1. Introduction
The COVID-19 pandemic has had a widespread and significant impact on society, including the loss of lives and livelihoods. It has also caused significant disruptions to the education of students globally, with schools, colleges, and universities being closed or transitioning to online learning in 192 countries, affecting almost 100% of the world's student population (Tabatabai, 2017). The pandemic's long-term economic and social effects on the educational system are undetermined. Schools worldwide have adopted online classes (Raman et al., 2021) through innovative technology and the internet's universality. Digital technology has transformed the high school and tertiary school lab experimentation, enabling e-learning through virtual reality, virtual worlds, dynamics-based virtual systems, and virtual laboratories. Combining digital and classroom resources with virtual labs has provided an inclusive educational experience that allows better retention of theoretical aspects and the development of practical skills (Raman et al., 2022).
The pandemic has also overwhelmed healthcare systems and the medical industry, leading to a lack of preparedness and response that has impacted health, education, and the economy, including efforts toward achieving the Sustainable Development Goals (SDG). Research has revealed that the SDGs are untackled, and countries must incorporate virtual learning environments into higher education curricula globally to achieve SDG, especially SDG4 (Quality Education) (Raman et al., 2022). The demand for technology-driven educational initiatives in medicine, including simulation-based teaching platforms, has increased in response to the COVID-19 pandemic. These platforms can accurately simulate different diseases and facilitate real-time clinical teaching and evaluation, helping with the formative assessment of students.
Simulation-based teaching platforms can improve clinical results, save time, and deliver electronic-based content through computers or mobile devices. They can also facilitate distance learning through video conferences and review clinical decisions with learners (Nestel & Bearman, 2014; Rosen, 2008). Clinical educators can use these platforms to conduct online case-based high-impact simulation training programs and run live, virtual OSCE (Objective Structured Clinical Exam) sessions (McGaghie et al., 2010). Virtual OSCE based on simulation can also provide a cloud-based platform for guiding standardized patients in a virtual environment with video capabilities (Nedungadi & Raman, 2016). This can help promote the core learning for clinical decision-making in the distance learning platform and the emerging demand for transforming clinical practice into telemedicine (Fioccola et al., 2016). The use of simulation training, including Virtual Patient simulation, has been increasing in popularity as technologies to support complex procedures become more widespread (Rossi et al., 2018). Virtual learning tools and remote learning have reshaped the conventional learning environments in medicine and brought knowledge to students who would otherwise be excluded (Al-Elq, 2010). Customized digital environments, such as simulation labs for high school experiments, virtual labs for engineering education, and multilingual interactive learning platforms for village-based education, have been successfully implemented (Nedungadi et al., 2019). Personalized health monitoring systems for community health workers have also been developed and deployed at scale (Nedungadi, Jayakumar, & Raman, 2018).
The pandemic has significantly impacted the education system of clinical instructors and students of health majors (Ahmed et al., 2020; Julio et al., 2022). However, there is limited research on the authenticity and reliability of Virtual Patient simulation training (Themistocklakis et al., 2014). There is a lack of data on how students perceived this method during the COVID-19 pandemic. During the first wave of the pandemic, medical students could not attend their regular clinical postings due to lockdowns and restrictions on in-person learning. This presented a challenge for faculty at medical colleges, who had to shift classes and clinical postings online using digital platforms like Google Meet and Microsoft Teams.
Simulation-Based Medical Education (SBME), which uses Virtual Patients, is a cost-effective alternative to mannequin-based simulations, which are usually very expensive (Williams 2020). A systematic review by Cook et al. observed that Virtual Patients were associated with better learning outcomes when compared to no intervention (Cook et al., 2010). They also offer the added benefit of ensuring the safety of patients and students through online or remote learning. SBME is a scalable option, as it can be easily accessed by increasing numbers of learners with the availability of cloud hosting and digital devices. SBME is superior to traditional instructional approaches, particularly in developing professional skills and improving patient safety (Watari et al., 2020). It allows trainees to learn from their failures in a controlled environment, helping them to avoid making the same mistakes in the real world (Wang et al., 2021). Studies have shown that SBME is an effective learning method for medical students, with age and gender distributions comparable to previous research (Nisar et al., 2021; Wang et al., 2021). The primary goal of these studies was to determine the effectiveness of SBME as a learning pedagogy for medical students. Proper education and hands-on practice are important for reducing medical errors and improving hospital patient safety. Using learners' errors as feedback can help identify gaps in knowledge and skill (D'Angelo & Kchir, 2021). However, it is also important for learners to have the opportunity to practice and train in a suitable environment to overcome such errors (Woodham et al., 2019). Incorporating error and stress-related components into learning can help learners develop stress management skills, alternative strategies, and plans (French, 2020). Simulations using Virtual Patients allow learners to make mistakes safely, improve awareness of medical errors, and reduce their occurrence while diagnosing a patient (Woodham et al., 2019). These activities can be particularly useful in a healthcare setting, where the consequences of errors can be serious. The focus of the study by Juan et al. (2022) was to analyze how clinical reasoning behaviors relate to diagnostic efficiency while working with Virtual Patients.
SBME can potentially impact the achievement of the Sustainable Development Goals (SDG). The Sustainable Development Goals (SDG) are a set of global goals adopted by the United Nations in 2015 to end poverty, protect the planet, and ensure peace and prosperity for all. The SDGs address various health, education, and economic development issues. Research on the impact of COVID-19 on sustainable development, particularly on health and well-being, has increased in countries such as India (Raman, Vinuesa, & Nedungadi, 2021). SBME can contribute specifically to SDG 3, which aims to ensure healthy lives and promote well-being for all ages, by enabling medical students to learn about patient care and medical procedures in a safe and controlled environment. Virtual Patients can be a valuable tool in medical education, contributing to SDG 4 (Quality Education) and providing students with an interactive and engaging learning experience. This can help improve the quality of medical education and prepare students to provide high-quality patient care.
The primary objective of this study was to examine the feasibility of learning clinical skills through MedSIM, a simulation-based teaching platform with Virtual Patients. and to understand how the perception of learning with this module changed during the COVID-19 pandemic. This involved surveying students on their experiences with MedSIM, collecting data on their performance on clinical skills assessments, and comparing the results to traditional methods of teaching clinical skills. The study also analyzed student feedback on using the MedSIM, including any challenges or benefits they experienced during the pandemic. This information could help educators understand the effectiveness of MedSIM as a tool for teaching clinical skills, how it compares to other methods, and how students perceived it during the pandemic.
Our paper is organized as follows. We start with an overview of the MedSIM platform and its modules. This is followed by the Methods section, which describes the sample, data collection, and analysis methods. The results and discussion section analyzes the survey results, followed by conclusions.
About MedSIM
MedSIM is a simulation-based teaching platform with Virtual Patients designed to supplement conventional teaching practices cost-effectively and promote the quality of medical education. It allows students to learn at their own pace without the fear of committing medical errors. The Virtual Patient simulator is a cutting-edge e-learning innovation for medical and other health professionals, consisting of a framework that supports various Virtual Patient cases developed by interdisciplinary medical teams. Each Virtual Patient case follows the critical path for a specific patient in a hospital setting, allowing students to learn about patient care and medical procedures in a simulated environment. Virtual Patients are a useful tool in medical education, as they can provide students with an opportunity to practice and hone their diagnostic and treatment skills in a simulated environment. Virtual Patients can also teach students about rare or unusual medical conditions and expose them to various clinical scenarios they may not encounter in their clinical rotations. MedSIM can be a useful tool for teaching clinical skills and promoting the quality of medical education. It can also provide a cost-effective supplement to traditional teaching methods, allowing students to learn at their own pace and providing a safe and controlled environment for learning.
