1. Introduction
Although not an exact proxy, the fecal microbiome reflects the trillions of microbes that reside in the gastrointestinal tract; microbes that collectively contribute to host digestion, immunity and pathogen defense, and intestinal barrier homeostasis [
1]. While the composition of the fecal microbiome is highly dynamic and can correlate with a range of host factors including age [
2,
3], sex [
4], body condition [
5], diet [
6,
7], habitat [
8,
9], and antibiotic use [
10], more persistent changes in composition have also been associated with disease and infections [
11,
12]. Compared to their healthy counterparts, the fecal microbiome of animals with the disease or infection may have reduced microbial diversity [
13], decreased abundances of functionally important microbes like fermentative or short-chain fatty acid (SCFA)-producing bacteria [
14], or elevated abundances of pathogenic taxa [
15,
16]. These perturbations to fecal microbiome composition can directly impact host health. Recent research shows that Fecal Microbiota Transplants (FMT), which involve the transfer of fecal microbes from a healthy donor into the gastrointestinal tract of a recipient animal, show promise in treating or preventing a range of health conditions and improving health outcomes [
17,
18,
19]. FMTs can repopulate the microbiome and restore fecal microbiome composition, diversity, and homeostasis by increasing microbiome diversity, enhancing the numbers of beneficial microbes, or outcompeting pathogens [
17,
18,
19]. FMTs can be an alternative to conventional treatment methods (particularly if these have proven ineffective) or they can supplement already existing treatment methods for an enhanced resolution of clinical signs.
FMT procedures have been used in veterinary practice since at least the 18th century to successfully treat cattle, horses, sheep, and other animals suffering from rumination disorders, indigestion, inappetence, and colitis [
20,
21]. More recent efforts have used FMTs to treat acute diarrhea, relapsing chronic diarrhea, canine parvovirus, and inflammatory bowel disease in dogs [
22,
23,
24,
25]. Fecal transplants can also be used as a preventative measure and be administered prior to pathogen exposure or disease onset to improve animal health [
18]. In nursing pigs, individuals given fecal material from healthy, high-parity sows experienced reduced mortality, increased weight gain, and sustained production of antibodies when infected with porcine circoviruses compared to individuals that did not undergo FMT treatment [
26]. Similarly, dogs given maternal fecal inoculum during the weaning period demonstrated decreased incidence of diarrhea compared to dogs who did not receive FMTs [
27]. These lines of evidence suggest that microbes can be introduced from a donor into the microbiome of a recipient, where they can be maintained for a period of time, potentially leading to improved health outcomes. Research also shows that complete microbiome engraftment may not be necessary for resolution of disease, thus, in some scenarios, one or a few rounds of FMT treatment could be effective [
26,
28].
While there is growing interest in the application of FMTs particularly to treat digestive disorders, there are few published studies that have evaluated their effectiveness in companion animals. Prior research is mostly limited to case studies of FMT treatment in a single individual or few individuals, but larger-scale analyses are missing, particularly for felids. In case studies of domestic cats (
Felis catus), FMT treatment led to long-term resolution of vomiting and diarrhea in a six year old cat [
29], and successfully resolved chronic ulcerative colitis in an adult cat [
30]. Here, we expand on this work and use 16S rRNA gene sequencing to examine fecal microbiome responses to an oral capsule FMT treatment in 68 domestic cats suffering from chronic digestive conditions, including vomiting, diarrhea, and/or constipation (
Table 1). First, we evaluate the effectiveness of FMT by reporting the number of individuals in which treatment led to a reduction in their clinical signs. Then, we describe detailed changes in the fecal microbiomes of FMT recipients and determine whether these responses were correlated with five host factors (clinical signs, IBD diagnosis, response to FMT treatment, recent antibiotic use, and diet category) (
Figure1A). Next, we identify the bacterial amplicon sequence variants (ASVs) – the most refined level of taxonomy behind species – that engrafted or were shared between FMT recipients and their stool donors (
Figure1B). We also examined whether FMT recipients varied in their ASV engraftment rates. Lastly, we evaluate the extent to which fecal microbiomes of FMT recipients resemble those of healthy pet cats after the conclusion of FMT treatment (
Figure1C). To our knowledge, this is the first study to evaluate fecal microbiome shifts as a response to FMT treatment in a cohort of cats, and compare the fecal microbiomes of FMT recipients to their stool donors and to a set of healthy pet cats.
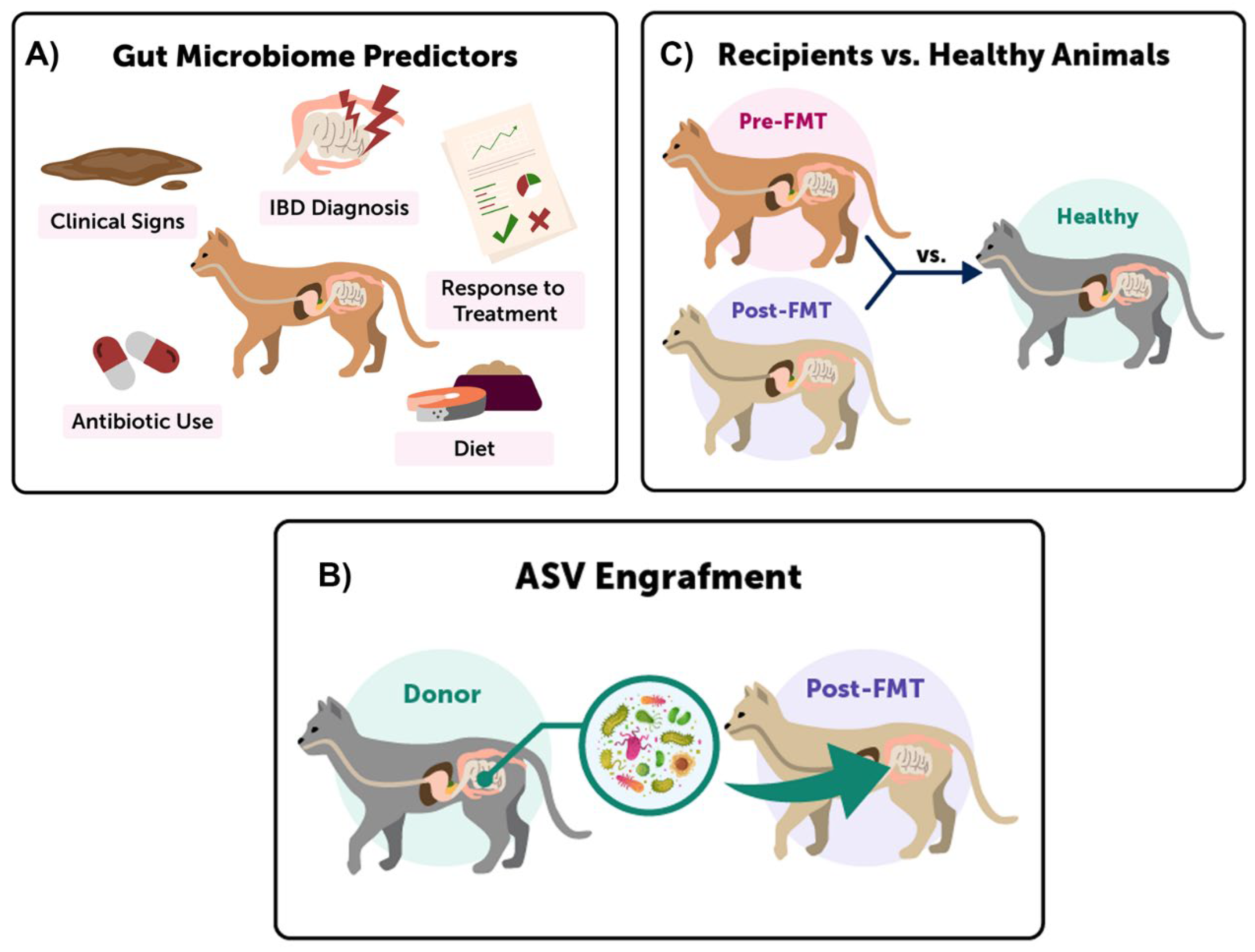
Figure 1.
Three main fecal microbiome comparisons were conducted in this study. A) We investigated shifts in the fecal microbiomes of FMT recipients by testing whether five host predictors were significantly associated with microbiome composition, alpha-diversity, and beta-diversity. B) We identified which ASVs ‘engrafted’ in FMT recipients by comparing the fecal microbiomes of FMT recipients to those of their FMT stool donors, and determining which ASVs were shared. C) Lastly, we examined whether the fecal microbiomes of FMT recipients after treatment became more similar to the microbiomes of healthy cats.
Figure 1.
Three main fecal microbiome comparisons were conducted in this study. A) We investigated shifts in the fecal microbiomes of FMT recipients by testing whether five host predictors were significantly associated with microbiome composition, alpha-diversity, and beta-diversity. B) We identified which ASVs ‘engrafted’ in FMT recipients by comparing the fecal microbiomes of FMT recipients to those of their FMT stool donors, and determining which ASVs were shared. C) Lastly, we examined whether the fecal microbiomes of FMT recipients after treatment became more similar to the microbiomes of healthy cats.
2. Materials and Methods
2.1. Study animals, sample collection, and surveys.
We used social media (primarily Facebook groups that focused on caring for cats with IBD, and posted on Facebook, Instagram, and Twitter) to recruit people with cats exhibiting symptoms of a chronic digestive condition (e.g. diarrhea, vomiting, and/or constipation) who were interested in adding oral FMT capsules to their care. All participants (N=68) signed an informed consent form and were sent a pilot study kit. Kits contained 50 FMT capsules, a health survey, and materials to collect two fecal samples. Participants gave one to two capsules to their cat orally with food each day for ~25 days. They were asked to collect fecal samples from their cats before and two weeks after the course of capsules to accurately assess changes in fecal microbiome composition. Owners also recorded the typical fecal consistency of their cat prior to beginning the capsules and following FMT treatment, using a fecal scoring scale ranging from 1 (hard and constipated) to 7 (watery diarrhea), with 3 and 4 considered a normal consistency [
31].
To collect demographic, physical, and lifestyle information on each cat, owners filled out health surveys that asked about their cat's age, breed, sex, spay or neuter status and diet. In addition, they scored their cat’s body condition, using a scale of 1 (severely underweight) to 10 (severely overweight), with 5 considered a healthy body condition. The survey also included questions about the general health description of their animal, and asked for any diagnoses the animals had received from veterinarians. Importantly, owners recorded the specific clinical signs they were hoping to alleviate with the FMT capsules and among the most common clinical signs were diarrhea, constipation, vomiting, and lack of appetite. Following the course of FMT capsules, owners were asked to describe their cat’s response to treatment, and we categorized their responses as successful, moderately successful, or not successful (e.g. recipients experienced no change or a worsening of their conditions). See Table 1 for a summary of the characteristics of FMT recipients.
Table 1.
Summary characteristics for the sixty-eight cats that underwent oral capsule FMT treatment.
Table 1.
Summary characteristics for the sixty-eight cats that underwent oral capsule FMT treatment.
| Characteristic |
Subcategory |
FMT recipients (N=68) |
| Age, in years |
|
9.35 ± 4.92 |
| Body condition (1-10) |
|
4.90 ± 1.57 |
| Sex |
Female |
30 (44%) |
| Male |
38 (56%) |
| Breed |
Domestic Shorthair |
38 (56%) |
| Other breed |
30 (44%) |
| Diet |
Wet |
8 (12%) |
| Dry |
7 (10%) |
| Raw |
16 (24%) |
| Wet & Dry |
20 (29%) |
| Wet & Raw |
9 (13%) |
| Other diet (including Wet & Dry & Raw; Raw & Dry) |
8 (12%) |
| Spayed or Neutered |
Yes |
67 (98%) |
| No |
1 (2%) |
| Antibiotics |
Yes |
34 (50%) |
| No |
33 (48%) |
| Unknown |
1 (2%) |
| IBD |
Yes |
35 (51%) |
| No |
20 (30%) |
| Maybe |
13 (19%) |
| Response to FMT |
Improved |
52 (77%) |
| No Change |
11 (16%) |
| Worsened |
5 (7%) |
| Initial symptoms |
Constipation (only) |
11 (16%) |
| Diarrhea (only) |
31 (46%) |
| Vomiting & Diarrhea |
17 (25%) |
| Other, including None, Vomiting & Constipation, Diarrhea & Constipation |
9 (13%) |
The study protocol and informed consent forms were in compliance with the Animal Welfare Act. The capsules were given in addition to the standard of care offered by their veterinarian for the chronic digestive condition. Participants were advised to consult with their veterinarian before participating in the study and they were informed that they could drop out of the study for any reason at any time.
