1. Introduction
The Coronavirus (COVID19) pandemic had major implications for emergency medical communication centres (EMCC) [
1,
2,
3] which had to be reorganised to respond effectively to the large influx of telephone calls from patients presenting with influenza-like illness and dyspnoea [
4,
5,
6]. Although online triage systems have been developed [
7,
8], the increase in calls to EMCCs due to the large number of respiratory distress situations was very significant [
9]. Some EMCCs developed a two-tiered response, where the first tier performed the initial triage (differentiating between sick/not-sick and mild/severe symptoms) and the second tier was comprised of clinicians (emergency physicians, advanced practice nurses or advanced paramedics) who assessed more complex and severe cases [
1,
5]. The aim of the EMCC restructuring was to improve the efficiency of telephone triage, and avoid, where possible, large uncontrolled influxes of patients attending medical facilities [
10,
11].
Since the widespread utilization of smartphones with video capability and concurrently improving satellite connectivity, live video telemedicine calls have presented exciting possibilities for improving patient care. Before the pandemic, the use of live video in EMCCs was in its infancy [
12,
13]. However, some centres had already tried to replace the dispatch of emergency physicians (EP) to support paramedics in the field with remote assistance [
14,
15]. A study conducted just prior to the pandemic demonstrated that the addition of live video to an emergency call was feasible and changed the perception of the emergency medical dispatcher in over half of cases [
16]. Another study showed that live video guidance (by Emergency Medical Dispatchers) of resuscitation manoeuvres resulted in a subjective improvement in the quality of resuscitation [
17].
The COVID19 pandemic was a catalyst in the use of live video as this capability limited the necessity of physician-patient contact and helped meet the increased demands placed on services during this period [
18]. The use of live video during the pandemic subsequently becomes increasingly prevalent and helped improve quality of care, in particular in the detection of respiratory distress and identify the requirement for emergency care [
19,
20].
To date, very few studies have been published which consider the reorganisation of EMCCs during the pandemic. No study has specifically measured the activity of physicians who triaged second line emergency calls in EMCCs during the COVID19 pandemic. There has also been no study to date measuring the use and impact of live video utilisation by second-line physicians in an EMCC.
The main objective of this study was therefore to measure the effect of the use of live video on medical decisions made by EMCC physicians in the remote assessment of suspected COVID19 patients during the first two waves of the pandemic.
Secondary objectives were to measure the frequency, relative indications and limitations of the use of live video in an EMCC, to describe the characteristics of patients assessed by helplines staff and the reorganisation of an EMCC in response to the pandemic.
2. Materials and Methods
Both the observational study and web-based survey were conducted during the COVID19 pandemic in Geneva (Switzerland) from the 1
st April 2020 until the 30
th April 2021. Data was derived from 1) the call assessment registry of Geneva Emergency Medical Communication Centre (EMCC) and 2) a closed web-based survey of EMCC physicians which was conducted at the same centre. The studies followed the STROBE [
21] and CHERRIES guidelines respectively [
22].
2.1. Setting
The Geneva canton covers an area of 282.48 km
2, is predominantly urban and had a recorded population of 508'774 at the outset of the study [
23]. Twenty one percent of residents were under 20, 16% over 64 and 52% women. There were additionally 100'000 cross-border workers commuting daily from France or neighbouring Swiss cantons to work in Geneva during this period [
23].
2.2. Geneva’s Typical EMCC and Emergency Medical System (EMS)
Geneva's EMCC receives all health related emergency calls in the canton, and the EMDs (paramedics or registered nurses) carried out approximately 40,000 telephone assessments annually of patients in 2019 (excluding inter-hospital transfers). The EMDs are either registered nurses or paramedics with a minimum of 5 years field experience. They handle all calls using a computer-aided dispatch system (ICAD® from Hexagon AB®). For telephone assessments of patients, Geneva’s EMDs use the symptom-based dispatch (SBD) system derived from the Swiss Emergency Triage Scale (SETS®) since 2013 [
24]. Historically there was not an Emergency Physician (EP) physically present in the EMCC, although EMD’s had always had remote access to a physician in case of an assessment concern or medical question.
In the Canton of Geneva, the EMS is two-tiered (or three) with different medical levels and skill sets. The first level is made up of ambulances, staffed by paramedics. There are fifteen ambulance bases scattered throughout the Canton of Geneva that operate according to the proximity of the base to the emergency site. The second level consists of a Mobile Emergency and Resuscitation Service or
SMUR, i.e. a light vehicle that operates with a certified paramedic and an emergency physician in training with at least 2 years of experience [
20]. To assist this junior emergency physicians or if the
SMUR is already busy with another emergency event, specialised senior emergency physicians are available 24 hours a day, 7 days a week to intervene on the spot (third level). The senior EP is available 24/7 to support both levels of response remotely and in the field.
For non-vital cases EMDs also have the option of contacting one of the three on-call general practitioner (GP) services, to arrange a home visit. In practice, there are typically between 1 to 5 GPs available, often with no night cover. In view of the limitations of this service it is relatively infrequently used.
