1. Introduction
The cavovarus foot is an acquired foot deformity with an incidence of about 1:100,000. It is due to progressive forefoot pronation, resulting in a high arch shape of the medial and middle foot and a compensatory varus of the hindfoot [
1]. The etiology of the cavovarus foot is complicated. According to the current research, the main factor leading to the cavovarus foot is the imbalance of muscle strength [
2]. The most common pathogenic factor is hereditary motor sensory neuropathy, found in 66% of children with hyper arch malformation [
2]. Other factors include myelomeningocele, poliomyelitis, residual malformation of horseshoe feet, post-traumatic high arches, etc. [
3,
4]. cavovarus is not a single planar deformity but a three-dimensional planar deformity of the foot.Foot deformities are complex, requiring careful medical history, physical examination, and imaging analysis to evaluate the cavovarus deformity of the foot in children fully.The selection of surgical methods for cavovarus feet is based on fully evaluating cavovarus foot deformity. The study by Coleman et al. [
5] proposed several evaluation methods: (1) For young children with mild cavovarus foot deformity accompanied by muscle imbalance, plantar fascia release combined with tendon transfer should be performed to restore muscle balance.② For older children with moderate-high arched deformity accompanied by muscle imbalance, plantar fascia release, tarsal osteotomy, and tendon transposition were performed.③ For older children with moderate and cavovarus deformity accompanied by first metatarsal saggy muscle imbalance, plantar fascia release, wedge osteotomy at the base of the first metatarsal, and extensor hallucis longus tendon transfer was performed.More specifically, an osteotomy is necessary for soft tissue release and tendon transfer in moderately high arches.However, various osteotomy procedures have been reported, and no single surgical procedure can be used as a standard surgical procedure for cavovarus.
Osteotomy should be performed in combination with soft tissue surgery. Most children with cavovarus deformities have intrinsic neuromuscular lesions, which require intraoperative adjustment of muscle strength to achieve a new balance of muscle strength to prevent the recurrence of the deformity. However, the efficacy after tendon transposition is difficult to predict and requires careful preoperative evaluation by the surgeon.Transfer of the fibula longus to the brevis is usually performed in conjunction with the surgical procedure.It eliminates plantar flexion of the peroneus longus near the first metatarsal, strengthens the valgus of the peroneus Breus, and indirectly improves the function of the tibialis anterior [
6]. In children with CMT, the strength of the tibialis anterior dorsalis extension of the ankle joint is weak.Therefore, the relative strength of the tibialis posterior muscle is too strong, resulting in varus deformity of the hind foot.In this case, partial transfer of the posterior tibialis tendon to the anterior tibialis tendon helps the patient realize the ankle better. It also helps to correct the posterior varus deformity indirectly [
7].
Currently, the transposition of the posterior tibial tendon [
8] is performed using the approach described by Hsu and Hoffer, which consists of four steps: (1) Complete dissection of the posterior tibial tendon from the scaphoid; (2) Make a complete incision on the medial side of the distal tibia to free the posterior tibial tendon completely; (3) The posterior tibial tendon was transferred from the medial incision to the anterior incision, and it was divided into two bundles; (4) The tendon was separated into two bundles, one of which was attached to the lateral cuneus and the other to the peroneus brevis.Not only adjust the balance of muscle force but also correct the force line of the foot so that the effect of osteotomy orthopedic surgery to maintain well.Currently, several osteotomy methods for the middle foot have been reported, and different osteotomy methods are selected according to the different characteristics of each patient.Generally, the apex of the cavovarus foot deformity is on the navicular cuneiform joint or the medial cuneus and can be corrected by the first metatarsal dorsal wedge osteotomy combined with the first cuneus metatarsal wedge osteotomy.
Mubarak et al. [
9] used the first sequence osteotomy to treat stiff high arches with an average age of 11 years. That is, the first step was to perform a closed dorsal wedge osteotomy of 20-30° at the proximal end of the metatarsal head and remove the bone fragments; the second step was to perform an open metatarsal osteotomy of 20-30° at the medial cuneus and put the bone fragments obtained in the first step into the cuneus space.The final follow-up time was 46 months, no serious complications occurred, and both imaging and clinical symptoms were improved.The first metatarsal osteotomy is a single-plane osteotomy with more sagittal plane correction.Although it is possible to correct adduction deformities of the middle foot with cuboid osteotomy, it is effective in orthosis for high arches with multiple planar deformities.
Japas [
10] described in 1968 the treatment of the "V" -shaped osteotomy of the tarsal bone in the middle foot, which could correct the deformity on all sides without removing bone or bone grafting. However, according to the research results, the effect of correcting the rotary deformity was limited. Chatterjee reported [
11] that 18 patients with neuromuscular cavovarus were treated with Japas, V-osteotomy. The mean follow-up time was 5.4 years, and the good rate was 77%.
Japas osteotomy of the middle foot preserves the ankle joint activity and sacrifices the intertarsal joint but does not remove the bone block and preserves the integrity of the foot. In addition, the osteotomy is closer to or even at the apex of the deformity, which can most effectively repair the deformity of the high arcs. Moreover, the middle foot osteotomy can correct the deformity of each plane, which has more advantages than the first sequence osteotomy. For children, both osteotomy methods belong to less traumatic osteotomy methods, and both retain the integrity of the foot, providing space for subsequent treatment. However, according to the current research, no study compares the two osteotomy methods, so it is impossible to evaluate them objectively. Therefore, it is necessary to study and evaluate the efficacy of the two surgical methods to provide some basis for selecting subsequent treatment methods and an optimal surgical method with minimal trauma to children.
2. Materials and Methods
2.1. Research Objects
2.1.1. Data Collection
Data sources We collected and retrospectively analyzed the children admitted to our department from January 2012 to January 2019, diagnosed as hyper arch, and underwent surgical treatment, including 30 cases of light and medium hyper arch who underwent osteotomy and orthosis based on soft tissue release. The first metatarsal osteotomy was performed on 22 feet of 16 patients, and Japas osteotomy was performed on 21 feet of 14 patients.
2.1.2. Inclusion Criteria
The inclusion standard age ranges from 8 to 14 years old; All cases were routinely examined by X-ray, spinal MRI, and neuro electromyography before surgery to exclude the hyper arches caused by other diseases and were finally diagnosed as neurogenic hyper arches. Imaging examination indicated that the apex of the cavovarus deformity was located in the medial cuneiform or navicular cuneiform joint.; Follow-up time was more than 1 year; Children who underwent middle foot Japas osteotomy and first metatarsal osteotomy; After orthopedic surgery, patients were followed up in the outpatient department of our hospital, and complete imaging data were kept.
2.1.2. Exclusion Criteria
We excluded patients who only underwent soft tissue surgery; Fixed varus deformity of the hindfoot; Children with mental disorders who cannot cooperate to complete the examination; Children with incomplete follow-up data.
2.2. Methods of Surgical Treatment
1. All the children underwent osteotomy and received plantar fascia release. Longitudinal incisions with a length of about 3cm were interrupted along the medial plantar.2. First metatarsal osteotomy group:1. The first metatarsal order bone amputation, a longitudinal incision of the first metatarsal column, about 6cm long, each layer is cut open to expose the first metatarsal bone and the inner bone. The proximal end of the first metatarsal bone opening toward the back V-shape bone amputation, the wedge bone block is removed, and then the medial wedge bone transverse bone amputation is performed, and the foot is placed in an orthopedic position. A Kirschner wire or two Kirschner wires were percutaneously introduced from the distal end of the first metatarsal to traverse the two osteotomy ends.
2. Closure of the lateral cuboid bone was added, and a longitudinal incision was made along the lateral edge of the midpoint of the cuboid in the middle foot to separate and avoid the sural nerve in order to prevent damage, releasing the sheath of the peroneus brevis tendon exposed the peroneus brevis muscle. It is pulled to the plantar side to expose the cuboid bone in the dorsal, lateral, and metatarsal periosteum. Two 25G syringe needles were inserted at the intended osteotomy points of the cuboid bone to ensure that a wedge of sufficient size could be removed to correct the adduction deformity at the lateral edge of the foot. The proximal needle should be perpendicular to the long axis of the fifth metatarsal. With the fluoroscopic guidance of the C-arm machine, a small swing saw was used to cut bone close to the needle, a wedge bone block was cut out, and the Kirschner wire was closed for fixation (
Figure 1).
2.3. Observation Indicators
The blood loss and operation time of the two methods were compared. Wicart scoring criteria (
Table 1) were used to score the children after surgery, and the anterior-lateral position of standing weight bearing was photographed. Meary, Hibb, and Pitch Angle were measured at the last follow-up to evaluate the clinical efficacy.
