Introduction
Various waves of SARS-CoV-2 virus infection in India has led to one of the world’s highest totals of confirmed COVID-19 case totals (45 million as of Oct 1, 2022), with about 3-4 million excess deaths in independent studies analysing registered deaths or national surveys. By contrast, only 0.6 million deaths are reported by official government data sources (Coronavirus.app, 2022; Jha et al., 2022).
Three major viral waves occurred in India. The first wave of 6 months occurred from June 2020-November 2020 and peaked in late September 2020, with moderate increases in excess deaths from the virus (Coronavirus.app, 2022). We refer to this wave as “Aleph”. The Aleph wave was due mostly to the original virus that originated from Wuhan Province China, with some B.1.1.7 (Alpha) and B.1.617.1 (Kappa) variants of concern. The Delta wave of 4 months occurred from March-June 2021 was due predominantly to the B.1.617.2 variant (which is known for greater transmissibility and reduced responsiveness to vaccines (Cherian et al., 2021; Mlcochova et al., 2021)) and was characterized by the largest spike in excess deaths. The Omicron wave mostly in January 2022 caused widespread infection but far lower mortality and was due predominately to the B.1.1.529 variant.
Despite India collecting large amounts of testing data in central repositories, little testing or viral load data are available publicly. In the absence of reasonably representative national data, careful examination of sub-national settings can inform our understanding of the virus and transmission patterns in India (Walker et al., 2021). Intergenerational households are the norm in Mumbai City, with 13 million people, and about 65% of its population live in cramped, often poorly ventilated slum housing, allowing for easy transmission of the virus (Ghosh et al., 2020). Moreover, Mumbai is considered a bellwether setting which showed the earliest increases and declines during each viral wave (Velumani et al., 2021). The Municipal Corporation of Greater Mumbai (MCGM) reports over one million real-time polymerase chain reaction (PCR) confirmed cases and 17,000 confirmed COVID deaths since March 2020 (Gov-MH, 2022; MCGM, 2022a). However, these reports underestimate true numbers as even by the end of the first wave, serosurveys suggested that about a third of adults including nearly half of adult slum dweller had SARS-CoV-2 antibodies (Velumani et al., 2021; NITI-Aayog et al., 2020).
Here, we examine data from a private but widely-used laboratory in Mumbai, capturing over 2.7 million individual PCR testing data with a subset providing information on viral load, as defined by inverse of the cycle threshold (Ct) values. Ct values are considered as a proxy for viral load, particularly if tested in early stages of the infection (He et al., 2020). We quantify differences in positivity and viral load during the three waves, and quantify each wave by sex, age, and slum population density, as well as the time lags.
Methods
Data Sources
We included 2.7 million people of all ages who underwent PCR testing between 9 April 2020 and 30 January 2022 by a large commercial laboratory (Thyrocare) with many franchises throughout Mumbai. Thyrocare has been approved by the Indian government for Covid-19 testing and conducts all testing in one facility in Navi Mumbai, with samples sent daily from franchise locations (ICMR, 2020). Participants had to pay 600-750 Rupees (
$8 to 10 USD) per test. All records were anonymised with no identifiable patient information. The available data includes the date of test, age, sex, and 6-digit postal code of tested individual. Reasons for testing were not recorded, but the tested population includes those referred by physicians, hospitals, quarantine centers, and self-referrals from both public and private sectors. For each record, we extracted the PCR results, and from 22 August 2020 onwards, the Ct values among all PCR positives. We mapped individual pin codes to municipal wards (
Table A2). Individuals from about 5% of pin codes that cut across municipal wards were assigned to the ward with the largest population in that pin code. We collected publicly available PCR confirmed cases and deaths, published in tabular form by age, sex, and municipal ward from the MCGM Covid-19 portal (MCGM, 2022a; 2022b; Banaji, 2022). MCGM provides estimates of the sex-specific total population and proportion living in slums (
Table A1) for each ward. Research Ethics approval was provided by Unity Health Toronto.
Laboratory Methods
Nasopharyngeal or oropharyngeal or combined specimens from each person were collected into a barcoded sterile tube containing transport medium and transported within one day to the central Thyrocare laboratory. All six commercial PCR kits used for diagnosis were approved by the Indian Council of Medical Research (ICMR;
Table A3), with independent validation to establish each assay’s high sensitivity and specificity. The Ct value was defined as the number of cycles required for the fluorescent signal to cross the detection threshold. Ct levels are inversely proportional to the amount of target nucleic acid in the sample (i.e., the lower the Ct level the greater the amount of target nucleic acid; each unit of Ct represents a doubling of viral load). Ct values between 0 to 35 ranges were considered as test positive (Das et al., 2021) and values <30 were considered strongly positive (Das et al., 2021; PHE, 2020; Service et al., 2022; Bayat et al., 2021).
Statistical Methods
Usually laboratory PCR test results were generally used only as binary positive or negative outcomes. However, these test results contain a great deal of information than that. Although there are challenges to relying on single Ct values for individual-level decision-making, even a limited aggregation of data from a population can inform on the trajectory of the pandemic (Hay et. al., 2021). We calculated the daily PCR positivity rate (percent positive among total tested) and median Ct values from Thyrocare data. We plotted the 7-day moving average of community-level PCR positivity rates and median Ct values from Thyrocare data along with official PCR confirmed cases and death counts from MCGM’s COVID-19 dashboard. We used Pearson correlation coefficients to determine the simple agreements between these time series.
We used generalized additive models (Wood, 2017; Andriamandimby et al., 2022) to model changes in the daily median Ct value and in PCR positivity over time. We modelled daily median Ct value with a normal distribution, and applied a logistic model for the number of daily positive/negative PCR tests. We included a day-of-week effect and a smoothly varying time trend having a second derivative penalty. The model included a daily (normally distributed) overdispersion term. Model parameters were estimated with maximum likelihood.
The age distributions of MCGM confirmed cases and Thyrocare cases were slightly varying between the outbreak periods (
Table A4 and
Table A5), thus we adjusted the ages to the 5-yearly age distribution of 2011 census (ORGCC, 2021) in all calculations of PCR positivity rates and median Ct values.
Given that the PCR positivity and the median Ct values varied by age, sex, and municipal wards over 3 pandemic waves, we created a multivariate logistic model to investigate the effects of age (10 yearly classified with 20-29 years as the reference), sex (males as the reference) and the slums population density (high: more than 60% of the population living in slums; medium: 33%-60%; and low: up to 32% with low slum density as the reference) on PCR positivity for each wave. We created a similar proportional logistic model with the same explanatory variables to examine high versus medium viral load groups for each viral wave by classifying the groups using Ct quartile ranges (high: 25% or less, medium: 25%-75%, low: 75% or more), comparing the highest viral load (i.e., low Ct) to the medium range as the reference. Comparisons of low Ct to the high Ct value quartiles yielded similar results (data not shown). We used R software version 4.1.0 to fit the generalized additive models and SAS software version 9.4 to perform all other statistical analyses (R Core Team, 2017; SAS Inc, 2015).
Results
Over 2.7 million PCR tests for SARS-CoV-2 were conducted at Thyrocare from April 2020 to January 2021, with 2.2 million during the non-outbreak months. The overall PCR positivity was 5.3%, ranging from 3.4% during the non-outbreak months, rising to 23.2% and 42.8% during the Aleph and Omicron waves, respectively, but a surprisingly small increase to 9.9% during the Delta wave. PCR positivity was generally higher in women than in men and higher at older ages and in areas with higher slum density (
Table 1).
The median Ct value for period from September 2020 to January 2022 was 24.0 (interquartile range 19.0-28.0). Median Ct values were similar during the non-outbreak months (25.0) and the Aleph wave (26.0) but notably lower during the Delta (23.0) and Omicron waves (23.2). The differences of about two Ct units from non-outbreak months represents an approximately 4-fold higher viral load. During the Aleph and Omicron waves, the median Ct values were similar in areas with low, medium or high slum density, but during the Delta wave, medium and high slum density areas had lower Ct values by two or three units in absolute Ct values (or 4-fold to 8-fold higher viral load).
The PCR testing data covered all 24 wards and 83 of 91 postal pin codes within Mumbai and suburban districts (
Table A1 and
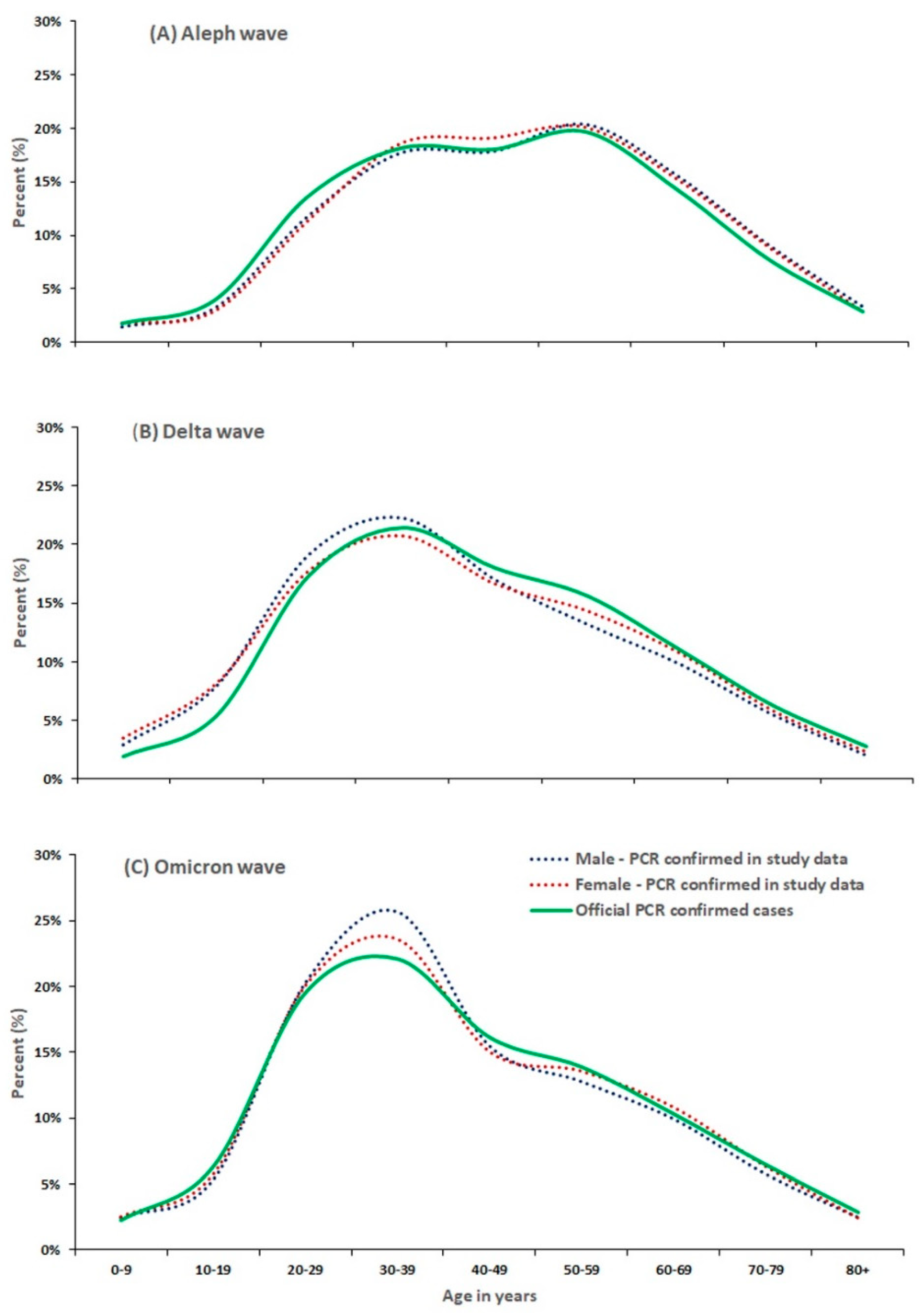
Table A2). The age distribution for men and women testing PCR positive in the Thyrocare laboratories was similar to the overall distributions among 830 000 confirmed cases, a subset of data reported by the MCGM (
Figure 1). In Thyrocare and MCGM data, the Aleph wave was characterized by a dual peak of PCR positivity around age 30 and at age 60 years, whereas PCR positivity during the Delta and Omicron waves peaked around age 30 years.