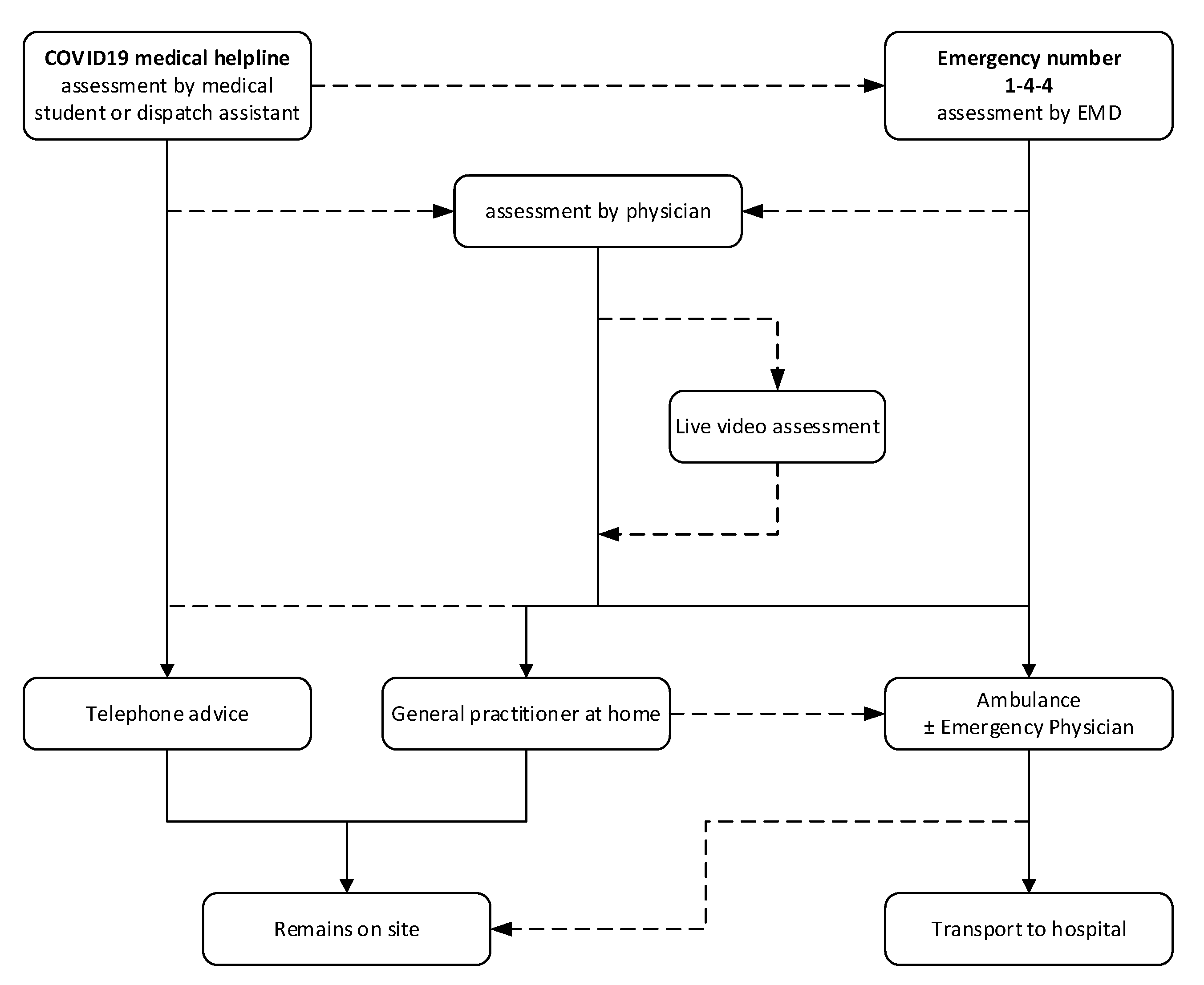
2.3. Re-organization of Geneva’s EMCC during the COVID19 pandemic
At the outset of the COVID19 pandemic (6th March 2020), Geneva’s EMCC was reorganized. Calls were separated into two streams: those made on the usual ‘144’ emergency number and those related to the COVID19 pandemic, made on a new dedicated COVID19 helpline. The staff responding to this new COVID19 helpline were medical students (between their 2nd and 4th years of study) and health professionals from a variety of backgrounds (dispatch assistants). They were specifically trained to assess patients with symptoms related to COVID19, using simplified assessment protocols. The EMD staff responding to the ‘144’ emergency line remained unchanged, and the initial protocol for assessment of suspected COVID19 patients was identical to that used by the other COVID19 helpline (investigation of the main symptom presented by the patient, assessment of general condition and breathing).
In addition, a physician was made available, to reassess difficult situations (EMCC Physician). Typically, they did not take first line calls and were only involved in the assessment of patients with suspected COVID19 infections. They came from a variety of medical specialties whose activities had been suspended due to the pandemic and rotated through the EMCC between one and six months. They were physically present 24/7 for the first two months but, as the pandemic progressed, this was reduced to day and evening cover and thereafter daytime only, a schedule which was adapted in accordance with COVID19 pandemic waves. The two main waves of infections linked to the COVID19 pandemic affected the canton of Geneva in March-April 2020 and from mid-October to mid-December 2020. In 2021, two further increases in infections were observed between April and September 2021 [
25].
