Introduction
Safe water, sanitation, and hygiene (WASH) are essential for human health and well-being. The WASH programme focuses on long-term prevention and control measures to improve health, build resilient communities, and respond to global emergencies and disease outbreaks (WHO, 2022). Despite the various activities of WASH, more than 884 million people around the world still do not have access to clean water (CDC, 2020, 2022; Lambeth, 2023). There are over 2.4 billion individuals worldwide who lack access to even the most fundamental sanitation services (CDC, 2022). Many people still choose to defecate in the open, despite the fact that this behavior puts the quality of the water that is used for drinking and other purposes at risk. Water that has been contaminated with human faeces, for example as a result of rain wash off from open latrines and septic tanks, is of particular concern, especially during rainy seasons, as it may contain organisms that are capable of causing severe illness or even death (Kabi, 2023; Malik, Yasar, Tabinda, & Abubakar, 2012; WHO, 2015b). There are over four billion instances of diarrhoea reported annually around the world, 88 percent of which are attributed to contaminated water used for drinking (Acheson; CDC, 2020, 2022; Levy, Smith, & Carlton, 2018; WHO, 2007).
Contaminated water is a source of many pathogens such as protozoa, helminths, bacteria and viruses. Some pathogens, particularly the free-living amoeba (FLA) helminths, cryptosporidium and giardia that can sometimes elicit debilitating illnesses are not often emphasised as waterborne diseases. For example, some types of FLA spread through water such as Naegleria spp., and Acanthamoeba spp are responsible for primary amebic meningoencephalitis (PAM) and granulomatous amoebic encephalitis (GAE) respectively (Sarink et al., 2022). Acanthamoeba is also a common cause of keratitis that often leads to permanent visual impairment (Reyes-Batlle, Sifaoui, Rodríguez-Expósito, Piñero, & Lorenzo-Morales, 2022). Although not reported often, these pathogens are likely very common in countries that lack clean water supply. Of the 884 million people worldwide who lack access to clean water, 40% are from Sub-Saharan Africa, and more than 300 million of these have limited access to safe drinking water, with many also unable to access safe water for bathing, washing, and recreation (Boelee, Geerling, van der Zaan, Blauw, & Vethaak, 2019; Rodriguez, 2019; WWF, 2023).
Despite the challenges that are associated with rural water supply in Africa, many people who use the water don't appear to care very much about the quality of the water they use (Murei et al., 2022; Omarova, Tussupova, Hjorth, Kalishev, & Dosmagambetova, 2019). A large number (55-85%) of rural households in Uganda access water that does not meet the minimum required standard (Godfrey Bwire et al., 2020; Mirembe, 2014; Ssemugabo et al., 2019). Poor water quality in rural areas of Uganda could be due to factors such as high population pressure and increased industrialisation, consequently leading to untreated waste water, sewage and other dangerous organic matter and chemicals entering the water supply system (Angiro, Abila, & Omara, 2020; Oguttu, Okullo, Bwire, Nsubuga, & Ario, 2017). Untreated organic matter (Bonilla-Lemus, Caballero Villegas, Carmona Jimenez, & Lugo Vazquez, 2014) and that containing faecal coliform or parasites can be harmful to the environment and the end users (Fawell & Nieuwenhuijsen, 2003). When this happens, the end users are faced with a variety of health challenges. Periodic outbreaks of waterborne diseases were reported in Uganda in 2009, 2011, 2012, 2013, 2015, 2019, 2020 and 2021 mainly due to poor water safety and hygiene associated causes (Abdulkadir & Kasirajan, 2016; Eurien et al., 2021; Mirembe, 2014; Muhereza, 2009; Oguttu et al., 2017). Despite all of the periodic outbreaks, the government has done little to provide appropriate control measures. The most effective way to prevent these types of disease outbreaks is to spread information about the potential waterborne diseases and how to avoid them.
It would be prudent to increase research on waterborne pathogens that could potentially be a threat to human and animal health in Uganda, as well as the dissemination of information about those pathogens. This study, therefore, was designed to determine the presence of waterborne protozoan and helminth parasites in Queen Elizabeth Protected Area (QEPA), an area which has one of the largest influxes of domestic and international tourists, and a rapidly growing local population of inhabitants.
Study areas
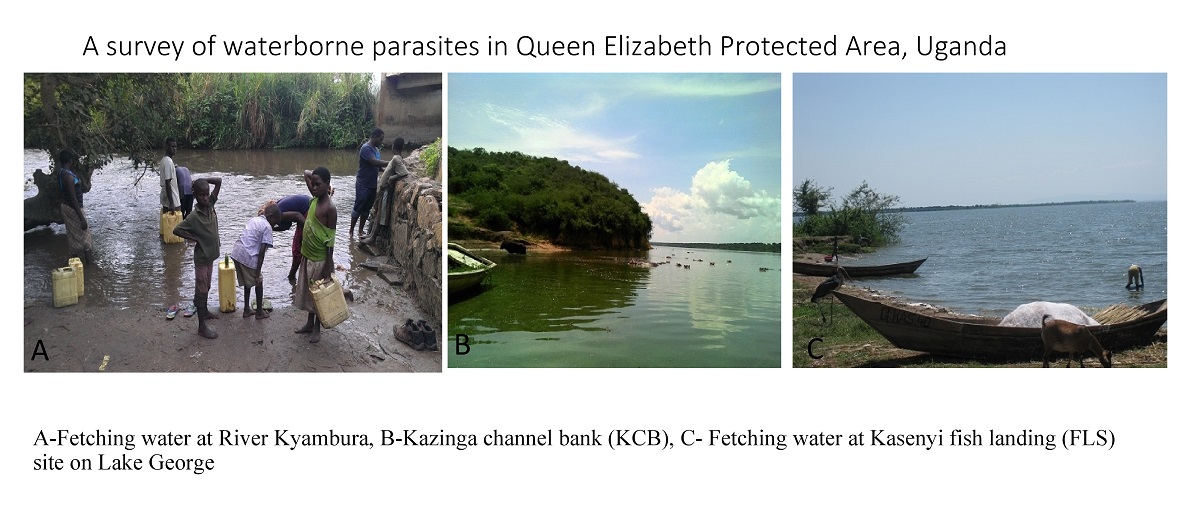
The research was carried out in Uganda's QEPA, which has a total area of 1,978 square kilometers, and is located at a latitude of 0.2000 and a longitude of 30.0000. Lakes George and Edward are part of QEPA, and the Kazinga Channel, which is forty kilometers long, connecting the two lakes. QEPA is designated as a "Man and Biosphere Reserve" by UNESCO and contains 11 village enclaves, all of which have a rapidly expanding human population. The primary economic activity in these communities are fishing and livestock rearing. Domestic water for human consumption in QEPA comes from natural sources such as the Kazinga channel (a 40km water stretch connecting Lake George and Lake Edward), the River Kyambura, Lake George, and Lake Edward. These natural water bodies are also used by the locals for swimming, bathing, and washing clothes.
