1. Introduction
As of 2020, there are approximately 40 million U.S residents who reside in rural areas making up 14% of the nation’s population [
1,
21]. While the definition of rurality is subject to change depending on the governmental agency, the most generic definition is simply land that has not been defined as urban. A typical rural county contained less than 10% of the population of a typical urban county in 2020—23,000 people compared with 245,000 [
21]. An area’s rurality or urbanicity determines what governmental funding is available to address the needs of the health of those communities.
While there are noticeable geographical and spatial differences between both urban and rural areas, there are also vastly different health outcomes associated with each area. The health of rural Americans has been significantly poorer than their urban counterparts due to various factors such as geographic isolation, lower socioeconomic status, poor health literacy, and broadband internet access for decades [
1].
While the recent expansion of Medicaid through the Affordable Care Act (ACA) has addressed some of the barriers rural Americans face regarding access to healthcare, it comes at a large cost for taxpayers, more notably those in a higher tax bracket. Overall, Medicare spending grew 3.5% to
$829.5 billion in 2020, which is 20% of the total nation health expenditure (NHE) [
2]. Medicaid spending grew 9.2% to
$671.2 billion [
2]. Although several states implemented the ACA Medicaid expansion, as of April 2017, 19 states have not yet adopted the Medicaid expansion to low-income adults [
3]. These non-expansion states are home to 59% of nonelderly uninsured individuals living in rural areas [
3]. In states where the expansion occurred, approximately two thirds of rural Americans do not meet the tight requirements to receive care under the ACA and are more likely to fall under the “coverage gap” than their urban counterparts. Likewise, rural residents pay more for their premiums in the insurance marketplace than their urban counterparts leading to larger out-of-pocket healthcare cost [
4]. Paying higher premiums may not be feasible in these communities who are generally poorer than urban areas. In return, rural Americans may not address their healthcare needs which can potentially lead to the progression of disease. As of 2016, the total cost of chronic disease in America is 1.1 trillion dollars [
5]. Combined, direct health care expenditures and the costs of lost productivity due to chronic diseases impose a significant economic burden on individuals, families, employers, and governments across the U.S [
5].
While historic policies such as the Hill-Burton Act, National Health Service Corps and resources such as federally qualified health centers and rural health clinics have improved health inequities existing in rural America, the impact of disease and disasters on rural health, such as the COVID-19 pandemic, are not well understood [
1]. Rural populations have limited access to primary care physicians in comparison to residents of urban areas, and are generally older, sicker, and poorer than their urban counterparts. Limited access to physicians and lower socioeconomic status may result in individuals not accessing healthcare to address any acute health concerns or chronic disease that may exist, which in return leads to poorer health outcomes. Consequently, the health disparities within rural populations continue to grow, widening the gap in overall health outcomes between rural and urban communities. The following key indicators were selected to examine the multi-factorial challenges to healthcare in rural communities.
Geographic Isolation
Geographic isolation can cause a significant burden to rural Americans due to travel time, cost, and time away from the workplace to seek medical treatment. For example, among the 25% of rural Americans whose travel time is the longest, it takes an average of 34 minutes to get to the nearest acute care facility while it only takes 19 minutes for their urban counterparts [
6]. While urban areas tend to have public transportation, such services are limited in rural communities. Rural populations are composed of older individuals who are subject to chronic diseases. As a result, older residents tend to require frequent outpatient appointments which may be difficult. A study completed by Chapman et al identified common themes surrounding missed doctor’s appointments as seen in rural communities, specifically those living below the poverty line. One major theme was difficulty with securing reliable transportation to and from doctor’s appointments. Respondents also reported that not having a car or not having the time to ride the bus was a major barrier to their attendance. Because of the distance between their homes and the clinic, it was noted that cost, time, and safety was of concern [
7]. In areas where medical transportation was available, it posed additional challenges by requiring individuals to request their services 24 hours prior to their clinic visit [
7].
Socioeconomic Status
Between 2000–2017, poverty rates declined across the United States, but urban poverty rates declined at a higher rate than in rural areas [
8]. In addition, the elderly and children poverty rates are higher among rural minority populations, especially in the rural Southeast and along the border. The distressed regions of poverty include Appalachia, the Mississippi Delta, Native American tribal lands, the borderlands between the United States and Mexico, and highly racially segregated urban areas including mostly black metro areas adjacent to the Great Lakes and in the Northeast [
9]. Rural African American residents had the highest incidence of poverty in 2019 at 30.7 percent, compared with 20.4 percent for that demographic group in urban areas [
8]. Rural American Indians or Alaska Natives had the second highest rate at 29.6 percent, compared with 19.4 percent in urban areas [
8]. The poverty rate for white residents was 13.3 percent in rural areas and 9.7 percent in urban settings [
8].
On average, per capita income in rural areas is
$9,242, which is lower than the average per capita income in the United States [
1]. In 2021, approximately 14% of adults, aged 18–64, who resided in rural areas were uninsured compared to 10% of their urban counterparts. Approximately 6% of children residing in rural areas were uninsured in comparison to only 4% in urban areas [
1]. In a 2016 issue brief from the Office of the Assistant Secretary for Planning and Evaluation, Impact of the Affordable Care Act Coverage Expansion on Rural and Urban Populations, found that 26.5% of uninsured rural residents delayed receiving healthcare in the past year due to cost. Rural Americans are more likely to rely on government assistance such as the Supplemental Nutrition Assistance Program (SNAP), Medicaid, and Medicare. Nearly 86% of eligible rural residents receive SNAP benefits compared to nearly 73% of eligible urban residents [
10]. Approximately 25% of rural Americans receive Medicaid while 22% are both dual enrolled in Medicaid and Medicare [
11].
Health Literacy
Health literacy plays a large role in an individual’s ability to understand and utilize health information [
12,
13]. Access to and the use of health information has shown to help individuals improve their knowledge, reduce health care expenditures, increase the use of health services, and improve the health and quality of life overall [
14,
15]. Access to health information can lead to increased health checkups, smoking cessation, decrease alcohol consumption, increase levels of exercise, and better-self rated health reports [
16]. Historically, rural communities have poorer health literacy levels than their urban counterparts [
1]. Lower health literacy can result in patients being reluctant to seek medical treatment since they cannot fully comprehend enough medical jargon to effectively communicate with their practitioner. Their ability to navigate the healthcare system and to find appropriate practitioners, subspecialists, and community health resources is limited, therefore can lead to poorer health outcomes [
1].
