Submitted:
21 February 2023
Posted:
22 February 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Description
2.2. Sample
-
School:
- -
- elementary public schools, from central and suburban and deprived areas from Petrolina-PE, Brazil;
- -
- indoor gym and with a minimum of one hundred students;
- -
- overweight children [85th percentile for sex and age, according to the World Health Organization [17]
-
Children:
- -
- overweight or obese [17];
- -
- properly enrolled in participating schools;
- -
- parental consent to participate.
2.3. Data Collection
- Anthropometric measurements
- Hemodynamic measurements
- Lipid and glucose profile
- Cardiorespiratory Fitness
- Left Ventricular Mass
- Physical activity and Sedentary Behaviour
- Data management and statistical analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Swinburn B, Egger G Fau - Raza F, Raza F (1999) Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med 29 (0091-7435 (Print)):8. [CrossRef]
- Rogers R, Eagle TF, Sheetz A, Woodward A, Leibowitz R, Song M, Sylvester R, Corriveau N, Kline-Rogers E, Jiang Q, Jackson EA, Eagle KA (2015) The Relationship between Childhood Obesity, Low Socioeconomic Status, and Race/Ethnicity: Lessons from Massachusetts. Child Obes 11 (6):6. [CrossRef]
- Ajala OA-O, Mold F, Boughton C, Cooke D, Whyte M (2017) Childhood predictors of cardiovascular disease in adulthood. A systematic review and meta-analysis. Obes Rev 18 (1467-789X (Electronic)):9. [CrossRef]
- Weihrauch-Blüher S, Wiegand S (2018) Risk Factors and Implications of Childhood Obesity. Curr Obes Rep 7 (4):6. [CrossRef]
- de Simone G, Devereux Rb Fau - Daniels SR, Daniels Sr Fau - Koren MJ, Koren Mj Fau - Meyer RA, Meyer Ra Fau - Laragh JH, Laragh JH (1995) Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol 25 (5):7. [CrossRef]
- Dušan P, Tamara I Fau - Goran V, Goran V Fau - Gordana M-L, Gordana Ml Fau - Amira P-A, Amira PA (2015) Left ventricular mass and diastolic function in obese children and adolescents. Pediatr Nephrol 30 (4):8. [CrossRef]
- Wang Y, Lim H (2012) The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry 24 (3):13. [CrossRef]
- Dinsa GD, Goryakin Y Fau - Fumagalli E, Fumagalli E Fau - Suhrcke M, Suhrcke M (2012) Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev 13 (11):13. [CrossRef]
- Ruiz JR, Cavero-Redondo I, Ortega FB, Welk GJ, Andersen LB, Martinez-Vizcaino V (2016) Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med 50 (23):8. [CrossRef]
- Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput JP, Saunders TJ, Katzmarzyk PT, Okely AD, Connor Gorber S, Kho ME, Sampson M, Lee H, Tremblay MS (2016) Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab 6 (1715-5320 (Electronic)):25. [CrossRef]
- Pearson N, Braithwaite Re Fau - Biddle SJH, Biddle Sj Fau - van Sluijs EMF, van Sluijs Em Fau - Atkin AJ, Atkin AJ (2014) Associations between sedentary behaviour and physical activity in children and adolescents: a meta-analysis. Obes Rev 15 (8):12. [CrossRef]
- Liu M, Li Xc Fau - Lu L, Lu L Fau - Cao Y, Cao Y Fau - Sun RR, Sun Rr Fau - Chen S, Chen S Fau - Zhang PY, Zhang PY (2014) Cardiovascular disease and its relationship with chronic kidney disease. Eur Rev Med Pharmacol Sci 18 (19):8.
- Zoran G, Bozidarka Z, Ivana R, Milan O, Aleksandar M, Djordje R, Esma RI (2017) Link between Metabolic Syndrome and Insulin Resistance. Current Vascular Pharmacology 15 (1):30-39. [CrossRef]
- Andersen LB, Wedderkopp N Fau - Hansen HS, Hansen Hs Fau - Cooper AR, Cooper Ar Fau - Froberg K, Froberg K (2003) Biological cardiovascular risk factors cluster in Danish children and adolescents: the European Youth Heart Study. Prev Med 37 (4):4. [CrossRef]
- Borsboom D, Cramer AO (2013) Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psycho 9 (1548-5951 (Electronic)):30. [CrossRef]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D (2013) Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology 31 (1):43-53. [CrossRef]
- Organization W-WH (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser, vol 854.
