Submitted:
20 January 2023
Posted:
24 January 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Definitions and Outcomes
2.4. Statistical Analysis
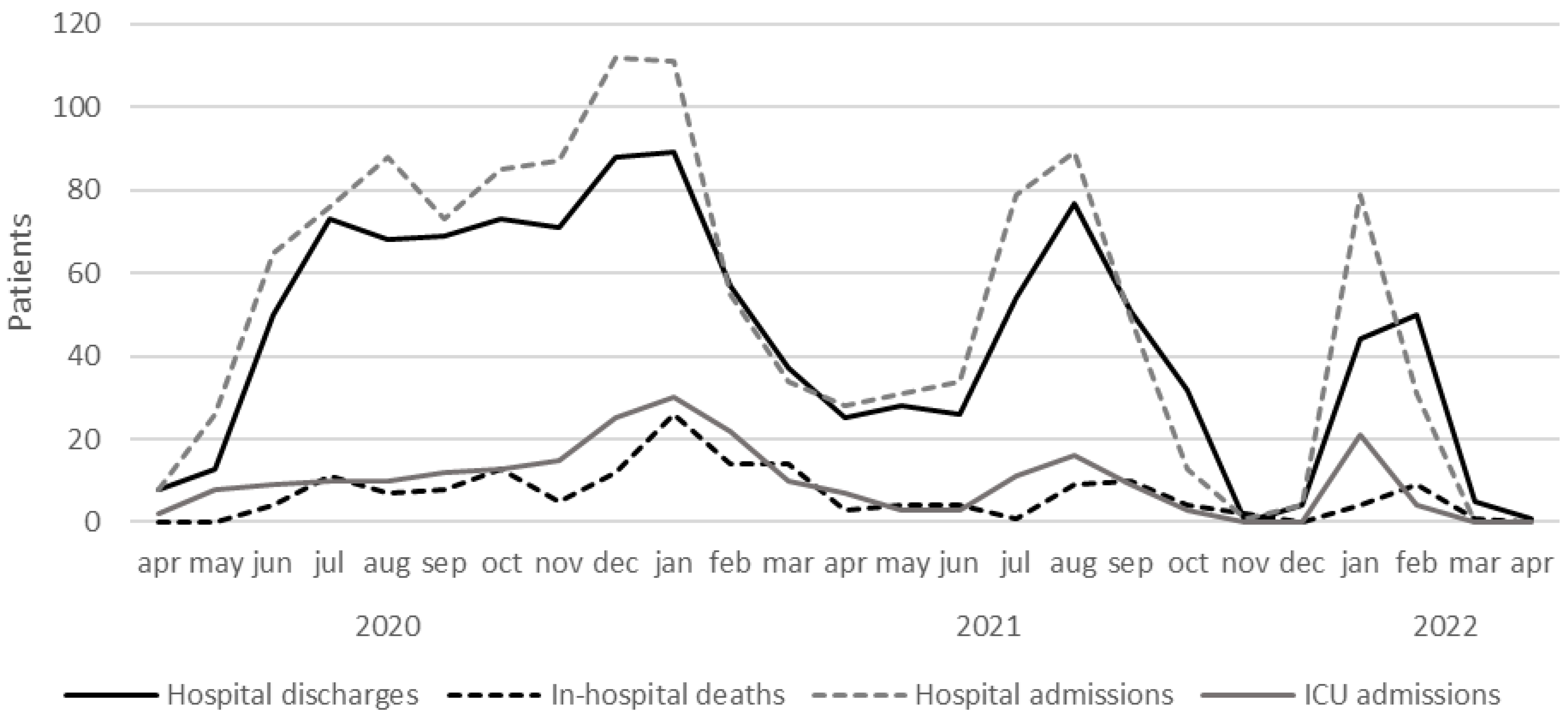
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ortiz-Brizuela, E.; Villanueva-Reza, M.; González-Lara, M.F.; Tamez-Torres, K.M.; Román-Montes, C.M.; Díaz-Mejía, B.A.; Pérez-García, E.; Olivas-Martínez, A.; Rajme-López, S.; Martinez-Guerra, B.A.; et al. Clinical and Epidemiological Characteristics of Patients Diagnosed With Covid-19 in a Tertiary Care Center in Mexico City: A Prospective Cohort Study. Rev. Invest. Clin. 2020, 72, 165–177. [Google Scholar] [CrossRef]
- Martos Pérez, F.; Luque del Pino, J.; Jiménez García, N.; Mora Ruiz, E.; Asencio Méndez, C.; García Jiménez, J.M.; Navarro Romero, F.; Núñez Rodríguez, M.V. Comorbilidad y Factores Pronósticos Al Ingreso En Una Cohorte COVID-19 de Un Hospital General. Rev. Clínica Española 2021, 221, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Qian, L.; Hong, V.; Wei, R.; Nadjafi, R.F.; Fischer, H.; Li, Z.; Shaw, S.F.; Caparosa, S.L.; Nau, C.L.; et al. Obesity and Mortality among Patients Diagnosed with COVID-19: Results from an Integrated Health Care Organization. Ann. Intern. Med. 2020, 173, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Mendizabal, M.; Pi, F.; Ridruejo, E.; Anders, M.; Silveyra, M.D.; Torre, A.; Montes, P.; Urzúa, A.; Pages, J.; Toro, L.G.; et al. Since January 2020 