1. Introduction
Osteoporosis is a major health issue of geriatrics and epidemiology, and occurrence of osteoporosis-related fractures lead to significant physical and economic burdens [
1]. However, osteoporosis is four times more common in women than in men because women have bone loss at a younger age and this rapidly increases in elderly women more than in men [
2]. Patients and family members need information and knowledge from health professionals to prevent such bone fragility, and multifaceted group education has shown positive impacts and could help the patient enhance their ability in managing osteoporosis [
3]. After formal education of osteoporosis, professionals may use scales to assess osteoporosis knowledge or health belief, although such scales only measure osteoporosis cogitation [
4,
5], without attitude or behaviors under treatment.
In this study, we developed the Osteoporosis Knowledge, Attitude, and Behaviors Questionnaire (OKABQ) to assess osteoporosis knowledge, attitude and behaviors in patients with osteoporosis. The questionnaire was developed based on the experiences and perceptions of the sampled patients, physicians, nurses and the related literature [
4,
6,
7], with the aim of (a) developing the preliminary version of the OKABQ, (b) constructing the validity of OKABQ, and (c) verifying a mediation model.
2. Materials and Methods
2.1. Hypothesis
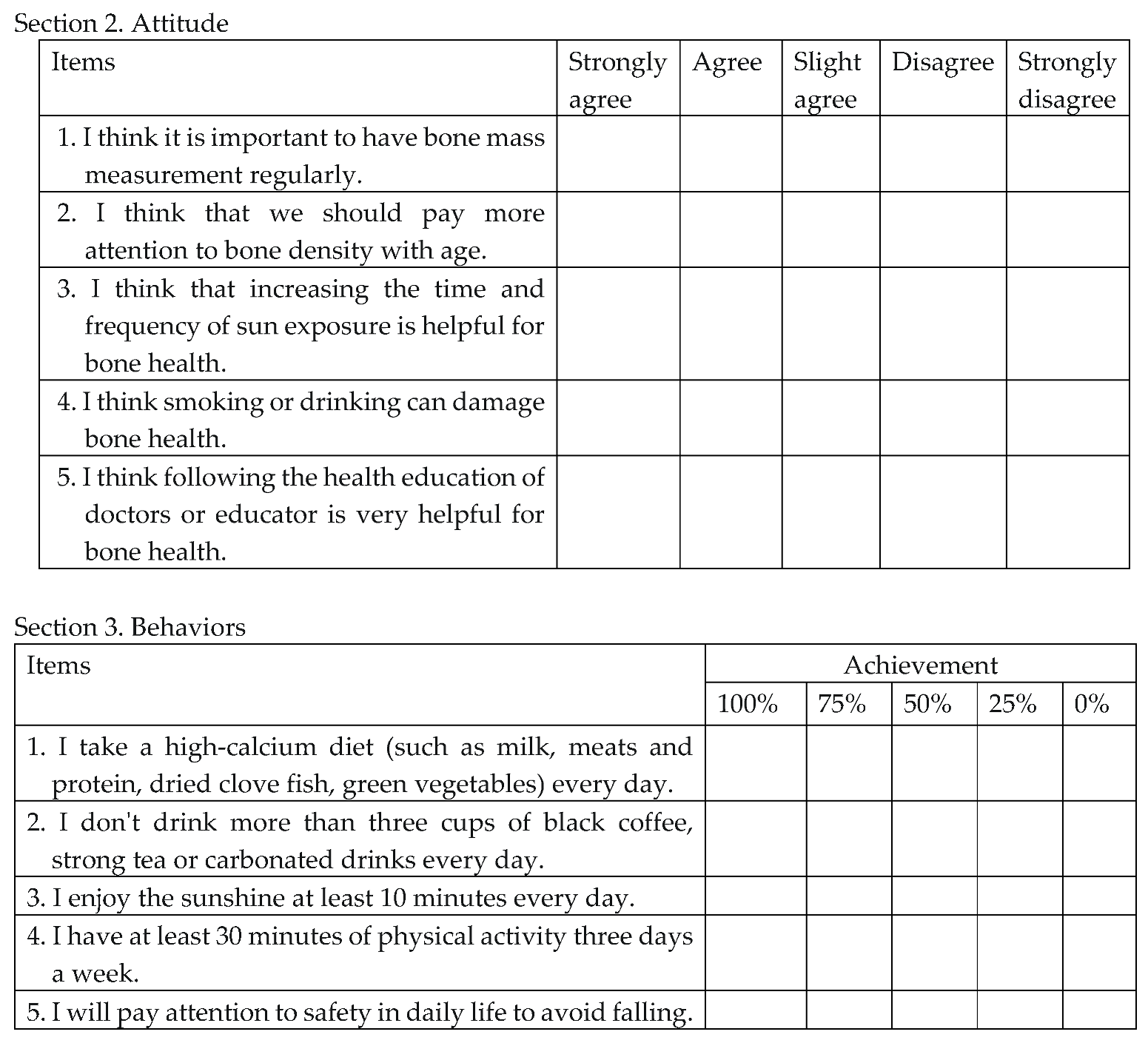
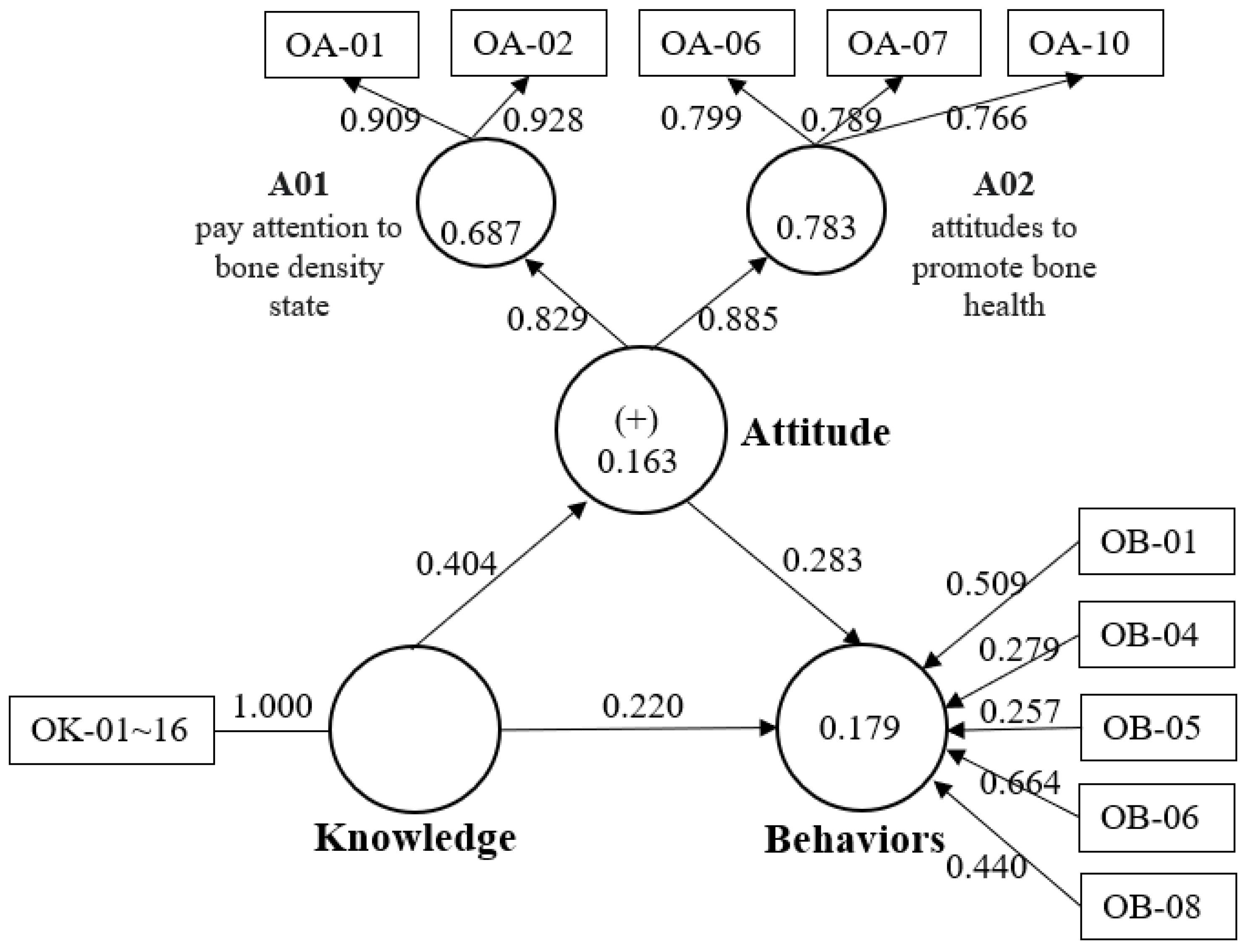
OKABQ has good psychometric properties of validity and reliability. It is to be used in the traditional Chinese context as an instrument for measuring the levels of osteoporosis knowledge about risk factors, attitude to disease and self-efficacy for bone health behavior change perceived in a comprehensive osteoporosis education program for the osteoporosis patient. Research framework (
Figure 1) indicates that the knowledge, attitude, and practice (KAP) model [