Study design and sampling strategy
This was a cross-sectional study. The sampling locations were chosen purposively, taking into account their proximity to the end-users. Natural (environmental) water samples were collected from areas where locals obtain water for domestic use as well as where they engage in recreational activities such as swimming. The water samples were got from piped tap water (PTW), and natural water sources namely; River Kyambura (RK), Kazinga channel banks (KCB), Middle of Kazinga channel (MKC), and Fish landing sites (FLS). A total number of 324 natural surface water and 84 piped tap water samples were collected using 50 ml sterile polypropylene falcon tubes (Discovery Labware, USA). The water samples were stored at room temperature and transported to the Makerere University parasitology laboratory immediately, within 48 hours.
Laboratory Assays
Different methods were used for the detection of the parasites: Xenic cultivation for FLA (Sente, Erume, Naigaga, Gabriela Namara, et al., 2016), Modified Ziehl-Neelsen staining technique for Cryptosporidium (Tahvildar-Biderouni & Salehi, 2014), Direct wet smears for some protozoan trophozoites (Khanna, Tilak, Rasheed, & Mukhopadhyay, 2014), Zinc Sulphate floatation technique for Giardia cysts and helminth eggs (Kim, Kim, & Lee, 1985), analytical sodium chloride floatation technique for helminth eggs (Collender, Kirby, Addiss, Freeman, & Remais, 2015; Setiawan, Nuryati, & Sofiarahma, 2020), and McMaster chambers for counting helminth eggs (Kochanowski, Dabrowska, Karamon, Cencek, & Osiński, 2013).
Centrifugation of the water samples
All the samples were centrifuged at 1000×g for 10 minutes to concentrate the oocysts, cysts and eggs (García-Rodríguez, Köster, & Ponce-Gordo, 2022). A pellet was left at the bottom of the falcon tube after the supernatant was poured off. The pellet underwent direct wet smear, xenic cultivation, Ziehl Neelsens stain, floatation and McMaster techniques to recover and quantify the organisms.
Direct Wet Mount
This was used mainly for protozoa trophozoites. A small amount of concentrated water pellet was put on a microscope slide. A drop of iodine was added. The slide was covered with a cover slip. This was put under a microscope and observed under 10X objective and then 40X objective
Xenic cultivation
The non-nutritive media (Cheesbrough, 2006; Sente, Erume, Naigaga, Gabriela Namara, et al., 2016)was seeded with 0.1 ml of a heat-inactivated culture of Escherichia coli BL2 (Cheesbrough, 2006). The samples of water contained in the 50 ml tubes were centrifuged at 1000×g for 15 minutes in order to expose the pellets, and the supernatant was drained out. After the pellets were withdrawn from the tubes, they were carefully plated on NNA-EI agar plates that had already been seeded. The plates were then placed in an incubator and set to 320 degrees Celsius for the night. The following day, each plate was placed in an individual polyethene bag, then inverted and placed in an incubator at the same temperature for seven days. For the detection of amoebae trophozoites, a Motic® AE2000 Binocular inverted microscope manufactured (TED PELLA Inc. USA). Counting the trophozoites was done using a haemocytometer (Combrinck et al., 2015).
Ziehl-Neelsen carbol fuchsin staining for Cryptosporidium
In order to detect the oocysts of Cryptosporidium spp., a modified version of Ziehl-(ZN) Neelsen's carbol-fuchsin stain was utilised (Gideon, Njine, Nola, Menbohan, & Ndayo, 2007). After centrifugation, a few drops of water were placed on a slide and stained with ZN-carbol fuchsin stain for two minutes. The slide was then rinsed with tap water to remove any remaining stains. After this step, the sample was rinsed with 3% hydrochloric acid in 70% ethanol and then with water from the tap. The finished object was then counterstained with Brilliant Green for two minutes before being rinsed with tap water to remove any excess stain. At long last, the slide was allowed to air-dry before being examined under a microscope.
Zinc Sulphate floatation technique
Zinc Sulphate floatation technique (Cheesbrough, 2006; Parameshwarappa, Chandrakanth, & Sunil, 2012) was used to identify protozoan cysts and helminth eggs. A solution of zinc sulfate with a specific gravity of 1.18-1.2 was placed inside of a test tube. 1.5 ml of the concentrated water was added to the ZnSO4 solution in the test tube, which was then stirred. Then, Zinc Sulphate solution was poured into the test tube until it was full. The full test tube was covered with a grease-free slip and left for 15 minutes to give the cysts time to float. Then the cover slip was removed from the test tube, and placed on the microscope slide to examine for the presence of protozoan cysts and helminth eggs.
McMaster Technique
After centrifuging the water samples, the resultant pellet was passed through a sieve into a dish containing 45ml of saturated salt solution (Parameshwarappa et al., 2012). A sample of the mixture was placed in one of the McMaster chamber slides using a pipette and the procedure was repeated to fill the second chamber. The total number of helminth eggs and (oo)cysts in both of the etched areas of the slide were counted and multiplied by 100 to determine the number of (oo)cysts/eggs per gram.
Statistical Analysis
Water sample data
Data was analysed using SPSS (IBM, USA). Variables were summarised by the use of mean and standard error of the mean (SEM). Application of univariate analysis to compare prevalence across sampling sites was executed using cross-tabulation with a χ² test. All variables with a p-value of ≤ 0.05 were considered significant.
Prevalence of Parasites
Cryptosporidium,
Giardia, and different genera of FLA and helminths were identified (
Table 1 and 2). Most of these parasites are not included on the Uganda water contaminants list shown in
Table 3.
Overall prevalence
The overall percentage prevalence of the protozoan water parasites in the 408 water samples collected were as follows from highest to lowest: - FLA (56.6%),
Cryptosporidium spp. (38.2%),
Giardia spp. (36.5%),
Eimeria spp. (20.3%) and
Paramecium spp. (2.7%). Helminth had the following prevalence: - Strongyles (38.2%),
Ascaris spp. (33.3%), Trematodes (25%), Strongyloides (10.5%),
Toxocara spp. and
Cappillaria spp. (3.2%). Details shown in
Table 1.
Prevalence and mean of parasites across different sampling sites
Table 2 presents the percentage of parasites that are present at each water source (both natural and tap water) as well as the numerous natural sites that were taken into consideration. FLA were the most prevalent parasite across all sources (PTW, 58.3%; Natural water, 56.2%; R. Kyambura, 64.6%; KCB, 73.8%; FLS, 76.7% and KCM 32.6%). Meanwhile for helminth parasites, Strongyle eggs were the most observed (PTW, 36.9%; Natural water, 38.6%; R. Kyambura, 37.5% and FLS, 31.7%). This was followed
Ascaris spp. (KCB, (52.4% and MKC, 45.5%). Water from KCB was the most contaminated with parasites followed by FLS, R. Kyambura and lastly, MKC.
Natural water had significantly higher mean values compared to Tap water (PTW) for
Giardia spp. (Natural, 101.72±8.02; Tap, 83.33±14.15),
Cryptosporidium spp. (Natural, 92.16±7.24; Tap, 45.24±9.34),
Ascaris spp. (Natural, 94.12±7.95; Tap, 35.71±10.11). On the other hand, KCB (
Cryptosporidium spp., 223.81±21.33;
Giardia spp., 152.38±21.39; Trematodes, 114.29±23.1;
Ascaris spp., 164.28±22.57; Strongyle, 333.33±99.42) and FLS (
Cryptosporidium spp., 101.67±16.03;
Giardia spp., 148.33±22.61;
Trematodes, 46.67±13.12) compared to R. Kyambura and MKC had more parasite burden (
Table 2).