Following assessment, there were three possible responses for the patient: 1) telephone advice, 2) home visit by a general practitioner (limited availability) or 3) EMS dispatch. In cases where patients remained home following assessment by a general practitioner or ambulance team, there was also the option for a (< 72h) telephone follow-up by the EMCC physician. The call source, organization of call handling and response are described in
Figure 1.
In addition, during the two waves of the pandemic, the organisation of hospitals in the canton of Geneva was reviewed, with the main public hospital (Geneva University Hospitals), which was defined as the "COVID19 hospital", receiving all patients with (or suspected of having) COVID19, and the other hospitals or private clinics which mainly received patients without COVID19 [
26].
2.4. Live video facilities
The Instantview® live video application from the company Urgentime® was also made available to EMCC physicians from the 20th March 2020. The operation of the live video system was simple to operate. The physician sent a web link via short message service (SMS), which, when accepted by the caller, allowed a web based application to open a live video feed between a callers’ smartphone and EMCC physician. This stream was unidirectional between the caller and physician (the physician sees the caller but the caller does not see the physician). This video stream was in addition to and remained separate from the original audio stream.
The live video was made available to all EMCC physicians. Physicians were given the option of using live video when they felt it would add value to their remote assessment of suspected COVID19 patients. There was no binding assessment protocol for the use of live video. The live video tool was only made available to them and they had all been trained individually in its use. The EMCC physicians therefore used live video at their discretion for the assessment of suspected COVID19 patients.
2.5. Web-based survey
An online survey form was created using the company Reallience®’s form creation tool available from the digital intelligence platform LogIC® (
https://www.logic-app.ch/). The people who could access the form were only those with a LogIC login and profile. A profile had been created for all staff working in the EMCC, but access was only given to physicians working in the EMCC. Instructions for use were provided orally and e-mailed to the physicians at the beginning of their rotation (on average one to three months).
The web-based form was a single page, structured questionnaire with a total of 16 questions. The first five questions identified the situation being assessed (Appendix 1, questions 1-5). Next were 10 closed questions for which only one answer was possible (Appendix 1, questions 6-15), and the last question was an open question (Appendix 1, question 16). There were no conditional questions. The form could only be validated if all the questions were answered. The event number was requested to avoid duplication and was destroyed after the forms were checked and extracted.
Physicians were informed of the study’s purpose and of its estimated length. Physicians who filled in the form were under no obligation to do so (even if they were encouraged to do so), and so they freely agreed to answer and thereby allow the data to be used and published for scientific research purposes.
Both the internet platform and the questionnaire were thoroughly tested for usability and user-friendliness by several study authors before beginning the study. Identity and contact of the investigators were given, and information regarding data handling was provided.
2.6. Study design
2.6.1. Data
The data used in this retrospective study was derived from two sources: 1) register of telephone assessments and 2) paper documentation of daily activity recorded by EMCC physicians (which was used to measure the monthly volume of medical activity).
Survey data was obtained via the web based form made available to all EMCC physicians (LogIC®) and live video use data was derived directly from the Instantview® application.
2.6.2. Inclusion and exclusion criteria
For the retrospective study, patient assessments made between 1st April 2020 and the 30th April 2021 (13 months) were included. This represented the first two COVID19 pandemic waves in Geneva. All calls received regarding a patient with a suspected or confirmed case of COVID19 on both the 144 emergency and dedicated COVID19 helplines were considered ("context" COVID19). Assessments of patients already in hospital (inter-hospital transfers) were excluded. All data from the Instantview® application regarding video calls made during this period was included.
For the web-based survey, all complete forms submitted were analysed.
2.6.3. Outcomes
The primary outcome was the contribution of live video to medical decision making during remote assessment of suspected COVID19 patients.
Secondary outcomes included the frequencies and characteristics of the populations assessed on the two emergency helplines, decisions made according to the lines called and the rate of assessments performed by a physician at Geneva’s EMCC. Secondary outcomes also included the frequency of physician live video use, reasons for using live video and limitations of using the platform.
2.6.4. Measures
This study evaluated the total number of calls to the EMCC regarding patients with a suspected or confirmed case of COVID19. This included all calls made to both the emergency (144) and dedicated COVID19 lines. The activity of EMCC physicians and the rate of their live video use was also measured.
The data from the Urgentime® live video application was analysed and the monthly video connection failure rate was additionally measured.
The results of the online survey, which focused on potential difficulties encountered and the estimated impact of live video on decision making, were also considered.
2.6.5. Statistical analysis
Comma-separated Value (CSV) files containing data related to suspected COVID19 patients from the Geneva SBD system registry and the web-based survey were imported into STATA® 16.0 software (StataCorp®, College Station, TX, USA). Additional data (from the application Instantview® and the count of paper forms) was processed directly in Microsoft Office® Excel® 2013.
Descriptive statistics calculations, including 95% confidence intervals, were performed using STATA® 16.0 software. The Student t-test was used for comparisons of means and the Chi2 test (STATA 16.0) was used to compare proportions of categorical variables.
A test result was considered significant when p < 0.05.
