Submitted:
13 January 2023
Posted:
16 January 2023
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
2. Literature Review
2.1. Management of Beds in Emergency Departments and Inpatient Care Units
2.2. The Importance of Bed Management
3. Methodological Procedures
3.1. Case study Selection and Characterization
3.2. Data Collection
4. Results
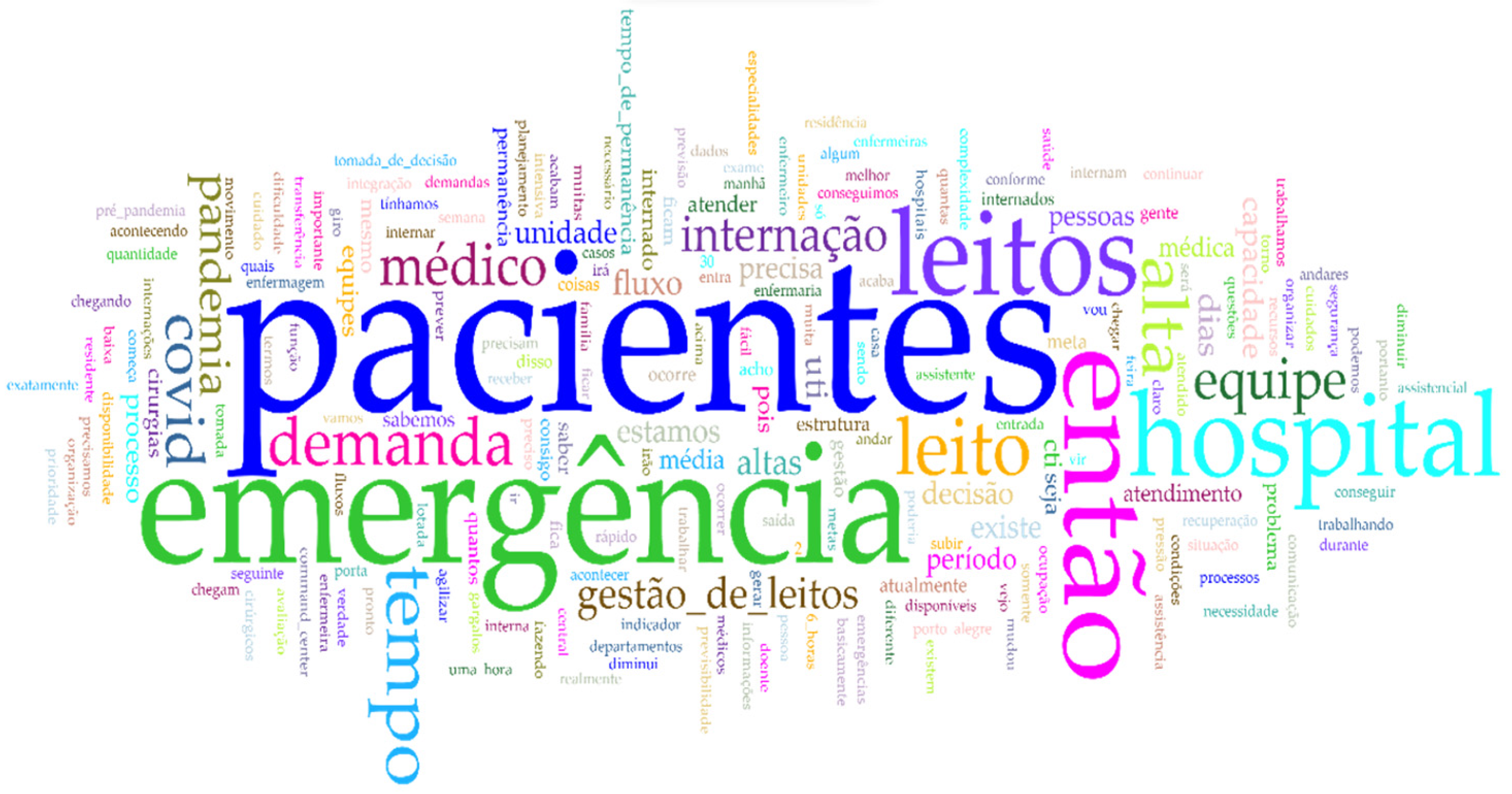
4.1. Textual Analysis and Triangulation of Factors for BM
5. Discussion
5.1. Family or Patient
5.2. Communication
5.3. Lenght of Stay
5.4. Discharge Planning by the Team
5.5. Performance Goals
5.6. Decisions Shared Between Units
5.7. Bed Occupancy Planning
5.8. Nurses
6. Final Considerations
Appendix A
| Questions |
|---|
| 1. Please tell us briefly about your career experience so far. What is your current job? How long have you been in this role? What are your functions and main activities? 2. How do you plan the number of beds to meet the emergency demand? 3. How does decision-making occur in emergency bed management? Do you consider that there is any inefficiency in this process? What is missing for this process to be efficient? 4. How do you predict the volume of patients? Do you use any method to predict the arrival of patients? If yes, what is the method, and how is it applied? What are the advantages and disadvantages of this method? 5. What are the main difficulties in bed management? Are there bottlenecks (factors that delay) or facilitators (factors that benefit) in this process? Name the ones that occur most often and that you remember. For each bottleneck indicated, what actions are taken to reduce its effects? 6. Regarding bed management in your emergency service, which management components are not automatable and create a demand for the manager's decision? 7. Can you anticipate future occupancy in the short term? If so, how and for how long? If not, why? 8. Is there any document (report) that identifies the seasonality of the emergency department's attendance in recent years? If so, can we have access? 9. In the context of bed management in the ED, is there anything you would like to highlight? Any final thoughts? |
References
- Adwok, J. (2014). Application of Brim’s and Simon’s Sequential Decision Theories in Healthcare Administration. Journal of Biology, Agriculture and Healthcare, 4(14), 23–32.