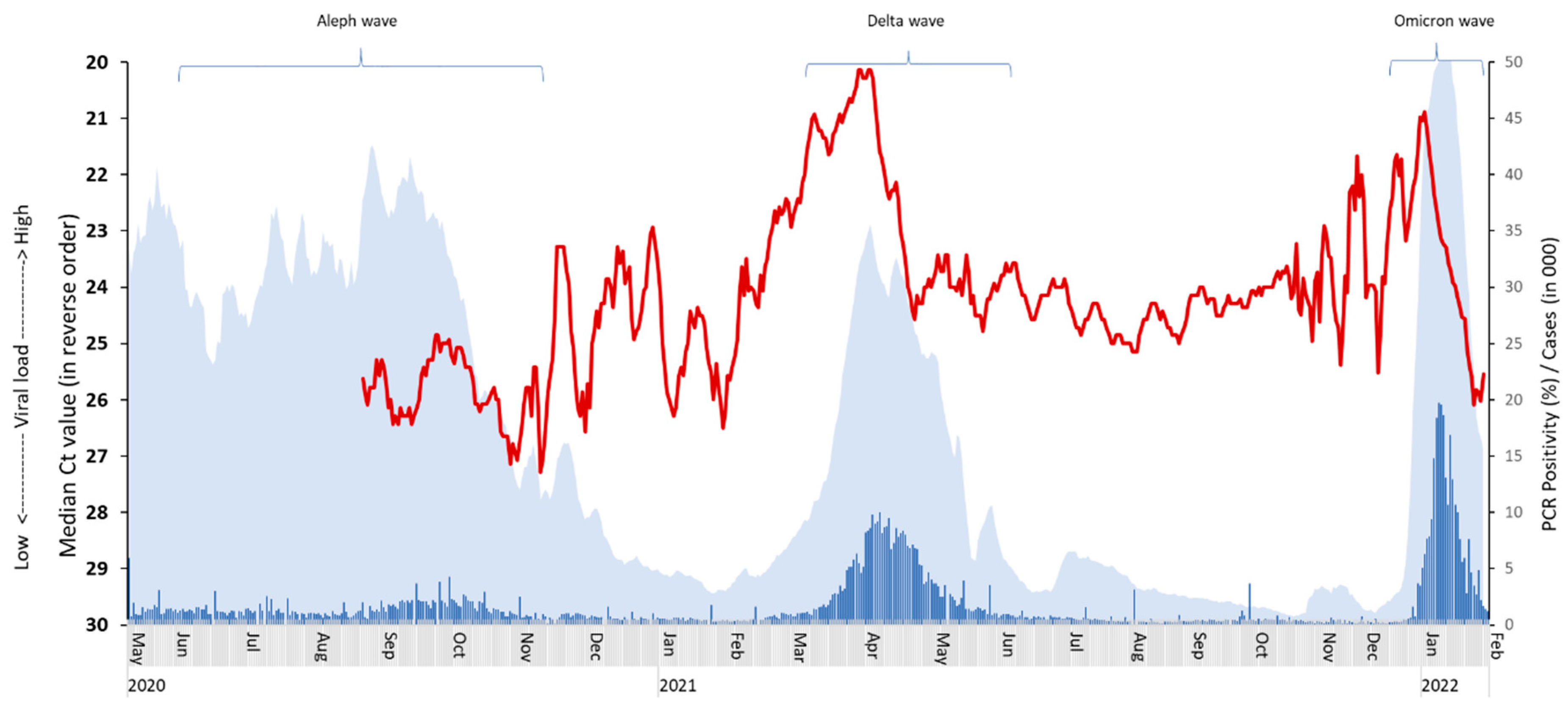
The 7-day averages of MCGM reported PCR confirmed cases correlated temporally with Thyrocare PCR positivity rates and the inverse of the median Ct values (
Figure A2; with higher viral load shown to rise vertically). The Pearson correlation coefficients showed agreement between PCR confirmed case counts in MCGM and PCR positivity and median Ct values for each wave were: Aleph (0.46, n.a.), Delta (0.94, -0.67) and Omicron (0.85, -0.88) respectively. Daily deaths, which are likely with substantial undercounts, were also correlated with Thyrocare results (data not shown).
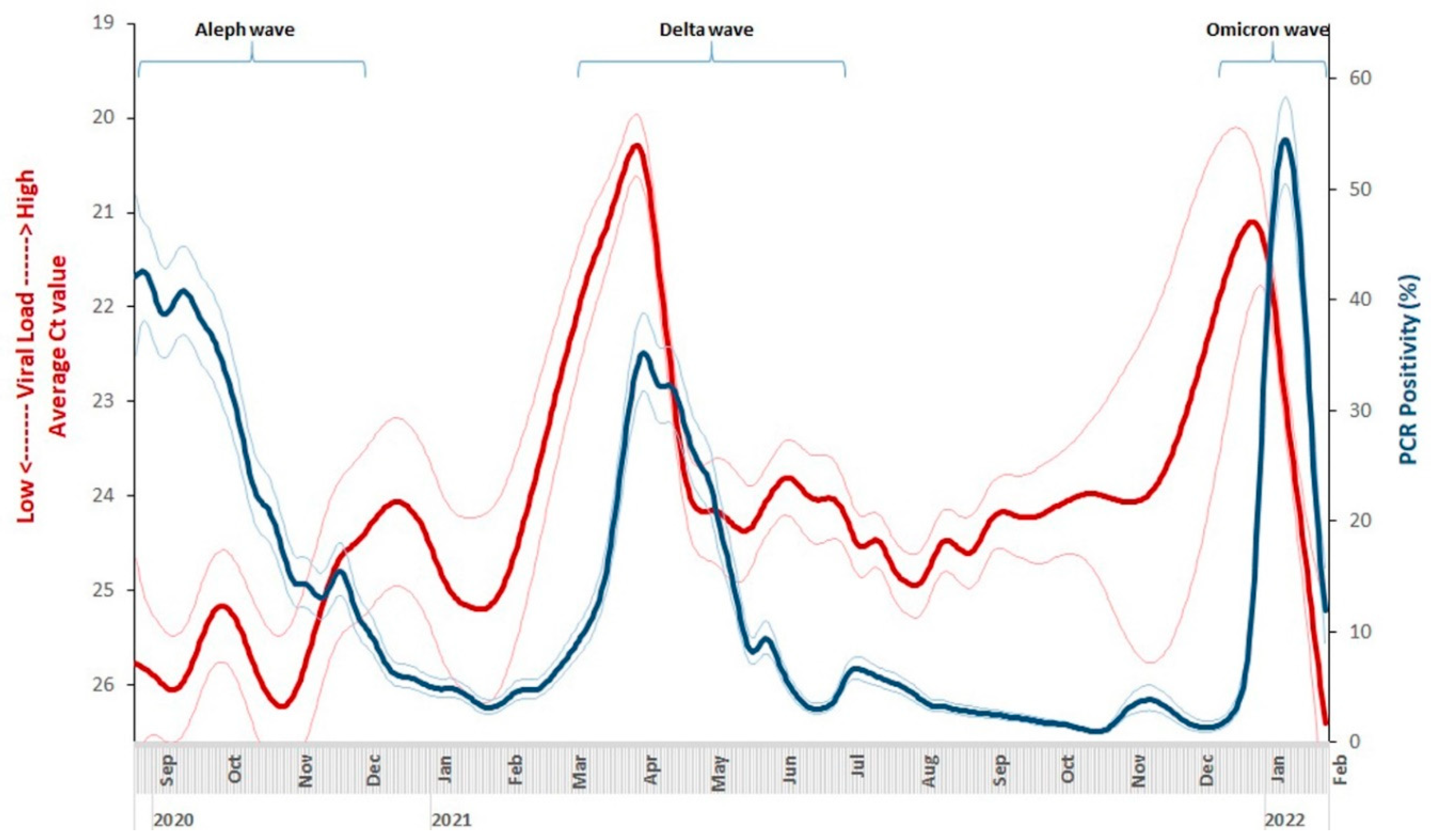
The rise in median viral load (inverse of Ct values) was substantial during the Delta wave, with a six-unit drop in Ct value representing a 64-fold increase in community viral load. By contrast, during the Omicron wave, the viral load rose less sharply with an absolute Ct value difference of about three, representing an 8-fold higher viral load, and the period of higher viral load was of a shorter duration that during the Delta wave. The predicted smoothed daily time series of PCR positivity and median Ct values from generalized additive models (
Figure 2) were similar to the 7-day daily median counterparts (
Figure A2). The 95% confidence intervals of the daily predicted values show higher uncertainty for daily median Ct value in September 2020 to February 2021 and for both daily median Ct value and PCR positivity in November to December 2022, largely reflecting reduced testing volumes during this period.
The beginning, peak, and the end of each COVID wave was determined from the rise and fall of individual curves of viral load (Ct values) and PCR positivity using the 7-day averages as shown in
Figure A2. In each wave, the first detected change was in the viral load, followed by PCR positivity and lastly by MCGM reported deaths (
Table A7). Ct values also declined first from the peaks. During the Delta wave, the increase in viral load began on February 1, 2021 and peaked on March 31, 2021, which were about 5 and 17 days earlier than the rise and peak in PCR positivity, respectively. During the Omicron wave, the increase in viral load (December 11, 2021) and the peak (January 2, 2022) also preceded the rise in cases and peak PCR positivity about 10 days. For the beginning-to-peak duration, the Delta wave lasted twice as many days (46-58) than the Omicron wave (20-22). For the peak-to-end duration for the Delta wave, viral load increases lasted for 49 days, PCR positivity for 72 days, MCGM reported confirmed cases for 90 days, and MCGM reported deaths lasted longest with 99 days.