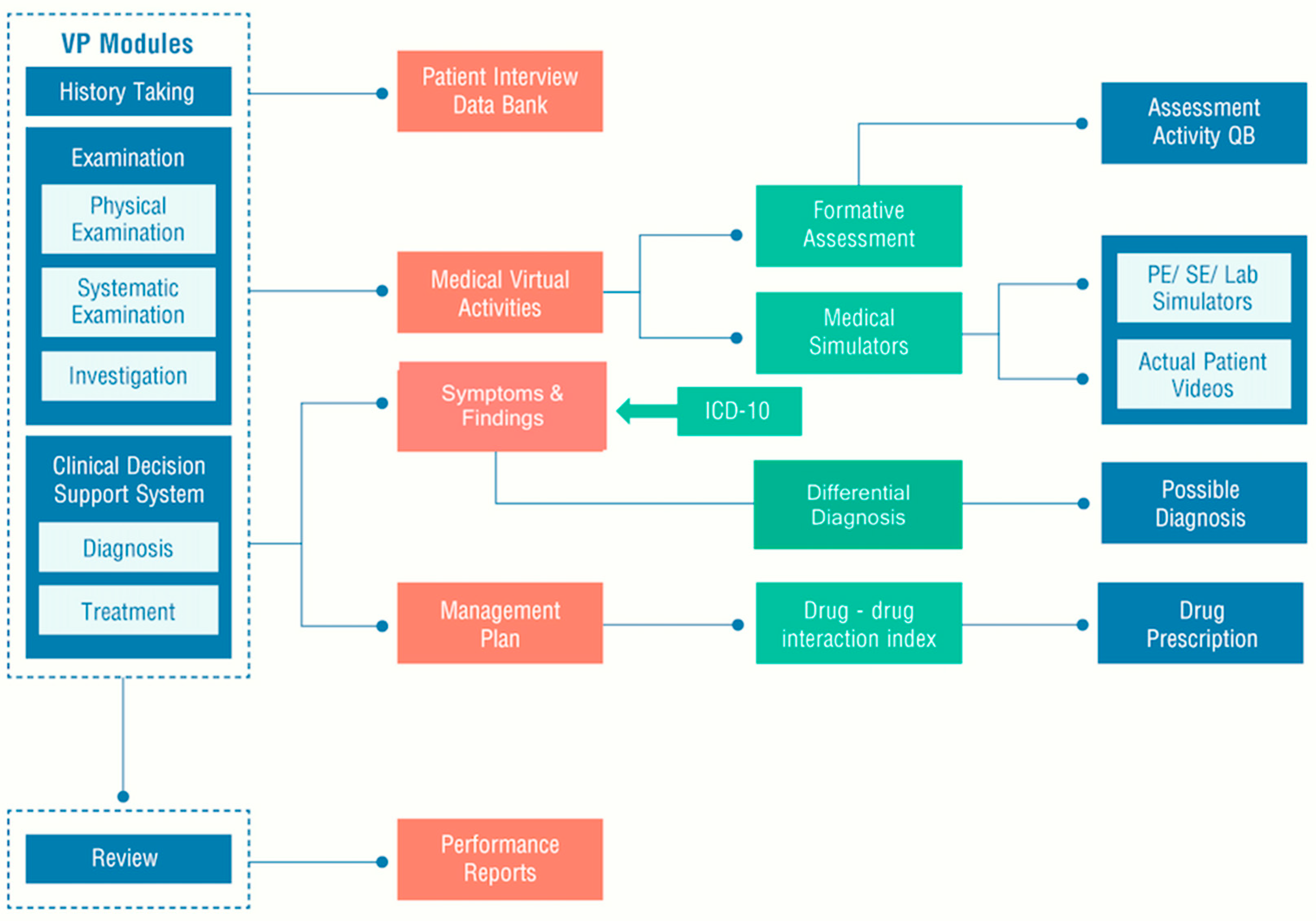
MedSIM consists of seven modules, including a Medical Learning Management System (MLMS) and portal with Virtual Patients, assessment, and reporting tools (
Figure 1). The Virtual Patients are enhanced with interactive simulations and animations to provide a more immersive and interactive learning experience. The MLMS and portal allow students to access Virtual Patients and track their progress through assessments and reporting tools. With their interactive simulations and animations, the Virtual Patients allow students to experience realistic patient scenarios and practice their clinical skills in a simulated environment.
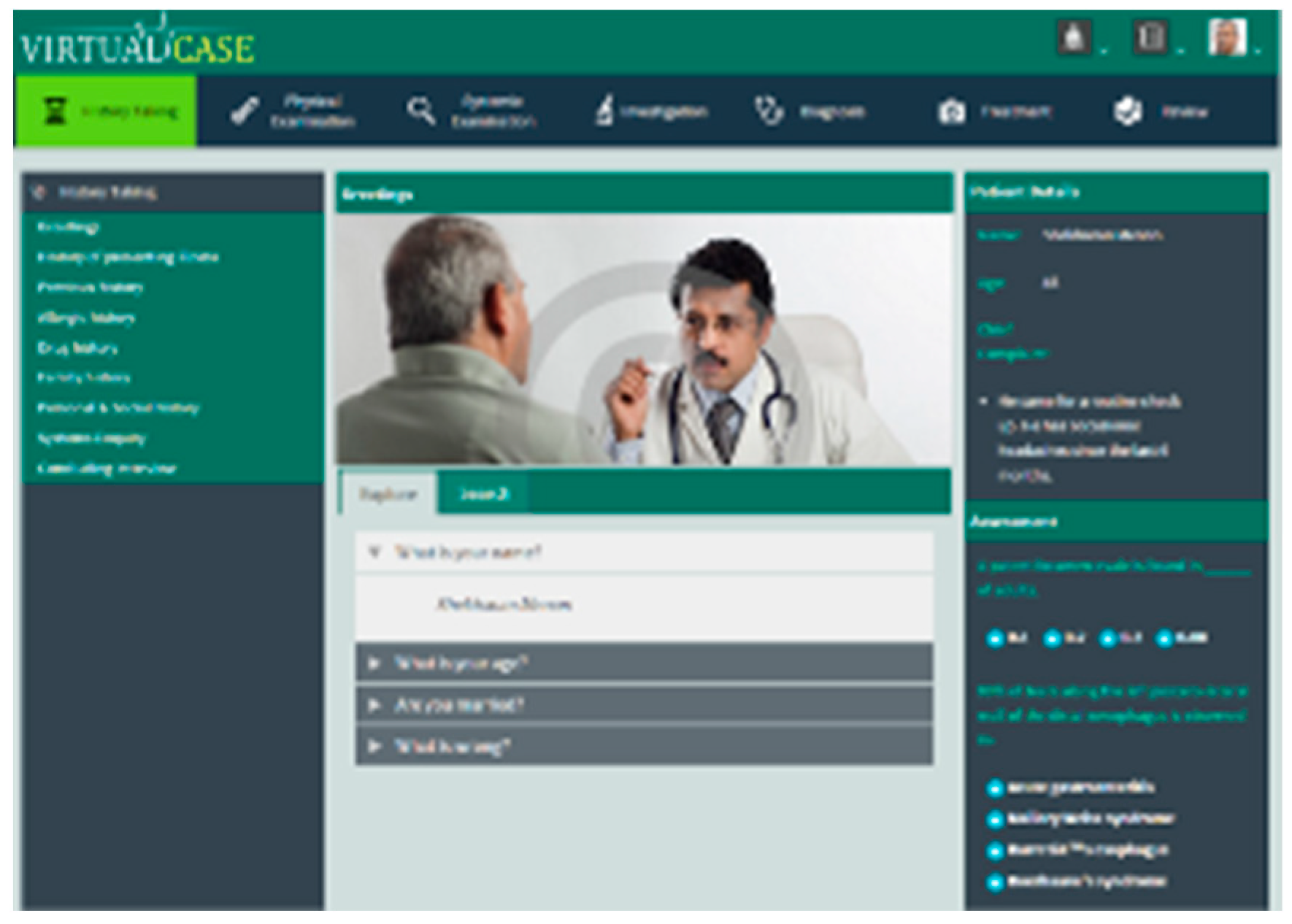
In MedSIM, students are presented with cases similar to patients coming to the hospital presenting different disease conditions and when a student selects a patient. The student can then proceed with the chosen clinical scenario or return to the complete patient list to view another Virtual Patient scenario. Once a clinical case is chosen, the student can interview the patient by selecting appropriate history-taking questions from a list provided on the portal. They can then move on to the examination modules, including the General Physical Examination and the Systemic Examination.
The simulation provided by MedSIM is divided into four main sections:
1. Identification of the symptoms of the disease through activities such as history taking, physical examination, systemic examination, and lab investigation.