- Alonso, C. da S., De Souza Pires Silva, D. E., Da Cruz Costa, F., Esmério Pimentel, F., Vieira Novaes, J. A., & Cabral de Castro e Silva, R. R. (2022). Desafios enfrentados por enfermeiros na gestão de leitos hospitalares durante a pandemia por COVID-19. Nursing (São Paulo), 25(291), 8342–8351. [CrossRef]
- American College of Emergency Physicians – ACEP. (2019). Crowding. Policy statement. Annals of Emergency Medicine, 61(6), 726–727. https://www.acep.org/patient-care/policy-statements/crowding/.
- BARDIN, L. Análise de conteúdo. São Paulo: edições 70, 2016. 280p. ISBN: 978-85-62938-04-7.
- Borges, F., Bernardino, E., Stegani, M. M., & Tonini, N. S. (2020). Performance of nurses in the bed management service of a teaching hospital. Revista Brasileira de Nursing, 73(4), 1–8. [CrossRef]
- Bryan, K., Gage, H., & Gilbert, K. (2006). Delayed transfers of older people from hospital: Causes and policy implications. Health Policy, 76(2), 194–201. [CrossRef]
- Camargo, B. V., & Justo, A. M. (2013). IRAMUTEQ: Um software gratuito para análise de dados textuais. Temas Em Psicologia, 21(2), 513–518. [CrossRef]
- Creswell, J. W., & Creswell, J. D. (2018). Research Design: Qualitative, Quantitative, and Mixed Methods Approaches (5th ed.). Sage publications.
- D’Aquino, S. F. (2017). Proposta de modelo de referência para o processo de gestão de leitos hospitalares. [Masters dissertation, Universidade Federal de Santa Catarina]. Repositório Institucional da UFSC. https://repositorio.ufsc.br/xmlui/handle/123456789/183604.
- Emergency Nurses Association – ENA. (2006). Emergency nurses association position statement: Crowding in the emergency department. Journal of Emergency Nursing, 32(1), 42–47. [CrossRef]
- Fiocruz. (2021). Observatório COVID-19 aponta maior colapso sanitário e hospitalar da história do Brasil. Fundação Oswaldo Cruz (Fiocruz). https://portal.fiocruz.br/sites/portal.fiocruz.br/files/documentos/boletim_extraordinario_2021-marco-16-red-red-red.pdf.
- Fogaça, C. S., Braga, L. A. S., Peres de Carvalho, E. M., & Göttems, L. B. D. (2021). Atuação do enfermeiro no gerenciamento dos leitos hospitalares na percepção dos profissionais de enfermagem. New Trends in Qualitative Research, 8, 528–537. [CrossRef]
- Fontana, G., Chesani, F. H., & Menezes, M. (2017). As significações dos profissionais da saúde sobre o processo de alta hospitalar. Health & Social Change, 8(2), 86–95.
- Fontana, G., Chesani, F. H., & Nalin, F. (2017). Percepções dos profissionais da saúde sobre o processo de alta hospitalar. Revista Da UNIFEBE, 1(21), 138–156.
- He, L., Chalil Madathil, S., Oberoi, A., Servis, G., & Khasawneh, M. T. (2019). A systematic review of research design and modeling techniques in inpatient bed management. Computers and Industrial Engineering, 127(October 2018), 451–466. [CrossRef]
- Jones, R. (2009). Emergency admissions and hospital beds. British Journal of Health Care Management, 15(6), 289–296. [CrossRef]
- La Forgia, G. M., & Couttolenc, B. F. (2009). Desempenho hospitalar no Brasil: em busca da excelência (1st ed.). Singular. https://pesquisa.bvsalud.org/portal/resource/pt/lil-695495.
- Landa, P., Sonnessa, M., Tànfani, E., & Testi, A. (2018). Multiobjective bed management considering emergency and elective patient flows. International Transactions in Operational Research, 25(1), 91–110. [CrossRef]
- Machado, D. de C., & Machado, A. C. A. (2019). A otimização do processo de gerenciamento de leitos e alta hospitalar. Revista Saúde Coletiva, 9(50), 1866–1872.
- Matos, F. de, & Bastos, C. M. de A. M. (2022). A interação dos setores no processo de gestão de leitos hospitalares. Scientia Academicus, 3(1), 2–16.
- Mattos, C. M., Farias de Oliveira, M. F. de O., Alves Vilar, A. M., Silvino, Z. R., Silvino, Z. R., & Andrade, M. (2019). A aplicação do Kanban como ferramenta de gestão em serviços de saúde: revisão integrativa. Nursing (São Paulo), 22(254), 3031–3038. [CrossRef]
- Melo, T. M., & Fucidji, J. R. (2016). Racionalidade limitada e a tomada de decisão em sistemas complexos. Revista de Economia Política, 36(3), 622–645. [CrossRef]
- Noronha, K. de S. V. M., Guedes, G. R., Turra, C. M., Andrade, M. V., Botega, L., Nogueira, D., Calazans, J. A., Carvalho, L., Servo, L., & Ferreira, M. F. (2020). Pandemia por COVID-19 no Brasil: análise da demanda e da oferta de leitos hospitalares e equipamentos de ventilação assistida segundo diferentes cenários. Cadernos de Saúde Pública, 36(6), 1–17. [CrossRef]
- Oliveira, B. D. P., & Bittencourt, R. J. (2020). Avaliação por triangulação de métodos de um núcleo de gestão de leitos em um hospital público do Distrito Federal. Revista de Gestão Em Sistemas de Saúde, 9(3), 406–432. [CrossRef]
- Oliveira, I. S. de, Lima, E. de F. A., Silva, R. I. C. da, Figueiredo, K. C., Dias, I. C. B., & Primo, C. C. (2020). Gerenciamento de leitos na urgência e emergência utilizando o kanban. Research, Society and Development, 9(10), e1329108354. [CrossRef]
- OPAS. (2021). Folha informativa sobre COVID-19. Organização Pan-Americana Da Saúde (OPAS). https://www.paho.org/pt/COVID-1919.