Broadband Access
Broadband access has posed as a significant challenge in utilizing methods such as telehealth in rural communities. Compared to their urban counterparts, rural individuals are nearly twice as likely to lack broadband access. In 287 of the nation’s most rural counties less than 70% of households had high-speed internet access [
17]. These areas include parts of Appalachia, the southeast (including the Mississippi Delta), the southwest (including American Indian reservations in Arizona and New Mexico), the northern Great Plains, and Alaska [
17]. Similar results were found in the Zahnd et al study, however, isolated rural areas with large African American and American Indian/Alaska Native populations were seen to have the greatest disparity compared to other ethnicities [
18]. Affordability of broadband services also poses a challenge to rural Americans. Reddick et al determined that there are five factors that influence the affordability of broadband access: geographical disparities, competition, profit-based discrimination, technology and deployment cost, and socioeconomic factors [
19]. In areas where broadband internet was available the monthly cost was significantly higher because building telecommunication networks in those areas is more costly. Services were also more costly simply because there was no competition due to a lack of providers in those areas. Providers often choose not to offer services in areas where the anticipated profit margins are too low [
20]. Lastly, lower income individuals participated in adopting broadband services, however, they would sometimes discontinue those services for financial or other reasons [
19]. Lack of broadband access poses a significant challenge for offering telemedicine services to these communities which again contributes to the ever-present health disparities that they face.
Mental Health
Access to mental health services is a significant challenge for rural communities nationwide. Roughly 15 million rural Americans struggle with substance dependence, mental illness, and medical-psychiatric comorbid conditions [
21]. The suicide rate in rural communities is approximately 18.9 deaths per 100,000 people compared to 13.2 deaths in urban counties [
1]. This difference in suicide rates between rural and urban areas has widened between 1999-2019, increasing by 50% in rural areas compared to 31% in their urban counterparts [
1]. Moreover, rural counties have seen a significant decline in mental health services and providers in recent years. Some examples of mental health services include counseling, recovery programs, medication, support groups, and inpatient and outpatient mental health treatments. A significant issue resulting from the shortage of mental health providers is that 60% of mental healthcare has been taken on by primary physicians instead of specialized professionals [
1]. Among 1,253 smaller rural counties with populations of 2,500 to 20,000, nearly three fourths of these rural counties lack a psychiatrist while 95% lack a child psychiatrist [
22]. The desire to seek mental health help has also been a challenge. The stigma and lack of anonymity in utilizing such services in these small communities can discourage individuals from obtaining services [
1]. Lastly, the affordability of such services remains one of the most significant barriers. Because most rural Americans lack or have limited health insurance, obtaining needed mental health resources becomes an out-of-pocket cost in communities that are typically poorer or have lower income [
1]. A study completed by Brenes et al. found that 58.4% of older Americans between the ages of 60-84 years old felt that cost was a significant barrier to receiving mental health treatment [
23]. For services such as therapy, out-of-pocket expenses can range anywhere between
$65-250 per hour which is a significant burden to those with a low income [
24]. Limited mental health services, physician shortages, and cost are significant barriers to receiving adequate mental health care, most notable in rural communities.
Substance Use
Substance use is a key indicator in determining the general physical, mental, and emotional health of a community. In 2014, substance use disorder treatment admission data showed the most common abused substances in rural communities was marijuana, alcohol, stimulants, and opiates [
1]. Differences between rural and urban illicit drug use varies by age and drug [
25]. In 2018, the National Survey on Drug Use and Health (NSDUH) found that young adults between the ages of 18-25 who lived in rural areas were almost twice as likely to use methamphetamines than their urban counterparts [
1]. Rural areas have been the site of production and distribution of methamphetamine due to the availability of ingredients, including agricultural fertilizer, distressed economic conditions and isolation [
26]. Rural youth between the ages of 12–17 years old were twice as likely to engage in alcohol and binge drinking in comparison to their urban counterparts [
25]. Although there has been a drastic decrease in the production of methamphetamines, recent reports indicate that cheaper and purer sources of methamphetamine from outside of the U.S. are contributing to a resurgence of use in rural areas. In the wake of the opioid epidemic, it was also reported that rural counties exhibited a higher rate of natural and semisynthetic opioid overdoses than urban counties especially in areas such as West Virginia and Kentucky [
1]. Those most susceptible to opiate use was those between the ages of 12–29, those with lower educational attainment, lower income, and those uninsured [
1]. Access to substance use treatment centers is also limited in rural areas. A study completed by Bond et al. found that rural centers had less access to highly educated counselors, were more likely to be nonprofit and funded by the public, offered fewer services such as pharmacotherapy and psychosocial therapy, and had less diverse specialized treatment options [
27]. In addition to limited providers and resources, there is a scarcity of methadone clinics in rural areas which results in a gap in effective treatment and low-cost medication for the treatment of opioid use disorders [
28]. There is a strong need to address not only the physician and substance abuse and resource shortage, but the stressors that may lead to higher rates of substance abuse in rural communities.