2.4. Measurement on X Line
2.4.1. Measurement Equipment
2.4.2. Measurement of Foot Front and Side Slices
1. Lateral radiographs of feet in standing weight-bearing position: Angle of the first metatarsal (Meary Angle), Angle of calcaneal inclination (pitch Angle), Angle of calcaneal (Hibb Angle).
2. Orthograph of foot in standing weight-bearing position: Angle of talus - first metatarsal, Angle of talus calcaneus. The Angle obtained from the lateral measurements reflects the alignment of the hindfoot and forefoot in the sagittal plane. These angles have the advantage of being simple and reproducible to distinguish foot shape, and they indicate the shape of the foot in the sagittal and horizontal planes.
2.4.3. Measurement Methods and Significance
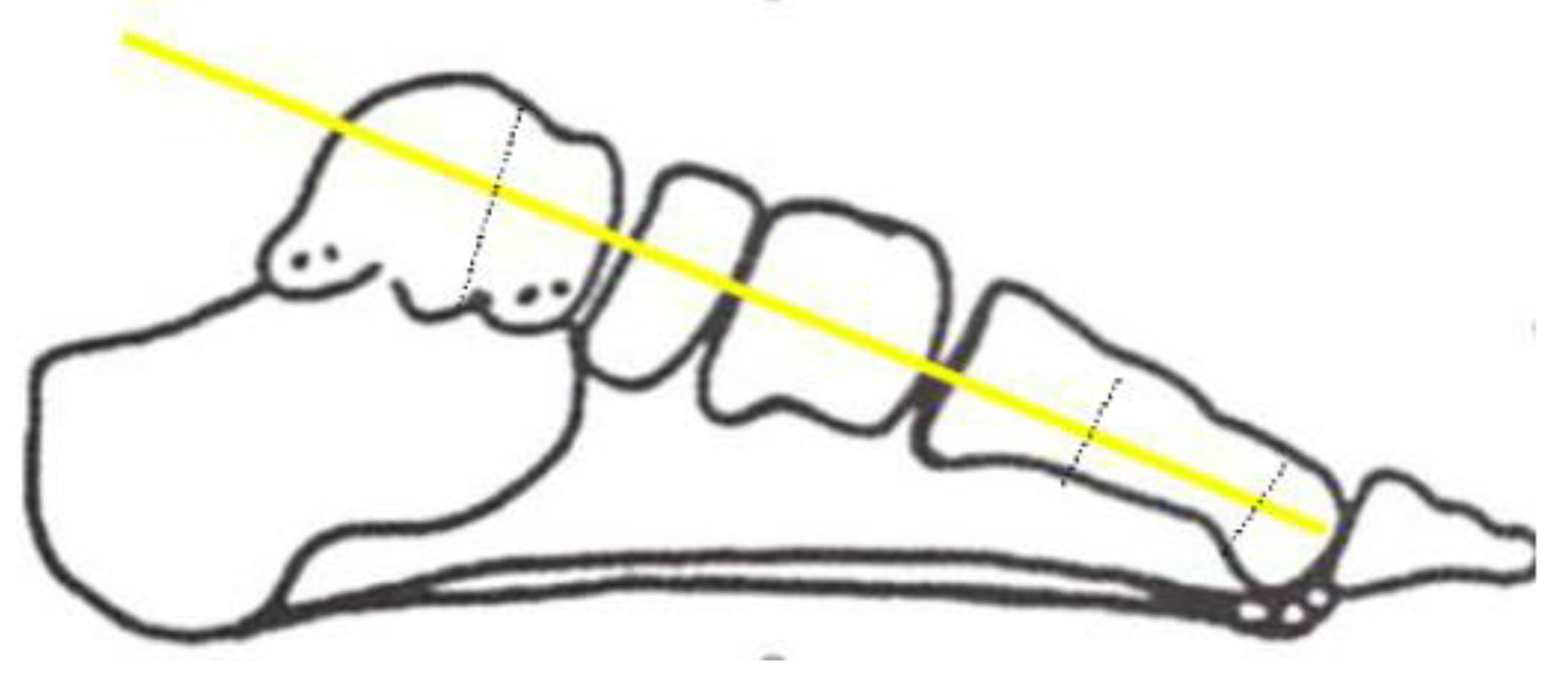
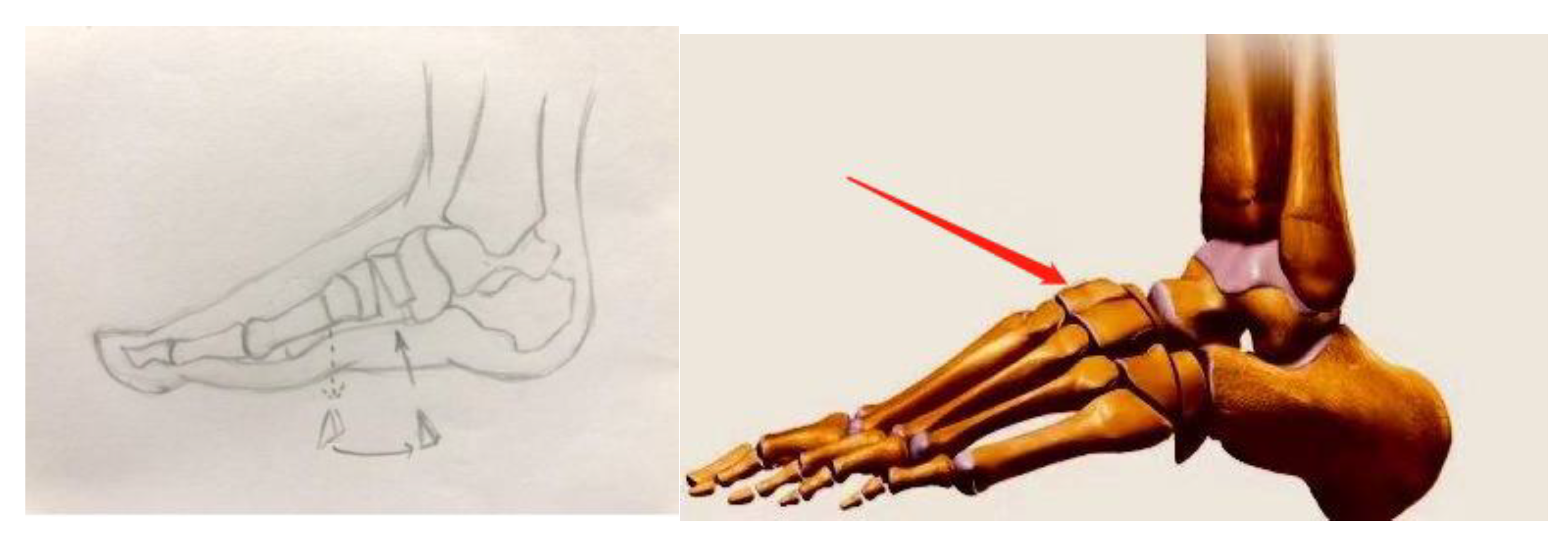
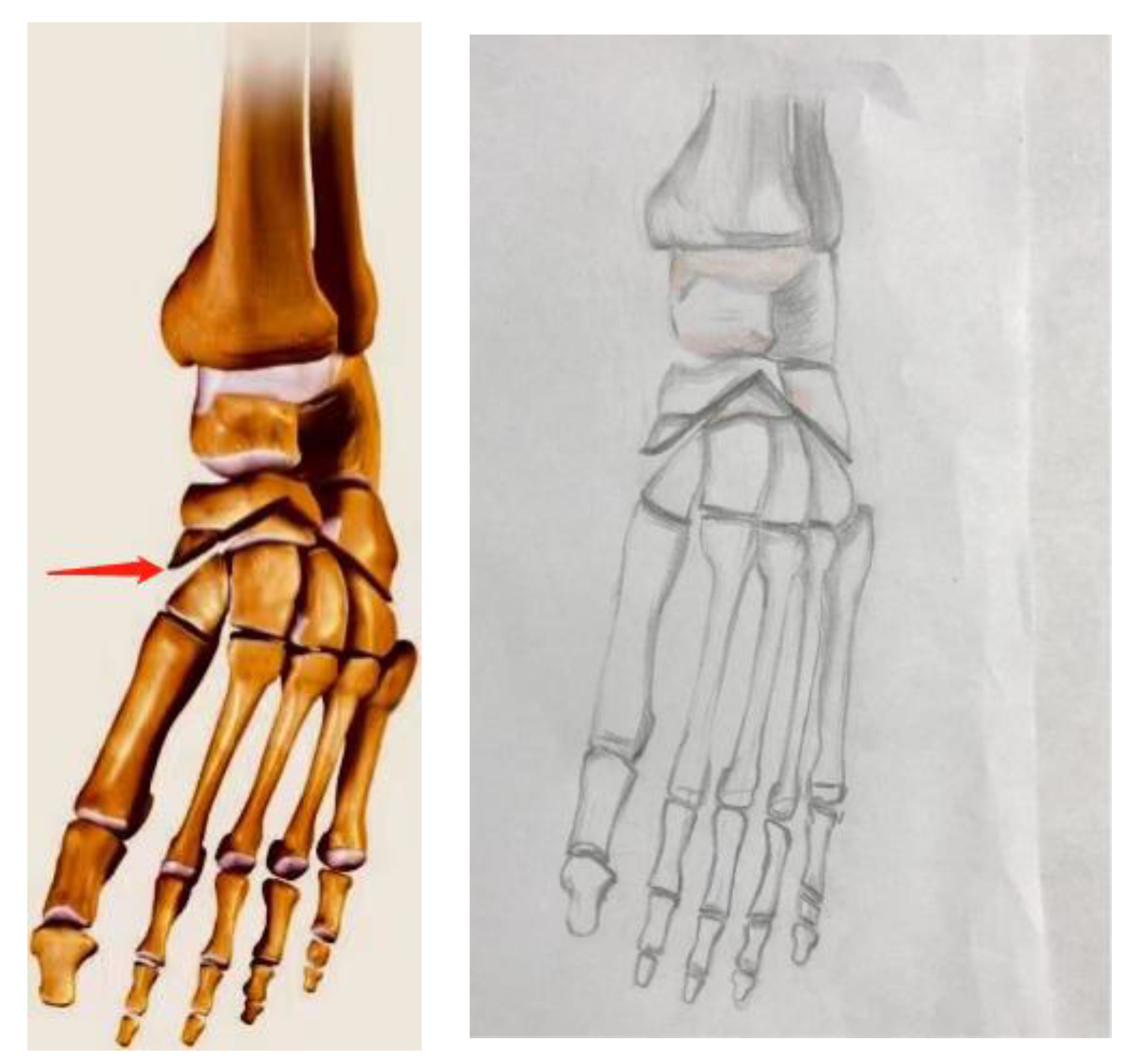
1. On lateral radiographs, the Angle of the first metatarsal talus (Meary Angle): The Angle between the midpoint of the upper and lower surfaces of the middle talus and the line between the midpoint of the neck of the talus and the line between the midpoint of the distal and proximal diaphysis of the