- Raffa, C. (2017). Análise das variáveis do ambiente interno para o gerenciamento de leitos em organizações hospitalares privadas. [Doctoral thesis, Fundação Getulio Vargas - Escola de Administração de Empresas de São Paulo]. http://hdl.handle.net/10438/18070.
- Raffa, C., Malik, A. M., & Pinochet, L. H. C. (2017a). A Tecnologia da informação no apoio À Gestão De Leitos: Um Estudo Multicaso Em Hospitais Privados. Revista Administração Em Diálogo, 19(3), 1–23. [CrossRef]
- Raffa, C., Malik, A. M., & Pinochet, L. H. C. (2017b). Análise das variáveis do ambiente Interno no gerenciamento de leitos em organizações hospitalares privadas: aplicação do software Nvivo. Revista de Administração Hospitalar e Inovação Em Saúde, 14(4), 20–39. [CrossRef]
- Raffa, C., Malik, A. M., & Pinochet, L. H. C. (2017c). O desafio de mapear variáveis na gestão de leitos em organizações hospitalares privadas. Revista de Gestão Em Sistemas de Saúde, 6(2), 124–141. [CrossRef]
- Richardson, R. J. (2009). Pesquisa social: métodos e técnicas (J. A. de S. Peres (ed.); 3rd ed.). Atlas.
- Rocha, H. A. L., Santos, A. K. L. da C., Alcântara, A. C. de C., Lima, C. S. S. da C., Rocha, S. G. M. O., Cardoso, R. M., & Cremonin, J. R. (2018). Bed management team with Kanban web-based application. International Journal for Quality in Health Care, 30(9), 708–714. [CrossRef]
- Silva, T. G. E., Silva, M. F. S. B. da, Vieira, L. C. N., Pimentel, C. A., & Musetti, M. A. (2021). Contribuições do kanban eletrônico e tradicional para a gerenciamento de leitos hospitalares. Revista Produção Online, 21(3), 818–836. [CrossRef]
- Silva, S. A. da, Valácio, R. A., Botelho, F. C., & Amaral, C. F. S. (2014). Fatores de atraso na alta hospitalar em hospitais de ensino. Revista de Saúde Pública, 48(2), 314–321. [CrossRef]
- Sinclair, S., & Rockwell, G. (2016). Voyant Tools. GitHub. http://voyant-tools.org/.
- SMS. (2021). Painel Diário COVID-19. Secretaria Municipal de Saúde (SMS) da Prefeitura Municipal de Porto Alegre. Painel Diário Coronavírus Secretaria Municipal de Saúde (SMS) Da Prefeitura Municipal de Porto Alegre. http://lproweb.procempa.com.br/pmpa/prefpoa/sms/usu_doc/painelcovi15marco.pdf.
- Souza, D. M., Vasconcelos, B. F., Viana, D. M. S., Ribeiro, L. da C. C., & Lima, A. M. D. J. (2020). Gestão de leitos em um hospital polo da região ampliada de saúde Jequitinhonha: aspectos organizacionais e operacionais do processo de trabalho. Journal of Health & Biological Sciences, 8(1), 1–5. [CrossRef]
- Suzuki, V. F., Carmona, E. V., & Lima, M. H. M. (2011). Planejamento da alta hospitalar do paciente diabético: construção de uma proposta. Revista da Escola de Nursing da USP, 45(2), 527–532. [CrossRef]
- Tampubolon, L., & Pujiyanto. (2018). Bed management strategy for overcrowding at the emergency department: A systematic review. KnE Life Sciences, 4(9), 50–59. [CrossRef]
- Wasgen, A. M., Terres, M. da S., & Machado, B. F. H. (2019). O impacto do gerenciamento de leitos na gestão hospitalar. Revista Hospitalidade, 16(2), 31–49. [CrossRef]
- Werner, S. M. (2017). Proposta de um modelo de gestão para alta hospitalar baseado na abordagem Lean. [Masters dissertation, Universidade Federal de Santa Catarina]. https://repositorio.ufsc.br/xmlui/handle/123456789/179794.
- Yin, R. K. (2014). Case study research design and methods (5th ed.). Sage publications.
