Introduction
Psychiatry has been considered to be in a long-term crisis as medical discipline, from the perspectives of both ontology and epistemology (Di Nicola and Stoyanov, 2021). From an epistemological point the main concerns are raised at the confidence in the methods of assessment and relevant taxonomy as well as in the entailed crisis of identity. The common issue for both is the problem of the diagnostic methods validity.
Traditional biomedical knowledge triangulates clinical diagnostic entities upon robust nomothetic networks comprised of molecular, imaging and physiological (functional) alteration bio-markers. As a rule, neither clinical assessment nor the laboratory confirmation methods can constitute a sole diagnostic entity but only the incremental combination between the different measures (Stoyanov 2015). As a results medicine has clear definition and boundaries of normal structures and functions, and delineates disease outside those normative boundaries.
By contrast psychiatry is operating with patchy reductionist paradigmatically framed, conventional diagnostic entities, which can hardly transcend beyond subjective narratives in the context of cultural pluralism (Stoyanov, 2021). Thus, psychopathology is missing consensual theory of normal personality, structure and functional range of mental systems and defines mental disorder very often as lack of manifest psychopathological deviation from the contextual cultural, political and societal norms. Therefore, psychopathological symptoms, signs, syndromes and nosology are seen more as social constructs rather than as real scientific objects or as real kinds with highly problematic taxonomy (Zachar 2014).
In the past decade our efforts were directed towards establishing of a new model of validation in psychiatry, the trans-disciplinary cross-validation, as exposed in detail elsewhere (Todeva 2020). In summary, according to this model, there are convergent and divergent validity operations, which may be tested across clinical diagnostic self-assessment tests and functional MRI in real time. Generally, the approach is adopted from psychometrics, where it is applied to comparisons between different measurement tools (self-administered or observer-based rating scales), which anyway dwell in the domain of subjective patients, or professional narratives. Convergent operations essentially mean that the scores on clinical assessments tools and brain activation as detected by the BOLD (blood oxygenation level dependent) signal in the brain are concordant, or in the same direction. When the two measures happen to be in the opposite directions, this is regarded as divergent validity.
This model has been tested empirically with the depressive scale, paranoid-depressive scale international affective pictures system and Stroop color and word test in various populations (Stoyanov, 2022a). Our group has demonstrated in earlier studies with task related MRI that simultaneous administration of depressive scale as contrasted with diagnostically neutral interest scale in block design, has produced meaningful results, able to distinguish patients with MDE from healthy controls. More specifically the depressive scale item versus neutral items responses yielded significant clusters of residual activation in middle frontal gyrus, reported in depressive patients, and not in controls (Stoyanov 2018).
The aim of the presents study is to further expand the model of translational cross-validation by investigating the brain circuits or networks which underpin the same tasks by means of group independent component analysis for FMRI toolbox (GIFT). We hypothesized that there will be neural network patterns of activation and deactivation, which correspond to real time performance on clinical self-evaluation scales.
Subjects and Methods
Subjects
There were included 42 subjects in this study: 20 healthy controls (HC) and 22 patients with major depressive episode (MDE). Each individual was evaluated by board certified psychiatrists using Mini International Neuropsychiatric interview (Sheehan 1998) and Montgomery–Åsberg Depression Rating Scale (MADRS) (Mongomery 1979). Exclusion criteria were defined as earlier history of comorbid mental disorders (considered for HC and for patients on a separate basis), systematic and organic neurological diseases, cranial trauma, or MRI incompatible metal implants. All participants signed in person a written informed consent following the Declaration of Helsinki. The study was approved by the Medical University of Plovdiv Ethical Committee (2/19.04.2018).
Demographic and Clinical Characteristics
There have been reported no significant differences between the two groups in terms of their age, sex and education distribution. Significantly higher MADRS score is reported for the patient group (see
Table 1).