first metatarsal shaft. Since the central axis of the talus and the first metatarsal bone is difficult to draw accurately, the dorsal tangent line between the talus and the first metatarsal bone is used to obtain the normal value of 0°. It is a direct method to measure the sagittal deformity of the foot.
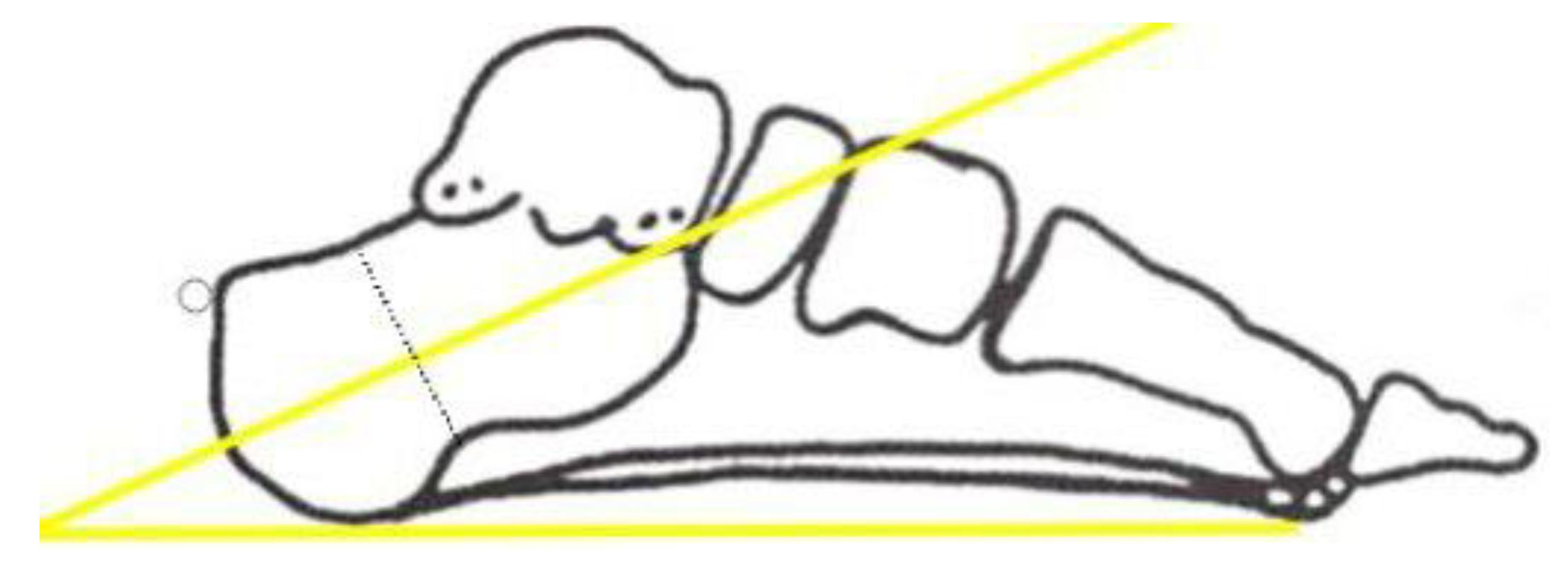
2. Calcaneal inclination Angle (pitch Angle) of lateral radiographs: the Angle between the line between the lower anterior margin of the calcaneus and the lowest point of the first metatarsal bone and the line between the lower anterior margin of the calcaneus and the lowermost margin of the anterior tubercle of the calcaneus.Normal value <30°.>30° indicates that the cavovarus originates from the hindfoot. The calcaneal inclination is the Angle between the calcaneus's lower surface and the calcaneus's supporting surface.
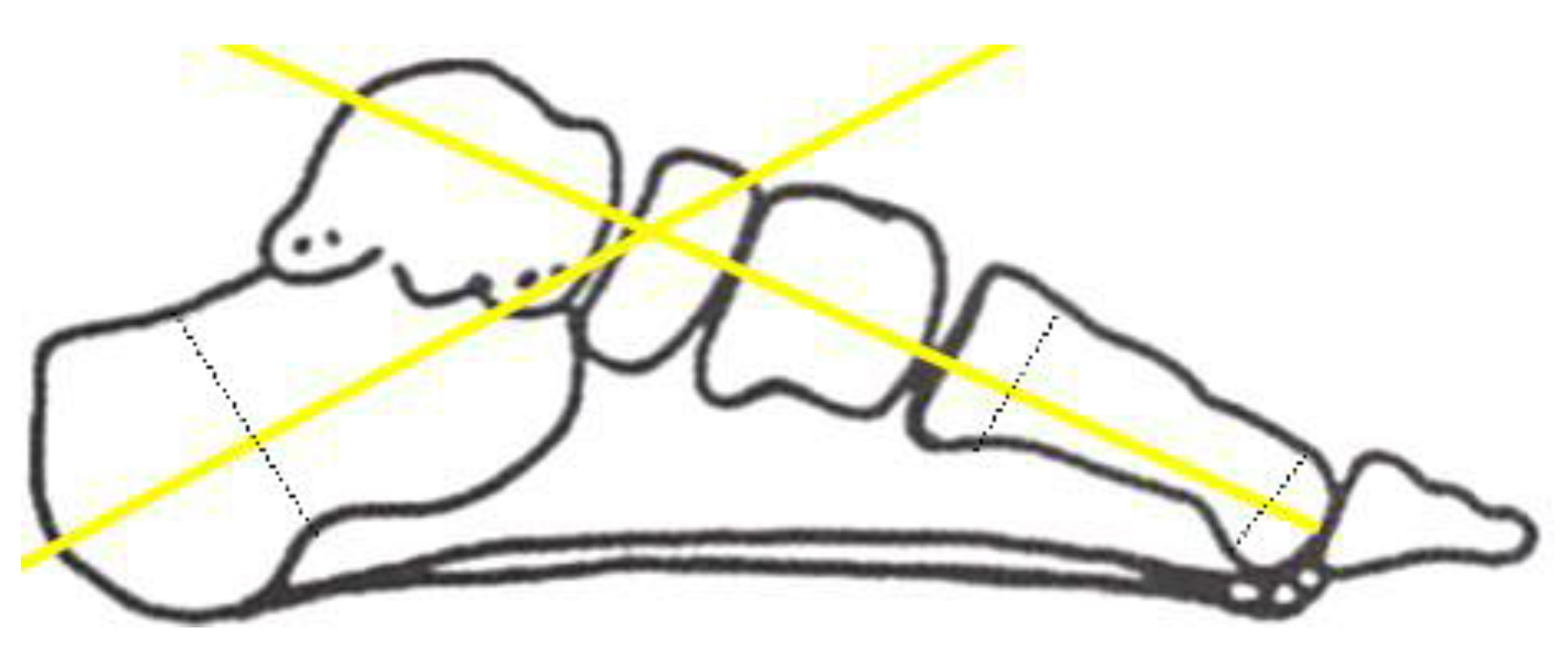
3. Angle of distance from the calcaneus (Hibb Angle) of lateral radiographs: refers to the Angle between the calcaneus axis and first metatarsal bone, which is generally less than 45°, and Hibb Angle of cavovarus deformity is generally greater than 90° (Figure 5).