| Authors | Research objective | Title* | Research method | Main results |
|---|---|---|---|---|
| Raffa & Malik (2017b) | Identifying variables related to the internal environment relevant to bed management in hospital organisations | Analysis of internal environmental variables in bed management in private hospital organizations: application of NVivo software | Systematic literature review, case study, and content analysis | Concerning the resource management practices, the author highlighted: occupancy planning, decision autonomy, and the use of goals and indicators. Regarding structural characteristics of service delivery, the hospital structure, information technology, equipment, and human resources stand out. In respect of processes, there are discharge planning, formalization, and clinical and communication protocols, which are determinants for management. Regarding operationalization, the decision-making of physicians and nurses' management knowledge were also factors that impacted BM. These authors concluded that these are the relevant internal factors for the performance and efficiency of BM. However, policies were inadequate and could be improved to achieve the organization's strategies, highlighting that it constitutes a strategic resource in hospitals. |
| Matos & Bastos (2018) | Introducing the complexity of BM and the importance of inter-sector teams’ interaction in the BM process | The interaction of the sectors in the process of management of hospital Beds | Scoping review | Communication and interaction between sectors can contribute to improving the management of hospital beds. |
| Rocha et al. (2018) | Measuring the effectiveness of e-Kanban in managing beds in a high complexity, private and accredited hospital | Bed management team with Kanban web-based application | Intervention research | The use of the e-Kaban tool in the management of hospital beds enabled the systematic monitoring and evaluation of patients by the multidisciplinary team. Kanban is continuously accessed via tablets, cell phones, or computers, reducing overall LOS and increasing bed turnover without reducing the occupancy rate. Finally, there was a decrease in the waiting time for hospitalization in EDs. |
| Wasgen et al. (2019) | Creating a theoretical model for BM | The impact of bedside management on hospital management | Literature review | According to the authors, the hospitals that adopted the measures proposed by their theoretical model can optimize the LOS of patients and increase the number of patients seen. |
| Machado & Machado (2019) | Identifying the reasons that interfere with hospital discharge and that impact on BM | Optimization of the hospital bed and hospital discharge management process | Integrative review | The main reasons are factors such as hospital discharge, lack of communication, discharge planning by the team, family refusal to remove the patient from the bed, and the increase of the LOS. These authors concluded that greater integration and effective team communication added to patients' follow-up through therapeutic plans. Besides, it can facilitate a more assertive management process. |
| Mattos et al. (2019) | To analyze the recent scientific production on the application of the Kanban tool in the management of health services, assessing the evidence and discussing the results | The application of Kanban as a management tool in health services: An integrative review | Integrative review | In the area of health care quality: Kanban contributed to cost reduction, error reduction, more effective care flows, and multidisciplinary teams informed in real time about the patient's status. In the area of patient flow: Kanban helped the multidisciplinary team in the management of inpatient and emergency beds, facilitated the identification of processes that needed to be improved or eliminated, and reduced waiting times for hospitalization, increasing the turnover of hospital beds. |
| Borges et al. (2020) | Analyzing the performance of nurses in BM service of a public teaching hospital | Performance of nurses in the bed management service of a teaching hospital | Theme-based content analysis | The knowledge employed by the nurse is mainly in patient management and flow. The main competencies were also reported, e.g., communication, agility, and decision-making. The main difficulties in managing hospital beds reported were poor communication, the clinical profile of the admitted patient incompatible with the care unit's capacity to provide care, and the organizational culture. The facilitator in the management of reported hospital beds was the centralization of management attributed to nurses. However, a limited autonomy of nurses regarding the management of beds was identified. |
| Souza et al. (2020) | Describing the organizational and operational aspects of the BM process at a hospital in the Jequitinhonha Expanded Health Region | Management of beds in a pole hospital of the Jequitinhonha expanded health region: organizational and operational aspects of the work process | Content analysis | Five main factors found were: the organization of patient admission and discharge processes, communication, correct referral of the patient to the appropriate ward, the organization of hospital care, and the organization of surgeries. They also found that there were efficiency gains in permanence, occupancy, and turnover rates after implementing BM. These authors concluded that strategic planning of hospital beds is essential to improve the operational aspects of hospital beds. |
| Oliveira et al. (2020) | Describe the development of protocols and flowcharts for the implementation of kanban in the urgency and emergency sector | Beds management in the urgency and emergency using kanban | Action research and content analysis | The participants considered the action research an adequate method to select the Kanban that was later implemented in the management of ED beds. The benefits and challenges identified in the tool's implementation were the optimization of beds, higher turnover of beds, an increase in the number of visits, and an improvement in the quality of the service provided. However, the participants had difficulties demonstrating to the managers the benefits of managing the ED and BM. |
| Oliveira & Bittencourt (2020) | Evaluating through the structure, process, and results. Also, presenting the perception of NGINT professionals about its operation | Evaluation by triangulation of methods in a bed management center of a public hospital in the Federal District | Case study | The results showed that the lack of personnel and recognition of well-performed work is not uncommon. The NGINT does not have the autonomy to decide about the beds; Ultimately, the admission and discharge of inpatients are determined by physicians. In addition, NGINT was evaluated as middling, with the occupancy rate and the average LOS rate below the expected performance. The decision-making over the beds was centered on the physician, not on the NGINT. In this way, a governance problem was diagnosed. Thus, establishing NGINT's power over beds was a measure recommended by the authors, who concluded that the established power structure was compromising the decision-making process of BM. |
| Silva et al. (2021) | Introducing the different features of traditional Kanban and e-Kanban for hospital BM | Contributions of electronic and traditional kanban to hospital bed management | Bibliographic review | A lean maturity improves the patient's LOS and assists in managing hospital beds. |