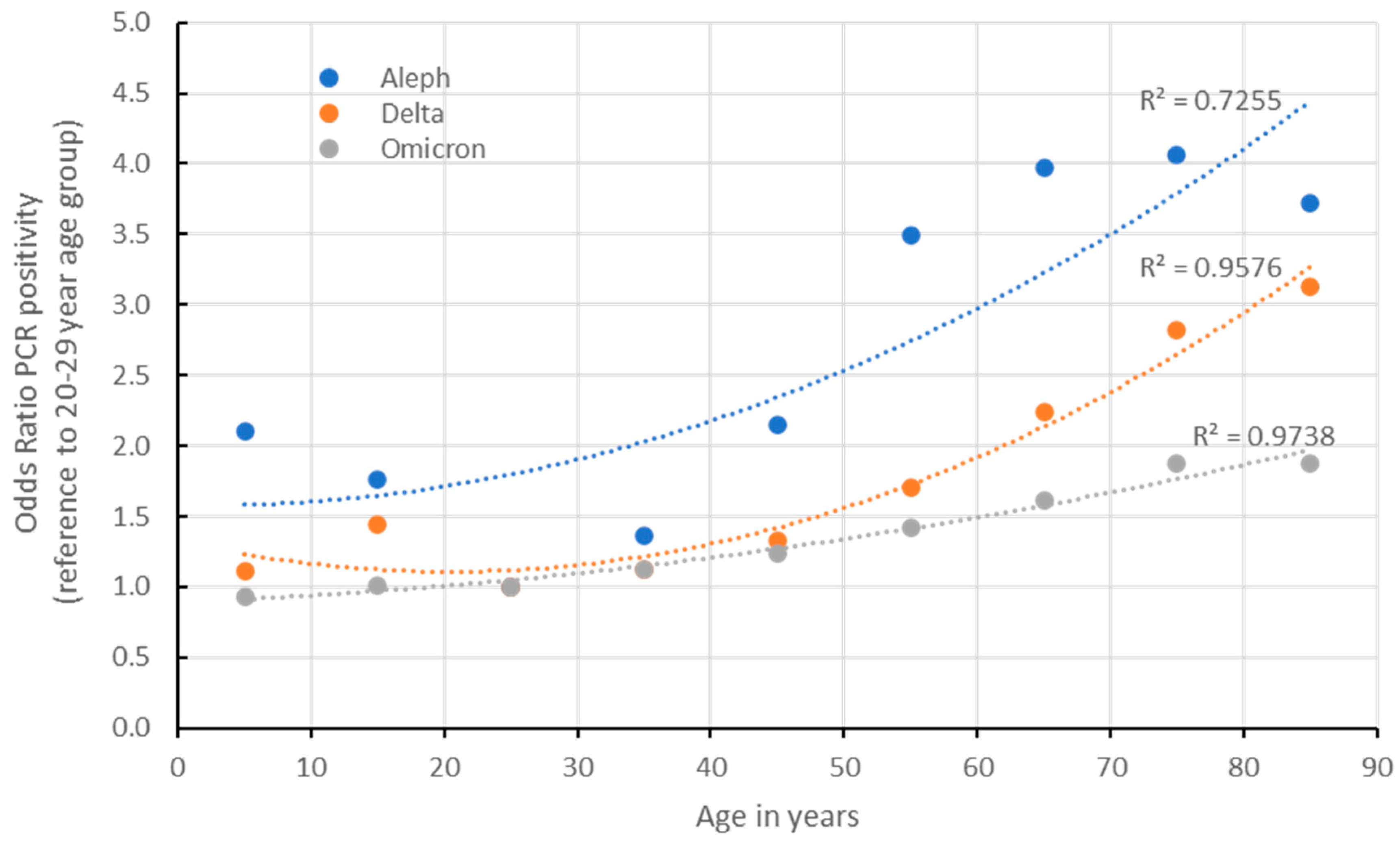
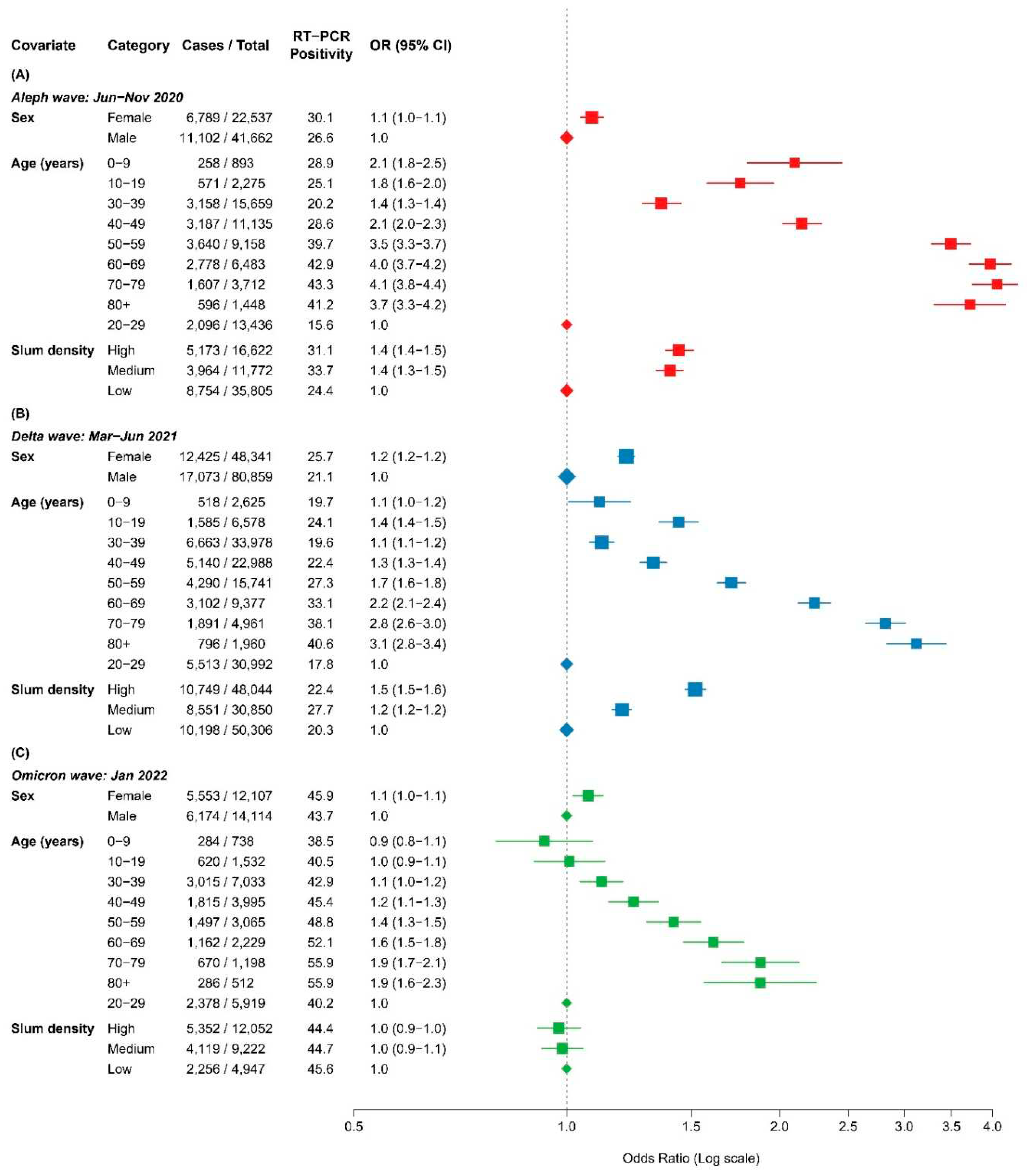
Because of the strong age, sex, and slum density patterns of both PCR positivity and median Ct values, multivariate analyses considering each is required. Among the Thyrocare tested population, PCR positivity was higher in females in all three viral waves (
Figure 3), and there was a notable age gradient in the multivariate odds ratio of being PCR positive when compared to the reference age group of 20-29 years (age test for trend for each has p <0.0001;
Figure A1). During the early Aleph and Delta waves, areas with high or medium slum density had higher odds of PCR positivity than low slum areas, but these differences were not seen during the Omicron wave.
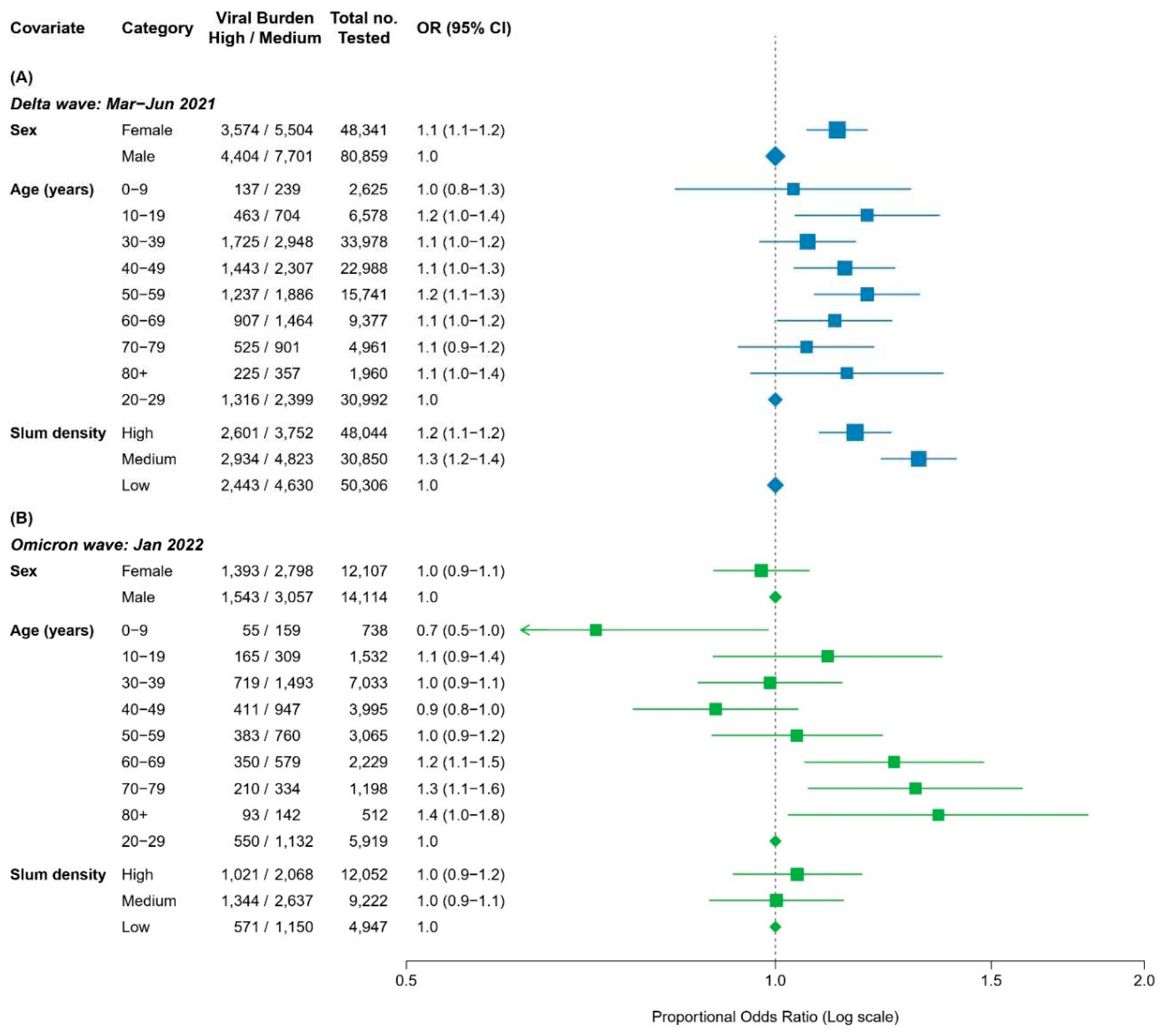
Figure 4 shows similar examination of the multivariate predictors of viral load, comparing the highest quartile to the middle two quartiles during the Delta and Omicron waves, which correspond to an absolute difference of 5 and 3.7 in Ct values (or 32-fold and 13-fold differences in community viral load). Females tended to have higher viral load during the Delta wave but not during the Omicron wave. Similarly, areas with high or medium slum density had higher odds ratio of high viral load during the Delta wave, but these differences disappeared during the Omicron wave. During the Delta wave, ages 30 years or older had somewhat higher odds ratio of high viral load, but during Omicron, the higher odds ratio were seen at ages 60 years and older.
Discussion
Our analyses of a large dataset covering PCR positivity and viral load in Mumbai, India show the remarkably high levels of transmission occurred during the Delta and Omicron waves. The Delta wave was characterized by rapid, 64-fold increases in population medians of viral load compared to the weeks prior to the Delta wave. The rise in viral load preceded changes in PCR confirmed cases by at least 7 days in both the Delta and Omicron waves, reflecting increases in transmission caused by these high viral loads. The Delta wave was noted for high viral loads in areas of high or medium slum density, and in women. By contrast, the differences in viral load by sex and for slum density had disappeared during the Omicron wave. This may reflect the lower pathogenicity of the Omicron strain in combination with (unobserved) changes in reasons for being tested. While all three waves showed rising PCR positivity with age, a notably increased risk of high viral load persisted among adults over age 60 years during the Omicron wave.
India’s Delta wave was particularly lethal, causing close to 3 million deaths (Jha et al., 2022). This high total arose from the biological features of the virus itself, including tropism for infecting lower respiratory tract cells that would directly influence case fatality rates. The major excess in Delta wave deaths may also reflect widespread community transmission, in particular by multiple exposures to infected people raising an individual’s probability of infection, as well as the probability of becoming infected with the most infectious strain. The rapid 64-fold increase in viral load during Delta was consistent with rapid and mostly uncontrolled community transmission, including widespread intergenerational household transmission. Paradoxically, the much smaller increase in PCR test positivity rates during the Delta wave (only about 10% versus 3% during non-outbreak weeks) than seen in other waves likely reflect such widespread multi-generational infection within homes, so that many infected individuals simply did not get tested. An alternative explanation might be that Delta was not highly transmissible but extremely pathogenic.