Figure 3.
Meary's Angle: The Angle between the midpoint of the upper and lower surfaces of the middle talus and the line between the midpoint of the neck of the talus and the line between the midpoint of the distal and proximal diaphysis of the first metatarsal shaft.
Figure 3.
Meary's Angle: The Angle between the midpoint of the upper and lower surfaces of the middle talus and the line between the midpoint of the neck of the talus and the line between the midpoint of the distal and proximal diaphysis of the first metatarsal shaft.
Figure 4.
Measurement of Pitch Angle: The Angle between the line between the lower anterior margin of the calcaneus and the lowest point of the first metatarsal bone and the line between the lower anterior margin of the calcaneus and the lowermost margin of the anterior tubercle of the calcaneus.Normal value <30°.>30° indicates that the cavovarus originates from the hindfoot.
Figure 4.
Measurement of Pitch Angle: The Angle between the line between the lower anterior margin of the calcaneus and the lowest point of the first metatarsal bone and the line between the lower anterior margin of the calcaneus and the lowermost margin of the anterior tubercle of the calcaneus.Normal value <30°.>30° indicates that the cavovarus originates from the hindfoot.
Figure 5.
Measurement method of Hibb Angle: Hibb Angle is the Angle between the calcaneal axis and the first metatarsal bone, which is generally less than 45°, and the Hibb Angle of cavovarus deformity is generally greater than 90°.
Figure 5.
Measurement method of Hibb Angle: Hibb Angle is the Angle between the calcaneal axis and the first metatarsal bone, which is generally less than 45°, and the Hibb Angle of cavovarus deformity is generally greater than 90°.
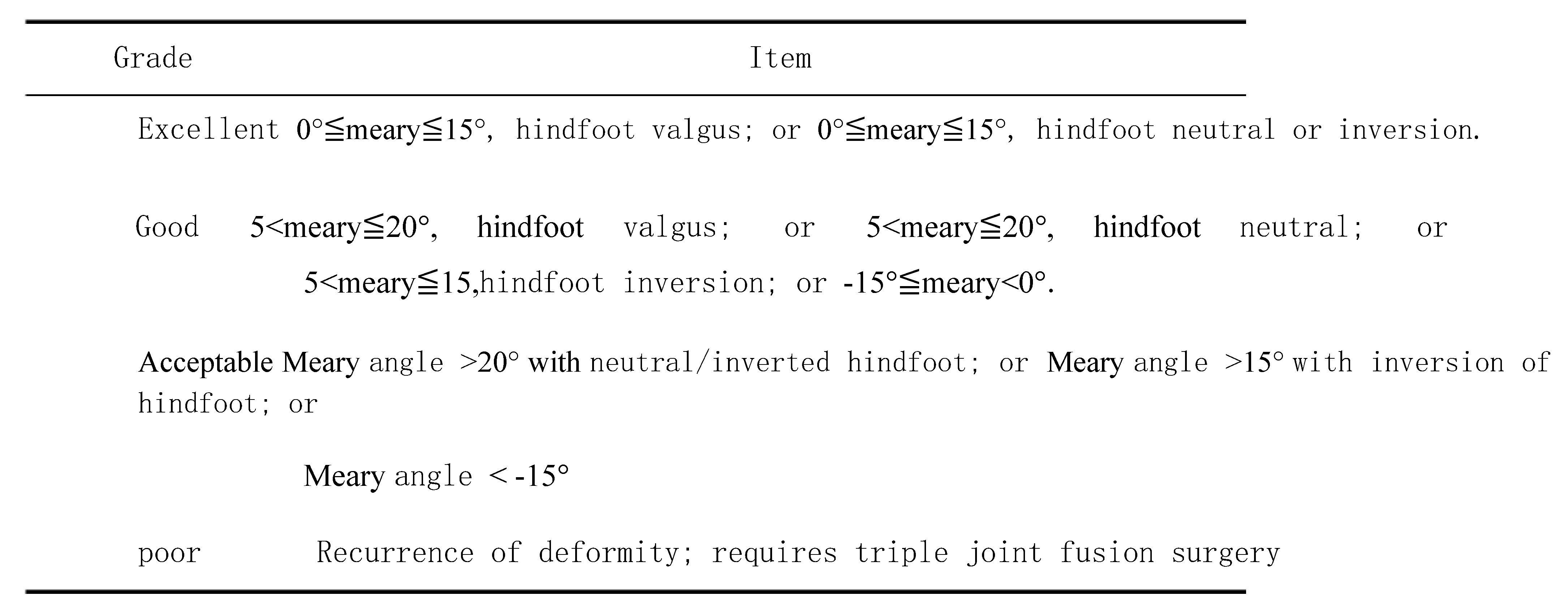
2.5. Efficacy Evaluation According to the Wicart Classification as an Indicator to Evaluate Early Prognosis, it is Divided into Four Grades [16]. (Table 1)
Table 1.
Wicart classification.
Table 1.
Wicart classification.
2.6. Statistical Methods of Operation Time and Blood Loss
Statistical methods of operation time: The time of operation was the time from the incision to the end of the skin suture.Statistics of the amount of blood loss: the amount of blood loss = the amount of blood in the storage perfusion + blood gauze + the amount of blood on the peripheral excipients of the incision.
2.7 Statistical Methods After data collection, SPSS24 software was used for processing, and SPSS statistical software was used for processing. Consistent measurement data were expressed as X±S, an independent sample t-test was used for the two surgical methods, and P<0.05 was considered statistically significant.
(1) To compare the results of Angle improvement between the two groups: an independent sample t-test was used to test Meary, Hibb, and Pitch Angle, respectively.
(2) Independent sample t-test was used to compare postoperative operation time and blood loss between the two groups.
(3) Fisher's exact probability method was used to test the good postoperative rate of the two groups.
3. Results
3.1. Follow-Up Results
Thirty children with high arches arcuate feet were included in the final follow-up. The first group included 16 children with the first sequence osteotomy, aged 8-13 years with an average age of 10.5±3.0 years, of whom 5 were bipedal, 7 were right foot, and 4 were left foot. In the second group, there were 14 cases with a median age of 11.1±2.8 years, ranging from 8 to 14 years. There were seven patients with two feet, three with right feet, and four with left feet. There was no statistical difference between the two groups regarding age and gender. The severity of the malformation did not differ significantly across groups. All patients were followed up for an average of 30 months. The children with the first metatarsal osteotomy and Japas osteotomy of the middle foot recovered well, and their daily activities were not significantly limited. There were 3 cases of cavovarus foot deformity recurrence, 2 cases in the first metatarsal osteotomy group, and 1 in the Japas osteotomy group, but the children's daily activities were not significantly limited.
3.2. Wicart Score Results
(1) At the last follow-up, the Wicart score of the first plantar-sequence osteotomy was excellent in 6 cases (37.5%), good in 8 cases (50.0%), fair in 2 cases (12.5%), and the rate of excellent and good was 87%. At the last follow-up, the Wicart score of Japas osteotomy in the middle foot was excellent in 6 cases (42.8%), good in 7 cases (50%), and fair in 1 case (7.1%) (see
Table 2).
3.2. Radiographic Assessment
1. The first plantar sequence cut bone and foot Japas bone cutting Angle of two groups of preoperative Meary respectively ± 22.3 (5.4) and (21.1 ± 3.2), P > 0.05, no statistically significant data, show that two groups of children with preoperative Meary Angle, there is no obvious difference. Postoperative Meary Angle respectively, the two groups at the time of the last follow-up ± 16.5 (5.7) and (14.3 ± 7.1), P>0.05, the data was not statistically significant, indicating that the Meary Angle of the two groups was the same at the last postoperative follow-up, and there was no significant difference.