Methods
MR Scanning
The MR scanning procedure was performed on a 3T MRI system (GE Discovery 750w). The experimental protocol is introduced comprehensively elsewhere (Stoyanov 2021)
fMRI Task
We used a standard block-design paradigm with two different active (ON) conditions and one resting (OFF) condition, with a total duration of 8 min and 32 s. Diagnostically specific (DS) blocks consisted of 4 statements from the 16 items von Zerssen depression scale (D-S by von Zerssen 1986) self-rated on a 4 degrees Likert scale by pressing buttons.
D-S blocks were contrasted with blocks of diagnostically neutral (DN) items selected from an interest scale. There were four active blocks of each type, alternating DS and DN conditions, and each ON block was followed by a resting state “OFF” block.
Detailed description of the paradigm structure has already been published (Stoyanov 2018, Stoyanov 2021).
Image Processing
Neuroimaging data were processed using SPM 12 software (Statistical Parametric Mapping,
http://www.fil.ion.ucl.ac.uk/spm/) running on MATLAB R2021 for Windows. The functional images of each participant were processed following established procedures - realignment, co-registration with the high-resolution anatomical image, and normalization to standard MNI space (for more comprehensive details see Stoyanov 2021, 2022).
Data Analysis
We analyzed the differences in brain activation patterns during the experimental conditions between HC and MDD patients. First, we identified brain networks that were activated in response to the task across all subjects. We considered the comparisons between the diagnostically specific (DS) vs rest (OFF) blocks, the diagnostically neutral (DN) vs rest blocks, and DS vs DN blocks using the circuit-based approach through the individual component analysis (see the “Independent component analysis” section). Then, we compared the activity of regions in the revealed brain networks between HC and MDD groups of subjects via statistical parametric mapping (see the “Statistical analysis” section).
Independent Component and Statistical Analysis
Group ICA (Calhoun et al. 2001 and 2003; Calhoun and Adali 2012) was performed to identify brain networks that were activated in response to a task (DS vs OFF, DN vs OFF, DS vs DN). ICA was performed on the BOLD fMRI scans of all 42 subjects using GIFT (
http://trendscenter.org/software/gift). We computed individual ICA solutions employing the Infomax algorithm (Bell 1995). For the group ICA, all subjects were analyzed concurrently, and principal component analysis (PCA) was used for compression. ICA attempts to decompose a multiple signal into independent, mostly non-Gaussian, signals. This approach has been widely used for fMRI data processing (Colato 2021; Forsyth, 2020; Morie, 2021).
The number of components selected was 50. The choice of the number of components is effectively a choice of the spatial scale of the results (fewer components leads to larger brain networks). The component time courses were analyzed using multiple regression to evaluate the components, which are modulated by the task. We first calculated slopes of regression for the conditions and obtained beta-weights for each of the components. The resulting beta values were analyzed via a one sample t-test across subjects to identify significant effects at the false discovery rate (FDR) corrected p<0.025. We extracted the list of the areas corresponding to the component activity in MNI and Talairach coordinates using the “Write Talairach Table” procedure in GIFT with the following parameters: threshold – 3.5 and the distance between the contiguous voxels – 4 mm.
Statistical Analysis
We used the statistical parametric mapping (SPM 12 software) to analyze the ICA component maps in order to reveal clusters of voxels (brain regions) that showed significant difference in response to the task between HC and MDD groups of subjects. Analysis included factorial design specification where we used a two-sample t-test with two groups (HC and MDD). The volumes of significantly changed components revealed in DS vs OFF, DN vs OFF, DS vs DN comparisons on the ICA analysis step were used as input data. An implicit mask was set by default. No global normalization was used. The restricted maximum likelihood method was used for the general linear model parameters estimation. This assumes the error correlation structure is the same at each voxel. For the contrasting we used t-contrast approach including two groups and [1 -1] and [-1 1] weights for the HC>MDD and MDD>HC conditions, respectively. Statistical significance was determined by cluster forming threshold of uncorrected p-value less than 0.05 and a peak level of p<0.001 uncorrected.
