1. Introduction
The 2019 novel coronavirus infection (COVID-19) changed the profile of patients seeking primary medical assistance. Concomitant injury to the lungs and myocardium in COVID-19 was observed using MRI in the very beginning of COVID-19 pandemic [
1,
2,
3,
4]. Recent data showed that the number of patients with heart problems indeed significantly increased during COVID-19 pandemic [
5,
6,
7,
8]. Most patients reported recent respiratory illness and confirmed COVID-19 infection caused by SARS-CoV-2 virus. Numerous studies focused on the possible mechanisms of damage to the cardiovascular system after COVID-19 [
6,
9,
10]. However, precise pathophysiological mechanisms remain poorly understood. From the very beginning of COVID-19 pandemic, magnetic resonance imaging (MRI) data suggested that COVID-19-associated damage occurs due to cellular and circulating factors present not only in the pulmonary parenchyma itself, but also in the vascular wall, myocardium [
11,
12], and brain tissue [
13]. A significant number of patients have been suffering from persisting symptoms even months following COVID-19 [
2,
5,
14] though the availability of effective vaccines resulted in a decrease in the burden of acute coronavirus infection [
15,
16].
In regard to cardiac health, diagnostic algorithms for COVID-19 typically aim at ruling out the inflammatory changes in the myocardium. At the same time, the incidence of other nosological entities, in particular, cardiomyopathy progressively increases. Contrast-enhanced cardiac MRI (CE-CMR) is considered the method of choice for instrumental diagnostics of cardiological pathology according to the recommendations of the European Society of Cardiology and American Heart Association [
17,
18], and Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection [
1]. Indeed, our previous data showed that CE-CMR allows to detect cardiac involvement in about 37% of patients with tomography-documented lung injury, and vast majority of these patients have multiple focal lesions [
13]. Considering that SARS-CoV-2 virulence and clinical manifestation of COVID-19 are fluctuating with time, continuous monitoring and development of effective strategy and tactics for administering the diagnostic procedures is required.
On the other hand, little is known about the experience, availability, and attitudes of population to MRI and other medical imaging modalities, while the administration of these methods represents essential resource for timely diagnosis and continuing monitoring of acute and chronic COVID-19. Considering that majority of population suffered from confirmed or unconfirmed COVID-19 infection with potential chronic complications, which may significantly differ from those of ordinary cold and may be severe, it is essential to understand the impact of COVID-19 pandemic on cardiac health of population and the ways to timely diagnosis and control of disease. The aim of the study was to gain insight into the epidemiology of MRI administration during COVID-19 pandemic with emphasis of COVID-19 impact on cardiac health.
2. Materials and Methods
The study was performed in accordance with the standards of Good Clinical Practice and the Declaration of Helsinki. Research comprised two cohorts from Tomsk and Tomsk Region. Two methodological approaches were used in two cohorts to provide integrative evaluation of epidemiology aspects of MRI administration during COVID-19 pandemic. The study comprised a total of 1,714 depersonalized residents of Tomsk and Tomsk Region whose estimated population was 1,062,726 people as of 2022.
Cohort 1 (
n = 727). The invitations to fill in the originally developed online questionnaire were distributed among the residents of Tomsk and Tomsk Region. A total of 78,317 target SMS messages were sent to deidentified residents using Target-SMS service provided by the telecommunication company Tele2 Russia with delivery rate of 77.4%, and 60,575 people received the invitations to fill in the originally developed online questionnaire available on the website
www.zdorov.tpu.ru at the time of survey. Mobile and PC versions of the website were available. The invitees were selected automatically based on the following criteria: (1) they agreed to receive target SMS messages from their mobile provider while concluding the agreement with the operator of mobile service; (2) they had Android or iOS device; (3) they resided in the Tomsk Region at the time of obtaining the Subscriber Identity Module card; (4) they agreed to participate in the survey; and (5) they left digital footprint via electronic media associated with healthcare and pharmacy within 90 days. The initial response rate, measured as the percentage of respondents who accepted the invitation and visited the website, was 3.2% (
n = 1,956); 1.8% of them (
n = 1,057) registered for taking the survey; 727 individuals validly completed the survey questionnaire so the response rate eventually settled down at 1.2%. The survey questionnaire presented the questions on demographic, social, behavioral, clinical, pharmacological factors as well as people’s experience and attitudes to diagnostic imaging relevant to COVID-19 pandemic. The present study investigated the answers given to selective set of questions including the questions on age, gender, history of COVID-19 and acute respiratory infections, presence of chronic diseases, experience, and attitudes to diagnostic imaging with emphasis on MRI (
Table 1).
Cohort 2 (n = 987). The retrospective observational cohort study was performed to analyze MRI data of 8,137 MRI studies performed in Cardiology Research Institute of Tomsk NRMC from January 01, 2019 to June 01, 2022. Cohort 2 comprised patients who underwent CE-CMR (n = 987). Referrals, clinical characteristics, diagnosis, gender, age, type of visit, MRI study protocols, and MRI data were analyzed. The CMR examinations comprised 12.13% of these studies. Inclusion criteria were age from 0 to 90 years, indications for CE-CMR study, and MRI of the heart performed within the above-mentioned period. Exclusion criteria were contraindications for paramagnetic contrast enhancement, implantation of artificial pacemaker, ferromagnetic clips in the brain and spinal cord, the presence of any foreign object partially or completely within the orbit, with or without penetration or perforation of the globe, implanted automatic drug dispensers, severe heart rhythm disorder, large joint prosthesis, the first trimester of pregnancy, claustrophobia. Medical records with the results of CMR examinations were acquired from the electronic module, previously designed to store data of instrumental studies. Data contained standard information of CMR report including patient demographic and clinical data, characteristics of CMR procedure, suspected diagnosis, verified diagnosis, and type of examination (inpatient or outpatient). Patients received standard diagnostic CE-CMR procedure using 1.5-tesla MRI system Vantage Titan 1.5T (Toshiba Medical Systems) with ECG and breathing synchronization and myocardial image acquisition along the short and long axes before and after administration of gadolinium-based contrast agent gadobutrol (Gadovist, Gadobuskan). The thickness of slices was 5–7 mm with recording the images into 256 × 256 matrix. Protocol of CRM study included Т1-, Т2-weighted sequences with fat tissue signal suppression for evaluation of myocardial condition, dynamic SSFP-sequences for assessment of the volumes and function of the left ventricle, gradient inversion recovery sequences (GR-IR) for detection of areas with pathologic contrasting. Inversion time was adjusted individually (on average TI = 300 ± 10 ms). Evaluation of affected areas in the myocardium was done using 17-segment system of topical characterization of the left ventricular myocardium. Statistical processing of data was done using STATISTICA 10 software; graphics and diagrams were created using Microsoft Excel 2010. Qualitative parameters are described as relative frequencies in percentage. Significance of differences between the groups of qualitative variables was assessed by Pearson's chi-squared test. Values were considered statistically significant when P was < 0.05.
The study was supported by grant of the Russian Science Foundation (project # 22-15-00313) with regard to study design, data acquisition, data analysis, data interpretation, and publication of research results.
3. Results
This section may be divided by subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
3.1. Online Survey (Cohort 1)
The respondents enrolled in the online survey (n = 727) aged 44.8 ± 14.9 years, and majority of them were female (74%). Only 28% of respondents felt well while 61% of respondents reported slight malady, and 11% felt unwell at the time of survey.
Cardiovascular disease reported 31% of respondents; 8.7% of people had chronic respiratory pathology; 29% of people in the survey considered themselves free of any chronic diseases. Among Cohort 1 individuals, the last respiratory infection occurred within one month in 29%, within one year in 45%, and over one year ago in 14%. 1.7% reported no respiratory infections in past history while 11% had respiratory infection at the time of survey. Over half of respondents (52%) had history of confirmed COVID-19 infection; 64% of respondents were vaccinated against COVID-19, and 41% of respondents were vaccinated against other infections within five years.