2. The first plantar sequence cut bone and foot Japas bone cutting Angle of two groups of preoperative Hibb respectively ± 125.6 (8.1) and (128.4 ± 7.6), P > 0.05, no statistically significant data, show that two groups of children with preoperative Hibb Angle, there is no obvious difference. Postoperative Hibb Angle respectively, the two groups at the time of the last follow-up ± 123.6 (9.0) and (117.3 ± 9.5), P > 0.05, no statistically significant data, shows that at the end of the postoperative follow-up time of two groups of children with Hibb Angle, there is no obvious difference.
3. The first plantar sequence cut the bone, and the foot Japas cut bone preoperative Pitch Angle of the two groups respectively ± 26.2 (7.9) and (31.3 ± 6.9), P > 0.05, no statistically significant data, shows that preoperative Pitch Angle of two groups of children with almost the same, there is no obvious difference. At the time of the last follow-up after two groups of Pitch Angle respectively ± 25.6 (6.7) and (26.2 ± 5.1), P > 0.05, no statistically significant data, shows that at the end of the postoperative follow-up time of two groups of children with Pitch Angle, there is no obvious difference.
3.3. Postoperative Blood Loss and Operation Time
1. The amount of intraoperative blood loss in the first metatarsal osteotomy group and Japas osteotomy group was (40±10.5) and (80±12.3) ml, respectively, P<0.05, indicating that there was a significant difference in the amount of blood loss between the two groups, and the amount of blood loss in the first metatarsal osteotomy was less than that in Japas osteotomy of the middle foot.
2. Operation time: The operation time of the first metatarsal osteotomy group and the middle foot Japas osteotomy group was (63±10.3) min and (78±13.6) min, respectively, P<0.05, indicating that there was a significant difference in the amount of blood loss between the two groups. The operation time of the first metatarsal osteotomy was less than that of the middle foot Japas osteotomy group.
Table 3.
Comparison of Meary, Hibb, and Pitch Angle between the two groups before and after surgery.
Table 3.
Comparison of Meary, Hibb, and Pitch Angle between the two groups before and after surgery.
| |
|
Meary° |
|
Hibb° |
|
Pitch° |
| |
Pre-operative |
Postoperative |
Pre-operative |
Postoperative |
Pre-operative |
Postoperative |
| First sequence osteotomy |
22.3 5.4 |
16.5 5.7 |
125.6 8.1 |
123.6 9.0 |
26.2 7.9 |
25.6 6.7 |
| Osteotomy of the midfoot tarsus |
21.1 3.2 |
14.3 7.1 |
128.4 7.6 |
117.3 9.5 |
31.3 6.9 |
26.2 5.1 |
| P |
=0.388 |
=0.498 |
=0.086 |
= 0.258 |
= 0.078 |
= 0.695 |
| |
|
|
|
|
|
|
Table 4.
Intraoperative blood loss and operation time.
Table 4.
Intraoperative blood loss and operation time.
| |
First sequence osteotomy |
Osteotomy of the midfoot tarsus |
|
| |
|
|
|
| Age |
10.5±3.0
|
11.1±2.8
|
P>0.05 |
| Gender (m %) |
8 (50%) |
8 (57%) |
P>0.05 |
| Bleeding volume (ml) |
40±10.5
|
80±12.3
|
P=0.00 |
| Operating time (min) |
63±10.3
|
78±13.6
|
P=0.00 |
3.3. Typical Cases
3.3.1 An 11-year-old male patient undergoing orthopedic osteotomy of the first metatarsal sequence came to our hospital for pain while walking on the left foot for over half a year. The corpus callosum was visible at the base of the first metatarsal bone and the base of the fifth metatarsal bone of the left foot, and the tenderness was obvious. During the passive activity, the patient has limited dorsalis extension and posterior varus. Coleman test showed no fixed deformity of the hind foot. The anteroposterior and lateral images of the foot suggested the presence of hyper arcuate deformity in the left foot, with a Meary Angle of 22°, pitch Angle of 26°, Hibb Angle of 120°.1. Cerebral palsy;2. Neuromuscular hyper arches. After the first metatarsal osteotomy and orthosis, the deformity of the high arch improved significantly. The stitches were removed and discharged 2 weeks after the surgery, the plaster was fixed for 2 months after discharge, and rehabilitation training was performed for 3 months after the plaster was removed. The follow-up was once every 3 months, and the final follow-up was 30 months.
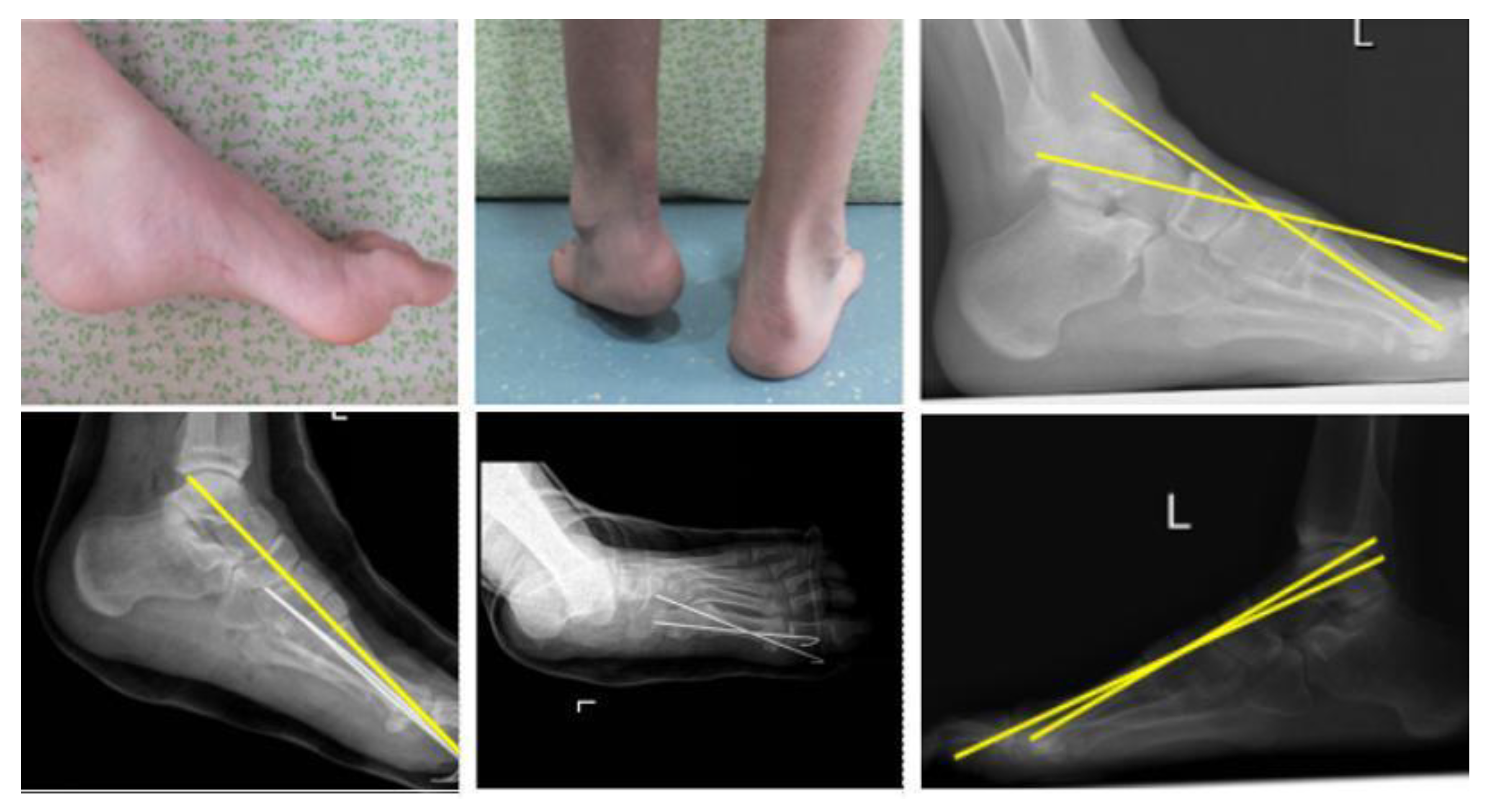
Figure 6.
(a,b) shows the external observation of the affected foot before surgery.c is preoperative radiography of the affected foot in the standing weight-bearing position, indicating the presence of cavovarus. d-e was a postoperative foot X-ray of the child, and Kirschner wire was fixed at the osteotomy of the first metatarsal sequence, showing that the deformity had been significantly improved. f is the lateral foot radiographs of the patient at the last follow-up, showing no recurrence of cavovarus foot deformity; the orthopedic effect is maintained well.