8] was used to examine the hypothesis that attitude is a mediating variable in affecting knowledge and behaviors.
2.2. Study Design and Participants
A cross-sectional, descriptive instrument development study was designed. Throughout May 2019, the sample of pilot study was convenience sampling obtained via personalized contact of the principal investigator and the physician of the outpatient clinic at the hospital in Taiwan.
The inclusion criteria of this study were as follows: (a) being diagnosed with osteoporosis by a physician; (b) women aged 40 years or older; (c) being conscious and able to communicate in Mandarin Chinese or Taiwanese; and (d) agreeing to participate in the study after giving informed consent. Patients were excluded if they (a) had any mental illness or pregnancy; or (b) joined other interventional studies during the study period. Two phases were used to develop the OKABQ.
2.2.1. Phase I—Initial item pool and pilot study
We used a Delphi Method to identified the concepts for osteoporosis key knowledge and attitude with the implementation of two rounds [
9,
10]. The first round, the preliminary version of the OKABQ, was drafted in Chinese language context and refined by five osteoporosis clinical researchers and physicians with expertise in bone health issues by in-person meeting and e-mail (from August- December 2018). Osteoporosis guidelines concerning risk-factors and health issues from the World Health Organization (WHO) and the International Osteoporosis Foundation (IOF) were used as references [
11,
12,
13,
14,
15,
16,
17,
18]. A literature review and KAP model [
19] provided the structure, the component of osteoporosis disease treatment and follow-up issues. In the second round, the experts had to evaluate the importance of each item using a Likert scale ranging from 1, “not relevant”, to 4, “highly relevant”. The process included comments about suitability and clarity that provided drafting or added words as revised opinion.