Elsevier Has Created a COVID-19 Resource Centre with Free Information in English and Mandarin on the Novel Coronavirus COVID- 19 . The COVID-19 Resource Centre Is Hosted on Elsevier Connect , the Company ’ s Public News and Information . 2020.
- Brill, S.E.; Jarvis, H.C.; Ozcan, E.; Burns, T.L.P.; Warraich, R.A.; Amani, L.J.; Jaffer, A.; Paget, S.; Sivaramakrishnan, A.; Creer, D.D. COVID-19: A Retrospective Cohort Study with Focus on the over-80s and Hospital-Onset Disease. BMC Med. 2020, 18, 1–9. [CrossRef]
- Álvarez-Arroyo, L.; Carrera-Hueso, F.J.; El-Qutob, D.; Robustillo-Villarino, M.; Girona-Sanz, A.M.; Pin-Godos, M.T.; Sánchez-Monzó, P.; Martínez-Gonzálbez, R.; Cepeda-Madrigal, S.; Martínez-Martínez, F. Estudio Descriptivo de Una Cohorte de Pacientes Con COVID-19 Hospitalizados En España. Gac. México 2021, 157, 80–87. [CrossRef]
- Marcela Vélez, C. COVID-19 and Vaccination in Latin America and the Caribbean: Challenges, Needs and Opportunities 2021, 1–88.
- The Covid-19 Pandemic in Latin America and the Caribbean. Popul. Dev. Rev. 2022, 48, 263–266. [CrossRef]
- Interventions, R. Revue Interventions Économiques Latin American Health Regimes in the Face of the Pandemic Revue Interventions Économiques Papers in Political Economy Latin American Health Regimes in the Face of the Pandemic Les Régimes de Santé Latino-Américains Face à L. 2022. [CrossRef]
- Estudios de La OCDE Sobre Los Sistemas de Salud: México 2016; 2016. ISBN 9789264230491.
