1. Introduction
Vector-borne diseases (VBDs) represent a significant global public and animal health challenge in the twenty-first century. These diseases are caused by pathogens transmitted through the bites of infected arthropods, including mosquitoes, fleas, sandflies, black flies, ticks, and bugs [
1]. VBDs account for more than 17% of all cases of infectious diseases, resulting in more than 700,000 deaths per year worldwide [
2]. A significant number of VBDs are prevalent in Asia such as dengue, malaria, chikungunya, leishmaniasis, yellow fever, lymphatic filariasis, Japanese encephalitis, and schistosomiasis [
3]. Recently, highly infectious fatal tick-borne diseases such as Crimean-Congo haemorrhagic fever, Kyasanur forest disease, and fatal tick-borne encephalitis have emerged in South and Southeast Asia [
4,
5]. Despite the significant vector borne disease burden, challenges persist in acquiring comprehensive data due to insufficient disease surveillance, inadequate diagnostics, and limited public health awareness.
VBD poses a risk to all nations irrespective of their socio-economic status, with vulnerability heightened where disease surveillance programs are absent particularly in low- and middle-income countries. Bangladesh and Malaysia, both characterized by high population density, rapid urbanization, geographic features conducive to VBD outbreaks, have recently faced significant VBD threats including dengue, Zika virus, and chikungunya. Dengue remains a major concern in both countries, with numerous outbreaks between 2010 and 2023 resulting in thousands of cases and several hundred deaths annually [
6,
7,
8,
9]. The geographic range of emerging VBDs, such as Zika virus, Japanese encephalitis, and yellow fever, has also expanded in South and Southeast Asia, with routine detection in both countries [
10,
11,
12,
13]. While malaria was once a major concern, it has been effectively controlled in both nations in recent years with a decline in mortalities attributed to continuous public health campaigns [
5].
Despite the significant challenges posed by VBDs to global health, particularly in low- and middle-income countries, control efforts have predominantly targeted urban localities. The challenges are often more severe in remote areas where low literacy rate, social prejudice, climatic vulnerabilities, and inadequate healthcare infrastructures exacerbate the problems. Remote areas, such as islands and hill tracts, present even greater difficulties due to their perceived inaccessibility, harsh weather conditions, and limited resources. Gaya Island, the largest island in the Tunku Abdul Rahman (TAR) Marine Park, situated near Kota Kinabalu in Sabah province of Malaysia, and Shahpori Island in Bangladesh, located across the maritime borders between Bangladesh and Myanmar, share similar geographic characteristics. Both islands are highly vulnerable to climate change, isolated, and constrained by limited resources, resulting in a lack of medical care facilities for residents.
The level of public health preparedness and awareness of disease risks, especially regarding emerging vector-borne diseases remains largely unknown in these island communities. Given the challenges and resource constraints, understanding how these underserved populations address the threats posed by VBDs is critical for the development of effective prevention, intervention, and control strategies. Moreover, enhancing education and knowledge dissemination about VBDs and mosquito control practices could help change residents' attitudes and encourage the adoption of protective behaviors. Previous knowledge, attitude, and practice (KAP) studies conducted in various regions of Malaysia and Bangladesh have highlighted significant knowledge gaps regarding VBD transmission, prevention, vector biology, and control measures [
14]. However, most of these studies have been conducted in highly accessible areas, such as cities or municipalities, and have not specifically targeted remote or marginalized island communities or focused on emerging VBDs. Therefore, this study aims to assess the knowledge, attitudes and practices towards VBDs in the remote localities of South and Southeast Asia.