2.2.2. Phase II—Item analysis, assess validity and reliability of OKABQ and mediation analysis
In this phase, we continued the study on the same patients to test the OKABQ between July 2019 to April 2020, having used convenience sampling to enroll osteoporosis patients by two researchers at the outpatient clinic. The questionnaire was provided as hard copies and collected at the same time, but a separate group of patients was randomized to attend the test for reliability and validity collected two weeks later.
The second version of OKABQ included 34 items in a first-order confirmatory model. The Root-Mean-Square error of approximation (RMSEA) was used, with a null-hypothesized RMSEA ≦ 0.05, alternative-hypothesized RMSEA of 0.08 and an anticipated effect size of 0.3, using normal α 0.05 and 80% power. Based on the assumptions, the minimum sample size was 170 to 291, and according to the model, it could be tested as a close-fit version [
20,
21,
22].
2.3. Data Analysis
In phase I, all statistical analyses and data entered were performed using SPSS (Version 20). The following results indicate the questionnaire was adequate in recommending a minimum S-CVI of 0.80 [
24]. The readability of the items was solicited and the validity of the questionnaire was obtained from statistical results.
In phase II, the overall internal consistency of the questionnaire was analyzed as stratified Cronbach's α. Both the test and the retest were calculated by Cronbach's α. The homogeneity and the Intraclass Correlation Coefficient (ICC) for temporal stability of the test-retest were evaluated; then, two Confirmatory Factor Analyses (CFA) model was used to evaluate the internal structure of the OKABQ by using structural equation modeling (SEM) in SmartPLS [
25] and its relationships with other variables at the latent level. CFA could test the hypothesized structure and relationships among the factors to check factor loading that allowed for estimation and removal [
26,
27] in order to construct a mediation model that followed SEM and set 5000 random subsamples in Bootstrapping [
23]. The KR-20 was 0.93 and Cronbach’s α was 0.70 [
16]. Composite reliability (CR) can measure internal consistency reliability proposed threshold value for confirmative research that values > 0.80 and must not be lower than 0.60, while average variance extracted (AVE) can measure convergent validity that proposed the threshold value: AVE > 0.50 [
23].
2.4. Ethical Aspects
The 3-year study was approved by the Institutional Review Board (KMUHIRB-E(I)-20180317). All the participants voluntarily took part in this study and were guaranteed anonymity and confidentiality of all data.
3. Results
3.1. Phase I
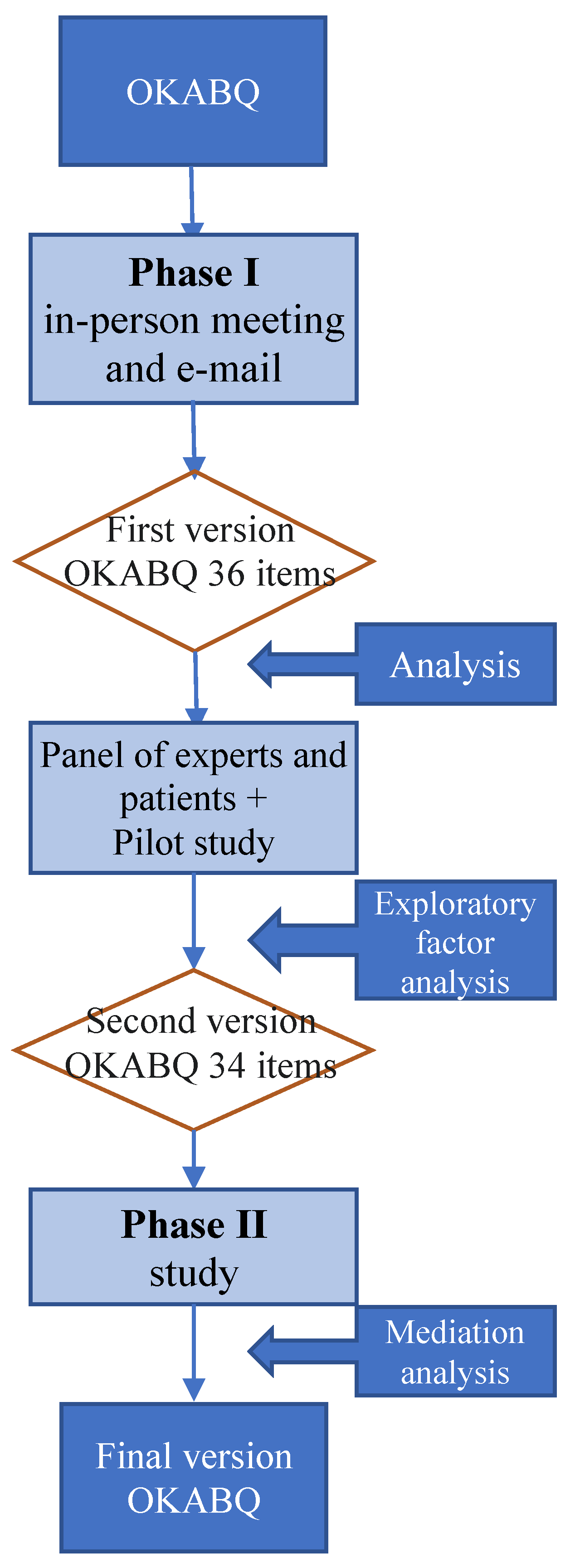
The development of OKABQ was structured and as follows (
Figure 2):
3.1.1. Preparatory and integration period
The first version of the OKABQ was obtained from the osteoporosis clinical researchers and experts in referring to a literature review of bone health issue; it comprised three sections of osteoporosis: Knowledge, Attitude and Behaviors that included 36 items.