Figure 6.
(a,b) shows the external observation of the affected foot before surgery.c is preoperative radiography of the affected foot in the standing weight-bearing position, indicating the presence of cavovarus. d-e was a postoperative foot X-ray of the child, and Kirschner wire was fixed at the osteotomy of the first metatarsal sequence, showing that the deformity had been significantly improved. f is the lateral foot radiographs of the patient at the last follow-up, showing no recurrence of cavovarus foot deformity; the orthopedic effect is maintained well.
3.3.2 A 12-year-old male patient with a middle foot Japas osteotomy came to our hospital for pain during walking on the left foot for more than 1 year. The corpus callosum was visible at the base of the first metatarsal bone and the base of the fifth metatarsal bone of the left foot, and the tenderness was obvious. During the passive activity, the patient has limited dorsalis extension and posterior varus. Coleman test showed no fixed deformity of the hind foot. The anteroposterior and lateral images of the foot suggested the presence of hyper arcuate deformity in the left foot, with a Meary Angle of 27°, pitch Angle of 26°, and Hibb Angle of 130°. The diagnosis was neuromuscular hyper arches. The cavovarus deformity was significantly improved after V-type osteotomy and orthosis. The cast was fixed for 2 months after discharge, and rehabilitation training was performed for 3 months after removing the cast. The follow-up was conducted every 3 months, and the final follow-up was 30 months. The final follow-up lasted for 30 months. At the last follow-up, walking gait was normal, there was no obvious pain in the left foot, and daily activities were unrestricted.
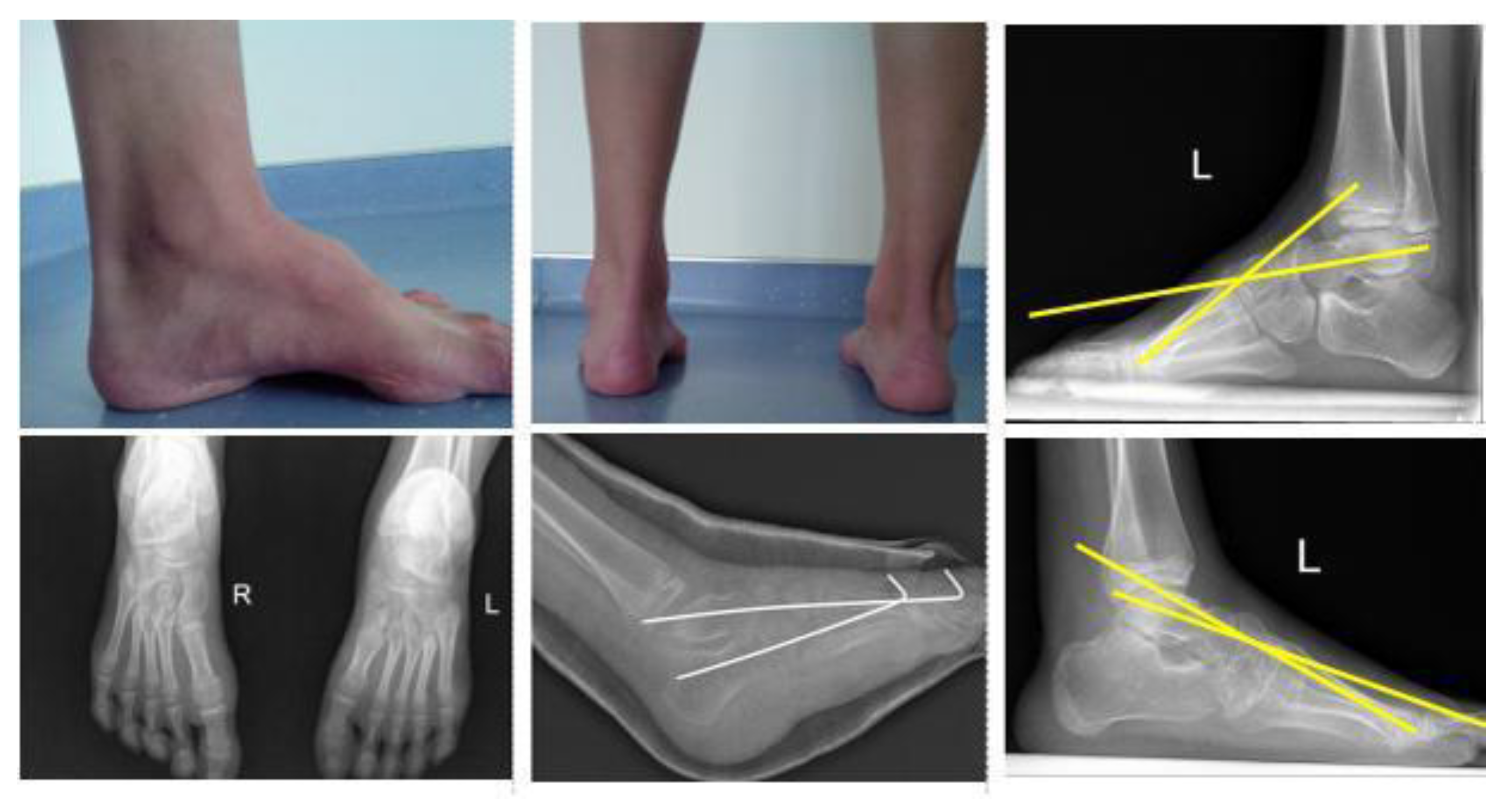
Figure 7.
(a,b) shows the external observation of the affected foot before surgery, indicating the presence of cavovarus. c is the postoperative X-ray of the child's foot, which reveals a cavovarus foot deformity; d is a simulated image of intraoperative deformity adjustment, and traditional 2-heel-Kirschner wires were fixed at the osteotomy [
19]. e is the postoperative X-ray of the child, which demonstrates that the deformity has been significantly improved; f is the lateral film of the child's foot bearing at the last follow-up, which demonstrates that there was no recurrence of the cavovarus foot deformity and that the orthopedic effect was well maintained.
Figure 7.
(a,b) shows the external observation of the affected foot before surgery, indicating the presence of cavovarus. c is the postoperative X-ray of the child's foot, which reveals a cavovarus foot deformity; d is a simulated image of intraoperative deformity adjustment, and traditional 2-heel-Kirschner wires were fixed at the osteotomy [
19]. e is the postoperative X-ray of the child, which demonstrates that the deformity has been significantly improved; f is the lateral film of the child's foot bearing at the last follow-up, which demonstrates that there was no recurrence of the cavovarus foot deformity and that the orthopedic effect was well maintained.
4. Discussion
4.1. Evaluation of Foot Flexibility
cavovarus are acquired foot malformations in which the first metatarsal bone sags due to progressive forefoot pronation, resulting in a cavovarus formation of the middle foot and a compensatory varus of the hind foot. The etiology of the cavovarus foot is complicated. According to the current research, the main factor leading to the cavovarus foot is the imbalance of muscle strength. Most cavovarus have no clear cause, and the most common causative factor is hereditary motor sensory neuropathy (CMT), which accounts for approximately 66% of all cavovarus [
1,
2,
3,
4].
CMT is due to the imbalance of muscle strength between superficial and deep muscles, leading to cavovarus in children, and cavovarus deformity is often progressive and aggravated [
4]. An important aspect of treating cavovarus is understanding whether the children's cavovarus are progressively aggravated. Therefore, treating children with cavovarus caused by CMT must be more aggressive to delay or avoid joint fusion surgery. The Coleman test is most commonly used to determine the foot's flexibility. The medial side of the foot was suspended in the air, the lateral side was placed on a 2.5cm wooden block, and the anterolateral X-ray film of the foot was taken. The alignment of the forefoot was restored to normal, and the deformity of the cavovarus was corrected, proving that only soft tissue could be performed [
5,
6]. If the alignment of the front foot does not return to normal, osteotomy of the front foot should be performed. If the back foot cannot be corrected, osteotomy of the calcaneus should be performed. Coleman et al [
5] straightened the affected limb of the child to correct the forefoot's cavovarus and subtalar joint artificially. If correct, it would be flexibility, which the author believed was more reliable than Coleman's test [
5]. However, we believe that the Coleman test is more objective. The Coleman test tested all the included cases for foot flexibility. No fixed varus deformity was found in the hind foot of all the children, and the posterior varus deformity could be restored to a neutral position after the correction of the cavovarus of the forefoot.