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J, Liechty JM, Wiley A, Teran-Garcia M, Jacobsohn GC (2011) Toward a Developmental Conceptualization of Contributors to Overweight and Obesity in Childhood: The Six-Cs Model. Child Development Perspectives 5 (1):50-58. [CrossRef]
- Furusawa EA, Ruiz Mf Fau - Saito MI, Saito Mi Fau - Koch VH, Koch VH (2005) Evaluation of the Omron 705-CP blood pressure measuring device for use in adolescents and young adults (Avaliação do monitor de medida de pressão arterial OMRON 705-CP para uso em adolescentes e adultos jovens. DEP - 20050524). Arq Bras Cardiol 84 (5):8. [CrossRef]
- Brandão AA, Rodrigues CIS, Consolim-Colombo F, Plavnik FL, Malachias MVB, Kohlmann Junior O, Ferreira Filho SJABC (2010) VI diretrizes brasileiras de hipertensão. vol 95.
- Souza CBd, Dourado CdS, Mill JG, Salaroli LB, Molina MdCBJIJoCS (2017) Prevalência de Hipertensão em Crianças de Escolas Públicas. International Journal of Cardiovascular Sciences 30 (1):42-51. [CrossRef]
- Xavier HT, Izar M, Faria Neto J, Assad M, Rocha V, Sposito A, Fonseca F, Dos Santos J, Santos R, Bertolami MJAbdc (2013) V Diretriz brasileira de dislipidemias e prevenção da aterosclerose. vol 101.
- Gaya A, Gaya A (2016) Projeto Esporte Brasil: manual de testes e avaliação versão 2016. UFRGS, Porto Alegre.
- Devereux Rb Fau - Alonso DR, Alonso Dr Fau - Lutas EM, Lutas Em Fau - Gottlieb GJ, Gottlieb Gj Fau - Campo E, Campo E Fau - Sachs I, Sachs I Fau - Reichek N, Reichek N (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57 (6):9. [CrossRef]
