacement of existing systems is unrealistic; BISHOP must coexist and gradually augment rather than replace established workflows
- Training Requirements: Healthcare staff must understand enough about the system to trust and effectively use it without requiring cryptography expertise
- Cost Distribution: Implementation costs must be fairly distributed among stakeholders (healthcare providers, researchers, technology vendors)
- Sustainable Maintenance: Long-term protocol governance and maintenance requires sustainable funding mechanisms
- Validated ROI: Clear demonstration of return on investment through quantifiable metrics (reduced breach risk, compliance costs, research acceleration)
6.8. Toward a Comprehensive Bohr Protocol Suite: The Seven Pillars
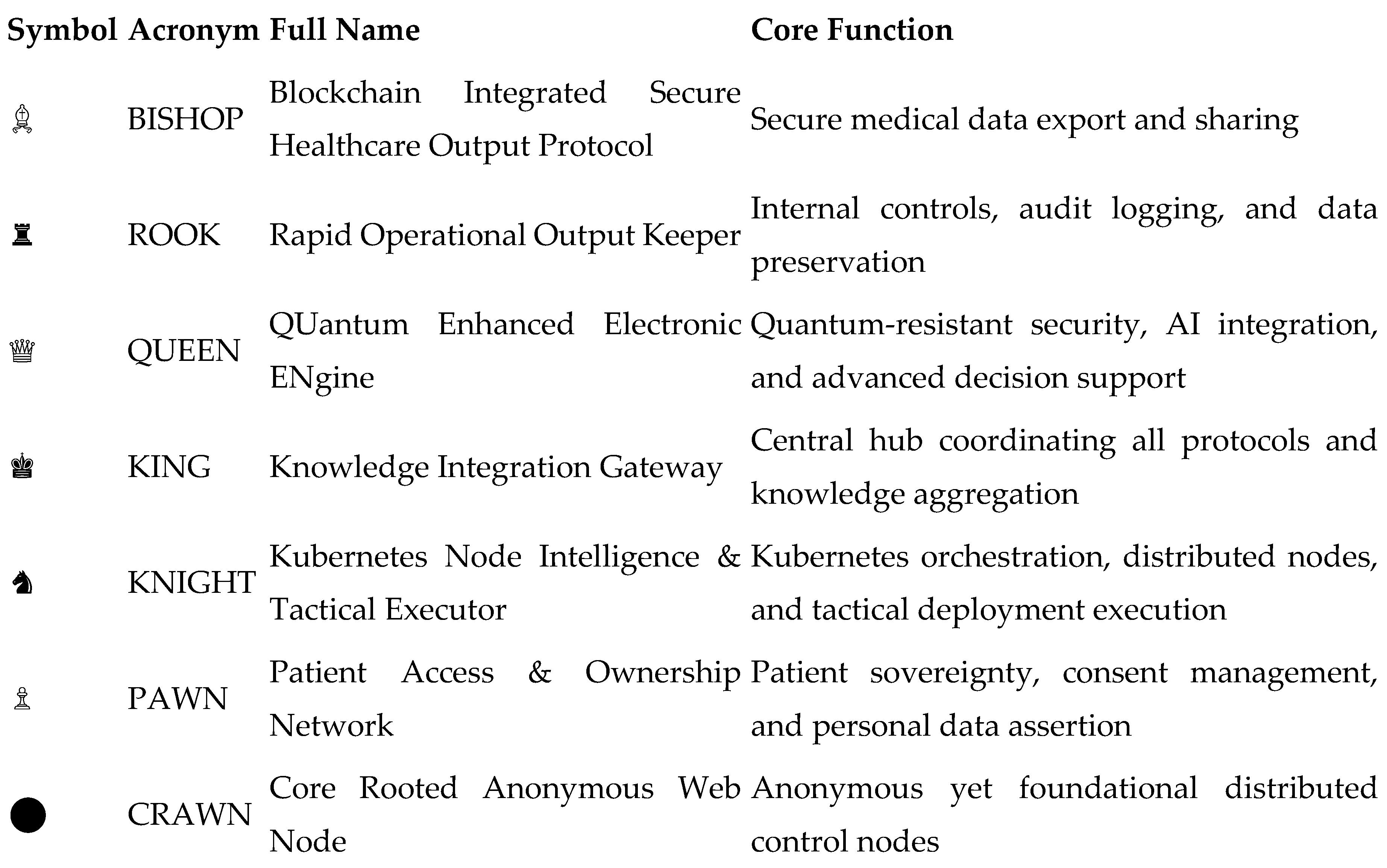
- ROOK would extend BISHOP's capabilities with enhanced operational controls and long-term data preservation strategies, ensuring both regulatory compliance and historical data integrity. The linear movement characteristic of the rook chess piece reflects the direct, unambiguous nature of audit trails and compliance verification.