Cats exhibiting symptoms of a chronic digestive condition (e.g. diarrhea, vomiting, and/or constipation) were recruited for this study. Owners completed a health and demographic survey on their cats and collected fecal samples before and two-weeks after oral capsule FMT treatment.
2.2. Preparation of FMT capsules.
Donated fecal matter was collected from ten healthy indoor cats: from six individual donors and two pairs of donors (where the fecal material of two cats who live together was combined). Donor animals had no antibiotic treatment in the past year, were not taking medications, had no known health conditions, current infections, or recent surgeries, and did not exhibit behavioral issues. Their ages ranged from 2-9 years old (average 4.73 ± 4.56 yrs), and the compositions of their fecal microbiomes were comparable to those of healthy cats in our reference database, as determined by 16S rRNA gene sequencing. All donor samples that had appropriate fecal consistencies (scores of 3-4) were submitted for pathogen screening using both qPCR and culturing to the University of California, Davis Real-time PCR and Diagnostics Core Facility. Samples were screened for Clostridiodes difficile toxins A and B, Cryptosporidium spp, Salmonella spp, Giardia spp, feline coronavirus, feline parvovirus (Panleukopenia), and Tritrichomonas foetus. Donors were also periodically screened for helminth parasites and protozoan oocysts via fecal flotation (IDEXX). Donor animals were on average 4.93 ± 3.43 years old, and mostly domestic shorthairs (75%) that consumed a diet of both wet food and dry food (50%; Table S1).
Fecal samples from the six individual donors and the two pairs of donors served as material for the FMT capsules (Table S1) that were administered to recipient animals. Donor material was collected on a daily basis. Any stool with a suboptimal fecal consistency, excess mucus, mold, flies, unpleasant odor, or color was discarded. Stool was cleaned of litter, hair, and any foreign material prior to mixing with 20% glycerol (wet weight) and freeze drying at -40° C to -50° C. Once the stool was completely freeze dried, it was stored at -20° C until it was ground into a fine powder and placed into size 4 capsules. We followed stringent quality control guidelines and standard operating procedures. Capsule batches were labeled by donor and lot number, and randomly assigned to FMT recipients.
Using data from Ganz
et al. 2022 [
3] (
Table S2), we compared a reference set of 166 healthy cats for comparison with FMT recipients with chronic digestive conditions. These cats had no known health conditions, clinical signs or diagnoses, had a body condition score between 3 and 6 (mean 5.14 ± 0.47) or a calculated BMI of less than or equal to 50, and had taken no antibiotics within the previous 12 months according to information reported by their owners. The cat’s ages were between 1-12 years of age (mean 4.99 ± 3.23 years of age), although for statistical analyses, FMT recipients were age-matched to cats from the healthy reference set (see ‘
Statistical analyses: fecal microbiome similarity between FMT recipients and healthy pet cats’). Of these 166 cats, 55% were female, about half were domestic shorthairs (52%), and almost all were spayed or neutered (91%) (
Table S2). The two most represented diets were wet and dry food (30%), just dry food (12%), or just raw food (11%).
2.3. DNA Extractions and 16S rRNA gene sequencing.
Owners placed fecal material from their cats (n=68) pre- and post-FMT treatment into 2 mL screw cap tubes containing 100% ethanol and silica beads. These were shipped to AnimalBiome’s facilities (Oakland, CA) and stored at 4 - 8° C until further laboratory analysis. Fecal material was isolated from the preservation buffer by centrifugation, and genomic DNA was extracted using QIAGEN DNeasy PowerSoil Kits (Germantown, MD). Briefly, samples were placed in bead tubes containing C1 solution, incubated at 65° C for 10 min, and placed in a bead beater for 2 mins, after which the manufacturer’s protocol was followed as written. DNA was extracted from the fecal samples of healthy pets (n=166) and donor animals (n=20) in the same fashion. For the donor animals, four cats had one fecal sample each, one cat had two samples, and another cat had 6 samples. The two pairs of donors (where two cats cohabited and their fecal material was combined), had three and five fecal samples, respectively. Thus, 20 fecal samples total were collected from ten donor animals for microbiome analysis.
Amplicon libraries of the V4 region of the 16S rRNA gene were generated from extracted DNA using a dual-indexing one-step PCR with complete fusion primers (505F/816R) (Ultramers, Integrated DNA Technologies) with multiple barcodes (indices), adapted for the Illumina Miniseq platform as detailed in Pichler
et al. 2018 [
33]. PCR reactions contained 0.3-30 ng template DNA, 0.1 µl Phusion High-Fidelity DNA Polymerase (Thermo Fisher), 1X HF PCR Buffer, 0.2 mM each dNTP, and 10 µM of the forward and reverse fusion primers. PCR conditions were as follows: denaturation at 98° C for 30 sec, 30 cycles of 98° C for 10 sec, 55° C for 30 sec, and 72° C for 30 sec. There was a final incubation at 72° C for 4 min 30 sec for a final extension, and a hold at 6°C until retrieval. PCR product amplification was assessed by running on 2% E-Gels with SYBR Safe (ThermoFisher). PCR products were then purified and normalized using the SequalPrep Normalization Kit (Thermo Fisher). PCR products were pooled into the final libraries; each contained 95 samples (not all from this study) and 1 negative control (blank sample extraction). The final libraries were quantified with QUBIT dsDNA HS assay (Thermo Fisher), diluted to 1.8 pM and denatured according to Illumina’s specifications for the MiniSeq. Identically treated phiX was included in the sequencing reaction at 15%. Paired-end sequencing (150 bp) was performed on one mid-output Illumina MiniSeq flow cell per final library.
2.4. 16. SrRNA sequence processing.
Raw 16S rRNA gene amplicon sequences were obtained from fecal samples of recipient animals (68 individuals, 136 fecal samples), donor animals (10 individuals, 20 fecal samples), and healthy reference animals (166 individuals, 166 fecal samples [
3]). Sequences were trimmed, quality-filtered and dereplicated using the Divisive Amplicon Denoising Algorithm (DADA2 v1.14.1) pipeline in R (v3.6.2) [
34,
35]. Specifically, forward reads were trimmed to 145 bp while reverse reads were trimmed to 140 bp. After calculating error rates, ASVs were inferred using DADA2’s core denoising algorithm and chimeras were removed. The DADA2 pipeline merges paired-end reads after ASV calling to achieve greater accuracy [
34]. Overall, samples from animals receiving FMT treatment contained an average of 56,615 ± 26,134 sequences after processing in DADA2, those from donor animals averaged 62,299 ± 23,558 sequences, and those from the healthy reference set contained on average 45,786 ± 27,918 sequences. Taxonomic classifications were assigned to ASVs using DADA2’s naïve Bayesian classifier against the Silva reference database (v138) [
36,
37] and ASVs classified as Eukarya, Chloroplasts, or Mitochondria were removed from the dataset. Overall, the recipient fecal microbiome dataset contained 3099 total ASVs, the donor dataset contained 2060 ASVs, and the healthy reference dataset had 2718 ASVs. The ASV relative abundance table, list of ASV taxonomic assignments, and metadata for every fecal sample from recipients, donors, and healthy animals is available as supplementary materials (
Table S3-S5).
2.5. Statistical analyses: defining host explanatory variables.
Unless otherwise stated, all statistical analyses and figures were performed in R (v3.6.2) [
35]. Throughout analyses, samples were classified as “recipient” samples if they came from cats that participated in the FMT capsule course treatment, “healthy” samples if they came from the 166 healthy cats, and “donors” if they came from any of the 10 stool donors. “Recipient” samples were further categorized into “preFMT” or “postFMT” depending on when they were collected.
For recipient samples, we conducted various statistical analyses that involved five host predictors of interest: response to treatment, initial clinical signs, IBD diagnosis, antibiotic use, and dietary category (Figure1A). For the response to treatment variable, recipient animals were categorized as “responders” if their owners reported improvement in their clinical signs following FMT treatment, or as “non-responders” if their owners reported no change or a worsening of clinical signs following FMT treatment. Clinical signs were categorized into Diarrhea only, Constipation only, and Vomiting with Diarrhea (Table 1). All other combinations of symptoms were clustered into an “Other” category. For IBD diagnosis, categories included animals who had been diagnosed with IBD by a veterinarian (“Yes”), animals that were suspected of having IBD but never received an official diagnosis (“Maybe”), and animals with no IBD diagnosis (“No”). Cats that were recently on antibiotics (within two weeks) were categorized as “Yes”, and all other cats as “No.” Lastly, host diet comprised six discrete categories: Dry food only, Wet food only, Raw food only, Wet and Dry food, Wet and Raw food, and Other. Table 1 lists sample sizes for each host factor and its subcategories.
We also had information on a cat’s breed, body condition score, spay or neuter status, etc., but these were not selected as variables for analysis because there was not sufficient variation among samples (Table 1). For example, 98% of cats had been sterilized, so this variable was not appropriate for statistical analysis.
2.6. Statistical analyses: fecal microbiome alpha-diversity and beta-diversity.
We calculated the fecal microbiome alpha-diversity of samples from FMT recipients. We did not rarefy samples by subsampling to an equal number of sequences as this has been shown to be statistically inappropriate for microbiome analyses [
38]. All samples had at least 8600 reads. ASV richness was calculated with phyloseq (v1.30.0) [
39], Pielou’s evenness with microbiome (v1.15.2) [
40], and Faith’s Phylogenetic Diversity with picante (v1.8.2) [
41]; the latter after supplying it with a phylogenetic tree of ASV sequences built with DECIPHER (v2.14.0) [
42] and phangorn (v2.5.5) [
43].
Linear mixed models evaluated whether FMT recipients varied in their fecal microbiome richness, evenness, or phylogenetic diversity, using the lme4 (v1.1-29) [
44] package. All models included one of the three alpha-diversity metrics as the dependent variable. Model #1 compared preFMT samples to postFMT samples and set individual identity as a random effect. Model #2 regressed preFMT (or postFMT) alpha-diversity values against the five host predictors (IBD diagnosis, clinical signs, antibiotic use, response to treatment, diet), and set host age and sex as random effects (
Figure1A). The statistical significance of the independent variables was determined via likelihood ratio tests (LRT) using the car package (v3.0-13) [
45], setting a=0.05. Boxplots of fecal microbiome alpha-diversity were made in ggplot2 (v3.3.6) [
46].
To analyze fecal microbiome beta-diversity in FMT recipients, we constructed two types of distance matrices from unrarefied data using phyloseq. The two distances were Bray-Curtis dissimilarity index, which captures compositional dissimilarity between samples, and Weighted Unifrac distance that considers the phylogenetic relationships among bacterial ASVs. We constructed Permutational Multivariate Analysis of Variance (PERMANOVA) models using the vegan package (v2.6-2) [
47] to examine whether FMT recipients varied in their fecal microbiome structure (e.g. beta-diversity). All models included one of the two distances as the dependent variable and used 999 permutations. Model #1 compared preFMT samples to postFMT samples and controlled for individual variation by including this variable as the first term in the model. Model #2 regressed preFMT (or postFMT) beta-diversity against the five host predictors of interest (IBD diagnosis, clinical signs, antibiotic use, response to treatment, and diet), plus two more variables we needed to account for (age, and sex) (
Figure1A). If PERMANOVA tests yielded statistically significant relationships (a=0.05), we used Permutational Analyses Of Multivariate Dispersions (PERMDISP) [
47] to test for differences in microbiome dispersion between groups. Principal Coordinates Analysis (PCoA) ordinations were made in ggplot2.