Results
Independent Component Analysis
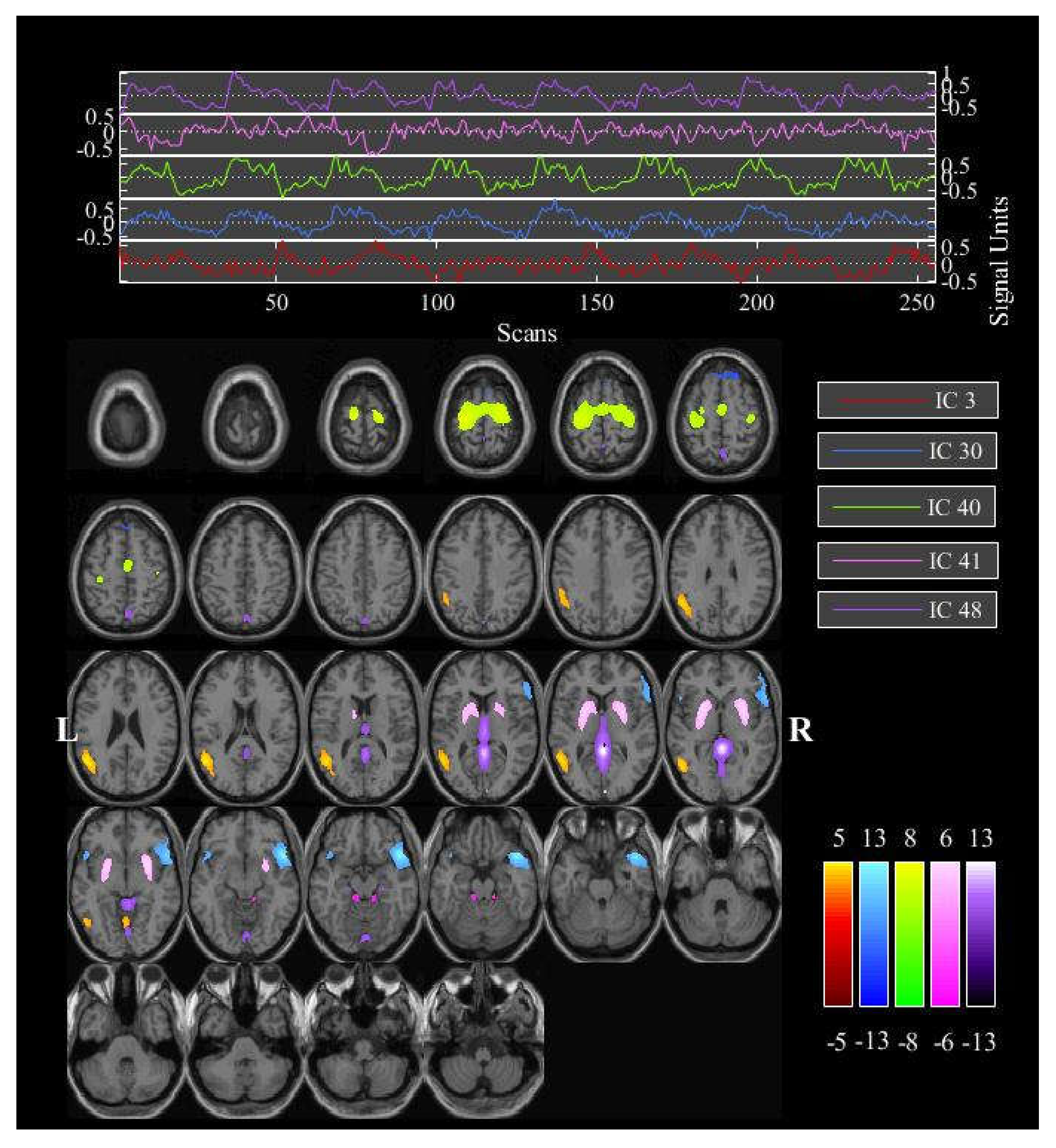
We first looked at which brain networks were activated when a subject responded to the task. The GIFT analysis identified one significantly activated component (#4) for the condition DS vs OFF, none – for the DN condition vs OFF, and five components – for the DS vs DN comparison (
Figure 1). The time series and activity areas corresponding to the components are shown in
Figures S1–S6 and
Tables S1 and S2 in the
Supplementary Materials.