The second round was held with a panel of experts and a pilot study. The CVI of the overall scale and the subscale were 0.99, 1.00, 1.00, and 0.96 respectively. We tested the readability and comprehension of these items by soliciting the comments of five experts and twenty-three patients in the pilot study (
Table 1).
Two items were rephrased and merged in the pilot test. The inter-rater reliability (IRR) of two researchers indicated a kappa of 1.00, representing perfect agreement [
28]. According to the research results, the second version of OKABQ was reduced to 34 items.
3.1.2. Construct period
Knowledge section showed Kaiser-Meyer-Olkin (KMO) was 0.61 and the Bartlett test of sphericity was significant (p < 0.0001), representing non-fit by using factor analysis. Attitude and Behaviors sections used Exploratory Factor Analysis (EFA) with varimax rotation to extract dimensions of the scale. KMO was 0.72 and 0.64 and Bartlett test of sphericity was significant (p < 0.0001), representing that these two sections were suitable for factor analysis.
3.2. Phase II
3.2.1. Descriptive analyses
In total, 262 patients with an age range from 47.2 to 96.6 and mean age of 71.7 (SD = 9.4) participated in the study (
Table 1). Most of them had an elementary school (29.0%) level of education, were married (57.3%), had postmenopausal period (92.0%), had never smoked (98.9%), but only 26.0% had a family history of osteoporosis.
Mean of total scores, Knowledge section, Attitude section and Behaviors section scored 47.12 (SD = 6.082), 12.08 (SD = 3.034), 18.33 (SD = 2.454), 16.71 (SD = 2.858) respectively. Based on Kelley’s derivation [
30], data was separated into high and low groups consisting of the top 27% and the lower 27% of extreme total score. Item discrimination between high and low groups was conducted using independent sample
