Submitted:
24 February 2023
Posted:
27 February 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
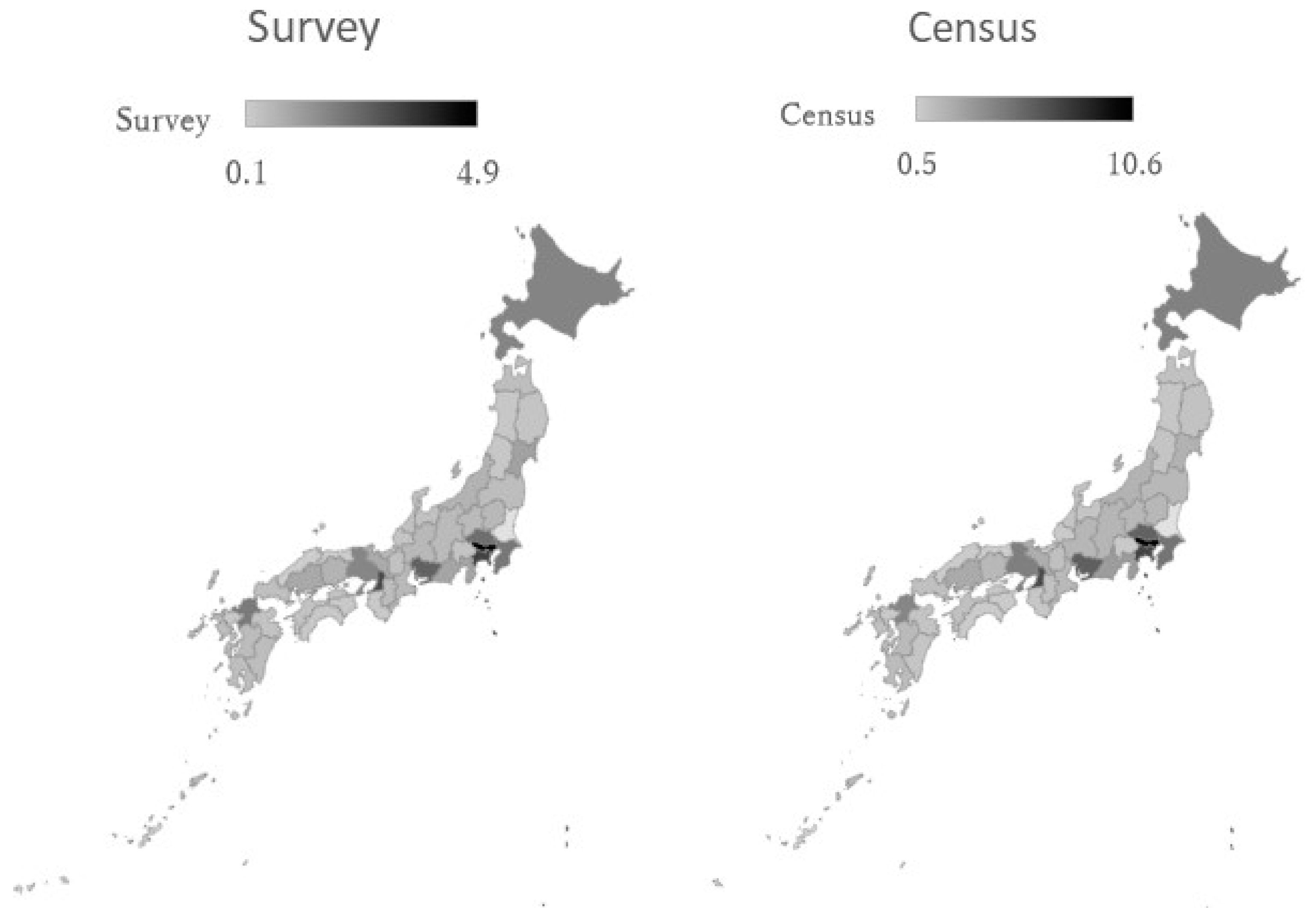
2. Materials and Methods
2.1. Data Collection
2.2. Ethical Considerations
2.3. Measurements
- (1)
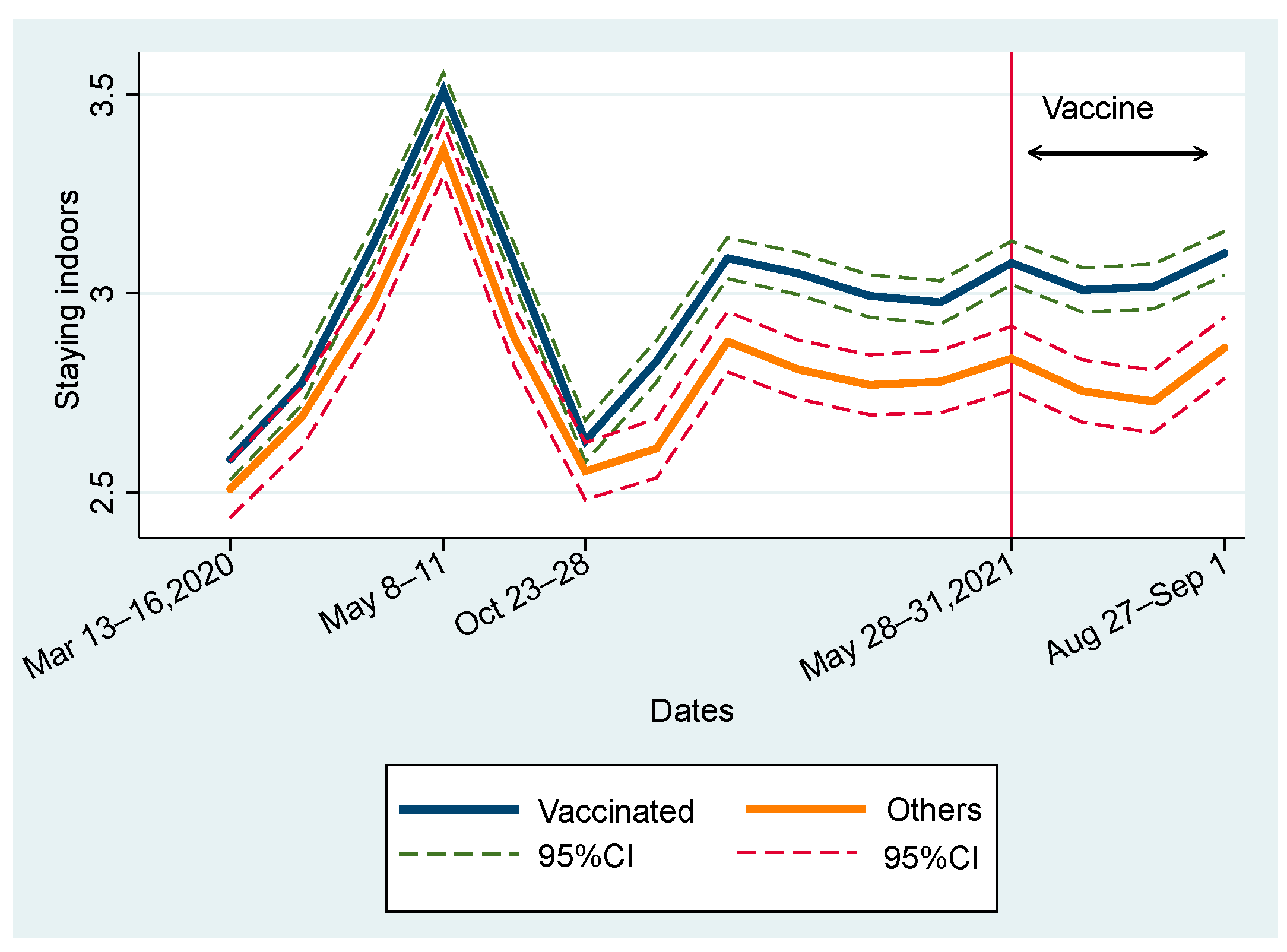
- Staying indoors
- (2)
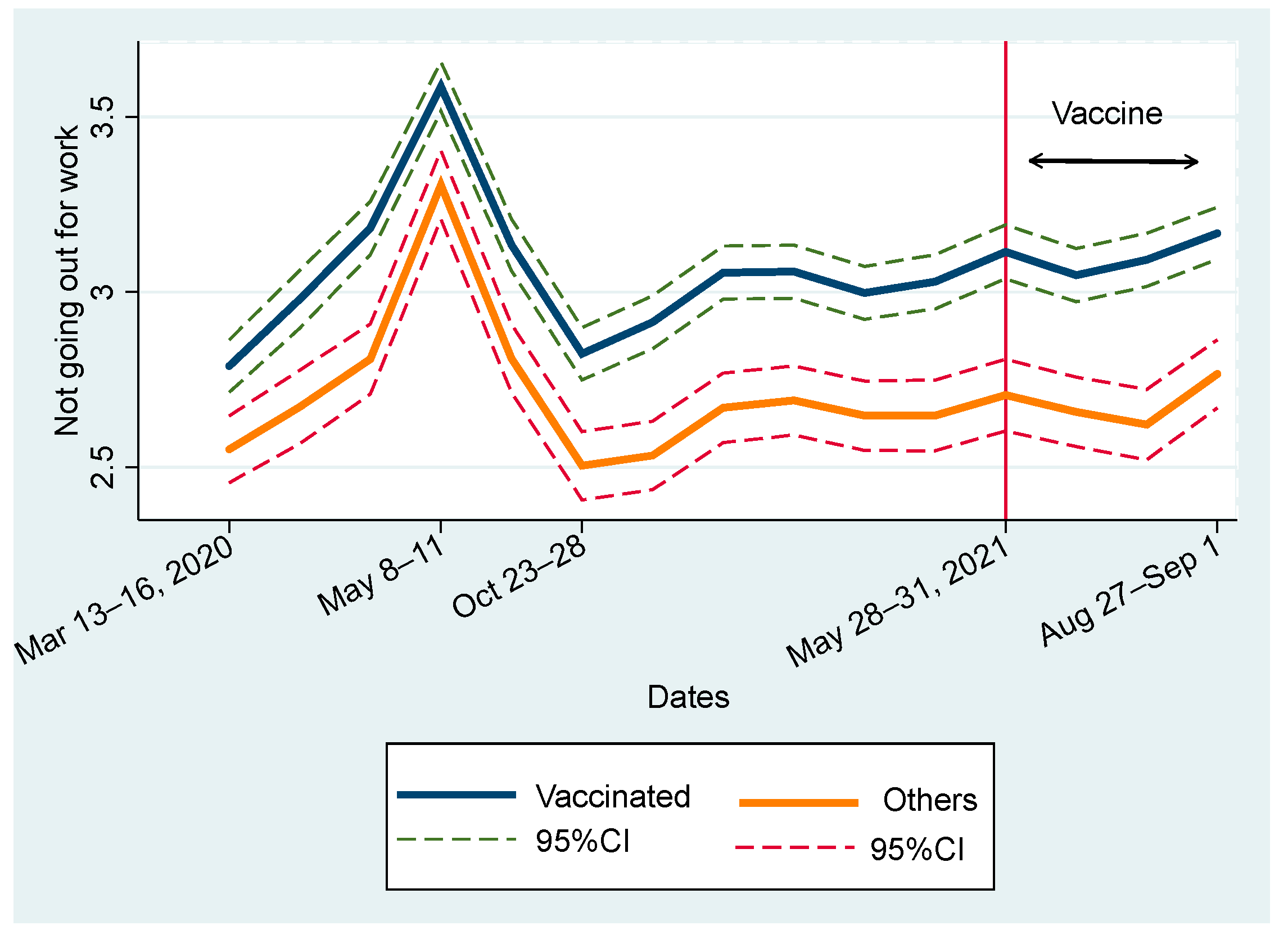
- Not going out to the workplace (or school)
- (3)
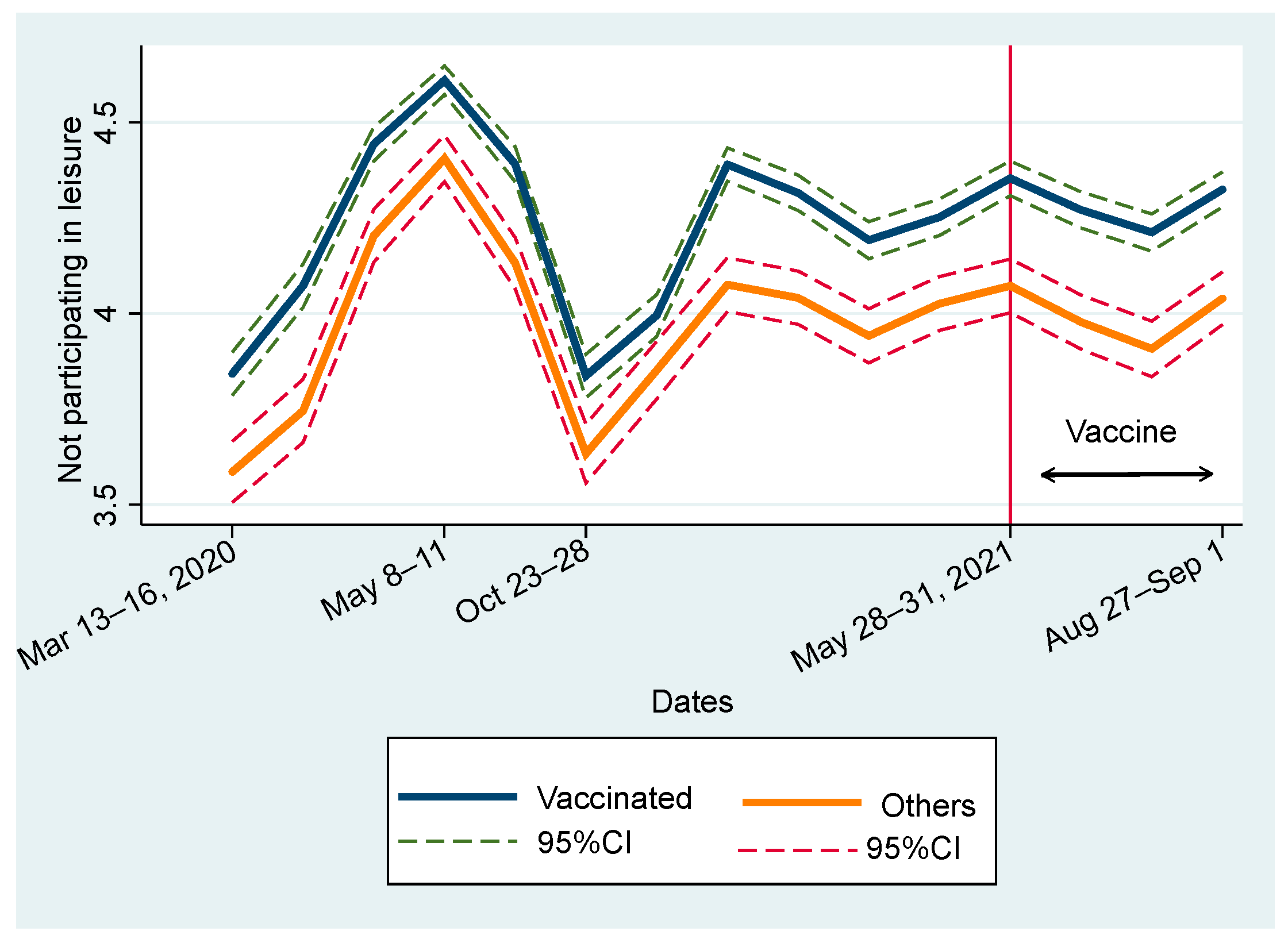
- Not going out to the events or travel
- (4)
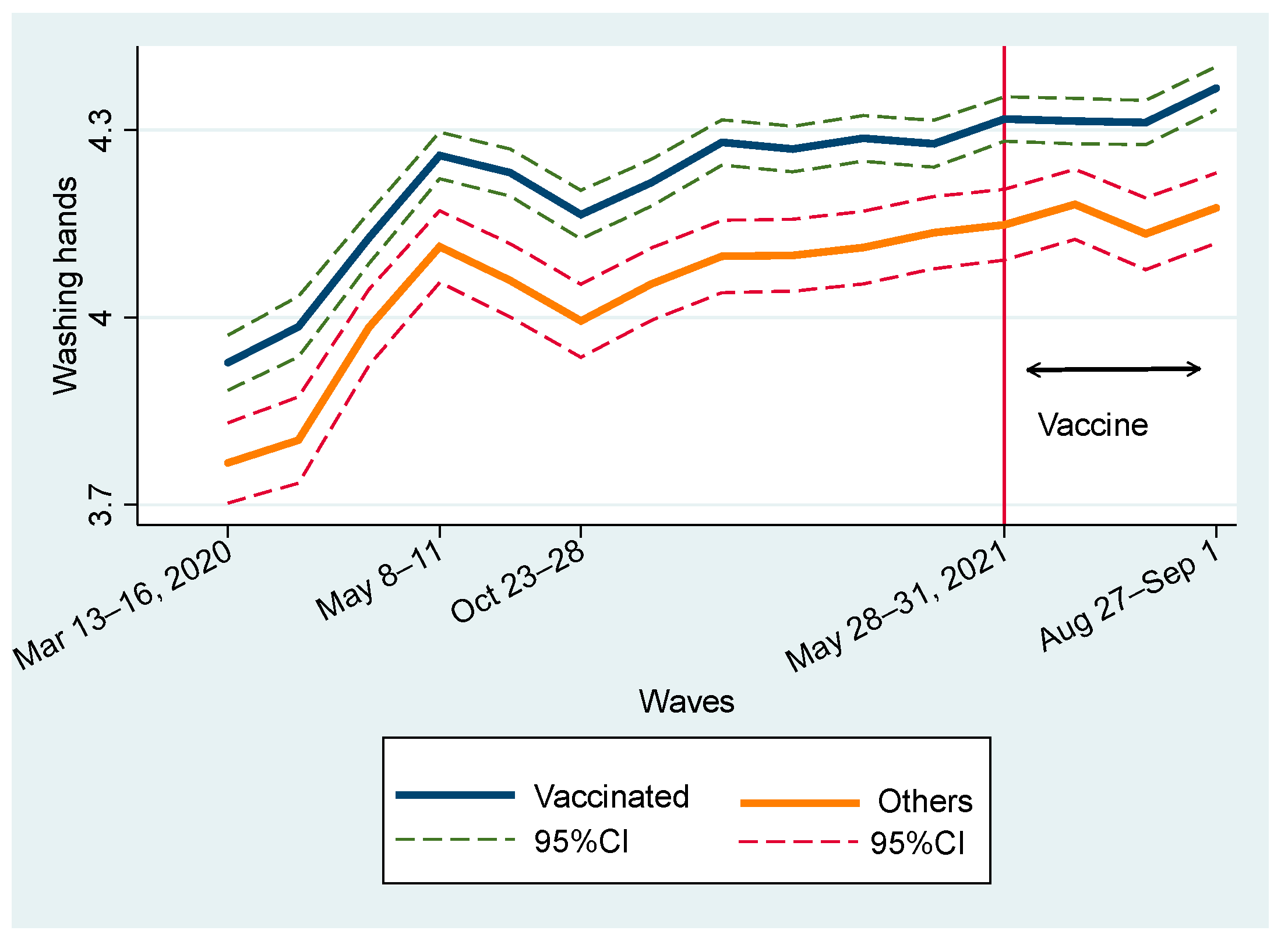