Statistical Parametric Mapping (SPM) Results
SPM mapping was utilized to analyze the regional brain network differences in within network connectivity between HC and MDD groups of subjects for the task modulated components. Within the 4th component, which is modulated by the DS vs OFF, we found three clusters of voxels with peaks located in left anterior cingulate gyrus, right middle frontal gyrus, and right calcarine cortex (
Table 2). It has significantly more connectivity in controls (HC) compared to patients (MDD). No significant clusters were found for the opposite MDD>HC contrast.
Within the 3rd component, which is modulated by the DS task relative to the DN task, we found one cluster of voxels with significantly more connectivity in HC compared to MDD and one more on a trend level p=0.07. Their peaks were located in right middle cingulate gyrus and right superior frontal gyrus respectively (
Table 3). No significant clusters were found for the opposite MDD>HC contrast. No significant clusters were found for the other components for either contrast.
Discussion
This study has demonstrated independent component analysis of brain networks positively or negatively modulated during processing of diagnostic specific task questions for major depressive disorder. The first important finding is the significant difference in the activation of component 4 in ICA and SPM for diagnostic condition contrasted to resting state blocks. It is of particular interest that no such difference exists for the neutral condition, which may well be considered as a measure of what has been defined as translational validity operation in the introduction. The component includes a distributed circuit of thalamus, caudate, middle temporal gyrus, superior and middle frontal gyri, inferior parietal lobule, and lingual gyrus.
The middle frontal gyrus has previously been associated with the residual activations during processing of depression scale versus neutral items in depressive patients (Stoyanov, 2018). The region is essential for the selective attention, working memory and inhibitory control, which are impaired during a major depressive episode. In addition, lingual and fusiform gyri appear to be a hub of disturbed connectivity in our most recent studies of functional connectivity (Stoyanov, 2022b). That may be interpreted in the sense of an over-arousal or vulnerability of the same region at rest, which is highlighted by the diagnostic task in patients with depression as hypo-activation.
These results are also consistent with the studies of Escamilla (2018) and Petckovsky (2013) with Word Association Test of Carl Gustav Jung. In those studies, emotionally significant complex triggering words activate similar patterns to the common network, including superior and middle frontal gyrus, caudate, temporal areas and deactivate precuneus, medial frontal gyrus, cingulate and thalamus. In our study, the associated regions also include inferior parietal lobule, including supramarginal gyrus and angular gyrus, which take part in the mechanisms of empathy and understanding of emotions and theory of mind. Lingual and fusiform gyrus have also been previously reported by our group to be hypo-activated in patients with depression during execution of Stroop Color and Word test (Simeonova, 2022). The impairment of those functions is pivotal for a major depressive episode.
The second finding of the current study is that the preferential processing of depression scale items as compared to neutral item responses is associated with patterns of activity in five independent components which encompass common, shared and distinct networks across components during the processing of the diagnostic specific scale items. The distinct may be subtracted from the common ones.
An executive summary of the same is presented in
Table 4. The common network for all or both DS vs OFF and DS vs DN independent components (IC) includes superior and middle frontal gyri, inferior parietal lobule (comprised of supramarginal gyrus and angular gyrus), middle and superior temporal gyri, middle occipital gyrus, thalamus (IC4 and IC48), caudate (IC4 and IC41) and lingual gyrus (IC4, IC3, IC41). The
shared circuit between DS vs DN components, involve cuneus, precuneus (all 5 IC), culmen (IC3 and IC48), parahippocampal gyrus (30 and 48), superior parietal lobule (IC40 and IC41); medial frontal gyrus (IC3 and IC40); and precentral gyrus (IC3, IC30, IC40). The
distinct or unique regions/networks which are revealed in IC3 includes inferior temporal gyrus, in IC41 - lentiform nucleus and in component 48 - posterior cingulate and fusiform gyrus.