- Narvaez, C.; Rivas, L.A.; Chavez, A. Modelos de Gestión de La Calidad En Instituciones Públicas de Salud En México. Rev. Innovaciones Negocios 2017, 12, 177–205. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Ángeles Correa, M.G.; Villarreal Ríos, E.; Galicia Rodríguez, L.; Vargas Daza, E.R.; Frontana Vázquez, G.; Monrroy Amaro, S.J.; Ruiz Pinal, V.; Álvarez, J.D.; Beltrán, S.S. Enfermedades Crónicas Degenerativas Como Factor de Riesgo de Letalidad Por COVID-19 En México. Rev. Panam. Salud Pública 2022, 46, 1. [Google Scholar] [CrossRef]
- Campos-Nonato, I.; Hernández-Barrera, L.; Flores-Coria, A.; Gómez-Álvarez, E.; Barquera, S. Prevalence, Diagnosis and Control of Hypertension in Mexican Adults with Vulnerable Condition. Results of the Ensanut 100k. Salud Publica Mex. 2019, 61, 888–897. [Google Scholar] [CrossRef]
- García-Peña, C.; Bello-Chavolla, O.Y.; Castrejón-Pérez, R.C.; Jácome-Maldonado, L.D.; Lozano-Juárez, L.R. Variability in Case Fatality Rate Risk Due to Covid-19 According to Health Services Provider in Mexico City Hospitals. Salud Publica Mex. 2022, 64, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Colchero, M.A.; Gómez, R.; Pineda-Antúnez, C.J.; Bautista-Arredondo, S. Health Care Utilization during the Covid-19 Pandemic in Mexico: The Cascade of Care. Salud Publica Mex. 2021, 63, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martínez, O.A.; Rodríguez-Brito, A. Vulnerability in Health and Social Capital: A Qualitative Analysis by Levels of Marginalization in Mexico. Int. J. Equity Health 2020, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Halpin, D.M.G.; Criner, G.J.; Papi, A.; Singh, D.; Anzueto, A.; Martinez, F.J.; Agusti, A.A.; Vogelmeier, C.F. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2021, 203, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Reddel, H.K.; Bacharier, L.B.; Bateman, E.D.; Brightling, C.E.; Brusselle, G.G.; Buhl, R.; Cruz, A.A.; Duijts, L.; Drazen, J.M.; FitzGerald, J.M.; et al. Global Initiative for Asthma Strategy 2021: Executive Summary and Rationale for Key Changes. Eur. Respir. J. 2022, 59. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J. Chronic Kidney Disease. Lancet (London, England) 2012, 379, 165–180. [Google Scholar] [CrossRef]
- Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S14–S31. [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertens. (Dallas, Tex. 1979) 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef]
- ECLAC Social Panorama of Latin America 2021; 2007. ISBN 9789211218244.
- Carrillo-Vega, M.F.; Salinas-Escudero, G.; García-Peña, C.; Gutiérrez-Robledo, L.M.; Parra-Rodríguez, L. Early Estimation of the Risk Factors for Hospitalization and Mortality by COVID-19 in Mexico. PLoS One 2020, 15, 1–11. [Google Scholar] [CrossRef]
- Salinas-Escudero, G.; Carrillo-Vega, M.F.; Granados-García, V.; Martínez-Valverde, S.; Toledano-Toledano, F.; Garduño-Espinosa, J. A Survival Analysis of COVID-19 in the Mexican Population. BMC Public Health 2020, 20, 1–8. [Google Scholar] [CrossRef]
- ECLAC-PAHO Health and the Economy: A Convergence Needed to Address COVID-19 and Retake the Path of Sustainable Development in Latin America and the Caribbean. 2020.
- NU. CEPAL The Recovery Paradox in Latin America and the Caribbean Growth amid Persisting Structural Problems: Inequality, Poverty and Low Investment and Productivity. 2021, 40.
- ECLAC-PAHO COVID-19 Report: The Prolongation of the Health Crisis and Its Impact on Health, the Economy and Social Development. 2020, 37.