| Fogaça et al. (2021) | Analysing nurses' perception of the work process in BM | Nurses’ performance in the management of hospital beds in the perception of nursing professionals | Content analysis | According to the nurses, knowledge in management, assistance, functioning of the hospital as a whole, and the interaction between the units are fundamental in the management of beds. The nurse's role reduces the average LOS, increasing bed turnover, reducing overcrowding in the emergency department, and improving communication and transparency in the use of resources. The main difficulties in managing hospital beds were the absence of beds in good working order to allocate patients, communication failures between the teams of inpatient units, lack of trained managers to work in the area of BM, and lack of knowledge of care unit teams of the importance of BM. The potentialities found were the nurses' abilities to streamline various BM processes, such as reducing the waiting time for inpatient surgeries, reducing the waiting time for outpatient procedures, speeding up the transfer to the inpatient units, and reducing the number of patients in the ED. |
| Alonso et al. (2022) | Reporting challenges faced by nurses in managing beds in a hospital inpatient unit during COVID-19 | Challenges faced by nurses in managing hospital beds during the COVID-19 pandemic | Ethnographic research | The authors identified the challenges, which include the need to increase social distancing, and sharing bathrooms in the wards. As the use of bathrooms was limited to confirmed or suspected cases, this led to a reduction in the availability of beds, an increase in beds for clinical stabilization, electrical adaptations, changes in bed profiles, cancellation or suspension of surgeries, and even effective communication between the multidisciplinary team when admitting patients. |
| Hospital (A) | Hospital (B) | |
|---|---|---|
| Nature | Public institution and university - Covenant | Membership - Philanthropic - Private |
| Dimension | Large | Large |
| Localization | Porto Alegre | Porto Alegre |
| Characteristics | High complexity services; Assistance in the social, educational, and professional areas | High complexity services; Assistance in the social, educational, and professional areas |
| Hospital beds | 59 total 46 adult 13 pediatric |
38 total 30 adult 8 pediatric |
| Patient profile | High Complexity | High Complexity |
| Accreditation | Collaborator for the quality of management and hospital care at the Brazilian Ministry of Health A3P Certificate from the Ministry of the Environment Joint Commission International (JCI) from 2013 to 2021 and academically linked to a federal university |
Hospital of Excellence by the Brazilian Ministry of Health ISO 9001:2015 3M – Black Diamond Joint Commission International Affiliation with Johns Hopkins University |
| Technology of Information |
Applications for hospital management (AGHUse), which is the hospital management support system itself | MV Soul Orquestra Sênior and Own System |
| Interviewee | (A1) | (A2) | (B1) | (B2) | (B3) | (B4) | (B5) |
| Hospital | Hospital A | Hospital A | Hospital B | Hospital B | Hospital B | Hospital B | Hospital B |
| Sex | ♀ | ♀ | ♀ | ♂ | ♂ | ♀ | ♀ |
| Bachelor | Nursing | Medicine | Nursing | Medicine | Nursing | Medicine | Nursing |
| Postgraduate studies | Master in nursing, and specializations in emergency and family health | Intensive medicine, residency in emergency medicine, and MBA in business management | Specializations in hospital management and best care practice management | Internal medicine residency | Master's in health sciences and specialization in risk management | Residency in intensive care, master's, doctorate in intensive care, and university professor | Master in nursing and specialization in neurology |
| Role | Nurse at the Internal Regulation Center - NIR | Medical manager and physician in the emergency | Hospital operations coordinator | Chief emergency service manager | Adult and pediatric emergency care coordinator | Medical head of the adult ICU | ICU nursing coordinator |
| Organization time and current role | Emergency nurse: 7 years, 2011-2018. Nurse at NIR: 3 years | Physician on duty: 8 years and 4 months. Medical manager: 4 years | Emergency supervisor: 21 years old Emergency coordinator: 9 years |
Physician on duty in the emergency: 10 years between 2000-2010 Chief manager: since 2013 |
Nurse in the emergency: 9 years Care coordinator: 4 years |
Intensive care physician: 18 years old. Medical head: 2 years | ICU nursing supervision: 2 years ICU nursing coordinator: 6 years |
| Total hospital time | 10 years | 12 years | 30 years | 18 years | 9 years | 20 years | 8 years |
| Defining the main categories | ||
|---|---|---|
| Family and patient: It is a common problem with patients and family members not being able to complete the patient discharge process for a variety of reasons. The literature on BM frequently presents this difficulty in finishing healthcare assistance in hospital organizations (D'Aquino, 2017; He et al., 2019; Machado & Machado, 2019; Silva et al., 2014; Suzuki et al., 2011; Werner, 2017). | ||
| Communication: Communication between departments and teams is an important task in BM and is considered one of the main variables that can affect BM (Borges et al., 2020; D'Aquino, 2017; He et al., 2019; Machado & Machado, 2019; Raffa et al., 2017b; Souza et al., 2020; Werner, 2017). Effective communication is one of WHO's International Patient Safety Goals. | ||
| Prolonged length of stay (pLOS): Average LOS is the total number of days in bed divided by total admissions (Jones, 2009). It is the duration between admission and discharge of a patient. It is a widely used metric, one of the quality indicators related to BM (He et al., 2019). However, the literature shows that unnecessary stays often occur, usually for non-clinical reasons (D'Aquino, 2017; He et al., 2019; Machado & Machado, 2019; Raffa, 2017; Souza et al., 2020). | ||
| Discharge planning by the team: It is an interdisciplinary, complex process that involves identifying the needs of patients, providing guidance for family members, and coordinating those involved (Suzuki et al., 2011). | ||
| Performance goals: The literature shows that regardless of the type of organization, the goals need to be known by the teams for BM to occur in the best way. Raising awareness can streamline processes, remove bottlenecks, and improve BM. | ||
| Occupancy planning: This is an important stage of BM defined through the management policy adopted in hospitals. | ||
| Nurses: Nurses play a key role in BM. | ||
| COVID-19: It is an infectious disease caused by the new coronavirus SARS-CoV-2 (OPAS, 2021) that has changed the BM process due to patient needs, increased demand, and exclusive teams for care, among other unexpected developments. | ||
| Dimension | Category | Excerpt from the interview |
| Processes (internal environment) | Family and/or patient | Interviewee B1: The demand for care and the degree of dependence patients have on health care is also a problem affecting the delay in vacating beds. I think that the fear and anxiety of family members about taking the patient home demands more dedication from professionals when providing post-discharge guidance. |
| Interviewee B2: The main difficulty I see concerns the LOS of the patient in the hospital. I believe that patients could spend less time in the hospital but stay longer than they need to. It occurs because several forces make this happen, for example, issues of convenience for patients and their families. So sometimes, a chronic patient is admitted to the hospital, and everything conspires for him to remain admitted to the hospital. The family prefers it, and the patient prefers it, all because the care at the hospital is better than at home. | ||