- Washing my hands thoroughly
- (5)
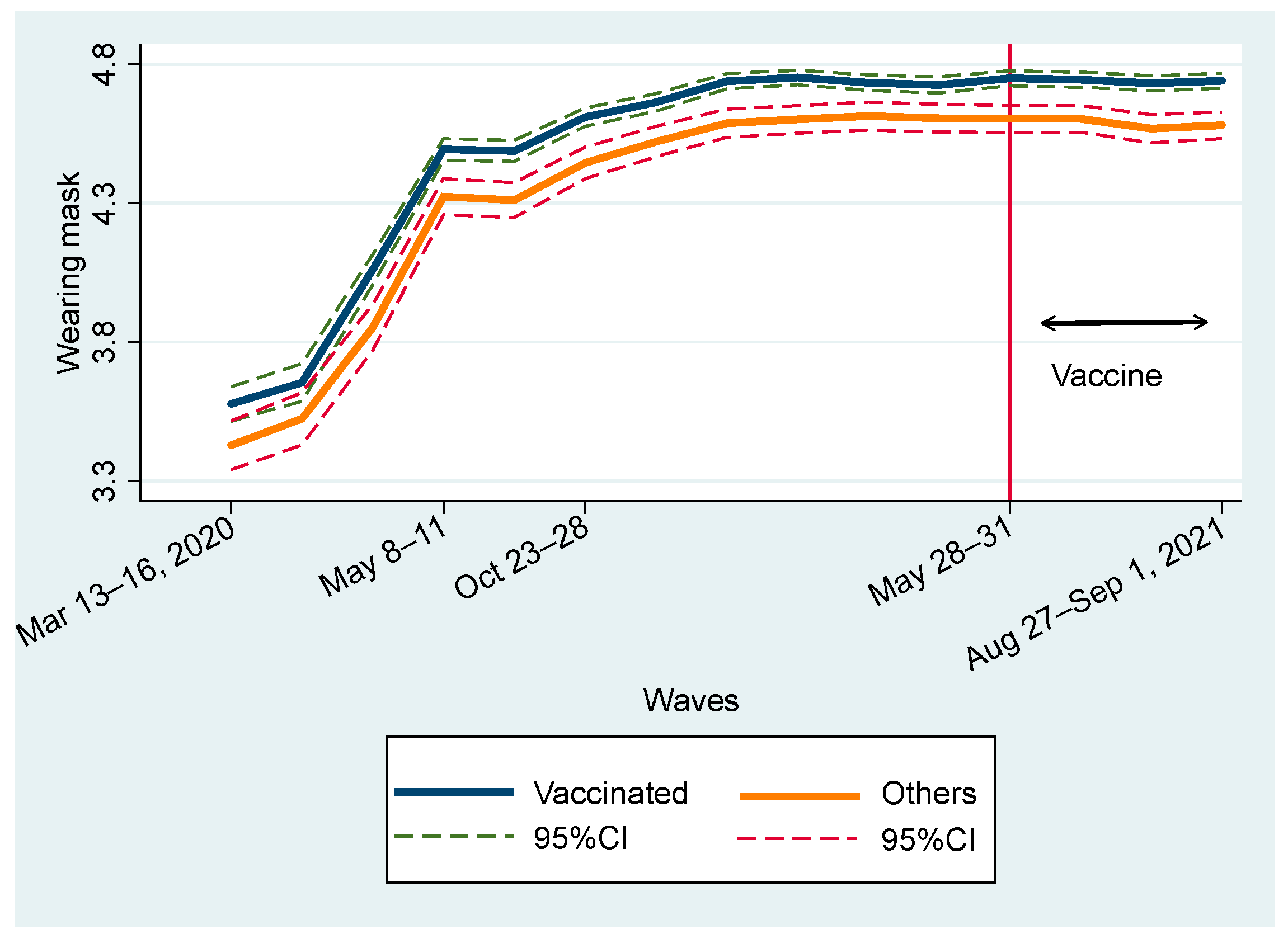
- Wearing a mask
2.4. Methods
3. Results
3.1. Full Sample Estimations
3.2. Subsample Estimations (Young vs Old Ages Groups)
4. Discussion
4.1. Strength
4.2. Limitation
Author Contributions
Funding
Availability of data and materials:
Declarations
Ethics Approval and Consent to Participate:
Consent for publication:
Conflicts of Interest:
References
- Born, B.; Dietrich, A.M.; Müller, G.J. The Lockdown Effect: A Counterfactual for Sweden. PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Liu, Y.; Li, Y.; Wu, C.-H.; Chen, B. Kraemer MUG An Investigation of Transmission Control Measures during the First 50 Days of the COVID-19 Epidemic in China. Science (1979) 2020, 368, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Imperial College COVID-19 Response Team; Flaxman S; Mishra S; Gandy A; Unwin HJT; Mellan TA Estimating the Effects of Non-Pharmaceutical Interventions on COVID-19 in Europe. Nature 2020, 584, 257–261.