3. Results
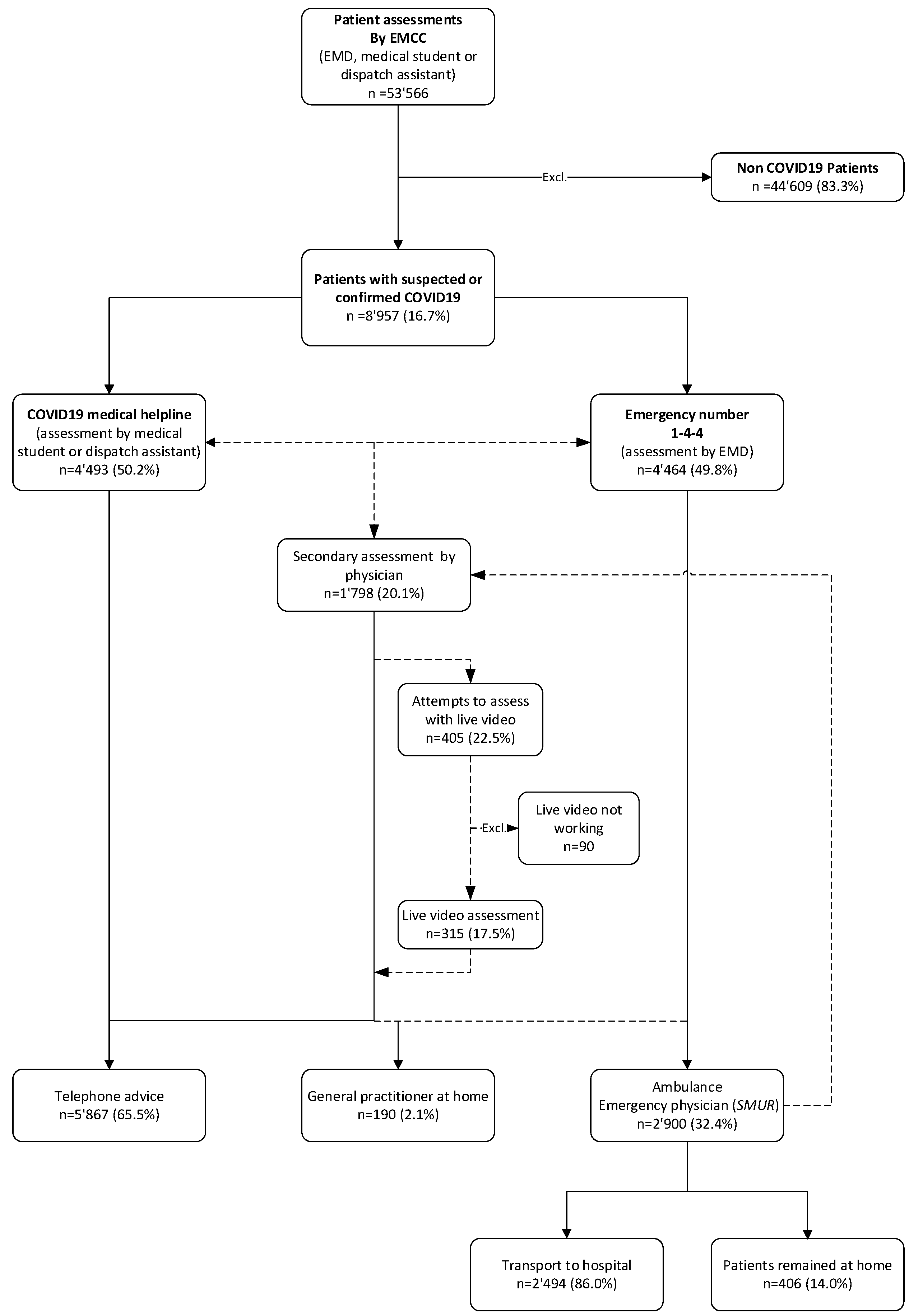
From 1st April 2020 to the 30th April 2021, 53’566 telephone assessments were made at Geneva EMCC on both lines (emergency line and COVID19 helpline). Of these, 8’957 (16.7%) had a suspected or confirmed case of COVID19. 4’464 (49.8%) of assessments were made by an EMD via the emergency ‘144’ line whilst 4’493 (50.2%) were made by medical students or dispatch assistants on the dedicated COVID19 line.
During this period, 1’798 (20.1%) of all COVID19 assessments were provided to the EMCC Physician for further (second line) evaluation. In 405 (22.5%) of these cases, by EMCC physicians tried live video, of which 315 (77.8%) were considered successful and 90 (22.2%) unsuccessful. The flow chart below (
Figure 2) describes the overall emergency assessment flow. Appendix 2 describes the monthly flow of remote assessments by physicians.
Significant differences were demonstrated between patients calling the 144 emergency line compared to the dedicated COVID19 helpline (
Table 1). Of these patients, it was found that the level of medical dispatch priority was significantly more urgent for patients calling the 144 emergency line (p<0.001). In turn significantly more ambulances were dispatched for patients calling the 144 emergency line (p<0.001). The more severe levels of medical dispatch priority decided upon when calls were made to the 144 emergency line were later reflected in higher (more severe) NACA scores seen in the field, than when calls were made to the COVID helpline19 (p<0.001).