While comparing the informativeness of diagnostic imaging modalities, 26% of respondents considered MRI the most informative method for detecting COVID-19-associated pneumonia. Computed tomography (CT), fluorography, X-ray, and scintigraphy were considered the best choice by 62%, 24%, 18%, and 1.9% of respondents, respectively.
About 10% of respondents used to receive diagnostic imaging procedures (MRI, CT, and ultrasound) on privately paid basis while 28% of people in the survey were unable to pay for diagnostic imaging procedures by themselves. 12% of respondents reported unavailability of MRI in their neighborhood. MRI was available and covered by compulsory health insurance in the place of residence with waiting time of two to four weeks in 25% and without the need to wait in 6.7% in Cohort 1. Privately paid MRI was available in the place of residence with waiting time of two to four weeks in 15% and without the need to wait in 41% of respondents.
For the past two years, respondents received the following diagnostic imaging examinations: fluorography (76%), ultrasound (69%), X-ray (41%), MRI (29%), CT (25%), and scintigraphy (1.5%). No diagnostic procedures within two past years reported 5.8% of respondents.
The detailed answers of the respondent are presented in
Table 1.
3.2. CE-CMR findings and pattern of administration (Cohort 2)
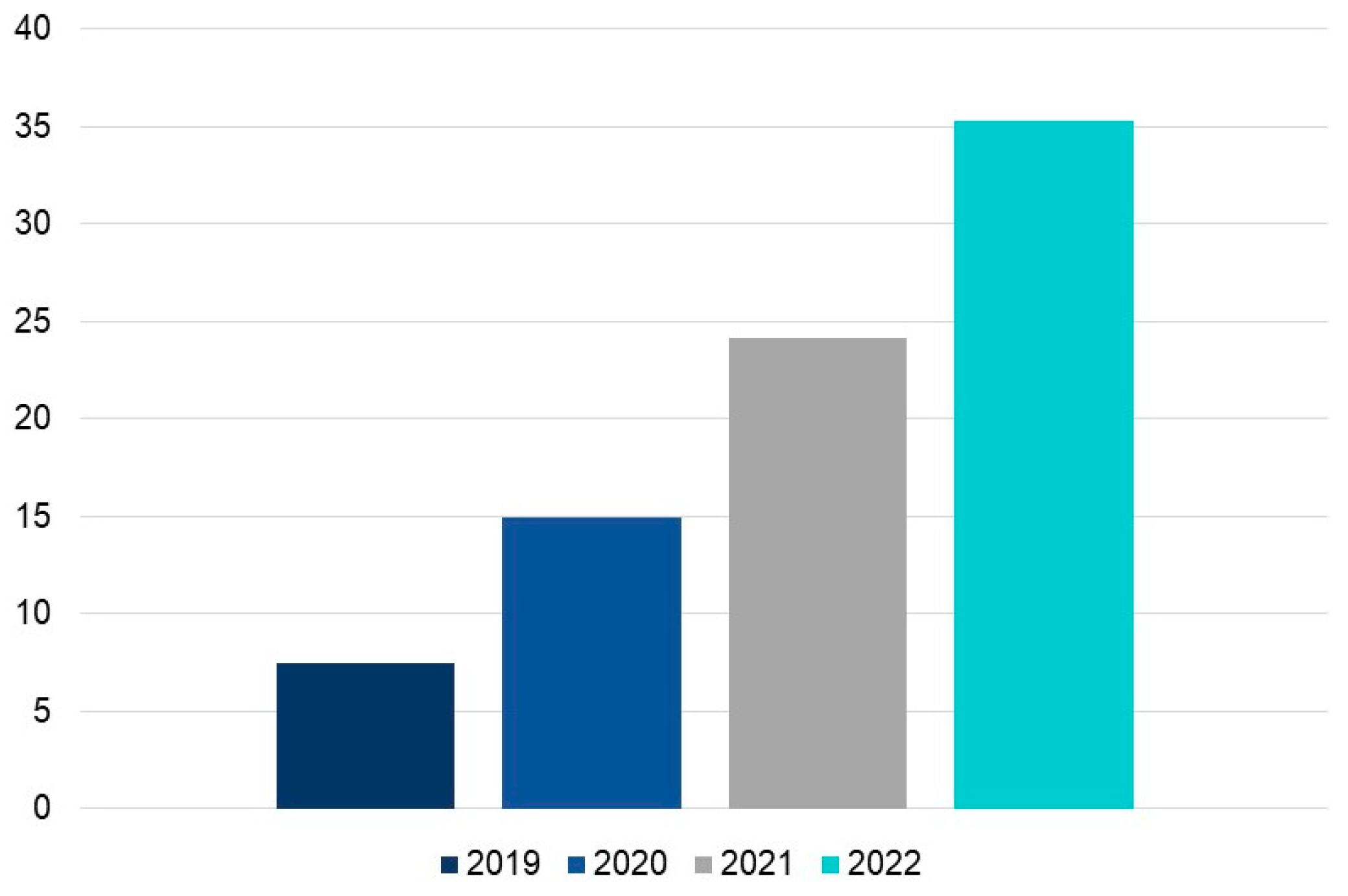
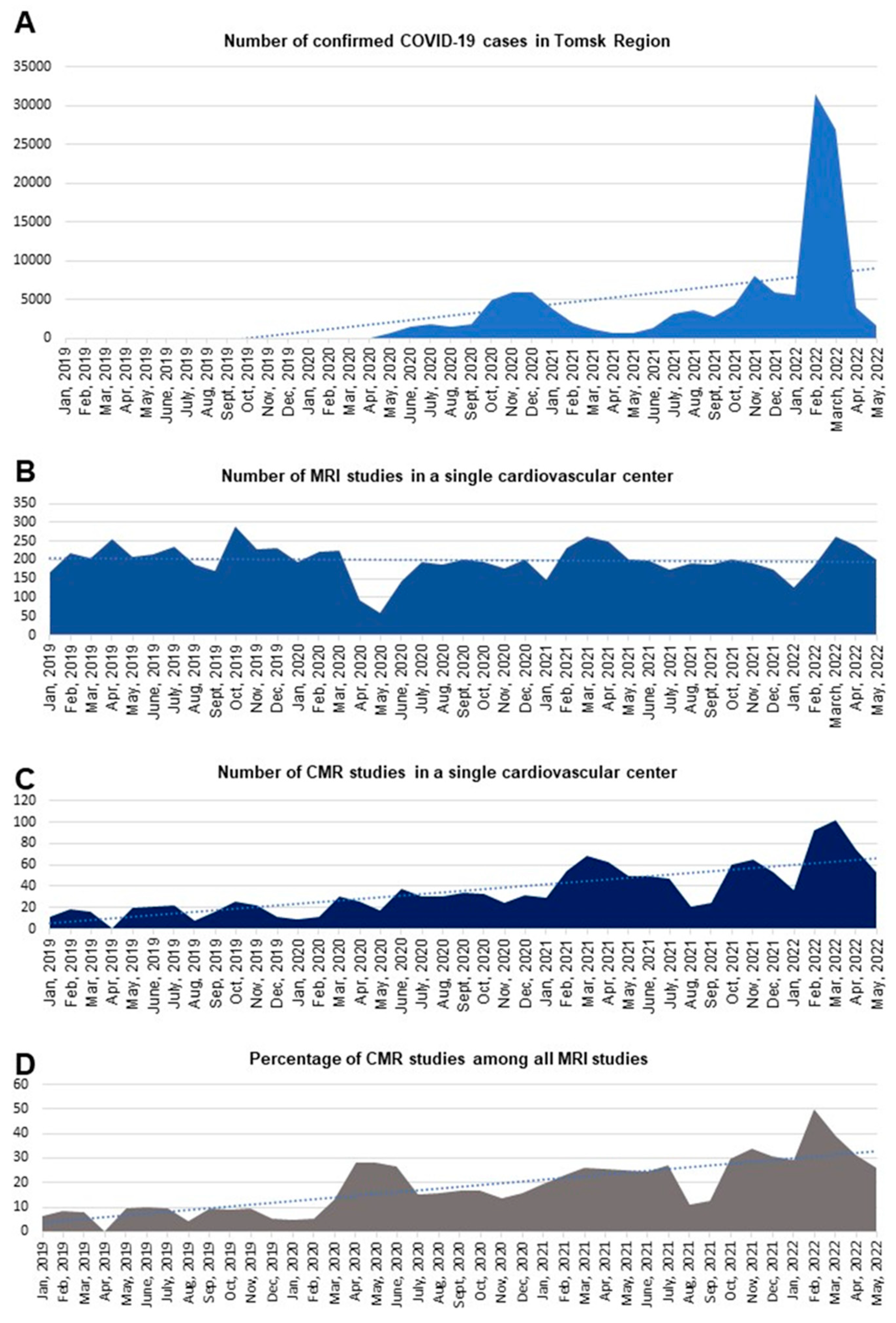
A year-by-year distribution of CMR procedures in our study was as follows: 198 studies (20.1%) were performed in 2019; 232 studies (23.5%) were done in 2020; 330 examinations (33.4%) were performed in 2021; and 227 studies (23%) were done within the first six months of 2022 (n = 987). Besides a significant increase in the absolute number of CMR procedures, the annual proportion of these studies increased and continued to increase among the total number of MRI exams (
p < 0.05). Our study showed a rise in the number of outpatients: 32 (16%) in 2019, 68 (29%) in 2020, 57 (17%) in 2021, and 40 patients (18%) during the first six months of 2022 (
Figure 1).