t-tests.
Table 2 shows significant difference (p < 0.001) in the total score of the scale between high and low groups, with the correlation coefficient significant between 0.130 – 0.762 (p < 0.01).
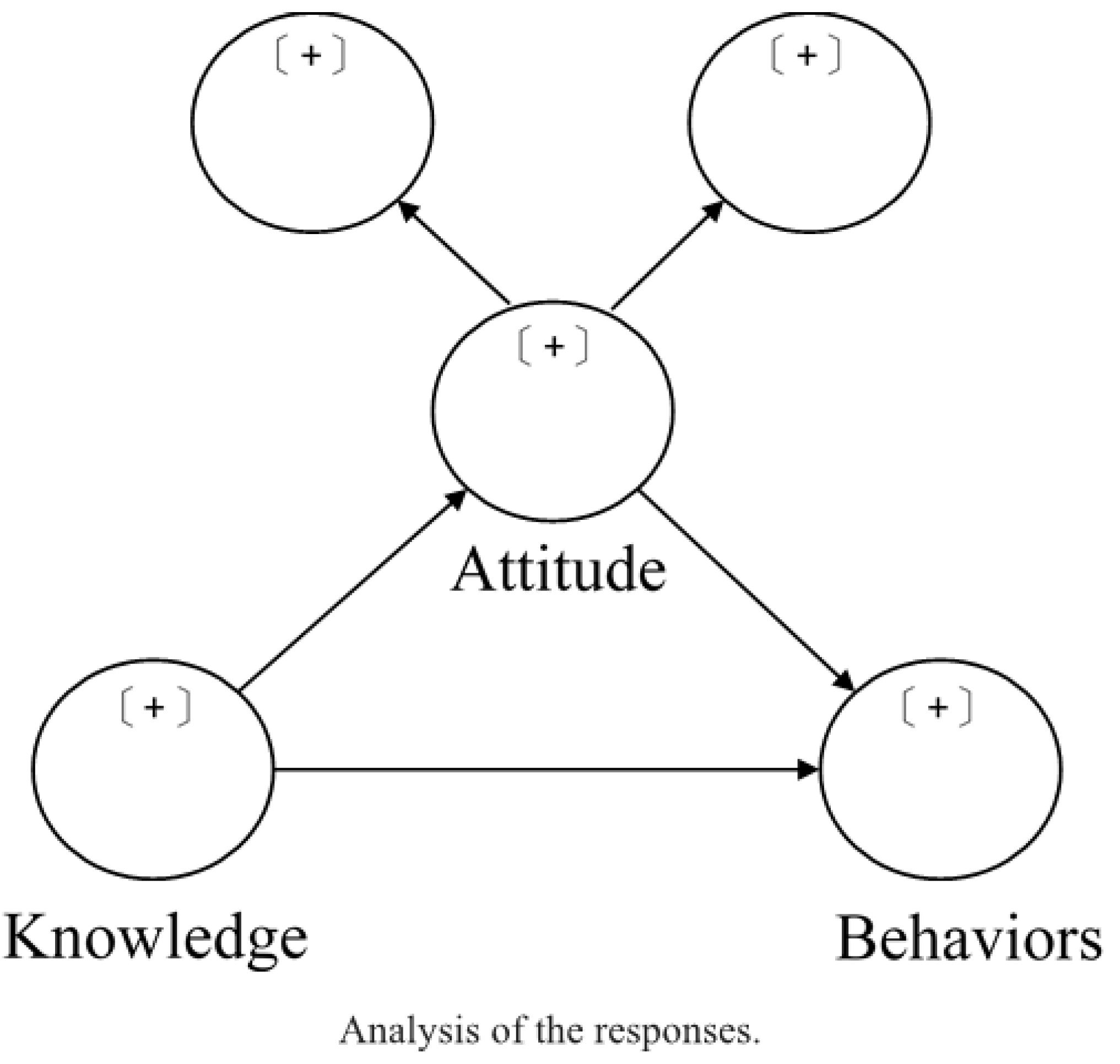
The mediation analysis used SmartPLS [
29]. The meaningful factors of the Attitude section were paying attention to bone density state (A01) and attitudes to promote bone health (A02); the Behaviors section factor was formed by five items (
Figure 3). After deleting these items, the final version of OKABQ (
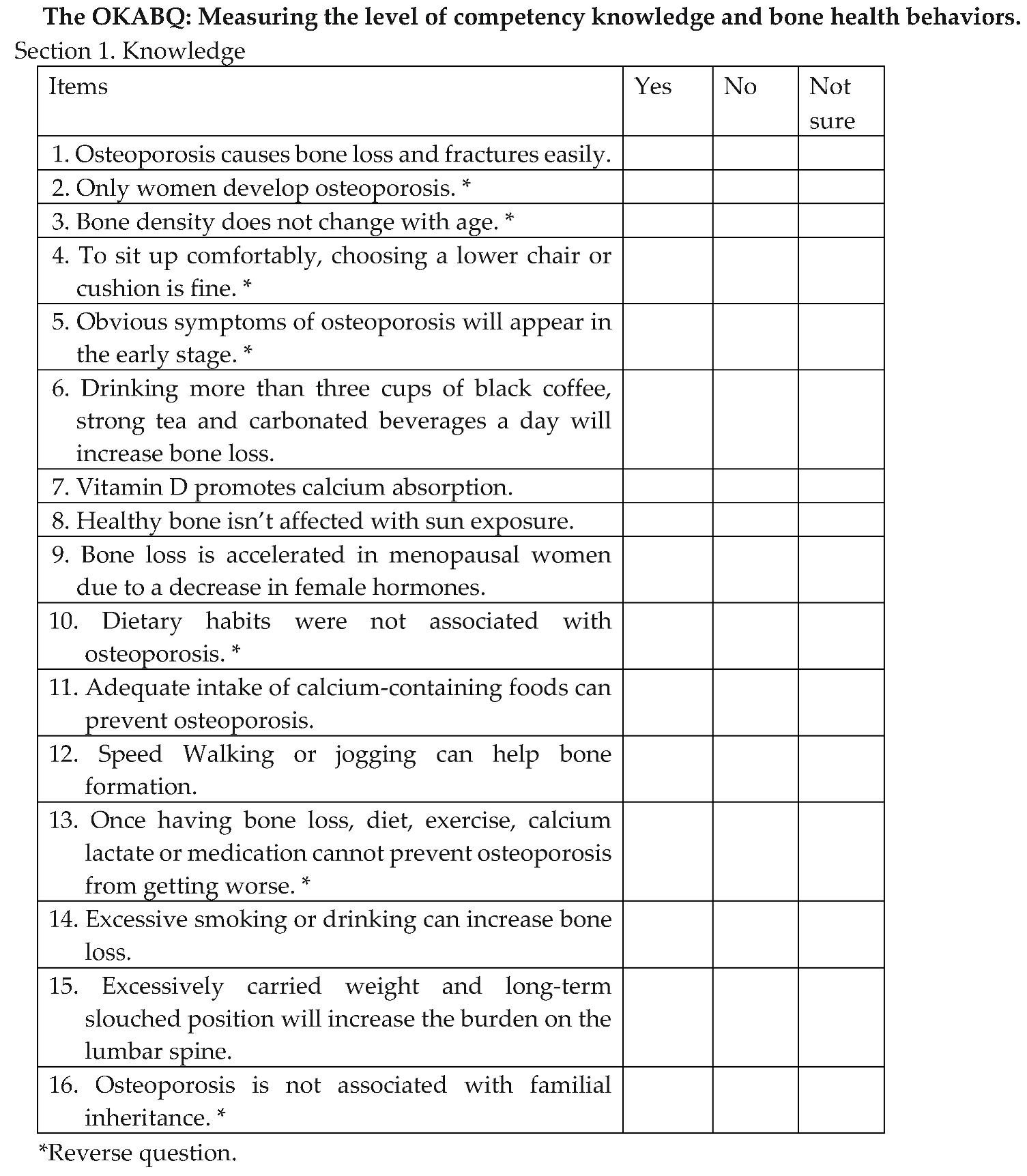
Box 1) was as follows: Knowledge (16 items) ranging from 0 to 16; Attitude (5 items) ranging from 0 to 20 and Behaviors (5 items) ranging from 0 to 20. The total score ranged from 0 to 56, with higher scores indicating higher positive bone health promotion behaviors.
Box 1. The final version of OKABQ.
3.2.2. Construct validity
Table 3 shows that Average Variance Extracted (AVE) 0.52 ~ 0.84 mean convergent validity was excellent [
23]. The Fornell-Larcker criterion of Attitude = 0.721 greater than those of Behaviors and Knowledge revealed its discriminant validity.
3.2.3. Reliability
The reliability measures with Cronbach’s α of the overall scale and the sections (Attitude and Behaviors) were 0.70, 0.71 and 0.61 respectively. The Knowledge section presented internal consistency as KR-20 coefficient was 0.78. This showed that the content validity and reliability of the overall scale were satisfactory but requires further validation with a larger study sample. In total, 28 patients completed the 30-day test-retest OKABQ for the second time, of which two were excluded for loss of contact. The mean time between test and retest was 16.3 ± 3.9 (range, 10-30) days. The intraclass correlation coefficient (ICC) showed good reliability.