- Kohsaka S, Sciacca Rr Fau - Sugioka K, Sugioka K Fau - Sacco RL, Sacco Rl Fau - Homma S, Homma S Fau - Di Tullio MR, Di Tullio MR (2005) Additional impact of electrocardiographic over echocardiographic diagnosis of left ventricular hypertrophy for predicting the risk of ischemic stroke. Am Heart J 149 (1):7. [CrossRef]
- Engelen L, Bundy Ac Fau - Naughton G, Naughton G Fau - Simpson JM, Simpson Jm Fau - Bauman A, Bauman A Fau - Ragen J, Ragen J Fau - Baur L, Baur L Fau - Wyver S, Wyver S Fau - Tranter P, Tranter P Fau - Niehues A, Niehues A Fau - Schiller W, Schiller W Fau - Perry G, Perry G Fau - Jessup G, Jessup G Fau - van der Ploeg HP, van der Ploeg HP (2013) Increasing physical activity in young primary school children--it’s child’s play: a cluster randomised controlled trial. Prev Med 56 (5):6. [CrossRef]
- Evenson KR, Catellier Dj Fau - Gill K, Gill K Fau - Ondrak KS, Ondrak Ks Fau - McMurray RG, McMurray RG (2008) Calibration of two objective measures of physical activity for children. J Sports Sci 26 (14):10. [CrossRef]
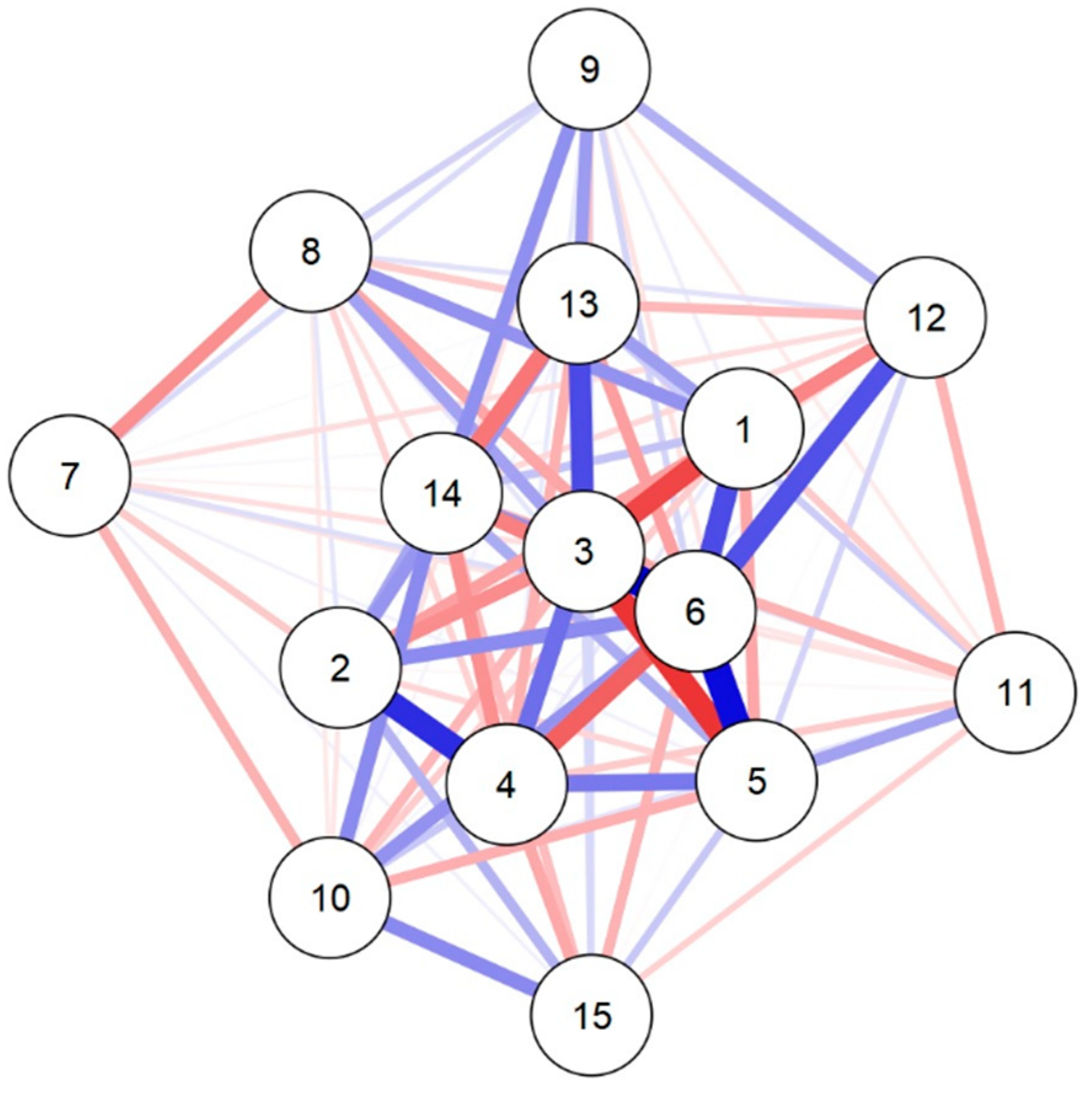
- Fruchterman TMJ, Reingold EM (1991) Graph drawing by force-directed placement. Software: Practice and Experience 21 (11):1129-1164. [CrossRef]
- Friedman J, Hastie T, Tibshirani R (2008) Sparse inverse covariance estimation with the graphical LASSO. Biostatistics (Oxford, England) 9:432-441. [CrossRef]
- Foygel R, Drton M Extended Bayesian information criteria for Gaussian graphical models. In: Advances in neural information processing systems, 2010. pp 604-612.
