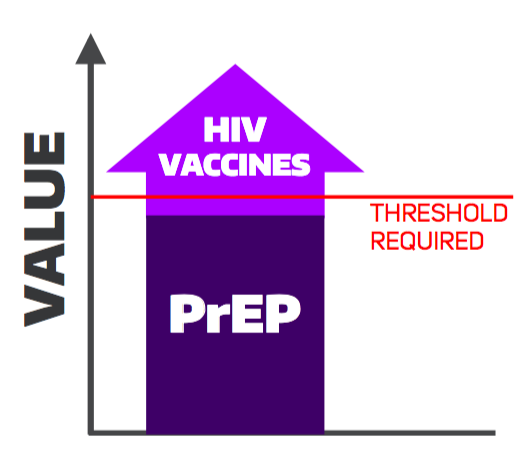
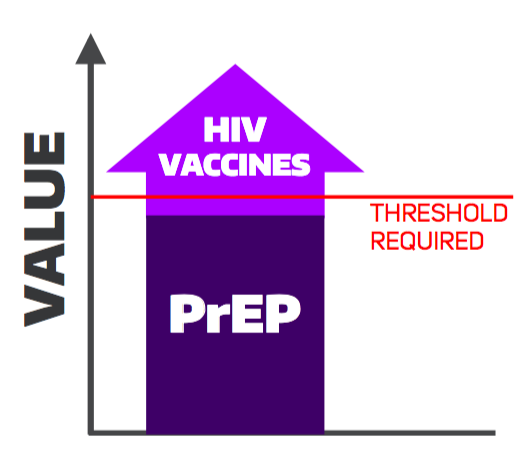
This economic evaluation aims to support policy-making on the combined use of pre-exposure prophylaxis (PrEP) with HIV vaccines by evaluating the potential cost-effectiveness of implementation that would support the design of clinical trials for assessment of combined product safety and efficacy. The target study population is a cohort of men who have sex with men (MSM) in the United States. Policy strategies considered include standard HIV prevention, daily oral PrEP, HIV vaccine, and their combination. We constructed a Markov model based on clinical trial data and published literature. We used a payer perspective, monthly cycle length, a lifetime horizon, and a 3% discount rate. We assumed a price of $500 per HIV vaccine series in the base case. HIV vaccines dominated standard care and PrEP. At current prices,PrEP was not cost-effective alone or in combination. A combination strategy had the greatest health benefit but was not cost-effective (ICER=$463,448/QALY) as compared to vaccination alone. Sensitivity analyses suggest a combination may be valuable for higher-risk men with good adherence. Vaccine durability and PrEP drug prices were key drivers of cost-effectiveness. Results suggest that boosting potential may be key to HIV vaccine value.