2. Differential diagnosis of the disease based on the identified signs and symptoms.
3. Treatment of the disease selected by the learner.
4. Evaluation of the learner through a performance report.
In the history Taking module, the students can access nine subsections that allow them to question the patient in a structured manner to gain insight into the patient's complaints, previous medical and surgical information, any relevant family problems, personal and environmental issues, etc. (
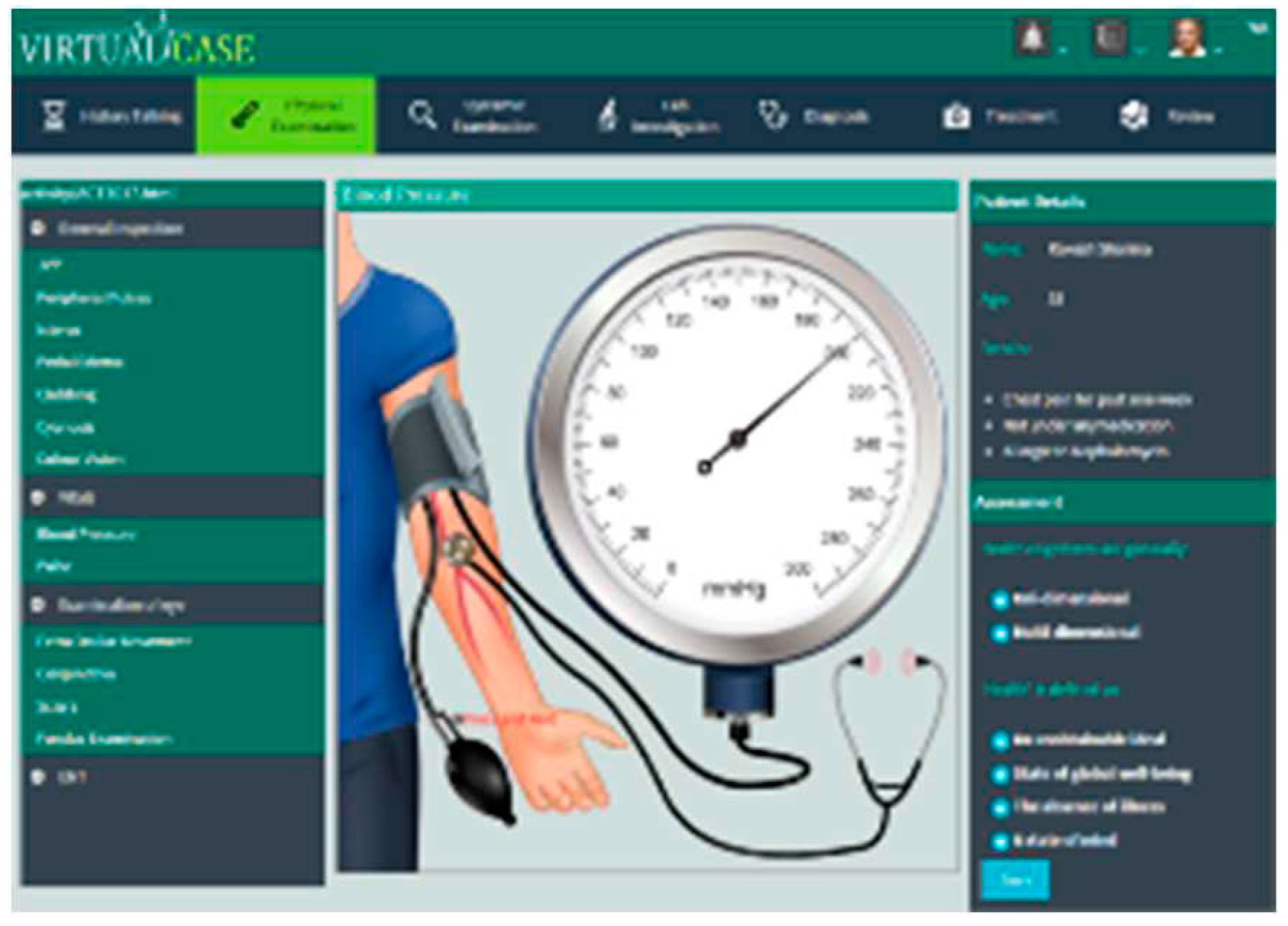
Figure 2). The Physical Examination module allows the student to examine the patient by navigating through four main sections, each consisting of related sub-sections that would enable the student to explore the vital signs and form an idea of the general physical status of the patient (
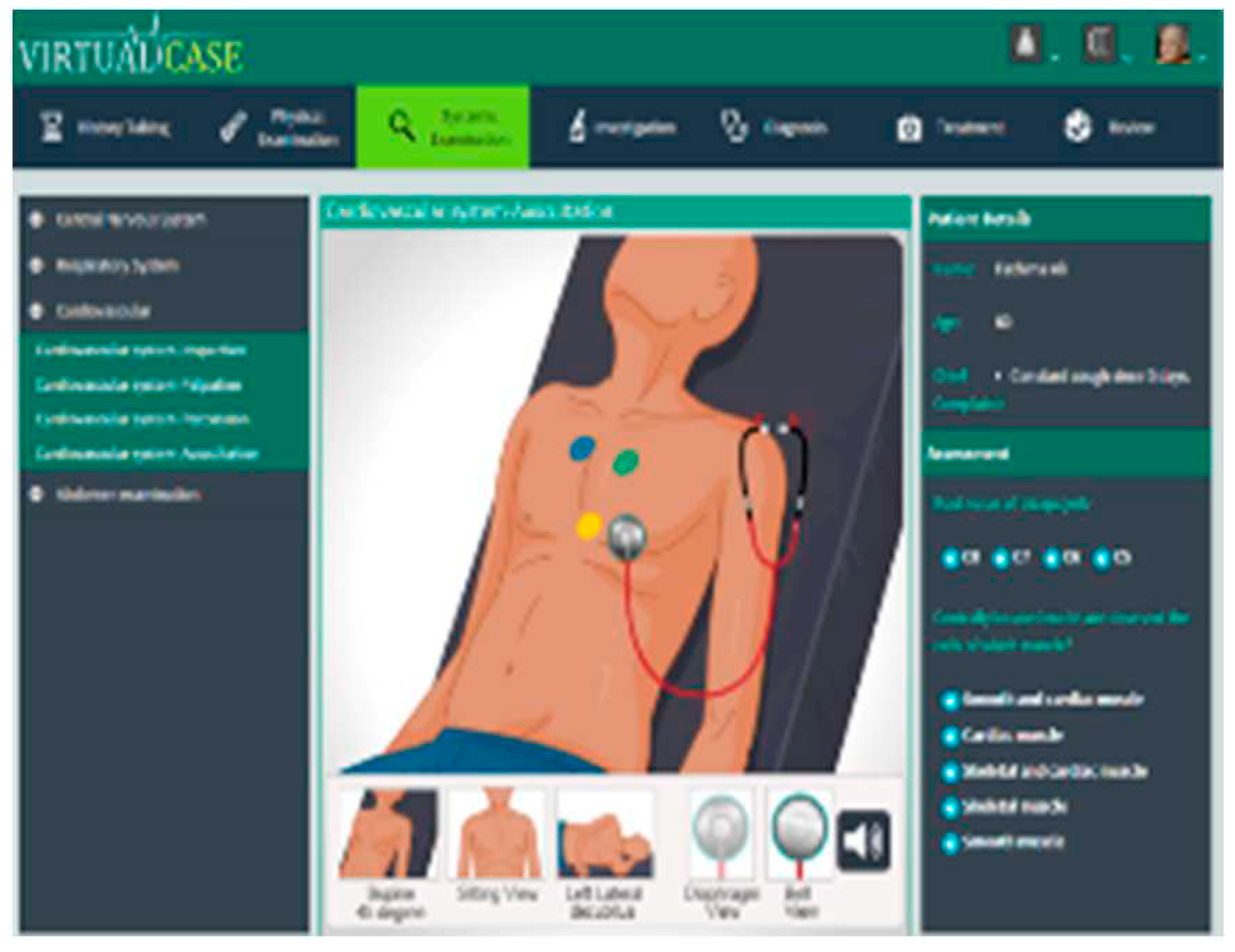
Figure 3). The Systemic Examination is one of the main determinants for diagnosing a patient's condition. After interviewing a patient, the student is expected to conduct a physical exam using four techniques: inspection, palpation, percussion, and auscultation. These findings must be integrated with the history findings and laboratory investigations to correctly arrive at the patient's diagnosis (
Figure 4). In the Investigation module, routine blood tests, urine exams, and specific investigations such as radiography, electrocardiogram, treadmill test, echocardiography, etc., are available for each virtual patient. These help narrow down the patient's possible diagnosis (
Figure 5).