Of the 405 video assessments, the failure rate was 22.2% (n=90) (
Table 2). This data comes from the Instantview® application database. Failure to use live video was either related to the users in the field (patients or callers) or to technical difficulties. Regarding user-related failures (slightly over half), not selecting the URL link in the SMS message comes first, followed by not allowing access to the smartphone camera. Regarding technical difficulties, the lack of a camera on the smartphone came first, followed by poor data connection.
The survey based on a web-based questionnaire (
Table 3) demonstrated that patients evaluated by video were rather young and, in majority, female. Of the 107 (26.5%) evaluations with live video that were documented in the web survey forms by 13 EMCC physicians, acceptance was rated as "very good or excellent" for the majority of patients/callers, and ease of use was rated as "very good or excellent" ease by the majority of physicians. Most of the time, these patients were accompanied and the indication for assessment with live video was mainly to assess the patient's breathing and general condition. For the majority of assessments, there were multiple indications for assessment using live video.
In
Table 4, it was noted that after the live video assessment, 15 ambulances (16.5%) were dispatched (7 in Dispatch Priority Level 1) in 91 situations, where it had not been deemed necessary prior to live video assessment. In addition, it was found physicians at Geneva EMCC that live video contributed to the outcome of their clinical decision in over 3/4 of situations.
4. Discussion
Physicians responding to our web-based survey felt that live video contributed to a change in their second-line assessment of suspected COVID19 patients in more than 75% of the situations. This rate is higher than in the Linderoth study, where the dispatchers' assessment was changed in “only” 51.1% of cases [
16]. This could be explained by a patient pre-screening bias, as the system is usually only used by physicians when a clear probable benefit has been pre-identified. Indeed, physicians used video in only 22.5% of their assessments when they could use it without any limitation. However, there was a similar rate (16.5% in our survey / 12.9% in Linderoth's study) of requalification in more critical situations or requiring an ambulance. In the second line live video assessments, there were a significant number of potentially life-threatening emergencies (7/91) that were detected (7.7%). The value of using live video, even after an advanced telephone assessment by a second-line physician, thus seems to persist. Another study showed that 22.4% of patients who were initially classified in the least severe category after telephone-only triage were reclassified to the most severe categories after reassessment using live video [
27].
It would also appear that live video, used by a physician, could help to provide the "right answer" for the patient, even when paramedics are on site, since a redirection of the ambulance to the hospital and inpatient units dedicated to COVID19 patients was performed in 10/16 situations. However, this study does not prove an advantage of live video, as there was no control group for this subgroup. Furthermore, another study concluded in COVID19 context that the use of live video by emergency physicians was not superior to the use of the telephone alone [
28]. Nevertheless, it seems that nurses/paramedics have difficulty in making an adequate "no transport" decision when they are sent to the patient [
29]. In these situations, having a remote physician could improve the appropriateness of transport decisions versus leaving the patient on site.
We noted that the failure rate of live video was 22.2%, which was slightly higher than the Danish study (17.8%) [
17] and the English study (16.9%) [
27]. It is possible that this is partly related to the fact that our EMCC only started using the Instantview® tool in 20 March 2020, so there was only a very short learning phase for physicians. As in the Danish study, the causes of failure, difficulties were mainly related to the users' handling of the smartphones or non-receipt/difficulty in accessing the SMS URL link. As with all published studies on the subject [
17,
27,
28,
30], acceptance of the video was excellent by both callers and physicians and was also considered easy to use.
We found significant differences between patients who called the 144 number and those who called the COVID19 medical helpline. In particular, patients who called the COVID19 helpline or those assessed by live video had a significantly lower mean age than those assessed after a call to the 1.4.4. number. This is comparable to studies that have assessed patients with suspected COVID19, which found similar mean ages for both video and non-video assessments [
5,
27].
The predominant symptoms during the telephone assessment also differed according to the telephone lines that were called. Dyspnoea predominates for calls to the 144 number and flu-like symptoms for the COVID19 medical helpline. In our EMCC, a fever was only mentioned if it was measured by the patient (the "feeling of fever" was not documented as a "fever"). This may explain the low proportion of fever documented in telephone assessments compared to other published studies [
5,
31]. Similarly, "dry cough" was not differentiated from other influenza symptoms. Taking these details into account, the majority of influenza-like symptoms were found in the mild forms of suspected COVID19. Our study seems to show that, for suspected COVID19, the presence of "dyspnoea" (including tachypnoea) at the initial telephone assessment does seem to be a criterion of severity at the time of the call.
The identification of dyspnoea or tachypnoea as a severity factor in remote assessments of suspected COVID19 patients probably explains why, in our study, the assessment of breathing is the first cause of indication for the addition of live video that is mentioned by 2nd line physicians. Indeed, the measurement of respiratory rate, the search for accessory muscle use or cyanosis, are clearly facilitated by visualisation of the patient. This has been demonstrated in several studies, especially in the paediatric context [
20,
32,
33].
The second main indication for the use of video was the "general condition of the patient", which is often associated with the patient's living situation in pre-hospital interventions. Live video allows the scene to be seen and can therefore provide valuable insights that can be missed completely by using the telephone alone. In the accident context, it has been argued that live video provides "more information from the scene of an incident and the clinical condition of the patient(s)" [
13].