The common circuit corresponds to major nodes from the triple network and is involved in word and language semantic processing, empathy and self-reflection. In that context verbal self-evaluation scale items are normally expected to yield activations in those regions.
The shared circuit between DS vs DN components, involves caudate, cuneus and precuneus, thalamus, medial frontal gyrus, culmen, parahippocampal gyrus, superior parietal lobule; and precentral gyrus. Thalamus and parahippocampal gyrus are implicated as connections of the limbic distributed system, whereas caudate and culmen belong to the basal ganglia, that play critical role in affective regulation and disorders (Ikemoto 2015, Macpherson, T & Hikida, T. 2019). They should be expected therefore to process emotional content of stimuli.
Medial frontal gyrus, precuneus and angular gyrus belong to a system of autobiographical memory and self-identity, which is apparently disturbed in depression. As it has been already demonstrated by means of effective connectivity measures and other task related paradigm (paranoid-depressive scale) in our previous publications, the latter regions are implicated in the mechanisms of affective disorders (Aryutova 2021). More specifically changes in effective connectivity of precuneus with orbitofrontal cortex as defined by means of dynamic causal modelling can potentially differentiate major psychiatric disorders (Kandilarova 2022). Activations in the same area during processing of a task with paranoid scale items differentiate schizophrenia from depression as well (Stoyanov 2021). This may well indicate that the modulation of precuneus and its connections have opposite dysfunctions in two major clusters of mental disorders: schizophrenia and depression.
The distinct or unique networks are found within Component 3 - inferior temporal gyrus, Component 41 - lentiform nucleus and Component 48 - posterior cingulate and fusiform gyrus. All of those areas are clearly and traditionally associated with neural systems regulating cognitive and emotional functions in health and disease (Squire, ed, 2012, Banich, M. T., & Compton, R. J. 2018, Cheng 2018)
In summary, the patterns of activation behind depression scale encompass components from triple and limbic networks, which are not activated during neutral items processing. Preferential processing of the depression scale items by those components indicates that they measure properly depression as diagnostic construct and thereby may reify it in terms of incremental validity (Zachar 2012, Stoyanov 2012, Stoyanov, 2020).
The third major finding of the present study is that there have been confirmed differences in the networks processing diagnostic (DS) versus off blocks between patients and controls in Components 4 with SPM, mainly anterior cingulate cortex and middle frontal gyrus. The deregulation of this crucial hub for processing of verbal information, convergence of dorsal and ventral attention networks and salience network, is consistent with our previous findings using the same paradigm in patients with depression (Stoyanov 2018) and with resting state fMRI (Kandilarova 2021).
The fourth and most significant finding of the current study is DS contrasted to DN conditions demonstrate differential activity of right superior frontal gyrus and right middle cingulate cortex in the comparison of patients with healthy controls. This finding implicates deregulation of the triple network in depression, critically affecting self-awareness and pro-social behavior. Although such dysfunctions have been previously reported (Zheng 2018, Cheng 2018, Liu 2017), it is for the first time when potential neuroimaging state dependent biomarker has been directly linked with clinical assessment self-evaluation scale, administered as stimuli simultaneously with the fMRI acquisition. It may be regarded as further evidence in support of the ability of both methods to concordantly distinguish groups by means of incremental translational cross-validation (Stoyanov, 2022a).
Limitations
This study is based on relatively small sample. However, in neuropsychiatric imaging, unless large-scale consortia are involved, this is not unusual, including when independent component analysis is used (see Liu 2021 for example). The limited size of the sample is partly compensated for by the intensive and comprehensive methodology. Replication studies under the same design are necessary in order to confirm the results.