- PAWN would focus on the critical aspect of patient agency, creating mechanisms for patients to directly control, monitor, and authorize the use of their medical data. Like chess pawns that can be promoted to more powerful pieces, PAWN empowers patients to transform from passive data subjects to active participants in their healthcare data journey.
- KNIGHT would address the deployment architecture, leveraging Kubernetes and modern container orchestration to enable flexible, scalable implementations across varied healthcare environments. The knight's unique movement pattern in chess parallels the protocol's ability to navigate complex infrastructure constraints.
- QUEEN, KING, and CRAWN represent future advanced components that would be developed as the ecosystem matures and as quantum computing, advanced AI, and fully decentralized architectures become more critical to healthcare data security.
- This modular approach allows healthcare institutions to begin with BISHOP—addressing the immediate security needs around medical imaging—while preparing for a more comprehensive implementation as resources and organizational readiness permit. The chess metaphor is not merely decorative but serves to illustrate how these components work together strategically, each with defined movements and capabilities, collectively protecting the most valuable pieces on the board: patient data and privacy.
- While the full realization of the Bohr Protocol Suite remains a future goal, the development of BISHOP represents the critical first step toward this more comprehensive vision of healthcare data security and sovereignty in the Web3.0 era.
7. Security Considerations
7.1. Current Challenges in Medical Imaging Security
- Lack of Traceability: There is no tracking mechanism for images once they are exported and used outside the system. This creates the "boomerang image" problem, where anonymized images reused in different contexts cannot be traced back to their original source.
- Insufficient Tamper Detection Mechanisms: DICOM image metadata can be relatively easily edited, and there is no standardized mechanism to detect tampering. This poses serious problems in clinical, legal, and research contexts.
- Fragmented Access Logs: Records of image access and manipulation are maintained only within central systems, making consistent log tracking across different systems difficult.
- Non-uniform Encryption Standards: While DICOM supports encryption, its implementation is optional, and the choice of cryptographic algorithms depends on the implementation.
7.2. Impact of Quantum Computing on Cryptographic Technologies
- Threat to Asymmetric Cryptography: Shor's algorithm, which can be executed on quantum computers, could potentially decrypt RSA and Elliptic Curve Cryptography (ECC)—the primary algorithms used for JWT signatures in BISHOP.
- Impact on Hash Functions: Grover's algorithm may enable quantum computers to perform hash function collisions or reversals more quickly than conventional computers, although its impact is not as immediate as with asymmetric cryptography.
- Difficulty of Transition: Quantum-resistant cryptographic technologies (post-quantum cryptography) are currently under development, with standardization processes underway by organizations like NIST, but widespread adoption will take time.
- "Harvest Now, Decrypt Later" Attacks: There is particular concern for medical data regarding attacks where encrypted data is collected now for decryption with future quantum computers. Medical data is especially vulnerable to this type of attack due to its long-term value.