2. Materials and Methods
2.1. Study Settings, Timeline, & Data Collection
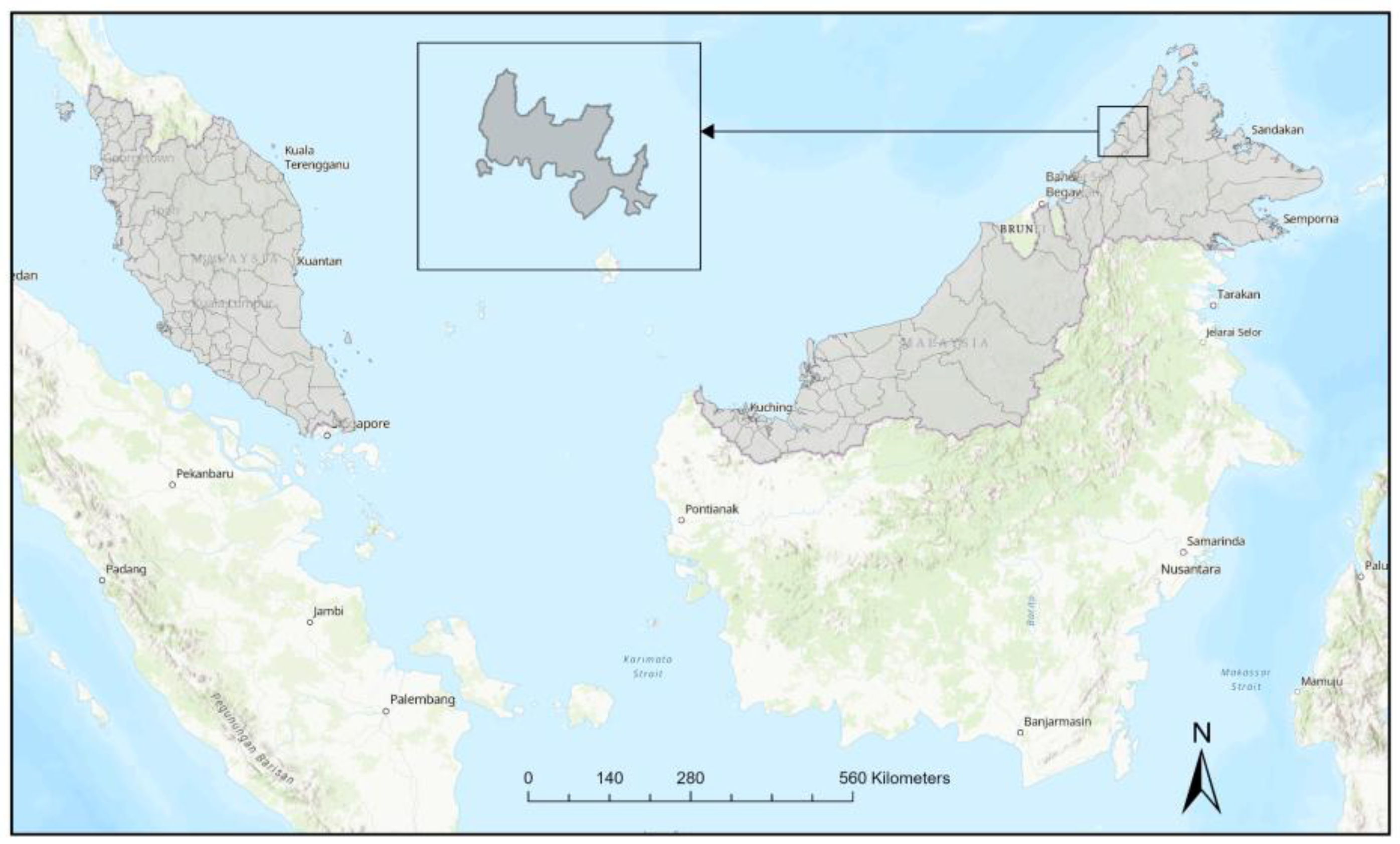
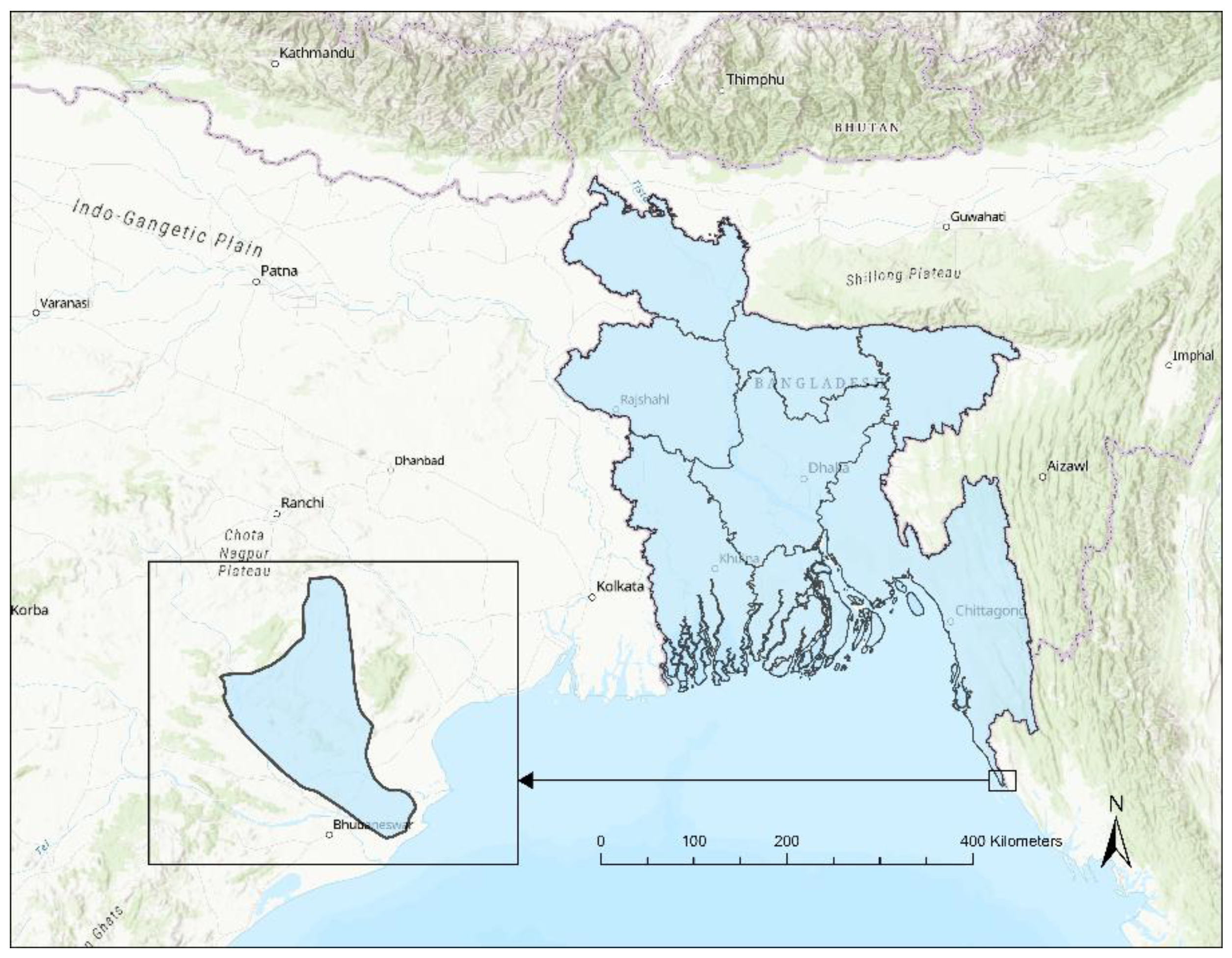
We carried out a community based cross-sectional survey in two remote Islands: Gaya Island, Sabah, Malaysia (
Figure 1), and Shahpori Island, Cox’s Bazar, Bangladesh (
Figure 2). A total of 300 adult participants (150 from Gaya Island and 150 from Shahpori Island) were enrolled from the local populations of both islands. Participants were selected using a simple random sampling method, with inclusion criteria specifying individuals who were native and had been residents of the study Islands for more than five years.
Between November 2018 and February 2020, we recruited study participants from the selected communities. Upon explaining the study objectives, participants provided oral consent and completed the pretested questionnaire The questionnaire covered various aspects of VBDs including demographics; socio-economic characteristics (such as gender, age, marital status, education level, employment status, occupation, income, and number of household members); knowledge and experiences with VBDs; attitudes and practices related to VBD prevention and control. Trained interviewers administered the questionnaire, simplifying questions as needed using the local dialect.
Participation was entirely voluntary, and no incentives were offered. The study protocol received approval from the University of Malaysia Sabah (UMS) Institutional Review Board for Research, prior to implementation in the field.