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D (2012) qgraph: Network Visualizations of Relationships in Psychometric Data. Journal of Statistical Software; Vol 1, Issue 4 (2012). [CrossRef]
- Raistenskis J, Sidlauskiene A, Strukcinskiene B, Uğur Baysal S, Buckus R (2016) Physical activity and physical fitness in obese, overweight, and normal-weight children. Turk J Med Sci 46 (2):8. [CrossRef]
- Bailey DP, Charman SJ, Ploetz T, Savory LA, Kerr CJ (2017) Associations between prolonged sedentary time and breaks in sedentary time with cardiometabolic risk in 10-14-year-old children: The HAPPY study. J Sports Sci 35 (22):8. [CrossRef]
- Ekelund U, Anderssen SA, Froberg K, Sardinha LB, Andersen LB, Brage S (2007) Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: the European youth heart study. Diabetologia 50 (9):9. [CrossRef]
- García-Hermoso A, Cerrillo-Urbina AJ, Herrera-Valenzuela T, Cristi-Montero C, Saavedra JM, Martínez-Vizcaíno V (2016) Is high-intensity interval training more effective on improving cardiometabolic risk and aerobic capacity than other forms of exercise in overweight and obese youth? A meta-analysis. Obes Rev 17 (6):10. [CrossRef]
- Valeria C, Daniela L, Erwan C, Annalisa De S, Paola B, Sebastiano A, Marisa A, Matteo V (2013) Improved metabolic and cardiorespiratory fitness during a recreational training program in obese children. Journal of Pediatric Endocrinology and Metabolism 26 (3-4):271-276. [CrossRef]
- Rajjo T, Mohammed K, Alsawas M, Ahmed AT, Farah W, Asi N, Almasri J, Prokop LJ, Murad MH (2017) Treatment of Pediatric Obesity: An Umbrella Systematic Review. The Journal of Clinical Endocrinology & Metabolism 102 (3):763-775. [CrossRef]
- Brown T, Moore Th Fau - Hooper L, Hooper L Fau - Gao Y, Gao Y Fau - Zayegh A, Zayegh A Fau - Ijaz S, Ijaz S Fau - Elwenspoek M, Elwenspoek M Fau - Foxen SC, Foxen Sc Fau - Magee L, Magee L Fau - O’Malley C, O’Malley C Fau - Waters E, Waters E Fau - Summerbell CD, Summerbell CD (2019) Interventions for preventing obesity in children. Cochrane Database Syst Rev 7 (7). [CrossRef]
- Hills A, Andersen L, Byrne N (2011) Physical activity and obesity in children. British journal of sports medicine 45:866-870. [CrossRef]
- Maron BJ, Fananapazir L (1992) Sudden cardiac death in hypertrophic cardiomyopathy. Circulation 1 (0009-7322 (Print)):7. 0009.
- Westerterp KR (2018) Exercise, energy balance and body composition. European Journal of Clinical Nutrition 72 (9):1246-1250. [CrossRef]
- Ridgers N, Timperio A, Cerin E, Salmon J (2014) Compensation of Physical Activity and Sedentary Time in Primary School Children. Medicine and science in sports and exercise 46. [CrossRef]
- Ekelund U, Luan Ja, Sherar L, Esliger D, Griew P, Cooper A (2012) Moderate to Vigorous Physical Activity and Sedentary Time and Cardiometabolic Risk Factors in Children and Adolescents. JAMA : the journal of the American Medical Association 307:704-712. [CrossRef]