Under the Differential Diagnosis module, a list of suspected diseases is displayed, from which the student identifies the most probable illness based on his previous interaction with the patient. If a condition is not included in differential diagnosis, it is not likely to be diagnosed. It is essential to include uncommon as well as common diseases in the differential diagnoses (
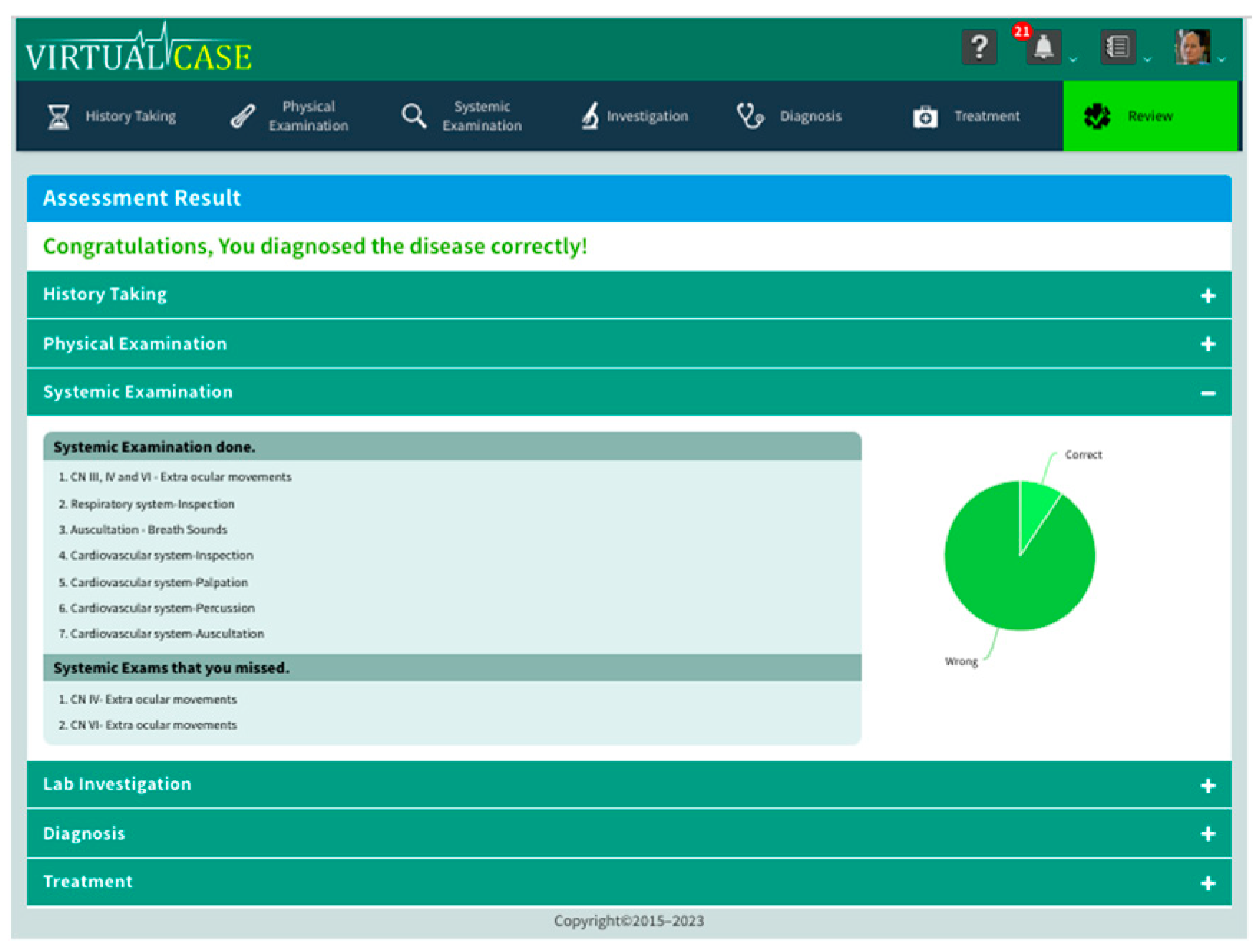
Figure 6). In the Treatment module, after confirming their diagnosis and ensuring they have not missed any valuable decision-making questions, examinations, or investigations in the previous modules, the student can move on to the Treatment module to manage the patient with appropriate therapeutic options. Finally, the Review section (
Figure 7) displays the student's performance and areas where improvement is needed in each module, allowing them to learn from their mistakes and perform better in case-taking, examining, and therapy.
These different modules expose the students to various aspects of patient care, including symptom identification, diagnosis, treatment, and evaluation. The simulation provides a realistic and interactive learning experience that allows students to apply their knowledge and skills in a simulated environment. This can help them develop their clinical skills and prepare them for real-world patient care situations.
The seven modules of MedSIM capture every aspect of the patient's clinical course, including history taking, physical examination, systemic examination, lab investigations, differential diagnosis, treatment, and review. Each module is further divided into detailed examination procedures with corresponding questions. Students are required to select only the relevant questions based on the case presented. The system logs the selected questions and marks them as relevant or irrelevant for future reference and review of the student's diagnosis. When the student starts the simulation, a timer is activated, which tracks the time to diagnose the disease. This time is displayed in the application title bar. This comprehensive approach allows students to practice a wide range of clinical skills and provides a realistic and interactive learning experience.
2. Methods
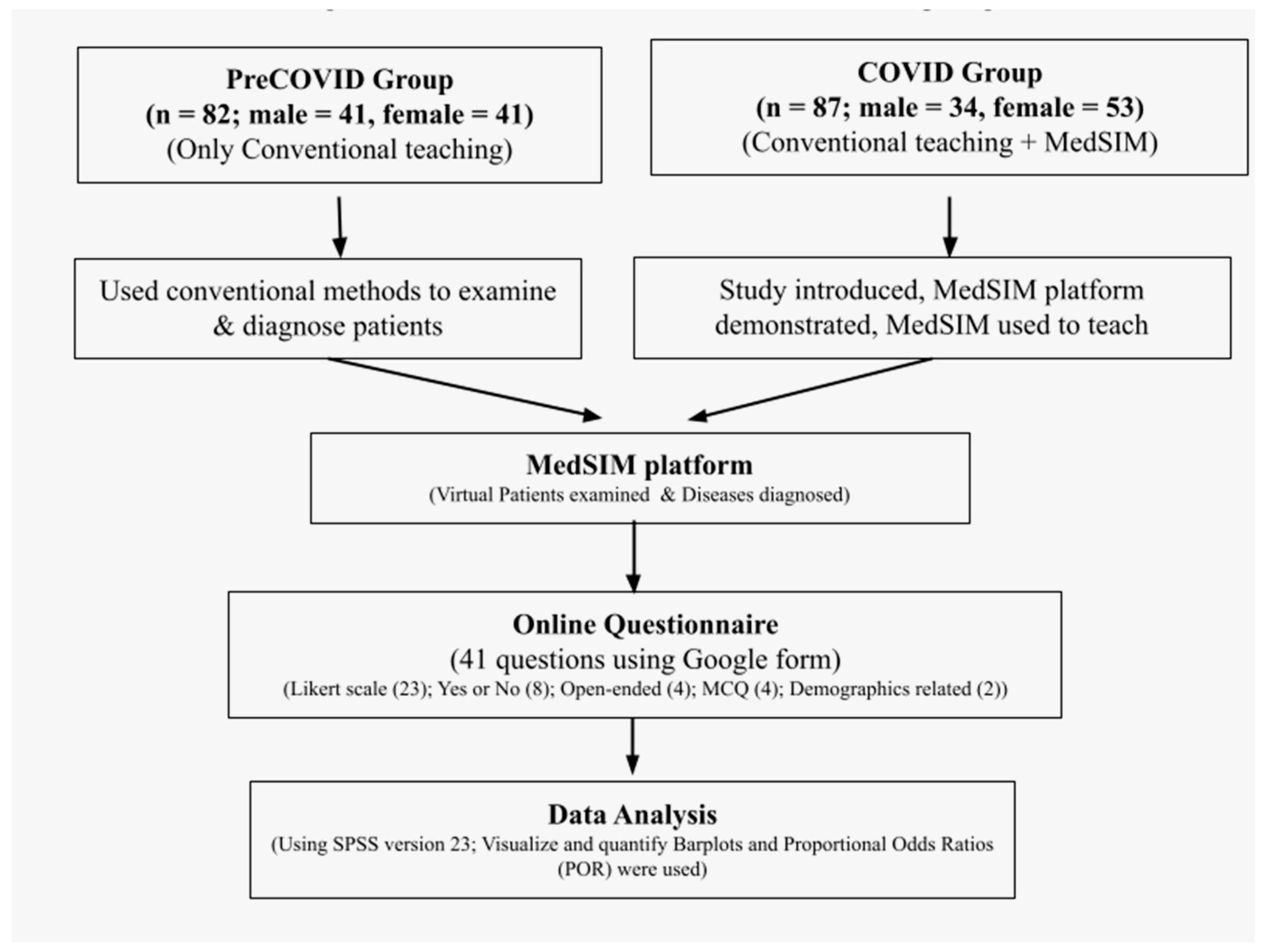
The study was a cross-sectional questionnaire-based study conducted at a tertiary care medical college and hospital in Kerala, India, for two years from 2020-2021 during the COVID-19 pandemic. The students (n = 169) were pursuing undergraduate 2
nd-year medical education. The study included two groups of students: the PreCOVID learning group (n = 82), who underwent conventional teaching methods before the pandemic, and the COVID learning group (n = 87), which received conventional teaching methods and further training on the MedSIM platform for clinical skills during the COVID pandemic (
Figure 8). The flexibility of MedSIM allowed students to use it on various platforms. However, the students included in the initial study used it mainly on their mobile phones.
The questionnaire consisted of 41 questions, including Likert scale questions (23), Yes or No questions (8), open-ended questions (4), MCQ (4), and demographics questions (2) about the students. The Likert scale questions asked students to rate their perception of the MedSIM simulation on a scale of five responses, from "strongly disagree" to "strongly agree." The questionnaire also asked about the students' existing teaching-learning infrastructure and areas for improvement. To measure the internal reliability of the questionnaire, Cronbach's alpha coefficient was calculated. The questionnaire was completed by 12 medical students giving a Cronbach's alpha value ranging from 0.68 to 0.79, considered adequate (Cronbach, L. J. (1951).
The PreCOVID group was given one hour to examine and diagnose their patients using conventional methods. They had fixed timetables for clinical classes, which included clinical case presentations for one hour on average. A similar pattern was followed in the COVID group, where the students had fixed timetables for theory and practical classes. Students in the COVID group taught with the help of MedSIM were also given one-hour sessions on average for Clinical case presentation. Medical simulations were designed to be user-friendly and easy to use. The program was tailored to hold the students' interest and make them aware of the different potentials and possibilities of MedSIM.