- Hyafil A; Moriña D Analysis of the Impact of Lockdown on the Reproduction Number of the SARS-Cov-2 in Spain. Gac Sanit 2020, S0213911120300984.
- Alfano V; Ercolano S The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl Health Econ Health Policy 2020, 18, 509–517. [CrossRef]
- Ambikapathy, B.; Krishnamurthy, K. Mathematical Modelling to Assess the Impact of Lockdown on COVID-19 Transmission in India: Model Development and Validation. JMIR Public Health Surveill 2020, 6, e19368. [Google Scholar] [CrossRef] [PubMed]
- Mottaleb, K.A.; Mainuddin, M.; Sonobe, T. COVID-19 Induced Economic Loss and Ensuring Food Security for Vulnerable Groups: Policy Implications from Bangladesh. PLoS One 2020, 15. [Google Scholar] [CrossRef]
- Inoue, H.; Murase, Y.; Todo, Y. Do Economic Effects of the Anti-COVID-19 Lockdowns in Different Regions Interact through Supply Chains? PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Chinna, K.; Sundarasen, S.; Khoshaim, H.B.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Hossain, S.F.A.; Sukayt, A.; Dalina, N.; Rajagopalan, U.; et al. Psychological Impact of COVID-19 and Lock down Measures: An Online Cross-Sectional Multicounty Study on Asian University Students. PLoS One 2021, 16. [Google Scholar] [CrossRef]
- Fiorenzato, E.; Zabberoni, S.; Costa, A.; Cona, G. Cognitive and Mental Health Changes and Their Vulnerability Factors Related to COVID-19 Lockdown in Italy. PLoS One 2021, 16. [Google Scholar] [CrossRef]
- Greyling, T.; Rossouw, S.; Adhikari, T. The Good, the Bad and the Ugly of Lockdowns during Covid-19. PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Ogden, R. Distortions to the Passage of Time during England’s Second National Lockdown: A Role for Depression. PLoS One 2021, 16. [Google Scholar] [CrossRef]
- Yamamura, E.; Tsutsui, Y. Impact of the State of Emergency Declaration for Covid-19 on Preventive Behaviours and Mental Conditions in Japan: Difference in Difference Analysis Using Panel Data. Covid Economics Vetted and Real-Time Papers 2020, 23, 303–324. [Google Scholar]
- WHO Coronavirus (COVID-19) Dashboard WHO Coronavirus Disease (COVID-19) Dashboard.
- Perez-Arce, F.; Angrisani, M.; Bennett, D.; Darling, J.; Kapteyn, A.; Thomas, K. COVID-19 Vaccines and Mental Distress. PLoS One 2021, 16, e0256406. [Google Scholar] [CrossRef]
- Pandey, K.; Thurman, M.; Johnson, S.D.; Acharya, A.; Johnston, M.; Klug, E.A.; Olwenyi, O.A.; Rajaiah, R.; Byrareddy, S.N. Mental Health Issues During and After COVID-19 Vaccine Era. Brain Res Bull 2021, 176, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Deng, Z.; Chen, M.; Yin, D.; Zheng, J.; Liu, Y.; Liu, X.; Zou, H.; Zhang, C.; Sun, C. Changes in Mental Health and Preventive Behaviors before and after COVID-19 Vaccination: A Propensity Score Matching (PSM) Study. Vaccines (Basel) 2021, 9. [Google Scholar] [CrossRef]
- Japan Times Japan Gives First COVID-19 Vaccines to Health Workers. Japan Times 2021.
- Mantzari, E.; Rubin, G.J.; Marteau, T.M. Is Risk Compensation Threatening Public Health in the Covid19 Pandemic? BMJ 2020, 370, m2913. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Benefit of COVID-19 Vaccination Accounting for Potential Risk Compensation. NPJ Vaccines 2021, 6. [Google Scholar] [CrossRef]
- Trogen, B.; Caplan, A. Risk Compensation and COVID-19 Vaccines. Ann Intern Med 2021, 174, 858–859. [Google Scholar] [CrossRef]
- Rubin, G.J.; Brainard, J.; Hunter, P.; Michie, S. Are People Letting down Their Guard Too Soon after Covid-19 Vaccination? BMJ Opinion 2021. [Google Scholar]
- Morikawa, M. COVID-19, Vaccination, and Consumper Behavior; RIETI; 2021.
- Sunohara, S.; Asakura, T.; Kimura, T.; Ozawa, S.; Oshima, S.; Yamauchi, D.; Tamakoshi, A. Effective Vaccine Allocation Strategies, Balancing Economy with Infection Control against COVID-19 in Japan. PLoS One 2021, 16, e0257107. [Google Scholar] [CrossRef]
- Wooldridge, J. Introductory Econometrics; 4th ed.; South-Western Cengage Learning, 2009.