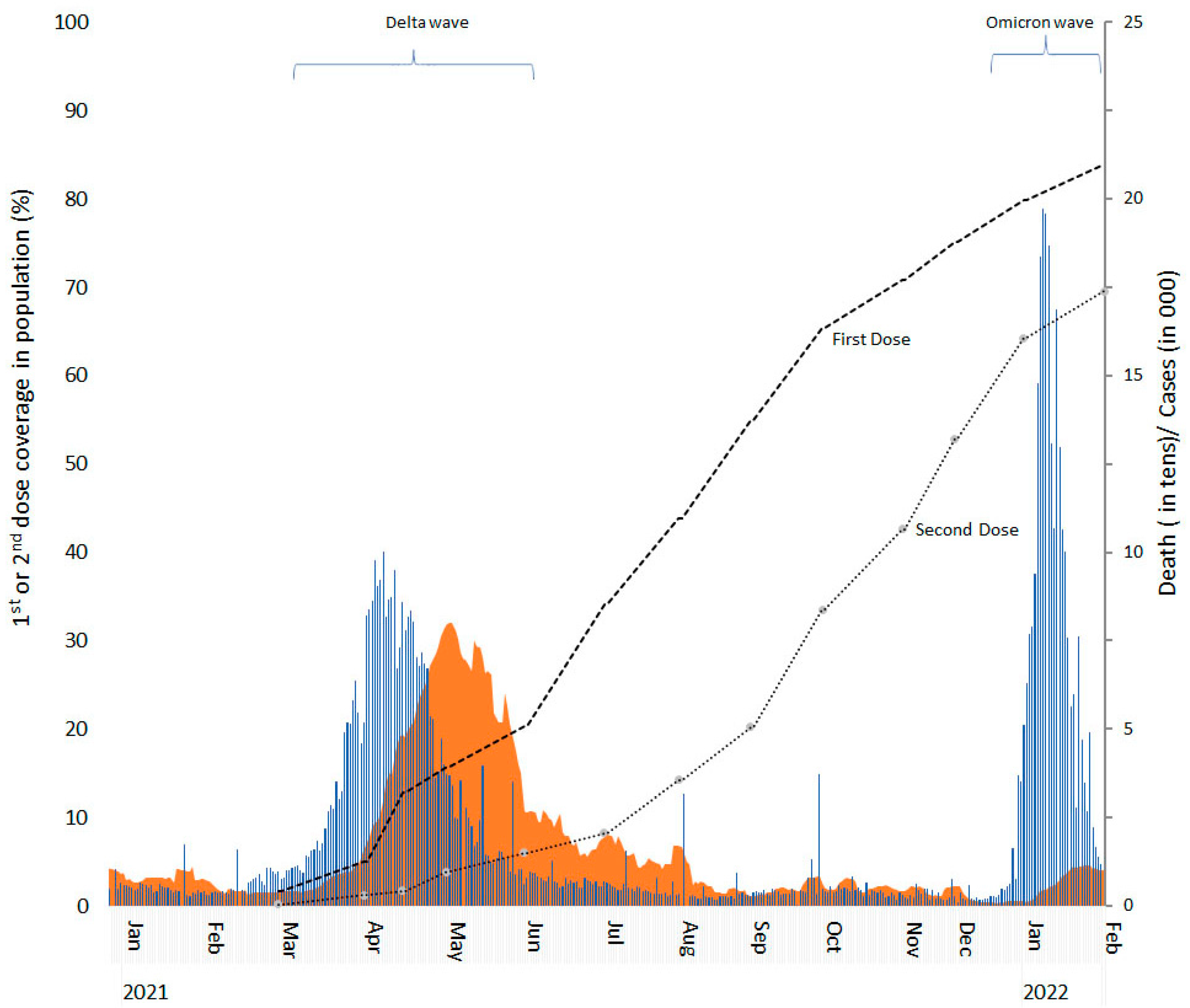
Women had higher PCR positivity during each of the waves, but the viral load difference was seen only during the Delta wave, and not the Omicron wave. This finding and the disappearance of differences by slum population density between the Delta and Omicron wave likely reflects widespread infection during Delta and the rapid uptake of SARS-CoV-2 vaccination in Mumbai (
Figure A3), which, like India’s overall vaccine roll out, aimed to reach slum populations quickly (Choudhary et al., 2021). If this is the explanation, it provides some reassurance against possible future waves. Some caution is needed however, as the highest viral load during the Omicron wave was seen in the oldest age groups (above 60 years) suggesting reduced hybrid immunity (from a combination of infection and vaccination) (Brown et al., 2022). Our finding lends further argument that followup vaccine doses for the elderly are needed in India as there are now reports of emergence of Omicron variant B 2.75, and given that the Delta wave occurred several months ago. Unfortunately, India has high coverage only of two doses (Foy et al., 2021; Ghosh, 2022; Masthi et al., 2022).
Our study adds to others suggesting that use of serial trends in Ct values, even in non-representative populations is robust to track viral load, particularly in low- and middle-income countries where PCR testing access is more limited (Research in Context Panel. Most Ct values studies are from high-income countries, which differ substantially from the intergenerational transmission commonly seen in low- and middle-income countries (LMIC). In our review of the literature, we identified 67 Ct studies of which only 6 were in LMICs including two from India. None explored determinants of viral load as we do. This holds true despite some obvious limitations of our study. First, we did not have data on why people got tested in these private laboratories. Subtle biases in who is tested are a limitation of the PCR positivity rates to map trajectories of the infection (Rehman et al., 2020), and we cannot exclude that such biases also affected the Ct values. However, changes in Ct values and its early signal were so dramatic, that we believe that the signal representing higher viral load at the community level was far stronger than the inherent noise in Ct values (Tom and Mina, 2020; Cava, 2023). Similarly, various PCR machines were used, and these might affect the trends in observed Ct values. However, the ICMR and others have established the high overall sensitivity and specificity of each machines independently. Finally, the study represents only one large urban setting in India, but Mumbai has been reflective of COVID-19 patterns for urban India from the origin of the pandemic (Velumani et al., 2021; Kumar, 2020).
Our study has several strengths also, notably a large sample size with testing procedures being mostly uniform over time. Moreover, the geographic and age distribution of the Thyrocare tested population resembled that of confirmed cases reported by the MCGM.
Future studies that apply Ct values should stratify populations by past infection or vaccination status, as the sequence of these might have quite an important bearing on the relationship between infection and viral load (Abu-Raddad et al., 2022). Routine access to Ct values collected by governments may also provide a more robust early warning system to track future pandemic waves of SARS-CoV-2.
Author Contributions
Conceived the idea and developed the study design: PJ, CN. Data analysis: WS, SHF, PB, NN Literature review: WS, HG. PJ and CN, WS wrote the initial draft, and all authors were involved in commenting on subsequent revisions. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
This study was funded by Canadian Institutes of Health Research.
Institutional Review Board Statement
No identifiable data on any patients were used in the study. Nonetheless, we obtained Research Ethics approval from Unity Health Toronto for analyses of these anonymized data.
Informed Consent Statement
Data available to this study are anonymous. Informed consent is not applicable.
Data Availability Statement
Data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank the extended help by Dr Murad Banaji for permitting access to his GitHub data archive on the MCGM Covid dashboard data collection (
https://github.com/muradbanaji/IndiaACMdata) and Dr Arokiaswamy Velumani and the staff at Thyrocare Laboratories, Mumbai for granting permission to use their Covid-19 laboratory testing data archives for this research. We also thanks Dr Raju Jotkar at Mother Child Health Nutrition Mission, India for assistance.
Conflicts of Interest
The authors have no competing interests to declare.
Appendix A
Table A1.
Mumbai ward wise slum and non-slum population.
Table A1.
Mumbai ward wise slum and non-slum population.
| |
Ward name |
Population 000 |
| Total |
Male |
Female |
Slums |
Non-slums |
% in slums |
| Low slum density wards |
| |
A |
185.0 |
101.2 |
83.8 |
22.3 |
162.7 |
12% |
| |
B |
127.3 |
70.4 |
56.8 |
12.7 |
114.6 |
10% |
| |
C |
166.2 |
98.0 |
68.1 |
16.6 |
149.6 |
10% |
| |
D |
346.9 |
183.0 |
163.9 |
34.7 |
312.2 |
10% |
| |
E |
393.3 |
216.1 |
177.2 |
124.2 |
269.1 |
32% |
| |
G South |
377.7 |
331.2 |
267.9 |
124.3 |
253.4 |
33% |
| |
H West |
307.6 |
305.9 |
251.4 |
82.6 |
225.0 |
27% |
| |
K West |
748.7 |
401.5 |
347.2 |
215.7 |
533.0 |
29% |
| |
R Central |
562.2 |
289.2 |
273.0 |
172.8 |
389.3 |
31% |
| |
T |
341.5 |
176.2 |
165.3 |
85.6 |
255.9 |
25% |
| Medium slum density wards |
| |
F North |
529.0 |
285.2 |
243.9 |
238.1 |
290.9 |
45% |
| |
F South |
361.0 |
190.7 |
170.2 |
180.1 |
180.8 |
50% |
| |
G North |
599.0 |
208.8 |
169.0 |
361.7 |
237.4 |
60% |
| |
M West |
411.9 |
217.6 |
194.3 |
165.0 |
246.9 |
40% |
| |
N |
622.9 |
332.6 |
290.2 |
249.2 |
373.6 |
40% |
| |
P South |
463.5 |
249.5 |
214.0 |
230.8 |
232.7 |
50% |
| |
R South |
691.2 |
379.3 |
311.9 |
414.4 |
276.8 |
60% |
| |
S |
743.8 |
398.9 |
344.9 |
408.4 |
335.3 |
55% |
| High slum density wards |
| |
H East |
557.2 |
161.7 |
145.9 |
388.9 |
168.3 |
70% |
| |
K East |
823.9 |
440.7 |
383.2 |
572.8 |
251.1 |
70% |
| |
L |
902.2 |
500.6 |
401.6 |
758.1 |
144.1 |
84% |
| |
M East |
807.7 |
436.6 |
371.2 |
686.0 |
121.7 |
85% |
| |
P North |
941.4 |
507.5 |
433.8 |
708.2 |
233.1 |
75% |
| |
R North |
431.4 |
233.7 |
197.7 |
281.2 |
150.2 |
65% |
| |
Total |
12,442.4 |
6,716.0 |
5,726.4 |
6,534.5 |
5,907.9 |
53% |
Table A2.
Mumbai postal pin codes mapped to municipal wards.
Table A2.
Mumbai postal pin codes mapped to municipal wards.
| Mumbai city district |
Mumbai Suburban district |
|
| Ward name |
Pin code |
Ward name |
Pin code |
|
| A |
400001 |
HE |
400029 |
|
| |
400005 |
|
400051 |
|
| |
400020 |
|
400055 |
|
| |
400021 |
|
400098 |
|
| |
400032 |
HW |
400050 |
|
| |
400039 |
|
400052 |
|
| B |
400003 |
|
400054 |
|
| |
400009 |
KE |
400057 |
|
| C |
400002 |
|
400059 |
|
| D |
400004 |
|
400060 |
|
| |
400006 |
|
400069 |
|
| |
400007 |
|
400093 |
|
| |
400026 |
|
400096 |
|
| |
400034 |
|
400099 |
|
| |
400035 |
KW |
400049 |
|
| E |
400008 |
|
400053 |
|
| |
400010 |
|
400056 |
|
| |
400011 |
|
400058 |
|
| |
400027 |
|
400102 |
|
| FN |
400014 |
L |
400024 |
|
| |
400019 |
|
400070 |
|
| |
400022 |
|
400072 |
|
| |
400031 |
|
400084 |
|
| |
400037 |
ME |
400043 |
|
| FS |
400012 |
|
400085 |
|
| |
400015 |
|
400088 |
|
| |
400033 |
|
400094 |
|
| GN |
400016 |
MW |
400071 |
|
| |
400017 |
|
400074 |
|
| |
400028 |
|
400089 |
|
| GS |
400013 |
N |
400075 |
|
| |
400018 |
|
400077 |
|
| |
400025 |
|
400079 |
|
| |
400030 |
|
400086 |
|
| |
|
PN |
400061 |
|
| |
|
|
400064 |
|
| |
|
|
400095 |
|
| |
|
|
400097 |
|
| |
|
PS |
400062 |
|
| |
|
|
400063 |
|
| |
|
|
400065 |
|
| |
|
|
400104 |
|
| |
|
RC |
400091 |
|
| |
|
|
400092 |
|
| |
|
RN |
400068 |
|
| |
|
|
400103 |
|
| |
|
RS |
400067 |
|
| |
|
|
400101 |
|
| |
|
S |
400042 |
|
| |
|
|
400076 |
|
| |
|
|
400078 |
|
| |
|
|
400083 |
|
| |
|
|
400087 |
|
| |
|
T |
400066 |
|
| |
|
|
400080 |
|
| |
|
|
400081 |
|
| |
|
|
400082 |
|
Table A3.
ICMR approved testing kits used at Thyrocare central laboratory for PCR diagnosis of SARS-CoV-2 infection.
Table A3.
ICMR approved testing kits used at Thyrocare central laboratory for PCR diagnosis of SARS-CoV-2 infection.
| No. |
Test Kit Name |
Targets (Genes)* |
LOD (Limit of Detection) |
| 1 |
RealStar®SARS-CoV-2PCRKit |
S, E |
0.014,0.025 PFU/ml |
| 2 |
Lab gun Siemens |
RdRp, E |
20 genomic RNA copies/μL |
| 3 |
TaqPath™COVID-19 Combo Kit |
S, ORF1ab, N |
10 GCE/reaction |
| 4 |
Detection expert1SSARS CoV-2 Gene store |
N1, N2 |
100 GCE/Reaction |
| 5 |
MerilCOVID-19One-stepPCRKit |
N, ORF1ab |
<500 RNA copies/mL |
| 6 |
COVIPATH |
N, ORF1ab |
10 GCE/reaction |
Table A4.
PCR confirmed Covid cases and deaths of Mumbai Covid dashboard at different viral outbreak periods from April 2020 - January 2022.
Table A4.