2.7. Statistical analyses: relative abundances of bacterial genera.
We investigated whether the relative abundances of core or potentially pathogenic taxa changed in recipient animals and whether these changes were associated with five host predictors. We defined core genera (N=21) as the genus-level bacterial taxa that were found in at least 55% of samples from a healthy population of cats [
3] (
Table S8). The potentially pathogenic taxa were five bacterial genera that may be pathogenic to felids (
Table S9) [
48,
49,
50,
51]. All taxa tested must have been found in at least 10% of samples from FMT recipients. The generalized linear models specified change (Δ) in the relative abundance of bacterial taxon
i (postFMT - preFMT) as the dependent variable and five host predictors as independent variables: host response to treatment (responder vs. nonresponder), initial presenting symptoms, antibiotic use, IBD status, and diet. These models did not include host sex or age as predictors since neither significantly predicted fecal microbiome alpha- or beta-diversity. We used the stats package [
35] for the linear models and statistical significance was evaluated using likelihood ratio tests as described earlier. Plots of the change (Δ) in relative abundance for statistically significant genera were constructed using ggplot2.
2.8. Statistical analyses: ASVs shared between FMT recipients and their stool donors.
The second objective of our study was to identify which donor microbes could engraft (i.e. transfer) in FMT recipients and calculate ASV sharing rates between FMT recipients and their stool donors (
Figure 1B). We used calculations adapted from a meta-analysis by Ianiro
et al. 2022 [
52], which examined strain engraftment after FMT in human cohorts across eight different diseases. In our study, ASV sharing rates were calculated by dividing the number of ASVs shared between postFMT samples and their stool donors (excluding taxa shared between preFMT samples and donors) by the total number of ASVs in the donor sample (excluding any taxa shared with preFMT samples). A linear mixed model evaluated whether an FMT recipient’s ASV engraftment rate correlated with the five host predictors of interest and set host age and sex as random effects. Another generalized linear model tested whether ASV engraftment rates varied among stool donors. Plots of ASV sharing rates were made in ggplot2.
2.9. Statistical analyses: fecal microbiome similarity between FMT recipients and healthy pet cats.
Lastly, we tested whether the fecal microbiomes of FMT recipients approximated or “became more similar” to the fecal microbiomes of age-matched healthy animals (
Figure 1C) [
3]. We wanted to investigate for example, whether the fecal microbiomes of cats with IBD became more similar or less similar to healthy animals compared to cats without IBD. For these analyses, we used the two beta-diversity distances and only kept pairwise comparisons between recipient animals and healthy animals (e.g. we excluded recipient vs. recipient comparisons or healthy vs. healthy comparisons). Only pairwise comparisons of cats whose ages were within 1 year of each other were retained. Change (Δ) in fecal microbiome similarity was calculated as follows:
[ similarity between postFMT sample for cat i and healthy animal ii ]
[ similarity between preFMT sample for cat i and healthy animal ii ].
These calculations were done for all 68 FMT recipients compared against their age-matched healthy counterparts, and the resulting data frame was used for statistical analysis. A generalized linear model tested whether the change (Δ) in fecal microbiome similarity was correlated with five host predictors: host response to treatment, initial presenting symptoms, antibiotic use, IBD status, and diet. Statistical significance was evaluated using likelihood ratio tests (LRT) as described earlier. Plots of Δ in fecal microbiome similarity (Bray-Curtis) were constructed using ggplot2.
3. Results
3.1. FMT clinical success and microbiome responses in recipients
A total of sixty-eight cats underwent oral capsule FMT treatment and provided data for this study. About half of the participants had been diagnosed with IBD by a veterinarian, and/or had been on antibiotics (Table 1). Prior to treatment, 46% of FMT recipients had been experiencing only diarrhea, 16% of recipients experienced only constipation, 25% experienced vomiting with diarrhea and 13% experienced other combinations of clinical signs. Two weeks after FMT treatment, about 77% of participants experienced an improvement in their health and a reduction of their clinical signs according to their owners (“Responders”) (Table 1), while 23% of participants experienced no noticeable change or a worsening of their condition (“Non-Responders”). Thus, the majority of participants experienced clinical success after the oral FMT capsule treatment.
A slightly greater proportion of ‘Responders’ were female, consumers of wet food with raw food, and cats experiencing constipation compared to ‘Non-Responders’ (Figure S1), which instead had a greater ratio of cats with IBD or suspected IBD, slightly greater ratio of cats with vomiting and diarrhea, and greater ratio of cats that ate wet food with dry food. Responder animals were slightly younger (8.96 yrs ± 5.02 yrs) than Non-Responders (10.30 yrs ± 4.57 yrs) (Table 1). About 50% of cats had recently taken antibiotics in both Responders and Non-Responders (Figure S1).
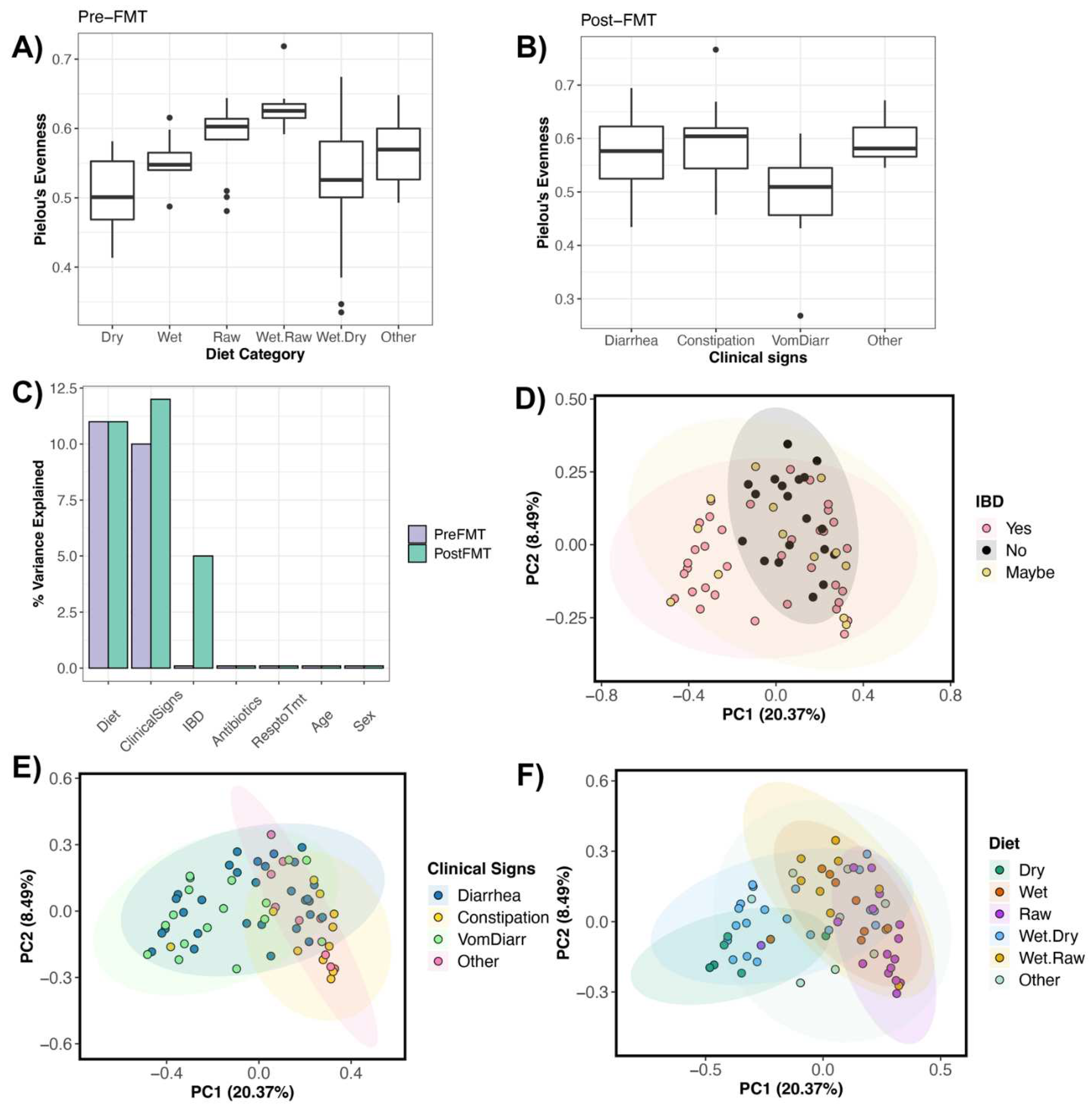
Next, we asked whether patterns in FMT clinical success were also observable at the microbiome level. Did FMT recipients exhibit variation in their fecal microbiomes? Were the fecal microbiomes of Responders distinct from those Non-Responders, or were cats with IBD distinct from cats without IBD? For this, we correlated fecal microbiome alpha- and beta-diversity with five main host factors of interest: response to treatment, initial presenting clinical signs, prior antibiotic use, IBD diagnosis, and diet (Figure 1A). Results showed that before FMT treatment, the fecal microbiome alpha-diversity of recipient animals was best predicted by dietary category (Table S6). Cats that consumed raw food or raw food in combination with wet food tended to harbor slightly more even fecal microbiomes than cats with other diets (Figure 2A). After FMT treatment, fecal microbiome diversity was significantly correlated with an individual’s pre-treatment clinical signs (Table S6). The bacterial communities of cats who suffered from both vomiting and diarrhea were less even than those of cats who had diarrhea, constipation, or other combinations of symptoms (Figure 2B). We did not detect differences in the richness, evenness, and phylogenetic diversity of preFMT and postFMT samples (GLM LRT ASV Richness χ2=0.49, P=0.48; Pielou’s evenness χ2=0.013, P=0.48; PD χ2=0.58, P=0.44), thus, preFMT samples did not start at lesser or greater levels of diversity compared to postFMT samples.
Fecal microbiome beta-diversity prior to FMT treatment was best predicted by clinical signs and dietary category, which each accounted for 10-11% of the variation in fecal microbiomes among individuals (Figure 2C, Table S7). Response to treatment, antibiotic use, IBD diagnosis, age (years), or sex were not significantly associated with variation in fecal microbiomes before FMT (Table S7). The fecal microbiome dispersions of hosts experiencing different clinical signs did not differ (PERMDISP Bray-Curtis F=1.45, P=0.23; Weighted Unifrac F=2.05, P=0.11) and the same was true of host diet (PERMDISP Bray-Curtis F=0.64, P=0.66; Weighted Unifrac F=1.70, P=0.14). Similarly to pre-FMT microbiomes, post-FMT microbiomes were also strongly correlated with clinical signs and dietary category, in addition to IBD diagnosis (Figure 2C-F). Host clinical signs accounted for 12% of the variation in the microbiome and host diet explained an additional 11% of the variation (Table S7). IBD diagnosis accounted for about 5% of the variation among individuals (Figure 2D, Table S7). Furthermore, the fecal microbiomes did not vary in how heterogenous they were; thus differences between samples of different IBD diagnoses, clinical signs, and diets could be fully attributed to differences in their microbiome structures rather than their dispersions (IBD PERMDISP Bray-Curtis F=1.72, P=0.18; Weighted Unifrac F=2.55, P=0.08) (Clinical signs PERMDISP Bray-Curtis F=1.47, P=0.23; Weighted Unifrac F=1.10, P=0.35) (Diet PERMDISP Bray-Curtis F=0.42, P=0.83; Weighted Unifrac F=0.35, P=0.87).