Chronic Diseases
Rural communities tend to have significantly higher rates of chronic diseases in comparison to their urban counterparts due to several factors. Examples of chronic disease are hypercholesterinemia, hypertension, arthritis, depressive disorder, asthma, diabetes, chronic obstructive pulmonary disease (COPD), and heart disease [
1]. In 2016, 22.6% of rural Americans had 2–3 chronic conditions in comparison to only 18.9% in urban communities [
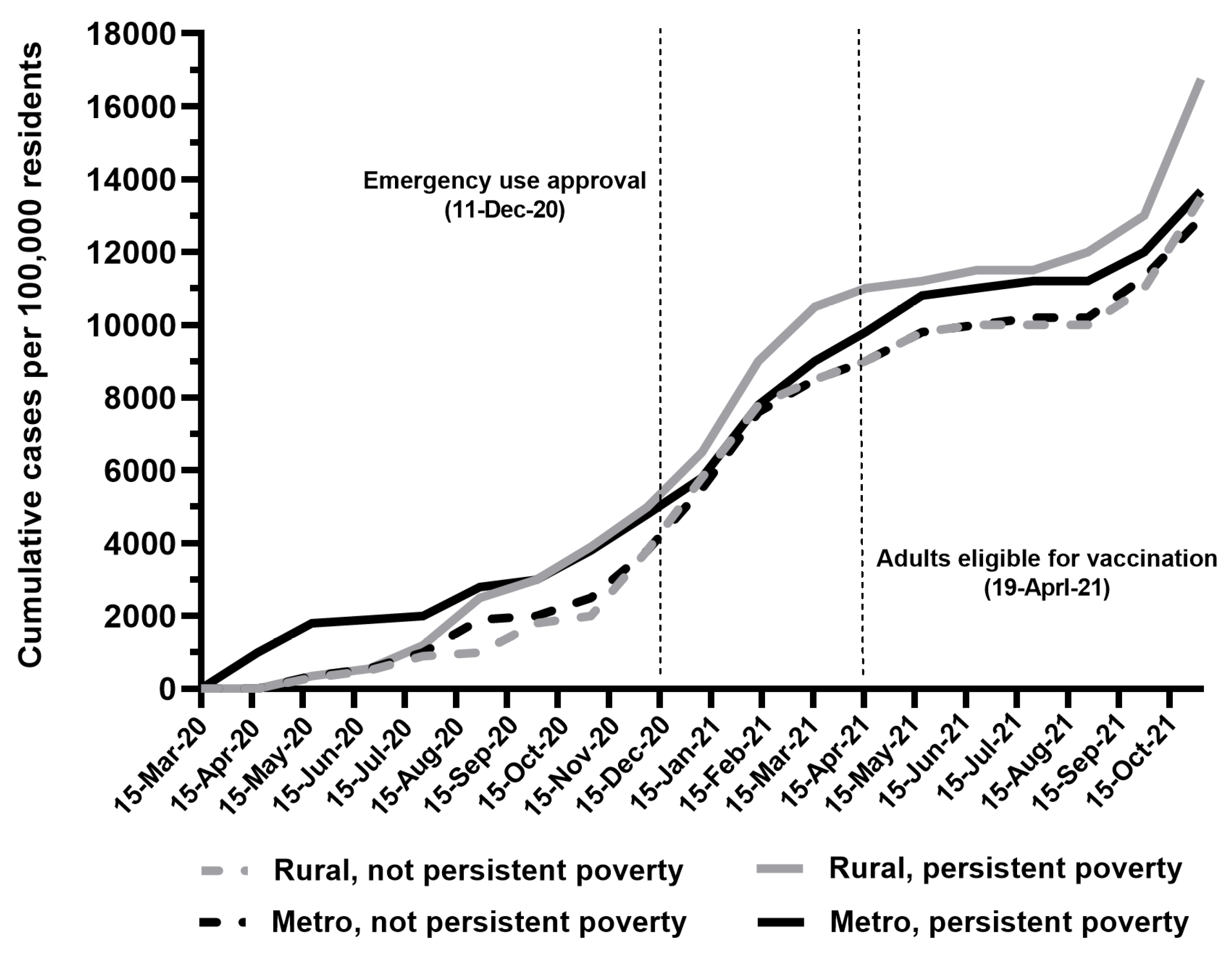
1]. As individuals age, their risk of chronic disease increases which makes chronic disease more prevalent in rural communities where 20% of the population is 65 years or older. Between 1999–2017, the leading causes of death in America was cancer, heart disease, chronic lower respiratory disease, stroke, and unintentional injury [
1]. Every year, the rates for each leading cause have been significantly higher in rural areas in comparison to urban areas. An increase in rates can be seen when accounting for a potential excess of death in rural and urban communities meaning death from potentially preventable conditions. In 2017, the percentages of deaths that were potentially excess from the five leading causes of death in rural counties were 64.1% for unintentional injury, 57.1% for chronic lower respiratory disease (CLRD), 44.9% for heart disease, 21.7% for cancer, and 37.8% for stroke [
29].
Regarding health behaviors, rural Americans tend to have higher rates of obesity, smoking, and are less like to engage in exercise. Although rural America makes up only a fraction of America's total population, it has been estimated that the prevalence of obesity is approximately 6.2 times higher than in urban America [
30]. Obesity has been identified as a significant risk factor for cardiovascular issues, cancer, and type 2 diabetes. Research has shown that low income and lack of resources to aid in weight reduction predispose rural Americans to obesity which places them at a higher risk of developing chronic disease [
30].
Rural communities have a higher rate of smoking than their urban counterparts due to demographic and psychosocial factors such as lower socioeconomic status, lower educational attainment, and higher unemployment rates [
31]. Tobacco crops are a source of income in many rural areas which further normalizes the use of tobacco [
31]. Tobacco use has been shown to increase the risk of chronic diseases such as heart and pulmonary disease as seen by the heart rates of both diseases in rural communities. Lax tobacco control and regulatory policies accompanied with the need for interventions centered around smoking cessation further widens the disparity gap between rural and urban communities [
32].
Sedentary lifestyles have shown to increase the risk of comorbidities such as diabetes and heart disease. Rural Americans are less likely to meet federal physical activity guidelines than their urban counterparts with the lowest rates affected the South [
33]. Geographic isolation and/or terrain has shown to decrease access to health-promoting resources. Research has shown associations between features of the environment that support active living (ex: streetlights, paths, access to recreational facilities, aesthetics) and physical activity based on the rurality or urbanicity of the community [
33]. Rural areas were shown to have less supportive physical activity environments that their urban counterparts [
33]. Kegler et al.’s findings indicate that main street investment increasing walkability (e.g., sidewalks, lighting, aesthetics, destinations) and other efforts to improve access to physical opportunities can increase leisure-time physical activity in rural communities, especially for lower-income households [
33].
COVID-19 in Rural Communities
The introduction of severe acute respiratory syndrome coronavirus-2 also known as COVID-19 affected population health in general; however, through this systematic literature review, we hypothesize that the pandemic further exacerbated pre-existing socioeconomic and health outcomes in rural communities. The current study examines the impact of COVID-19 on preexisting rural health disparities using the key indicators previously described while examining all new relevant challenges to rural health. Secondarily, the current study examines the efficacy of rural health resources available to these communities.