Table 2.
Prevalence and mean cross water sources.
Table 2.
Prevalence and mean cross water sources.
| Parasite |
|
Source |
|
|
|
|
|
| Protozoa |
|
PTW (n=84) |
Environ water (n=324) |
R. Kyambura (n=48) |
KCB (n=84) |
FLS (n=60) |
MKC (n=132) |
| FLA |
(+)(%) |
49(58.3) |
182(56.2) |
31(64.6) |
62(73.8) |
46(76.7) |
43(32.6) |
| |
Mean(±SEM) |
16.50±2.67 |
14.25±1.36 |
9.42±2.72 |
16.00±2.62 |
27.33±5.64 |
7.53±1.90 |
|
Cryptosporidium spp. |
(+)(%) |
22(26.2) |
134(41.4) |
14(29.2) |
62(73.8) |
28(46.7) |
30(22.7) |
| |
Mean(±SEM) |
45.24±9.34 |
92.16±7.24 |
37.50±9.24 |
223.81±21.33 |
101.67±16.03 |
53.79±10.28 |
|
Giardia spp. |
(+)(%) |
32(38.1) |
117(36.1) |
12(25) |
38(45.2) |
32(53.3) |
35(26.5) |
| |
Mean(±SEM) |
83.33±14.15 |
101.72±8.016 |
43.75±11.87 |
152.38±21.39 |
148.33±22.61 |
81.06±13.95 |
|
Eimeria spp. |
(+)(%) |
21(25) |
62(19.1) |
3(6.3) |
24(28.6) |
12(20) |
23(17.4) |
| |
Mean(±SEM) |
51.19±12.84 |
40.19±4.87 |
12.50±7.66 |
47.63±9.94 |
46.67±15.12 |
35.61±7.98 |
|
Paramecium spp |
(+)(%) |
0 |
11(3.4) |
3(6.3) |
6(7.1) |
0 |
2(1.5) |
| |
Mean(±SEM) |
0 |
3.80±1.31 |
8.33±5.012 |
11.91±5.46 |
0 |
1.14±.84 |
| Helminth |
|
|
|
|
|
|
|
| Trematodes |
(+)(%) |
16(19) |
85(26.2) |
8(16.7) |
30(35.7) |
12(20) |
17(12.9) |
| |
Mean(±SEM) |
47.62±11.67 |
49.51±6.36 |
18.75±6.42 |
114.29±23.1 |
46.67±13.12 |
28.79±7.18 |
|
Toxocara spp |
(+)(%) |
10(11.9) |
24(7.4) |
2(4.1) |
10(11.9) |
0 |
12(9.1) |
| |
Mean(±SEM) |
34.52±11.79 |
21.81±4.04 |
4.17±2.91 |
34.52±11.67 |
0 |
21.97±6.39 |
|
Ascaris spp |
(+)(%) |
13(15.5) |
123(38) |
8(16.7) |
44(52.4) |
11(18.3) |
60(45.5) |
| |
Mean(±SEM) |
35.71±10.11 |
94.12±7.95 |
16.67±5.44 |
164.28±22.57 |
53.33±17.38 |
133.33±14.85 |
| Strongyles |
(+)(%) |
31(36.9) |
125(38.6) |
18(37.5) |
40(47.6) |
19(31.7) |
48(36.4) |
| |
Mean(±SEM) |
152.38±30.88 |
171.32±23.66 |
83.33±25.50 |
333.33±99.42 |
111.67±30.54 |
139.39±23.65 |
| Strongyloides |
(+)(%) |
8(9.5) |
34(10.5) |
0 |
16(19) |
8(13.3) |
10(7.6) |
| |
Mean(±SEM) |
14.27±5.12 |
14.71±2.42 |
0 |
21.43±5.10 |
21.67±7.55 |
12.88±4.74 |
|
Cappillaria spp |
(+)(%) |
0 |
13(4) |
0 |
0 |
6(10) |
7(5.3) |
| |
Mean(±SEM) |
0 |
6.62±2.02 |
0 |
0 |
16.67±6.79 |
12.88±5.31 |
Table 3.
Water contaminant candidates list for Uganda.
Table 3.
Water contaminant candidates list for Uganda.
| Microbial contaminant name |
Information |
| Faecal coliforms |
Facultative anaerobic, rod-shaped, gram-negative, non-sporulating bacterium, that originates in the intestines of warm-blooded animals. In Uganda, they have been found in natural and domestic water (Haruna, Ejobi, & Kabagambe, 2005). Rapid recharge of the springs and other water bodies after rainfall leads to increased microbiological contamination (Howard, Pedley, Barrett, Nalubega, & Johal, 2003). |
| Total coliforms |
The total coliform counts in 90% of the samples collected from Kampala exceeded the WHO guideline for portable water (Haruna et al., 2005). |
| Faecal streptococcus |
Predominant in areas with low sanitation (Howard et al., 2003). |
|
Salmonella species |
Outbreaks due to the microbes (typhoid) have been predominant in many areas of the country, with more reports in Kampala (Parker et al., 2010; WHO, 2015a). Many strains isolated from several water sources in Kampala (Afema et al., 2016). |
| Escherichia coli |
Humans harbouring E. coli bacteria that is ≈75% similar to the one from primates (Goldberg, Gillespie, Rwego, Estoff, & Chapman, 2008). High levels found in Kampala water (Byamukama, Kansiime, Mach, & Farnleitner, 2000). |
Fresh water strains
(Actinobacteria,
Alpha-Betaproteobacteria, Bacteroidetes,
and Spirochaeta) |
65 strains from surface freshwater habitats (Hahn, Stadler, Wu, & Pockl, 2004). |
|
Legionella species |
Commonly isolated and is associated with industrial water plant and household water heaters (Anacarso et al., 2010). |
| Hepatitis |
Hepatitis A & E associated with water, mainly faecal oral route transmission (CDC, 2016; Teshale et al., 2010). |
|
Cryptosporidium species |
Faecal-oral route. It is a big problem in children, pregnant women, and immunocompromised individuals (Desai, Sarkar, & Kang, 2012; Salyer, Gillespie, Rwego, Chapman, & Goldberg, 2012). |
| Giardia lamblia |
Faecal-oral route. A big problem in children, pregnant women, and immunocompromised individuals (McElligott, Naaktgeboren, Makuma-Massa, Summer, & Deal, 2013). |
|
Mycobacterium species |
Tuberculous and non-tuberculous can exist in soil and water (Eaton, Falkinham, Aisu, & Daniel, 1995; Kankya et al., 2011) |
|
Shigella species |
Faecal-oral routes and many strains exist (Legros, Ochola, Lwanga, & Guma, 1998). |
|
Helicobacter species |
Unexpected variation in the prevalence of H. pylori infection in Uganda (Baingana, Enyaru, & Davidsson, 2014). |
| Vibrio cholerae |
Responsible for many death in many areas of Uganda (G. Bwire et al., 2013; G. Bwire, Mwesawina, Baluku, Kanyanda, & Orach, 2016). |
| |
|
Discussion
Even though many of them have the potential to have an effect on public health, free-living amoeba and helminths are not included on the list of contaminants that can be found in Uganda's drinking water. As a result, not a lot of attention is paid to finding out how they affect the quality of the water. This, combined with the ignorance and apathy of the local community toward the correct way to use water, creates an opportunity for water to serve as a hub for the transmission of parasites between humans, animals, and the environment. Exposure to a number of waterborne diseases can be caused by a confluence of factors, some of which include ignorance (Acheson; Mehta, 2013), environmental contamination, climate change (Levy et al., 2018), and improper waste disposal (Godfrey Bwire et al., 2020; Malik et al., 2012).