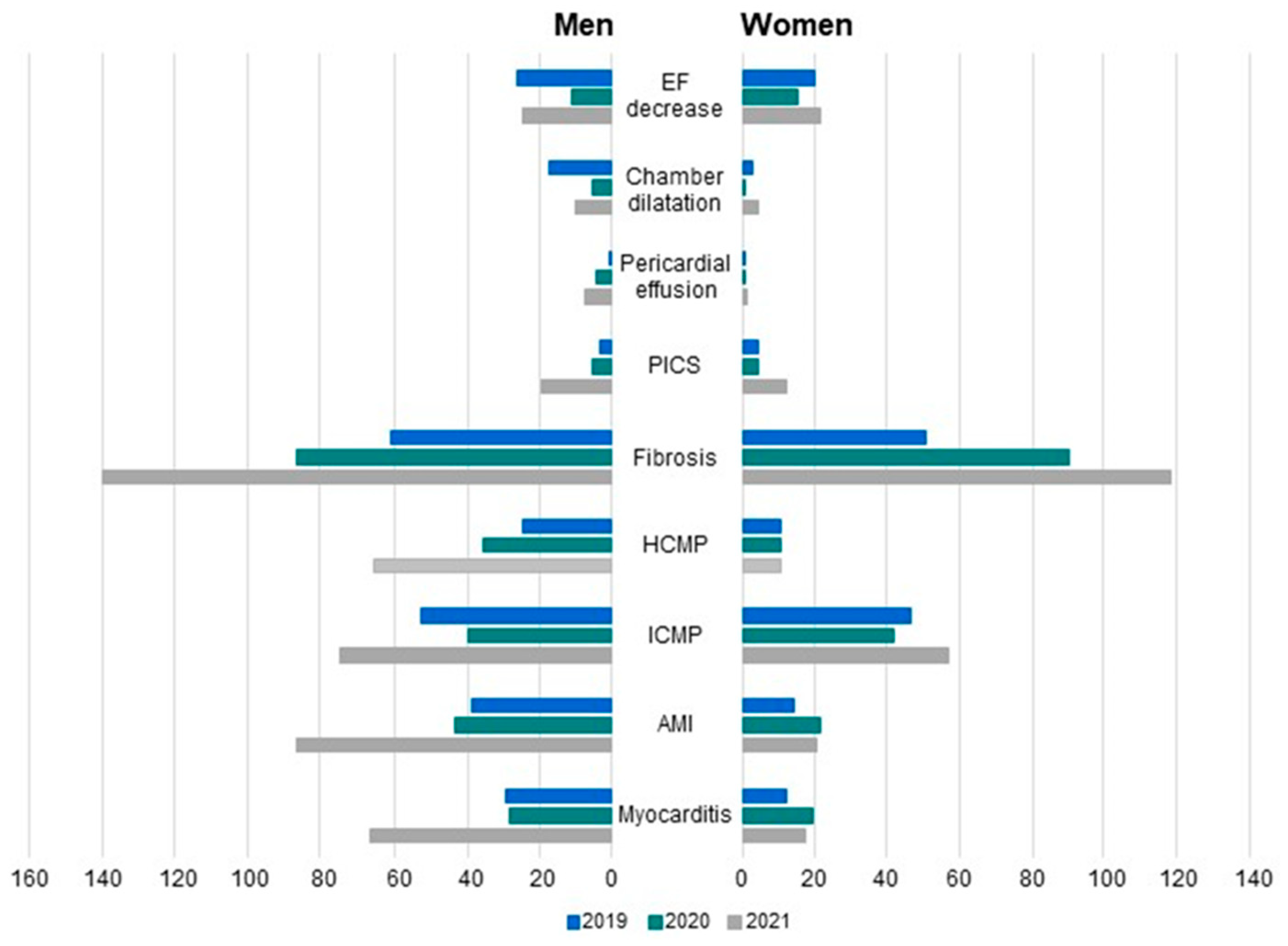
The rates of male cardiac patients who received CMR examinations were 58.59% in 2019, 51.72% in 2020, and 56.36% in 2021, and the rate significantly increased to 73.13% during the first six months of 2022. The incidence of fibrous-dystrophic changes in the myocardium significantly increased and continued to increase to 2022 in both male (from 52.57% in 2019 to 81.03% in 2022), and female patients (from 62.20% in 2019 to 87.39% in 2022). The number of detected acute myocarditis drastically decreased to 10% in male and to 13% in female patients in 2020 among all detected cardiac pathologies with subsequent gradual increase in 2021 (
Figure 2).