2. Materials and Methods
This umbrella review followed the Preferred Reporting Items for Systematic Reviews guidelines. The included articles were searched on the electronic databases, PubMed, Web of Science, Scopus, USDA, Economic Research Service, Johns Hopkins University Center for system Science and Engineering, U.S. Department of Commerce, Bureau of Census, Current Population Survey, and annual American Community Survey estimates. Systematic review was included if published between the 1st of January 1998 and to the 30th of December 2022. Different key words and phrases were adopted: “COVID-19”, “Rural”, “Preventative Measures”, “heart disease”, “Diabetes”, “Substance Abuse Use”, “Access to Healthcare”, “Telehealth”, “Mental Health” and “Vaccines”. The keywords were matched through the Boolean operators AND or OR in the databases. Information related to the first author and year of publication, the objective of the study, the conclusion of the study, population screened, and main results were stored. A description and narrative synthesis was adopted to describe the results.
3. Results
Rural Health:
Rural health is defined as the general health of those living in rural areas. While rurality has been subject to many vague definitions, the U.S. Census Bureau, the Office of Management and Budget, and the Economic Research Service of the U.S. Department of Agriculture define rural health as everything that is not considered urban [
1]. Rural Health introduces a keen set of challenges, most notably, often affecting the population's overall health and health outcomes. Due to a multitude of risk factors such as geographic isolation, lack of access to healthcare, lower socioeconomic status, and limited job opportunities, rural populations are subjected to lower health outcomes in comparison to their urban counterparts [
34]. Rural communities tend to be older with more than 8 million people who are 65 years of age or older [
35]. These populations are at a greater risk of dying from cancer, heart disease, accidental injury, chronic lower respiratory disease, and stroke [
34,
36]. Rurality accompanied by pre-existing comorbidities appears to significantly lower the health outcomes of rural Americans.
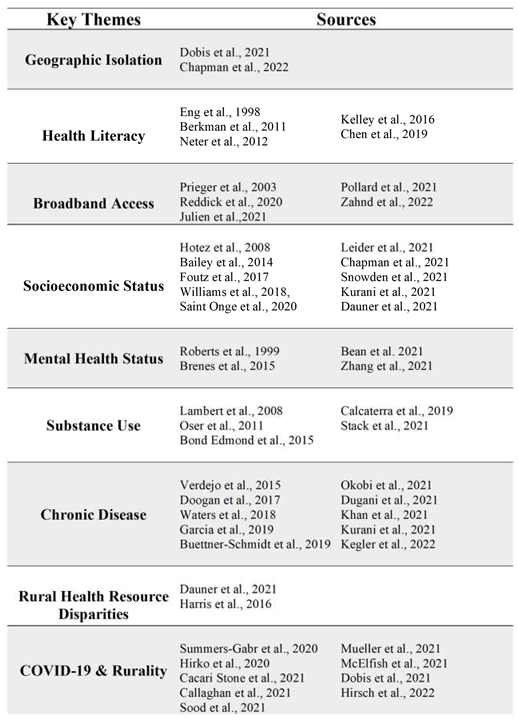
COVID-19 Pandemic
As the COVID-19 pandemic continues to disrupt regional, national, and world-wide health infrastructure with the introduction of new variants, vulnerable populations continue to be subjected to worsening health disparities. As the pandemic evolved, indicators of social and economic well-being such as poverty rates were strong predictors of high COVID-19 case and mortality rates at the county level. During the second surge in July and August 2020, the pandemic spread to rural areas, with persistently poor rural counties leading weekly rates of new infections and gradually closing in on the cumulative case rate in persistently poor urban counties [
6]. Starting in late September 2020, rural and persistently poor counties led the nation in cumulative cases per 100,000 residents [
6] (
Figure 1).
The COVID-19 pandemic exacerbated the disparities affecting minorities such as African Americans, Native Americans, and Hispanics. In comparison to the 1918 Spanish Flu and 2009 H1N1 Influenza A flu epidemic, COVID-19 has proven no different with its high rate of susceptibility particularly in the African American communities [
37]. For instance, in Louisiana, 72% of COVID-related deaths were African Americans although they only make up 32% of the population. According to the 2020 surveillance data taken from the CDC, African Americans, represent approximately 13.4% of the total US population and contributed to 18.2% of COVID-related cases. African Americans contributed to 20.9% of COVID-related deaths. They are also 3.4 times more likely to become ill with COVID in comparison to their white counterparts [
38].
The pandemic also exposed the lack of preparedness of rural areas, as rural communities were not equipped for managing large-scale public health crises. Since the 2008 recession, rural areas have yet to see economic recovery, workforce investment, or public sector investment which further sets them apart from their urban counterparts [
39]. Smaller budgets have led to the dismantling of smaller rural healthcare facilities. Rural hospitals made up 59% of U.S. community-based hospitals that closed between 2015-2019 [
35]. COVID-19 further unveiled the lack of infectious disease specialists, lack of access to larger medical centers with substantial numbers of ICU beds and ventilators, and an overall lack of preparedness [
11]. Although rural and urban areas have a similar number of beds per capita, rural areas have significantly less ICU beds. In total, there are approximately ten times as many ICU beds located in urban areas (77,642) compared to rural areas (7,605) [
6]. In 2019, approximately 49% of U.S. rural community hospitals had 25 or less beds available in their facilities while only 16% had 100 or more [
35]. Rural residents were also shown to be less likely to take COVID-19 preventative measures, further exacerbating the transmission of the virus and overwhelming the ill-prepared hospitals [
36]. The pandemic has further highlighted the need for adequate funding for rural health institutions to increase their level of functionality and preparedness.