- Kidokoro T, Suzuki K, Naito H, Balasekaran G, Song JK, Park SY, Liou YM, Lu D, Poh BK, Kijboonchoo K, Hui SS-C (2019) Moderate-to-vigorous physical activity attenuates the detrimental effects of television viewing on the cardiorespiratory fitness in Asian adolescents: the Asia-fit study. BMC Public Health 19 (1):1737-1737. [CrossRef]
- Júdice PB, Silva AM, Berria J, Petroski EL, Ekelund U, Sardinha LB (2017) Sedentary patterns, physical activity and health-related physical fitness in youth: a cross-sectional study. Int J Behav Nutr Phys Act 14 (1):25-25. [CrossRef]
- Mäkikallio K, Shah J, Slorach C, Qin H, Kingdom J, Keating S, Kelly E, Manlhiot C, Redington A, Jaeggi E (2015) Fetal growth restriction and cardiovascular outcome in early human infancy: a prospective longitudinal study. Heart and vessels 31. [CrossRef]
- Ji F, Ning F, Duan H, Kaprio J, Zhang D, Zhang D, Wang S, Qiao Q, Sun J, Liang J, Pang Z, Silventoinen K (2014) Genetic and Environmental Influences on Cardiovascular Disease Risk Factors: A Study of Chinese Twin Children and Adolescents. Twin Research and Human Genetics 17 (2):72-79. [CrossRef]
- Bull CJ, Northstone K (2016) Childhood dietary patterns and cardiovascular risk factors in adolescence: results from the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort. Public Health Nutrition 19 (18):3369-3377. [CrossRef]
- Sönmez H, Canpolat N, Ağbaş A, Mehmet T, Ekmekçi Ö, Alikaşifoğlu M, Sever L, Caliskan S (2019) The Relationship between the Waist Circumference and Increased Carotid Intima Thickness in Obese Children. Childhood Obesity 15. [CrossRef]
- Bassali R, Waller J, Gower B, Allison J, Davis C (2009) Utility of waist circumference percentile for risk evaluation in obese children. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity 5:97-101. [CrossRef]
- Sönmez H, Canpolat N, Ağbaş A, Mehmet T, Ekmekçi Ö, Alikaşifoğlu M, Sever L, Caliskan S (2019). The Relationship between the Waist Circumference and Increased Carotid Intima Thickness in Obese Children. Childhood Obesity 15.
- Zampetti S, Campagna G, Leto G, Lucantoni F, D’Onofrio L, Marandola L, Moretti C, Chiesa C, Pacifico L, Buzzetti R (2018) Relation Between Wrist Circumference and Left Ventricular Structure in Overweight Children. The American Journal of Cardiology 121. [CrossRef]
- Zimmet P, Alberti G Fau - Kaufman F, Kaufman F Fau - Tajima N, Tajima N Fau - Silink M, Silink M Fau - Arslanian S, Arslanian S Fau - Wong G, Wong G Fau - Bennett P, Bennett P Fau - Shaw J, Shaw J Fau - Caprio S, Caprio S (2007) The metabolic syndrome in children and adolescents. Lancet 369 (9579):3. [CrossRef]
- Nehus E, Mitsnefes M (2019) Childhood Obesity and the Metabolic Syndrome. Pediatric Clinics of North America 66 (1):31-43. [CrossRef]
| Variables | Boys (n = 18) (Mean ± SD) |
Girls (n = 23) (Mean ± SD) |
p | d’ Cohen |
|---|---|---|---|---|
| Age | 7.7 ± 0.9 | 8.0 ± 1.0 | 0.277 | -0.347 |