Lastly, the fecal microbiomes of preFMT samples were not dissimilar from the fecal microbiomes of postFMT samples, suggesting that the patterns observed were not an artifact or bias of our sampling (PERMANOVA Bray-Curtis catID R2=0.82, P=0.001, sample type R2=0.002, P=0.53; Weighted Unifrac catID R2=0.84, P=0.001, sample type R2=0.001, P=0.48) (Figure S2). Interestingly, cat individual identity explained 83% of the variance in the fecal microbiome, indicating that there is remarkable consistency in the fecal microbiomes of samples from the same individual before and after treatment. This also suggests that differences between pre-FMT and post-FMT microbiomes are not global but may be specific to the relative abundances of particular bacterial taxa.
Figure 2.
Host predictors of fecal microbiome alpha- and beta-diversity in FMT recipients. Boxplots of microbiome evenness (Pielou’s Evenness) by
A) dietary category for preFMT samples and
B) clinical signs for postFMT samples.
C) Percent variance explained by host predictors according to PERMANOVA tests (averaged across Bray-Curtis and Weighted Unifrac distances; see
Table S7 for exact values). PCoA ordinations based on Bray-Curtis distances showing the clustering of postFMT samples by
D) IBD diagnosis,
E) Clinical signs, or
F) dietary category.
Figure 2.
Host predictors of fecal microbiome alpha- and beta-diversity in FMT recipients. Boxplots of microbiome evenness (Pielou’s Evenness) by
A) dietary category for preFMT samples and
B) clinical signs for postFMT samples.
C) Percent variance explained by host predictors according to PERMANOVA tests (averaged across Bray-Curtis and Weighted Unifrac distances; see
Table S7 for exact values). PCoA ordinations based on Bray-Curtis distances showing the clustering of postFMT samples by
D) IBD diagnosis,
E) Clinical signs, or
F) dietary category.
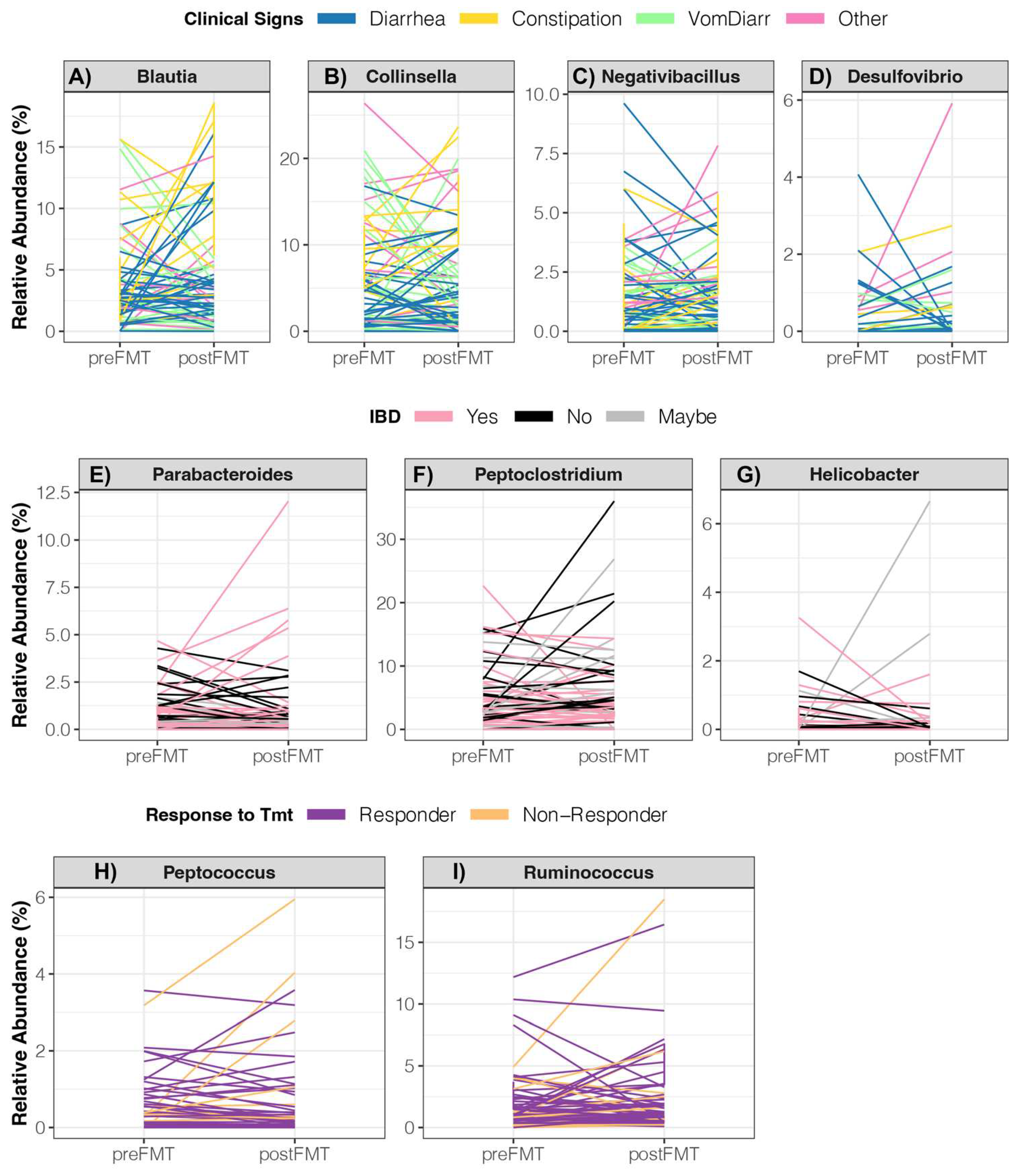
3.2. Changes in the relative abundances of core and pathogenic bacterial genera in FMT recipients
Next, we conducted more fine-scale analyses to discern the particular bacterial taxa that may be underlying changes in the fecal microbiome two weeks post FMT treatment. For some individuals, certain taxa may have decreased or increased in relative abundance over the course of FMT treatment. Specifically, we tested whether the change in relative abundance (postFMT – preFMT) of core genera or potentially pathogenic genera was correlated with host response to treatment (responder vs. nonresponder), initial presenting symptoms, antibiotic use, IBD status, and diet (
Figure 1A). Of the 21 bacteria genera that constitute the core in the fecal microbiomes of healthy pet cats [
3] (
Table S8), the relative abundances of three genera (
Blautia, Collinsella, and Negativibacillus) were associated with clinical signs. Specifically, the relative abundances of all three taxa tended to decrease in cats suffering from vomiting with diarrhea (
Figure 3A-C,
Figure S3). The relative abundances of
Parabacteroides and
Peptoclostridium varied with IBD diagnosis such that cats that had IBD experienced increases in
Parabacteroides relative abundances but a decrease in
Peptoclostridium relative abundances compared to cats without the condition (
Figure 3E-F,
Figure S3,
Table S8). The abundance of two bacterial genera changed differentially in responder animals vs. non-responder animals (
Figure 3H-I,
Table S8). Specifically,
Peptococcus and
Ruminococcus relative abundances slightly increased in non-responder animals and mainly stayed the same in responder animals (
Figure S3). No statistically significant changes in the relative abundance of core genera were detected in cats that had previously taken antibiotics vs. cats that had not taken antibiotics (
Table S8).
Lachnoclostridium relative abundances decreased in cats that ate canned wet food with dry kibble compared to other surveyed cats (
Figure S3,
Table S8).
When examining the change in the relative abundances of the five potentially pathogenic genera, FMT recipients who exhibited constipation in combination with other symptoms experienced a slight increase in their Desulfovibrio load, compared to animals that only had diarrhea (Figure 3G, Figure S3, Table S9). Furthermore, cats that may perhaps have IBD tended to experience an increase in their Helicobacter relative abundances compared to the rest of the surveyed cats (Figure 3D, Figure S3). Lastly, animals fed a 100% dry kibble diet tended to exhibit increases in their Veillonella relative abundances compared to cats fed other diets (Figure S3, Table S9).
Figure 3.
Changes in the relative abundances of bacterial genera in cats receiving FMT treatment. Linear mixed models indicated that the changes in the relative abundance of 10 bacterial genera were significantly associated with
A-D) host clinical signs,
E-G) IBD diagnosis, or
H-I) response to treatment. For the statistical output of posthoc testing using Tukey linear contrasts, see
Figure S3.
Figure 3.
Changes in the relative abundances of bacterial genera in cats receiving FMT treatment. Linear mixed models indicated that the changes in the relative abundance of 10 bacterial genera were significantly associated with
A-D) host clinical signs,
E-G) IBD diagnosis, or
H-I) response to treatment. For the statistical output of posthoc testing using Tukey linear contrasts, see
Figure S3.
3.3. ASVs shared between FMT recipients and their stool donors
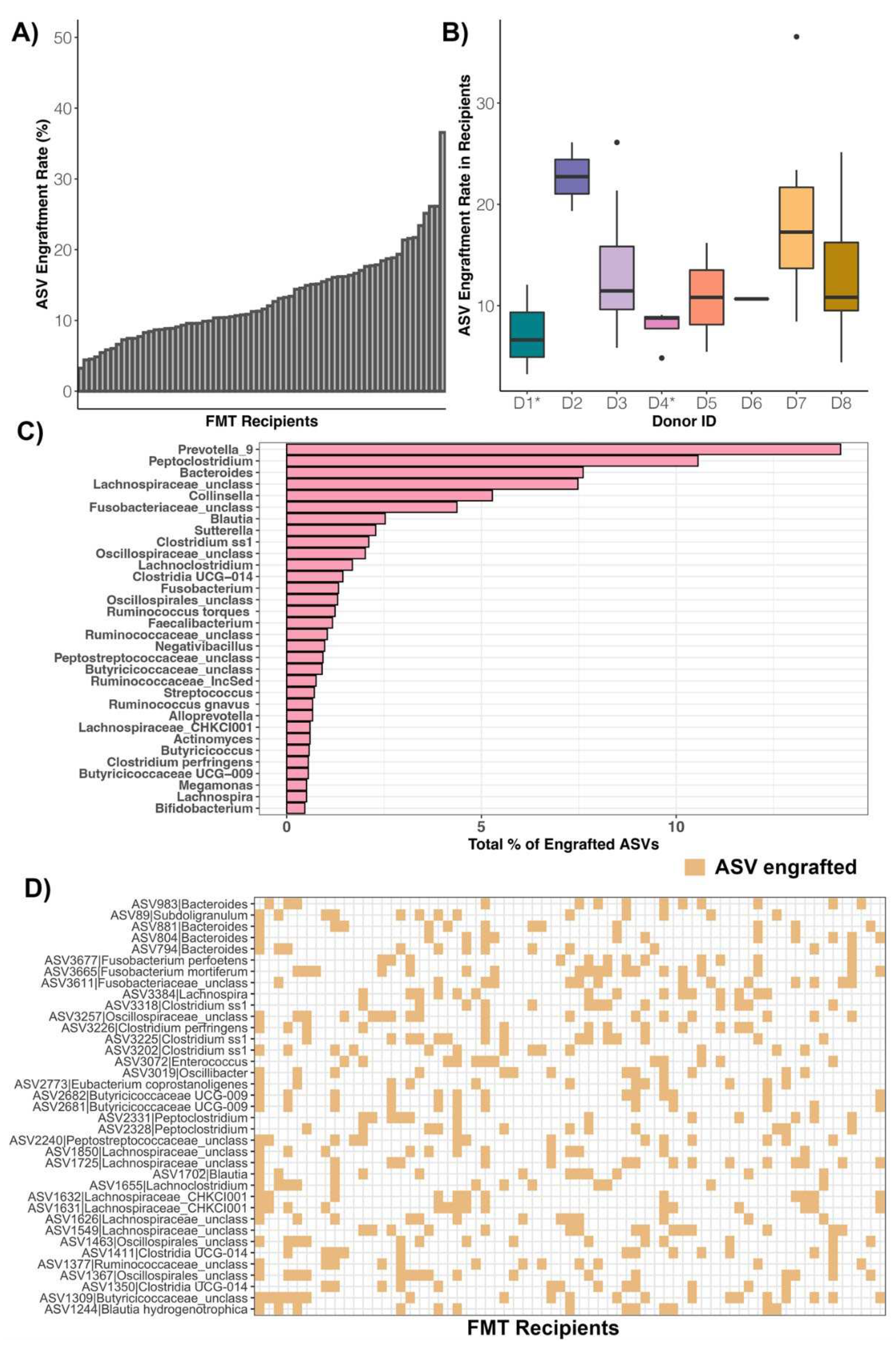
Another objective of our study was to compare the fecal microbiomes of FMT recipients with those of their donors to identify the bacterial ASVs that were more likely to be shared or engraft in FMT recipients (Figure 1B). We also tested whether individuals varied in their ASV engraftment efficiency and correlated these values with host predictors. For this, we analyzed the ASVs that were shared between the fecal microbiomes of FMT recipients postFMT and their specific stool donors, excluding any ASVs that were shared between recipients preFMT and their donors. ASV engraftment rates indicated the proportion of donor ASVs that engrafted into FMT recipients relative to the total number of donor ASVs that had the capacity to engraft.