The study was divided into two sessions. The first session included a brief introduction to the MedSIM platform and the study objectives, followed by a demonstration of more than sixty skills developed for the platform. The amount of clinical and theory topics covered for the students in the PreCOVID group and the COVID group before the introduction of MedSIM is the same. The background clinical knowledge of the students among both groups can be considered equal. With the introduction of MedSIM, the two approaches to clinical education were compared.
The PreCOVID group continued the conventional method of bedside teaching, where they were taught selected clinical cases and were given an hour to examine and diagnose their patients. The COVID group, on the other hand, was introduced to Virtual Patients in the MedSIM platform who had symptoms, signs, and clinical findings similar to the commonly seen diseases in the outpatient clinic of various departments. A preset of ten Virtual Patients with different diseases was configured in the MedSIM platform (
Table 1). The students in the COVID group were taught these selected clinical cases. They were also given an hour to examine the Virtual Patients via the MedSIM modules and arrive at a diagnosis. The session allowed each student to get familiar with examining a Virtual Patient's case, from history taking to physical examination and then referring the Virtual patient to the laboratory for further investigations. Finally, the students could diagnose their Virtual Patients and treat their disease conditions.
We collected data using an online Google form. The data was collected as part of a Virtual Patient simulation training exercise, and the students participated voluntarily and anonymously. The data was analyzed using SPSS version 23, and bar plots and proportional odds ratios (POR) were used to visualize and quantify the differences in the ratings from PreCOVID to COVID.
It is important to ensure that research involving human subjects is conducted ethically and by the principles outlined in the Declaration of Helsinki. In this study, the Ethics Committee of the University Hospital did not conduct a review due to the anonymous nature of the study, the lack of personal information being made available, the voluntary participation of the study students, and the fact that the MedSIM platform is widely used and considered safe.
3. Results and Discussion
The study showed that the MedSIM platform was effective in helping students in the COVID group learn how to manage infrequently occurring medical conditions, with 79.3% "Strongly agreeing" or "Agreeing" with this statement. A similar percentage (77.0%) "Strongly agreed" or "Agreed" that the platform accelerated their progress in learning curves for skills development. Furthermore, 71.3% of the COVID group students felt that the platform enabled them to perform procedures on patients in a way similar to real clinical environments and showed cues and consequences similar to those found in natural clinical environments.
The COVID group students also reported that the MedSIM platform enhanced their skills in various aspects of medical practice, such as physical assessment (74.4%), psychosocial assessment (70.1%), problem-solving and decision-making (78.2%), developing a plan of action (75.9%), applying psychosocial interventions (74.7%), documenting information (76.7%), understanding the basis for interventions (78.2%), working with diverse populations or groups (75.6%), and developing their role within the profession (75.9%). Over 50% of students in the PreCOVID and COVID groups "Agreed" that MedSIM had benefited them in all these areas.
3.1. Online performance, control, and degree of simulation
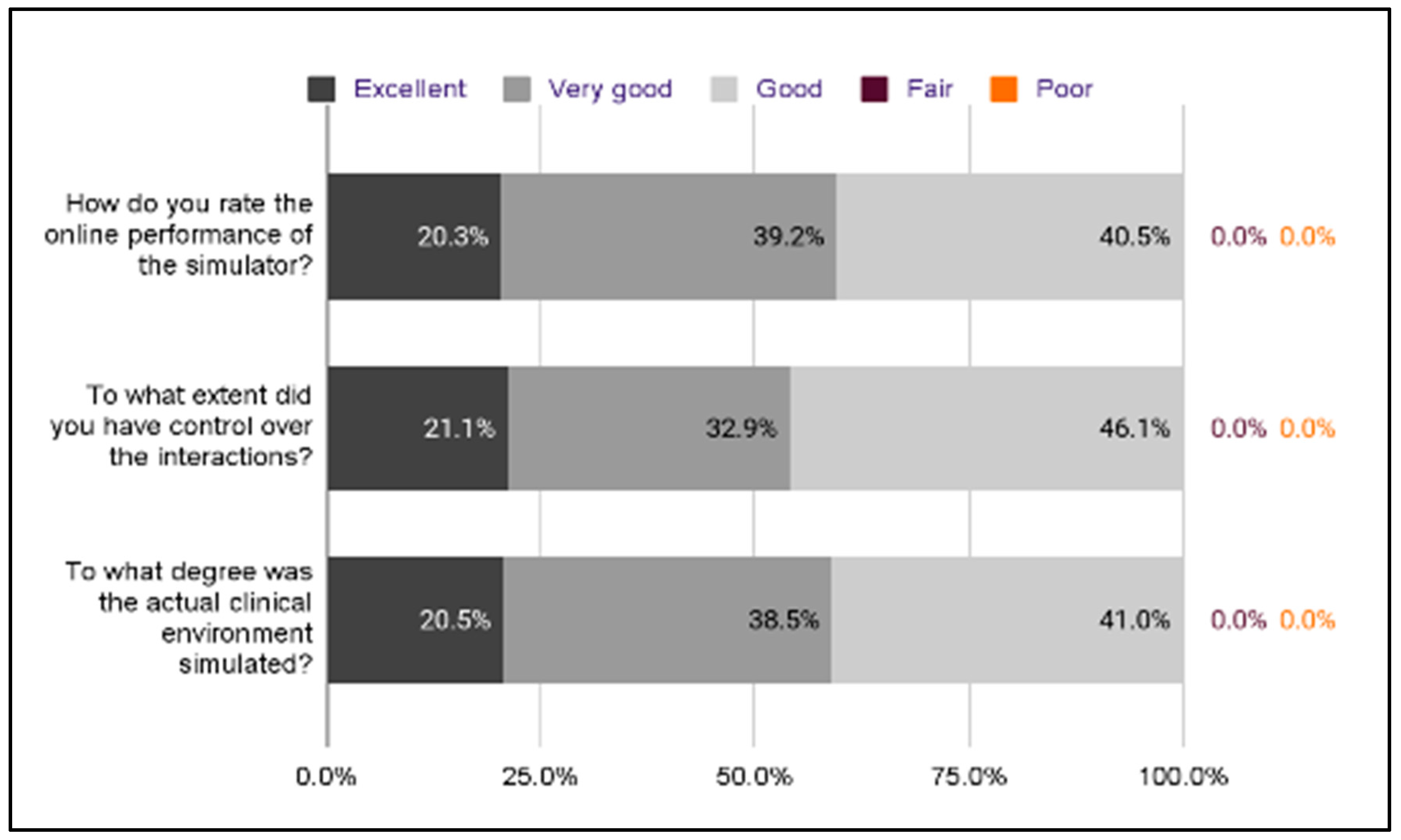
As seen in
Figure 9, students from both the PreCOVID and COVID groups rated the online performance of the MedSIM simulator as "Very good." 13 students from the PreCOVID group (18.8%) and 16 students from the COVID group (20.3%) rated the performance as "Excellent. The remaining students rated the performance as "Good" (PreCOVID 36.2%, COVID 40.5%). The COVID group also reported "Excellent" control (21.1%), "Very good" control (32.9%), and "Good" control (46.1%) over their interactions with the MedSIM simulator. 41% of the COVID group agreed that the simulated clinical environment provided by the software was "Good," 38.5% felt it was "Very good," and 21% agreed it was "Excellent."
According to the study results, as shown in
Table 2, both the PreCOVID and COVID groups had a high percentage of students who "Agreed" or "Strongly agreed" that the MedSIM platform helped them learn how to manage infrequently occurring medical conditions, with 79.3% of the COVID group and 71.3% of the PreCOVID group expressing this opinion. Similarly, a high percentage of both groups also "Agreed" or "Strongly agreed" that the platform accelerated their progress in learning curves for skills development, with 77.0% of the COVID group and 68.3% of the PreCOVID group expressing this opinion. Regarding the ability to perform all kinds of procedures on patients and the realism of cues and consequences in natural clinical environments, 71.3% of the COVID group and 62.2% of the PreCOVID group "Agreed" or "Strongly agreed" that MedSIM was effective.
In terms of the specific skills that the platform enhanced, both the PreCOVID and COVID groups had a high percentage of students who "Agreed" or "Strongly agreed" that MedSIM helped with physical assessment, with 74.4% of the COVID group and 67.1% of the PreCOVID group expressing this opinion. Similarly, a high percentage of both groups also "Agreed" or "Strongly agreed" that the platform helped with psychosocial assessment, with 70.1% of the COVID group and 68.3% of the PreCOVID group expressing this opinion. Regarding problem-solving and decision-making, 78.2% of the COVID group and 68.3% of the PreCOVID group "Agreed" or "Strongly agreed" that MedSIM was effective. Other skills that both groups had high percentages of "Agreement" or "Strong agreement" for included developing a plan of action, applying psychosocial interventions, documenting information, understanding the basis for interventions, working with diverse populations or groups, and developing one's role within the profession.