PCR confirmed Covid cases and deaths of Mumbai Covid dashboard at different viral outbreak periods from April 2020 - January 2022.
| |
|
Cases |
|
Deaths |
|
| |
|
Total since Apr 2020 to Jan 2022 |
Periods no major outbreaks |
Outbreak periods |
Total since Apr 2020 to Jan 2022 |
No major outbreaks |
Outbreak periods |
|
| |
Characteristics |
Aleph Wave: Jun-Nov 2020 (6 mo.) |
Delta wave: Mar-Jun 2021 (4 mo.) |
Omicron: Jan 2022 (till Jan17) (1 mo.) |
Aleph wave: May-Oct 2020 (6 mo.) |
Delta wave: Mar-Jun 2021 (4 mo.) |
Omicron wave: Jan 2022 (till Jan17) (1 mo.) |
| |
No. of months |
22 |
11 |
6 |
4 |
1 |
22 |
11 |
6 |
4 |
1 |
| PCR confirmed cases |
|
|
|
|
|
|
|
|
|
| Total |
1,022,979 |
160,288 |
232,484 |
376,528 |
253,679 |
16,668 |
2,850 |
9,627 |
3,980 |
211 |
| Annualized rate per 1000 population** |
|
|
|
| |
All ages |
192 |
13 |
34 |
82 |
222 |
1.5 |
0.2 |
1.4 |
0.9 |
0.2 |
| |
0-9 |
29 |
2 |
4 |
11 |
36 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
| |
10-19 |
66 |
4 |
8 |
26 |
83 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
| |
20-29 |
163 |
9 |
21 |
66 |
201 |
0.1 |
0.0 |
0.1 |
0.0 |
0.0 |
| |
30-39 |
237 |
14 |
36 |
102 |
284 |
0.3 |
0.1 |
0.2 |
0.2 |
0.0 |
| |
40-49 |
248 |
17 |
47 |
115 |
276 |
1.0 |
0.2 |
0.9 |
0.7 |
0.1 |
| |
50-59 |
332 |
25 |
77 |
149 |
357 |
3.3 |
0.6 |
3.4 |
2.0 |
0.1 |
| |
60-69 |
414 |
33 |
95 |
179 |
452 |
7.8 |
1.2 |
7.9 |
4.3 |
0.8 |
| |
70-79 |
559 |
41 |
115 |
229 |
638 |
15.9 |
2.1 |
15.1 |
9.2 |
2.6 |
| |
80+ |
588 |
39 |
104 |
247 |
688 |
23.3 |
3.2 |
19.5 |
14.0 |
6.1 |
| Sex |
|
|
|
|
|
|
|
|
|
| |
Female |
n.a. |
n.a. |
29 |
76 |
192 |
n.a. |
n.a. |
n.a. |
n.a. |
n.a. |
| |
Male |
n.a. |
n.a. |
38 |
88 |
248 |
n.a. |
n.a. |
n.a. |
n.a. |
n.a. |
| Municipal ward, Slum density |
|
|
|
|
|
|
|
|
|
| Low slum areas |
261.2 |
16.4 |
45.1 |
123.5 |
262.5 |
|
|
|
|
|
| |
A |
379 |
23 |
55 |
132 |
484 |
|
|
|
|
|
| |
B |
79 |
9 |
23 |
34 |
79 |
Deaths by wards not available |
|
| |
C |
101 |
8 |
37 |
46 |
93 |
|
|
|
|
|
| |
D |
316 |
22 |
61 |
148 |
349 |
|
|
|
|
|
| |
E |
155 |
15 |
33 |
73 |
162 |
|
|
|
|
|
| |
G South |
193 |
16 |
38 |
81 |
219 |
|
|
|
|
|
| |
H West |
470 |
25 |
53 |
159 |
625 |
|
|
|
|
|
| |
K West |
324 |
17 |
38 |
116 |
422 |
|
|
|
|
|
| |
R Central |
257 |
16 |
61 |
131 |
264 |
|
|
|
|
|
| |
T |
266 |
22 |
66 |
138 |
261 |
|
|
|
|
|
| Medium slum areas |
173.8 |
13.1 |
32.8 |
77.4 |
195.7 |
|
|
|
|
|
| |
F North |
179 |
15 |
27 |
80 |
205 |
|
|
|
|
|
| |
F South |
169 |
14 |
43 |
65 |
186 |
|
|
|
|
|
| |
G North |
137 |
12 |
32 |
60 |
148 |
|
|
|
|
|
| |
M West |
216 |
14 |
30 |
85 |
267 |
|
|
|
|
|
| |
N |
149 |
12 |
34 |
74 |
152 |
|
|
|
|
|
| |
P South |
270 |
14 |
39 |
123 |
319 |
|
|
|
|
|
| |
R South |
209 |
12 |
41 |
100 |
231 |
|
|
|
|
|
| |
S |
150 |
10 |
29 |
62 |
174 |
|
|
|
|
|
| High slum areas |
151.5 |
8.2 |
25.9 |
68.8 |
164.3 |
|
|
|
|
|
| |
H East # |
166 |
12 |
22 |
68 |
203 |
|
|
|
|
|
| |
K East |
206 |
12 |
31 |
88 |
247 |
|
|
|
|
|
| |
L |
99 |
8 |
16 |
40 |
119 |
|
|
|
|
|
| |
M East # |
91 |
7 |
15 |
38 |
108 |
|
|
|
|
|
| |
P North |
144 |
8 |
30 |
70 |
157 |
|
|
|
|
|
| |
R North |
159 |
8 |
34 |
77 |
172 |
|
|
|
|
|
Table A5.
Descriptive PCR positivity rates (%) of the Thyrocare tested population at different viral outbreak periods from April 2020 to January 2022.
Table A5.
Descriptive PCR positivity rates (%) of the Thyrocare tested population at different viral outbreak periods from April 2020 to January 2022.
| |
|
Total period |
Aleph wave |
Delta wave |
Omicron wave |
Periods no major outbreaks Apr 2020 - Jan 2022 |
| |
|
Jun-Nov 2020 (6 months) |
Mar-Jun 2021 (4 months) |
Jan 2022 (1 months) |
Characteristics
|
No. tested (000) |
No. tested (000) |
PCR Positivity % * |
No. tested (000) |
PCR Positivity % * |
No. tested (000) |
PCR Positivity % * |
No. tested (000) |
PCR Positivity % * |
| Total no. tested |
2,717.3 |
64.2 |
23.2 |
445.1 |
9.9 |
26.2 |
42.8 |
2,181.7 |
3.4 |
| (No. positive) |
(155.0) |
(17.9) |
|
(46.6) |
|
(11.7) |
|
(78.8) |
|
| Age in 10 years |
|
|
|
|
|
|
|
|
| |
0-9 |
73.7 |
0.9 |
28.9 |
14.1 |
9.8 |
0.7 |
38.5 |
58.0 |
5.3 |
| |
10-19 |
269.5 |
2.3 |
25.0 |
39.6 |
9.3 |
1.5 |
40.5 |
226.1 |
4.1 |
| |
20-29 |
641.5 |
13.4 |
15.6 |
103.2 |
8.7 |
5.9 |
40.2 |
518.9 |
2.7 |
| |
30-39 |
580.5 |
15.7 |
20.1 |
99.2 |
10.5 |
7.0 |
42.8 |
458.6 |
3.6 |
| |
40-49 |
457.7 |
11.1 |
28.4 |
75.6 |
10.6 |
4.0 |
45.5 |
367.0 |
3.6 |
| |
50-59 |
329.2 |
9.2 |
39.5 |
53.7 |
11.3 |
3.1 |
48.7 |
263.2 |
3.7 |
| |
60-69 |
233.0 |
6.5 |
42.9 |
37.1 |
12.2 |
2.2 |
51.7 |
187.2 |
4.2 |
| |
70-79 |
106.7 |
3.7 |
43.5 |
17.9 |
14.0 |
1.2 |
55.7 |
84.0 |
4.4 |
| |
80+ |
25.3 |
1.4 |
41.2 |
4.7 |
20.5 |
0.5 |
55.9 |
18.7 |
6.1 |
| Sex |
|
|
|
|
|
|
|
|
|
|
| |
Female |
1,105.3 |
22.5 |
25.9 |
166.4 |
11.5 |
12.1 |
44.1 |
904.2 |
3.8 |
| |
Male |
1,612.0 |
41.7 |
21.9 |
278.7 |
9.0 |
14.1 |
41.8 |
1,277.5 |
3.2 |
| District, Municipal wards and slum density |
| |
Mumbai |
2,567.0 |
33.7 |
22.0 |
386.7 |
7.8 |
12.6 |
41.3 |
2,134.0 |
3.4 |
| |
Mumbai Suburban |
150.3 |
30.5 |
24.7 |
58.5 |
23.5 |
13.6 |
44.2 |
47.8 |
6.5 |
| Low slum areas |
2,519.1 |
35.8 |
20.4 |
366.2 |
7.2 |
4.9 |
44.3 |
2,112.1 |
3.3 |
| |
A |
2,386.8 |
6.1 |
7.8 |
321.9 |
5.6 |
0.3 |
35.2 |
2,058.5 |
3.3 |
| |
B |
12.6 |
4.1 |
46.6 |
5.5 |
19.7 |
0.0 |
43.5 |
2.9 |
5.2 |
| |
C |
2.7 |
0.6 |
11.4 |
0.8 |
15.5 |
0.2 |
35.0 |
1.0 |
4.9 |
| |
D |
48.2 |
6.0 |
16.0 |
14.7 |
12.8 |
0.8 |
42.1 |
27.5 |
4.2 |
| |
E |
11.8 |
0.9 |
9.4 |
5.8 |
17.3 |
- |
- |
4.3 |
3.3 |
| |
GS |
9.1 |
3.1 |
15.0 |
2.3 |
18.9 |
0.4 |
45.1 |
3.3 |
7.1 |
| |
H West |
6.1 |
1.2 |
18.6 |
2.5 |
20.6 |
0.3 |
47.5 |
2.1 |
6.8 |
| |
K West |
24.8 |
8.6 |
23.1 |
6.9 |
23.7 |
1.5 |
42.7 |
7.8 |
8.8 |
| |
R Central |
9.3 |
3.1 |
33.6 |
3.0 |
24.5 |
0.3 |
50.9 |
2.9 |
11.6 |
| |
T |
7.8 |
2.0 |
15.9 |
2.9 |
35.2 |
1.2 |
48.8 |
1.7 |
8.9 |
| Medium slum areas |
79.1 |
11.8 |
28.8 |
30.9 |
25.3 |
9.2 |
42.2 |
27.3 |
8.3 |
| |
F North |
11.8 |
3.2 |
38.4 |
4.4 |
24.6 |
0.9 |
47.0 |
3.3 |
21.7 |
| |
F South |
6.0 |
0.5 |
25.9 |
2.4 |
16.2 |
0.3 |
32.6 |
2.8 |
2.2 |
| |
G North |
21.2 |
3.7 |
26.3 |
7.0 |
20.5 |
2.7 |
37.0 |
7.9 |
7.3 |
| |
M West |
5.8 |
0.8 |
24.8 |
2.5 |
24.2 |
0.5 |
45.9 |
1.8 |
4.4 |
| |
N |
10.5 |
0.6 |
38.2 |
4.2 |
23.5 |
1.8 |
43.8 |
4.0 |
7.4 |
| |
P South |
10.0 |
1.6 |
15.1 |
4.4 |
30.5 |
1.3 |
38.6 |
2.7 |
8.0 |
| |
R South |
10.3 |
1.1 |
32.4 |
5.0 |
35.9 |
1.3 |
55.0 |
2.9 |
8.6 |
| |
S |
3.6 |
0.3 |
29.5 |
1.0 |
21.2 |
0.5 |
32.6 |
1.7 |
3.9 |
| High slum areas |
119.0 |
16.6 |
25.8 |
48.0 |
19.9 |
12.1 |
42.8 |
42.3 |
5.2 |
| |
H East |
36.0 |
5.9 |
21.6 |
16.2 |
16.4 |
2.4 |
36.2 |
11.5 |
3.7 |
| |
K East |
26.1 |
2.8 |
12.4 |
10.0 |
20.9 |
2.9 |
43.3 |
10.4 |
4.7 |
| |
L |
24.0 |
1.5 |
20.4 |
9.1 |
15.7 |
2.7 |
41.0 |
10.7 |
5.2 |
| |
M East |
8.2 |
1.7 |
23.8 |
2.8 |
19.4 |
0.9 |
43.9 |
2.8 |
8.1 |
| |
P North |
17.9 |
3.3 |
50.8 |
7.2 |
29.3 |
2.3 |
47.0 |
5.1 |
8.3 |
| |
R North |
6.8 |
1.4 |
34.9 |
2.7 |
29.2 |
0.8 |
56.0 |
1.9 |
6.5 |
Table A6.
Descriptive Ct values of the Thyrocare tested population during different viral waves from April 2020 to January 2022.
Table A6.