In Uganda, published information about waterborne parasites is scarce and only contains a few organisms that have occurred through major disease outbreaks. Although studies have been done on certain waterborne parasites, a lot remains unknown in many of Uganda’s naturally occurring water systems from where the largest percentage of rural communities obtain their water for domestic use. Monitoring of naturally occurring water from lakes, rivers, waterholes, and other ground water types is not given much attention in Uganda as evidently observed by scanty published information on waterborne parasites.
In the present study, we investigated the presence of waterborne parasites in natural water and piped tap water in QEPA. Both protozoan and helminth parasites were more abundant.
Free-living amoeba (FLA)
Piped Tap water had a higher prevalence of FLA than the natural water source, whereas, for the specific natural water sites, prevalence and mean numbers of FLA were higher in KCB, FLS and R. Kyambura compared to MKC. The high numbers could be explained by the presence of organic matter from rotting leaves, animal and human faeces which are from the run-off from the land, that often concentrate at the banks of the water bodies. This is consistent with findings from other studies which explain that microorganisms settle on the inner surfaces of water pipes later becoming a source of secondary microbial contamination (Rozej, Cydzik-Kwiatkowska, Kowalska, & Kowalski, 2015; Sente, Erume, Naigaga, Gabriela Namara, et al., 2016; Sente, Erume, Naigaga, Mulindwa, et al., 2016).
Cryptosporidium and Giardia
There is very scanty published information on Cryptosporidium spp. and Giardia spp. isolated from water samples in Uganda. The present study reports an overall prevalence of Cryptosporidium spp. and Giardia spp. from water at 38.2% and 36.5% respectively. The Prevalence of both parasites was higher at KCB (Cryptosporidium spp., spp. 73.8%; Giardia, 45.2%) and FLS (Cryptosporidium spp., 46.7%; Giardia spp., 53.3%) compared to R. Kyambura and MKC. In tap water, Cryptosporidium spp. was 26.2% and Giardia spp. 38.1%, with no significant difference when compared to natural water. Although there is limited published work on waterborne diseases in Uganda to compare these values with, some work has been done on faecal Cryptosporidium spp. and Giardia spp. in animals and humans (Nizeyi et al., 1999; Salyer et al., 2012; Salzer, Rwego, Goldberg, Kuhlenschmidt, & Gillespie, 2007). Elsewhere, in Ethiopia, 102 (26%) and 31 (8.1%) Giardia spp. and Cryptosporidium spp. infections were reported out of the 384 children’s stool samples examined (Tigabu, Petros, & Endeshaw, 2010). Findings by other researchers reveal that Cryptosporidium spp. and Giardia spp. have been more studied in faecal samples rather than directly from water samples, masking high risks to individuals getting the infections from contaminated water that is often falsely presumed clean and free of these parasites.
Over the past decade, Cryptosporidium spp. and Giardia spp. have emerged as major waterborne pathogens affecting the gastrointestinal tract of a wide range of vertebrates including humans, livestock, and non-human primates (Carmena, 2010; Xiao, Lal, & Jiang, 2004). Cryptosporidium spp. and Giardia spp. are known to cause human Cryptosporidiosis and Giardiasis, respectively. These diseases are associated with severe protozoan diarrhoea which often results in considerable morbidities and mortalities. Cryptosporidiosis and Giardiasis can be fatal in individuals with immune system disorders such as those with HIV/AIDS, or those that have recently undergone organ transplant or dialysis (CDC, 2015).
Helminths
Strongyle (38.2%) followed by Ascaris spp. (33.3%) were the commonest helminth types isolated, followed by trematodes (25%) and Strongyloides (10.5). Helminth eggs were found in all the Tap and Natural water sources. Helminth eggs can directly or indirectly have a significant health effect on humans, depending on the level of contamination of the water consumed, consequently causing gastrointestinal helminthiasis in children and adults. The presence of helminth eggs in domestic water sources in Uganda poses a risk of human infection in children and immunocompromised individuals (Kabatereine et al., 2014; Lwanga, Kirunda, & Orach, 2012). Use of untreated water is highly associated with higher odds of helminth infection (Strunz et al., 2014). Infection with helminth is often not considered lethal, but certain helminthic infections can cause devastating consequences in humans. Some trematodes such as Dicrocoelium and Fasciola can cause severe biliary obstruction (CDC, 2013; Cengiz, Yilmaz, Dulger, & Cicek, 2010) whereas Ascarids and large strongyles can cause intestinal obstruction if many of them occupy the lumen of the intestines (Haburchak, 2015). Strongyloides is known for causing gastrointestinal, pulmonary and dermatologic systems impairment (Hays, Thompson, Esterman, & McDermott, 2016; Rathor, Khillan, & Sarin, 2016). Haemonchus spp. for impairing normal platelet hemostatic function (Ghadirian & Arfaa, 1973) and Cappillaria spp. for hepatic capillariasis; hepatomegaly, eosinophilia, diarrhoea and weight loss (Hwang, 1998).
Parasite transmission through water: Risks and Public health concerns
Infective (oo)cysts of protozoa and helminth eggs shed by animals and humans into the environment are maintained and spread by water during rainy seasons when there is runoff of water containing human and animal faecal matter from land into the water bodies, which eventually end up at the points where communities fetch and utilise the water. Most protozoan and helminth parasite prevalence and mean intensities are higher in the rainy season than dry season (Nzeako, 1992; Obiamiwe, 1977; Woodburn et al., 2009). However, parasite incidences can be high throughout the rainy and dry seasons, often indicating poor disposal of human and animal excreta and a continuous pattern of infection (Woodburn et al., 2009). In natural water environment, the pathogens have been isolated widely from many water sources such as rivers, lakes, streams, water holes, roadside gutters and reservoirs that are used as sources of water for most rural dwelling households (Bonilla-Lemus et al., 2014; Kumar et al., 2014; Onichandran et al., 2014). Often inadequately treated domestic water (drinking water, bathing, cooking and recreational water) have an abundance of these pathogens. Although most of these pathogens are ubiquitous and naturally occurring in nature in normal concentrations, they are exacerbated by the addition of higher concentrations of (oo)cysts and eggs from agricultural run-off, urban wastewater effluents (Carmena, 2010) and for the case of QEPA, from continued unnecessary high human and animal faecal contamination. The QEPA local communities have poor personal hygiene habits, and few poorly built latrines, most of which are already filled up, compelling many to digging small holes in the ground and defecating outside, on open land. When there is a heavy downpour of rain, the faecal material is washed off into the River Kyambura, Kazinga channel, Lake George, Lake Edward and other water bodies that provide domestic water supply to the communities, and the protected area premises. Upon using this water, exposure to a variety of protozoa and helminth is not uncommon. The risk of human infection is much higher in immunocompromised individuals such as those with HIV/AIDS, diabetes, cancer and those who have recently undergone organ transport (CDC, 2015).