Rural Health Communities and COVID-19 Preventative Measures
In the wake of the pandemic, the CDC issued several guidelines and mandates to limit the transmission of COVID-19. Preventative measures such as wearing a mask, standing six feet apart, limiting time spent in public areas, and washing hand regularly was highly encouraged. To better understand the differences in compliance within rural and urban populations, Callaghan et al issued a survey to 5009 U.S. adults to assess their participation in preventative measures. In comparison to their urban counterparts, rural Americans were 49% less likely to wear a mask [
36]. Rural Americans were 49% less likely to work from home, 29% less likely to sanitize their homes or workspaces, and 27% less likely to avoid dining at restaurants and bars [
36]. Rural Americans were also 17% less likely to change their travel plans in the wake of COVID-19 [
36]. Based on these data, it is plausible that rural Americans are at a greater risk of contracting the virus, thus increasing the incidence rate in these communities. Given the limited access to healthcare and struggling healthcare infrastructure, these risky behaviors can again exacerbate the health outcomes of rural communities.
Rural Health Comorbidities and Their Challenges
Diabetes
Over time, rural disparities in diabetes-related mortality have continued to grow. A nationwide inpatient sample taken between 2009–2015 showed 29% higher odds of mortality in rural versus nonrural counties within the South, Midwest, and West [
40]. While the association between geographic location and likelihood of diabetes-related mortality is poorly understood, there are some factors that may contribute to ongoing disparities afflicting rural communities specifically. In 2013, comprehensive data from the CDC showed that the prevalence of five optimal lifestyle factors (sufficient sleep, nonsmoking, normal body weight, nondrinking/moderate alcohol, and physical activity) were lower in rural communities in comparison to their urban counterparts. National Health Interview Survey results in conjunction with a 2016 Behavioral Risk Factor Surveillance System (BRFSS) report indicated a higher frequency of comorbidities such as obesity and limited physical activity in rural areas in comparison to their urban counterparts. Notably, these five factors are linked to a higher risk of Type 2 Diabetes Mellitus [
40].
Management of diabetes also plays a significant role in determining the health outcome of a diabetic patient. A study completed by Kurani et al. found that adult patients living in more deprived and rural areas were significantly less likely to receive high-quality diabetes care. Patients living in socioeconomically deprived areas faced multiple obstacles to receiving adequate care such as lack of financial resources, lower health literacy, greater comorbidity burden, and higher food insecurity [
41]. Individuals residing in rural communities were more likely to be unable to afford blood glucose test strips and more likely to not attend screening appointments [
41]. Prior research identified that rural residents had higher rates of being uninsured or underinsured contributing to their inability to afford blood glucose strips and any other diabetes-specific treatment. Rural areas also have significantly less primary care physicians, specialists, and diabetes educators when compared to their urban counterparts [
41].
While COVID-19 and its biological effects on diabetic patients is poorly understood, the pandemic has affected patients in multiple facets. To reduce clinic capacity, many facilities have limited visits to emergencies only. Therefore, a large proportion of diabetic patients were left in a vulnerable state with the inability to get routine checkups and receive necessary treatments [
42]. COVID-19’s complete impact on the diabetic community has yet to be determined; however, it is likely that the overall health of rural diabetics has continued to worsen in comparison to their urban counterparts.
Heart Disease and Heart Failure
In 2017, 44.9% of heart disease deaths among persons aged <80 years in rural counties were potentially excess deaths, compared with 18.5% in urban counties, which had the lowest percentage of deaths that were potentially excess [
29]. A total of 64.1% of deaths among persons aged <80 years from unintentional injury in rural counties were potentially excess deaths, compared with 47.8% in urban counties [
29]. The largest disparity in potentially excess deaths between the most rural and most urban counties was from CLRD, for which 57.1% of deaths were potentially excess in rural counties and 13.0% in large urban counties [
29] (
Figure 2). Risk for severe coronavirus disease 2019 (COVID-19) associated illness (illness requiring hospitalization, intensive care unit [ICU] admission, mechanical ventilation, or resulting in death) increases with increasing age as well as presence of underlying medical conditions that have shown strong and consistent evidence, including cardiovascular disease [
43]. Rural communities are almost twice as likely than their urban counterparts to be hospitalized for potentially preventable chronic diseases, such as chronic heart failure (HF) [
44]. The risk has increased over the last decade despite a decline in the rate of admissions for remote rural areas [
44]. In a study conducted by Manemann et al, rurality was strongly associated with a decreased risk of ED visits and hospitalizations (ED-adjusted HR, 0.89 [95% CI, 0.82–0.97]; hospitalization-adjusted HR, 0.78 [95% CI, 0.73–0.84]). Rural areas also experience higher mortality from ischemic heart disease, heart failure, and stroke and have experienced fewer reductions in age-adjusted mortality rate than their urban counterparts [
45]. Poorer cardiovascular outcomes among rural areas can be contributed to poorer cardiovascular risk factor profile such as obesity, a sedentary lifestyle, and tobacco smoking [
45]. In addition to individual risk factor profiles, the limited resource availability, initial diagnostic delay, suboptimal management, and lack of an integrated clinical information system contribute to the decreased access to healthcare [
45].
Substance Use Disorder
COVID-19 has exacerbated many pre-existing health disparities in rural communities, it has also increased the use of illicit substances. A series of in-depth interviews conducted by Stacke et al. reveals COVID-19’s influence on mental health, variable substance availability, and overdose concerns in five rural counties in Oregon. Many participants who reported only using methamphetamines described a decrease in use due to lack of funds or lack of availability. Some participants saw an increase in drug cost due to their dealer’s knowledge of government-issued stimulus checks being given in the height of the pandemic. Participants who used heroin-only or both heroin and methamphetamines reported an increase in use due to boredom or worry associated with the ongoing pandemic. While most participants expressed a lack of concern regarding overdosing during COVID-19, many admitted to taking preventative measures such as carrying Naloxone in the case of an overdose [
46].
In a study conducted by Bolinski et al., natives of rural Illinois reported an increase of fentanyl use due to the scarcity of heroin during the height of the pandemic. Participants admitted to using drugs more frequently due to the mandated stay-at-home orders and/or job loss. Many individuals experienced significant anxiety and depression due to the unpredictability of the pandemic on their financial situations which further exacerbated their drug use. While alcohol use varies by rurality, rural areas were found to have a higher rate of alcohol use disorders when compared to their urban counterparts although rural individuals were more likely to abstain from alcohol use.