2.2. Data Analysis
Descriptive statistics were used to summarize the socio-demographic and VBD-related characteristics of participants from Gaya Island, Malaysia and Shahpori Island, Bangladesh. Frequency distributions and percentages were calculated separately for each island and for the combined data across both locations. Comparative analyses were performed to assess socio-demographic differences between the islands, using chi-square tests for categorical variables and Wilcoxon rank-sum tests for continuous variables, when normality assumptions were violated. The normality of continuous variables was assessed using the Shapiro-Wilk test, and non-parametric tests were applied for variables that did not meet normality (p < 0.05). A questionnaire was administered to 150 residents on each island, focusing on VBD-related questions. For each participant, the percentage of correct answers was calculated to create a continuous outcome variable reflecting overall VBD knowledge. This measure represents the proportion of correct responses out of the total questions answered, providing a continuous measure of VBD knowledge for each participant.
To identify the factors associated with knowledge of VBDs, a mixed-effects Poisson regression model was employed. This approach allowed us to account for both individual-level predictors and island-level differences between Shahpori and Gaya islands. The fixed effects in the model included demographic variables such as age, gender, education level, income, household size, occupation, and exposure to health communication. Random effects were incorporated to account for variability at the island level, capturing unobserved island-specific factors, as well as individual-level variations in VBD knowledge not explained by the fixed effects. Model fit was evaluated using a range of statistics, including Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), -2 Res Log Pseudo-Likelihood, and Generalized Chi-Square/DF ratio. These fit statistics helped us to assess the adequacy of the model in accounting for the observed data. Specifically, the Generalized Chi-Square/DF ratio of 0.98 indicated a good model fit, with no evidence of over- or under dispersion. The significance of the fixed effects was evaluated through Wald tests or likelihood ratio tests. Statistical significance was considered at p < 0.05 for all analyses. Data analysis was conducted using SAS version 9.4.
3. Results
A total of 300 participants were surveyed, with 150 from each island. There was a significant disparity in the gender distribution between the islands. Due to the absence of female interviewers in Shahpori Island, only one female respondent was included, which resulted in 99.3% of participants from Shahpori Island being male. In contrast, Gaya Island had a balanced gender distribution, with 50% male and 50% female participants. No significant difference in marital status was observed between the islands (p = 0.5139). A higher proportion of respondents from Gaya Island reported higher education levels compared to those from Shahpori Island, with 54.6% of Gaya respondents having completed secondary school or higher, compared to just 22.6% on Shahpori Island (p < 0.0001). Gaya islanders also reported significantly higher average monthly incomes (USD 170.97) compared to Shahpori islanders (USD 130.03) (p < 0.0001). The mean age of respondents from Shahpori Island (35.64 years) was significantly younger than that of Gaya Island (39.4 years) (p = 0.0107), while mean household size did not differ significantly between the islands (p = 0.9775).
Knowledge of VBDs varied significantly between the two islands. A significantly higher proportion of Gaya islanders (98.7%) had heard of vector-borne diseases such as malaria, dengue, chikungunya, and other VBDs, compared to 89.3% of Shahpori islanders (p = 0.001). While most respondents from both islands recognized fever as a symptom of VBDs, Gaya islanders demonstrated much greater awareness, with 89.3% correctly identified that fever as a symptom, compared to only 42.7% on Shahpori Island (p < 0.0001). Gaya respondents also had a better understanding of the primary cause of these diseases, with 94.7% identifying mosquito bites as the main transmission route, compared to 70% on Shahpori Island (p < 0.0001;
Table 2).
A higher proportion of Gaya islanders (42.7%) were aware of the importance of preventing or destroying mosquito breeding sites, while none of the respondents from Shahpori Island were aware of this practice (p < 0.0001). Regarding prevention methods, residents of Shahpori Island were more likely to report using bed nets (52.7%) compared to Gaya islanders (24%), whereas Gaya islanders preferred a combination of bed nets and mosquito coils (23.3%). In terms of treatment costs, significantly more Gaya islanders (54%) reported spending money on treatment for mosquito-borne diseases than Shahpori islanders (16%) (p < 0.0001). Furthermore, Gaya islanders primarily sought medical care from government hospitals (98.7%), while Shahpori islanders tended to use rural unregistered healthcare providers (61.3%) (p < 0.0001;
Table 3).