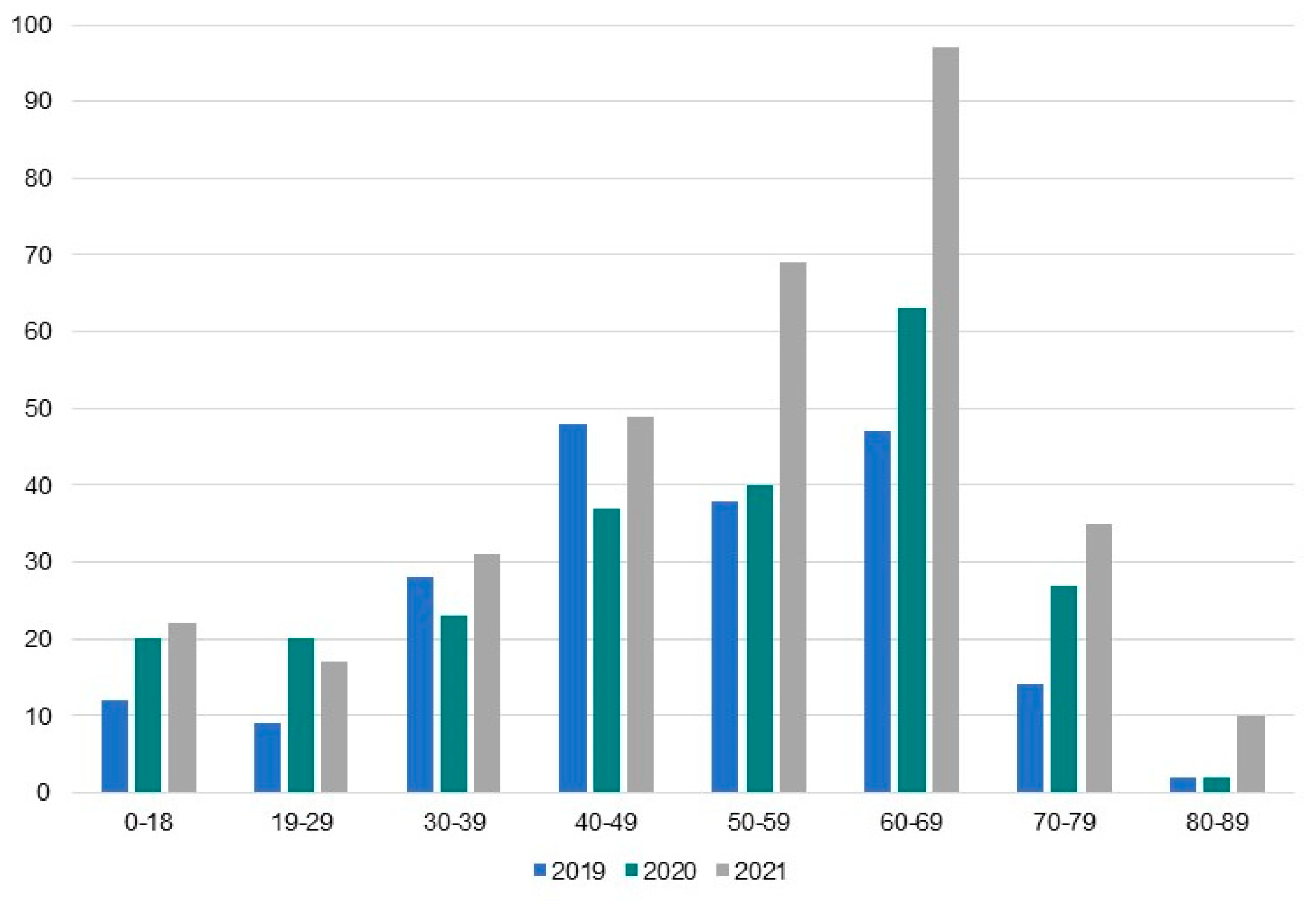
The age-related analysis showed that the peak in the number of patients in each age group was in 2021, and the incidence was the highest in 60-69-year-old patients from group of high risk for severe course and complications of COVID-19. Among the total amount of CMR studies, patients aged 60-69 years comprised 11.90% in 2019, 15.95% in 2020, 24.56% in 2021, and 18.73% in 2022 (
Figure 3).
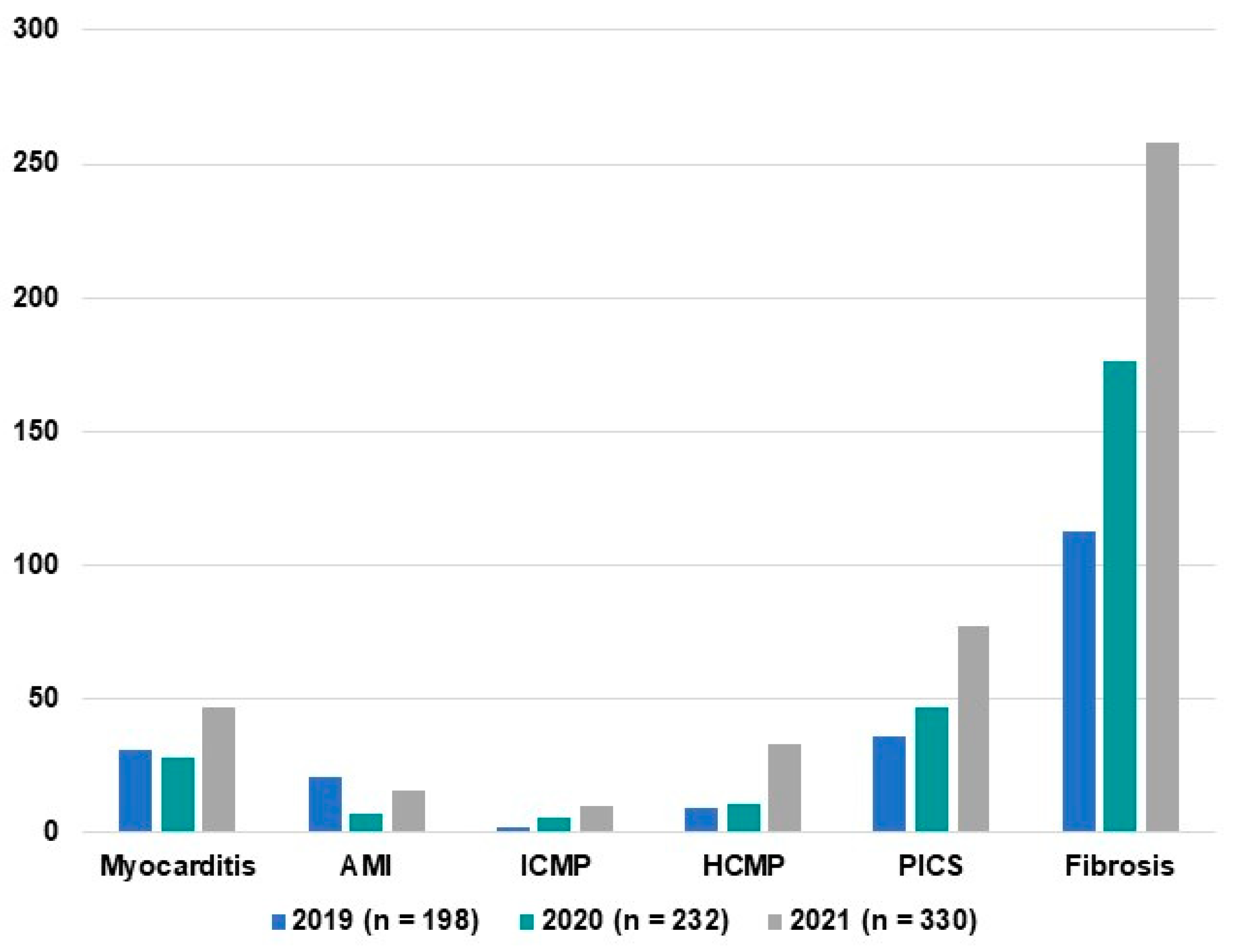
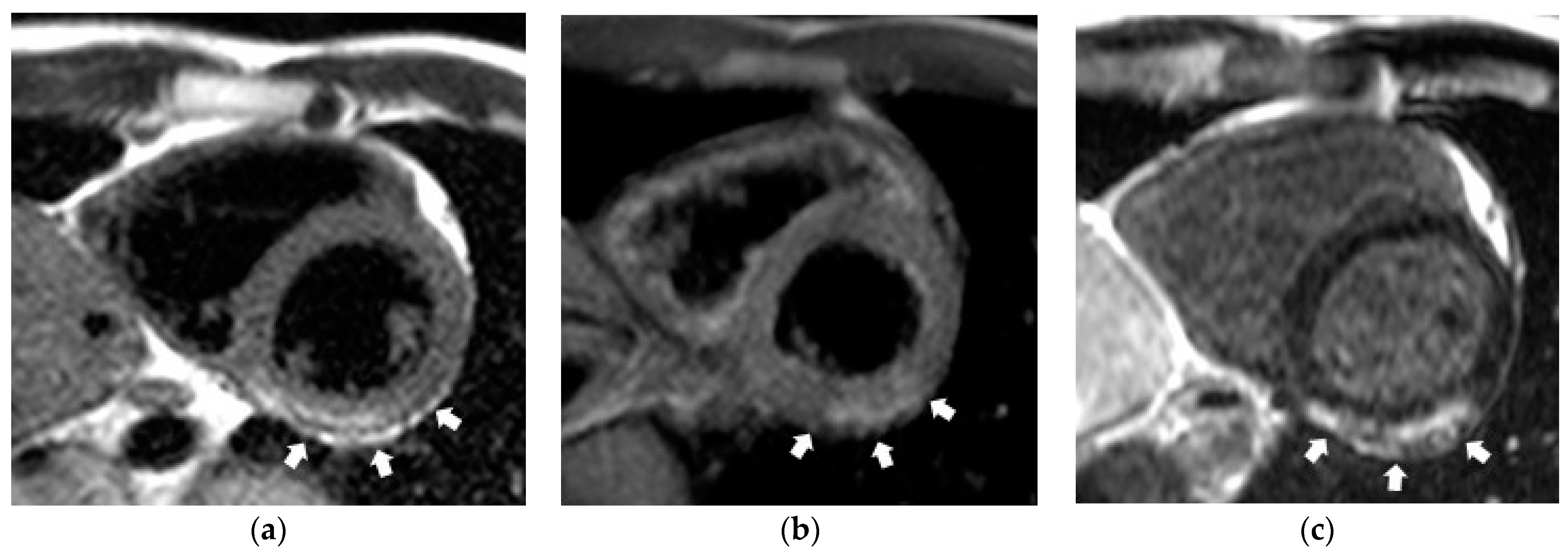
The main diagnostic entities of cardiovascular pathology, detected by CE-CMR, were myocarditis, acute myocardial infarction, ischemic cardiomyopathy, hypertrophic cardiomyopathy, postinfarction cardiosclerosis, and myocardial fibrosis (
Figure 4). Myocardial fibrosis was characterized by the presence of non-coronarogenic fibrotic foci (
Figure 5).