Rural “Mental Health” During The COVID-19 Pandemic
Not only has COVID-19 taken a toll on individuals’ physical wellbeing but their mental health as well. Historically, rural communities have had higher rates of both substance abuse use and mental health issues [
47]. Between 2005-2016, individuals living in rural communities were 1.5 times more likely to attempt suicide than their rural counterparts [
48]. Many factors such as a lack of access to healthcare and a lack of mental health services available contributed significantly [
48]. Rural areas have less psychologists and psychiatrists as well [
47]. In the climate of COVID-19, there has been a notable rise in individuals experiencing anxiety and depression due to physical isolation. The Global Burden of Disease 2020 estimated that the pandemic has led to an additional 53 million and 76 million cases of anxiety and major depressive disorders respectively [
49]. While urban communities have been able to easily utilize telemedicine to connect individuals with mental health providers, rural communities are negatively impacted. The reliance of broadband internet and accessibility to technology in these rural areas has continued to be a challenge. After analyzing ACS estimates from 2014-2018, Zahnd et al found that only 70% of isolated rural areas had broadband access. Areas with high percentages of African American residents had lower broadband access, particularly in isolated rural tracts (54.9%). Decreased access to broadband was spatially clustered in the Southeast, Southwest, and northern plains [
18]. Rural isolation accompanied with the unknowns regarding COVID-19 further exacerbated existing mental health issues and further highlighted the need for better access to care for rural communities.
Access To Rural Health Care During The COVID-19 Pandemic
Geographical
Geographic isolation can be identified as one of rural America’s largest obstacles. While some populations are near large academic centers, most are not. Rural communities must rely on either smaller community hospitals, a critical access hospital (CAH), or low-volume hospitals when seeking medical treatment [
1]. While most of these institutions are required to be within 15-35 miles of each other, in rural communities this geographical space can be a significant long distance in areas where public transportation is limited or unavailable [
1]. Moreover, the COVID-19 pandemic only exacerbated the challenges that rural hospitals faced which has led to more closures due to consolidation, provider shortages, and low patient volume. The patient-to- primary care physician ratio in rural areas is 39.8 physicians per 100,000 people, compared to 53.3 physicians per 100,000 in urban areas [
50]. The low availability of beds in the ICU and decline in critical care specialists in these hospitals forced patients to travel further for COVID-19 treatment. According to the NIHM, in rural areas, there are 1.7 Intensive Care Unit (ICU) beds per 10,000 people in comparison to 2.8 ICU beds in urban areas [
1]. As the challenges surrounding the infrastructure of rural hospitals continue to emerge, COVID-19 continues to increase the burden of depleted communities.
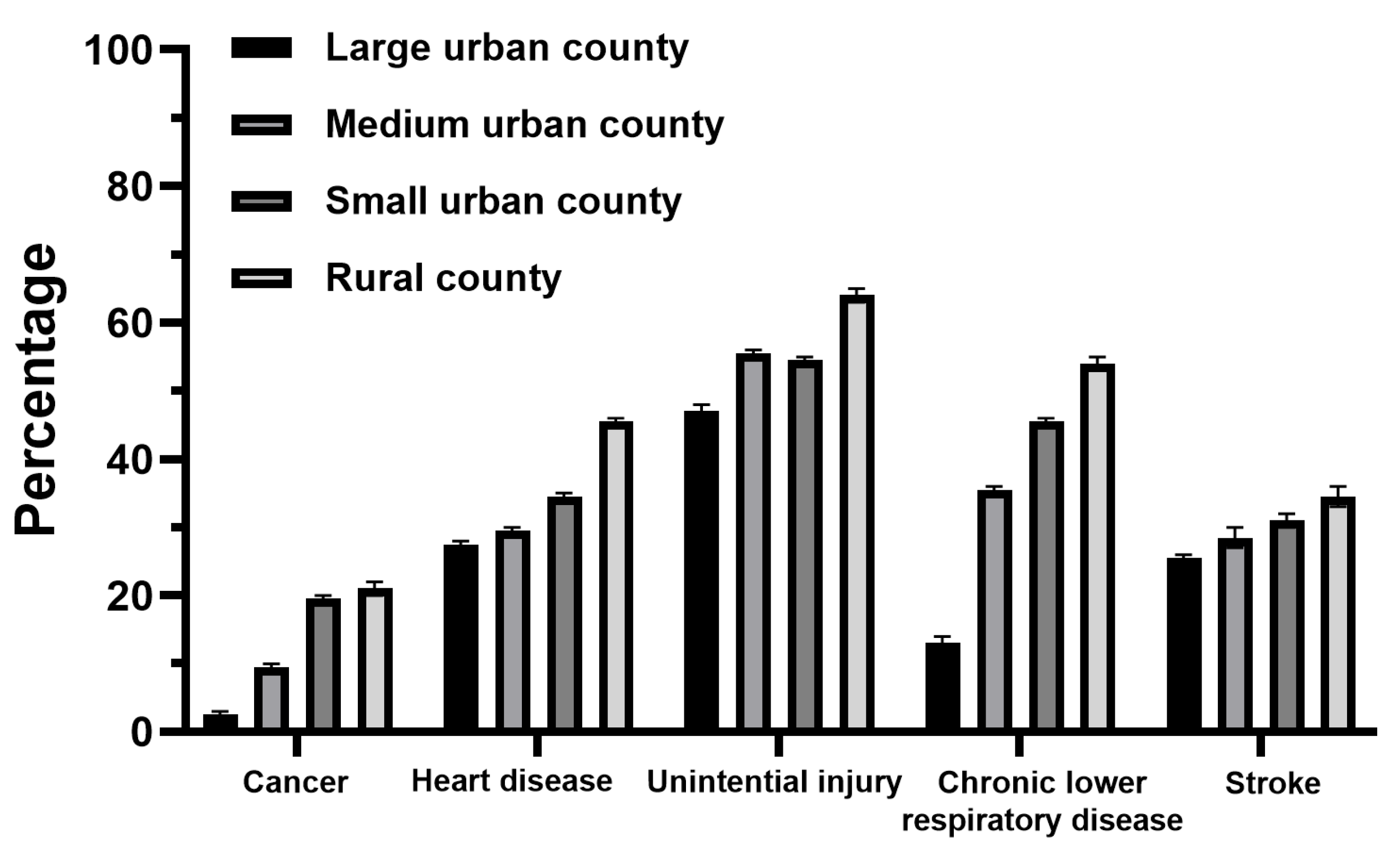
Socioeconomic
The socioeconomic status of rural American puts them at a sizeable disadvantage for affording proper healthcare. According to the most recent estimates from the 2019 American Community Survey (ACS), the rural poverty rate was 15.4 percent in 2019, compared with 11.9 percent for urban areas [
8] (
Figure 3). Statistically, rural areas tend to have a higher percentage of residents who are uninsured, older with co-morbidities, have a lower SES status, and limited access to health care institutions. Due to these factors, this special population is more susceptible to COVID-19 associated morbidity and mortality. Because most rural communities heavily rely on industries that are highly susceptible to pandemic-related closures, such as factory work, tourism, outdoor recreation, rural areas may be particularly more vulnerable to COVID-19−related economic disparities [
51]. Of the rural westerners surveyed by Mueller et. al, approximately 12% were temporarily unemployed due to the pandemic, a 9.74 increase from their normal rate. At the time of the study, the national unemployment rate only increased by 7% between June 2019-2020 [
51]. Of those employed full-time prior to the pandemic, 21% were no longer employed. Of those 21%, a total of 49% were temporarily unemployed and 21% had been converted to part-time. Approximately 72% of participants who were part-time employees prior to the pandemic, no longer were employed by the conclusion of the study. Respondents who were 18-29 years old or had no high school education were also more likely to perform informal work such as “for cash” jobs Approximately 60% of the participates perceived their county as having poor economic health due to the pandemic [
51].