Across FMT recipients, ASV engraftment rates ranged from 3.25% to 36.56%, with an average of 13.26% (± 6.24%) (Figure 4A, Table S10). That is, of the bacterial ASVs present in FMT stool donors with the capacity to engraft or be shared (x̅: 538 ASVs, range: 189-1086 ASVs), about 13% on average (x̅: 65 ASVs, range: 14-172 ASVs) successfully engrafted in the FMT recipient (Table S10). Thus, complete microbiome engraftment was not observed in this cohort of cats. An FMT recipient’s ASV engraftment rate was not significantly associated with response to treatment, initial clinical signs, IBD diagnosis, prior antibiotic use, or diet (LMM LRT Response χ2=0.63, P=0.42; Clinical signs χ2=0.52, P=0.91; IBD χ2=1.5, P=0.47; Antibiotics χ2=0.09, P=0.76; Diet χ2=5.37, P=0.37). ASV sharing rates however, were significantly predicted by donor’s identity (Kruskal Test χ2=16.84, P=0.018), with two donors in particular (D3 and D7) having bacterial ASVs that were shared at a larger frequency than the ASVs of other donors (Figure 4B, Table S10). The ASV engraftment rate was the lowest for two donors- D1 and D4, both instances where the fecal material of two cohabiting cats was combined to make one donor. These donors had diverse fecal microbiomes to start with, but not higher than other donors, so it is not completely clear why much fewer ASVs engrafted from these two donors.
The most commonly shared ASVs (ASVs that engrafted > 12 of the 68 FMT recipients) were classified as Bacteroides, Clostridium, Lachnospira, Oscillibacter, Subdoligranulum, Fusobacterium, Clostridium, Blautia, unclassified Butyricicoccaceae, unclassified Oscillospiraceae, unclassified Oscillospirales, and unclassified Lachnospiraceae (Figure 4D, Table S11). Of all of the bacterial ASVs that engrafted across the fecal microbiomes of FMT recipients, 14.56% were classified as Prevotella 9, 10.74% as Peptoclostridium, 7.54% as Bacteroides, 7.33% as unclassified Lachnospiraceae, and 5.29% as Collinsella (Figure 4C). Not surprisingly, the most common genera of engrafted ASVs were also the most abundant bacterial genera across the fecal microbiomes of recipients postFMT and preFMT. Prevotella was found at a mean relative abundance of 14.08% across samples from FMT recipients, Bacteroides at 12.1%, Collinsella at 6.2%, and Peptoclostridium at 5.07% (Table S12). This indicates that FMT recipients are not necessarily gaining taxonomically novel microbes but instead ASVs that are taxonomically similar to those that they start with, albeit with some genomic variation.
Figure 4.
ASVs shared between FMT recipients and their stool donors. Plots of ASV engraftment or sharing rates across A) FMT recipients or B) stool donors (asterisks indicate where the fecal material of two cohabiting cats constituted one donor). ASV sharing rates were calculated by dividing the number of ASVs shared between postFMT samples of FMT recipients and their stool donors (excluding taxa shared between preFMT samples and donors) by the total number of ASVs in the donor sample (excluding any taxa shared with the preFMT samples of FMT recipients). C) Taxonomic breakdown of ASVs shared between FMT recipients and their stool donors. D) Heatmap showing the most commonly engrafted ASVs across FMT recipients. Tan color indicates that the FMT recipient shared that ASV with its stool donor.
Figure 4.
ASVs shared between FMT recipients and their stool donors. Plots of ASV engraftment or sharing rates across A) FMT recipients or B) stool donors (asterisks indicate where the fecal material of two cohabiting cats constituted one donor). ASV sharing rates were calculated by dividing the number of ASVs shared between postFMT samples of FMT recipients and their stool donors (excluding taxa shared between preFMT samples and donors) by the total number of ASVs in the donor sample (excluding any taxa shared with the preFMT samples of FMT recipients). C) Taxonomic breakdown of ASVs shared between FMT recipients and their stool donors. D) Heatmap showing the most commonly engrafted ASVs across FMT recipients. Tan color indicates that the FMT recipient shared that ASV with its stool donor.
3.4. Comparing the fecal microbiomes of FMT recipients and healthy animals
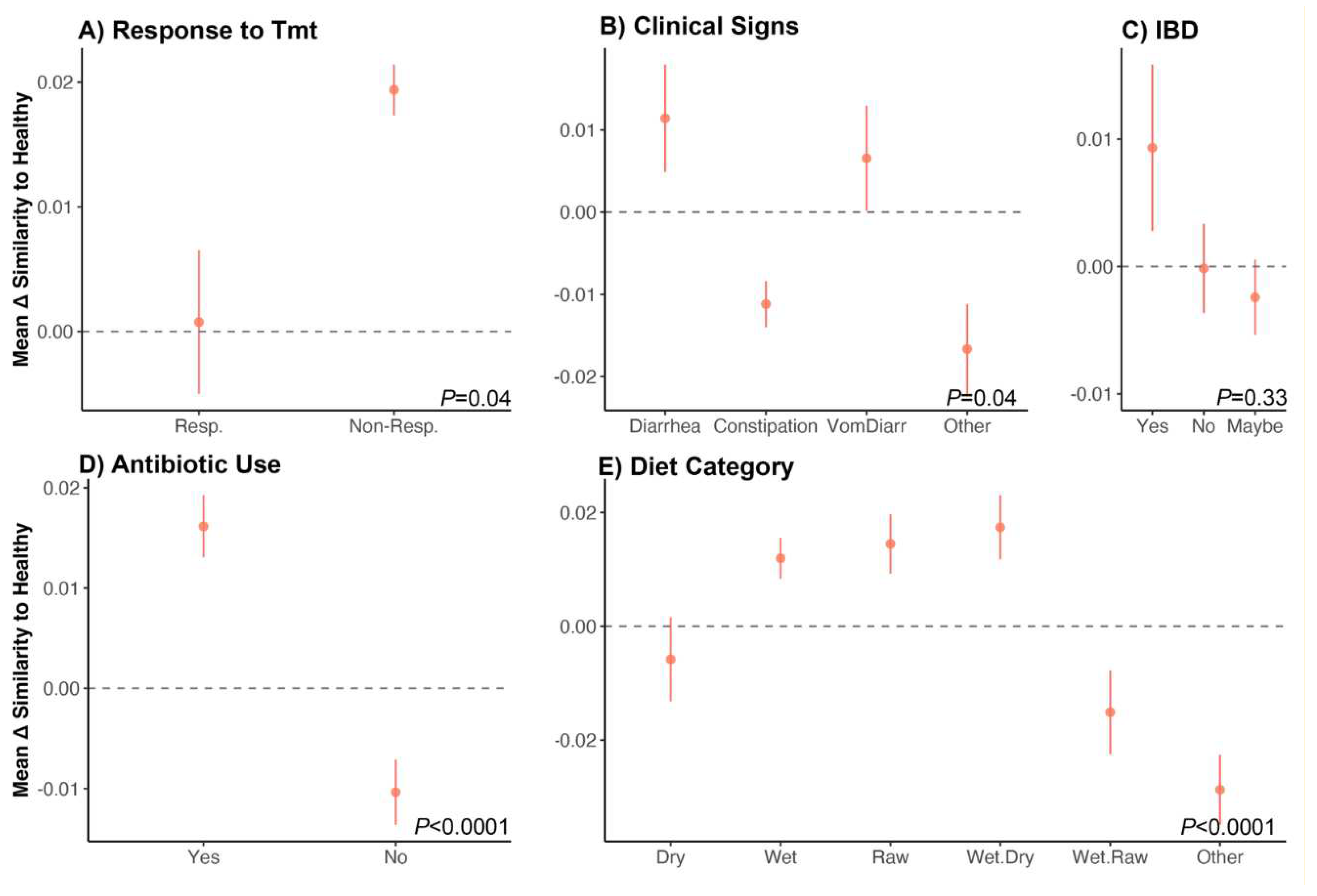
Lastly, we investigated whether the fecal microbiomes of FMT recipients two weeks after the conclusion of treatment became similar to those of age-matched individuals from the healthy reference set (Figure 1C). Perhaps there were groups of cats whose fecal microbiomes shifted closer to those of healthy animals compared to other groups of cats. For this, we computed the similarity between a cat’s preFMT microbiome and a fecal microbiome from the healthy reference set, and the similarity between a cat’s postFMT microbiome and that same healthy cat’s fecal microbiome. We then subtracted the two values (post – pre) to get (Δ) similarity for every FMT recipient – aged-matched healthy animal dyad. The difference between the ages of the FMT recipient and healthy animal must not have exceeded 1 year. This change in similarity (Δ) would indicate whether a cat’s fecal microbiome overall became more (if a positive value) or less (if a negative value) similar to fecal microbiomes from the healthy reference set. We used linear models to test whether an FMT recipient’s response to treatment, clinical signs, IBD diagnosis, prior antibiotic use, or diet correlated with how similar their microbiome became to those of healthy pet cats.
We found that the fecal microbiomes of cats who did not responded favorably to treatment became slightly more similar (mean similarity x̅: 0.01) to those of healthy animals compared to cats who responded well to treatment (x̅ 0.0007) (Figure 5A, Table S13). Additionally, the fecal microbiomes of cats who had diarrhea (x̅ 0.011) or diarrhea with vomiting (x̅ 0.006) became marginally more similar to those of the healthy reference set than cats who experienced other symptoms (x̅ -0.011 for constipation, x̅ -0.016 for ‘Other’ symptoms) (Figure 5B, Table S13). The fecal microbiomes of cats with IBD became equally similar (x̅ 0.009) to those of healthy animals than did cats without IBD (x̅ -0.001) (Figure 5C-D). The fecal microbiomes of cats that had recently taken antibiotics shifted closer to those of healthy animals (x̅ 0.016) compared to animals who had not taken any antibiotics (x̅ -0.01). It is important to note that our effect sizes for these analyses were modest. Lastly, cats that ate only dry food (x̅ -0.005) or wet and raw food (x̅ -0.015) had fecal microbiomes that were less similar to those of healthy animals more than cats with other diets (x̅ 0.011 for wet food, x̅ 0.014 for raw food, x̅ 0.017 for wet and dry food) (Figure 5E, Table S13). This last finding could be simply be an attribute of our dataset: only 13% of healthy animals had a dry food or wet and raw food diet (Table S2). Thus, our findings could differ if diets were more evenly distributed in our dataset in terms of their sample sizes and one diet was not more prevalent than other diets.
Figure 5.