- Hsiao, C. Aalysis of Panel Data; Cambridge University Press: New York, 1986. [Google Scholar]
- Baltagi, B. Econometric Analysis of Panel Data; John Wiley & Sons: New York, 1995. [Google Scholar]
- Nagasu, M.; Yamamoto, I. Impact of Socioeconomic- And Lifestyle-Related Risk Factors on Poor Mental Health Conditions: A Nationwide Longitudinal 5-Wave Panel Study in Japan. PLoS One 2020, 15. [Google Scholar] [CrossRef]
- Wooldridge, J. Econometric Analysis of Cross Section and Panel Data; MIT Press: Cambridge, 2002. [Google Scholar]
- Greene, W. Econometric Analysis, 6th ed.; Pearson, Preantice Hall: New York, 2008. [Google Scholar]
- Yamamura, E.; Tsutsui, Y. The Impact of Closing Schools on Working from Home during the COVID-19 Pandemic: Evidence Using Panel Data from Japan. Rev Econ Househ 2021, 19, 41–60. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I. The Health Belief Model and Preventive Behavior. Health Education & Behavior 1974, 2, 27–59. [Google Scholar]
- Rosenstock, I.; Strecher, V.; Becker, M. Social Learning Theory and the Health Belief Model. Health Education & Behavior 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Asri, A.; Asri, V.; Renerte, B.; Föllmi-Heusi, F.; Leuppi, J.D.; Muser, J.; Nüesch, R.; Schuler, D.; Fischbacher, U. Wearing a Mask-For Yourself or for Others? Behavioral Correlates of Mask Wearing among COVID-19 Frontline Workers. PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Travis, J.; Harris, S.; Fadel, T.; Webb, G. Identifying the Determinants of COVID-19 Preventative Behaviors and Vaccine Intentions among South Carolina Residents. PLoS One 2021, 16, e0256178. [Google Scholar] [CrossRef]
- Japan Times 75% of Japan’s Older Residents Have Received First COVID-19 Vaccine Shot. Japan Times 2021.
- Japan Times Japan to Start COVID-19 Vaccinations at Workplaces and Universities on June 21. Japan Times 2021.
- Department of Medical Genome Sciences, R.I. for F.M.S.M.U.S. of M.JAPAN. Transition of COVID-19 Vaccination Rates by Country.
- Rose, G. The Determinants of Individual Cases Sick Individuals and Sick Populations; 2001; Vol. 30.
- Cheng, K.K.; Lam, T.H.; Leung, C.C. Wearing Face Masks in the Community during the COVID-19 Pandemic: Altruism and Solidarity. The Lancet 2020. [CrossRef] [PubMed]
- Powdthavee, N.; Riyanto, Y.E.; Wong, E.C.L.; Yeo, J.X.W.; Chan, Q.Y. When Face Masks Signal Social Identity: Explaining the Deep Face-Mask Divide during the COVID-19 Pandemic. PLoS One 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Weisel, O. Vaccinationasasocialcontract:ThecaseofCOVID-19 and US Political Partisanship. Proc Natl Acad Sci U S A 2021, 118. [Google Scholar]
- Agüero, J.; Beleche, T. Health Shocks and Their Long-Lasting Impact on Health Behaviors: Evidence from the 2009 H1N1 Pandemic in Mexico. J Health Econ 2017, 54, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Health Experts of UNICEF What to Do before, during and after Getting Vaccinated for COVID-19.
- Allcott, H. Social Norms and Energy Conservation. J Public Econ 2011, 95, 1082–1095. https://doi.org/0/?tab=wm&ogbl#inbox.
- Allcott, H.; Knittel, C. Are Consumers Poorly Informed about Fuel Economy? Evidence from Two Experiments. Am Econ J Econ Policy 2019, 11, 1–37. [Google Scholar] [CrossRef]
- Sasaki, S.; Kurokawa, H.; Ohtake, F. Effective but Fragile? Responses to Repeated Nudge-Based Messages for Preventing the Spread of COVID-19 Infection. Japanese Economic Review 2021, 72, 371–408. [Google Scholar] [CrossRef] [PubMed]
- Zeballos Rivas, D.R.; Lopez Jaldin, M.L.; Nina Canaviri, B.; Portugal Escalante, L.F.; Alanes Fernández, A.M.C.; Aguilar Ticona, J.P. Social Media Exposure, Risk Perception, Preventive Behaviors and Attitudes during the COVID-19 Epidemic in La Paz, Bolivia: A Cross Sectional Study. PLoS One 2021, 16, e0245859. [Google Scholar] [CrossRef] [PubMed]
- Muto, K.; Yamamoto, I.; Nagasu, M.; Tanaka, M.; Wada, K. Japanese Citizens’ Behavioral Changes and Preparedness against COVID-19: An Online Survey during the Early Phase of the Pandemic. PLoS One 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Desrichard, O.; Desrichard@unige, O.; Moussaoui, L.; Ofosu, N. Do Vaccinated People Reduce Their Precautionary Behaviours? A Test on a British Cohort. 2021. [Google Scholar] [CrossRef]
- Wright, L.; Steptoe, A.; Mak, H.W.; Fancourt, D. Do People Reduce Compliance with COVID-19 Guidelines Following Vaccination? A Longitudinal Analysis of Matched UK Adults. Journal of Epidemiology & Community Health (Forthcoming), 2021. [Google Scholar] [CrossRef]
- Korn, L.; Böhm, R.; Meier, N.W.; Betsch, C. Vaccination as a Social Contract. PNAS 2020, 117, 14890–14899. [Google Scholar] [CrossRef]