Descriptive Ct values of the Thyrocare tested population during different viral waves from April 2020 to January 2022.
| |
|
Total period |
Aleph wave
Jun-Nov 2020 (6 mo.) |
Delta wave
Mar-Jun 2021 (4 mo.) |
Omicron wave
Jan 2022 (1 mo.) |
Periods no major outbreaks
Apr 2020 - Jan 2022 |
| |
Characteristics |
No. tested (000) |
No. tested (000) |
Median Ct value |
No. tested (000) |
Median Ct value |
No. tested (000) |
Median Ct value |
No. tested (000) |
Median Ct value |
| |
Total |
2,717.3 |
64.2 |
26.0 |
445.1 |
23.0 |
23.2 |
23.6 |
2,181.7 |
25.0 |
| Age in 10 years |
|
|
|
|
|
|
|
|
|
| |
0-9 |
73.7 |
0.9 |
24.0 |
14.1 |
24.0 |
0.7 |
22.9 |
58.0 |
25.0 |
| |
10-19 |
269.5 |
2.3 |
25.0 |
39.6 |
23.0 |
1.5 |
23.1 |
226.1 |
25.0 |
| |
20-29 |
641.5 |
13.4 |
25.0 |
103.2 |
23.0 |
5.9 |
23.7 |
518.9 |
25.0 |
| |
30-39 |
580.5 |
15.7 |
26.0 |
99.2 |
23.0 |
7.0 |
23.2 |
458.6 |
24.0 |
| |
40-49 |
457.7 |
11.1 |
26.0 |
75.6 |
23.0 |
4.0 |
23.0 |
367.0 |
25.0 |
| |
50-59 |
329.2 |
9.2 |
26.0 |
53.7 |
22.0 |
3.1 |
22.8 |
263.2 |
25.0 |
| |
60-69 |
233.0 |
6.5 |
26.0 |
37.1 |
22.0 |
2.2 |
21.9 |
187.2 |
24.0 |
| |
70-79 |
106.7 |
3.7 |
26.0 |
17.9 |
22.0 |
1.2 |
21.8 |
84.0 |
24.0 |
| |
80+ |
25.3 |
1.4 |
26.0 |
4.7 |
22.0 |
0.5 |
21.4 |
18.7 |
24.0 |
| Sex |
|
|
|
|
|
|
|
|
|
- |
| |
Female |
1,105.3 |
22.5 |
25.0 |
166.4 |
23.0 |
12.1 |
23.1 |
904.2 |
25.0 |
| |
Male |
1,612.0 |
41.7 |
26.0 |
278.7 |
23.0 |
14.1 |
23.2 |
1,277.5 |
24.0 |
District, municipal wards and slum density
|
|
|
|
|
|
|
|
| |
Mumbai |
2,567.0 |
33.7 |
26.0 |
386.7 |
23.0 |
12.6 |
23.2 |
2,134.0 |
25.0 |
| |
Mumbai Suburban |
150.3 |
30.5 |
25.0 |
58.5 |
22.0 |
13.6 |
23.2 |
47.8 |
23.5 |
Low slum areas
|
2,519.1 |
35.8 |
26.0 |
366.2 |
24.0 |
4.9 |
22.9 |
2,112.1 |
25.0 |
| |
A |
2,386.8 |
6.1 |
29.0 |
321.9 |
24.0 |
0.3 |
23.6 |
2,058.5 |
25.0 |
| |
B |
12.6 |
4.1 |
26.0 |
5.5 |
22.0 |
0.0 |
20.8 |
2.9 |
26.0 |
| |
C |
2.7 |
0.6 |
26.0 |
0.8 |
23.0 |
0.2 |
25.5 |
1.0 |
22.1 |
| |
D |
48.2 |
6.0 |
28.0 |
14.7 |
24.0 |
- |
- |
27.5 |
26.0 |
| |
E |
11.8 |
0.9 |
27.0 |
5.8 |
23.0 |
0.8 |
23.3 |
4.3 |
22.8 |
| |
G South |
9.1 |
3.1 |
27.0 |
2.3 |
22.0 |
0.4 |
22.6 |
3.3 |
22.2 |
| |
H West |
6.1 |
1.2 |
25.0 |
2.5 |
22.0 |
0.3 |
23.5 |
2.1 |
22.0 |
| |
K West |
24.8 |
8.6 |
25.0 |
6.9 |
22.0 |
1.5 |
22.9 |
7.8 |
23.0 |
| |
R Central |
9.3 |
3.1 |
24.0 |
3.0 |
22.0 |
0.3 |
22.1 |
2.9 |
22.0 |
| |
T |
7.8 |
2.0 |
26.0 |
2.9 |
21.0 |
1.2 |
22.7 |
1.7 |
22.0 |
| Medium slum areas |
79.1 |
11.8 |
25.0 |
30.9 |
21.0 |
9.2 |
23.0 |
27.3 |
23.0 |
| |
F North |
11.8 |
3.2 |
26.0 |
4.4 |
21.0 |
0.9 |
23.1 |
3.3 |
22.0 |
| |
F South |
6.0 |
0.5 |
27.0 |
2.4 |
22.0 |
0.3 |
24.4 |
2.8 |
23.0 |
| |
G North |
21.2 |
3.7 |
25.0 |
7.0 |
21.0 |
2.7 |
23.3 |
7.9 |
23.0 |
| |
M West |
5.8 |
0.8 |
28.0 |
2.5 |
24.0 |
0.5 |
23.0 |
1.8 |
25.0 |
| |
N |
10.5 |
0.6 |
23.0 |
4.2 |
21.0 |
1.8 |
22.8 |
4.0 |
22.0 |
| |
P South |
10.0 |
1.6 |
25.0 |
4.4 |
21.0 |
1.3 |
22.7 |
2.7 |
22.0 |
| |
R South |
10.3 |
1.1 |
25.0 |
5.0 |
20.0 |
1.3 |
22.6 |
2.9 |
23.0 |
| |
S |
3.6 |
0.3 |
26.0 |
1.0 |
22.0 |
0.5 |
23.4 |
1.7 |
22.3 |
| High slum areas |
119.0 |
16.6 |
25.5 |
26.0 |
22.5 |
22.0 |
23.7 |
23.4 |
|
| |
H East |
36.0 |
5.9 |
26.0 |
16.2 |
23.0 |
2.4 |
25.0 |
11.5 |
24.0 |
| |
K East |
26.1 |
2.8 |
25.0 |
10.0 |
22.0 |
2.9 |
23.1 |
10.4 |
22.0 |
| |
L |
24.0 |
1.5 |
26.0 |
9.1 |
22.0 |
2.7 |
23.2 |
10.7 |
23.0 |
| |
M East |
8.2 |
1.7 |
26.0 |
2.8 |
22.0 |
0.9 |
23.3 |
2.8 |
21.0 |
| |
P North |
17.9 |
3.3 |
25.0 |
7.2 |
22.0 |
2.3 |
22.8 |
5.1 |
24.0 |
| |
R North |
6.8 |
1.4 |
26.0 |
2.7 |
21.0 |
0.8 |
22.9 |
1.9 |
25.0 |
Table A7.
The begin, peak and end of viral waves observed in Ct values, PCR positivity, confirmed Covid case and deaths at Delta and Omicron outbreaks.
Table A7.
The begin, peak and end of viral waves observed in Ct values, PCR positivity, confirmed Covid case and deaths at Delta and Omicron outbreaks.
Pandemic period/
Time series |
The earliest date of change observed at |
No. of days from the earliest observed date ¥ |
Number of days beginning to peak and peak to end |
| Beginning |
Peak |
End |
Beginning |
Peak |
End |
Beginning to peak |
Peak to end |
Overall |
| Delta wave (Mar-Jun 2021) |
|
|
|
|
|
|
|
|
|
| |
Thyrocare study data |
|
|
|
|
|
|
|
|
|
| |
Ct value |
1-Feb-2021 |
31-Mar-2021 |
19-May-2021 |
0 |
0 |
0 |
58 |
49 |
107 |
| PCR Positivity |
18-Feb-2021 |
5-Apr-2021 |
16-Jun-2021 |
17 |
5 |
28 |
46 |
72 |
118 |
| MCGM official PCR confirmed |
|
|
|
|
|
|
|
|
| Cases |
9-Feb-2021 |
5-Apr-2021 |
4-Jul-2021 |
8 |
5 |
46 |
55 |
90 |
145 |
| Deaths |
13-Mar-2021 |
1-May-2021 |
8-Aug-2021 |
40 |
31 |
81 |
49 |
99 |
148 |
| Omicron wave (Jan 2022) |
|
|
|
|
|
|
|
|
|
| |
Thyrocare study data |
|
|
|
|
|
|
|
|
|
| |
Ct value |
11-Dec-2021 |
2-Jan-2022 |
30-Jan-2022* |
0 |
0 |
* |
22 |
28* |
50* |
| PCR Positivity |
22-Dec-2021 |
11-Jan-2022 |
30-Jan-2022* |
11 |
9 |
* |
20 |
19* |
39* |
| MCGM official PCR confirmed |
|
|
|
|
|
|
|
|
| Cases |
18-Dec-2021 |
10-Jan-2022 |
29-Jan-2022* |
7 |
8 |
* |
23 |
19* |
42* |
| Deaths |
4-Jan-2022 |
24-Jan-2022 |
30-Jan-2022* |
24 |
22 |
* |
20 |
6* |
26* |
Figure A1.
Age trend of PCR positivity during Aleph, Delta, and Omicron viral waves. The dotted scatter represents the gender and slum status adjusted odds ratios of PCR positivity for 10 yearly age groups. Odds ratios were measured relative to the age 20-29 year group whom always had the lowest positivity rate. The dotted curves are the polynomial trends for each viral wave. R-squared for each viral wave: Aleph 0.73, Delta 0.96 and Omicron 0.97. The original odds ratios used in this figure were extracted from
Figure 3, forest plot. We tested for trend of age using Cochran-Armitage Trend Test: Aleph (p<0.0001), Delta (p<0.0001) and Omicron (p<0.0001).
Figure A1.
Age trend of PCR positivity during Aleph, Delta, and Omicron viral waves. The dotted scatter represents the gender and slum status adjusted odds ratios of PCR positivity for 10 yearly age groups. Odds ratios were measured relative to the age 20-29 year group whom always had the lowest positivity rate. The dotted curves are the polynomial trends for each viral wave. R-squared for each viral wave: Aleph 0.73, Delta 0.96 and Omicron 0.97. The original odds ratios used in this figure were extracted from
Figure 3, forest plot. We tested for trend of age using Cochran-Armitage Trend Test: Aleph (p<0.0001), Delta (p<0.0001) and Omicron (p<0.0001).
Figure A2.
Overview of Mumbai SARS-CoV-2 viral outbreaks - daily time series of MCGM Covid-19 dashboard and Thyrocare study data. First pandemic outbreak was from Jun-Nov 2020 (Aleph wave), second from Mar-Jun 2021 (Delta wave), and third in January 2022 (Omicron wave). Daily PCR confirmed case counts in 000 (blue bar) are as reported in Mumbai Covid dashboard. 7-day average PCR positivity (gray area) and daily median Ct values (red curve) are from Thyrocare data. The red curve represents the median Ct values refers to Y-axis on the left and all other time series refer to Y-axis on the right. Left Y-axis is shown in reverse order so a lower Ct value implies a higher viral load.
Figure A2.
Overview of Mumbai SARS-CoV-2 viral outbreaks - daily time series of MCGM Covid-19 dashboard and Thyrocare study data. First pandemic outbreak was from Jun-Nov 2020 (Aleph wave), second from Mar-Jun 2021 (Delta wave), and third in January 2022 (Omicron wave). Daily PCR confirmed case counts in 000 (blue bar) are as reported in Mumbai Covid dashboard. 7-day average PCR positivity (gray area) and daily median Ct values (red curve) are from Thyrocare data. The red curve represents the median Ct values refers to Y-axis on the left and all other time series refer to Y-axis on the right. Left Y-axis is shown in reverse order so a lower Ct value implies a higher viral load.
Figure A3.
Vaccine coverage, daily time series of PCR confirmed cases and deaths from COVID-19 from January 2021 - January 2022 in Mumbai. The first pandemic outbreak wave was from Jun-Nov 2020 (Aleph wave), second from Mar-Jun 2021 (Delta wave), and third in January 2022 (Omicron wave). First pandemic wave is not shown here because vaccine coverage was not substantial at the period. Daily PCR confirmed case counts in 000 (blue bar), deaths in tens (orange area), percentage of vaccine coverage (thick dotted line - 1st dose, thin dotted line - 2nd dose) are as reported in Mumbai Covid dashboard. The vaccine coverage refers to Y-axis in left and all other time series refer to Y-axis in right.
Figure A3.
Vaccine coverage, daily time series of PCR confirmed cases and deaths from COVID-19 from January 2021 - January 2022 in Mumbai. The first pandemic outbreak wave was from Jun-Nov 2020 (Aleph wave), second from Mar-Jun 2021 (Delta wave), and third in January 2022 (Omicron wave). First pandemic wave is not shown here because vaccine coverage was not substantial at the period. Daily PCR confirmed case counts in 000 (blue bar), deaths in tens (orange area), percentage of vaccine coverage (thick dotted line - 1st dose, thin dotted line - 2nd dose) are as reported in Mumbai Covid dashboard. The vaccine coverage refers to Y-axis in left and all other time series refer to Y-axis in right.