Do the fecal microbiomes of cats receiving FMT treatment become similar to the microbiomes of healthy cats? We examined shifts in the fecal microbiome of FMT recipients by quantifying how similar their fecal microbiomes were (before and after FMT treatment) to those from an age-matched healthy reference set. We computed the difference between the two similarity scores (postFMT similarity - preFMT similarity) to generate the change in similarity (Δ) for each FMT recipient–healthy animal dyad. We then correlated these Δ values with host characteristics using generalized linear models.
A-E) Average Δ similarity scores for each group (± St.Error). A value of 0 indicates no shift in similarity. Bray-Curtis distances were used. See
Table S13 for model statistics.
Figure 5.
Do the fecal microbiomes of cats receiving FMT treatment become similar to the microbiomes of healthy cats? We examined shifts in the fecal microbiome of FMT recipients by quantifying how similar their fecal microbiomes were (before and after FMT treatment) to those from an age-matched healthy reference set. We computed the difference between the two similarity scores (postFMT similarity - preFMT similarity) to generate the change in similarity (Δ) for each FMT recipient–healthy animal dyad. We then correlated these Δ values with host characteristics using generalized linear models.
A-E) Average Δ similarity scores for each group (± St.Error). A value of 0 indicates no shift in similarity. Bray-Curtis distances were used. See
Table S13 for model statistics.
4. Discussion
4.1. Effectiveness of FMT treatment
In our study, 77% of cats that underwent oral capsule FMT treatment for their chronic digestive issues were reported to have an improvement in their clinical signs at two weeks post FMT according to their owners. These cats (termed ‘Responders’) were of distinct ages and sexes, and experienced vomiting, diarrhea, and/or constipation. This means that this particular FMT treatment is potentially effective at alleviating a range of symptoms, not just one particular symptom. Interestingly, a slightly greater proportion of cats with constipation were found in the ‘Responder’ group compared to ‘Non-Responders’ indicating that cats with constipation may be particularly responsive to the treatment. A prior study showed that FMT resolved vomiting and diarrhea in one cat [
29], and our work expands on this and finds that FMT treatment can help resolve constipation, in addition to vomiting and diarrhea in a group of 68 pet cats, as early as two weeks after FMT treatment. In dogs, FMT is effective at treating acute diarrhea, relapsing chronic diarrhea, canine parvovirus, and inflammatory bowel disease [
22,
23,
24,
25].
FMT treatment in the form of oral capsules specifically, has been shown to be effective in treating IBD in 16 dogs [
53]. Furthermore, in a 9 year old dog suffering from chronic enteropathy (CE), a two-cycle oral treatment of FMT was able to resolve all gastrointestinal and systemic symptoms, and restore the dog’s appetite and body weight [
54]. In a larger study involving 56 dogs with CE treated with FMT capsules, clinical signs of improvement – as determined by changes in the canine chronic enteropathy clinical activity index – were observed in 74% of receivers [
55]. Thus, oral capsule FMT treatment shows promise in being able to treat gastrointestinal issues in companion animals. This is significant as oral capsules are easier to administer and are less invasive and likely less costly than administering FMT via an endoscopy, colonoscopy, or via a nasogastric route [
56].
4.2. Host predictors of fecal microbiome alpha- and beta-diversity
The fecal microbiomes of FMT recipients varied depending on the initial clinical signs, IBD diagnosis, and diet of the individual. Specifically, cats that consumed a raw diet had more diverse fecal microbiomes than cats that did not incorporate any raw food in their diet. A raw food diet, which consists of skeletal muscle, fat, tissue, cartilage, and bones, is typically richer in protein and fat and lower in carbohydrates compared to dry kibble or canned wet food [
57]. Our findings are consistent with those of a prior study conducted in dogs, which reported that individuals fed a raw meat diet exhibited more diverse fecal microbiomes than individuals fed commercial foods [
58]; although other studies report a contrasting finding [
59]. Diet is a major determinant of fecal microbiome composition in animals, given that microbes that are able to metabolize the dietary components outcompete those that do not. However, it is not clear why a raw food diet in particular may enable a greater diversity of microbes to co-exist in the gut. We also found that the fecal microbiome beta-diversity of FMT recipients was strongly correlated with host diet. This is expected, as the type of food a cat is eating (raw vs. canned wet food vs. dry kibble) will select for distinct microbiome compositions depending on its protein, fat, carbohydrate, fiber, and macronutrient composition [
60,
61,
62,
63].
We also found that cats with vomiting and diarrhea had less diverse microbiomes than cats experiencing other clinical signs. Host clinical signs in general explained 12% of the variation in fecal microbiomes among individuals. Vomiting, diarrhea, and constipation are usually not standalone symptoms and may reflect distinct disorders or diseases. Diarrhea for example is quite common in felines, and maybe a symptom of a bacterial, protozoan or viral infection [
64]. It may also be a clinical sign of inflammatory bowel disease (IBD) or low-grade lymphoma [
65]. Vomiting is also extremely common in cats [
66], and may be caused by food intolerance, inflammatory bowel disease, liver disease, pancreatitis, hyperthyroidism, and uremia [
67,
68,
69]. Historically, constipation in cats has been tied to dehydration, and is associated with chronic kidney disease (CKD), diabetes mellitus and hyperthyroidism [
70]. It is evident that the clinical symptoms exhibited by cats are strongly tied to their health and physiology, which may partially explain the differences in their fecal microbiomes. Cats with diarrhea compared to cats with constipation or vomiting may have slightly different gastrointestinal physiologies, digestion, gut transit times [
71], or overall health. They may have taken distinct antibiotics or medical treatments to treat their symptoms. All of these differences may be contributing to fecal microbiome divergence among FMT recipients. Overall, our work aligns with prior findings that the fecal microbiome of cats varies with IBD diagnosis [
72] and degrees of intestinal dysbiosis or enteropathy [
73,
74].
Interestingly, our study also reported that the fecal microbiomes of FMT recipients that had recently taken antibiotics became slightly more similar to the healthy reference set than did other surveyed cats. A plethora of studies have shown associations between fecal microbiome composition and antibiotic use in companion animals [
75,
76,
77]. Other studies have also highlighted how FMT treatment might restore fecal microbiome composition after antibiotic-associated disruptions [
78], but here we are discussing how FMT may be effective despite prior antibiotic administration. Perhaps antibiotic administration disrupts the fecal microbiome to an extent, and facilitates the colonization of microbes from FMT capsules or fecal slurries. Oral decontamination with antibiotics appears to enhance the efficacy of FMT in human patients that are colonized by beta-lactamase producing
Enterobacteriaceae or
Acinetobacter [
79,
80]. However, these findings are not widespread and antibiotic use may also enable the growth of pathogenic bacteria. No studies have experimentally compared the effectiveness of FMT treatment after antibiotic administration in cats.
4.3. ASV engraftment rates in FMT recipients
FMT effectiveness can also be assessed by examining which donor microbes were able to colonize the intestine of the recipient following FMT treatment. In our study, we could not directly sample the gut contents of FMT recipients, but we did quantify the degree of ASV sharing between recipients and their stool donors. We found that donors shared about 13% of their ASVs (range 3-36%) with FMT recipients after treatment (excluding ASVs shared between donors and FMT recipients before FMT, which ranged from 54 ASVs to 349 ASVs). This finding indicates that complete microbiome engraftment is not occurring in this group of cats, and may not be necessary for FMT success, given that FMT was still successful in the majority of FMT recipients. Not many FMT studies have quantified engraftment rate, but a prior study reported that in humans with HIV taking antiretroviral medication, modest microbiome engraftment was observed after FMT administration via a colonoscopy. The recipient’s fecal microbiota remained significantly distant from donors eight weeks after FMT [
81]. A small clinical trial of 12 patients who had mild to moderate ulcerative colitis reported that the proportion of bacteria transferred from the donor to the FMT recipient varied from 15% to 85% [
82]. The transferred bacteria spanned the phylogenetic diversity of the donor’s bacteria.
Furthermore, while we found that ASV engraftment rates were not correlated with host factors such as IBD diagnosis, diet, or antibiotic use, these were strongly tied to donor identity. In other words, ASV engraftment rates depended on the fecal microbiome of donors. This echoes prior work which showed that strain engraftment for patients with recurrent
C. difficile (rCDI) infection was largely predicted by the abundance and phylogeny of bacteria in the donor and the bacteria already present in the FMT recipient [
83]. Another study examining FMT treatment in patients with rCDI found that donor-derived strains constituted a larger fraction of the post-FMT microbiota than did novel undetected strains not present in donors or recipients [
84]. These findings reinforce the notion that potential FMT stool donors need to be strictly screened, given the large impact they could have on the fecal microbiomes of FMT recipients. However, we cannot discount the potential influences of the FMT recipient as well. A meta-analysis examined strain engraftment in the gut of human patients across eight disease types, including rCDI, irritable bowel syndrome, Crohn’s disease, renal carcinoma, and Tourette’s syndrome. They reported that the most important predictors of strain-level retention were the diversity and the abundances of bacterial species in FMT recipients [
85]. A similar meta-analysis using some of these same human cohorts found that increased engraftment was observed in individuals that received FMT from multiple routes (e.g. via both capsules and colonoscopy) [
52]. Increased engraftment was also observed in individuals that had been treated with antibiotics for their infections or disease [
52]. Furthermore, as Danne and colleagues (2022) [
86] note, an FMT recipient’s genetics, immunity, microbiota, and lifestyle, may also impact bacterial engraftment and clinical efficacy.
We found that the most commonly shared ASVs belonged to the genus
Prevotella,
Collinsella,
Bacteroides, and
Peptoclostridium. Interestingly, all of these genera form part of the core microbiome in healthy pet cats [
3]. These four bacterial genera are also correlated with SCFA (propionate, acetate, butyrate) production in the mammalian intestine [
87]. SCFAs act as indispensable sources of energy for host colonocytes, stimulate colonic blood flow and motility, and may promote the growth of commensal and resident bacteria [
88,
89,
90]. There is also increasing evidence that gut microbial metabolites like SCFAs may act as regulators of gene expression or as signaling molecules [
91]. Thus, it appears that potentially beneficial microbes are being shared between stool donors and FMT recipients in our cohort of cats. In a study examining strain engraftment in humans treated with FMT for rCDI, the fecal microbiomes of FMT recipients were also enriched in
Bacteroides (and
Alistipes and
Parabacteroides) after FMT [
92].
5. Limitations
Our study has several limitations and we advise readers to interpret our findings with caution. First, the data on FMT effectiveness was solely derived from information provided by pet owners. No diagnostic tests were conducted by a veterinarian to examine whether the animal experienced improvement in their clinical signs based on established metrics (e.g. chronic enteropathy clinical activity index, dysbiosis index). Thus, FMT effectiveness reflects perceived effectiveness by the owner, and is subject to biases and inaccuracies. Nonetheless, even with these limitations, our study provides valuable insights regarding effectiveness of FMT oral capsules in cats with chronic digestive issues.
Second, we did not carry out metagenomic sequencing or measure strain-level patterns when determining bacterial engraftment rates. Our analysis on bacterial sharing was instead done at the level of bacterial ASVs. We also did not directly sample microbes from the GI tract; fecal samples most likely reflect bacteria from the lower portion of the intestine. Thus, we cannot say for sure which bacteria ‘engrafted’ or actually transferred from the stool donor to the FMT recipient.
Lastly, our fecal microbiome surveys reflect the fecal microbiome of FMT recipients at two weeks post-FMT treatment. We do not know how the microbiome changed after those two weeks, nor can we say which bacterial ASVs were retained at 1, 3, 4, or 8 weeks after FMT. Our analyses are focused on the fecal microbiomes of cats during a particular window and we encourage future studies to examine fecal microbiomes at distinct time windows post-FMT.