- Puig, A.; Pagán, J.A.; Wong, R. Assessing Quality across Healthcare Subsystems in Mexico. J. Ambul. Care Manage. 2009, 32, 123–131. [Google Scholar] [CrossRef]
- Shi, C.; Wang, L.; Ye, J.; Gu, Z.; Wang, S.; Xia, J.; Xie, Y.; Li, Q.; Xu, R.; Lin, N. Predictors of Mortality in Patients with Coronavirus Disease 2019: A Systematic Review and Meta-Analysis. BMC Infect. Dis. 2021, 21, 1–15. [Google Scholar] [CrossRef]
- Zhang, J.J.; Dong, X.; Liu, G.H.; Gao, Y.D. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 2022. [Google Scholar] [CrossRef]
- Leidman, E.; Doocy, S.; Heymsfield, G.; Sebushishe, A.; Mbong, E.N.; Majer, J.; Bollemeijer, I. Risk Factors for Hospitalisation and Death from COVID-19: A Prospective Cohort Study in South Sudan and Eastern Democratic Republic of the Congo. BMJ Open 2022, 12, e060639. [Google Scholar] [CrossRef]
- Mesas, A.E.; Andrade, S.M. De; Sequı, I. Predictors of In-Hospital COVID-19 Mortality : A Comprehensive Systematic Review and Meta- Analysis Exploring Differences by Age , Sex and Health Conditions. 2020, 6, 1–23. [CrossRef]
- Toledo-tapia, R.; Mayoral-ortiz, A.; Tlecuitl-mendoza, N.; Toledo-tapia, M.; Ortega-aguirre, M.; Amaro-balderas, E. Influencia de Factores de Riesgo Sobre Mortalidad Por COVID-19. 2022, 60.
- Yu, H.; Wang, T.; Chen, Z. Blood Urea Nitrogen to Serum Albumin Ratio (BAR) Predicts Critical Illness in Patients with Coronavirus Disease 2019 (COVID-19). 2021.
- Henkens, M.T.H.M.; Raafs, A.G.; Verdonschot, J.A.J.; Linschoten, M.; van Smeden, M.; Wang, P.; van der Hooft, B.H.M.; Tieleman, R.; Janssen, M.L.F.; ter Bekke, R.M.A.; et al. Age Is the Main Determinant of COVID-19 Related in-Hospital Mortality with Minimal Impact of Pre-Existing Comorbidities, a Retrospective Cohort Study. BMC Geriatr. 2022, 22, 1–11. [Google Scholar] [CrossRef]
- Cordero, A.; Santos García-Gallego, C.; Bertomeu-González, V.; Fácila, L.; Rodríguez-Mañero, M.; Escribano, D.; Castellano, J.M.; Zuazola, P.; Núñez, J.; Badimón, J.J.; et al. Mortality Associated with Cardiovascular Disease in Patients with COVID-19. REC CardioClinics 2021, 56, 30–38. [Google Scholar] [CrossRef]
- Ranucci, M.; Parati, G.; Di Dedda, U.; Bussotti, M.; Agricola, E.; Menicanti, L.; Bombace, S.; De Martino, F.; Giovinazzo, S.; Zambon, A.; et al. When Outcomes Diverge: Age and Cardiovascular Risk as Determinants of Mortality and ICU Admission in COVID-19. J. Clin. Med. 2022, 11. [Google Scholar] [CrossRef]
- Rosso, F.; Tafurt, E.; Valle, F.; Icesi, U.; Cauca, V.; Valle, F.; Cauca, V. Downloaded from Https://Academic.Oup.Com/Ofid/Article/8/Supplement_1/S274/6450193 by Guest on 01 September 2022. 2021, 8, 2021.
- Ortiz-Hernández, L.; Pérez-Sastré, M.A. Social Inequalities in the Progression of COVID-19 in the Mexican Population. Rev. Panam. Salud Publica/Pan Am. J. Public Heal. 2020, 44, 1–8. [Google Scholar] [CrossRef]
- Marcela Vélez, C. COVID-19 and Vaccination in Latin America and the Caribbean: Challenges, Needs and Opportunities 2021, 1–88.