4.2. Selection of Evaluation Indicators
Imaging examination can quantify children's cavovarus foot deformity. The foot stand weight can measure cavovarus of the malformation rate is side a little while Meary Angle (from the first metatarsal bone and attachment Angle), normal Meary Angle of 0 ± 5 °, prompt the axis of the talus and the axis of the first metatarsal in the same line. Meary Angle >5° indicates metatarsal flexion of the first metatarsal bone. The Meary Angle of the high arcuate foot is 18° on average. Deformities of the hind foot were assessed by measuring calcaneal Pitch Angle and Hibb Angle on standing weight-bearing lateral radiographs. The Pitch Angle of the calcaneus is the Angle formed by the horizontal line connecting the calcaneus to the ground and the calcaneus' axis. The normal Pith Angle of the calcaneus is 22°, and the Pitch Angle of calcaneus >30° indicates a Cavovarus; the deformity originates from the hindfoot. The Hibb Angle is the Angle between the calcaneus axis and the first metatarsal bone, which is generally less than 45°, and the Hibb Angle ofCavovarus deformity is generally greater than 90°. Bilateral standing anterioradiography can be used to understand coronal deformities. The overlap between metatarsal bones indicates pronation of the forefoot, and the Angle between the talus and calcaneus is greater than 7°, indicating adduction deformity of the forefoot [
7,
12]. Several studies have adopted these three Angle indicators for postoperative follow-up evaluation of surgical efficacy [
9,
12,
13,
14].In this study, these three imaging indicators were the indicators to evaluate the severity of the deformity before surgery and the exact measurement indicators of the orthopedic effect during the postoperative follow-up.
4.3. Treatment of Cavovarus
4.3.1. Conservative Treatment
Currently, there is no universally recognized treatment for cavovarus at home and abroad, and the effect of conservative treatment for cavovarus is not exact. Recent studies have shown that conservative therapy can also have certain effects, especially for younger children, suggesting that although the efficacy of conservative therapy for neurogenic children is limited, conservative therapy should also be used as an adjuvant therapy strategy [
9,
15]. Astorg reported that through conservative treatment of children with cavovarus foot deformity, the good and good rate reached 65% during 4.5 years of follow-up, resulting in surgery being avoided or delayed for 4.5 years [
12]. A randomized trial by Maas proved that for neurogenic cavovarus, children had poor compliance with conservative treatment, and conservative treatment could not prevent the progression of the deformity [
16]. In this study, our treatment concept is similar to that of Maas. The patients included in this study are all hyper arches foot lesions caused by neuromuscular origin. Even if conservative treatment is adopted, the course of the disease cannot be blocked, so we believe that more active surgical intervention should be taken for this type of child to achieve satisfactory therapeutic effects.
4.3.2. Soft Tissue Release and Tendon Transposition
At present, there is a great controversy on the selection of surgical methods for the treatment of children's neuromuscular cavovarus, but there is no consensus on a single surgical method for the treatment of children's cavovarus. Regardless of the surgical method, the purpose of treatment is to achieve foot rebalancing, normal plantar pressure distribution, no recurrence or progression of the deformity, and delay or even avoid the occurrence of arthritis [
17,
18]. For the treatment of cavovarus, especially in children with neurogenic cavovarus, the strength of the anterior tibialis muscle dorsalis extension of the ankle joint is weak. Therefore, the relative strength of the tibialis posterior muscle is too strong, resulting in varus deformity of the hind foot. In this case, transferring the posterior tibialis tendon to the anterior tibialis tendon may help the patient better realize the ankle joint and may also help to correct the posterior varus deformity indirectly. Currently, the procedure described by Hsu and Hoffer [
18] for the transposition of the posterior tibial tendon consists mostly of four steps: ① Completely detach the posterior tibial tendon from the scaphoid;② Completely free the posterior tibial tendon on the medial side of the distal tibia;③ Transfer the posterior tibial tendon from the medial incision to the anterior incision, and divide it into two bundles;(4) Fix one bundle to the lateral cuneus and the other bundle to the peroneus brevis. This kind of operation not only strengthens the strength of the dorsalis extension but also strengthens the strength of the valgus and has an obvious effect on the orthosis of cavovarus deformity. However, tendon transfer is often difficult to predict and is usually performed in conjunction with osteotomy surgery to achieve the desired outcome.
4.3.3. Osteotomy Treatment
A combined osteotomy is needed to achieve clinical efficacy when soft tissue surgery fails to achieve an orthotic effect. The osteotomy, should be as close as possible to the apex of the deformity in order to achieve a good orthopedic effect. The apex of the deformity should be determined based on an objective preoperative examination, which can be located at the proximal end of the first metatarsal bone, the first metatarsal cuneus joint, the medial cuneus joint, the navicular cuneiform joint., etc. [
19]. The metatarsal side wedge osteotomy of the first metatarsal bone can correct the metatarsal flexion deformity of the first metatarsal bone. However, for most children with cavovarus feet, it is far from the apex of the deformity and only applies to the cavovarus foot to a very light degree. After the open osteotomy of the medial wedge bone, it is close to the apex of the deformity, the metatarsal flexion deformity of the first metatarsal bone is corrected, and the joint of the foot is preserved, and the sagittal deformity of the cavovarus foot can be corrected. Combined cuboid osteotomy for correcting forefoot adduction is suitable for treating light and medium-sized cavovarus, especially for cavovarus caused by metatarsal flexion of the first metatarsal bone. Mubarak performed extra-articular osteotomies on 13 cases and 20 feet of children with high-arched foot deformity. This consisted of the dorsal closure of the proximal first metatarsal wedge osteotomy, the open wedge osteotomy of the medial cuneiform metatarsal, the closed wedge osteotomy of the dice bone, and, if necessary, additional first to third metatarsal osteotomy. An impressive 85 percent of patients were still being followed up after an average of 49 months [
9]. Krhenbühl et al. used the first metatarsal wedge osteotomy combined with soft tissue release to treat children with cavovarus foot deformity, and the postoperative excellent and good rate was 88%, and the follow-up found that children could obtain a good distribution of plantar pressure [
17].In this study, the average follow-up time was 30 months. The postoperative excellent and good rate of the first plantar osteotomy group was 87%, which was similar to the results of the previous study, indicating that the first plantar osteotomy can achieve a good therapeutic effect for the light and medium-sized cavovarus with the apex of the deformity located at the medial cuneus or navicular cuneiform joint. However, the first metatarsal osteotomy is a single-plane deformity orthosis, which corrects more sagittal deformity and can not achieve a good orthopedic effect for severe cavovarus foot deformity with multiple planes.
Japas osteotomy of the middle foot preserves the ankle joint activity and sacrifices the intertarsal joint but does not remove the bone block and preserves the integrity of the foot. In addition, the osteotomy is closer to or even at the apex of the deformity, which can most effectively repair the deformity of the high arcs. Moreover, the middle foot osteotomy can correct the deformity of each plane, which has more advantages than the first sequence osteotomy.
Japas [
10] described in 1968 the treatment of the “V” -shaped osteotomy of the tarsal bone in the middle foot, which could correct the deformity on all sides without removing bone or bone grafting. However, according to the research results, the effect of correcting the rotary deformity was limited.
However, the study's results showed limited success in correcting the rotational deformity.
Chatterjee reported [
11] that Japas osteotomy was used to treat 18 children with neuromuscular hyper arches. The mean follow-up time was 5.4 years, with an excellent and good rate of 77%. This paper adopted Japas middle foot "V" osteotomy for tarsal bone osteotomy. The patients in this group were followed up for 30 months, and the postoperative excellent and good rate reached 93%, which was higher than that of Chatterjee, which may be because the follow-up time was not long enough in this study. For children with a neuromuscular origin, further extension of follow-up time is needed to support the results of this study. Although there is no statistical difference between the postoperative effects of the first metatarsal osteotomy and the Japas osteotomy of the middle foot, the latter is more traumatic than the former and results in the loss of the intertarsal joint of the middle foot.
In contrast, the former is the standard treatment for mild, moderate, and severe arcuate foot deformity with the apex at the medial cuneus or navicular cuneiform joint. The advantage of Japas osteotomy of the middle foot lies in that it can correct various planar deformities. These aspects have obvious advantages over the first plantar-sequence osteotomy for severe hyper arch deformity and hyper arch deformity with a more posterior apex.