- Chan, Y. Eugene Moral Foundations Underlying Behavioural Compliance during the COVID-19 Pandemic. Pers Individ Dif 2021, 171. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Lippke, S.; Liang, W.; Shang, B.; Keller, F.M.; Wagner, P.; Baker, J.S.; He, J. Association of Social-Cognitive Factors with Individual Preventive Behaviors of COVID-19 among a Mixed-Sample of Older Adults from China and Germany. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef]
- Li, F.; Liang, W.; Rhodes, R.E.; Duan, Y.; Wang, X.; Shang, B.; Yang, Y.; Jiao, J.; Yang, M.; Supriya, R.; et al. A Systematic Review and Meta-Analysis on the Preventive Behaviors in Response to the COVID-19 Pandemic among Children and Adolescents. BMC Public Health 2022, 22. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Duan, Y.; Li, F.; Rhodes, R.E.; Wang, X.; Peiris, D.L.I.H.K.; Zhou, L.; Shang, B.; Yang, Y.; Baker, J.S.; et al. Psychosocial Determinants of Hand Hygiene, Facemask Wearing, and Physical Distancing during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Annals of Behavioral Medicine 2022, 56, 1174–1187. [Google Scholar] [CrossRef] [PubMed]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S.; Stowe, J.; Tessier, E.; Groves, N.; Dabrera, G.; et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. New England Journal of Medicine 2021, 385, 585–594. [Google Scholar] [CrossRef]
- Duan, Y.; Shang, B.; Liang, W.; Lin, Z.; Hu, C.; Baker, J.S.; Wang, Y.; He, J. Predicting Hand Washing, Mask Wearing and Social Distancing Behaviors among Older Adults during the Covid-19 Pandemic: An Integrated Social Cognition Model. BMC Geriatr 2022, 22. [Google Scholar] [CrossRef]
| Variables | Definition |
| Dependent variables | |
| STAYING INDOORS | In the last week, how consistent were you at “not going out of home?” Please choose among 5 choices. 1 (not completed at all) to 5 (completely consistent). |
| NOT GOING TO WORK | In the last week, how consistent were you at “not going out to work (or school)?” Please choose among 5 choices. 1 (not completed at all) to 5 (completely achieved). |
| NOT FOR LEISURE | In the last week, how consistent were you at “not going out to events or travel?” Please choose among 5 choices. 1 (not completed at all) to 5 (completely achieved). |
| HANDWASHING | In the last week, how consistent were you at “washing your hands?” Please choose among 5 choices. 1 (not completed at all) to 5 (completely achieved). |
| WEARING MASK | In the last week, how consistent were you at “wearing a mask?” Please choose among 5 choices. 1 (not completed at all) to 5 (completely achieved). |
| Confounders (Independent variables) | |
| VACCINE FIRST | Did you get the first shot (but not yet the second one)? 1 (Yes) or 0 (No) |
| VACCINE SECOND | Did you get the second shot? 1 (Yes) or 0 (No) |
| VACCINE SECOND_1 | Did you get the second shot in this month? 1 (Yes) or 0 (No) |
| VACCINE SECOND_2 | Did you get the second shot last month? 1 (Yes) or 0 (No) |
| VACCINE SECOND_3 | Did you get the second shot two months ago? 1 (Yes) or 0 (No) |
| VACCINE SECOND_4 | Did you get the second shot three months ago? 1 (Yes) or 0 (No) |
| PROB_COVID19 | What percentage do you think the probability of your taking the COVID-19? 0 to 100 (%) |
| SEVERITY COVID19 | How serious are your symptoms if you are infected with the novel coronavirus? Choose from 6 choices. 1 (very small influence) to 6 (death) |
| EMERGENCY | Is your area under a state of emergency. 1 (Yes) or 0 (No) |
| FEAR | How intense is your feeling of fear? Please answer in a scale from 1 (I have not felt this emotion at all) to 5 (I have felt this emotion strongly). |
| ANXIETY | How intense is your feeling of anxiety? Please answer in a scale from 1 (I have not felt this emotion at all) to 5 (I have felt this emotion strongly). |
| ANGER | How intense is your feeling of anger? Please answer in a scale from 1 (I have not felt this emotion at all) to 5 (I have felt this emotion strongly). |
| AGE | Ages |
| MALE | Select 1 if you are male and 0 if otherwise. |
| UNIVERSITY | Select 1 if you graduated from university and 0 if otherwise. |
| Waves | Obs. | Loss rate % |
| 1 | 4,359 | 0 |
| 2 | 3,495 | 19.8 |
| 3 | 4,013 | 7.9 |
| 4 | 3,996 | 8.3 |
| 5 | 3,877 | 11.1 |
| 6 | 3,626 | 16.8 |
| 7 | 3,491 | 19.9 |
| 8 | 3,509 | 19.5 |
| 9 | 3,529 | 19.0 |
| 10 | 3,440 | 21.1 |
| 11 | 3,304 | 24.2 |
| 12 | 3,280 | 24.8 |
| 13 | 3,392 | 22.2 |
| 14 | 3,349 | 23.2 |
| 15 | 3,347 | 23.2 |
| Variables | Mean | s.d. |
| STAYING INDOORS | 2.91 | 1.25 |
| NOT GOING TO WORK | 2.94 | 1.73 |
| NOT FOR LEISURE | 4.12 | 1.18 |
| HANDWASHING | 4.14 | 0.95 |