The analysis of year-by-year distribution of these cardiac pathologies showed that the incidence of each detected entity peaked in 2021. Besides, the proportion of patients with myocardial fibrosis, which could be a consequence of myocardial inflammation, significantly increased among total number of patients who received CMR study: 67.17% in 2019, 76.29% in 2020, 78.18% in 2021, and 84.14% before June, 2022 (p < 0.05) (
Figure 4).
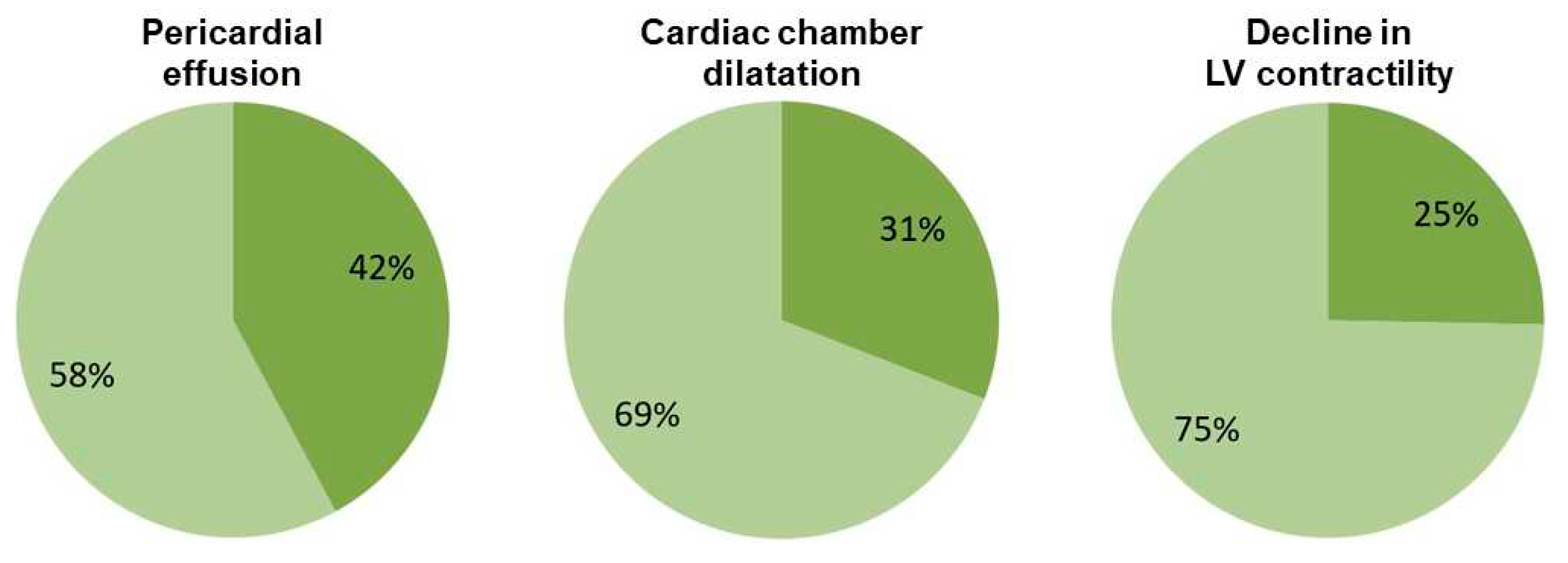
CE-CMR studies in patients with non-coronarogenic myocardial fibrosis showed the presence of pericardial effusion (42%), dilatation of cardiac chambers (31%), and decrease in the left ventricular contractile function (25%) (
Figure 6).
The COVID-19 incidence was characterized by a cyclic behavior at the population level. The first wave of coronavirus infection had the most negative impact on a patient stream in our institute (April to May, 2020) when there was a dramatic drop in the total number of performed studies (p < 0.001) perhaps due to restrictive measures, self-isolation, decline in pre-arranged hospital care, etc. (
Figure 7).
4. Discussion
To create a “portrait” of patient with past COVID-19 infection in our region, we studied two Cohorts. We analyzed the results of online survey of 727 residents of Tomsk and Tomsk Region to learn their experience with diagnostic imaging during COVID-19 pandemic. We also studied MRI database [
19] to establish the temporal patterns and findings of MRI studies performed in a single cardiovascular center. Therefore, our study gives the insights into administration of medical visualization during the pandemic from two perspectives: as seen by the population and medical specialists.
Interestingly, three quarters of respondents in our online survey were females. Strikingly, majority of respondents reported slight malady or felt unwell, and only 28% of them reported to feeling well. Over a half of respondents had history of confirmed COVID-19 infection, and the incidence of cardiovascular diseases in the Cohort 1 was as high as 31% despite relatively young age of the people surveyed (~45 years). Considering that many cases, first of all, of mild COVID-19 infection could remain unconfirmed, the vast majority of surveyed population had history of COVID-19, and the rates of vaccination reached 64%. Though MRI was available to majority of people in the survey, it was only the fourth most popular diagnostic imaging method. Privately paid MRI could ensure shorter waiting times, but most of respondent could not afford it a regular situation.
Global COVID-19 pandemic put unprecedented pressure on the healthcare system worldwide. The first wave of this viral infection was associated with a decline in the most areas of healthcare such as planned and screening procedures including examinations requiring MRI [
20,
21,
22,
23]. It is not surprising that a significant drop in the number of diagnostic MRI procedures was observed in our cardiovascular center during the first months of COVID-19 pandemic (
Figure 1).
The analysis of MRI studies performed in 2019–2022 showed a significant increase in the number of myocardial imaging procedures. This observation agrees well with data of world statistics and confirms the need in cardiac exams considering sometimes direct (to a lesser degree) and largely indirect (through systemic inflammatory reaction) impact of SARS-CoV-2 on the cardiovascular system. Besides, one of the serious problems consists in a heart damage associated with the side effects of drugs administered for COVID-19 treatment, especially when antiviral medications are used. Another essential and poorly studied problem is potential drug-drug interactions between the antiviral drugs, oral anticoagulants, and other medications for COVID-19 treatment [
2,
24,
25].