Rural Health Disparities And COVID-19 Vaccines
With the emergence of the rapidly spreading COVID-19 virus, the rollout out of the vaccine has proven to be crucial in combating and controlling the spread world-wide. The push for vaccine acceptance has however highlighted, the underlying distrust that many Americans have with the healthcare system in the United States. Most notably, vaccine hesitancy was shown to be prevalent in minority populations and those with lower socioeconomic status, all commonalties of populations residing in rural America. In a survey completed by McElfish et al, 47% of women, 63% of African Americans, and younger participants reported being less trusting of the vaccine. African Americans were three times as likely to report less confidence than their Caucasian counterparts [
52]. Interestingly, it was determined in the Sun and Monnat 2021 study that lower vaccination numbers in rural areas was attributed to not only lower income but also a larger Trump share vote as well. Ultimately, while people of color, lower educational status, and lower income make up the vast majority of those who are disproportionately affected, the addition of vaccine distrust and hesitancy further widens the gap in health disparities.
Telehealth Response and the COVID-19 Pandemic
In the wake of nationwide stay-at-home orders and curfews, many health systems began to transition to utilizing telemedicine for patient visits. Telemedicine offers two options: audio-only and audio-visual visits. Audio-visual visits allows for the capability to perform visual medication reconciliation, review test results via screenshare capabilities, and perform limited elements of the physical examination such as jugular vein and lower extremity edema assessment [
53]. Videoconferencing can also provider with physician with a new context to the realities of a patient’s living conditions and offer the beginnings of a home safety assessment [
53]. While telemedicine presented itself as a relatively inexpensive and viable opportunity to continue patient care in urban areas, it posed another challenge to rural Americans and created an additional healthcare disparity. Although many rural populations have seen some of the benefits of telemedicine, there is still a significant number of people who do not have access to broadband internet. Approximately 33% of rural Americans do not have access to broadband internet to support telehealth visits [
54]. In addition to broadband access, factors such as affordability of broadband services and devices such as phones, computers, and tablet as well as eHealth literacy are to be considered.
COVID-19 And Health Literacy of Rural Americans
Health literacy has continued to be a concern nationwide since the overall health of the nation is largely dependent on populations’ ability to truly understand health information. While distance and internet access has continued to be a challenge in rural communities, it has additionally made it harder to even find health information in general. According to the Health People initiative, non-healthcare related challenges and social determinants of health such as living in poverty, lack of insurance/adequate coverage, low educational attainment, and limited English proficiency have a significant impact on health literacy [
1].
Approximately, more than half of Americans between the ages of 16 and 74 (54%) read below the equivalent of a sixth-grade level [
55]. These low literacy skills include the ability to recognize phonemics and phonics which is critical for comprehension. In a time where reliance on health information has become all too important, populations with lower literacy levels found it more difficult to understand COVID-19, thus affecting compliance with preventative measures. Given the circumstances, these individuals are more likely to trust word of mouth information or social media claims versus written descriptions or infographics related to the disease.
A study conducted in 2020, determined that of the respondents, 68% of individuals relied solely on Donald Trump or the taskforce for COVID-19 news. Of these respondents, 68% of them reported believing that the pandemic was overhyped [
56]. As expected, individuals were more inclined to not participate in COVID-19 preventative measures.
Rural Health Resource Disparities
Assessing the availability or, lack thereof, of community resources in rural America is pertinent to better understanding the gap in health disparities in rural America comparison to their urban counterparts. It has been well documented that rural local health departments are more reliant on federal, state, and clinical revenues, while urban LHDs have proportionally more access to local revenues [
34]. Much of this can be attributed to struggling rural economies and declining populations that make it difficult to provide tax support for local governmental agencies [
34]. When utilizing the Rural-Urban Commuting Area Code (RUCA), approximately 47% of local health departments (LHDs) are rural and serve 13% of the U.S. population. A typical rural LHD serves approximately 15,000 people and has roughly a
$500,000 annual budget and 9 full-time staff [
57]. Compared with their urban counterparts, smaller, rural jurisdictions have lower compliance rates, are less likely to report using evidence or administrative based decision making, report providing less services, and report using fewer strategies to combat health disparities [
57]. Service types performed less frequently in small, rural jurisdictions were early and periodic screening, diagnostic, and treatment services for infants and children, other maternal and child health functions, access to medical care, access to dental care, and behavioral health services [
57].
A qualitative study conducted by Dauner et al found that community health workers reported areas where resource shortages existed included the need for mental health clinicians; transportation; Internet; long-term care including memory care, respite, personal care services and hospice; specialty care; emergency medical services; public health department staffing; general workforce; and housing, specifically Section 8 housing [
58]. Due to these shortages, their ability to address social determinants of health was very limited [
58]. Resources such as transportation assistance was limited due to a complete lack of staff to assist or the inability for the healthcare worker themselves to participate due to legal hurdles.