- Islam, N.; Lacey, B.; Shabnam, S.; Erzurumluoglu, A.M.; Dambha-Miller, H.; Chowell, G.; Kawachi, I.; Marmot, M. Social Inequality and the Syndemic of Chronic Disease and COVID-19: County-Level Analysis in the USA. J. Epidemiol. Community Health 2021, 75, 496–500. [Google Scholar] [CrossRef]
| Variable | Total n (%) |
Survivor n (%) |
Non-survivor n (%) |
P Value |
|---|---|---|---|---|
| Sex (Male/Female), n | 845/413 | 741/352 | 104/61 | 0.248 |
| ± S.D.) years | 56.2 ± 16.5 | 54.4 ± 16.0 | 68.3 ± 14.2 | <0.001 |
| BMI classification, % | ||||
| Underweight | 10 (0.8%) | 9 (0.8%) | 1 (0.6%) | |
| Normal BMI | 240 (19.1%) | 199 (18.4%) | 41 (24.8%) | |
| Overweight | 486 (38.6%) | 423 (38.3%) | 63 (38.2%) | 0.399 |
| Obesity grade I | 322 (25.6%) | 285 (26.1%) | 37 (22.4%) | |
| Obesity grade II | 114 (9.1%) | 103 (9.3%) | 11 (6.7%) | |
| Obesity grade III | 86 (6.8%) | 74 (7.0%) | 12 (7.3%) | |
| Hypertension (%) | 427 (33.9%) | 346 (31.7%) | 81 (49.1%) | <0.001 |
| Diabetes (%) | 270 (21.5%) | 216 (19.8%) | 54 (32.7%) | <0.001 |
| COPD (%) | 34 (2.7%) | 22 (2.0%) | 12 (7.3%) | 0.001 |
| Asma (%) | 27 (2.1%) | 25 (2.3%) | 2 (1.2%) | 0.422 |
| Immunosuppression (%) | 56 (4.5%) | 42 (3.8%) | 14 (8.5%) | 0.010 |
| Cancer (%) | 60 (4.8%) | 42 (3.8%) | 18 (10.9%) | <0.001 |
| HIV (%) | 2 (0.2%) | 2 (0.2%) | 0 (0%) | >0.999 |
| Previous stroke (%) | 16 (1.3%) | 11 (1.0%) | 5 (3.0%) | >0.999 |
| CKD (%) | 49 (3.9%) | 39 (3.6%) | 10 (6.1%) | 0.021 |
| Organ transplant recipient (%) | 16 (1.3%) | 14 (1.3%) | 2 (1.2%) | >0.999 |
| Chronic liver disease (%) | 9 (0.7%) | 8 (0.7%) | 1 (0.6%) | >0.999 |
| ACEI/ARA (%) | 283 (22.5%) | 234 (21.4%) | 49 (29.7%) | 0.021 |
| Previous myocardial infarction (%) | 35 (2.8%) | 23 (2.1%) | 12 (7.3%) | 0.001 |
| Depression (%) | 17 (1.4%) | 15 (1.4%) | 2 (1.2%) | 0.830 |
| Smoker (%) | ||||
| Never | 808 (64.2%) | 715 (65.4%) | 93 (56.4%) | |
| Unknown | 301 (23.9%) | 257 (23.5%) | 44 (26.7%) | 0.071 |
| Currently | 65 (5.2%) | 54 (4.9%) | 11 (6.7%) | |
| Former | 84 (6.7%) | 67 (6.1%) | 17 (10.3%) | |
| Alcohol use (%) | ||||
| Never | 805 (64.0%) | 700 (64.0%) | 105 (63.6%) | |
| Unknown | 330 (26.2%) | 279 (25.5%) | 51 (30.9%) | 0.114 |
| Currently | 109 (8.7%) | 102 (9.3%) | 7 (4.2%) | |