7.3. BISHOP's Quantum Security Response Strategy
7.3.1. Current Countermeasures: Multi-layered Defense Approach
- Limited Role of JWT: The protocol limits the purpose of tokens primarily to integrity verification and proof of origin, avoiding reliance on them for protecting confidential information. This design ensures that even if the cryptographic guarantees of JWT are weakened in the future, critical security breaches can be prevented.
- Short-term Valid Tokens: Token expiration times are appropriately set to mitigate long-term security risks. This partially mitigates the risk of "Harvest Now, Decrypt Later" attacks.
- Blockchain Verification: The protocol provides an additional verification layer through distributed ledgers, not relying on a single cryptographic technology. This prevents a single cryptographic vulnerability from endangering the entire system.
- Hash Chaining: The use of hash functions like SHA-256, which are relatively resistant to quantum attacks in their current state, guarantees data integrity.
7.3.2. Future Extensions: Migration Path to Quantum-resistant Cryptography
- Cryptographic Agility: The core parts of the protocol are separated from the underlying cryptographic algorithms, facilitating transition to new algorithms. This allows for smooth migration when NIST's post-quantum cryptography standards are established.
- Preparation for Adoption of Lattice-based Cryptography: The protocol is preparing for the adoption of promising lattice-based cryptographic algorithms such as CRYSTALS-Kyber (for key encapsulation) and CRYSTALS-Dilithium (for digital signatures).
- Hash-based Signature Mechanisms: The evaluation and adoption of hash-based signature schemes such as XMSS (eXtended Merkle Signature Scheme) and LMS (Leighton-Micali Signature) are being considered.
- Ensuring Backward Compatibility: Migration mechanisms are designed to allow the coexistence of existing tokens and new quantum-resistant tokens.
7.4. Specific Security Use Cases
7.4.1. Image Preservation as Forensic Evidence
- Recording the hash value of the original image on the blockchain
- Maintaining a complete history of image export, editing, and import
- Providing cryptographically verifiable proof of tampering or proof of non-tampering
7.4.2. Ensuring Research Data Integrity
- Embedding unique tokens in each image exported for research
- Including anonymization level and scope of research consent in the token
- Making it possible to track the source of images incorporated into research databases
7.4.3. Detection of Malicious Internal Threats
- Requiring multi-factor authentication for all legitimate outputs
- Explicit recording of output purpose and subject
- Automatic detection of abnormal patterns (such as large volume outputs during late night hours)
7.5. Balance Between Security and Usability
- Context-dependent Authentication: Applying different security levels for outputs from in-hospital terminals versus external connections
- Emergency Override: Enabling rapid access in emergency clinical scenarios while ensuring post-event auditing
- Batch Processing Options: Optimization for smooth bulk image output for educational and research purposes
- Usability Testing: Continuous evaluation and improvement to minimize workflow impact in actual medical environments
References
- HL7 FHIR R5 Specification. Health Level Seven International. https://www.hl7.org/fhir/.
- DICOM Standards Committee. Digital Imaging and Communications in Medicine (DICOM). https://www.dicomstandard.org/.
- European Parliament. General Data Protection Regulation (GDPR), Regulation (EU) 2016/679.
- U.S. Department of Health and Human Services. Health Insurance Portability and Accountability Act of 1996 (HIPAA).
- Hyperledger Fabric Documentation. https://hyperledger-fabric.readthedocs.io.
- WebAuthn Level 2. W3C Recommendation. https://www.w3.org/TR/webauthn-2/.
- Guardtime. (2016). "Estonian eHealth Authority Partners with Guardtime to Accelerate Transparency and Auditability in Health Care." https://guardtime.com/blog/estonian-ehealth-partners-guardtime-blockchain-based-transparency.
- Azaria, A., Ekblaw, A., Vieira, T., & Lippman, A. (2016). "MedRec: Using Blockchain for Medical Data Access and Permission Management." 2nd International Conference on Open and Big Data. [CrossRef]
- MediBloc. (2017). "Blockchain-based Healthcare Information Ecosystem." https://medibloc.org/en.