6. Conclusions
Our study is the first to show that FMT treatment in the form of oral capsules was effective at resolving diarrhea, constipation, and/or vomiting in a group of sixty-eight domestic cats. Fecal microbiome responses to FMT were potentially modulated by an individual’s clinical signs, IBD diagnosis, prior antibiotic use, and diet, which are all factors to consider when studying the fecal microbiomes of cats. Partial stool donor bacterial engraftment was observed in FMT recipients, illustrating that microbes are being shared between a stool donor and its recipient, and that complete microbiome engraftment is not necessary for FMT effectiveness. The fecal microbiomes of certain subsets of FMT recipients grew more similar to those from age-matched healthy individuals, further supporting FMT effectiveness.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Figure S1 Characteristics of “Responder” and “Non-Responder” FMT recipients, Figure S2 Fecal microbiomes of recipient animals do not cluster by timepoint (preFMT vs. postFMT), Figure S3 Posthoc testing of bacterial genera that were found to significantly correlate with host predictors according to a linear model, Table S1 Characteristics of donor animals, Table S2 Characteristics of healthy animals, Table S3 Sample metadata, Table S4 ASV abundance table, Table S5 ASV taxonomy, Table S6 Microbiome Alpha-diversity ~ host predictors (recipient animals), Table S7 Microbiome Beta-diversity ~ host predictors (recipient animals), Table S8 Generalized linear models of 22 core genera ~ host predictors (recipient animals), Table S9 Generalized linear models of 5 pathogenic genera ~ host predictors (recipient animals), Table S10 ASV sharing rates between FMT recipients and their stool donors, Table S11 Taxonomy of ASVs shared between FMT recipients and their stool donors, Table S12 Average abundances of bacterial taxa across preFMT or postFMT samples, Table S13 PERMANOVA of FMT microbiome similarity to the microbiomes of healthy pet cats
Author Contributions
Z.E., J.K.J., G.J., and H.H.G recruited FMT participants, collected and sequenced the fecal samples, and curated the associated metadata. C.A.R. analyzed the data and wrote the manuscript. All authors provided feedback on the manuscript and approved its final version.Conceptualization, H.H.G., A.M., D.D.K. and J.K.J.; Methodology, H.H.G., C.A.R., Z.E., J.K.G., and G.J.; Software, C.A.R. and J.G.; Validation, C.A.R. and J.G.; Formal Analysis, C.A.R. and H.H.G.; Investigation, C.A.R.; Resources, H.H.G. and A.M.; Data Curation, Z.E., J.G., J.K.J. and C.A.R.; Writing – Original Draft Preparation, C.A.R.; Writing – Review & Editing, all authors; Visualization, C.A.R.; Supervision, H.H.G. and C.A.R.; Project Administration, H.H.G.; Funding Acquisition, H.H.G. and A.M.”
Funding
This work was funded in its entirety by AnimalBiome.
Institutional Review Board Statement
The study protocol and informed consent forms were in compliance with the Animal Welfare Act. The capsules were given in addition to the standard of care offered by their veterinarian for the chronic digestive condition. Participants were advised to consult with their veterinarian before participating in the study and they were informed that they could drop out of the study for any reason at any time.
Informed Consent Statement
Not applicable.
Data availability
Raw amplicon sequences are available upon request by emailing the corresponding author. The ASV relative abundance table, ASV taxonomic classifications, and corresponding sample metadata are available as supplementary materials. The R code for conducting all statistical analyses and generating all figures presented in this article is stored in a public GitHub repository (
https://github.com/AnimalBiome/MicrobiomeResponsestoFMT_inCats).
Acknowledgments
We would like to thank the FMT recipients and their owners for participating in our research.
Conflicts of Interest
H.H.G, J.K.G., G.J., D.D.K., A.M., and Z.E. are all employees of AnimalBiome, a company based in Oakland, CA and have stock options. C.A.R is a consultant for AnimalBiome. J.A.E. is an advisor for AnimalBiome and has stock options.
References
- Takiishi T, Fenero CIM, Câmara NOS. Intestinal barrier and gut microbiota: Shaping our immune responses throughout life. Tissue Barriers. 2017;5:e1373208. [CrossRef]
- Yao L, Li X, Zhou Z, Shi D, Li Z, Li S, et al. Age-Based Variations in the Gut Microbiome of the Shennongjia (Hubei) Golden Snub-Nosed Monkey (Rhinopithecus roxellana hubeiensis). Biomed Res Int. 2021;2021:6667715. [CrossRef]
- Ganz HH, Jospin G, Rojas CA, Martin AL, Dahlhausen K, Kingsbury DD, et al. The Kitty Microbiome Project: Defining the Healthy Fecal “Core Microbiome” in Pet Domestic Cats. Veterinary Sciences. 2022;9:635. [CrossRef]
- Taggart PL, Liddicoat C, Tong WH, Breed MF, Weinstein P, Wheeler D, et al. Gut microbiota composition does not associate with toxoplasma infection in rats. Mol Ecol. 2022;31:3963–70. [CrossRef]
- Chun JL, Ji SY, Lee SD, Lee YK, Kim B, Kim KH. Difference of gut microbiota c-mposition based on the body condition scores in dogs. Hanguk Tongmul Chawon Kwahakhoe Chi. 2020;62:239–46.
- Li F, Yang S, Zhang L, Qiao L, Wang L, He S, et al. Comparative metagenomics analysis reveals how the diet shapes the gut microbiota in several small mammals. Ecol Evol. 2022;12:e8470. [CrossRef]
- Hickmott AJ, Waller MT, Wakefield ML, Malone N, Brand CM, White FJ. A Test of Foraging Models Using Dietary Diversity Indices for the Lomako Forest Bonobos. Folia Primatol . 2021;92:211–26. [CrossRef]
- Eisenhofer R, Helgen KM, Taggart D. Signatures of landscape and captivity in the gut microbiota of Southern Hairy-nosed Wombats (Lasiorhinus latifrons). Anim Microbiome. 2021;3:4. [CrossRef]
- Wolf JF, Kriss KD, MacAulay KM, Munro K, Patterson BR, Shafer ABA. Gut microbiome composition predicts summer core range size in two divergent ungulates. FEMS Microbiol Ecol. 2021;97:fiab048. [CrossRef]
- Bornbusch SL, Harris RL, Grebe NM, Roche K, Dimac-Stohl K, Drea CM. Antibiotics and fecal transfaunation differentially affect microbiota recovery, associations, and antibiotic resistance in lemur guts. Anim Microbiome. 2021;3:65. [CrossRef]
- Sabey KA, Song SJ, Jolles A, Knight R, Ezenwa VO. Coinfection and infection duration shape how pathogens affect the African buffalo gut microbiota. ISME J. 2021;15:1359–71. [CrossRef]
- Zhao W, Ren Z, Luo Y, Cheng J, Wang J, Wang Y, et al. Metagenomics analysis of the gut microbiome in healthy and bacterial pneumonia forest musk deer. Genes Genomics. 2021;43:43–53. [CrossRef]
- Chen H, Mozzicafreddo M, Pierella E, Carletti V, Piersanti A, Ali SM, et al. Dissection of the gut microbiota in mothers and children with chronic Trichuris trichiura infection in Pemba Island, Tanzania. Parasit Vectors. 2021;14:62.
- Sencio V, Gallerand A, Gomes Machado M, Deruyter L, Heumel S, Soulard D, et al. Influenza Virus Infection Impairs the Gut’s Barrier Properties and Favors Secondary Enteric Bacterial Infection through Reduced Production of Short-Chain Fatty Acids. Infect Immun. 2021;89:e0073420. [CrossRef]
- Wang S, El-Fahmawi A, Christian DA, Fang Q, Radaelli E, Chen L, et al. Infection-Induced Intestinal Dysbiosis Is Mediated by Macrophage Activation and Nitrate Production. MBio. 2019;10. [CrossRef]
- Bertolini M, Ranjan A, Thompson A, Diaz PI, Sobue T, Maas K, et al. Candida albicans induces mucosal bacterial dysbiosis that promotes invasive infection. PLoS Pathog. 2019;15:e1007717. [CrossRef]
- Zheng L, Ji Y-Y, Wen X-L, Duan S-L. Fecal microbiota transplantation in the metabolic diseases: Current status and perspectives. World J Gastroenterol. 2022;28:2546–60. [CrossRef]
- Niederwerder MC. Fecal microbiota transplantation as a tool to treat and reduce susceptibility to disease in animals. Vet Immunol Immunopathol. 2018;206:65–72. [CrossRef]
- Tuniyazi M, Hu X, Fu Y, Zhang N. Canine Fecal Microbiota Transplantation: Current Application and Possible Mechanisms. Vet Sci China. 2022;9. [CrossRef]
- DePeters EJ, George LW. Rumen transfaunation. Immunol Lett. 2014;162 2 Pt A:69–76.
- Mandal, Joshi, Balamurugan. Rumen transfaunation an effective method for treating simple indigestion in ruminants. North East J Leg Stud.
- Chaitman J, Ziese A-L, Pilla R, Minamoto Y, Blake AB, Guard BC, et al. Fecal Microbial and Metabolic Profiles in Dogs With Acute Diarrhea Receiving Either Fecal Microbiota Transplantation or Oral Metronidazole. Front Vet Sci. 2020;7:192. [CrossRef]
- Pereira GQ, Gomes LA, Santos IS, Alfieri AF, Weese JS, Costa MC. Fecal microbiota transplantation in puppies with canine parvovirus infection. J Vet Intern Med. 2018;32:707–11. [CrossRef]
- Niina A, Kibe R, Suzuki R, Yuchi Y, Teshima T, Matsumoto H, et al. Fecal microbiota transplantation as a new treatment for canine inflammatory bowel disease. Biosci Microbiota Food Health. 2021;40:98–104. [CrossRef]
- Collier A. Fecal Microbiota alterations in illness and efficacy of fecal Microbiota transplantation in treatment of inflammatory bowel disease in dogs. University of Guelph; 2022.
- Niederwerder MC, Constance LA, Rowland RRR, Abbas W, Fernando SC, Potter ML, et al. Fecal Microbiota Transplantation Is Associated With Reduced Morbidity and Mortality in Porcine Circovirus Associated Disease. Front Microbiol. 2018;9:1631. [CrossRef]
- Burton EN, O’Connor E, Ericsson AC, Franklin CL. Evaluation of Fecal Microbiota Transfer as Treatment for Postweaning Diarrhea in Research-Colony Puppies. J Am Assoc Lab Anim Sci. 2016;55:582–7.
- Wang J-W, Kuo C-H, Kuo F-C, Wang Y-K, Hsu W-H, Yu F-J, et al. Fecal microbiota transplantation: Review and update. J Formos Med Assoc. 2019;118 Suppl 1:S23–31. [CrossRef]
- Weese, Costa, Webb. Preliminary clinical and microbiome assessment of stool transplantation in the dog and cat. J At Mol Phys.
- Furmanski, Mor. First case report of fecal microbiota transplantation in a cat in Israel. Isr J Vet Med.
- Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920–4. [CrossRef]
- Comeau André M., Douglas Gavin M., Langille Morgan G. I. Microbiome Helper: a Custom and Streamlined Workflow for Microbiome Research. mSystems. 2017;2:e00127–16.
- Pichler M, Coskun ÖK, Ortega-Arbulú A-S, Conci N, Wörheide G, Vargas S, et al. A 16S rRNA gene sequencing and analysis protocol for the Illumina MiniSeq platform. Microbiologyopen. 2018;7:e00611. [CrossRef]
- Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP. DADA2: High-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13:581–3. [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. 2021.
- Quast C, Pruesse E, Yilmaz P, Gerken J, Schweer T, Yarza P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41 Database issue:D590–6.
- Yilmaz P, Parfrey LW, Yarza P, Gerken J, Pruesse E, Quast C, et al. The SILVA and “All-species Living Tree Project (LTP)” taxonomic frameworks. Nucleic Acids Res. 2013;42:D643–8.