Conclusions
In the recent decade much progress has been achieved toward implementation of functional MRI studies in neuropsychiatry. Yet translation between neuroimaging findings and psychopathology remains a major challenge. The current contribution adds to a body of evidence that the translation may be facilitated by validation of clinical evaluation tests as integrated into task - based fMRI paradigm. Given the non-linear temporal complexity of both mental and neural system dynamics, a methodological frameshift from mainstream statistics toward non-conventional approaches for data analysis such as GIFT would also have potential impact on incremental validity of clinical methods.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
References
- Aryutova, K., Stoyanov, D. S., Kandilarova, S., Todeva-Radneva, A., & Kostianev, S. S. (2021). Clinical Use of Neurophysiological Biomarkers and Self-Assessment Scales to Predict and Monitor Treatment Response for Psychotic and Affective disorders. Current Pharmaceutical Design, 27(39), 4039-4048. [CrossRef]
- Aryutova, K., Paunova, R., Kandilarova, S., Stoyanova, K., Maes, M. H., & Stoyanov, D. (2021). Differential aberrant connectivity of precuneus and anterior insula may underpin the diagnosis of schizophrenia and mood disorders. World Journal of Psychiatry, 11(12), 1274. [CrossRef]
- Bell AJ, Sejnowski TJ. Afrn information-maximization approach to blind separation and blind deconvolution. Neural Computation. 1995;7(6):1129–1159. [CrossRef]
- Calhoun, V. D., Adali, T., Pearlson, G., & Pekar, J. (2001, December). Group ICA of functional MRI data: separability, stationarity, and inference. In Proc. Int. Conf. on ICA and BSS San Diego, CA. p (Vol. 155).
- Calhoun, V. D., Adali, T., Pekar, J. J., & Pearlson, G. D. (2003). Latency (in) sensitive ICA: group independent component analysis of fMRI data in the temporal frequency domain. NeuroImage, 20(3), 1661-1669. [CrossRef]
- Banich, M. T., & Compton, R. J. (2018). Cognitive neuroscience. Cambridge University Press.
- Chen Z, Xia M, Zhao Y, Kuang W, Jia Z, Gong Q. Characteristics of Intrinsic Brain Functional Connectivity Alterations in Major Depressive Disorder Patients With Suicide Behavior. J Magn Reson Imaging. 2021 Dec;54(6):1867-1875. Epub 2021 Jun 16. [CrossRef] [PubMed]
- Cheng, W., Rolls, E. T., Qiu, J., Yang, D., Ruan, H., Wei, D., ... & Feng, J. (2018). Functional connectivity of the precuneus in unmedicated patients with depression. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(12), 1040-1049. [CrossRef]
- Cheng, W., Rolls, E. T., Qiu, J., Xie, X., Wei, D., Huang, C. C., ... & Feng, J. (2018). Increased functional connectivity of the posterior cingulate cortex with the lateral orbitofrontal cortex in depression. Translational Psychiatry, 8(1), 1-10. [CrossRef]
- Colato E, Stutters J, Tur C, Narayanan S, Arnold DL, Gandini Wheeler-Kingshott CAM, Barkhof F, Ciccarelli O, Chard DT, Eshaghi A. Predicting disability progression and cognitive worsening in multiple sclerosis using patterns of grey matter volumes. J Neurol Neurosurg Psychiatry. 2021 Sep;92(9):995-1006. [CrossRef]
- Forsyth A, McMillan R, Campbell D, Malpas G, Maxwell E, Sleigh J, Dukart J, Hipp J, Muthukumaraswamy SD. Modulation of simultaneously collected hemodynamic and electrophysiological functional connectivity by ketamine and midazolam. Hum Brain Mapp. 2020 Apr 15;41(6):1472-1494. [CrossRef]
- Di Nicola, V., & Stoyanov, D. (2021). Psychiatry in Crisis: At the Crossroads of Social Sciences, the Humanities, and Neuroscience. Springer Nature.
- Du, Y., Fu, Z., Sui, J., Gao, S., Xing, Y., Lin, D., & Calhoun, V. (2019). NeuroMark: an adaptive independent component analysis framework for estimating reproducible and comparable fMRI biomarkers among brain disorders. MedRxiv, 19008631.