| Interviewee B3: More often, the patient is asked to remain hospitalized at the request of the patient's family but also of the social organization or physician. The physician, to feel safe, prefers to release the patient to be discharged and go home with a prepared family to receive the patient. So, sometimes this can be a bottleneck, mainly because hospitalized patients need to leave with greater care, and the family has to structure itself better at home, with caregivers or someone helping at home. You know, it's not easy to care for a patient who has just been released at home. | ||
| Communication | Interviewee A2: I think this problem is also a cultural situation, you know. This is the way the hospital works. The resident physician comes here today, and he/she will discuss the decision the next day. It would be better if the resident could call the professor and discuss it over the phone or make a video call. But of course, this involves the work contract and the person's availability. Anyway, I think it could be done in other ways to speed up decision-making. Even more now, we are making video calls frequently. It has become part of our work routine. So we have many ways to make that decision on the same day. I don't know. Can you see the difference it makes? For example, if the resident examined the patient, and it will be discussed the next day at noon (12:00 am), if an examination is needed, the truth is, in fact, the resident could have already requested this examination in her/his first contact with the patient. So the next day, the exam would be ready with a diagnosis. | |
| Interviewee B2: As much as we have improved, patient transfer is still a problem. Sometimes the transfer situation of the patient admitted to the ED is already available. We have the bed ready and clean in the inpatient ward, but there is still takes time to transfer the patient and handover. Communication between the parties is still not quite as we would like. We want patients to be pulled and not pushed. Not that we had to push them, as a bed is ready to receive a new patient, but if the sector itself (hospital ward) already called and pulled and made us a movement so that it would be easier for the patient to leave the ED. However, often, we see that this does not happen. We have to push, which generates a period of idleness with an empty bed. | ||
| Resource management (internal environment) | Discharge planning by the team | Interviewee A2: The resident physician needs validation from a professor. The resident cannot make any clinical decision alone, so, for example, at the end of the afternoon, as the professor is not present in the hospital, the resident has no one to discuss and validate her/his decision with, so he/she will not make any decisions. Unless it's an emergency, if it's not an emergency and that's something that can wait until the next day, then your decision-making will be postponed until the morning of the next day. |
| Interviewee B1: The delay in discharge occurs mainly due to the lack of a discharge forecast, in which the family does not agree with the physician, so there is often a surprise when the patient is discharged. The family is not prepared to receive the patient. So this is a problem we work with daily due to the lack of predictability of hospital discharge. So, there is still an inefficiency related to the planning and predictability of discharge. This is an inefficiency that we see in the hospital very clearly. If I worked with predictability, I would have a much better bed turnover. | ||
| Interviewee B2: We have to think on a more systemic level and on a day-to-day basis to see where they are and what types of bottlenecks exist. At the same time, knowing what patients were not discharged but could have already been discharged from the hospital and trying to interfere with that. Although we cannot interfere in the physician's decision to discharge (...) When the ED is full, we start to put pressure on discharges to occur. Sometimes, we find patients who are not discharged early, and their discharges are necessary to free up beds, and the ED manages to vent and make the wheel turn as well. | ||
| Prolonged LOS (pLOS) | Interviewee A2: We have been doing a lot of work, especially within the ED and in the hospital, so that the time that the patient remains hospitalized is reduced as much as possible (...) Eventually, yes, the patient stays longer than he should have because he/she needs to take an exam or surgery was canceled. Many patients come from the interior of Porto Alegre to be treated at the ED, so it depends on the municipal ambulance to come and pick them up. So, these are times I think there is still room for improvement. Afterwards, there has also been this effort, in recent years, to reduce this situation of the patient staying longer than necessary. | |
| Interviewee B1: I believe that it happens that the patient stays in the hospital bed longer than necessary (...) Today we can see, even from the demand for care, patients stay in bed much longer than before the pandemic. | ||
| Interviewee B2: There are long-stay patients beyond the necessary time who end up occupying the bed for more days. And one more day that the patient is hospitalized unnecessarily is more one day that another patient is waiting in the ED. So, the permanence rate, this extended stay of hospitalized patients, has everything to do with overcrowding in the ED (...). It does happen that the patient unnecessarily occupies a space in the ED, as they no longer need to be in the ED (...). | ||
| Interviewee B3: The stay in the ED to later go to an inpatient unit occurs in a way that the patient stays longer than he should. | ||
| Interviewee A2: Concerning goals, I am sure the entire team is not clear about our BM goals. Although I work on this aspect by promoting goals among them, most of the team doesn't understand why this is necessary. | ||
| Interviewee B1: Our goal is that after medical discharge, the patient has one hour to vacate the bed. After this period, the nurse has to take action. The nurse's goal is for the bed to be vacated quickly, within one hour. The goal is known, as we hold monthly meetings with the teams responsible for beds and show the efficiency of each team. When we started with the command center, we had time to vacate (release) beds for more than three hours. Afterward, we had less than an hour to release the bed, but due to COVID-19, we are working with an average of one hour and twenty minutes (1h:20min). | ||
| Interviewee B2: There are indicators and targets for everything, from the moment the patients arrive at the door of the ED to the time they are seen, from registration to the nurse's care, when the physician sees them, then the time that it will take the physician to decide between discharge and hospitalization, the period of examinations and evaluations that we also seek to reduce, both the LOS of the patient in the ED and the effectiveness of our actions in the ED so that the patient has a feeling that they have been well taken care of and also to stay for less time and thus accommodate the other patients who arrive (...). So yes, those on the front line (at the end) do not conduct their actions directly based on goals, but everyone knows that there is an indirect demand for productivity, speed, and agility so that this wheel turns faster. | ||