Control measures
Preventive measures are the most reliable approaches to curbing the risks associated with waterborne parasites (Carmena, 2010). Since contamination of domestic water supplies is the major source of infection, applying measures to reduce the number, and spread of (oo)cysts and eggs in the natural environment as well as improving water treatment techniques is vital (Bonilla-Lemus et al., 2014). The following approaches can be used to achieve this in QEPA:- (1) proper personal hygiene, and ensuring that water carrying vessels are regularly cleaned, (2) construction of ecosan toilets that will prevent human faecal material from entering into the water bodies, (3) good agricultural practices that minimise direct animal faecal contamination of natural waters, (4) providing water catchment protection to restrict access to important water point sources by animals, (5) regular water quality assessment to detect parasite types and levels of concentration, (6) applying innovative parasite detection techniques that are practical and cost-effective, yet with higher sensitivities and able o differentiate parasite species, (oo)cysts or eggs, and finally (6) be able to optimise water treatment methods, to get the best performing chemicals that can kill or reduce the parasites to a minimal non-worrying levels.
Conclusions
The findings of this study suggest that natural water bodies such as lakes, rivers, streams, and other related natural water sources pose a major risk of contamination of domestic water with parasites. The findings can also be used to predict future waterborne disease outbreaks. Although for the case of QEPA, after previous disease outbreaks, there has been minimal change in the use of water in ways that are likely to be safe. It is a big puzzle to explain this but probably these communities still require more sensitisation and an engagement with their political leaders or the government should be tasked to build more effective domestic water management and sanitation policies. Access to improved water sources should be corroborated with access to improved sanitation. Proper sanitation (e.g. improved toilets, latrines, and drainage systems) means there will be fewer effluents ending up in domestic water supply systems, hence clean water and fewer disease manifestations. For complete safety, it is also advisable not to take chances, but to use multiple control measure (personal hygiene, regular cleaning of vessels, proper storage, treating or boiling water) to avoid water-related illnesses.
In addition, given that QEPA is one of the protected areas in Uganda that receives the highest number of visitors from tourists, the piped tap water that flows in hotels and restaurants ought to be treated in a more efficient manner so as to prevent any waterborne parasites from causing illness in tourists.
Availability of data and materials
The majority of the information created or analysed during this study is presented in this article. The associated authors will provide the remaining data upon reasonable request.
Author Contributions
CS implemented field data collection, laboratory work, and drafting of the manuscript. MO supervised the work. AT and HO analysed the data. BM, BGN, JGM, CKD and PS developed the field study designs and participated in manuscript drafting. All authors read and approved the final version of the manuscript.
Authors Information: CS is a wildlife Veterinarian/public health professional and currently a Lecturer at Makerere University. HO is a PhD student. AT is a bio-statistician and lecture at Makerere University. BM is a lecturer at Makerere University. BGN is a medical doctors, microbiologist and public health expert. MO is an epidemiologist, Professor at Makerere University.
Acknowledgments
We would like to express our gratitude to the communities of QEPA, who allowed us to collect the samples. In addition, we would like to thank the teams working on parasitology at the College of Veterinary Medicine, Animal Resources and Biosecurity (COVAB) for the time they invested in the laboratory diagnostics.
Conflicts of Interest
There are no competing interests.
List of Abbreviations
| +ve: |
Positive |
| ⁰C: |
Celsius |
| AK: |
Amoebic Keratitis |
| FLA: |
Free-living amoeba |
| FLS: |
Fish landing site |
| GAE: |
Granulomatous amoebic encephalitis |
| g |
gravitational force |
| g: |
Grams |
| HIV/AIDS: |
Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome |
| KCB: |
Kazinga channel bank |
| MKC: |
Mid Kazinga channel |
| l: |
Liter |
| mg: |
Milligrams |
| ml: |
Milliliters |
| mM: |
millimolar |
| o.: |
Number |
| PA: |
Protected Area |
| PAM: |
Primary amoebic meningoencephalitis |
| pg: |
picogram |
| pmol: |
picomoles |
| Prev: |
Prevalence |
| QEPA: |
Queen Elizabeth Protected Area |
| rpm: |
revolutions per minute |
| SG: |
Specific Gravity |
| μS: |
Microseconds |
| UNESCO |
United Nations Educational, Scientific and Cultural Organization |
References
- Abdulkadir, N., & Kasirajan, A. The Occurrence of Waterborne Diseases inDrinking Water inNakaloke Sub-County, Mbale District, Uganda. International Journal of Science and Research (IJSR) 2016, 5, 1416.
- Acheson, D. W. K. Food and Waterborne Illnesses: Encyclopedia of Microbiology. 2009, 365-81. [CrossRef]
- Afema, J.A.; Byarugaba, D.K.; Shah, D.H.; Atukwase, E.; Nambi, M.; Sischo, W.M. Potential Sources and Transmission of Salmonella and Antimicrobial Resistance in Kampala, Uganda. PLOS ONE 2016, 11, e0152130–e0152130. [Google Scholar] [CrossRef] [PubMed]
- Anacarso, I.; Guerrieri, E.; Bondi, M.; de Niederhäusern, S.; Iseppi, R.; Sabia, C.; Contri, M.; Borella, P.; Messi, P. Influence of Legionella pneumophila and other water bacteria on the survival and growth of Acanthamoeba polyphaga. Arch. Microbiol. 2010, 192, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Angiro, C.; Abila, P.P.; Omara, T. Effects of industrial effluents on the quality of water in Namanve stream, Kampala Industrial and Business Park, Uganda. BMC Res. Notes 2020, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Baingana, R.K.; Enyaru, J.K.; Davidsson, L. Helicobacter pylori infection in pregnant women in four districts of Uganda: role of geographic location, education and water sources. BMC Public Heal. 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Boelee, E.; Geerling, G.; van der Zaan, B.; Blauw, A.; Vethaak, A.D. Water and health: From environmental pressures to integrated responses. Acta Trop. 2019, 193, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Lemus, P.; Villegas, A.S.C.; Jiménez, J.C.; Vázquez, A.L. Occurrence of free-living amoebae in streams of the Mexico Basin. Exp. Parasitol. 2014, 145, S28–S33. [Google Scholar] [CrossRef] [PubMed]
- Bwire, G.; Malimbo, M.; Maskery, B.; Kim, Y.E.; Mogasale, V.; Levin, A. The Burden of Cholera in Uganda. PLOS Neglected Trop. Dis. 2013, 7, e2545. [Google Scholar] [CrossRef] [PubMed]
- Bwire, G.; Mwesawina, M.; Baluku, Y.; Kanyanda, S.S.E.; Orach, C.G. Cross-Border Cholera Outbreaks in Sub-Saharan Africa, the Mystery behind the Silent Illness: What Needs to Be Done? PLoS ONE 2016, 11, e0156674. [Google Scholar] [CrossRef]
- Bwire, G.; Sack, D.A.; Kagirita, A.; Obala, T.; Debes, A.K.; Ram, M.; Komakech, H.; George, C.M.; Orach, C.G. The quality of drinking and domestic water from the surface water sources (lakes, rivers, irrigation canals and ponds) and springs in cholera prone communities of Uganda: an analysis of vital physicochemical parameters. BMC Public Heal. 2020, 20, 1–18. [Google Scholar] [CrossRef]
- Byamukama, D.; Kansiime, F.; Mach, R.L.; Farnleitner, A.H. Determination of Escherichia coli Contamination with Chromocult Coliform Agar Showed a High Level of Discrimination Efficiency for Differing Fecal Pollution Levels in Tropical Waters of Kampala, Uganda. Appl. Environ. Microbiol. 2000, 66, 864–868. [Google Scholar] [CrossRef]
- Carmena, D. (2010). Waterborne transmission of Cryptosporidium and Giardia: detection, surveillance and implications for public health. UK.