| Former | 14 (1.1%) | 12 (1.1%) | 2 (1.2%) | |
| COVID-19 pneumonia on imaging (%) | 1,133 (90.1%) | 981 (90.2) | 152 (92.1) | 0.480 |
| NIH severity scale (%) | ||||
| Critical | 64 (5.1%) | 26 (2.4%) | 38 (23.0%) | |
| Moderate | 90 (7.2%) | 85 (7.8%) | 5 (3.0%) | <0.001 |
| Severe | 1,104 (87.8%) | 982 (89.8%) | 122 (73.9%) | |
| ± S.D.) | 6.3 ± 3.3 | 6.0 ± 3.2 | 8.3 ± 3.6 | <0.001 |
| ± S.D.) | 2.1 ± 2.9 | 1.8 ± 3.0 | 3.5 ± 2.1 | <0.001 |
| qSOFA (%) n | ||||
| 0 | 354 (28.1%) | 329 (30.1%) | 25 (15.2%) | |
| 1 | 816 (64.9%) | 714 (65.3%) | 102 (61.8%) | <0.001 |
| 2 | 71 (5.6%) | 47 (4.3%) | 24 (14.5%) | |
| 3 | 17 (1.4%) | 3 (0.3%) | 14 (8.5%) | |
| ± S.D.) | 6.3 ± 2.5 | 6.1 ± 2.2 | 7.9 ± 3.1 | <0.001 |
| Variable | Total n (%) |
Survivor n (%) |
Non-survivor n (%) |
P value |
|---|---|---|---|---|
| Days onset symptom-admission (x ̅ ± S.D.) | 9.2 ± 5.2 | 9.1 ± 5.1 | 10.1 ± 6.1 | 0.027 |
| Length of stay, days (x ̅ ± S.D.) | 12.2 ± 13.7 | 10.6 ± 10.4 | 22.9 ± 24.5 | <0.001 |
| Heart rate (x ̅ ± S.D.) | 89.0 ± 19.2 | 88.6 ± 18.1 | 91.8 ± 24.9 | 0.043 |
| Respiratory rate (x ̅ ± S.D.) | 25.4 ± 7.3 | 25.2 ± 7.0 | 27.5 ± 8.7 | <0.001 |
| ± S.D.) | 82.1 ± 11.6 | 83.4 ± 10.2 | 74.0 ± 15.9 | <0.001 |
| Fever (%) n | 60.1% | 60.2% | 59.4% | 0.865 |
| AVPU score | ||||
| Alert | 1,196 (95.1%) | 1,066 (97.5%) | 130 (78.8%) | |
| Voice | 30 (2.4%) | 17 (1.6%) | 13 (7.9%) | <0.001 |
| Pain | 7 (0.6%) | 1 (0.1%) | 6 (3.6%) | |
| Unresponsive | 25 (2.0%) | 9 (0.8%) | 16 (9.7%) | |
| Cough (%) | 838 (66.6%) | 726 (66.4%) | 112 (67.9%) | 0.724 |
| Headache (%) | 538 (42.8%) | 478 (43.7%) | 60 (36.4%) | 0.077 |
| Dyspnea (%) | 1,041 (82.8%) | 892 (81.6%) | 149 (90.3%) | 0.008 |
| Diarrhea (%) | 252 (20.0%) | 224 (20.5%) | 28 (17.0%) | 0.300 |
| Chest pain (%) | 224 (17.8%) | 193 (17.7%) | 31 (18.8%) | 0.743 |
| Chills (%) | 309 (24.6%) | 275 (25.7%) | 34 (16.4%) | 0.210 |
| Odynophagia (%) | 308 (24.5%) | 281 (37.4) | 27 (29.7%) | 0.011 |
| Myalgias (%) | 458 (36.4%) | 409 (37.4%) | 49 (29.7%) | 0.057 |
| Arthralgias (%) | 406 (32.3%) | 357 (32.7%) | 49 (29.7%) | 0.476 |
| Malaise (%) | 880 (70.0%) | 769 (70.4%) | 111 (67.3%) | 0.466 |
| Rhinorrhea (%) | 151 (12.0%) | 135 (12.4%) | 16 (9.7%) | 0.370 |