| Interviewee B3: These days, teams are more focused on goals. Before, not so much, but when we started to share information between the units, through the command center, from then on, we started to have clearer and more established goals; the LOS of the patient in the ED waiting for a bed, the waiting time of the patient who entered the ED waiting for a bed in the destination unit, the time of transfer of the patient after getting a bed. We are currently working with a hospital bed forecast. It is interesting and a possibility that did not exist before. | ||
| Interviewee B4: I think that the whole team is well-prepared. We work as a multidisciplinary team, and everyone is very engaged. Of course, with all the changes caused by the pandemic, a lot of new people have entered. This creates a greater inconvenience since I don't think all the latest are well-engaged concerning goals. | ||
| Interviewee B5: The care team is part of the BM, making them aware of our bed planning and goals. | ||
| Decisions shared between units | Interviewee A2: There is a head of the entire ED and three medical managers, so we don't have a specific area, but we divide the tasks. | |
| Interviewee B1: Decision-making for BM is shared in the hospital. As I mentioned, we have the managers who participate in this meeting and make the decision together so that everyone sees the “problem” or the solution together. | ||
| Interviewee B2: We participate in the management of beds in the command center because patients leave the ED in two ways: discharge or hospitalization (...) The command center, which meets every morning, analyzes the main points of hospital bottlenecks. | ||
| Interviewee B3: Every day in the morning, at the central bed command meeting, there are representatives of all hospital units who meet to plan the workday and to check which are the sectors with the highest priority, departments with the highest pressure for beds that day, the departments that will demand more beds. (...) In the ED, we share information among the multidisciplinary team (...). We use admission criteria, discharge criteria, and transfer criteria. This is all discussed with the medical team, and then we share it with everyone. And the nurse's responsibility is to share the decisions taken in the ED with the bed center team (...). We monitor the resources and communicate and share with the bed center to show how the situation in the sector is, informing how the flow of patients is and if there is a need to relieve the burden on the sector. | ||
| Interviewee B5: We also manage critical patients in the hospital. The care team is part of this BM, making them aware of our bed planning. So this management of beds is shared by many people. It is not just one person responsible. It is a whole team responsible for managing the beds, from senior management to the people who are here at the end, so we have this exchange for allowing us to have successful results. | ||
| Bed occupancy planning | Interviewee A2: The occupancy rate is very high, so a free bed is a rarity. As soon as the bed is vacated, another patient already occupies it. Here, it depends on hospitalized patients being discharged to, from there, assist new patients. Availability is something that varies a lot because sometimes there are days when the wards have more discharges, and there are days when there are no discharges, so it is something that we were unable to have an accurate forecast of the number of beds available. | |
| Interviewee B1: We work with clinical staff and have a predictive discharge before ten o'clock in the morning, so we encourage discharges of the day to occur until ten o'clock. This is, in fact, very difficult to manage, so at times of high occupancy, we call the physicians, it is an action we do, but the physicians have their lives outside the hospital where they work in offices until noon and come to discharge them later from noon. Then the physicians tell me, yes, I have discharges to give, but I will go to the hospital only afternoon. This is also an obstacle in the hospital because we do not have a discharge team, a medical team that performs discharges. It is the attending physician who performs discharges at the hospital. This physician is not a contractor. He is not available exactly when we need him because he has a job outside the hospital, which is a difficulty we have at the hospital. | ||
| structural characteristics of the provision of care services (internal environment) | Nurses | Interviewee A2: The nurse is a streamliner of flows. He controls the exams and conditions, as he has an overview of the patient's progress during the follow-up. For me, the nurse has a fundamental role in speeding up the process. The nurse coordinates the exchange of patients in the wards and ED. |
| Interviewee B1: In the bed command center, a nurse manages the entire flow of inputs and outputs. If I have a bed reserved for a patient in the ED, they ensure that the transfer happens as quickly as possible. If I have a discharged patient, the nurse's responsibility is for this patient to leave as soon as possible. The nurse's goal is for the bed to be vacated quickly, within one hour. | ||
| Interviewee B3: The nurse's role is not to allow the system as a whole to collapse. Because it is the nurse who manages the flow of patients within the ED. So the nurses must let me know, and I can see through the system. The nurse is an important link with BM because every time a patient is hospitalized, the nurse puts them in the BM queue. In the ED, we have units by specialties, so we deliver the patient to the necessary specialty for BM to be able to organize itself; if it takes too long to carry out this process, the demands will accumulate throughout the day, so the nurse already has to make the link with the bed center and notify them as soon as the patient is admitted. The bed center should then receive the patient's pathology, but it needs to be notified beforehand. So the nurse can make this whole flow rotate more easily. The nurse is a facilitator because when he/she sees that the system is about to collapse, he/she has to communicate with the coordination, so I (coordination) shoot for the rest of the hospital, and from that, we carry out measures that the hospital must take to not leave the ED overcrowded, as this is not good for the hospital nor for the patients who are admitted to the ED. | ||
| Interviewee B5: We were able to carry out an entire assessment of the total number of patients that we have today together with the medical team to see our discharges and move forward together with the distribution of beds, which can already be ready for admissions that we know that they come from the operating room according to the schedule, or we are constantly sharing information with physicians and nurses to be able to admit the patients scheduled for intensive care. | ||
| Hospital demand (external environment) | COVID-19 | Interviewee A2: The pandemic changed everything. I think it brought some good things, greater integration between the departments with the ED (...). For example, last month's ED (April/2021) had its worst moment, in which psychiatrists and other specialties were all on duty in the ED. This is not common. These physicians have their teams on other floors, but they have become aware of the situation. And they realized that if they took their time to discharge patients, more patients would stay in the ED in a situation where they saw how it works. This exchange of experiences was valid, as I believe it should impact the agility of the beds on the floors in the coming months. |