According to a significant proportion of students in the COVID group, MedSIM improved their skills in psychosocial assessment (POR = 1.91, p = .03). The COVID group also reported that MedSIM's more complex clinical scenarios enhanced their clinical reasoning and judgment skills (POR = 1.91, p = .03)
In terms of the online performance and control over interactions with the simulator, both the PreCOVID and COVID groups had a high percentage of students who rated the performance as "Very good" or "Excellent," with 31 students in both groups rating it as "Very good" and 13 students in the PreCOVID group (18.8%) and 16 students in the COVID group (20.3%) rating it as "Excellent." The remaining students in both groups rated the performance as "Good." (
Table 3)
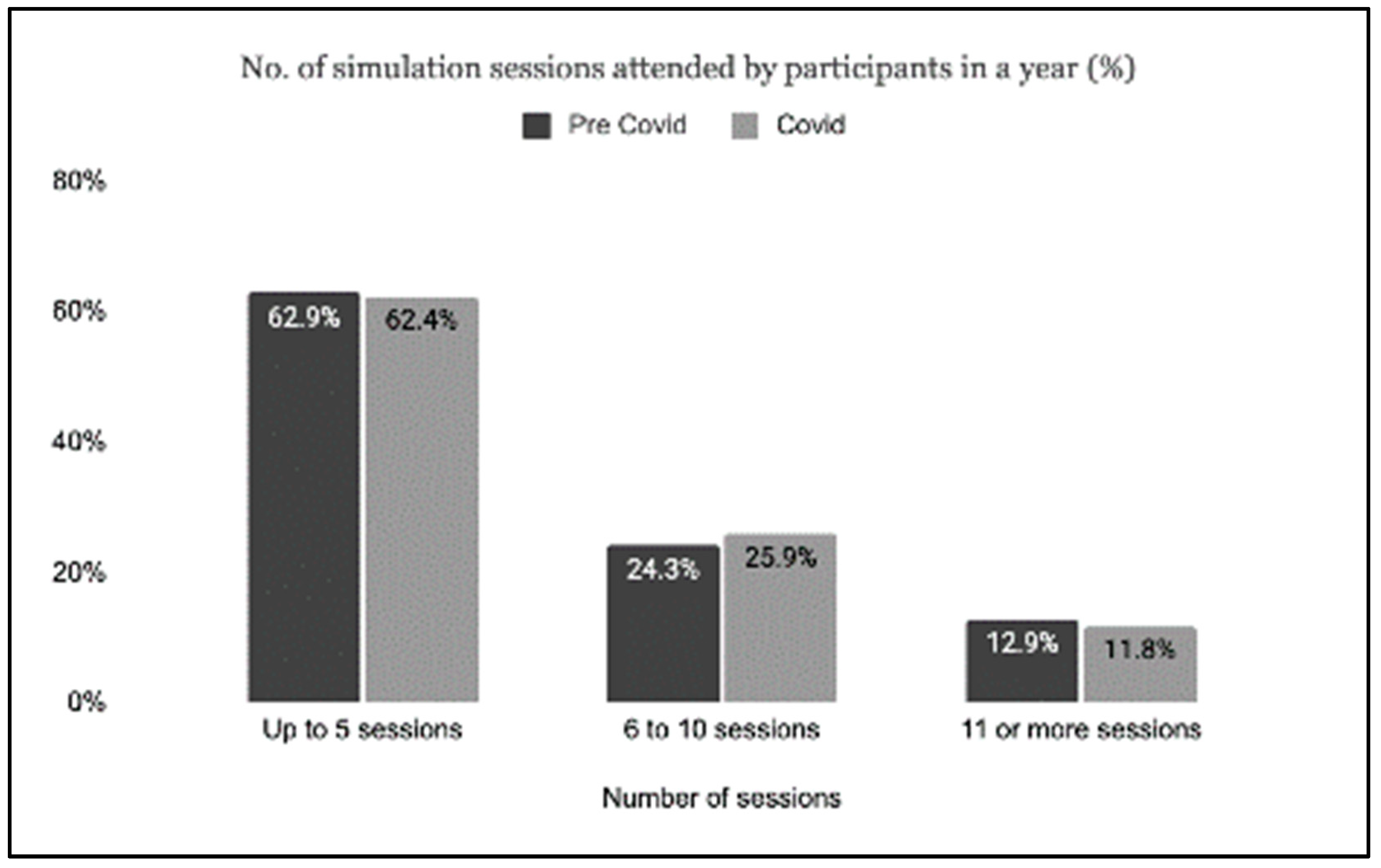
3.2. Simulation sessions
Both the study groups reflected a similar percentage regarding the number of simulation sessions attended by students in a year (
Figure 10). Fewer students attended 11 sessions or more (PreCOVID n = 9, 12.9%; COVID n = 10, 11.8%). The percentage who attended 6 to 10 sessions was again similar in the PreCOVID and COVID groups (24.3% and 25.9%, respectively). On the other hand, there were more numbers in those who attended five sessions (PreCOVID n = 44, 62.9%; COVID n = 53, 62.4%).
3.3. Text mining of open-ended questions
Open-ended questions can be useful for collecting detailed and specific feedback from students. They allow students to express their thoughts and opinions in their own words rather than being limited to pre-specified answer choices.
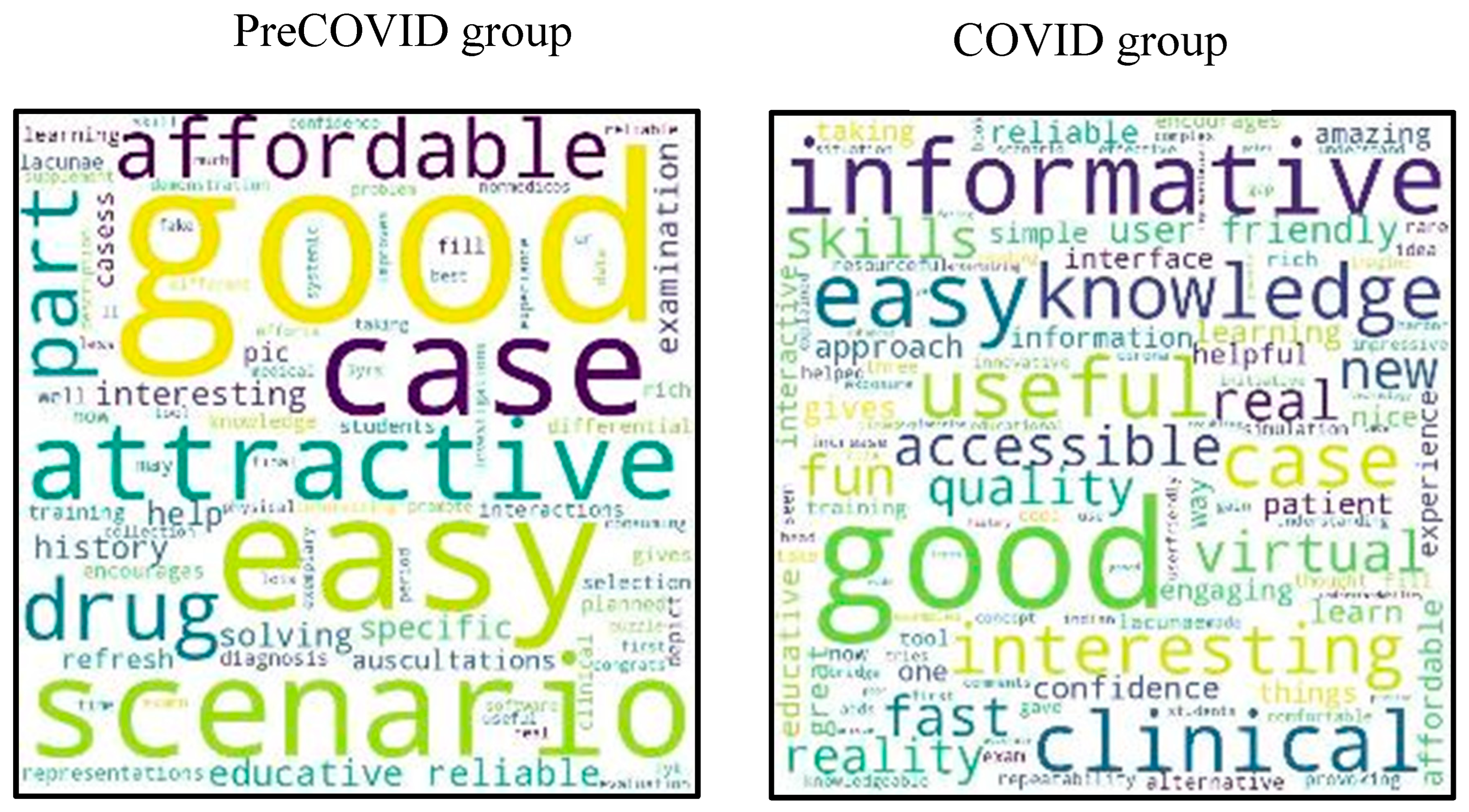
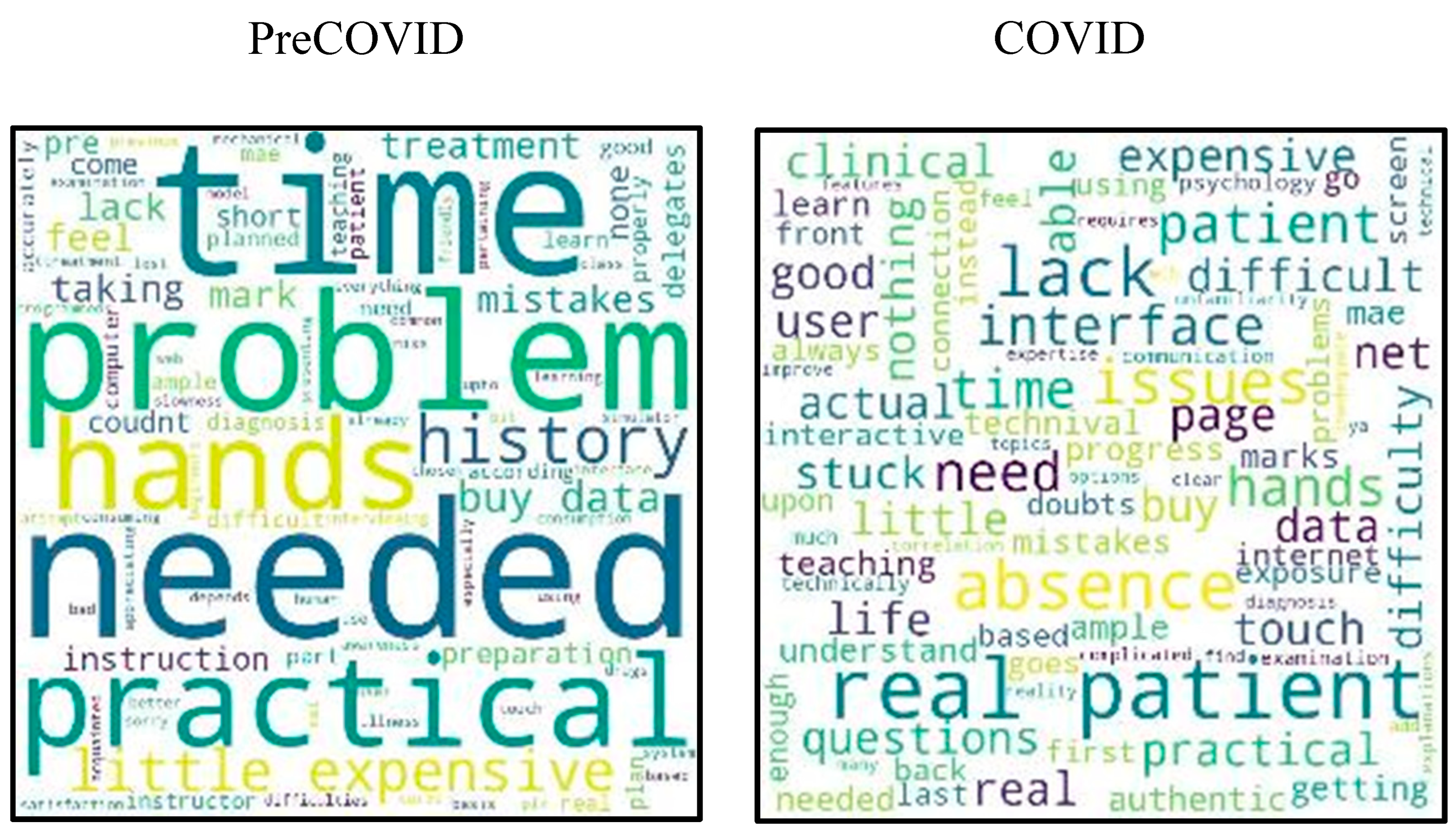
During the COVID pandemic, 87 students provided 218 responses to open-ended questions. During the PreCOVID time, there were 160 responses from 82 students. The open-ended questions in the questionnaire were analyzed using Python Text Analytics software and visualized using a word cloud. The size of each word in the word cloud reflects its importance and frequency in the text. The word frequencies table shows the frequency, rank, and number of documents in which a specific word appears. In addition, the text was analyzed using Quote Matrix based on socio-demographic data. In both groups, the majority of responses were positive. The word cloud for three questions is shown in
Figure 5,
Figure 6 and
Figure 7.
The responses from students analyzed using a customized word cloud for MedSIM indicated that most students found MedSIM to be good and of educational value. The word "easy" also frequently appeared, suggesting that students found MedSIM easy to use and understand. The high percentage of positive responses and lack of negative responses demonstrate the effectiveness of MedSIM as a learning tool. In a multicentre study conducted by Andrew Thomas et al. in 2020, students reported that they enjoyed the convenience of online classes and the ability to learn at their own pace. However, students who did not like online classes cited network problems as the main reason (Thomas et al., 2020).
During the COVID pandemic, there were around 218 responses from 87 students in the COVID group and 160 responses from 82 students in the PreCOVID group. The responses were mostly positive. When asked to describe three interesting things about MedSIM (
Figure 11), the word cloud for the first study group (PreCOVID) included words such as "good," "learning tool," "representation," "educative," "easy to learn," "useful," "fun," "accessible," "easy to use," and "easy to understand." In the COVID group, common words included "informative," "easy," "knowledge," "interesting," "useful," and "good."
When asked to specify three problems/difficulties they faced while performing the simulator (
Figure 12), the PreCOVID students mentioned time-related challenges such as "time was short" and "time-consuming." A few said that guidance was required to familiarize themselves with the platform, mentioning problems such as "lack of instruction" and "lack of instruction from the instructor." In the COVID group, the words frequently included "lack of real patients" and "difficulty."