In our study, citizens could call two numbers, the usual emergency number in case an ambulance (number 144) was needed, and another number dedicated to "remote medical assessments in case of suspected COVID19" for situations that the callers themselves considered as "non-urgent". Then, patient assessments were carried out in the same way, in the same EMCC, regardless of the telephone line initially called. We found that callers assessed their situation fairly well themselves, as only 5 (0.1%) serious situations (for 4,464 assessments) were identified following a call to the COVID19 medical helpline , compared with 735 (16.3%) serious situations (for 4,493 assessments) on the 144 number (table 1). The provision of two telephone helplines (urgent or ambulance/non-urgent) therefore contributes to the performance of the EMCC triage, as the prevalence of severity is completely different depending on which line is called [
24]. The skills available and the assessment tools used in EMCCs should be adapted to the condition of the patients assessed. Medical skills and tools for live video are needed for patients requiring an ambulance, but also for low acuity situations [
16,
17,
27,
30,
34].
The most likely outcome of a live video call in this study was for the patient to remain at home with no further follow-up required. It can therefore be inferred that the EMCC physician was able to completely satisfy a patient’s needs and no further resources were required in these cases. This can be considered a particularly successful outcome in view of the fact that the patients being reviewed by the physician were second line and therefore likely to be more complex scenarios. It was also particularly relevant to the COVID19 pandemic where limiting patient-clinician contact reduced the likelihood of disease transmission. This outcome not only saves precious resources but is also positive for CO2 emissions, reducing the requirement of unnecessary journeys by prehospital teams or patients.
The exponential increase in calls to EMCCs during the pandemic, mainly for remote triage of patients suspected of COVID19 [
4], has resulted in a change in the missions of these EMCCs from "situation-related emergency medical dispatch" to "remote triage of patients". In this context, EMCCs are increasingly performing "tele triage", and this is part of the "virtually perfect" evolution of emergency telemedicine [
35].
There are several limitations to our study. Firstly, this was a retrospective, single-centre study. Few organisations are comparable to the EMCC in Geneva with two levels (1st level with nurses or paramedics and 2nd level with a physician), and this limits the generalisation of the results. Secondly, the second part was a web-based survey with all the known limitations associated with this method. The questionnaire was only completed for 26.4% of the videos made live. As it was not compulsory, there may have been confounding factors influencing a physician’s decision to complete the questionnaire. The live video facility was only made available to EMCC physicians. As a consequence, it was only employed for second line patient evaluation. This data is therefore not generalisable to first line patient evaluations made at an EMCC. It was possible that if first line responders had also had access to the live video facility it may have reduced their requirement for a second line evaluation/ EMCC physician input. While the live video facility was made available to all EMCC physicians, the decision to use it was at their own discretion which, with no guidelines or specific protocols in place likely resulted in inter physician variability. Contributing factors may have included their familiarity with the system, previous telemedicine experience, understanding and training regarding suitable indications. The most frequent indication for its use was to evaluate respiratory function. As respiratory involvement is the main complaint of COVID19, it likely that this finding was specific to the COVID19 patients and ungeneralizable to the general patient population calling an EMCC.
It would be interesting to see in future studies how patient management decisions could be influenced if first line responders also had access to this live video facility. It would also be interesting to further evaluate the time taken to make a patient assessment with or without live video as this is also a consideration when implementing a new system into an EMCC where patient assessments can be time critical and resource limited. This may influence future decisions regarding appropriate patient selection. Finally, it would be interesting to explore further indications which could also benefit from the use of live video in the future.
5. Conclusions
During the first two waves of the pandemic, a large number of suspected COVID19 patients, mainly with influenza-like symptoms or breathing difficulties, were triaged by paramedics, nurses or medical student at the Geneva EMCC. 1 in 5 patients required second-line evaluation by a physician.
Physicians used live video in 22.5% of cases, primarily to assess patients' breathing and general condition, and found the tool easy to use. The acceptance of live video use by patients or callers was generally very good, but there was a failure rate observed in 22.2% of live video calls.
In the web-based survey, physicians felt that live video influenced their medical decision in 75.7% of assessments. For these live video calls, the most likely outcome was that the patient remained at home without further follow-up, but there were still a significant number of life-threatening emergencies that were caught.
It appears that live video used by physicians integrated into an EMCC contributes to better remote assessment and triage of suspected COVID19 patients, particularly when these patients present with breathing difficulties. Further studies are needed to confirm these results.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Appendix 1: Web-based survey questionnaire; Appendix 2: Monthly flow of remote assessments performed by physicians.
Author Contributions
Conceptualization, R. Larribau and B. Healey; methodology, R. Larribau, V N. Chappuis and B. Healey; software, R. Larribau and T. Herren; validation, L. Suppan and B. Gartner; formal analysis, R. Larribau, V N. Chappuis and B. Healey; investigation, R. Larribau and V.N. Chappuis; resources, R. Larribau; data curation, R. Larribau, F. Guiche and D. Boussard; writing—original draft preparation, R. Larribau, B. Healey; writing—review and editing, R. Larribau, B. Healey, V N. Chappuis, D. Boussard, F. Guiche, T. Herren, B. Gartner, L. Suppan ; supervision, B. Gartner and L. Suppan; project administration, R. Larribau, F. Guiche and D. Boussard; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Approval for the use of the data from the call assessment registry was given by the Cantonal Commission for Research and Ethics of Geneva (project n°2018-00789) on 12th June 2018.