Significant predictors of KAP regarding VBDs were identified through Poisson regression analysis. Occupation categories did not exhibit significant associations with VBD-related knowledge. Specifically, the β for the "business" category (β = 0.05840) suggested a marginal increase in VBD knowledge among individuals in this category, but this effect was not statistically significant (p = 0.4042). Similarly, the occupation categories "private job" (β = -0.02526), "housewife" (β = -0.03913), and "other occupation" (β = 0.01046) showed no significant associations with VBD knowledge, with p-values exceeding 0.05 (p = 0.7621, p = 0.6980, and p = 0.8770, respectively). Education was identified as a significant predictor of VBD knowledge, attitudes, and practices. Individuals with higher education levels (secondary school or above) demonstrated significantly better knowledge of VBDs (β = 0.2024, p = 0.0003). Marital status was also a significant predictor, with unmarried or single respondents exhibiting lower knowledge levels compared to their married counterparts (β = -0.1657, p = 0.0372). Age was a positive predictor of VBD knowledge, with each additional year of age contributing to a slight increase in VBD awareness (β = 0.005125, p = 0.0119). Income did not emerge as a significant predictor of VBD knowledge, as the negative β (β = -0.00017) suggested a marginal decrease in VBD knowledge with higher income, but this effect was not statistically significant (p = 0.5589). Household members/size also did not significantly impact VBD knowledge (β = 0.001985, p = 0.8086). Gender was not significant also.
4. Discussion
Our study revealed considerable disparities in knowledge, attitude, and prevention practices regarding VBDs between the islands of Shahpori (Bangladesh) and Gaya (Malaysia), despite their similar remote geographical settings. The socio-economic and educational status significantly differed between the two islands. Only 22.6% of Shahpori residents had completed their post-high school education, whereas 54.6% of Gaya residents had attained a similar level of education. Education has long been recognized as a key determinant of health, and our findings align with previous studies that suggest a correlation between low educational attainment and limited VBD-related knowledge [
15,
16,
17,,
18,
19]. While both islands have a limited number of educational institutions, Shahpori Island suffers from an insufficient provision of educational facilities in contrast to its counterpart.
The occupational distribution among the residents of both islands exhibited similarities, encompassing roles such as small-scale business owners, day laborers, low-income private service, housewife, fishermen, and farmers. In Gaya, many participants were housewives but contributed to the family income by selling handmade mats, crafts made from shells and other sea products in the nearby market. A small proportion of these homemakers made shell ornaments and sold them in the nearby municipalities for their livelihood. The residents of Gaya often commuted to Kota Kinabalu, the capital of Sabah, where they engaged in various occupations such as day laborers, small-scale business, or shopkeepers. Meanwhile, we observed a slightly different pattern in Shahpori Island, where all the participants were predominantly male workforce, with men playing the primary role in supporting family income. Most of our respondents were day laborer in Gaya Island (38%). Residents from both islands frequently commute to nearby municipalities by engine boat or speed boat, however, during dry season, residents of Shahpori can commute to the mainland on foot.
Despite these socio-economic differences, participants from both islands exhibited a basic level of awareness regarding VBDs, with only a small fraction of respondents (6%) reporting no prior knowledge or having never heard of mosquito-borne diseases. In our study, 12.3% of respondents were unaware of symptoms associated with emerging VBDs such as Zika virus and Chikungunya. The majority of the participants on both islands recognized that mosquito bites could lead to mosquito-borne diseases, consistent with the findings reported in different other settings in both countries and other geographic regions of different countries [
20,
21,
22]. Interestingly, only 2.6% of our respondents were aware of other potential causes of VBDs other than mosquito bites, suggesting significant gaps in understanding the broader etiologies of VBDs.
In terms of preventive measures, Gaya Island residents demonstrated better awareness than those from Shahpori counterparts. However, both populations lack knowledge of the detailed life cycle of mosquitoes, mosquito breeding sites, and the natural history of the diseases. While respondents from both islands recognized mosquito bites as a key risk factor and reported using preventive measures such as mosquito nets and repellents, the actual prevalence and implementation of these measures were relatively low compared to other regions [
23,
24]. The disparity in prevalence may arise from spatial and socio-economic discrepancies, limited resources, and the rural nature of these areas. Strategies to prevent the mosquito breeding sites are not commonly adopted in the rural areas of Bangladesh, although some urban areas have implemented mosquito breeding prevention measures [
25]. However, at Shahpori island, these practices have never been adopted. Similarly, while there is a comprehensive mosquito prevention program in operation in urban areas of Malaysia [
26], no such program has been reported on Gaya Island.