The construct reliability and validity for reflective index as Attitude used the SmartPLS (
Table 3).
Table 3 illustrates Cronbach's α ranged from 0.68 to 0.82, representing a satisfactory and Composite Reliability (CR) = 0.83 ~ 0.92 mean good internal consistency reliability [
23].
3.2.4. Estimated Model
Figure 3 reveals path model results indicating A01 and A02 as reflective index. The loadings and outer weights of all items show most were significant. Although OB-05 was not significant, it was not removed because of indicator weight = -0.257 is greater than 0.02 (
Table 4) [
31]. The hypothesis formulated for the mediation model was confirmed (
Table 5). The effect sizes are represented by f
2 [
32]. Q
2 values higher than 0 represent the model has predictive relevance. The R
2 = 0.179 as weak depicted that Attitude caused 17.9% variance in Behaviors. [
33].
Table 6 presents total, indirect and direct effects for the influence of Knowledge on Behaviors. A direct effect is the pathway estimates of a construct to Behaviors. The total effect was the sum of direct and indirect effects. The results illustrate direct effect from Knowledge to Behaviors (β = 0.220, t = 2.561, p = 0.010) and indirect effect Attitudes mediates between the relationship of Knowledge and Behaviors (β = 0.114, t = 2.627, p < 0.001), as being positive and statistically significant.
4. Discussion
This study developed a new scale for measuring the Knowledge, Attitudes and Behaviors of osteoporosis patients, the OKABQ scale, which was modified from the KAP model, international guidelines and literature review. We conducted a pilot study and scale validation using physicians, experts and osteoporosis patients. The current analyses have shown moderate total scores on the OKABQ scale, substantial construct validity, and good test-retest substantiation.
The total scores showed high level where more than 35.5% of the patients reported enhanced and positive behaviors for bone health, which might be influenced by the Hawthorne effect [
34] and the undergoing of osteoporosis therapy. Clinicians should evaluate patient’s personal characteristics, preferences and unconscious judgements that affect their bone health issue. One clear indication is sample selection bias (volunteer bias) where patients willing to participate in research might possess more positive behaviors [
35,
36], so volunteers were found to be healthier than non-volunteers in some reports.
The KAP model is one of the most popular and widely used models in medical practice, determining knowledge is the base of attitude toward behaviors [
8]. Evidences indicates that education programs are effective in changing knowledge, beliefs, and practice toward osteoporosis [
37]. The Knowledge section scores moderate levels similar with these studies reporting low to moderate knowledge of osteoporosis [
38,
39,
40]. Preventing osteoporosis is positively correlated with higher education level in patients as having more opportunities to develop adequate knowledge and good attitude toward preventing osteoporosis [
41], and this illustrates that educators should consider educational level regarding enhancement of participants' understanding.
During phase II, the OKABQ had good structure and validity. The model contains formative indicator (Attitude) and reflective indicator (Behaviors). SEM is popular for indirect examination through a mediator process [
42] and PLS offers an incorporating formative and reflective measurement model [
43]. Among these, the R
2 value and the path coefficients value are the main indicators for judging the quality of the model [
33].The R
2 value was 0.163 to 0.179 and most of the path coefficients were significant. The Attitude section had two principal components: paying attention to bone density state (A01) and attitudes to promote bone health (A02). The study showed declining BMD testing reasons were high cost, misconceptions with lifestyle management sufficient to prevent osteoporosis, and poor awareness of the disease [
38]. Although it is suggested by WHO, IOF and bone health research that having a fracture risk-assessment tool such as FRAX® to detect bone loss is advantageous [
44], BMD has a reassessed recommendation that 12-24 months after starting therapy [
45] is important to understand the degree of deterioration. Promotion of bone health is about lifestyle modification for nutrition, Vitamin D, exercise, and avoiding tobacco and alcohol [
46]. The most trustworthy and reliable source of health information is the clinician, but patients often felt too rushed to obtain sufficient detailed information during visits [
47]; accordingly, regular health educators are required to provide more comprehensive osteoporosis education in clinical settings.
The intentions toward behavior are influenced by attitudes [
48] and attitude can be the boundary between knowledge and individuals’ behaviors [
49], so we planned to check prediction of behavior from attitude, but the R
2 values weakly depicted Attitude causing 17.9% variance in Behaviors. The attitude-behavior intra-research shows that attitudes and behaviors have mediator call behavioral intentions [
50].
In this study, adding behaviors intentions and merging TPB theory [
19] at the beginning of the design could increase the predictive power of attitudes on behavior. Self-efficacy has been used to establish and evaluate applications designed to improve general health [
51]. The key content of osteoporosis education will form the basis of behaviors, so this section presents formative indicators. These five items can provide significant measures as formative indicators of Behaviors (
Figure 3) as being: “having a high-calcium diet, reduction of caffeine absorption, avoiding sunbathing, overly vigorous physical activity and avoidance of falling." Formative indicators are observed variables as causes affect a latent variable [
52], meaning if any measure increases/decreases it will positively/negatively affect latent variables (but others indicators do not change).