- Escamilla, M., Sandoval, H., Calhoun, V., & Ramirez, M. (2018). Brain activation patterns in response to complex triggers in the Word Association Test: results from a new study in the United States. Journal of Analytical Psychology, 63(4), 484-509. [CrossRef]
- Ikemoto, S., Yang, C., & Tan, A. (2015). Basal ganglia circuit loops, dopamine and motivation: a review and enquiry. Behavioural brain research, 290, 17-31. [CrossRef]
- Kandilarova, S., Stoyanov, D. S., Paunova, R., Todeva-Radneva, A., Aryutova, K., & Maes, M. (2021). Effective connectivity between major nodes of the limbic system, salience and frontoparietal networks differentiates schizophrenia and mood disorders from healthy controls. Journal of Personalized Medicine, 11(11), 1110. [CrossRef]
- Kandilarova, S., Stoyanov, D., Aryutova, K., Paunova, R., Mantarkov, M., Mitrev, I., ... & Specht, K. (2022). Effective Connectivity Between the Orbitofrontal Cortex and the Precuneus Differentiates Major Psychiatric Disorders: Results from a Transdiagnostic Spectral DCM Study. CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders). [CrossRef]
- Liu, C. H., Ma, X., Yuan, Z., Song, L. P., Jing, B., Lu, H. Y., ... & Wang, C. Y. (2017). Decreased resting-state activity in the precuneus is associated with depressive episodes in recurrent depression. The Journal of clinical psychiatry, 78(4), 22409. [CrossRef]
- Liu, G., Jiao, K., Zhong, Y., Hao, Z., Wang, C., Xu, H., ... & Wang, C. (2021). The alteration of cognitive function networks in remitted patients with major depressive disorder: an independent component analysis. Behavioural Brain Research, 400, 113018. [CrossRef]
- Macpherson, T., & Hikida, T. (2019). Role of basal ganglia neurocircuitry in the pathology of psychiatric disorders. Psychiatry and clinical neurosciences, 73(6), 289-301. [CrossRef]
- Maglanoc, L. A., Kaufmann, T., Jonassen, R., Hilland, E., Beck, D., Landrø, N. I., & Westlye, L. T. (2020). Multimodal fusion of structural and functional brain imaging in depression using linked independent component analysis. Human brain mapping, 41(1), 241-255. [CrossRef]
- Maes, M. H., & Stoyanov, D. (2022). False dogmas in mood disorders research: Towards a nomothetic network approach. World Journal of Psychiatry, 12(5), 651. [CrossRef]
- Montgomery, S.A.; Åsberg, M. A New Depression Scale Designed to be Sensitive to Change. Br. J. Psychiatry 1979, 134, 382–389. [CrossRef]
- Morie KP, DeVito EE, Potenza MN, Worhunsky PD. Longitudinal changes in network engagement during cognitive control in cocaine use disorder. Drug Alcohol Depend. 2021 Dec 1;229(Pt A):109151. [CrossRef]
- Petchkovsky, L., Petchkovsky, M., Morris, P., Dickson, P., Montgomery, D., Dwyer, J., & Burnett, P. (2013). fMRI responses to Jung’s Word Association Test: implications for theory, treatment and research. Journal of Analytical Psychology, 58(3), 409-431. [CrossRef]
- Simeonova, D., Paunova, R., Stoyanova, K., Todeva-Radneva, A., Kandilarova, S., & Stoyanov, D. (2022). Functional MRI Correlates of Stroop N-Back Test Underpin the Diagnosis of Major Depression. Journal of Integrative Neuroscience, 21(4), 113. [CrossRef]
- Stoyanov, D., Machamer, P. K., Schaffner, K. F., & Rivera-Hernández, R. (2012). The meta-language of psychiatry as cross-disciplinary effort: In response to Zachar (2012). Journal of Evaluation in Clinical Practice, 18(3), 710-720. [CrossRef]
- Stoyanov, D. S., Stieglitz, R. D., Lenz, C., & Borgwardt, S. (2015). The translational validation as novel approach to intergration of neuroscience and psychiatry. In Stoyanov D (Ed), New developments in Clinical Psychology Research, NY: Nova Science.