The medical infrastructure and diagnostic capabilities on both islands are significantly limited as reflected in our study findings. While all individuals on Gaya Island reported receiving medical treatment at government health facilities, residents of Shahpori predominantly sought medical care from rural, non-registered practitioners or minimally educated rural pharmacy staff, with government and private healthcare facilities serving as secondary options. The absence of registered medical practitioners in both locations indicates a significant healthcare infrastructure gap. Notably, Gaya Island does not have any 'bomoh' or traditional village healers commonly found in other rural areas of Malysia [
26]. The absence of these traditional healers suggests that Gaya residents neither rely on nor perceive traditional healers as primary healthcare providers. This contrasts with the situation on Shahpori Island, where participants frequently depend on non-registered rural practitioners due to the lack of registered medical professionals and infrastructure. Access to healthcare on Shahpori is particularly challenging, as residents must undertake strenuous journeys to the nearest municipality to receive medical care. Previous research in Bangladesh has shown a preference among the majority of individuals to seek medical care from rural, non-registered practitioners, attributed to inadequate medical infrastructure, high poverty rates, and limited availability of registered
medical physicians [
25].
Although respondents from both islands have limited knowledge about VBDs including their causes, symptoms, and preventive measures, they demonstrated positive attitudes toward VBD prevention. This may be linked to the significant public health implications of VBDs, and the existence of some awareness initiatives disseminated through mass media channels. However, these efforts remain remarkably insufficient given the severe adverse effects of VBDs. Most importantly, VBDs frequently evade diagnosis due to the absence of well-equipped laboratories, technicians, and trained medical professionals, leading to treatments based on presumptive diagnoses or left untreated. Furthermore, Shahpori Island is particularly vulnerable due to ongoing refugee crisis, socio-political unrest, armed conflicts, inadequate immunization, massive ecological degradation, and reports of drug-resistant malaria in the regions [
27,
28].
This study has some limitations, including a relatively small sample size and the exclusion of female participants from Shahpori Island due to logistical challenges. The random selection of participants in these remote island territories was based on transportation convenience, which may have introduced sampling bias. As a result, the gender comparison between the islands was not possible. Nevertheless, our study provides valuable insights into the gaps in knowledge and prevention practices related to VBDs in remote islands of South and Southeast Asia. These findings underscore the need for targeted public health interventions tailored to the unique socio-economic and geographic contexts of these populations. Furthermore, the implementation of integrated vector control programs is critical for mitigating the health risks associated with VBDs in these vulnerable communities. Coordinated outreach and educational campaigns, particularly those focused on increasing awareness of mosquito breeding sites and encouraging appropriate medical care-seeking behaviors, are crucial steps toward improving the prevention and management of VBDs on both islands.
Funding
The authors did not receive specific funding for this work.
Ethical approval
The study was approved by the Ethics Committee of Universiti Malaysia Sabah. Written informed consent was obtained from all participants prior to data collection.
CRediT authorship contribution statement
Muhammad Belal Hossain: Conceptualization, Writing – review & editing, Writing – original draft, Software, Project administration, Methodology, Investigation, Formal analysis, Data curation. Sadia Chowdhury Shimmi: Conceptualization, Writing – review & editing, Project administration, Visualization, Validation, Supervision, Data curation. M Tanveer Hossain Parash: Writing – review & editing, Investigation, Software, Visualization. Phoebe Tran: Writing – review & editing, Validation, Methodology, Formal analysis.
Declaration of competing Interests
The authors declare no competing interests.
Acknowledgments
The authors would like to express their sincere gratitude to the residents of Gaya Island, Sabah, Malaysia, and Shahpori Island, Cox’s Bazar, Bangladesh for their participation and valuable contributions to this study. We extend our heartfelt thanks to Rostum Ali and the survey team for their dedicated efforts in data collection, as well as to all individuals involved in the overall implementation of the study.
Appendix A. Supplementary Table
Table A1.
Comparative model fit statistics.
Table A1.