Our study confirmed the effect of patient age and sex on the risk of developing cardiovascular complications, which also agrees with literature data [
26]. The age-related analysis showed that cardiovascular pathology is significantly more often detected in group of 60-69-year-old patients.
The CMR-based assessment of inflammatory changes in the myocardium was performed in our center using the Lake Louise Criteria [
27], which specifies three aspects of myocardial inflammation: edema, hyperemia, and necrosis and/or fibrosis based on assessment of signal intensity on T2-weighted images, in regimes of early and delayed contrast enhancement of the myocardium. These criteria were identified based on a limited number of published studies, and, at that time, their diagnostic accuracy, sensitivity, and specificity were estimated to be 78%, 67%, and 91%, respectively. Though some criteria and approaches to their assessment have been a matter of debate, these numbers were largely confirmed and validated by the later studies [
28].
However, tissue characteristics for the detection of edema based on CMR of the myocardium using only signal intensity have some disadvantages. When inflammatory processes become more generalized (it happens more often after the first days of disease when myocarditis transits from acute to subacute), the intensity of T2-weighted images and contrasting also become more uniformed to the degree when individual lesions can no longer be easily detected by qualitative review.
Indeed, in our study, the CMR-based signs of acute inflammatory process in the myocardium were present only in 24.3% of patient among the entire number of patients who were referred to the exam in 2019, with a gradual decrease in the number of such patients to 9.4% in 2022 though the majority of patients who recovered from COVID-19 reported heart symptoms. This phenomenon may be caused by two causes. First, it is possible that the chest symptoms were caused by the residual lung disease, but this hypothesis requires further studies. Second, considering that the mean time between the occurrence of the first symptoms and CMR scan ranged one to two months, the study could be performed during the subacute stage (during edema regression). The new methods of CMR have been recently proposed including T1- and T2- relaxation time mapping and determination of extracellular volume fraction that perhaps expand diagnostic capabilities of this method in patients with myocarditis [
29]. T1- and T2-mapping allow to quantitatively assess the diffuse changes in the myocardium (diffuse edema, fibrosis). Unfortunately, the methods of mapping were not used in our center.
The small foci of myocardial fibrosis of non-coronarogenic genesis were detected in the vast majority of patients who received CMR in our center, which agrees with our previously published works [
12,
13]. The presence of pericardial effusion and/or abnormal contractile function of the left ventricle were observed in some of our patients in this group (
Figure 7). The detected changes may be an outcome of past inflammatory process triggering cardiac remodeling. Indeed, literature suggests that myocardial remodeling may precede the functional left ventricular remodeling [
30]. Our results are in compliance with this conclusion as the abnormalities were detected mostly in the left myocardial structure rather than function in the majority of subjects. Therefore, the patients of this group require a long-term follow up whereas CE-CMR is a sensitive tool for the monitoring of further recovery progress.
It is worth emphasizing that we observed an increase in the incidence, though not that high, of other cardiovascular pathology (ischemic cardiomyopathy, hypertrophic cardiomyopathy, etc.) during COVID-19 pandemic, which does not rule out the adverse effects of SARS-CoV-2 or side effects of pharmacological treatment, which also requires further study. Interestingly, we found the increases in the rates of diagnostic procedures and detected pathological changes of cardiovascular system during the third year of COVID-19 pandemic, which also may suggest chronic course of this disease. Prospects for wider use of MRI in diagnosing not only chronic cardiac, but also chronic lung complications of COVID-19 require further exploration considering that pilot data show MRI an accurate and informative imaging modality in this regard [
12,
31,
32,
33,
34,
35].
The limitation of our online survey was the fact that Cohort 1 mostly represented the population leaving digital footprint in healthcare and pharmacy and having iOS and Android devices, but not the entire population. People interested in health were naturally more likely to take part in survey. Using the criteria of health-related digital shadow enriched the response rate, prevented unnecessary loss of potential respondents, and enlarged the sample by people with relevant experience. This limitation was carefully balanced with other poorly understood potential drawbacks of forming population sample by means of telecommunication technologies. Besides, a pilot study of groups leaving or not leaving digital shadow gained similar results between these categories of respondents. The limitation of our study in Cohort 2 was impossibility of using the MRI mapping protocols due to limited capabilities of the equipment available in our center. Besides, most of enrolled patients who received CMR had history of moderate COVID-19 so our report does not cover the entire spectrum of manifestations of this pathology because we did not study critically ill patients or those who suffered from severe COVID-19. The proportion of patients with cardiac involvement, detected in our study, may not be extrapolated to a wider population and other patient cohorts. Nevertheless, the present study demonstrates the phenomenon of cardiac involvement after COVID-19, and the obtained results may be useful because they contribute to developing the awareness of medical specialists. It is all the more essential considering that under-diagnosis of cardiac lesions most likely occurs in patients with mild form of SARS-CoV-2 infection. However, our data agree with the observation that mild SARS-CoV-2 infection leaves long-lasting effects on cardiovascular health [
5]. At last, we completed the cross-sectional observational electronic medical record-based MRI investigation whereas prolonged observation would be helpful for the evaluation of myocardial condition over time especially considering the risk of developing chronic cardiac pathology in patients with past history of mild and moderate COVID-19.
5. Conclusions
According to our online survey, over 60% of our population sample reported slight malady at the time of survey; more than a half of them had confirmed COVID-19 infection in the past, a third of them had cardiovascular diseases. MRI was the fourth most common diagnostic imaging modality administered to the respondents within two years prior to the survey. MRI was available to majority of people in the survey though relatively high proportion of people could not afford MRI procedure or receive it for other reasons like residing in remote areas. Privately paid MRI was associated with shorter waiting times and was readily available for about every tenth person. The COVID-19 pandemic was associated with increased demand in CE-CMR. Patients who suffered from COVID-19 had residual symptoms and the onset of new symptoms specific for cardiac pathology with tendency to chronic course. Focal myocardial fibrosis was the main finding on CE-CMR images in these patients. Patients with cardiac symptoms and past history of COVID-19 require continuous follow up to prevent potential remodeling of the myocardium. Educational and organizational efforts are needed to promote the use of MRI and other relevant imaging modalities among population. An increase in affordability and availability of medical visualization is strategically essential for population health.
Author Contributions
Conceptualization, A.S.M.; T.A.S.; N.I.R.; W.Y.U. and N.D.A.; methodology, A.S.M.; T.A.S.; N.I.R.; V.K.V.; A.D.K.; N.P.C.; W.Y.U. and N.D.A.; software, V.K.V. and A.D.K.; validation, I.A.T.; O.M.N.; A.B.N. and N.P.C.; formal analysis, A.S.M.; T.A.S.; N.I.R.; A.D.K.; and N.D.A.; investigation, A.S.M.; T.A.S.; N.I.R.; O.V.M.; O.M.N., A.B.N., A.D.K.; W.Y.U. and N.D.A.; resources, N.D.A.; data curation, N.D.A.; writing—original draft preparation, A.S.M.; T.A.S.; N.I.R.; W.Y.U. and N.D.A.; writing—review and editing, A.S.M.; T.A.S.; N.I.R.; O.V.M.; V.K.V.; I.A.T.; O.M.N.; A.D.K.; A.B.N.; N.P.C.; W.Y.U.; N.D.A.; visualization, A.S.M.; T.A.S.; N.I.R.; O.V.M. and W.Y.U.; supervision, N.D.A. and I.A.T.; project administration, N.D.A.; funding acquisition, N.D.A. All authors have read and agreed to the published version of the manuscript.