- CDC. (2013). Laboratory Identification of Parasitic Diseases of Public Health Concern. Retrieved from USA.
- CDC. (2015). Domestic Water, Sanitation, and Hygiene Epidemiology. Retrieved from http://www.cdc.gov/ncezid/dfwed/waterborne/domestic.html., from Center for Disease Control, United States of America http://www.cdc.gov/ncezid/dfwed/waterborne/domestic.html.
- CDC. (2016). Health Information for Travelers to UgandaTraveler View. Retrieved from http://wwwnc.cdc.gov/travel/destinations/traveler/none/uganda.
- CDC. (2020). Disease Threats and Global WASH Killers: Cholera, Typhoid, and Other Waterborne Infections. Retrieved from https://www.cdc.gov/healthywater/global/WASH.
- CDC. (2022). Global WASH Fast Facts. Retrieved from https://www.cdc.gov/healthywater/global/wash_statistics.
- Cengiz, Z.T.; Yilmaz, H.; Dülger, A.C.; Çiçek, M. Human infection with Dicrocoelium dendriticum in Turkey. Ann. Saudi Med. 2010, 30, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Cheesbrough, M. (2006). District Laboratory Practice in Tropical Countries (2nd ed.). New York, USA: Cambridge University Press.
- Collender, P.A.; Kirby, A.E.; Addiss, D.G.; Freeman, M.C.; Remais, J.V. Methods for Quantification of Soil-Transmitted Helminths in Environmental Media: Current Techniques and Recent Advances. Trends Parasitol. 2015, 31, 625–639. [Google Scholar] [CrossRef]
- Combrinck, J.M.; Fong, K.Y.; Gibhard, L.; Smith, P.J.; Wright, D.W.; Egan, T.J. Optimization of a multi-well colorimetric assay to determine haem species in Plasmodium falciparum in the presence of anti-malarials. Malar. J. 2015, 14, 1–14. [Google Scholar] [CrossRef]
- Kang, G.; Sarkar, R.; Desai, N.T. Cryptosporidiosis: An under-recognized public health problem. Trop. Parasitol. 2012, 2, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Eaton, T.; Falkinham, J.; Aisu, T.; Daniel, T. Isolation and characteristics of Mycobacterium avium complex from water and soil samples in Uganda. Tuber. Lung Dis. 1995, 76, 570–574. [Google Scholar] [CrossRef]
- Eurien, D.; Mirembe, B.B.; Musewa, A.; Kisaakye, E.; Kwesiga, B.; Ogole, F.; Ayen, D.O.; Kadobera, D.; Bulage, L.; Ario, A.R.; et al. Cholera outbreak caused by drinking unprotected well water contaminated with faeces from an open storm water drainage: Kampala City, Uganda, January 2019. BMC Infect. Dis. 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Fawell, J., & Nieuwenhuijsen, M. J. (2003). Contaminants in drinking water. Br Med Bull, 68, 199-208.
- García-Rodríguez, J.J.; Köster, P.C.; Ponce-Gordo, F. Cyst detection and viability assessment of Balantioides coli in environmental samples: Current status and future needs. Food Waterborne Parasitol. 2022, 26, e00143. [Google Scholar] [CrossRef]
- Ghadirian, E.; Arfaa, F. First Report of Human Infection with Haemonchus contortus, Ostertagia ostertagi, and Marshallagia marshalli (Family Trichostrongylidae) in Iran. J. Parasitol. 1973, 59, 1144–5. [Google Scholar] [CrossRef]
- Gideon, A.A.; Njine, T.; Nola, M.; Menbohan, S.F.; Ndayo, M.W. Évaluation de l’abondance des formes de résistance de deux protozoaires pathogènes (Giardia sp et Cryptosporidium sp) dans deux biotopes aquatiques de Yaoundé (Cameroun). 2008. [CrossRef]
- Goldberg, T.L.; Gillespie, T.R.; Rwego, I.B.; Estoff, E.L.; Chapman, C.A. Forest Fragmentation as Cause of Bacterial Transmission among Nonhuman Primates, Humans, and Livestock, Uganda. Emerg. Infect. Dis. 2008, 14, 1375–1382. [Google Scholar] [CrossRef]
- Haburchak, D. (2015). Ascariasis. Retrieved from USA: http://emedicine.medscape.com/article/212510-overview.
- Hahn, M.W.; Stadler, P.; Wu, Q.L.; Pöckl, M. The filtration–acclimatization method for isolation of an important fraction of the not readily cultivable bacteria. J. Microbiol. Methods 2004, 57, 379–390. [Google Scholar] [CrossRef]
- Haruna, R.; Ejobi, F.; Kabagambe, E.K. The quality of water from protected springs in Katwe and Kisenyi parishes, Kampala city. Uganda 2005, 5, 14–20. [Google Scholar]
- Hays, R.; Thompson, F.; Esterman, A.; McDermott, R. Strongyloides stercoralis, Eosinophilia, and Type 2 Diabetes Mellitus: The Predictive Value of Eosinophilia in the Diagnosis of S stercoralis Infection in an Endemic Community. Open Forum Infect. Dis. 2016, 3, ofw029. [Google Scholar] [CrossRef]
- Howard, G.; Pedley, S.; Barrett, M.; Nalubega, M.; Johal, K. Risk factors contributing to microbiological contamination of shallow groundwater in Kampala, Uganda. Water Res. 2003, 37, 3421–3429. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.P. Human intestinal capillariasis (Capillaria philippinensis) in Taiwan. 1998, 39, 82–5. [Google Scholar] [PubMed]
- Kabatereine, N.; Fleming, F.; Thuo, W.; Tinkitina, B.; Tukahebwa, E.M.; Fenwick, A. Community perceptions, attitude, practices and treatment seeking behaviour for schistosomiasis in L. Victoria islands in Uganda. BMC Res. Notes 2014, 7, 900. [Google Scholar] [CrossRef] [PubMed]
- Kabi, P. (2023). Factories Leave Trail of Faeces, Chemically Polluted Water in Two Major Towns. Retrieved from https://pulitzercenter.org/stories/factories-leave-trail-faeces-chemically-polluted-water-two-major-towns.