Informed Consent Statement
The Geneva Cantonal Research and Ethics Commission considered that the patient’s consent could not be obtained and was not necessary for the study. Information about the online survey (purpose and estimated duration) was sent by e-mail to the physicians of the EMCC, and they had to validate their consent electronically before starting the questionnaire.
Acknowledgments
We would like to acknowledge assistance provided by Jane Schurtz-Taylor with the English translation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kristal, R.; Rowell, M.; Kress, M.; Keeley, C.; Jackson, H.; Piwnica-Worms, K.; Hendricks, L.; Long, T.G.; Wallach, A.B. A Phone Call Away: New York's Hotline And Public Health In The Rapidly Changing COVID-19 Pandemic. Health affairs (Project Hope) 2020, 39, 1431–1436. [Google Scholar] [CrossRef] [PubMed]
- Marrazzo, F.; Spina, S.; Pepe, P.E.; D'Ambrosio, A.; Bernasconi, F.; Manzoni, P.; Graci, C.; Frigerio, C.; Sacchi, M.; Stucchi, R.; et al. Rapid reorganization of the Milan metropolitan public safety answering point operations during the initial phase of the COVID-19 outbreak in Italy. Journal of the American College of Emergency Physicians open 2020, 1, 1240–1249. [Google Scholar] [CrossRef] [PubMed]
- Saberian, P.; Conovaloff, J.L.; Vahidi, E.; Hasani-Sharamin, P.; Kolivand, P.H. How the COVID-19 Epidemic Affected Prehospital Emergency Medical Services in Tehran, Iran. The western journal of emergency medicine 2020, 21, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Prezant, D.J.; Lancet, E.A.; Zeig-Owens, R.; Lai, P.H.; Appel, D.; Webber, M.P.; Braun, J.; Hall, C.B.; Asaeda, G.; Kaufman, B.; et al. System impacts of the COVID-19 pandemic on New York City's emergency medical services. Journal of the American College of Emergency Physicians open 2020, 1, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Lapostolle, F.; Schneider, E.; Vianu, I.; Dollet, G.; Roche, B.; Berdah, J.; Michel, J.; Goix, L.; Chanzy, E.; Petrovic, T.; et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: the COVID-call study. Internal and emergency medicine 2020, 15, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Dami, F.; Berthoz, V. Lausanne medical dispatch centre's response to COVID-19. Scandinavian journal of trauma, resuscitation and emergency medicine 2020, 28, 37. [Google Scholar] [CrossRef] [PubMed]
- Hautz, W.E.; Exadaktylos, A.; Sauter, T.C. Online forward triage during the COVID-19 outbreak. Emergency medicine journal : EMJ 2021, 38, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Galmiche, S.; Rahbe, E.; Fontanet, A.; Dinh, A.; Bénézit, F.; Lescure, F.X.; Denis, F. Implementation of a Self-Triage Web Application for Suspected COVID-19 and Its Impact on Emergency Call Centers: Observational Study. J Med Internet Res 2020, 22, e22924. [Google Scholar] [CrossRef] [PubMed]
- Vuilleumier, S.; Spichiger, T.; Dénéréaz, S.; Fiorentino, A. Not only COVID-19 disease impacts ambulance emergency demands but also lockdowns and quarantines. BMC emergency medicine 2023, 23, 4. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R. The Role of Israel's Emergency Medical Services During a Pandemic in the Pre-Exposure Period. 2020, 1-5. [CrossRef]
- Jaffe, E.; Sonkin, R.; Alpert, E.A.; Magid, A.; Knobler, H.Y. Flattening the COVID-19 Curve: The Unique Role of Emergency Medical Services in Containing a Global Pandemic. The Israel Medical Association journal : IMAJ 2020, 22, 476–482. [Google Scholar]
- Johansson, A.; Esbjörnsson, M.; Nordqvist, P.; Wiinberg, S.; Andersson, R.; Ivarsson, B.; Möller, S. Technical feasibility and ambulance nurses' view of a digital telemedicine system in pre-hospital stroke care - A pilot study. Int Emerg Nurs 2019, 44, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Ter Avest, E.; Lambert, E.; de Coverly, R.; Tucker, H.; Griggs, J.; Wilson, M.H.; Ghorbangholi, A.; Williams, J.; Lyon, R.M. Live video footage from scene to aid helicopter emergency medical service dispatch: a feasibility study. Scandinavian journal of trauma, resuscitation and emergency medicine 2019, 27, 55. [Google Scholar] [CrossRef] [PubMed]
- Felzen, M.; Beckers, S.K.; Kork, F.; Hirsch, F.; Bergrath, S.; Sommer, A.; Brokmann, J.C.; Czaplik, M.; Rossaint, R. Utilization, Safety, and Technical Performance of a Telemedicine System for Prehospital Emergency Care: Observational Study. JMIR 2019, 21, e14907. [Google Scholar] [CrossRef] [PubMed]
- Vicente, V.; Johansson, A.; Ivarsson, B.; Todorova, L.; Möller, S. The Experience of Using Video Support in Ambulance Care: An Interview Study with Physicians in the Role of Regional Medical Support. Healthcare (Basel, Switzerland) 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Linderoth, G.; Lippert, F.; Østergaard, D.; Ersbøll, A.K.; Meyhoff, C.S.; Folke, F.; Christensen, H.C. Live video from bystanders' smartphones to medical dispatchers in real emergencies. Resuscitation 2021, 21, 101. [Google Scholar] [CrossRef] [PubMed]
- Linderoth, G.; Rosenkrantz, O.; Lippert, F.; Østergaard, D.; Ersbøll, A.K.; Meyhoff, C.S.; Folke, F.; Christensen, H.C. Live video from bystanders' smartphones to improve cardiopulmonary resuscitation. Resuscitation 2021. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Wherton, J.; Shaw, S.; Morrison, C. Video consultations for covid-19. BMJ 2020, 368, m998. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC public health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- Ponnapalli, A.; Khare, Y.; Dominic, C.; Ganesh, S.; Bhalla, G.; Gokani, S.A. Remote risk-stratification of dyspnoea in acute respiratory disorders: a systematic review of the literature. The journal of the Royal College of Physicians of Edinburgh 2021, 51, 221–229. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- (OCSTAT), O.C.d.l.s. Etat et évolution de la population. Available online: https://statistique.ge.ch/domaines/apercu.asp?