When asked about the benefits of using MedSIM, students in the COVID group reported that it helped accelerate their progress in learning curves for skills development (77.0%), enabled them to perform all kinds of procedures on patients (71.3%), showed cues and consequences similar to those in natural clinical environments (71.3%), and enhanced their skills in various aspects such as physical assessment (74.4%), psychosocial assessment (70.1%), problem-solving and decision-making (78.2%), developing a plan of action (75.9%), applying psychosocial interventions (74.7%), documenting information (76.7%), understanding the basis for interventions (78.2%), working with diverse populations or groups (75.6%), and developing their role within the profession (75.9%). Over 50% of both groups agreed that MedSIM was beneficial in all these areas.
The study's results showed that most PreCOVID and COVID students attended an average of 6 to 10 simulation sessions. This finding is similar to other studies conducted worldwide (Alabdulwahhab et al., 2021; Nisar et al., 2021; Thomas et al., 2020). In this study, more students in the COVID group participated in simulation sessions than in the PreCOVID group. This could be due to the availability of virtual learning tools during the COVID pandemic, which allowed students to access simulation training remotely.
According to the data collected, all of the medical students in the COVID group who used the MedSIM platform rated their online performance as either good (40.5%), very good (39.2%), or excellent (20.3%). Additionally, the ratings of the extent of control over the interactions and simulation of the natural clinical environment showed similar levels of satisfaction (
Figure 9). This positive response to simulation-based learning aligns with the findings of a study conducted by Nahla Khamis et al. in 2020 (Ibrahim et al., 2021). It is worth noting that the specifics of the study involved comparing the number of simulation sessions attended by students in the PreCOVID and COVID periods. A higher percentage of students were found to attend an average of 6 to 10 sessions during the COVID period (
Figure 4). These results were consistent with other studies conducted worldwide (Alabdulwahhab et al., 2021; Nisar et al., 2021; Thomas et al., 2020.
4. Conclusions and future research
Due to the COVID-19 pandemic and the need for social distancing, traditional medical training has been disrupted. However, Virtual Patient case platforms, like MedSIM, have proven to be a valuable supplement to prevent interruption in medical education. MedSIM was used to supplement medical training during the COVID-19 pandemic. The MedSIM platform was found to be beneficial for students in medical and surgical courses, and students recommended using it for learning purposes in clinical practice skills. Our study found that the MedSIM platform was effective in helping students learn how to manage infrequently occurring medical conditions and accelerate their progress in clinical skills development. Students also reported that the MedSIM enabled them to perform procedures in a way that was similar to real clinical environments and showed cues and consequences similar to those found in natural clinical environments. Most students who used the MedSIM platform found it helpful and educational, with many noting that it was easy to use and understand. Most responses to the open-ended question were positive, indicating the effectiveness of MedSIM as a learning tool for medical students.
MedSIM integrates real-life images, audio, animations, and simulations of the entire learning process into a Virtual Patient case to provide an end-to-end learning and assessment tool for medical students. This comprehensive approach to simulation-based learning can help students build confidence in communication and examination skills while also avoiding the physical and emotional distress caused to actual patients by repetitive interactions with multiple students. Virtual Patient cases can simulate clinical scenarios that replicate specific disorders or situations.