- Kankya, C.; Muwonge, A.; Djønne, B.; Munyeme, M.; Opuda-Asibo, J.; Skjerve, E.; Oloya, J.; Edvardsen, V.; Johansen, T.B. Isolation of non-tuberculous mycobacteria from pastoral ecosystems of Uganda: Public Health significance. BMC Public Heal. 2011, 11, 320–320. [Google Scholar] [CrossRef]
- Khanna, V.; Tilak, K.; Rasheed, S.; Mukhopadhyay, C. Identification and Preservation of Intestinal Parasites Using Methylene Blue-Glycerol Mount: A New Approach to Stool Microscopy. J. Parasitol. Res. 2014, 2014, 1–4. [Google Scholar] [CrossRef]
- Kim, Y.C.; Kim, J.J.; Lee, K.T. Evaluation of Giardia lamblia detection method in stool specimens fixed with SAF solution. Korean J. Parasitol. 1985, 23, 285–292. [Google Scholar] [CrossRef]
- Kochanowski, M.; Dąbrowska, J.; Karamon, J.; Cencek, T.; Osiński, Z. Analysis of the accuracy and precision of the McMaster method in detection of the eggs of Toxocara and Trichuris species (Nematoda) in dog faeces. Folia Parasitol. 2013, 60, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Kumar, T.; Lim, Y.A.L.; Sulaiman, W.Y.W.; Sawangjaroen, N.; Salibay, C.C.; Dungca, J.Z.; Onichandran, S.; Lau, Y.L.; Ithoi, I.; Nissapatorn, V.; et al. Comparative Study on Waterborne Parasites between Malaysia and Thailand: A New Insight. Am. J. Trop. Med. Hyg. 2014, 90, 682–689. [Google Scholar] [CrossRef] [PubMed]
- Lambeth, M. (2023). It’s 2023 and There’s Still a Global Water Crisis. Retrieved from https://impakter.com/its-2023-and-theres-still-a-global-water-crisis/.
- Legros, D.; Ochola, D.; Lwanga, N.; Guma, G. Antibiotic sensitivity of endemic Shigella in Mbarara. Uganda 1998, 75, 160–1. [Google Scholar]
- Levy, K.; Smith, S.M.; Carlton, E.J. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr. Environ. Heal. Rep. 2018, 5, 272–282. [Google Scholar] [CrossRef]
- Lwanga, F.; Kirunda, B.E.; Orach, C.G. Intestinal Helminth Infections and Nutritional Status of Children Attending Primary Schools in Wakiso District, Central Uganda. Int. J. Environ. Res. Public Heal. 2012, 9, 2910–2921. [Google Scholar] [CrossRef]
- Malik, A.; Yasar, A.; Tabinda, A.; Abubakar, M. Water-Borne Diseases, Cost of Illness and Willingness to Pay for Diseases Interventions in Rural Communities of Developing Countries. 2012, 41, 39–49.
- McElligott, J.T.; Naaktgeboren, C.; Makuma-Massa, H.; Summer, A.P.; Deal, J.L. Prevalence of intestinal protozoa in communities along the Lake Victoria region of Uganda. Int. J. Infect. Dis. 2013, 17, e658–e659. [Google Scholar] [CrossRef] [PubMed]
- Mehta, B. (2013). KNOWLEDGE ATTITUDE AND PRACTICES REGARDING WATER HANDLING AND WATER QUALITY ASSESSMENT IN A RURAL BLOCK OF HARYANA.
- Mirembe, L. (2014). Uganda rural water services: inadequate quantity, low quality, satisfied users. Retrieved from Uganda: http://www.ircwash.org/news/uganda-rural-water-services-inadequate-quantity-low-quality-satisfied-users.
- Muhereza, R. (Producer). (2009, 20-03-2016). Cholera, diarrhea & dysentery update 2009, Africa. Retrieved from http://promedmail.chip.org/pipermail/promed-eafr/2009-November/000137.html.
- Murei, A.; Mogane, B.; Mothiba, D.P.; Mochware, O.T.W.; Sekgobela, J.M.; Mudau, M.; Musumuvhi, N.; Khabo-Mmekoa, C.M.; Moropeng, R.C.; Momba, M.N.B. Barriers to Water and Sanitation Safety Plans in Rural Areas of South Africa—A Case Study in the Vhembe District, Limpopo Province. Water 2022, 14, 1244. [Google Scholar] [CrossRef]
- Nizeyi, J.B.; Mwebe, R.; Nanteza, A.; Cranfield, M.R.; Kalema, G.R.N.N.; Graczyk, T.K. Cryptosporidium sp. and Giardia sp. Infections in Mountain Gorillas (Gorilla gorilla beringei) of the Bwindi Impenetrable National Park, Uganda. J. Parasitol. 1999, 85, 1084–8. [Google Scholar] [CrossRef]
- Nzeako, B.C. Seasonal prevalence of protozoan parasites in Nsukka. Nigeria 1992, 24, 224–30. [Google Scholar]
- Obiamiwe, B.A. The pattern of parasitic infection in human gut at the Specialist Hospital, Benin City, Nigeria. Ann. Trop. Med. Parasitol. 1977, 71, 35–43. [Google Scholar] [CrossRef]
- Oguttu, D.W.; Okullo, A.; Bwire, G.; Nsubuga, P.; Ario, A. Cholera outbreak caused by drinking lake water contaminated with human faeces in Kaiso Village, Hoima District, Western Uganda, October 2015. Infect. Dis. Poverty 2017, 6, 146. [Google Scholar] [CrossRef] [PubMed]
- Omarova, A.; Tussupova, K.; Hjorth, P.; Kalishev, M.; Dosmagambetova, R. Water Supply Challenges in Rural Areas: A Case Study from Central Kazakhstan. Int. J. Environ. Res. Public Heal. 2019, 16, 688. [Google Scholar] [CrossRef] [PubMed]
- Onichandran, S.; Kumar, T.; Salibay, C.C.; Dungca, J.Z.; AL Tabo, H.; Tabo, N.; Tan, T.-C.; AL Lim, Y.; Sawangjaroen, N.; Phiriyasamith, S.; et al. Waterborne parasites: a current status from the Philippines. Parasites Vectors 2014, 7, 244–244. [Google Scholar] [CrossRef]
- Parameshwarappa, K., Chandrakanth, C., & Sunil, B. (2012). The Prevalence of Intestinal Parasitic Infestations and the Evaluation of Different Concentration Techniques of the Stool Examination Clinical and Diagnostic Research, 6(7), 1188 - 1191.