Funding
Authors thank the Russian Science Foundation for support of this work (#22-15-00313).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol of the study was approved by the Institutional Review Board of Cardiology Research Institute of Tomsk NRMC together with the Expert Review Board of the Russian Science Foundation with conclusion of an Agreement #2-15-00313 from May 13, 2022. The Research Team was assigned the task of completing the study in 2022-2024 (Cardiology Research Institute Order #49 from June 03, 2022).
Informed Consent Statement
No identifiable patient information has been provided in the manuscript. The paper contains only aggregate data, which are completely depersonalized. None of the patients was specifically invited to undergo CMR to participate in the study. Electronic medical records stored in the specifically developed MRI database were studied retrospectively. The material of our study in Cohort 1 was data, not patients themselves. However, when relevant, patients signed the informed consent form. All the patients signed the standard Informed Consent Form for medical examination. The online survey in Cohort 2 was depersonalized/anonymized. The participants had the option to provide their contact information (phone number or/and email) if they chose to apply for an update of published study results. Each participant provided the informed consent agreement signing it online by checking the appropriate box. The original informed consent form is available on the website developed for the online survey at
www.zdorov.tpu.ru.
Data Availability Statement
Deidentified individual participant data (text, tables, figures, and appendices), underlying the results of the trial, will be shared with researchers to achieve the aims in the approved proposal. Time Frame: Proposals may be submitted up to 36 months following publication of the results of the trial. After 36 months, the data will be available in the Center's data ware house but without investigator support other than deposited metadata. Access Criteria: Information regarding submitting proposals and accessing data may be requested from the corresponding author by e-mail.
Acknowledgments
Authors thank Tele2 Russia and Mrs. Liana Ishkulova for impeccable telecommunication services.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Kelle, S.; Bucciarelli-Ducci, C.; Judd, R.M.; Kwong, R.Y.; Simonetti, O.; Plein, S.; Raimondi, F.; Weinsaft, J.W.; Wong, T.C.; Carr, J. Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection. J Cardiovasc Magn Reson 2020, 22, 61. [Google Scholar] [CrossRef] [PubMed]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: from an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci 2021, 58, 297–310. [Google Scholar] [CrossRef]
- Ussov, W.Yu.; Nudnov, N.V.; Ignatenko, G.A.; Fisenko, A.Yu.; Gulyaev, V.M.; Maritskii, S.V.; Kalyuzhin, V.V.; Lukyanenok, P.I. Evaluation of lung damage in pneumonia, from chest magnetic resonance imaging, in primary diagnosis and in the follow-up of treatment. Medical Visualization 2020, 24, 63–77. [Google Scholar] [CrossRef]
- Ussov, W.Yu.; Nudnov, N.V.; Ignatenko, G.A.; Gulyaev, V.M.; Pervak, M.B.; Shelkovnikova, T.A.; Dubovaya, A.V.; Bergen, T.A. Primary and prospective imaging of the chest using magnetic resonance imaging in patients with viral lung damage in COVID-19. Medical Visualization 2020, 24, 11–26. [Google Scholar] [CrossRef]
- Todorovic, V. Mild SARS-CoV-2 infection leaves long-lasting effects on cardiovascular health. Nat Cardiovasc Res 2022, 1, 870. [Google Scholar] [CrossRef]
- Ramadan, M.S.; Bertolino, L.; Zampino, R.; Durante-Mangoni, E.; Monaldi Hospital Cardiovascular Infection Study Group. Cardiac sequelae after coronavirus disease 2019 recovery: a systematic review. Clin Microbiol Infect 2021, 27, 1250–1261. [Google Scholar] [CrossRef] [PubMed]
- Ansheles, A.A.; Sergienko, V.B.; Sinitsyn, V.E.; Vakhromeeva, M.N.; Kokov, A.N.; Zavadovsky, K.V.; Ryzhkova, D.V.; Karalkin, A.V.; Shurupova, I.V.; Pospelov, V.A.; Migunova, E.V.; Sayfullina, G.B.; Dariy, O. Yu.; Zhuravlev, K.N.; Itskovich, I.E.; Gagarina, N.V.; Hirschfeld, C.; Williams, M.C.; Shaw, L.J.; Malkovskiy, E.; Better, N.; Cerci, R.; Dorbala, Sh.; Karthikeyan, G.; Pascual, T.N.B.; Villines, T.; Vitola, J.V.; Cohen, Y.; Randazzo, M.; Sewanan, L.; Pynda, Y.; Dondi, M.; Paez, D.; Einstein, A.J. Analysis of the restoration of cardiology diagnostics scope in the Russian federation during the COVID-19 pandemic: Results of the Russian segment of the INCAPS COVID 2 study under the auspices of the International Atomic Energy Agency. Russian Journal of Cardiology 2022, 27, 5170, (In Russ.). [Google Scholar] [CrossRef]
- Sudakov, D.V.; Sudakov, O.V.; Shevtsov, A.N.; Belov, E.V.; Androsova, O.A. Analysis of complications among patients after previous new coronoviral COVID-19 infection. System Analysis and Management in Biomedical Systems 2021, 20, 15–23, (In Russ.). [Google Scholar] [CrossRef]
- Italia, L.; Tomasoni, D.; Bisegna, S.; Pancaldi, E.; Stretti, L.; Adamo, M.; Metra, M. COVID-19 and Heart Failure: From Epidemiology During the Pandemic to Myocardial Injury, Myocarditis, and Heart Failure Sequelae. Front Cardiovasc Med 2021, 8, 713560. [Google Scholar] [CrossRef]
- Fisun, A.Y.; Lobzin, Y.V.; Cherkashin, D.V.; Tyrenko, V.V.; Tkachenko, K.N.; Kachnov, V.A.; Kutelev, G.G.; Rudchenko, I.V.; Sobolev, A.D. Mechanisms of damage to the cardiovascular system in COVID-19. Annals of the Russian Academy of Medical Sciences 2021, 76, 287–297, (In Russ.). [Google Scholar] [CrossRef]
- Kobelev, E.; Bergen, T.A.; Tarkova, A.R.; Vasiltseva, O.Ya.; Kamenskaya, O.V.; Usov, V. Yu.; Chernyavsky, A.M. COVID-19 as a cause of chronic pulmonary hypertension: pathophysiological rationale and potential of instrumental investigations. Cardiovascular Therapy and Prevention 2021, 20, 126–133, (In Russ.). [Google Scholar] [CrossRef]
- Shelkovnikova, T.A.; Pushnikova, E.Yu.; Baev, A.E.; Ryabov, V.V.; Ussov, W.Yu. Magnetic resonance syndromes of myocardial damage in patients after new coronavirus infection (COVID-19) - two typical clinical cases. Siberian Journal of Clinical and Experimental Medicine 2022, 37, 135–141, (In Russ.). [Google Scholar] [CrossRef]
- Ussov, W.Yu.; Ignatenko, G.A.; Nudnov, N.V.; Bergen, T.A.; Gulyaev, V.M.; Pervak, M.B.; Yaroshevsky, S.P.; Dubovaya, A.V.; Karmazanovsky, G.G. Comprehensive MRI of the chest and brain in the diagnosis of injury to thoracic organs, myocardium, and brain in COVID-19. The University Clinic 2021, Suppl.I, 144-145. (In Russ.). Available at https://dnmu.ru/wp-content/uploads/2021/02/materConfCovid_010221.pdf.