References
- Abu-Raddad LJ, Chemaitelly H, Ayoub HH, et al. Relative infectiousness of SARS-CoV-2 vaccine breakthrough infections, reinfections, and primary infections. Nature communications 2022, 13, 532. [Google Scholar] [CrossRef] [PubMed]
- Andriamandimby SF, Brook CE, Razanajatovo N, et al. Cross-sectional cycle threshold values reflect epidemic dynamics of COVID-19 in Madagascar. Epidemics 2022, 38, 100533. [Google Scholar] [CrossRef] [PubMed]
- Banaji M. India ACM data depository in GitHub - Data on Mumbai’s COVID-19 epidemic. 2022. https://github.com/muradbanaji/IndiaACMdata (accessed 11 February 2022).
- Bayat Al S, Mundodan J, Hasnain S, et al. Can the cycle threshold (Ct) value of RT-PCR test for SARS CoV2 predict infectivity among close contacts? Journal of Infection and Public Health 2021, 14, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Brown PE, Fu SH, Bansal A, et al. Omicron BA.1/1.1 SARS-CoV-2 Infection among Vaccinated Canadian Adults. New England Journal of Medicine 2022, 386, 2337–2339.
- Cava, F. , San Román J., Barreiro P., et al. Temporal Series Analysis of Population Cycle Threshold Counts as a Predictor of Surge in Cases and Hospitalizations during the SARS-CoV-2 Pandemic. Viruses 2023, 15, 421. [Google Scholar] [CrossRef] [PubMed]
- Cherian S, Potdar V, Jadhav S, et al. Convergent evolution of SARS-CoV-2 spike mutations. L452R, E484Q and P681R, in the second wave of COVID-19 in Maharashtra, India. Microorganisms 2021, 9, 1542. [Google Scholar] [CrossRef] [PubMed]
- Choudhary OP, Choudhary P, Singh I. India’s COVID-19 vaccination drive: key challenges and resolutions. Lancet Infectious Diseases 2021, 21, 1483–1484. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus.app. The Coronavirus App [Internet]. Taipei, Taiwan: Coronavirus.app; 2022. https://coronavirus.app/map (accessed 24 August 2022).
- Das P, Mondal S, Pal S, et al. COVID diagnostics by molecular methods: A systematic review of nucleic acid based testing systems. Indian Journal of Medical Microbiology 2021, 39, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Foy BH, Wahl B, Mehta K, et al. Comparing COVID-19 vaccine allocation strategies in India: A mathematical modelling study. International Journal of Infectious Diseases 2021, 103, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Ghosh A. 11% of 69 crore eligible people have taken Covid precaution dose, says govt, blames waning fear. The Print 2022. https://theprint.in/health/11-of-69-crore-eligible-people-have-taken-covid-precaution-dose-says-govt-blames-waning-fear/1055999/ (accessed 24 August 2022).
- Ghosh S, Seth P, Tiwary H. How does Covid-19 aggravate the multidimensional vulnerability of slums in India? A Commentary. Social Sciences & Humanities Open 2020, 2, 100068. [Google Scholar]
- Government of Maharashtra (Gov-MH). COVID-19 Dashboard by Government of Maharashtra. 2022. https://www.covid19maharashtragov.in/mh-covid/dashboard (accessed 31 January 2022).
- Hay JA, Kennedy-Shaffer L, Kanjilal S, Lennon NJ, Gabriel SB, Lipsitch M, Mina MJ. Estimating epidemiologic dynamics from cross-sectional viral load distributions. Science. 2021, 373, eabh0635. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nature medicine 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed]
- IDFC Institute. Data from BMC’s COVID-19 Response War Room – GitHub data depository. 2022. https://github.com/IDFC-Institute/mumbai-covid-data (accessed 30 June 2022).
- Indian Council of Medical Research (ICMR). List of Government (Green) and Private (Blue) Laboratories that can test COVID-19. 2020. https://covid-19-info.hbcse.tifr.res.in/wp-content/uploads/2020/03/ICMR-approved-Labs-Govt-Private-25march2020.pdf (accessed 3 March 2021).
- Jha P, Deshmukh Y, Tumbe C, et al. COVID mortality in India: National survey data and health facility deaths. Science 2022, 375, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Kumar A. Modeling geographical spread of COVID-19 in India using network-based approach. medRxiv 2020, published online April 27. https://www.medrxiv.org/content/10.1101/2020.04.23.20076489v1 (preprint).
- Masthi NR R, Brahmajosyula A, Khamar A, et al. Coverage of Coronavirus Disease-2019 (COVID-19) Booster Dose (Precautionary) in the Adult Population: An Online Survey. Cureus 2022, 14, e26912. [Google Scholar]
- Mlcochova P, Kemp SA, Dhar MS, et al. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature 2021, 599, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Municipal Corporation of Greater Mumbai (MCGM). MCGM COVID 19 dashboard. 2022a. https://stopcoronavirus.mcgm.gov.in/key-updates-trends (accessed 31 January 2022).
- Municipal Corporation of Greater Mumbai (MCGM). Demographics and Vital Statistics Report. 2022b. https://www.mcgm.gov.in/irj/portal/anonymous/qlvitalstatsreport?guest_user=english (accessed 3 March 2021).
- NITI-Aayog, Municipal Corporation Greater Mumbai (MCGM), Tata Institute of Fundamental Research (TIFR), et al. SARS-CoV2 Serological Survey in Mumbai - Preliminary Report of Round 2. 2020. https://www.tifr.res.in/TSN/article/Mumbai-Serosurvey%20Technical%20report-NITI_BMC-Round-2%20for%20TIFR%20website.pdf (accessed 3 March 2021).
- Office of the Registrar General & Census Commissioner (ORGCC), India. Population Census 2011 - Table C-14: Population in five year age group by residence and sex, India - 2011. 2021. https://censusindia.gov.in/nada/index.php/catalog/1541 (accessed 21 January 2022).
- Public Health England (PHE). Understanding cycle threshold (Ct) in SARS-CoV-2 RT-PCR. A guide for health protection teams. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/926410/Understanding_Cycle_Threshold__Ct__in_SARS-CoV-2_RT-PCR_.pdf (accessed 11 February 2022).
- R Core Team. R: A language and environment for statistical computing. 2017. https://www.R-project.org/ (accessed 30 June 2022).
- Rehman T, Keepanasseril A, Maurya DK, et al. Factors Associated with Maternal Referral System in South India: A Hospital Based Cross sectional Analytical Study. Journal of Natural Science, Biology and Medicine 2020, 11, 158–163. [Google Scholar]
- SAS Institute Inc. SAS/STAT® 14.1 User’s Guide. Cary, NC: SAS Institute Inc.; 2015. https://support.sas.com/documentation/onlinedoc/stat/141/qreg.pdf (accessed 24 August 2022).
- Service RF. One number could help reveal how infectious a COVID-19 patient is. Should test results include it? Science Insider Health 2022. https://www.science.org/content/article/one-number-could-help-reveal-how-infectious-covid-19-patient-should-test-results (accessed 11 February 2022).
- Tom MR, Mina MJ. To interpret the SARS-CoV-2 test, consider the cycle threshold value. Clinical Infectious Diseases 2020, 71, 2252–2254. [Google Scholar] [CrossRef]
- Velumani A, Nikam C, Suraweera W, et al. SARS-CoV-2 seroprevalence in 12 cities of India from July-December 2020. medRxiv 2021, published online March 24. https://www.medrxiv.org/content/10.1101/2021.03.19.21253429v1 (preprint).
- Walker AS, Pritchard E, House T, et al. Ct threshold values, a proxy for viral load in community SARS-CoV-2 cases, demonstrate wide variation across populations and over time. eLife 2021, 10, e64683. [Google Scholar] [CrossRef] [PubMed]
- Wood SN. Generalized additive models: an introduction with R. New York: Chapman and Hall/CRC; 2017.
Figure 1.
Age distribution of PCR confirmed cases between MCGM Covid dashboard and Thyrocare study data during the three viral waves. Aleph wave (Jun 2020-Nov 2020), (B) Delta wave (Mar 2021-Jun 2021), (C) Omicron wave (Jan 2022). This figure compares the similarity of age-sex distributions of PCR confirmed Covid cases (863,000 individuals; solid green line) reported in MCGM dashboard data (Banaji, 2022; IDFC Ins, 2022) and the PCR tested population in Thyrocare study data (76,000 individuals; dotted red are males, dotted blue are females). P-values of Kruskal-Wallis similarity test for age distributions were 0.53, 0.31 and 0.73 respectively.
Figure 1.
Age distribution of PCR confirmed cases between MCGM Covid dashboard and Thyrocare study data during the three viral waves. Aleph wave (Jun 2020-Nov 2020), (B) Delta wave (Mar 2021-Jun 2021), (C) Omicron wave (Jan 2022). This figure compares the similarity of age-sex distributions of PCR confirmed Covid cases (863,000 individuals; solid green line) reported in MCGM dashboard data (Banaji, 2022; IDFC Ins, 2022) and the PCR tested population in Thyrocare study data (76,000 individuals; dotted red are males, dotted blue are females). P-values of Kruskal-Wallis similarity test for age distributions were 0.53, 0.31 and 0.73 respectively.
Figure 2.
Trends in smoothed daily viral loads (inverse of cycle thresholds) and polymerase chain reaction (PCR) positivity in Thyrocare laboratory data in Mumbai, India. The trend graphs apply generalized additive models to examine changes in the daily median Ct value and PCR positivity over time. The thick red line represents the smoothed daily Ct values and surround pink lines are the corresponding 95% confidence intervals; the thick dark blue line represents the smoothed daily PCR positivity and the surround light blue lines are the corresponding 95% confidence intervals. Daily Ct values are plotted on reverse y-axis on the left, with lower Ct value correspond to higher viral load. The 95% confidence intervals of the daily predicted values show higher uncertainty for daily median Ct value in September 2020 to February 2021 and also show higher uncertainty both Ct daily median Ct value and PCR positivity in November to December 2022. The graph is restricted to the time period of August 24, 2020 to January 30, 2022, therefore only partially covered the Aleph wave which occurred from June – November 2020.
Figure 2.
Trends in smoothed daily viral loads (inverse of cycle thresholds) and polymerase chain reaction (PCR) positivity in Thyrocare laboratory data in Mumbai, India. The trend graphs apply generalized additive models to examine changes in the daily median Ct value and PCR positivity over time. The thick red line represents the smoothed daily Ct values and surround pink lines are the corresponding 95% confidence intervals; the thick dark blue line represents the smoothed daily PCR positivity and the surround light blue lines are the corresponding 95% confidence intervals. Daily Ct values are plotted on reverse y-axis on the left, with lower Ct value correspond to higher viral load. The 95% confidence intervals of the daily predicted values show higher uncertainty for daily median Ct value in September 2020 to February 2021 and also show higher uncertainty both Ct daily median Ct value and PCR positivity in November to December 2022. The graph is restricted to the time period of August 24, 2020 to January 30, 2022, therefore only partially covered the Aleph wave which occurred from June – November 2020.