| MVPA (min/day) | 34.6 ± 16.4 | 24.6 ± 13.5 | 0.037 | 0.679 |
| SB (min/day) | 330.4 ± 44.6 | 389.0 ± 68.6 | 0.003 | -0.987 |
| BMI (kg/m²) | 21.7 ± 3.2 | 22.1 ± 2.6 | 0.621 | -0.157 |
| WC (cm) | 68.8 ± 3.2 | 22.1 ± 2.6 | 0.822 | 0.071 |
| Fat (%) | 34.2 ± 9.2 | 34.7 ± 6.5 | 0.841 | -0.063 |
| MBP (mmHg) | 84.5 ± 6.9 | 80.3 ± 8.2 | 0.091 | 0.546 |
| TC (mg/dl) | 159.2 ± 35.3 | 156.6 ± 35.4 | 0.800 | 0.080 |
| HDL-C (mg/dl) | 37.4 ± 3.8 | 37.3 ± 7.8 | 0.962 | 0.015 |
| LDL-C (mg/dl) | 101.9 ± 29.8 | 97.8 ± 25.7 | 0.635 | 0.151 |
| TG (mg/dl) | 96.3 ± 45.1 | 100.9 ± 52.3 | 0.769 | -0.093 |
| Glucose (mg/dl) | 82.4 ± 5.8 | 82.7 ± 6.2 | 0.891 | -0.044 |
| CRF (meters) | 748.6 ± 73.7 | 752.0 ± 95.3 | 0.901 | -0.039 |
| LVM (g) | 49.9 ± 9.4 | 48.2 ± 12.4 | 0.629 | 0.153 |
| Sokolow-Lyon | 33.4 ± 6.9 | 31.7 ± 5.6 | 0.384 | 0.277 |
| Variables | MVPA | SB | Age | Sex | BMI | WC | MBP | HDL | LDL | TGL | Glucose | Fat | CRF | LVM | Sokolov |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MVPA | 0.000 | ||||||||||||||
| SB | -0.267 | 0.000 | |||||||||||||
| Age | -0.513 | -0.319 | 0.000 | ||||||||||||
| Sex | 0.062 | 0.581 | 0.408 | 0.000 | |||||||||||
| BMI | -0.251 | -0.116 | -0.561 | 0.378 | 0.000 | ||||||||||
| WC | 0.499 | 0.326 | 0.716 | -0.444 | 0.664 | 0.000 | |||||||||
| MBP | 0.016 | -0.097 | -0.094 | -0.151 | 0.037 | 0.092 | 0.000 | ||||||||
| HDL-C | 0.307 | 0.069 | 0.263 | -0.127 | 0.072 | -0.253 | -0.315 | 0.000 | |||||||
| LDL-C | 0.047 | 0.008 | -0.174 | 0.065 | -0.086 | 0.122 | 0.105 | 0.129 | 0.000 | ||||||
| TG | -0.144 | -0.073 | -0.204 | 0.156 | -0.228 | 0.305 | -0.219 | -0.062 | -0.083 | 0.000 | |||||
| Glucose | -0.148 | -0.020 | 0.084 | -0.150 | 0.265 | -0.072 | -0.080 | 0.004 | -0.060 | 0.079 | 0.000 | ||||
| Fat | -0.341 | -0.092 | -0.115 | 0.035 | 0.123 | 0.485 | -0.099 | 0.084 | 0.224 | 0.021 | -0.212 | 0.000 | |||
| CRF | 0.276 | 0.296 | 0.503 | -0.223 | 0.164 | -0.271 | 0.011 | -0.146 | 0.277 | 0.031 | 0.144 | -0.199 | 0.000 | ||
| LVM | 0.171 | 0.250 | 0.318 | -0.311 | 0.237 | -0.355 | -0.027 | -0.089 | 0.314 | 0.329 | -0.217 | -0.108 | -0.386 | 0.000 | |
| Sokolov | 0.203 | 0.215 | 0.110 | -0.248 | 0.158 | -0.216 | 0.038 | -0.093 | 0.112 | 0.331 | -0.128 | -0.012 | -0.075 | -0.187 | 0.000 |
| Variables | Network | ||
|---|---|---|---|
| Betweenness | Closeness | Strength | |
| MVPA | -0.502 | 0.585 | 0.480 |
| SB | -0.662 | -0.029 | -0.044 |
| Age | 0.459 | 1.506 | 1.628 |
| Sex | -0.182 | 0.596 | 0.576 |
| BMI | 0.139 | 0.504 | 0.574 |
| WC | 3.182 | 1.809 | 2.069 |
| Fat | -0.662 | 0.074 | -0.627 |
| MBP | -0.662 | -1.602 | -1.403 |
| HDL-C | 0.299 | -0.831 | -0.764 |
| LDL-C | -0.662 | -1.062 | -0.976 |
| TG | -0.182 | -0.211 | -0.510 |
| Glucose | -0.662 | -1.307 | -1.120 |
| CRF | -0.021 | 0.159 | 0.233 |
| LVM | 0.779 | 0.717 | 0.536 |
| Sokolow-Lyon | -0.662 | -0.908 | -0.651 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