| Vomiting (%) | 93 (7.4%) | 83 (7.6%) | 10 (6.1%) | 0.529 |
| Abdominal pain (%) | 77 (6.1%) | 64 (5.9%) | 13 (7.9%) | 0.382 |
| Conjunctivitis (%) | 22 (1.7%) | 20 (1.8%) | 2 (1.2%) | 0.757 |
| Cyanosis (%) | 101 (8.0%) | 71 (6.5%) | 30 (18.2%) | <0.001 |
| Anosmia (%) | 145 (11.5%) | 135 (12.4%) | 10 (6.1%) | 0.018 |
| Dysgeusia (%) | 129 (10.3%) | 118 (10.8%) | 11 (6.7%) | 0.129 |
| Glasgow Coma Scale <15 (%) | 77 (6.1%) | 43 (3.9%) | 34 (20.6) | <0.001 |
| Variable | Total | Survivor | Non-survivor | P value |
|---|---|---|---|---|
| ± S.D.) | 44.1 ± 30.1 | 41.8 ± 26.8 | 59.3 ± 43.4 | <0.001 |
| ± S.D.) | 1.0 ± 1.1 | 1.0 ± 1.2 | 1.1 ± 0.8 | 0.489 |
| ± S.D.) | 0.7 ± 0.6 | 0.8 ± 0.6 | 0.8 ± 0.4 | 0.757 |
| ± S.D.) | 60.8 ± 57.8 | 60.0 ± 53.6 | 66.8 ± 82.3 | 0.242 |
| ± S.D.) | 60.9 ± 67.4 | 62.6 ± 69.9 | 48.2 ± 43.2 | 0.033 |
| ± S.D.) | 102.1 ± 61.4 | 101.4 ± 59.8 | 107.2 ± 72.2 | 0.349 |
| ± S.D.) | 3.6 ± 0.5 | 3.7 ± 0.5 | 3.3 ± 0.5 | <0.001 |
| ± S.D.) | 132.2 ± 101.3 | 128.4 ± 99.5 | 158.9 ± 110.1 | 0.001 |
| ± S.D.) | 9.9 ± 6.8 | 9.6 ± 6.8 | 12.0 ± 6.5 | <0.001 |
| ± S.D.) | 14.4 ± 2.2 | 14.5 ± 2.2 | 13.7 ± 2.4 | <0.001 |
| ± S.D.) | 431.8 ± 5674.5 | 456.7 ± 6092.0 | 269.0 ± 176.9 | 0.700 |
| ± S.D.) | 1285.1 ± 1089.6 | 1260.6 ± 905.3 | 1447.6 ± 1903.7 | 0.234 |
| ± S.D.) | 7173.3 ± 3960.6 | 6978.7± 3832.7 | 8535.34 ± 547.3 | <0.001 |
| ± S.D.) | 7.3 ± 6.3 | 6.8 ± 5.2 | 10.7 ± 10.4 | <0.001 |
| ± S.D.) | 1109.3 ± 2194.0 | 933.8 ± 1947.3 | 2342.0 ± 3214.6 | <0.001 |
| ± S.D.) | 213.0 ± 658.6 | 219.0 ± 699.8 | 179.5 ± 354.5 | 0.718 |
| ± S.D.) | 387.9 ± 212.2 | 371.6 ± 183.0 | 501.1 ± 334.0 | <0.001 |
| ± S.D.) | 422.5 ± 170.6 | 414.0 ± 162.2 | 490.5 ± 299.1 | 0.566 |
| ± S.D.) | 0.18 ± 3.4 | 0.0 ± 0.1 | 1.1 ± 9.0 | 0.291 |
| ± S.D.) | 7.4 ± 0.1 | 7.4 ± 0.1 | 7.4 ± 0.1 | 0.064 |
| ± S.D.) | 80.4 ± 40.1 | 79.0 ± 39.6 | 82.9 ± 41.2 | 0.555 |
| ± S.D.) | 42.4 ± 18.2 | 38.2 ± 12.7 | 49.9 ± 23.4 | 0.001 |
| ± S.D.) | 567.3 ± 5005.8 | 445.0 ± 4448.9 | 784.0 ± 5902.1 | 0.684 |
| Variable | Exp (B) | 95% CI | P Value |
|---|---|---|---|
| >60 years | 2.445 | 1.679-3.561 | <0.001 |
| Cyanosis | 1.825 | 1.195 to 2.787 | 0.005 |
| Previous myocardial infarction | 1.930 | 1.058 to 3.520 | 0.032 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