- Patel, V. (2019). "A framework for secure and decentralized sharing of medical imaging data via blockchain consensus." Health Informatics Journal, 25(4), 1398-1411. [CrossRef]
- Tang, H., Tong, N., & Ouyang, J. (2018). "Medical images sharing system based on blockchain and smart contract of credit scores." In Proceedings of 2018 IEEE Hot Information-Centric Networking, pp. 240-241.
- National Institute of Standards and Technology. (2022). "Post-Quantum Cryptography Standardization." https://csrc.nist.gov/Projects/post-quantum-cryptography.
- Bernstein, D. J., & Lange, T. (2017). "Post-quantum cryptography." Nature, 549(7671), 188-194.
- Alagic, G., et al. (2020). "Status Report on the Second Round of the NIST Post-Quantum Cryptography Standardization Process." NIST Interagency Report 8309.
- Johnson, D., et al. (2021). "Quantum-Resistant Cryptography: Challenges and Solutions for the Digital Era." IEEE Security & Privacy, 19(3), 49-57.
- Kuo, T. T., Kim, H. E., & Ohno-Machado, L. (2017). "Blockchain distributed ledger technologies for biomedical and health care applications." Journal of the American Medical Informatics Association, 24(6), 1211-1220. [CrossRef]
- Roehrs, A., da Costa, C. A., & da Rosa Righi, R. (2017). "OmniPHR: A distributed architecture model to integrate personal health records." Journal of Biomedical Informatics, 71, 70-81. [CrossRef]
- Liang, X., et al. (2018). "Integrating blockchain for data sharing and collaboration in mobile healthcare applications." IEEE 28th International Conference on Personal, Indoor, and Mobile Radio Communications. [CrossRef]
- McGhin, T., et al. (2019). "Blockchain in healthcare applications: Research challenges and opportunities." Journal of Network and Computer Applications, 135, 62-75. [CrossRef]
- Esposito, C., et al. (2021). "Blockchain-based authentication and authorization for smart city applications." Information Processing & Management, 58(2), 102468. [CrossRef]
- DICOM Standards Committee. (2022). "DICOM PS3.15: Security and System Management Profiles." https://dicom.nema.org/medical/dicom/current/output/html/part15.html.
- RFC 7519. (2015). "JSON Web Token (JWT)." Internet Engineering Task Force (IETF). https://datatracker.ietf.org/doc/html/rfc7519.
- Abbas, A., & Khan, S. U. (2014). "A review on the state-of-the-art privacy-preserving approaches in the e-health clouds." IEEE Journal of Biomedical and Health Informatics, 18(4), 1431-1441. [CrossRef]
- Wong, D. R., Bhattacharya, S., & Butte, A. J. (2019). "Prototype of running clinical trials in an untrustworthy environment using blockchain." Nature Communications, 10(1), 917. [CrossRef]
- Dagher, G. G., et al. (2018). "Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology." Sustainable Cities and Society, 39, 283-297. [CrossRef]
- Hasselgren, A., et al. (2020). "Blockchain in healthcare and health sciences—A scoping review." International Journal of Medical Informatics, 134, 104040. [CrossRef]
- Moll, J., Rexhepi, H., & Cajander, Å. (2020). "Patient Empowerment and Access to Health Records." In Proceedings of 2020 IEEE International Conference on Healthcare Informatics, pp. 1-6.
- Kumar, R., et al. (2021). "BIoT: Blockchain for the Internet of Things." In Proceedings of 2021 IEEE International Conference on Blockchain, pp. 144-151.
- Dhieb, N., et al. (2022). "Blockchain-based Schemes for Integration, Interoperability and Secure Sharing of Medical Imaging Data." In Proceedings of 2022 IEEE International Conference on Healthcare Informatics, pp. 342-348.
- Al-Jaroodi, J., & Mohamed, N. (2019). "Blockchain in Industries: A Survey." IEEE Access, 7, 36500-36515.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