- Parker, A.H.; Youlten, R.; Dillon, M.; Nussbaumer, T.; Carter, R.C.; Tyrrel, S.F.; Webster, J. An assessment of microbiological water quality of six water source categories in north-east Uganda. J. Water Heal. 2010, 8, 550–560. [Google Scholar] [CrossRef] [PubMed]
- Khillan, V.; Rathor, N.; Sarin, S.K. Strongyloides stercoralis hyperinfection in patient with autoimmune hepatitis and purpura fulminans. Indian J. Crit. Care Med. 2016, 20, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Batlle, M.; Sifaoui, I.; Rodríguez-Expósito, R.L.; Piñero, J.E.; Lorenzo-Morales, J. New Insights in Acanthamoeba. Pathogens 2022, 11, 609. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L. (2019). Factors Driving the Water & Sanitation Crisis in Africa. Retrieved from https://www.globalcitizen.org/en/content/water-and-sanitation-crisis-sub-saharan-africa/#:~:text=Of%20the%20783%20million%20people,are%20in%20sub%2DSaharan%20Africa.
- Rożej, A.; Cydzik-Kwiatkowska, A.; Kowalska, B.; Kowalski, D. Structure and microbial diversity of biofilms on different pipe materials of a model drinking water distribution systems. World J. Microbiol. Biotechnol. 2014, 31, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Salyer, S.J.; Gillespie, T.R.; Rwego, I.B.; Chapman, C.A.; Goldberg, T.L. Epidemiology and Molecular Relationships of Cryptosporidium spp. in People, Primates, and Livestock from Western Uganda. PLOS Neglected Trop. Dis. 2012, 6, e1597. [Google Scholar] [CrossRef] [PubMed]
- Salzer, J.S.; Rwego, I.B.; Goldberg, T.L.; Kuhlenschmidt, M.S.; Gillespie, T.R. Giardia sp. and Cryptosporidium sp. Infections in Primates in Fragmented and Undisturbed Forest in Western Uganda. J. Parasitol. 2007, 93, 439–440. [Google Scholar] [CrossRef]
- Sarink, M.J.; van der Meijs, N.L.; Denzer, K.; Koenderman, L.; Tielens, A.G.M.; van Hellemond, J.J. Three encephalitis-causing amoebae and their distinct interactions with the host. Trends Parasitol. 2022, 38, 230–245. [Google Scholar] [CrossRef]
- Sente, C.; Erume, J.; Naigaga, I.; Namara, B.G.; Mulindwa, J.; Ochwo, S.; Magambo, P.K.; Kato, C.D.; Tamale, A.; Ocaido, M. Xenic Cultivation and Genotyping of Pathogenic Free-Living Amoeba from Public Water Supply Sources in Uganda. New J. Sci. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Sente, C.; Erume, J.; Naigaga, I.; Mulindwa, J.; Ochwo, S.; Magambo, P.K.; Namara, B.G.; Kato, C.D.; Sebyatika, G.; Muwonge, K.; et al. Prevalence of pathogenic free-living amoeba and other protozoa in natural and communal piped tap water from Queen Elizabeth protected area, Uganda. Infect. Dis. Poverty 2016, 5, 1–14. [Google Scholar] [CrossRef]
- Setiawan, B., Nuryati, A., & Sofiarahma, A. (2020). Sensitivity and Specificity of NaCl and ZnSo 4 Solution Flotation Method for Examination of Worm Eggssoil Transmitted Helminths (STH). Pakistan Journal of Medical and Health Sciences, 14, 1524.
- Ssemugabo, C.; Wafula, S.T.; Ndejjo, R.; Oporia, F.; Osuret, J.; Musoke, D.; Halage, A.A. Knowledge and practices of households on safe water chain maintenance in a slum community in Kampala City, Uganda. Environ. Heal. Prev. Med. 2019, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Strunz, E.C.; Addiss, D.G.; Stocks, M.E.; Ogden, S.; Utzinger, J.; Freeman, M.C. Water, Sanitation, Hygiene, and Soil-Transmitted Helminth Infection: A Systematic Review and Meta-Analysis. PLOS Med. 2014, 11, e1001620. [Google Scholar] [CrossRef] [PubMed]
- Tahvildar-Biderouni, F.; Salehi, N. Detection of Cryptosporidium infection by modified ziehl-neelsen and PCR methods in children with diarrheal samples in pediatric hospitals in Tehran. 2014, 7, 125–130.
- Teshale, E.H.; Howard, C.M.; Grytdal, S.P.; Handzel, T.R.; Barry, V.; Kamili, S.; Drobeniuc, J.; Okware, S.; Downing, R.; Tappero, J.W.; et al. Hepatitis E Epidemic, Uganda. Emerg. Infect. Dis. 2010, 16, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Tigabu, E.; Petros, B.; Endeshaw, T. Prevalence of Giardiasis and Cryptosporidiosis among children in relation to water sources in Selected Village of Pawi Special District in Benishangul-Gumuz Region, Northwestern Ethiopia. Ethiop. J. Heal. Dev. 2011, 24. [Google Scholar] [CrossRef]
- WHO. (2007). Combating waterborne disease at the household level. Retrieved from USA. : http://www.who.int/household_water/advocacy/combating_disease/en/.
- WHO. (2015a). Emergencies preparedness, and response to Typhoid fever, Uganda. Retrieved from http://www.who.int/csr/don/17-march-2015-uganda/en/. Retrieved 2015/12/09, from WHO Regional Office for Africa http://www.who.int/csr/don/17-march-2015-uganda/en/.
- WHO. (2015b). Typhoid fever – Uganda; Emergencies preparedness, response Retrieved from USA: http://www.who.int/csr/don/17-march-2015-uganda/en/.
- WHO. (2022). Water, sanitation and hygiene (WASH). Retrieved from https://www.who.
- Woodburn, P.W.; Muhangi, L.; Hillier, S.; Ndibazza, J.; Namujju, P.B.; Kizza, M.; Ameke, C.; Omoding, N.E.; Booth, M.; Elliott, A.M. Risk Factors for Helminth, Malaria, and HIV Infection in Pregnancy in Entebbe, Uganda. PLOS Neglected Trop. Dis. 2009, 3, e473. [Google Scholar] [CrossRef]
- WWF Water Scarcity | Threats | WWF. Available online: https://www.worldwildlife.org/threats/water-scarcity (accessed on 27 February 2021).
- Xiao, L.; Lal, A. A.; Jiang, J. Detection and differentiation of Cryptosporidium oocysts in water by PCR-RFLP. Methods Mol Biol 2004, 268, 163–176. [Google Scholar] [CrossRef]
Table 1.
Overall prevalence of water parasites.
Table 1.
Overall prevalence of water parasites.
| Overall Prevalence |
|
|
| Parasite |
Frequency (n=408) |
Prevalence (%) |
| Protozoa |
|
|
| Free Living Amoeba |
231 |
56.6 |
|
Cryptosporidium sp |
156 |
38.2 |
|
Giardia sp. |
149 |
36.5 |
|
Eimeria sp. |
83 |
20.3 |
|
Paramecium spp |
11 |
2.7 |
| Helminths |
|
|
| Strongyles |
156 |
38.2 |
|
Ascaris spp. |
136 |
33.3 |
| Strongyloides |
42 |
10.5 |
|
Toxocara spp. |
34 |
8.3 |
|
Cappillaria spp. |
13 |
3.2 |
| Trematodes |
101 |
25 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).