5. Conclusions
The OKABQ demonstrates good construct validity, reliability, test-retest agreement, and perfect inter-rater agreement. Professionals could apply the OKABQ to obtain knowledge, attitude and behavior measures of osteoporosis patients thereby providing more holistic educational information. Nevertheless, with the influence of knowledge on behaviors, attitude plays a mediating effect, and professionals are reminded to understand patients' osteoporosis attitudes deeper to improve the effect of health education and case management. Patients also are required to better understand their deficiencies in these three issues concerning osteoporosis in adjusting to a more positive bone health lifestyle.
6. Limitation
There are three main limitations of the study. Firstly, longitudinal research would be more beneficial to observe changes in the knowledge, attitude and behaviors of women with osteoporosis. Secondly, further studies could involve male osteoporosis patients to evaluate the applicability of the OKABQ to both genders, and finally, the mediation model should be further tested using a larger sample size.
Author Contributions
I.-C. H.: Conceptualization, methodology, investigation, formal analysis, writing- original draft. H.-C. W.: Conceptualization, investigation. C.-L. L.: Resources. H.-H. W.: Writing - review & editing, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by a three-year grant (2018–2020) from the National Science and Technology Council of Taiwan (MOST 107-2314-B-037-018-MY3).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Kaohsiung Medical University Chung-Ho Memorial Hospital (KMUHIRB-E(I)-20180317, 16 July 2019 revised).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Acknowledgements
We thank all participating osteoporosis patients.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hernlun Development and Validation of the Osteoporosis Knowledge, Attitude, and Behaviors Questionnaire for Female Osteoporosis Patients in Taiwan: A Mediation Model d E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JAJAoo (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. 8:1-115.
- Alswat KA (2017) Gender Disparities in Osteoporosis. J Clin Med Res 9:382-387. [CrossRef]
- Jensen AL, Lomborg K, Wind G, Langdahl BJOI (2014) Effectiveness and characteristics of multifaceted osteoporosis group education—a systematic review. 25:1209-1224. [CrossRef]
- Sayed-Hassan RM, Bashour HN (2013) The reliability of the Arabic version of osteoporosis knowledge assessment tool (OKAT) and the osteoporosis health belief scale (OHBS). BMC Res Notes 6:138. [CrossRef]
- Sayed-Hassan RM, Bashour HNJBrn (2013) The reliability of the Arabic version of osteoporosis knowledge assessment tool (OKAT) and the osteoporosis health belief scale (OHBS). 6:1-7. [CrossRef]
- Kamal S, Mubeen SM, Kamal S, Mubashir SM (2021) Beliefs and knowledge of osteoporosis amongst female graduate students in Karachi, Pakistan: A cross-sectional study. JPMA The Journal of the Pakistan Medical Association 71:1910-1913. [CrossRef]
- Winzenberg TM, Oldenburg B, Frendin S, Jones GJBmd (2003) The design of a valid and reliable questionnaire to measure osteoporosis knowledge in women: the Osteoporosis Knowledge Assessment Tool (OKAT). 4:1-7. [CrossRef]
- Launiala A (2009) How much can a KAP survey tell us about people's knowledge, attitudes and practices? Some observations from medical anthropology research on malaria in pregnancy in Malawi. Anthropology Matters 11:. [CrossRef]
- Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti CJPo (2011) Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. 6:e20476. [CrossRef]
- Fish LS, Busby DMJRmift (1996) The delphi method. 469:482.
- International Osteoporosis Foundation I (2017) Osteoporosis - EPIDEMIOLOGY. https://www.iofbonehealth.org/epidemiology.
- Group W (1995) The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Social science & medicine 41:1403-1409. [CrossRef]
- International Osteoporosis Foundation I (2018) PATHOPHYSIOLOGY: BIOLOGICAL CAUSES OF OSTEOPOROSIS. https://www.iofbonehealth.org/pathophysiology-biological-causes-osteoporosis.
- International Osteoporosis Foundation I (2017) Osteoporosis -WHO'S AT RISK? https://www.iofbonehealth.org/whos-risk.
- World Health Organization W (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992].
- Hsu Y-H (2006) Factors Influencing Osteoporosis Prevention Knowledge and Behaviors Among Secondary Osteoporosis High Risk Population. 護理學研究所. Taipai Mediacal University, Taipei, p 153.
- Taiwan Osteoporosis Association T (2021) 2021 Consensus and Guidelines on Prevention and Treatment of Adult Osteoporosis in Taiwan. Taiwan Osteoporosis Association.
- International Osteoporosis Foundation I (2022) RISK FACTORS. https://www.osteoporosis.foundation/patients/about-osteoporosis/risk-factors.
- Ajzen I (1991) The theory of planned behavior. Organizational behavior and human decision processes 50:179-211. [CrossRef]
- Anthoine E, Moret L, Regnault A, Sébille V, Hardouin J-BJH, outcomes qol (2014) Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. 12:1-10. [CrossRef]
- Preacher KJ, Coffman DL (2006) Computing power and minimum sample size for RMSEA.
- MacCallum RC, Browne MW, Sugawara HMJPm (1996) Power analysis and determination of sample size for covariance structure modeling. 1:130. [CrossRef]
- Urbach N, Ahlemann F (2010) Structural equation modeling in information systems research using partial least squares. Journal of Information Technology Theory and Application (JITTA) 11:2.
- Polit DF, Beck CT (2006) The content validity index: Are you sure you know what's being reported? critique and recommendations. Research in Nursing & Health 29:489-497. [CrossRef]
- Wong WK, Dean S, Nair S (2018) Comparison between endoscopic and external dacryocystorhinostomy by using the Lacrimal Symptom Questionnaire: A pilot study. American journal of rhinology & allergy 32:46. [CrossRef]
- Ullman JBJJopa (2006) Structural equation modeling: Reviewing the basics and moving forward. 87:35-50.