- Larribau, R.; Chappuis, V.N.; Cottet, P.; Regard, S.; Deham, H.; Guiche, F.; Sarasin, F.P.; Niquille, M. Symptom-Based Dispatching in an Emergency Medical Communication Centre: Sensitivity, Specificity, and the Area under the ROC Curve. International journal of environmental research and public health 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Genecand, C.; Mongin, D.; Koegler, F.; Lebowitz, D.; Regard, S.; Falcone, J.L.; Nehme, M.; Braillard, O.; Grira, M.; Joubert, D.; et al. Cohort profile: Actionable Register of Geneva Outpatients and inpatients with SARS-CoV-2 (ARGOS). BMJ open 2021, 11, e048946. [Google Scholar] [CrossRef]
- Midez, R.; Fehlmann, C.A.; Marti, C.; Larribau, R.; Rouyer, F.; Boroli, F.; Suppan, L.; Gartner, B.A. Association between Prehospital Hypoxemia and Admission to Intensive Care Unit during the COVID-19 Pandemic: A Retrospective Cohort Study. Medicina (Kaunas) 2021, 57. [Google Scholar] [CrossRef] [PubMed]
- Bell, F.; Pilbery, R.; Connell, R.; Fletcher, D.; Leatherland, T.; Cottrell, L.; Webster, P. The acceptability and safety of video triage for ambulance service patients and clinicians during the COVID-19 pandemic. British paramedic journal 2021, 6, 49–58. [Google Scholar] [CrossRef]
- Sykora, R.; Renza, M.; Ruzicka, J.; Bakurova, P.; Kukacka, M.; Smetana, J.; Duska, F. Audiovisual Consults by Paramedics to Reduce Hospital Transport After Low-Urgency Calls: Randomized Controlled Trial. Prehospital and disaster medicine 2020, 35, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Breeman, W.; Poublon, N.A.; Verhofstad, M.H.J.; Van Lieshout, E.M.M. Safety of on-scene medical care by EMS nurses in non-transported patients: a prospective, observational study. Scandinavian journal of trauma, resuscitation and emergency medicine 2018, 26, 79. [Google Scholar] [CrossRef]
- Sýkora, R.; Peřan, D.; Renza, M.; Bradna, J.; Smetana, J.; Duška, F. Video Emergency Calls in Medical Dispatching: A Scoping Review. Prehospital and disaster medicine 2022, 37, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, E.; Sonkin, R.; Strugo, R.; Zerath, E. Evolution of emergency medical calls during a pandemic - An emergency medical service during the COVID-19 outbreak. The American journal of emergency medicine 2020. [Google Scholar] [CrossRef]
- Gattu, R.; Scollan, J.; DeSouza, A.; Devereaux, D.; Weaver, H.; Agthe, A.G. Telemedicine: A Reliable Tool to Assess the Severity of Respiratory Distress in Children. Hosp Pediatr 2016, 6, 476–482. [Google Scholar] [CrossRef]
- Siew, L.; Hsiao, A.; McCarthy, P.; Agarwal, A.; Lee, E.; Chen, L. Reliability of Telemedicine in the Assessment of Seriously Ill Children. Pediatrics 2016, 137, e20150712. [Google Scholar] [CrossRef] [PubMed]
- Boggan, J.C.; Shoup, J.P.; Whited, J.D.; Van Voorhees, E.; Gordon, A.M.; Rushton, S.; Lewinski, A.A.; Tabriz, A.A.; Adam, S.; Fulton, J.; et al. Effectiveness of Acute Care Remote Triage Systems: a Systematic Review. J Gen Intern Med 2020, 35, 2136–2145. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for Covid-19. The New England journal of medicine 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).