Comparative model fit statistics.
| Fit Statistic |
Poisson |
Negative Binomial |
| -2 Log Likelihood |
1422.77 |
1463.00 |
| AIC |
1446.77 |
1489.00 |
| AICC |
1447.87 |
1490.29 |
| BIC |
1491.01 |
1536.93 |
| CAIC |
1503.01 |
1549.93 |
| HQIC |
1464.48 |
1508.19 |
| Pearson Chi-Square |
276.94 |
358.75 |
| Pearson Chi-Square / DF |
0.98 |
1.27 |
References
- Hill, C.A.; Kafatos, F.C.; Stansfield, S.K.; Collins, F.H. Arthropod-borne diseases: vector control in the genomics era. Nature Reviews Microbiology 2005, 3, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Rocklöv, J.; Dubrow, R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nature immunology 2020, 21, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Servadio, J.L.; Rosenthal, S.R.; Carlson, L.; Bauer, C. Climate patterns and mosquito-borne disease outbreaks in South and Southeast Asia. Journal of Infection and Public Health 2018, 11, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Mourya, D.T.; Yadav, P.D.; Patil, D.Y. Highly infectious tick-borne viral diseases: Kyasanur forest disease and Crimean-Congo haemorrhagic fever in India. WHO South-East Asia Journal of Public Health 2014, 3, 8–21. [Google Scholar] [CrossRef]
- Subramaniam, N.; Anua, S.M.; Mat, N.F.C. Knowledge, Attitude and Practices (KAP) On Aedes Mosquito-Borne Diseases Amongst Community Members in Malaysia: A Review. Malaysian Journal of Medicine & Health Sciences 2021, 17. [Google Scholar]
- Teng, A.K.; Singh, S. Epidemiology and new initiatives in the prevention and control of dengue in Malaysia. 2001.
- Hsan, K.; Hossain, M.M.; Sarwar, M.S.; Wilder-Smith, A.; Gozal, D. Unprecedented rise in dengue outbreaks in Bangladesh. The Lancet Infectious Diseases 2019, 19, 1287. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.S.; Noman, A.A.; Mamun, S.; Mosabbir, A.A. Twenty-two years of dengue outbreaks in Bangladesh: epidemiology, clinical spectrum, serotypes, and future disease risks. Tropical Medicine and Health 2023, 51, 1–14. [Google Scholar] [CrossRef]
- AbuBakar, S.; Puteh, S.E.W.; Kastner, R.; Oliver, L.; Lim, S.H.; Hanley, R.; Gallagher, E. Epidemiology (2012-2019) and costs (2009-2019) of dengue in Malaysia: a systematic literature review. International journal of infectious diseases 2022, 124, 240–247. [Google Scholar] [CrossRef]
- Rahman, M.; Yamagishi, J.; Rahim, R.; Hasan, A.; Sobhan, A. East/central/south african genotype in a chikungunya outbreak, Dhaka, Bangladesh, 2017. Emerging Infectious Diseases 2019, 25, 370. [Google Scholar] [CrossRef]
- Khoo, H.-Y.; Lee, H.-Y.; Khor, C.-S.; Tan, K.-K.; bin Hassan, M.R.; Wong, C.M.; Agustar, H.K.; Samsusah, N.A.; Rahim, S.S.S.A.; bin Jeffree, M.S. Seroprevalence of Zika virus among forest fringe communities in peninsular Malaysia and Sabah: general population-based study. The American Journal of Tropical Medicine and Hygiene 2022, 107, 560. [Google Scholar] [CrossRef]
- Maluda, M.C.M.; Jelip, J.; Ibrahim, M.Y.; Suleiman, M.; Jeffree, M.S.; Aziz, A.F.B.; Jani, J.; Yahiro, T.; Ahmed, K. Nineteen years of Japanese encephalitis surveillance in Sabah, Malaysian borneo. The American journal of tropical medicine and hygiene 2020, 103, 864. [Google Scholar] [CrossRef] [PubMed]
- Paul, K.K.; Sazzad, H.M.; Rahman, M.; Sultana, S.; Hossain, M.J.; Ledermann, J.P.; Burns, P.; Friedman, M.S.; Flora, M.S.; Fischer, M. Hospital-based surveillance for Japanese encephalitis in Bangladesh, 2007–2016: Implications for introduction of immunization. International Journal of Infectious Diseases 2020, 99, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Bashar, K.; Al-Amin, H.; Reza, M.S.; Islam, M.; Asaduzzaman; Ahmed, T. U. Socio-demographic factors influencing knowledge, attitude and practice (KAP) regarding malaria in Bangladesh. BMC Public Health 2012, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Shafie, A.; Roslan, M.A.; Ngui, R.; Lim, Y.A.L.; Sulaiman, W.Y.W. Mosquito Biology and Mosquito-Borne Disease Awareness Among Island Communities In Malaysia. Journal of the American Mosquito Control Association 2016, 32, 273–281. [Google Scholar] [CrossRef]