- Farooq RJJoAiMR (2016) Role of structural equation modeling in scale development. [CrossRef]
- Hallgren KAJTiqmfp (2012) Computing inter-rater reliability for observational data: an overview and tutorial. 8:23. [CrossRef]
- Ringle CM, Wende S, Becker J-M (2015) SmartPLS 3. Boenningstedt: SmartPLS GmbH 584:.
- Kelley TL (1939) The selection of upper and lower groups for the validation of test items. Journal of educational psychology 30:17. [CrossRef]
- Abdulameer SA, Syed Sulaiman SA, Hassali MA, Subramaniam K, Sahib MN (2013) Psychometric properties of Osteoporosis Knowledge Tool and self-management behaviours among Malaysian type 2 diabetic patients. Journal of community health 38:95-105. [CrossRef]
- Cohen J (2013) Statistical power analysis for the behavioral sciences. Routledge.
- Chin WW (1998) The partial least squares approach to structural equation modeling. Modern methods for business research 295:295-336.
- Sedgwick P, Greenwood N (2015) Understanding the Hawthorne effect. Bmj 351:. [CrossRef]
- Dodge HH, Katsumata Y, Zhu J, Mattek N, Bowman M, Gregor M, Wild K, Kaye JA (2014) Characteristics associated with willingness to participate in a randomized controlled behavioral clinical trial using home-based personal computers and a webcam. Trials 15:508. [CrossRef]
- de Souto Barreto P, Ferrandez A-M, Saliba-Serre B (2013) Are older adults who volunteer to participate in an exercise study fitter and healthier than nonvolunteers? The participation bias of the study population. Journal of Physical Activity and Health 10:359-367. [CrossRef]
- Chan CY, Subramaniam S, Chin K-Y, Ima-Nirwana S, Muhammad N, Fairus A, Ng PY, Aini JN, Aziz NA, Mohamed N (2022) Effect of a screening and education Programme on knowledge, beliefs, and practices regarding osteoporosis among Malaysians. International Journal of Environmental Research and Public Health 19:6072. [CrossRef]
- Lulla D, Teo CW, Shen X, Loi ZBJ, Quek KW, Lis HLA, Koh SA, Chan ET, Lim SWC, Low LL (2021) Assessing the knowledge, attitude and practice of osteoporosis among Singaporean women aged 65 years and above at two SingHealth polyclinics. Singapore Med J 62:190-194. [CrossRef]
- Oba S, Kajiyama N (2022) Knowledge of Osteoporosis and Its Associated Factors among Public Health Professionals in a Municipal Office in Japan. Healthcare. MDPI, p 681. [CrossRef]
- Chelf S, Davis RE, Bass MA, Ford MA, Firouzabadi AD, Leo JT, Nahar VK (2022) Osteoporosis knowledge and health beliefs among middle-aged men and women in the Southern United States. Journal of Osteopathic Medicine. [CrossRef]
- Puttapitakpong P, Chaikittisilpa S, Panyakhamlerd K, Nimnuan C, Jaisamrarn U, N. T (2014) Puttapitakpong_Inter-correlation of knowledge, attitude, and osteoporosis preventive behaviors. BMC Women's Health 14:1-4. [CrossRef]
- Iacobucci D (2010) Structural equations modeling: Fit indices, sample size, and advanced topics. Journal of consumer psychology 20:90-98. [CrossRef]
- Abdulameer SA, Syed Sulaiman SA, Hassali MA, Sahib MN, Subramaniam K (2014) Psychometric properties of the Malay version of the Osteoporosis Health Belief Scale (OHBS-M) among Type 2 diabetic patients. International journal of rheumatic diseases 17:93-105. [CrossRef]
- Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. The Lancet 359:1929-1936. [CrossRef]
- The National Osteoporosis Guideline Group N (2021) CLINICAL GUIDELINE FOR THE PREVENTION AND TREATMENT OF OSTEOPOROSIS. https://www.nogg.org.uk/full-guideline.
- Jones G, Winzenberg TM, Callisaya ML, Laslett LL (2014) Lifestyle modifications to improve musculoskeletal and bone health and reduce disability–A life-course approach. Best Practice & Research Clinical Rheumatology 28:461-478. [CrossRef]
- Noel SE, Arevalo SP, Mena NZ, Mangano K, Velez M, Dawson-Hughes B, Tucker KL (2019) Knowledge, attitudes, beliefs, and health behaviors of bone health among Caribbean Hispanic/Latino adults. Archives of osteoporosis 14:1-17. [CrossRef]
- Ajzen I (2001) Nature and operation of attitudes. Annual review of psychology 52:27-58. [CrossRef]
- Abdolalipour S, Mirghafourvand M (2021) Effect of Education on Preventive Behaviors of Osteoporosis in Adolescents: A Systematic Review and Meta-Analysis. International Quarterly of Community Health Education 41:325-347. [CrossRef]
- KIM M-S, HUNTER JE (1993) Relationships Among Attitudes, Behavioral Intentions, and Behavior:A Meta-Analysis of Past Research, Part 2. Communication Research 20:331-364. [CrossRef]
- Bandura A, Wessels S (1994) Self-efficacy. na.
- Diamantopoulos A, Winklhofer HM (2001) Index construction with formative indicators: An alternative to scale development. Journal of marketing research 38:269-277. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).