- Stoyanov, D., Kandilarova, S., & Borgwardt, S. (2017). Translational functional neuroimaging in the explanation of depression. Balkan Medical Journal, 34(6), 493-503. [CrossRef]
- Stoyanov, D., Kandilarova, S., Borgwardt, S., Stieglitz, R. D., Hugdahl, K., & Kostianev, S. (2018). Psychopathology assessment methods revisited: on translational cross-validation of clinical self-evaluation scale and fMRI. Frontiers in Psychiatry, 9, 21. [CrossRef]
- Stoyanov, D. (2020). The reification of diagnosis in psychiatry. Neurotoxicity Research, 37(3), 772-774.). [CrossRef]
- Stoyanov, D., Fulford, B., Stanghellini, G., Van Staden, W., & Wong, M. T. (2021). International perspectives in values-based mental health practice: Case studies and commentaries (p. 436). Springer Nature. [CrossRef]
- Stoyanov, D., Aryutova, K., Kandilarova, S., Paunova, R., Arabadzhiev, Z., Todeva-Radneva, A., ... & Borgwardt, S. (2021). Diagnostic task specific activations in functional MRI and aberrant connectivity of insula with middle frontal gyrus can inform the differential diagnosis of sychosis. Diagnostics, 11(1), 95. [CrossRef]
- Stoyanov, D. (2022a). Perspectives before incremental trans-disciplinary cross-validation of clinical self-evaluation tools and functional MRI in psychiatry: 10 years later. Frontiers in Psychiatry, 13. [CrossRef]
- Stoyanov, D., Khorev, V., Paunova, R., Kandilarova, S., Simeonova, D., Badarin, A., ... & Kurkin, S. (2022b), Resting-State Functional Connectivity Impairment in Patients with Major Depressive Episode. International Journal of Environmental Research and Public Health, 19(21), 14045.). [CrossRef]
- Squire, L., Berg, D., Bloom, F. E., Du Lac, S., Ghosh, A., & Spitzer, N. C. (Eds.). (2012). Fundamental neuroscience. Academic press.
- Todeva-Radneva, A., Paunova, R., Simeonova, D., Kandilarova, S., & Stoyanov, D. (2020). Transdisciplinary Validation of Clinical Psychological Scales and Functional MRI. SAGE Publications Ltd.
- Todeva-Radneva, A., Paunova, R., Kandilarova, S., & St Stoyanov, D. (2020). The value of neuroimaging techniques in the translation and Transdiagnostic validation of psychiatric diagnoses-selective review. Current Topics in Medicinal Chemistry, 20(7), 540-553. [CrossRef]
- Rodriguez, P. A., Calhoun, V. D., & Adalı, T. (2012). De-noising, phase ambiguity correction and visualization techniques for complex-valued ICA of group fMRI data. Pattern recognition, 45(6), 2050-2063. [CrossRef]
- Reddy MS. Depression: the disorder and the burden. Indian J Psychol Med. 2010 Jan;32(1):1-. [CrossRef] [PubMed] [PubMed Central]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Balker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. S20), 22–33.
- von Zerssen D. Clinical Self-Rating Scales (CSRS) of the MunichPsychiatric Information System (PSYCHIS München). In: Sartorius N,Ban TA, editors. Assessment of depression. Berlin: Springer (1986). [CrossRef]
- Zachar, P. (2012). Is incremental validity too incremental in the long run? A commentary on Stoyanov D., Machamer PK & Schaffner, KF (2012). Journal of Evaluation in Clinical Practice, 18 (1) 149-154. Journal of evaluation in clinical practice, 18(1), 157-158. [CrossRef]
- Zachar, P., Stoyanov, D. S., Aragona, M., & Jablensky, A. (Eds.). (2014). Alternative perspectives on psychiatric validation. OUP Oxford.
- Zheng, H., Li, F., Bo, Q., Li, X., Yao, L., Yao, Z., ... & Wu, X. (2018). The dynamic characteristics of the anterior cingulate cortex in resting-state fMRI of patients with depression. Journal of affective disorders, 227, 391-397. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).