- McMurdie PJ, Holmes S. Waste not, want not: why rarefying microbiome data is inadmissible. PLoS Comput Biol. 2014;10:e1003531. [CrossRef]
- McMurdie PJ, Holmes S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS One. 2013;8:e61217. [CrossRef]
- Lahti L, Shetty S, Others. Introduction to the microbiome R package. 2018.
- Kembel SW, Cowan PD, Helmus MR, Cornwell WK, Morlon H, Ackerly DD, et al. Picante: R tools for integrating phylogenies and ecology. Bioinformatics. 2010;26:1463–4. [CrossRef]
- Wright. Using DECIPHER v2. 0 to analyze big biological sequence data in R. R J.
- Schliep KP. phangorn: phylogenetic analysis in R. Bioinformatics. 2011;27:592–3. [CrossRef]
- Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models using lme4. arXiv [stat.CO]. 2014.
- Fox J, Weisberg S. An R Companion to Applied Regression. SAGE Publications; 2018.
- Wickham H. ggplot2: elegant graphics for data analysis Springer-Verlag New York; 2009. 2016.
- Oksanen J. vegan : Community Ecology Package. R package version 1.8-5. http://www.cran.r-project.org. 2007.
- Grześkowiak Ł, Endo A, Beasley S, Salminen S. Microbiota and probiotics in canine and feline welfare. Anaerobe. 2015;34:14–23. [CrossRef]
- Suchodolski JS. Companion animals symposium: microbes and gastrointestinal health of dogs and cats. J Anim Sci. 2011;89:1520–30. [CrossRef]
- Dumitru A, Aliuş C, Nica AE, Antoniac I, Gheorghiță D, Grădinaru S. Fatal outcome of gastric perforation due to infection with Sarcina spp. A case report. IDCases. 2020;19:e00711. [CrossRef]
- Griego RD, Rosen T, Orengo IF, Wolf JE. Dog, cat, and human bites: a review. J Am Acad Dermatol. 1995;33:1019–29. [CrossRef]
- Ianiro G, Punčochář M, Karcher N, Porcari S, Armanini F, Asnicar F, et al. Variability of strain engraftment and predictability of microbiome composition after fecal microbiota transplantation across different diseases. Nat Med. 2022;28:1913–23. [CrossRef]
- Bottero E, Benvenuti E, Ruggiero P, Others. Fecal microbiota transplantation (FMT) in 16 dogs with idiopathic IBD. Veterinaria. 2017;31:31–45.
- Berlanda M, Innocente G, Simionati B, Di Camillo B, Facchin S, Giron MC, et al. Faecal Microbiome Transplantation as a Solution to Chronic Enteropathies in Dogs: A Case Study of Beneficial Microbial Evolution. Animals (Basel). 2021;11. [CrossRef]
- Innocente G, Patuzzi I, Furlanello T, Di Camillo B, Bargelloni L, Giron MC, et al. Machine Learning and Canine Chronic Enteropathies: A New Approach to Investigate FMT Effects. Vet Sci China. 2022;9. [CrossRef]
- Gulati M, Singh SK, Corrie L, Kaur IP, Chandwani L. Delivery routes for faecal microbiota transplants: Available, anticipated and aspired. Pharmacol Res. 2020;159:104954. [CrossRef]
- Butowski CF, Moon CD, Thomas DG, Young W, Bermingham EN. The effects of raw-meat diets on the gastrointestinal microbiota of the cat and dog: a review. N Z Vet J. 2022;70:1–9. [CrossRef]
- Kim J, An J-U, Kim W, Lee S, Cho S. Differences in the gut microbiota of dogs (Canis lupus familiaris) fed a natural diet or a commercial feed revealed by the Illumina MiSeq platform. Gut Pathog. 2017;9:68. [CrossRef]
- Schmidt M, Unterer S, Suchodolski JS, Honneffer JB, Guard BC, Lidbury JA, et al. The fecal microbiome and metabolome differs between dogs fed Bones and Raw Food (BARF) diets and dogs fed commercial diets. PLoS One. 2018;13:e0201279. [CrossRef]
- Bermingham EN, Young W, Butowski CF, Moon CD, Maclean PH, Rosendale D, et al. The Fecal Microbiota in the Domestic Cat (Felis catus) Is Influenced by Interactions Between Age and Diet; A Five Year Longitudinal Study. Front Microbiol. 2018;9:1231. [CrossRef]
- Wernimont SM, Radosevich J, Jackson MI, Ephraim E, Badri DV, MacLeay JM, et al. The Effects of Nutrition on the Gastrointestinal Microbiome of Cats and Dogs: Impact on Health and Disease. Front Microbiol. 2020;11:1266. [CrossRef]
- Li Q, Pan Y. Differential Responses to Dietary Protein and Carbohydrate Ratio on Gut Microbiome in Obese vs. Lean Cats. Front Microbiol. 2020;11:591462. [CrossRef]
- Paßlack N, Thies LV, Vahjen W, Zentek J. Effects of the Protein Concentration and Quality in a Canned Diet on the Fecal Microbiota of Healthy Adult Cats. Metabolites. 2022;12. [CrossRef]
- Cook AK. Feline infectious diarrhea. Top Companion Anim Med. 2008;23:169–76. [CrossRef]
- Barrs VR, Beatty JA. Feline alimentary lymphoma: 1. Classification, risk factors, clinical signs and non-invasive diagnostics. J Feline Med Surg. 2012;14:182–90.
- Lund EM, Armstrong PJ, Kirk CA, Kolar LM, Klausner JS. Health status and population characteristics of dogs and cats examined at private veterinary practices in the United States. J Am Vet Med Assoc. 1999;214:1336–41.
- Batchelor DJ, Devauchelle P, Elliott J, Elwood CM, Freiche V, Gualtieri M, et al. Mechanisms, causes, investigation and management of vomiting disorders in cats: a literature review. J Feline Med Surg. 2013;15:237–65. [CrossRef]
- Hauck SR, Gisselman K, Cordner A, Nicholson AG. Chronic Vomiting in Cats: Etiology and Diagnostic Testing. J Am Anim Hosp Assoc. 2016;52:269–76.
- Peterson ME, Kintzer PP, Cavanagh PG, Fox PR, Ferguson DC, Johnson GF, et al. Feline hyperthyroidism: pretreatment clinical and laboratory evaluation of 131 cases. J Am Vet Med Assoc. 1983;183:103–10.
- Bertoy RW. Megacolon in the cat. Vet Clin North Am Small Anim Pract. 2002;32:901–15.
- Russo M, Martinelli M, Sciorio E, Botta C, Miele E, Vallone G, et al. Stool consistency, but not frequency, correlates with total gastrointestinal transit time in children. J Pediatr. 2013;162:1188–92. [CrossRef]
- Marsilio S, Pilla R, Sarawichitr B, Chow B, Hill SL, Ackermann MR, et al. Characterization of the fecal microbiome in cats with inflammatory bowel disease or alimentary small cell lymphoma. Sci Rep. 2019;9:19208. [CrossRef]
- Sung C-H, Marsilio S, Chow B, Zornow KA, Slovak JE, Pilla R, et al. Dysbiosis index to evaluate the fecal microbiota in healthy cats and cats with chronic enteropathies. J Feline Med Surg. 2022;24:e1–12. [CrossRef]
- Kathrani A, Yen S, Swann JR, Hall EJ. The effect of a hydrolyzed protein diet on the fecal microbiota in cats with chronic enteropathy. Sci Rep. 2022;12:2746. [CrossRef]
- Stavroulaki EM, Suchodolski JS, Pilla R, Fosgate GT, Sung C-H, Lidbury JA, et al. Short- and long-term effects of amoxicillin/clavulanic acid or doxycycline on the gastrointestinal microbiome of growing cats. PLoS One. 2021;16:e0253031. [CrossRef]
- Schmid SM, Suchodolski JS, Price JM, Tolbert MK. Omeprazole Minimally Alters the Fecal Microbial Community in Six Cats: A Pilot Study. Front Vet Sci. 2018;5:79. [CrossRef]
- Whittemore JC, Stokes JE, Price JM, Suchodolski JS. Effects of a synbiotic on the fecal microbiome and metabolomic profiles of healthy research cats administered clindamycin: a randomized, controlled trial. Gut Microbes. 2019;10:521–39. [CrossRef]
- Mullish BH, McDonald JAK, Thursz MR, Marchesi JR. Antibiotic-Associated Disruption of Microbiota Composition and Function in Cirrhosis Is Restored by Fecal Transplant. Hepatology. 2018;68:1205. [CrossRef]
- Saïdani N, Lagier J-C, Cassir N, Million M, Baron S, Dubourg G, et al. Faecal microbiota transplantation shortens the colonisation period and allows re-entry of patients carrying carbapenamase-producing bacteria into medical care facilities. Int J Antimicrob Agents. 2019;53:355–61. [CrossRef]
- Mullish BH, Ghani R, McDonald JAK, Marchesi JR. Faecal microbiota transplant for eradication of multidrug-resistant Enterobacteriaceae: a lesson in applying best practice? Re: “A five-day course of oral antibiotics followed by faecal transplantation to eradicate carriage of multidrug-resistant Enterobacteriaceae: A Randomized Clinical Trial.” Clinical Microbiology and Infection. 2019;25:912–3. [CrossRef]
- Vujkovic-Cvijin I, Rutishauser RL, Pao M, Hunt PW, Lynch SV, McCune JM, et al. Limited engraftment of donor microbiome via one-time fecal microbial transplantation in treated HIV-infected individuals. Gut Microbes. 2017;8:440–50. [CrossRef]
- Chu ND, Crothers JW, Nguyen LTT, Kearney SM, Smith MB, Kassam Z, et al. Dynamic Colonization of Microbes and Their Functions after Fecal Microbiota Transplantation for Inflammatory Bowel Disease. MBio. 2021;12:e0097521. [CrossRef]
- Smillie CS, Sauk J, Gevers D, Friedman J, Sung J, Youngster I, et al. Strain Tracking Reveals the Determinants of Bacterial Engraftment in the Human Gut Following Fecal Microbiota Transplantation. Cell Host Microbe. 2018;23:229–40.e5. [CrossRef]
- Podlesny D, Fricke WF. Microbial strain engraftment, persistence and replacement after fecal Microbiota transplantation. bioRxiv. 2020.
- Schmidt TSB, Li SS, Maistrenko OM, Akanni W, Coelho LP, Dolai S, et al. Drivers and determinants of strain dynamics following fecal microbiota transplantation. Nat Med. 2022;28:1902–12. [CrossRef]
- Danne C, Rolhion N, Sokol H. Recipient factors in faecal microbiota transplantation: one stool does not fit all. Nat Rev Gastroenterol Hepatol. 2021;18:503–13. [CrossRef]
- Butowski CF, Thomas DG, Young W, Cave NJ, McKenzie CM, Rosendale DI, et al. Addition of plant dietary fibre to a raw red meat high protein, high fat diet, alters the faecal bacteriome and organic acid profiles of the domestic cat (Felis catus). PLoS One. 2019;14:e0216072. [CrossRef]
- Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell. 2016;165:1332–45. [CrossRef]
- Richards JL, Yap YA, McLeod KH, Mackay CR, Mariño E. Dietary metabolites and the gut microbiota: an alternative approach to control inflammatory and autoimmune diseases. Clin Transl Immunology. 2016;5:e82. [CrossRef]
- Louis P, Flint HJ. Formation of propionate and butyrate by the human colonic microbiota. Environ Microbiol. 2017;19:29–41. [CrossRef]
- Sun M, Wu W, Liu Z, Cong Y. Microbiota metabolite short chain fatty acids, GPCR, and inflammatory bowel diseases. J Gastroenterol. 2017;52:1–8. [CrossRef]
- Hamilton MJ, Weingarden AR, Unno T, Khoruts A, Sadowsky MJ. High-throughput DNA sequence analysis reveals stable engraftment of gut microbiota following transplantation of previously frozen fecal bacteria. Gut Microbes. 2013;4:125–35. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).