- Baig, A.M. Chronic COVID syndrome: Need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol 2021, 93, 2555–2556. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; McGettigan, J.; Khetan, S.; Segall, N.; Solis, J.; Brosz, A.; Fierro, C.; Schwartz, H.; Neuzil, K.; Corey, L.; Gilbert, P.; Janes, H.; Follmann, D.; Marovich, M.; Mascola, J.; Polakowski, L.; Ledgerwood, J.; Graham, B.S.; Bennett, H.; Pajon, R.; Knightly, C.; Leav, B.; Deng, W.; Zhou, H.; Han, S.; Ivarsson, M.; Miller, J.; Zaks, T.; COVE Study Group. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; Bailey, R.; Swanson, K.A.; Roychoudhury, S.; Koury, K.; Li, P.; Kalina, W.V.; Cooper, D.; Frenck, R.W. Jr.; Hammitt, L.L.; Türeci, Ö.; Nell, H.; Schaefer, A.; Ünal, S.; Tresnan, D.B.; Mather, S.; Dormitzer, P.R.; Şahin, U.; Jansen, K.U.; Gruber, W.C.; C4591001 Clinical Trial Group. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; Fang, J.C.; Fedson, S.E.; Fonarow, G.C.; Hayek, S.S.; Hernandez, A.F.; Khazanie, P.; Kittleson, M.M.; Lee, C.S.; Link, M.S.; Milano, C.A.; Nnacheta, L.C.; Sandhu, A.T.; Stevenson, L.W.; Vardeny, O.; Vest, A.R.; Yancy, C.W. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022, 79, e263–e421. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.E.; Friedrich, M.G.; Leiner, T.; Elias, M.D.; Ferreira, V.M.; Fenski, M.; Flamm, S.D.; Fogel, M.; Garg, R.; Halushka, M.K.; Hays, A.G.; Kawel-Boehm, N.; Kramer, C.M.; Nagel, E.; Ntusi, N.A.B.; Ostenfeld, E.; Pennell, D.J.; Raisi-Estabragh, Z.; Reeder, S.B.; Rochitte, C.E.; Starekova, J.; Suchá, D.; Tao, Q.; Schulz-Menger, J.; Bluemke, D.A. Cardiovascular Magnetic Resonance for Patients With COVID-19. JACC Cardiovasc Imaging 2022, 15, 685–699. [Google Scholar] [CrossRef] [PubMed]
- Ussov, W.Yu.; Mochula, O.V.; Ryumshina, N.I.; Shelkovnikova, T.A.; Sukhareva, A.E.; Maksimova, A.S.; Velichko, O.B.; Vaizov, V.Kh.; Ovchinnikov, P.P.; Zavadovsky, K.V.; Boshchenko, A.A. Certificate of the state registration for database No. 2022622669 Russian Federation. Register of magnetic resonance imaging studies: No. 2022622644: submitted 24.10.2022: published 28.10.2022; applicant: Tomsk NRMC. – EDN XWWUWA. Available at https://www.elibrary.ru/download/elibrary_49774441_46558053.PDF.
- de Pelsemaeker, M.C.; Guiot, Y.; Vanderveken, J.; Galant, C.; Van Bockstal, M.R. The Impact of the COVID-19 Pandemic and the Associated Belgian Governmental Measures on Cancer Screening, Surgical Pathology and Cytopathology. Pathobiology 2021, 88, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Keizman, E.; Ram, E.; Kachel, E.; Sternik, L.; Raanani, E. The impact of COVID-19 pandemic on cardiac surgery in Israel. J Cardiothorac Surg 2020, 15, 294. [Google Scholar] [CrossRef]
- Saban, M.; Reznik, A.; Shachar, T.; Wilf-Miron, R.; Sivan-Hoffmann, R. The effect of the COVID-19 pandemic on ED referrals and care for stroke patients: A four-year comparative study. J Crit Care 2021, 62, 230–234. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V.; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Anfinogenova, N.D.; Trubacheva, I.A.; Popov, S.V.; Efimova, E.V.; Ussov, W.Y. Trends and concerns of potentially inappropriate medication use in patients with cardiovascular diseases. Expert Opin Drug Saf. 2021;20(10):1191-1206. [CrossRef]
- Cattaneo, D.; Pasina, L.; Maggioni, A.P.; Oreni, L.; Conti, F.; Pezzati, L.; Casalini, G.; Bonazzetti, C.; Morena, V.; Ridolfo, A.; Antinori, S.; Gervasoni, C. Drug-Drug Interactions and Prescription Appropriateness at Hospital Discharge: Experience with COVID-19 Patients. Drugs Aging 2021, 38, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Vakili, S.; Savardashtaki, A.; Jamalnia, S.; Tabrizi, R.; Nematollahi, M.H.; Jafarinia, M.; Akbari, H. Laboratory Findings of COVID-19 Infection are Conflicting in Different Age Groups and Pregnant Women: A Literature Review. Arch Med Res 2020, 51, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; Aletras, A.; Laissy, J.P.; Paterson, I.; Filipchuk, N.G.; Kumar, A.; Pauschinger, M.; Liu, P.; International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Lagan, J.; Schmitt, M.; Miller, C.A. Clinical applications of multi-parametric CMR in myocarditis and systemic inflammatory diseases. Int J Cardiovasc Imaging 2018, 34, 35–54. [Google Scholar] [CrossRef] [PubMed]
- Liguori, C.; Farina, D.; Vaccher, F.; Ferrandino, G.; Bellini, D.; Carbone, I. Myocarditis: imaging up to date. Radiol Med 2020, 125, 1124–1134. [Google Scholar] [CrossRef] [PubMed]
- Dixit, N.M.; Churchill, A.; Nsair, A.; Hsu, J.J. Post-Acute COVID-19 Syndrome and the cardiovascular system: What is known? Am Heart J Plus 2021, 5, 100025. [Google Scholar] [CrossRef] [PubMed]
- Ignatenko, G.A.; Pervak, M.B.; Usov, V.Yu.; Dubovaya, A.V.; Gerasimenko, V.V. Computed-tomographic evaluation of the lung changes in COVID-19 after 4-6 months: Comparison with the results of the study in the acute period of the disease and clinical data. Archives of Clinical and Experimental Medicine 2022, 31, 112–118, Available at https://portal.dnmu.ru/fileadmin/EDITDATA/bibl/AKEHM_2022_No2.pdf. [Google Scholar]
- Wojtowicz, D.; Dorniak, K.; Ławrynowicz, M.; Wąż, P.; Fijałkowska, J.; Kulawiak-Gałąska, D.; Rejszel-Baranowska, J.; Knut, R.; Haberka, M.; Szurowska, E.; Koziński, M. Cardiac Magnetic Resonance Findings in Patients Recovered from COVID-19 Pneumonia and Presenting with Persistent Cardiac Symptoms: The TRICITY-CMR Trial. Biology (Basel) 2022, 11, 1848. [Google Scholar] [CrossRef] [PubMed]
- Kersten, J.; Baumhardt, M.; Hartveg, P.; Hoyo, L.; Hüll, E.; Imhof, A.; Kropf-Sanchen, C.; Nita, N.; Mörike, J.; Rattka, M.; Andreß, S.; Scharnbeck, D.; Schmidtke-Schrezenmeier, G.; Tadic, M.; Wolf, A.; Rottbauer, W.; Buckert, D. Long COVID: Distinction between Organ Damage and Deconditioning. J Clin Med 2021, 10, 3782. [Google Scholar] [CrossRef]
- Camastra, G.; Arcari, L.; Ciolina, F.; Danti, M.; Ansalone, G.; Cacciotti, L.; Sbarbati, S. Characterization of COVID-19-Related Lung Involvement in Patients Undergoing Magnetic Resonance T1 and T2 Mapping Imaging: A Pilot Study. J Imaging 2022, 8, 314. [Google Scholar] [CrossRef]
- Drakos, S.; Chatzantonis, G.; Bietenbeck, M.; Evers, G.; Schulze, A.B.; Mohr, M.; Fonfara, H.; Meier, C.; Yilmaz, A. A cardiovascular magnetic resonance imaging-based pilot study to assess coronary microvascular disease in COVID-19 patients. Sci Rep 2021, 11, 15667. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).