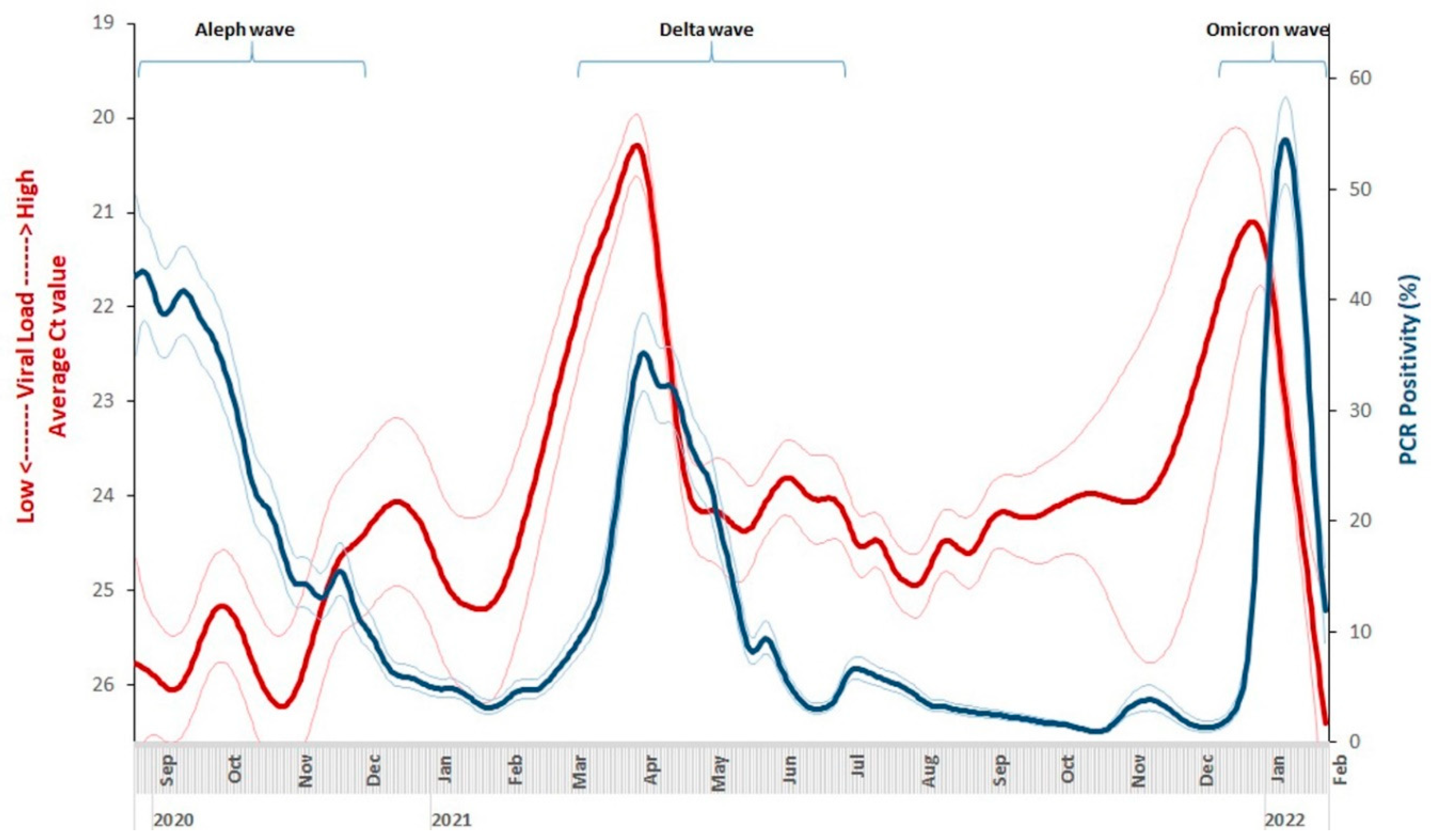
Figure 3.
Adjusted odds ratios of PCR positivity at 3 viral outbreak periods in Thyrocare data. For each pandemic outbreak period, a separate multivariable binary logistic model was fitted on PCR positivity in study data to assess the independent effects of covariates age (10 yearly groups), sex, and slum status of residence ward. The age group of 20-29 years usually had the lowest reporting PCR positivity among age groups, male in sex, and areas of low slum density that represents higher social status of living were selected as the relevant reference groups.
Figure 3.
Adjusted odds ratios of PCR positivity at 3 viral outbreak periods in Thyrocare data. For each pandemic outbreak period, a separate multivariable binary logistic model was fitted on PCR positivity in study data to assess the independent effects of covariates age (10 yearly groups), sex, and slum status of residence ward. The age group of 20-29 years usually had the lowest reporting PCR positivity among age groups, male in sex, and areas of low slum density that represents higher social status of living were selected as the relevant reference groups.
Figure 4.
Proportional odds ratios of high (lowest 25% of Ct values) vs medium (25%-75% of Ct values) viral load groups. (A) Delta wave: March-June 2021, (B) Omicron wave: January 2022. We fitted two separate multivariable proportional logistic models for Delta wave and for Omicron wave to assess the effects of age, sex, and slum density of residence ward between viral load categories (distingwished by Ct value quartile ranges high viral load: lowest 25% of Ct, medium: 25%-75%, low: highest 75% of Ct). The median quartile range was chosen as the reference group. The related (25%, 50%, 75%) quartile values of each viral wave were: Delta wave: (18.0, 23.0, 28.0) and Omicron wave: (19.5, 23.2, 27.6). We assess the effects of each independent covariates including age (10 yearly groups), sex, and slum density of residence ward on high viral loads vs medium viral loads using the proportional odds ratios. The age group of 20-29 years usually had the lowest reporting PCR positivity among age groups, male in sex, and areas of low slum density that represents higher social status of living were selected as the relevant reference groups.
Figure 4.
Proportional odds ratios of high (lowest 25% of Ct values) vs medium (25%-75% of Ct values) viral load groups. (A) Delta wave: March-June 2021, (B) Omicron wave: January 2022. We fitted two separate multivariable proportional logistic models for Delta wave and for Omicron wave to assess the effects of age, sex, and slum density of residence ward between viral load categories (distingwished by Ct value quartile ranges high viral load: lowest 25% of Ct, medium: 25%-75%, low: highest 75% of Ct). The median quartile range was chosen as the reference group. The related (25%, 50%, 75%) quartile values of each viral wave were: Delta wave: (18.0, 23.0, 28.0) and Omicron wave: (19.5, 23.2, 27.6). We assess the effects of each independent covariates including age (10 yearly groups), sex, and slum density of residence ward on high viral loads vs medium viral loads using the proportional odds ratios. The age group of 20-29 years usually had the lowest reporting PCR positivity among age groups, male in sex, and areas of low slum density that represents higher social status of living were selected as the relevant reference groups.
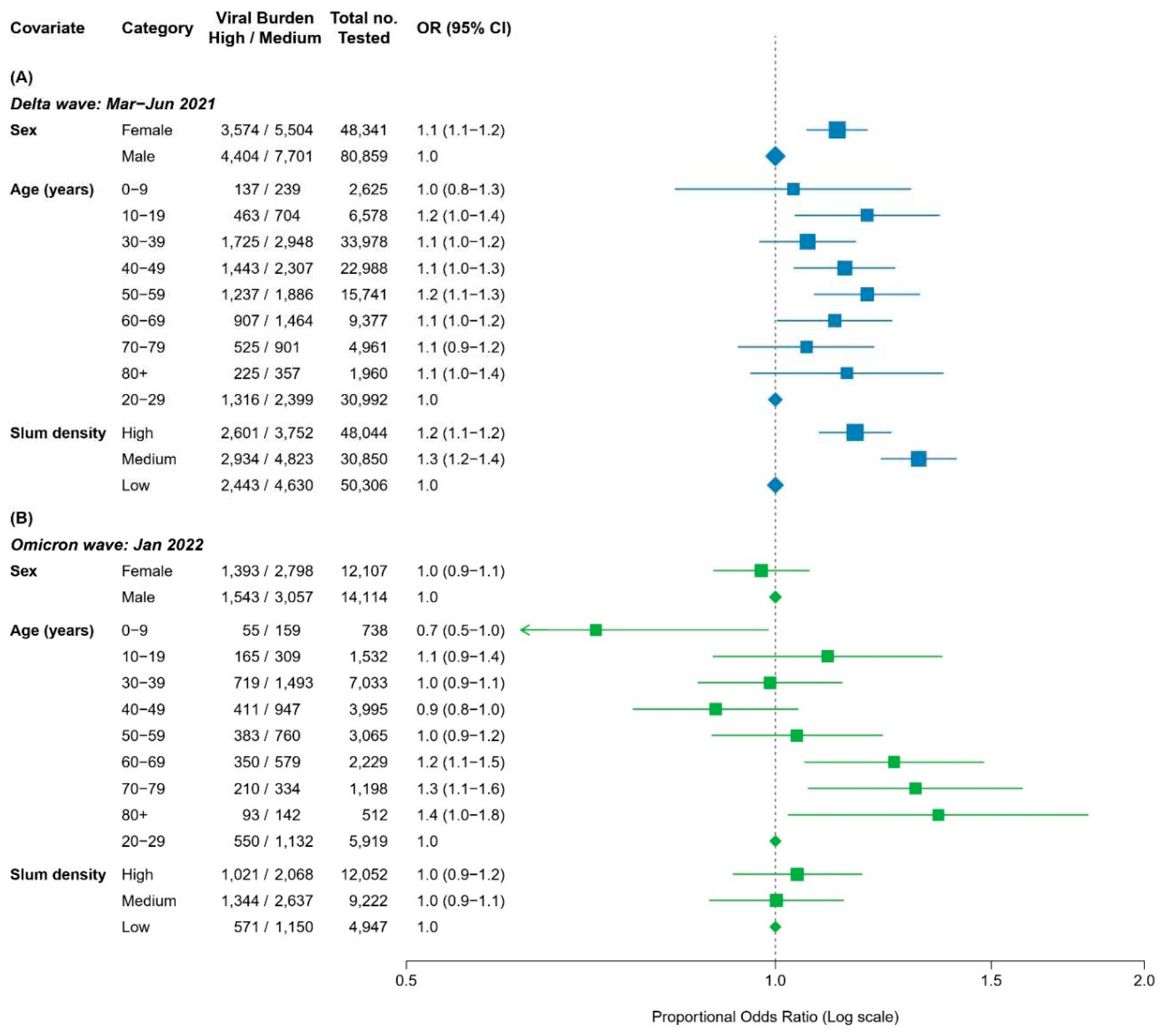
Table 1.
Summary of official case counts, community-level PCR positivity rates and median Ct values from MCGM Covid-19 dashboard and Thyrocare tested population during the pandemic period from Apr 2020 to Jan 2022.
Table 1.
Summary of official case counts, community-level PCR positivity rates and median Ct values from MCGM Covid-19 dashboard and Thyrocare tested population during the pandemic period from Apr 2020 to Jan 2022.
Data source/
Characteristics |
Overall period Apr 2020 to
Jan 2022
(22 months) |
Pandemic periods |
Non outbreak periods
(11 months) |
Aleph wave
(Jun-Nov 2020)
6 months |
Delta wave
(Mar-Jun 2021)
4 months |
Omicron wave
(Jan 2022)
1 month |
| Government Covid dashboard |
|
|
|
|
Official PCR confirmed cases
|
1,022,979 |
160,288 |
232,484 |
376,528 |
253,679 |
|
Case rate per 1000 population*
|
191.6 |
12.8 |
33.9 |
82.4 |
222.1 |
| |
Age <40 years |
130.5 |
7.6 |
18.1 |
54.3 |
159.1 |
| Age >= 40 years |
334.9 |
24.8 |
71.0 |
148.4 |
369.9 |
| Female |
n.a. |
n.a. |
29.0 |
76.1 |
191.6 |
| Male |
n.a. |
n.a. |
38.1 |
87.8 |
248.1 |
| Low slum areas |
261.2 |
16.4 |
45.1 |
123.5 |
262.5 |
| Medium slum areas |
173.8 |
13.1 |
32.8 |
77.4 |
195.7 |
| High slums |
151.5 |
8.2 |
25.9 |
68.8 |
164.3 |
| Thyrocare PCR testing |
|
|
|
|
| |
Total No. tested in 000 |
2,717.3 |
2,181.7 |
64.2 |
445.1 |
26.2 |
| |
Test positive in 000 |
155.0 |
78.8 |
17.9 |
46.6 |
11.7 |
| Overall PCR Positivity (%)† |
|
|
|
|
| |
All ages |
5.3 |
3.4 |
23.2 |
9.9‡ |
42.8 |
| Age < 40 years |
5.1 |
3.4 |
18.8 |
9.5 |
41.3 |
| Age ≥ 40 years |
6.5 |
3.9 |
36.9 |
11.7 |
49.2 |
| Female |
5.75 |
3.75 |
25.87 |
11.46 |
44.06 |
| Male |
4.98 |
3.2 |
21.91 |
8.98 |
41.82 |
| Low slum areas§ |
4.2 |
3.3 |
20.4 |
7.2 |
44.3 |
| Medium slum areas§ |
21.7 |
8.3 |
28.8 |
25.3 |
42.2 |
| High slum areas§ |
17.7 |
5.2 |
25.8 |
19.9 |
42.8 |
|
Median Ct value†
|
|
|
|
|
| |
Overall |
24.0 |
25.0 |
26.0 |
23.0 |
23.2 |
Inter quartile range
(Q1, Q3) |
(19.0,28.0) |
(20.0, 28.0) |
(21.0,31.0) |
(18.0, 28.0) |
(19.5, 27.6) |
| Age < 40 years |
24.0 |
25.0 |
25.0 |
23.0 |
23.1 |
| Age ≥ 40 years |
24.0 |
24.0 |
26.0 |
22.0 |
21.9 |
| Female |
24.0 |
25 |
25.0 |
23.0 |
23.1 |
| Male |
24.0 |
24 |
26.0 |
23.0 |
23.2 |
| Low slum areas§ |
24.0 |
25.0 |
26.0 |
24.0 |
22.9 |
| Medium slum areas§ |
22.3 |
23.0 |
25.0 |
21.0 |
23.0 |
| High slum areas§ |
23.0 |
23.1 |
26.0 |
22.0 |
23.4 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).