| Interviewee B2: We had two inflows to protect non-COVID-19 patients. Everything was already complicated with a single input and processing stream. We had to divide human resources, materials, and physical spaces during the pandemic. We operate with two input streams; one for patients with COVID-19 and the other for patients without COVID-19. All this because the professionals who care for both patients cannot mix to ensure the safety of the uninfected patient. Right now, for example, we continue to have a duplicate structure, but the demand for COVID-19 beds has decreased, but we don't know how long it should stay like this. We don't know, so we have to maintain the structure. The demand for COVID-19 has dropped, but we have to be prepared for an increase, so it is a challenge to continue maintaining this structure in duplicate and with all the variables that they have for both things, that is, they have duplicated the variables. So this is the biggest challenge of this isolation issue. It is to avoid the contagion of non-COVID-19 patients. | ||
| Interviewee B3: The pandemic came to change everything. Everything that worked until then currently has a different meaning. So BM had to update to the new reality of the pandemic (COVID-19), along with infection control, taking initiatives in BM in the flows of these patients. This is important, as there is a workflow for the suspected patient of COVID-19, another stream for patients who are confirmed with COVID-19, and a third stream of the patient who is no longer contagious and is not in the period of transmission of COVID-19 to other patients. | ||
| Interviewee B4: The pandemic influenced everything. For example, now I'm working here on WhatsApp it's 24/7. A lot of demand, number of extra beds, more teams, they are a huge problem because that's what I told you, there are a lot of people new, in all areas the hospital works with processes, with organization, with planning, and it has a way of working that needs to be maintained and must be maintained for the benefit and quality of care and care safety. So I'll tell you this, it's practically insane what happened and what's still happening. Of course, we have a whole structure with equipment and a technological park, but what makes the hospital work out are the people. So this had a huge impact not only on the nursing part but on the medical part as well. Previously, it was a door where 100 patients passed, and now it is passing about 500, and it has to pass because if it does not pass, it means death. Our objective here is mainly two: care safety, also for us, for the entire multidisciplinary team, and also that the patient is attended to and that they are not left without assistance when they come to the hospital. | ||
| Interviewee B5: New hires had an impact, and this view on the BM all the time for what has been happening is important. We are going through this pandemic period with some higher peaks, others more moderate, and others a little lighter. We are always reorganizing ourselves as necessary. | ||
| Factors | Problems | Solutions | Authors | Interviewees |
|---|---|---|---|---|
| Family or patient | Resistance to accepting discharge and leaving the hospital. | - Promote care guidelines for patient and family members, thus enabling better self-care conditions for the patient. | D’Aquino (2017), Fontana, Chesani, & Menezes (2017), Fontana, Chesani, & Nalin (2017), Werner (2017), Machado & Machado (2019) and He et al. (2019). | B1, B2 and B3. |
| Communication | Communication failures with other hospital units. | - In hospital systems, share the arrival and departure of patients in the units in real-time. This measure requires the sharing of information regarding the transfer of patients, occupancy rate, expected discharge, and average LOS. - Develop means of streamlining communication between supervising and assistant physicians to expedite discharges. |
D’Aquino (2017), Fontana et al. (2017), Werner (2017), Raffa (2017b), Machado & Machado (2019), He et al. (2019), Borges et al. (2020), Souza et al. (2020) and Alonso et al. (2022). | A1, A2 and B1. |
| Lenght of stay | pLOS. The patient occupies the bed longer than necessary. | - A team with hospital discharge autonomy for any time of the day on any day. - A team responsible for managing hospital beds as a whole, with exclusive dedication. - Technological support in order to efficiently map all processes related to BM. |
Jones (2009), Suzuki et al. (2011), Silva et al. (2014), D’Aquino (2017), Raffa et al. (2017a), Machado & Machado (2019), He et al. (2019), Wasgen et al. (2019), Oliveira & Bittencourt (2020) and Souza et al. (2020). | A1, A2, B1, B2 and B3. |
| Hospital discharge planning by the team | Delay in the hospital discharge process; overcrowding in the ED. | - Improve intra-hospital transfer prediction in the ED with real-time monitoring of bed availability in other units. - A dedicated cleaning team responsible for cleaning the released beds to speed up the availability of beds. |
Suzuki et al. (2011), D’Aquino (2017), Werner (2017), Raffa (2017b), Raffa et al. (2017b), Machado & Machado (2019), He et al. (2019) and Wasgen et al. (2019). | A1, A2, B1 and B2. |
| Performance goals | Goals are not known by the entire team or achieved. | - Promote awareness and engagement of the goals for the teams involved, as well as for those responsible for managing beds in general. - Accompany the goals on a daily basis and carry out an action plan in order to achieve them. |
Raffa (2017), Raffa et al. (2017a) and Raffa et al. (2017b). | A1, A2, B1, B2, B3, B4 and B5. |
| Decisions shared between units | Misaligned expectations; lack of team mentality; departmentalization; competition for resources; | - Decentralize the decision-making process. - Multidisciplinary meetings (huddles). |
Raffa et al. (2017a), Landa et al. (2018) and He et al. (2019). | A1, A2, B1, B2, B3 and B5. |
| Bed management policies | Management policies are not adequate for organizational needs. | - Collaboratively develop management policy changes to increase the efficiency of emergency BM. - Listen carefully to all stakeholders. |
Raffa (2017), Raffa et al. (2017b), He et al. (2019) and Borges et al. (2020). | A2 and B3. |
| Hospital bed occupancy planning | Difficulties in cooperation and information integration; difficulties in managing hospital discharges in periods of high occupancy rates; uncertainty about arrival rate; pressure to prioritize patients in overcrowded settings (Sophie's choices). | - Determine criteria for vacating prioritization and updating as soon as possible discharge planning; - Incorporating forecast models based on historical patient arrival data to aid and support planning. |
D’Aquino (2017), Raffa et al. (2017a), Raffa et al. (2017b), Raffa et al. (2017c), Machado & Machado (2019), He et al. (2019), Wasgen et al. (2019), Oliveira & Bittencourt (2020) and Souza et al. (2020). | A1 and B1. |
| Enfermeiros | Lack of autonomy related to ED hospital beds. | - Allow greater autonomy for nurses in the BM process in the ED. | Raffa (2017), Raffa et al. (2017a), Raffa et al. (2017b), Borges et al. (2020), Oliveira & Bittencourt (2020), Souza et al. (2020) and Alonso et al. (2022). | A1, A2, B1, B4 and B5. |
| COVID-19 | Unforeseen change in the BM process in the ED due to patient needs. Increased demand and need for dedicated teams for care. | - Promote diligent changes in the BM policy, adapting it to the demands of the pandemic. | Noronha et al. (2020) and Alonso et al. (2022). | A1, A2, B1, B2, B3, B4 and B5. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