| WEARING MASK | 4.41 | 1.05 |
| VACCINE FIRST | 0.03 | 0.17 |
| VACCINE SECOND | 0.06 | 0.24 |
| VACCINE SECOND_1 | 0.03 | 0.18 |
| VACCINE SECOND_2 | 0.02 | 0.14 |
| VACCINE SECOND_3 | 0.01 | 0.08 |
| VACCINE SECOND_4 | 0.001 | 0.04 |
| PROB_COVID19 | 20.4 | 22.3 |
| SEVERITY COVID19 | 3.57 | 1.21 |
| EMERGENCY | 0.29 | 0.45 |
| FEAR | 3.06 | 1.14 |
| ANXIETY | 3.28 | 1.15 |
| ANGER | 2.98 | 1.10 |
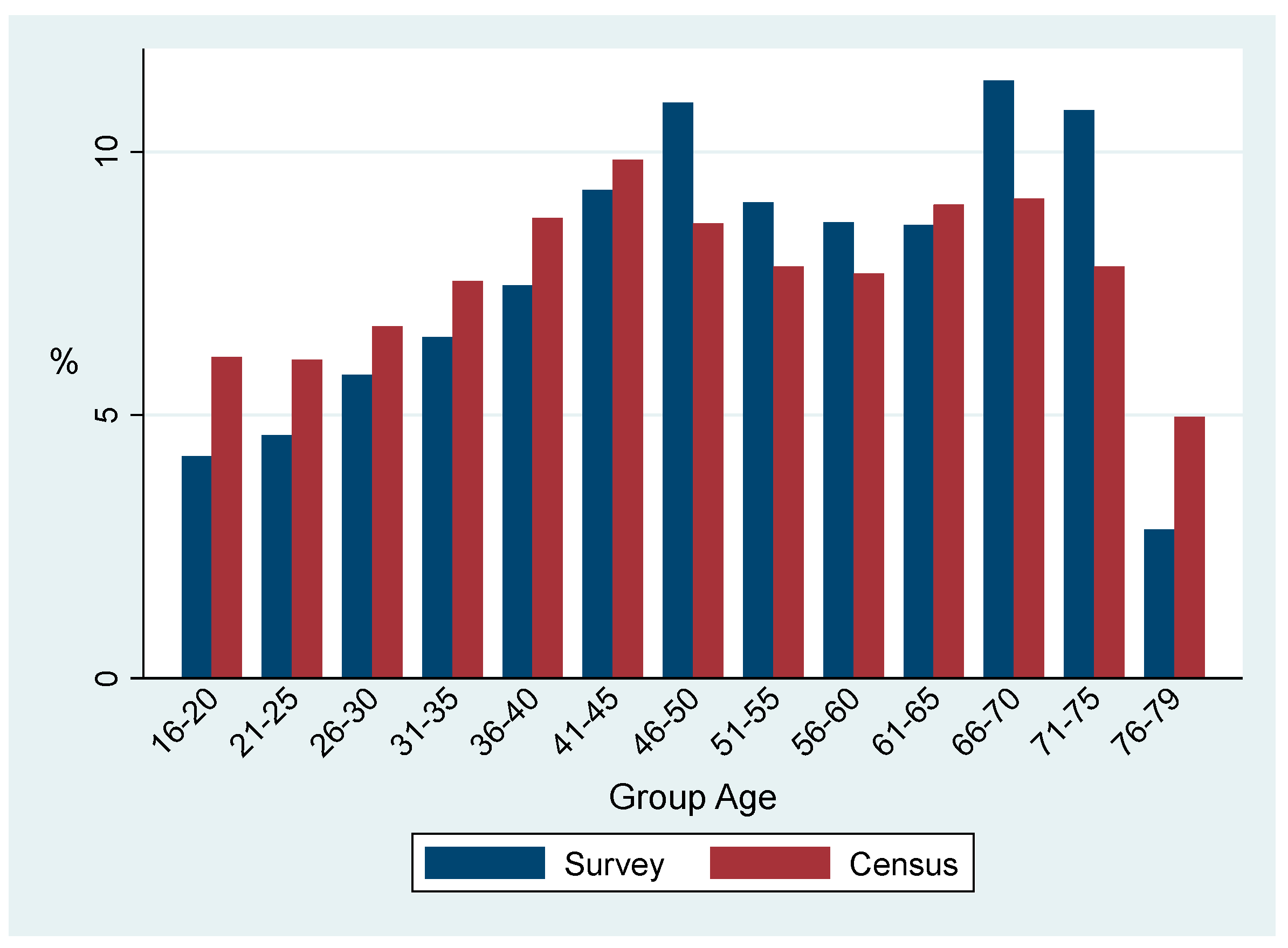
| AGE | 48.7 | 17.3 |
| MALE | 0.50 | 0.50 |
| UNIVERSITY | 0.43 | 0.49 |
| Waves | Dates | All % |
Age>40 % |
Age<=40 % |
| 1 | March 13–16, 2020 | 0 | 0 | 0 |
| 2 | March 27–30, 2020 | 0 | 0 | 0 |
| 3 | Apr. 10–13, 2020 | 0 | 0 | 0 |
| 4 | May 8–11, 2020 | 0 | 0 | 0 |
| 5 | June 12–15, 2020 | 0 | 0 | 0 |
| 6 | Oct 23–28, 2020 | 0 | 0 | 0 |
| 7 | Dec 4–8, 2020 | 0 | 0 | 0 |
| 8 | Jan. 15–19, 2021 | 0 | 0 | 0 |
| 9 | Feb. 17–22, 2021 | 0 | 0 | 0 |
| 10 | Mar. 24–29, 2021 | 0 | 0 | 0 |
| 11 | Apr. 23–26, 2021 | 0 | 0 | 0 |
| 12 | May 28–31, 2021 | 8.2 | 9.1 | 5.4 |
| 13 | June 25–30, 2021 | 25.1 | 30.7 | 7.8 |
| 14 | July 30–Aug 4, 2021 | 50.0 | 58.3 | 23.8. |
| 15 | Aug 27–Sep. 1, 2021 | 64.2 | 72.3 | 39.5 |
| Dates | Before (1) |
After (2) |
Difference (2) – (1) |
|
STAYING INDOORS |
2.96 | 3.11 | 0.14*** (0.10-0.18) |
|
NOT GOING TO WORK |
3.03 | 3.22 | 0.19*** (0.13-0.24) |
|
NOT FOR LEISURE |
4.21 | 4.32 | 0.10*** (0.07-0.14) |
|
HANDWASHING |
4.19 | 4.36 | 0.16*** (0.13-0.19) |
|
WEARING MASK |
4.45 | 4.75 | 0.29*** (0.26-0.32) |
| (1) STAYING INDOORS |
(2) NOT GOING TO WORK |
(3) NOT FOR LEISURE |
(4) HANDWASHING |
(5) WEARING MASK |
|
| VACCINE FIRST | 0.057** (0.007-0.106) |
0.032 (−0.016-0.080) |
0.027 (−0.014-0.069) |
0.026* (−0.001-0.054) |
−0.001 (−0.047-0.045) |
| VACCINE SECOND_1 | 0.099*** (0.058-0.140) |
0.070** (0.007-0.132) |
0.077*** (0.031-0.122) |
0.006 (−0.029-0.041) |
−0.006 (−0.046-0.034) |
| VACCINE SECOND_2 | 0.123*** (0.061-0.187) |
0.123*** (0.042-0.204) |
0.106*** (0.047-0.165) |
−0.012 (−0.051-0.027) |
−0.0003 (−0.048-0.047) |
| VACCINE SECOND_3 | 0.097 (−0.023-0.217) | 0.092 (−0.020-0.206) |
0.018 (−0.097-0.133) |
0.035 (−0.023-0.095) |
−0.027 (−0.094-0.040) |
| VACCINE SECOND_4 | 0.014 (−0.335-0.365) |
−0.019 (−0.167-0.128) |
−0.106 (−0.341-0.128) |
−0.018 (−0.142-0.105) |
−0.040 (−0.177-0.095) |
| PROBABILITY COVID19 | −0.291 (−1.064-0.480) |
−0.532 (−1.657-0.591) |
0.103 (−0.328-0.535) |
0.428* (−0.079-0.936) |
−0.472 (−1.208-0.263) |
| SEVERITY COVID19 | 0.016*** (0.007-0.026) |
0.017* (−0.001-0.036) |
0.036*** (0.019-0.053) |
0.018*** (0.006-0.030) |
0.033*** (0.021-0.045) |
|
EMERGENCY |
0.022 (−0.008-0.054) |
0.034** (0.007-0.062) |
0.047*** (0.017-0.078) |
−0.001 (−0.016-0.014) |
0.013 (−0.002-0.020) |
|
ANGER |
0.035*** (0.025-0.046) |
0.023*** (0.007-0.039) |
0.054*** (0.038-0.069) |
0.018*** (0.009-0.027) |
0.009 (−0.002-0.020) |
|
FEAR |
0.051*** (0.035-0.066) |
0.031*** (0.009-0.053) |
0.045*** (0.024-0.067) |
0.018*** (0.007-0.028) |
0.036*** (0.021-0.052) |
|
ANXIETY |
0.037*** (0.023-0.051) |
0.021* (−0.001-0.044) |
0.049*** (0.034-0.063) |
0.026*** (0.015-0.036) |
0.029*** (0.012-0.047) |
| WAVE 1 | <Default> | ||||
|
WAVE 2 |
0.126*** (0.085-0.167) | 0.092*** (0.048-0.137) |
0.170*** (0.113-0.226) |
0.043** (0.009-0.077) |
0.047*** (0.016-0.079) |
|
WAVE 3 |
0.446*** (0.355-0.536) |
0.273*** (0.181-0.365) |
0.516*** (0.450-0.582) |
0.177*** (0.144-0.210) |
0.386*** (0.332-0.440) |
|
WAVE 4 |
0.829*** (0.738-0.920) | 0.687*** (0.592-0.782) |
0.698*** (0.622-0.773) |
0.329*** (0.286-0.373) |
0.833*** (0.755-0.915) |
|
WAVE 5 |
0.435*** (0.353-0.517) |
0.269*** (0.185-0.354) |
0.517*** (0.456-0.577) |
0.289*** (0.260-0.318) |
0.862*** (0.802-0.924) |
|
WAVE 6 |
0.052 (−0.014-0.119) |
−0.010 (−0.082-0.060) |
0.025 (−0.038-0.090) |
0.237*** (0.203-0.272) |
1.010 (0.942-1.079) |
|
WAVE 7 |
0.161*** (0.101-0.221) | 0.017 (−0.046-0.081) |
0.157*** (0.108-0.206) |
0.267*** (0.235-0.300) |
1.061*** (0.993-1.130) |
|
WAVE 8 |
0.389*** (0.307-0.470) |
0.141*** (0.061-0.220) |
0.458*** (0.391-0.525) |
0.317*** (0.278-0.356) |
1.122*** (1.040-1.204) |
|
WAVE 9 |
0.368*** (0.306-0.431) |
0.153*** (0.095-0.210) |
0.417*** (0.0357-0.477) |
0.319*** (0.274-0.365) |
1.146*** (1.068-1.224) |
|
WAVE 10 |
0.344*** (0.271-0.416) | 0.140*** (0.070-0.210) | 0.323*** (0.259-0.387) |
0.339*** (0.305-0.374) |
1.133*** (1.065-1.201) |
|
WAVE 11 |
0.304*** (0.239-0.369) |
0.132*** (0.071-0.192) |
0.373*** (0.309-0.436) |
0.336*** (0.300-0.372) |
1.126*** (1.053-1.198) |
|
WAVE 12 |
0.375*** (0.304-0.446) |
0.195*** (0.132-0.259) |
0.442*** (0.375-0509) |
0.363*** (0.322-0.405) |
1.139*** (1.064-1.213) |
|
WAVE 13 |
0.309*** (0.233-0.385) | 0.141*** (0.079-0.201) |