- Alobuia, W.M.; Missikpode, C.; Aung, M.; Jolly, P.E. Knowledge, attitude, and practices regarding vector-borne diseases in Western Jamaica. Annals of global health 2015, 81, 654–663. [Google Scholar] [CrossRef]
- Aerts, C.; Revilla, M.; Duval, L.; Paaijmans, K.; Chandrabose, J.; Cox, H.; Sicuri, E. Understanding the role of disease knowledge and risk perception in shaping preventive behavior for selected vector-borne diseases in Guyana. PLoS neglected tropical diseases 2020, 14, e0008149. [Google Scholar] [CrossRef]
- Nava-Doctor, J.E.; Sandoval-Ruiz, C.A.; Fernández-Crispín, A. Knowledge, attitudes, and practices regarding vector-borne diseases in central Mexico. Journal of ethnobiology and ethnomedicine 2021, 17, 1–14. [Google Scholar] [CrossRef]
- Nguyen-Tien, T.; Pham, L.T.; Vu, D.T.; Tran, S.H.; Vu, L.T.; Bui, V.N.; Bui, A.N.; Hoang, T.D.; Vu, T.T.; Nguyen-Viet, H. Knowledge and practice on prevention of mosquito-borne diseases in livestock-keeping and non-livestock-keeping communities in Hanoi city, Vietnam: A mixed-method study. Plos one 2021, 16, e0246032. [Google Scholar] [CrossRef]
- Jaramillo Ramírez, G.I.; Álvarez, L.S.B. Knowledge, attitudes and practices regarding dengue, chikungunya, and zika and their vector Aedes aegypti in Villavicencio, Colombia. The Open Public Health Journal 2017, 10. [Google Scholar] [CrossRef]
- Pandit, N.; Patel, Y.; Bhavsar, B. Awareness and practice about preventive method against mosquito bite in Gujarat. Healthline 2010, 1, 16–20. [Google Scholar]
- Fritzell, C.; Raude, J.; Adde, A.; Dusfour, I.; Quenel, P.; Flamand, C. Knowledge, attitude and practices of vector-borne disease prevention during the emergence of a new arbovirus: implications for the control of chikungunya virus in French Guiana. PLoS Neglected Tropical Diseases 2016, 10, e0005081. [Google Scholar] [CrossRef] [PubMed]
- Morse, W.; Izenour, K.; McKenzie, B.; Lessard, S.; Zohdy, S. Perceptions and practices of mosquito-borne diseases in Alabama–is concern where it should be? BMC public health 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, M.M.; Jacob, G.P.; Kamath, A.; Guha, S.; Ramireddy, M. Knowledge, attitude and practices regarding mosquito borne diseases among adults in Udupi District, Karnataka.
- Sizear, M.M.I.; Nababan, H.Y.; Siddique, M.K.B.; Islam, S.; Paul, S.; Paul, A.K.; Ahmed, S.M. Perceptions of appropriate treatment among the informal allopathic providers: insights from a qualitative study in two peri-urban areas in Bangladesh. BMC Health Services Research 2019, 19, 424. [Google Scholar] [CrossRef]
- Haque, A. Culture-bound syndromes and healing practices in Malaysia. Mental Health, Religion and Culture 2008, 11, 685–696. [Google Scholar] [CrossRef]
- Haque, U.; Glass, G.E.; Haque, W.; Islam, N.; Roy, S.; Karim, J.; Noedl, H. Antimalarial drug resistance in Bangladesh, 1996-2012. Trans R Soc Trop Med Hyg 2013, 107, 745–752. [Google Scholar] [CrossRef]
- Nima, M.K.; Mukherjee, A.; Sazed, S.A.; Hossainey, M.R.H.; Phru, C.S.; Johora, F.T.; Safeukui, I.; Saha, A.; Khan, A.A.; Marma, A.S.P.; et al. Assessment of Plasmodium falciparum Artemisinin Resistance Independent of kelch13 Polymorphisms and with Escalating Malaria in Bangladesh. mBio 2022, 13, e0344421. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).