While Virtual Patient cases can be used as training tools and supplement clinical evaluations, it is not always possible to fully replace in-person clinical evaluations. The main differences during the COVID-19 pandemic included the need for remote access to actual patients due to lockdowns and increased demand for medical simulations. Our findings suggest that MedSIM can help acquire skills typically gained through in-person training. The data in this study indicate that combining traditional bedside teaching with online access to virtual resources such as MedSIM should be considered for future use.
MedSIM platform can help to achieve SDG 3 (Good Health and Well-Being) by improving the skills and knowledge of healthcare professionals, which can lead to better patient outcomes and increased access to healthcare services. It can also contribute to SDG 4 (Quality Education) by providing a platform for healthcare professionals to learn and practice essential skills in a safe and controlled environment. In addition, medical simulation can contribute to SDG 17 (Partnerships for the Goals) by enabling collaboration and knowledge-sharing between stakeholders, including healthcare providers, educational institutions, and industry partners.
In the future versions of MedSIM, there will be dedicated online skills labs for preclinical and paraclinical subjects that teach theoretical concepts, offer videos such as dissections and physiology experiments, and provide simulations, animations, and assessments. The platform will also include Virtual Patient cases with interactive 2D & 3D simulations and animations. The learning management system includes administrative, assessment, and reporting tools that allow for direct reporting on student and class performance to heads of departments.
The use of MedSIM as a training method during the COVID-19 pandemic was a short-term solution to meet the needs of students and prevent delays in their careers. However, this study was limited in its ability to fully evaluate the effectiveness of using the MedSIM virtual platform for assessing students' scores and progress in clinical reasoning skills, as it required a dedicated team of personnel. Additionally, the experiences of teachers and the potential long-term benefits of using this Virtual Patient simulation method at our center were not evaluated in this study. Finally, further research with a larger sample size and a randomized, prospective design is needed to determine the added value of this training method and whether medical students who use Virtual Patients show improved medical knowledge and clinical reasoning skills compared to traditional training methods.
Declarations
We would like to confirm that the research presented in this manuscript is original and has not been published elsewhere. To our knowledge, there is no conflict of interest to disclose. The authors declare that they have no competing interests in the manuscript.
Data availability
Data available on request from the authors
References
- Alabdulwahhab, K. M., Kazmi, S. Y., Sami, W., Almujel, K. N., Alanazi, M. H., Alanazi, K. F., … Al Alwadani, F. (2021). Use of online resources by undergraduate medical students at College of Medicine, Majmaah University, Kingdom of Saudi Arabia. PLOS ONE, 16(8), e0255635. [CrossRef]
- Al-Balas, M., Al-Balas, H. I., Jaber, H. M., Obeidat, K., Al-Balas, H., Aborajooh, E. A., … Al-Balas, B. (2020). Correction to: Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives (BMC Medical Education, (2020), 20, 1, (341), 10.1186/s12909-020-02257-4). BMC Medical Education, 20(1), 1–1. [CrossRef]
- Al-Elq, A. H. (2010). Simulation-based medical teaching and learning. Journal of Family & Community Medicine, 17(1), 35–40. [CrossRef]
- Chan, K. S., & Zary, N. (2019). Applications and challenges of implementing artificial intelligence in medical education: an integrative review. JMIR medical education, 5(1), e13930. [CrossRef]
- Cook, D. A., Erwin, P. J., & Triola, M. M. (2010). Computerized virtual patients in health professions education: a systematic review and meta-analysis. Academic Medicine, 85(10), 1589-1602. [CrossRef]
- Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika 16, 297–334. [CrossRef]
- D'Angelo AL, Kchir H. Error Management Training in Medical Simulation. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546709/.
- Fioccola, G. B., Sommese, R., Tufano, I., Canonico, R., & Ventre, G. (2016). Polluino: An efficient cloud-based management of IoT devices for air quality monitoring. 2016 IEEE 2nd International Forum on Research and Technologies for Society and Industry Leveraging a Better Tomorrow, RTSI 2016. [CrossRef]
- French, A.J. (2020). Simulation and Modeling Applications in Global Health Security. In: Masys, A., Izurieta, R., Reina Ortiz, M. (eds) Global Health Security. Advanced Sciences and Technologies for Security Applications. Springer, Cham. [CrossRef]
- Frenk, J., Chen, L. C., Chandran, L., Groff, E. O., King, R., Meleis, A., & Fineberg, H. V. (2022). Challenges and opportunities for educating health professionals after the COVID-19 pandemic. The Lancet, 400(10362), 1539-1556. [CrossRef]
- H.Higham, B.Baxendale . To err is human: use of simulation to enhance training and patient safety in anaesthesia.
- Ibrahim, N. K., Al Raddadi, R., AlDarmasi, M., Al Ghamdi, A., Gaddoury, M., AlBar, H. M., & Ramadan, I. K. (2021). Medical 'students' acceptance and perceptions of e-learning during the COVID-19 closure time in King Abdulaziz University, Jeddah. Journal of Infection and Public Health, 14(1), 17–23. [CrossRef]
- Khetrapal, S., & Bhatia, R. (2020). Impact of COVID-19 pandemic on health system & Sustainable Development Goal 3. The Indian Journal of Medical Research, 151(5), 395. [CrossRef]
- McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., & Scalese, R. J. (2010). A critical review of simulation-based medical education research: 2003-2009. Medical Education, 44(1), 50–63. [CrossRef]
- Nedungadi, P., Jinachandran, R., Mohan, A., & Raman, R. (2019). Rural Health in Digital India: Interactive Simulations for Community Health Workers. In Proceedings - IEEE 10th International Conference on Technology for Education, T4E 2019. [CrossRef]
- Nedungadi, Prema, & Raman, R. (2016). The medical Virtual Patient simulator (MedVPS) platform. Advances in Intelligent Systems and Computing, 384, 59–67. [CrossRef]
- Nedungadi, Prema, Jayakumar, A., & Raman, R. (2018). Personalized Health Monitoring System for Managing Well-Being in Rural Areas. Journal of Medical Systems, 42(1). [CrossRef]
- Nestel, D., & Bearman, M. (2014). Simulated Patient Methodology: Theory, Evidence and Practice. John Wiley & Sons, New Jersey. Retrieved from https://www.wiley.com/en-it/Simulated+Patient+Methodology%3A+Theory%2C+Evidence+and+Practice-p-9781118760956.
- Nisar, S., Mahboob, U., Khan, R. A., & Rehman, D. (2021). Challenges of peer assisted learning in online clinical skills training of ophthalmology module. BMC Medical Education, 21(1), 1–6. [CrossRef]
- Raman, R., Vinuesa, R., & Nedungadi, P. (2021). Bibliometric Analysis of SARS, MERS, and COVID-19 Studies from India and Connection to Sustainable Development Goals. Sustainability 2021, Vol. 13, Page 7555, 13(14), 7555. [CrossRef]
- Raman R, Vinuesa R, Nedungadi P. Acquisition and User Behavior in Online Science Laboratories before and during the COVID-19 pandemic. Multimodal Technologies and Interaction. 2021; 5(8):46. [CrossRef]
- Raman R, Achuthan K, Nair VK, Nedungadi P. Virtual Laboratories- A historical review and bibliometric analysis of the past three decades. Educ Inf Technol (Dordr). 2022;27(8):11055-11087. Epub 2022 Apr 28. PMID: 35502162; PMCID: PMC9046012. [CrossRef] [PubMed]
- Rosen, K. R. (2008). The history of medical simulation. Journal of Critical Care, 23(2), 157–166. [CrossRef]
- Tabatabai, S. (2017). Necessity of Designing a National Model of Foresight-Based Policy-Making in Medical Education. Strides in Development of Medical Education, 14(3). [CrossRef]
- Thomas, A., Jemima Cox, M., Shenoy, M. T., Shenoy, K. T., Suresh Kumar, S., Sidheeque, A., … P, S. (2020). Survey Among Medical Students During COVID-19 Lockdown: The Online Class Dilemma. International Journal of Medical Students, 8(2), 102–106. [CrossRef]
- Wang, S., Ren, X., Ye, J., Wang, W., Huang, H., & Qin, C. (2021). Exploration of simulation-based medical education for undergraduate students. Medicine, 100(20), e25982. [CrossRef]
- Watari et al., 2020.
- Watari T, Tokuda Y, Owada M, Onigata K. The Utility of Virtual Patient Simulations for Clinical Reasoning Education. Int J Environ Res Public Health. 2020;17(15):5325. Published 2020 Jul 24. [CrossRef]
- Williams, M. (2022). Virtual reality in ophthalmology education: simulating pupil examination. Eye, 36(11), 2084-2085. [CrossRef]
- Woodham, Luke A et al. "Virtual Patients designed for training against medical error: Exploring the impact of decision-making on learner motivation. PLoS One. 2019;14(4):e0215597. Published 2019 Apr 23. [CrossRef]
- Zheng, J., Li, S., & Lajoie, S. P. (2022). Diagnosing virtual patients in a technology-rich learning environment: A sequential mining of students' efficiency and behavioral patterns. Education and Information Technologies, 1-17. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).