0.365*** (0.206-0.350) |
0.372*** (0.334-0.410) |
1.132*** (1.059-1.206) |
|
WAVE 14 |
0.282*** (0.207-0.357) |
0.156*** (0.078-0.232) | 0.278*** (0.206-0.350) |
0.355*** (0.315-0.395) |
1.111*** (1.036-1.185) |
|
WAVE 15 |
0.346*** (0.248-0.444) |
0.231*** (0.141-0.322) |
0.384*** (0.299-0.469) |
0.413*** (0.360-0.467) |
1.135*** (1.051-1.219) |
| Adj R2 Obs. |
0.37 54,007 |
0.65 54,007 |
0.37 54,007 |
0.62 54,007 |
0.49 54,007 |
| (1) STAYING INDOORS |
(2) NOT GOING TO WORK |
(3) NOT FOR LEISURE |
(4) HANDWASHING |
(5) WEARING MASK |
|
| VACCINE FIRST | 0.057** (0.007-1.077) | 0.032 (−0.015-0.080) |
0.028 (−0.014-0.069) |
0.028** (0.0003-0.057) | 0.003 (−0.044-0.050) |
| VACCINE SECOND | 0.107*** (0.059-0.154) |
0.090*** (0.028-0.152) |
0.079*** (0.0355-0.123) |
0.008 (−0.024-0.041) |
0.005 (−0.038-0.048) |
| Adj R2 Obs. |
0.52 54,007 |
0.66 54,007 |
0.37 54,007 |
0.62 54,007 |
0.49 54,007 |
| (1) STAYING INDOORS |
(2) NOT GOING TO WORK |
(3) NOT FOR LEISURE |
(4) HANDWASHING |
(5) WEARING MASK |
|
|
VACCINE FIRST |
|||||
| (Prob [y=1]) |
−0.019** (−0.036 - −0.003) |
−0.016 (−0.047 - 0.014) |
−0.003 (−0.011 - 0.004) |
−0.003** (−0.006 - −0.001) |
−0.009* (−0.019 - 0.0004) |
| (Prob [y=2) | −0.010** (−0.019 - −0.001) |
−0.017 (−0.004 - −0.001) |
−0.002 (−0.006 - 0.002) |
−0.007** (−0.013 - −0.001) |
−0.006* (−0.014 - 0.0003) |
| (Prob [y=3) | −0.0007** (−0.001 - −0.0001) |
0.0004 (−0.0003 - 0.001) |
−0.007 (−0.024 - 0.009) |
−0.022** (−0.041 - −0.003) |
−0.014* (−0.029 - 0.0006) |
| (Prob [y=4) | 0.019** (0.003 - 0.036) |
0.002 (−0.001-0.005) |
−0.002 (−0.005 - 0.002) |
−0.006** (−0.012 - −0.001) |
−0.015* (−0.032 - 0.007) |
| (Prob [y=5) | 0.011** (0.001 - 0.021) |
0.011 (−0.013-0.046) |
0.015 (−0.018 - 0.049) |
0.004** (0.007 - 0.073) |
0.047* (−0.002 - 0.096) |
|
VACCINE SECOND |
|||||
| (Prob [y=1]) |
−0.036*** (−0.054 - −0.018) |
−0.050*** (−0.084 - −0.015) |
−0.012*** (−0.020 - −0.004) |
−0.002 (−0.005 - 0.001) |
−0.014*** (−0.023 - −0.004) |
| (Prob [y=2) | −0.019*** (−0.029 - −0.009) |
−0.005*** (−0.008 - −0.001) |
−0.007*** (−0.011 - −0.002) |
−0.004 (−0.010 - 0.001) |
−0.010*** (−0.017 - −0.003) |
| (Prob [y=3) | −0.001*** (−0.002 - −0.0006) |
0.001*** (0.0003 - 0.002) |
−0.027*** (−0.043 - −0.010) |
−0.013 (−0.032 - 0.005) |
−0.021*** (−0.035 - −0.006) |
| (Prob [y=4) | 0.036*** (0.018 - 0.053) |
0.005*** (0.001 - 0.009) |
−0.006*** (−0.010 - 0.002) |
−0.004 (−0.009 - 0.002) |
−0.023*** (−0.039 - 0.006) |
| (Prob [y=5) | 0.021*** (0.010 - 0.031) |
0.048*** (0.015 - 0.081) |
0.053*** (0.020 - 0.086) |
0.023 (−0.010 - 0.057) |
0.068*** (0.020 - 0.115) |
| Wald-chi2 Obs. |
2,551 54,007 |
1,269 54,007 |
2,340 54,007 |
1,232 54,007 |
3,426 54,007 |
| (1) STAYING INDOORS |
(2) NOT GOING TO WORK |
(3) NOT FOR LEISURE |
(4) HANDWASHING |
(5) WEARING MASK |
|
| VACCINE FIRST | −0.095 (−0.127-0.108) |
−0.037 (−0.167 - 0.092) |
−0.025 (−0.143 - 0.093) |
−0.031 (−0.056 - 0.092) |
0.017 (−0.053 - 0.027) |
| VACCINE SECOND_1 | −0.106 (−0274 - 0.60) |
−0.249*** (−0.386 - −0.111) |
0.049 (−0.083 - 0.187) |
−0.060 (−0.068 - 0.111) |
0.021 (−0.059 - 0.025) |
| VACCINE SECOND_2 | −0.283** (−0.556 - −0.010) |
−0.392** (−0.594 - − 0.191) |
0.029 (−0.210 - 0.269) |
0.0002 (−0.069 - 0.176) |
0.053 (−0.074 - 0.031) |
| VACCINE SECOND_3 | −0.288* (−0.600 - 0.022) |
−0.347* (−0.713 – 0.017) |
−0.079 (−0.337 - 0.179) |
−0.053 (−0.129 - 0.413) |
0.142 (−0.101 - 0.013) |
| VACCINE SECOND_4 | −0.467 (−1.086 - 0.151) |
−0.615*** (− 0.875 - −0.355) |
−0.140 (−0.740 - 0.458) |
0.004 (−0.116 - 0.245) |
0.064 (−0.243 - 0.088) |
| Adj R2 Obs. |
0.49 15,407 |
0.56 15,407 |
0.37 15,407 |
0.52 15,407 |
0.58 15,407 |
| (1) STAYING INDOORS |
(2) NOT GOING TO WORK |
(3) NOT FOR LEISURE |
(4) HANDWASHING |
(5) WEARING MASK |
|
| VACCINE FIRST | 0.036 (−0.022 - 0.095) |
0.026 (−0.034 - 0.086) |
0.013 (−0.030 - 0.056) |
0.024* (−0.003 - 0.051) |
− 0.012 (−0.003 - 0.051) |
| VACCINE SECOND_1 | 0.089*** (0.036 - 0.143) |
0.105** (0.040 - 0.170) |
0.051* (−0.001 - 0.103) |
−0.001 (−0.046 - 0.043) |
−0.016 (−0.046 - 0.043) |
| VACCINE SECOND_2 | 0.120*** (0.053 - 0.187) |
0.175*** (0.097 - 0.252) |
0.084*** (0.023 - 0.144) |
−0.024 (−0.074 - 0.025) |
−0.021 (−0.074 - 0.025) |
| VACCINE SECOND_3 | 0.118* (− 0.002 - 0.239) |
0.170*** (0.058 - 0.282) |
0.005 (− 0.123 - 0.135) |
0.012 (−0.052 - 0.078) |
−0.043 (−0.052 - 0.078) |
| VACCINE SECOND_4 | 0.131 (−0.219 - 0.481 ) |
0.167* (−0.024 - 0.358) |
−0.123 (−0.384 - 0.136) |
−0.048 (−0.211 - 0.115) |
−0.077 (−0.211 - 0.115) |
| Adj R2 Obs. |
0.52 38,600 |
0.68 38,600 |
0.35 38,600 |
0.63 38,600 |
0.53 38,600 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