The intraoperative blood loss and operation time of the first metatarsal osteotomy and Japas osteotomy of the middle foot were 40.5±10.5 ml and 60.2±12.3ml, respectively, indicating that the intraoperative blood loss of the first metatarsal osteotomy was less than that of Japas osteotomy of the middle foot. Less traumatic. Regarding the operation time, the operation time of the first metatarsal osteotomy and middle foot osteotomy was 63.3±10.3min and 78.4±13.6min, respectively. The difference was statistically significant, indicating that the operation time cost of the first metatarsal osteotomy was less than that of the middle-foot Japas osteotomy, and the trauma of the first metatarsal osteotomy was less than that of the middle-foot osteotomy. For the orthosis of light and medium-cavovarus foot deformity in this study, there was no significant difference in the medium-term efficacy between the first metatarsal osteotomy and the middle foot osteotomy. However, compared with the operation time and intraoperative blood loss, the first metatarsal osteotomy had an advantage over the middle foot osteotomy, which could achieve the same orthopedic effect with less trauma to the children. Therefore, a first metatarsal osteotomy may be considered for orthopedic treatment of light and medium-cavovarus with the apex of the deformity located at the medial cuneus or navicular cuneiform joint.
4.4. Postoperative Complications
The main complication in the early postoperative period is impaired blood flow to the extremity, especially in children treated with osteotomy. A tourniquet should be applied continuously for less than 1 hour during the operation. If a child is found to have impaired blood flow to the extremity after surgery, The cast should be released immediately and vasodilators administered. In this study, one child in the foot and tarsal osteotomy group presented with impaired blood flow to the extremity. One child in the tarsal osteotomy group in this study had impaired blood flow to the extremity, which improved after the treatment described above. The main long-term complication was the recurrence of the cavovarus deformity. Wicart et al.[
20]treated 26 cases and 36 feet of neuromuscular clubfoot in children by selective metatarsal fascial release, cuneiform metatarsal open osteotomy, and heel osteotomy with a mean follow-up of 6.9 years and a recurrence rate of 23%.
Weiner et al. [
21] followed up 89 patients with 139 rigid cavovarus foot osteotomy for up to 7.6 years, and the recurrence rate was 24%. The author concluded that the main factors for the recurrence of the deformity were age <8 years, serious deformity, insufficient correction of muscle imbalance, and uncorrected posterior foot fixation deformity. He Rongguo et al. [
22] treated 20 feet of 16 children with cavovarus with plantar fascia release combined with tarsal V-osteotomy, among which 3 feet had a recurrence of cavovarus. The author believed that the reason for recurrence might be related to the imbalance of muscle strength of cavovarus and the failure to correct residual posterior foot fixation deformity. In this group, the muscle strength of the children was carefully assessed by imaging and physical examination, and adequate intraoperative adjustments were made. After 30 months of follow-up, the deformity recurred in three children, two in the first metatarsal sequence group and one in the midfoot Japas group.
The first metatarsal osteotomy group may be because, in this study, all children with neuromuscular hyperkyphosis had incomplete or inadequate correction of the intraoperative muscular imbalance. Midfoot The Japas osteotomy corrected the deformity in multiple planes but was less effective in correcting the adductor deformity, which was recurrent in this case. The recurrence of this case was mainly due to inadequate correction of the adductor deformity.
4.4. Limitations and Problems
There are still several things that could be improved in this study. ① In some cases in this study, foot radiographs were not strictly taken in the standing weight-bearing position, and there were certain errors in Angle measurement. ② The number of children was not enough, which limited the extrapolation of results to a certain extent. (3) The follow-up time of the children was not long enough, and the cases included in this study were all neuromuscular children whose deformities were progressing continuously. (4) Even if combined with muscle balance surgery, the existing muscle strength problems could not be changed, and further extension of follow-up time was needed to support the results of this study.
5. Conclusion
There is no significant difference in postoperative efficacy between first metatarsal osteotomy and Japas osteotomy for light and medium-cavovarus foot deformity with the apex of the deformity located at the medial cuneus or navicular cuneiform joint. However, the amount of intraoperative blood loss and operative time of the first metatarsal osteotomy is superior to Japas osteotomy of the middle foot.
Author Contributions
D.T.A.V. did the Writing—original draft preparation, Conceptualization, Writing - review & editing, Data curation and Software, ; Methodology and Data curation; Investigation. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
The authors declare that the research was conducted without any financial or commercial support, so there cannot be a potential conflict of interest.
Data Availability Statement
The data that support this study’s findings are available in this article.
Acknowledgments
This work would not have been possible without the support of all my colleagues has supported my career goals and worked actively to provide me with academic knowledge and time to pursue those goals. I extend my gratitude to everyone who helped me during this project. thank my university for its support.
Conflicts of Interest
There is no conflict of interest.
Abbreviations:
| CMT |
Charcot-Marie-Tooth disease |
| MJO |
Midfoot Japas osteotomy |
| FRO |
First ray osteotomy |
References
- Wicart, P. Cavus foot from neonates to adolescents. Orthop Traumatol Surg Res 2012; 98(7):813-28. [CrossRef]
- Ghanem I, Zeller R, Seringe R. The foot in hereditary motor and sensory neuropathies in children. Rev Chir Orthop Reparatrice Appar Mot 1996; 82(2):152 -60.
- Laura M, Singh D, Ramdharry G, et al. Prevalence and orthopedic management of foot and ankle deformities in Charcot-Marie-Tooth disease. Muscle Nerve 2018; 57(2):255-9. [CrossRef]
- Lin T, Gibbons P, Mudge A. Surgical outcomes of cavovarus foot deformity in children with Charcot-Marie-Tooth disease. J Neuromuscul Disord; 2019,29(6 ):427-436. [CrossRef]
- Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop Relat Res 1977; (123):60-2. [CrossRef]
- Harrasser N, Lenze F. Cavovarus foot.[J]. Orthopade.2021,50(1):75-85. [CrossRef]
- Akoh CC; Phisitkul P; Clinical Examination and Radiographic Assessment of the Cavus Foot. [J]. Foot Ankle Clin. 2019, 24(2):183-193. [CrossRef]
- Ziebarth, K; Krause, F; Updates in Pediatric Cavovarus Deformity. [J]. Foot Ankle Clin. 2019, 24(2):205-217. [CrossRef]
- Mubarak SJ, Van Valin SE. Osteotomies of the foot for cavus deformities in children. J Pediatr Orthop 2009; 29(3):294-9. [CrossRef]
- Japas, LM. Surgical treatment of pes cavus by tarsal V osteotomy: Preliminary Report. J Bone Joint Surg Am 1968. p. 50. [CrossRef]
- Chatterjee, P; Sahu, MK; A prospective study of Japas' osteotomy in paralytic pes cavus deformity in adolescent feet. [J]. Indian J Orthop. 2009, 43(3):281-5. [CrossRef]
- d'Astorg H, Rampal V, Seringe R, et al. Is non-operative management of childhood neurologic cavovarus foot effective? Orthop Traumatol Surg Res 2016; 102(8):1087-91. [CrossRef]
- Watanabe, K. Treatment for patients with Charcot-Marie-Tooth disease: orthopaedic aspects. Brain Nerve 2016; 68(1):51-7.
- Zhou Y, Zhou B, Liu J, et al. A prospective study of midfoot osteotomy combined with adjacent joint sparing internal fixation in treatment of rigid pes J Orthop Surg Res 2014; 9:44. [CrossRef]
- Pin T, Dyke P, Chan M. The effectiveness of passive stretching in children with cerebral palsy. Dev Med Child Neurol 2006; 48(10):855-62. [CrossRef]
- Maas J, Dallmeijer A, Huijing P, et al. A randomized controlled trial studying the efficacy and tolerance of a knee-ankle-foot orthosis used to prevent equinus in children with spastic cerebral palsy. Clin Rehabil 2014; 28(10):1025-38. [CrossRef]
- Krhenbühl N, Weinberg MW. Anatomy and Biomechanics of Cavovarus Deformity.J Foot Ankle Clin.2019,24(2):173-181. [CrossRef]
- Ziebarth, K; Krause, F; Updates in Pediatric Cavovarus Deformity. [J]. Foot Ankle Clin. 2019, 24(2):205-217. [CrossRef]
- Weiner, DS; Jones, K; Jonah, D; et al. Management of the rigid cavus foot in children and adolescents. [J]. Foot Ankle Clin. 2013, 18(4):727-41. [CrossRef]
- Wicart P, Seringe R. Plantar opening-wedge osteotomy of cuneiform bones combined with selective plantar release and Dwyer osteotomy for pes cavovarus J Pediatr Orthop 2006; 26(1):100-8. [CrossRef]
- Weiner, DS; Morscher, M; Junko, JT; et al. The Akron dome midfoot osteotomy as a salvage procedure for the treatment of rigid pes cavus: a retrospective review. [J]. J Pediatr Orthop. 2008, 28(1):68-80. [CrossRef]
- He RG, Xu RJ, Wang Y. Treatment of high arched foot deformity in children with lateral plantar release and V-shaped tarsal osteotomy. Chinese Journal of Pediatric Surgery, 2002, 23(6):534-537.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).