Partner capacity appeared to be another challenge when addressing the needs of rural communities. Because social service partners did not have the capacity to take on more work, lower socioeconomic and less densely populated communities were adversely affected [
58]. It was noted that in the wake of COVID-19, while some community partners noticed more engagement between each other, others stated that the pandemic exacerbated their internal issues and they struggled to stay aware of all the resources available between agencies [
58].
Limitations and Future Directions
It was noted that there was an abundance of literature available comparing the effects of COVID-19 in rural and urban communities internationally, but limited research on rural U.S. specifically. An important limitation of this review is the heterogeneity of the included studies. In addition, the incomplete COVID-19 data available for the time frame inclusion criteria is a limitation. Future studies should focus on the longitudinal effects of the pandemic on rural health and disparities on U.S. healthcare.
4. Discussion
Despite the important limitations, these findings suggest that the COVID-19 pandemic has directly and indirectly exacerbated the vulnerabilities that have existed in rural communities for decades. Rural Americans continue to face challenges accessing hospitals and clinics along with outpatient resources, efficiently utilizing telemedicine, partaking in behaviors to prevent or reduce chronic diseases and illnesses, and navigating and understanding the healthcare system in general. The current study shows that within rural communities, individuals who are younger, belong to an underrepresented minority, or have a lower socioeconomic status were most vulnerable to COVID-19.
Specifically, African Americans, Hispanics, and Native Americans contributed to the highest number of COVID-19 cases. African Americans were approximately four times more likely to contract the virus compared to their Caucasian counterparts. This poses the question, “What are the underlying mechanisms within these subsets of communities and why are they most vulnerable in comparison to the population as a whole?” This question may be answered, in part, by analyzing the public’s response to the COVID-19 rollout and their participation in preventative measures such as wearing masks, avoiding public places, working from home, etc. As noted in the McElfish et al study, approximately 63% of African Americans and younger participants reported being less trusting of the vaccine and less confident in its administration. Poorer health outcomes of underrepresented minorities and their lack of trust in the government is recorded across the nation despite urbanicity or rurality. The implementation of interventions targeted towards minorities can help break the chain of generational health disparities that these populations confront. Likewise, ongoing evaluations of new and current interventions is critical for lasting progress.
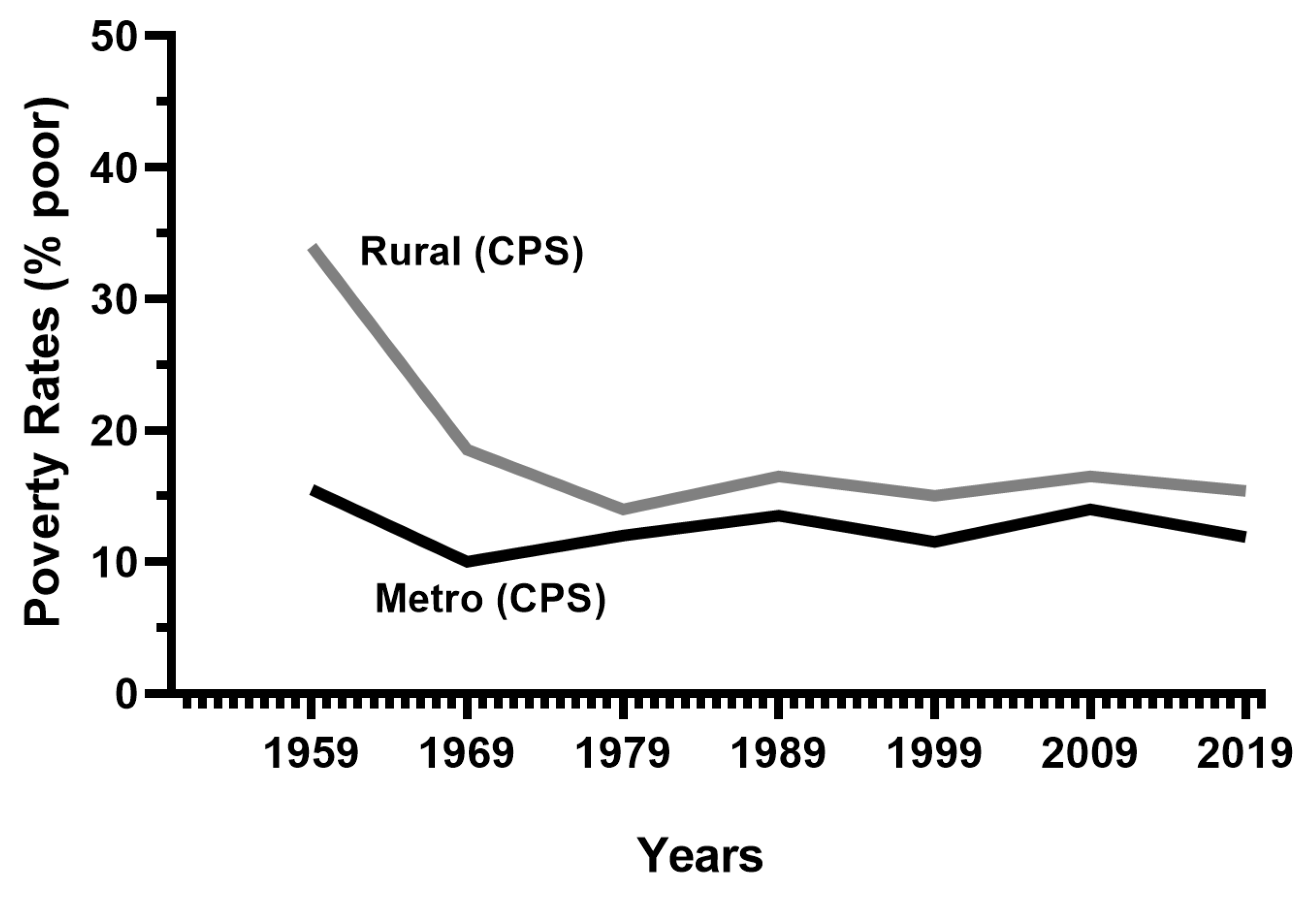
Rural Americans face individual challenges to improve their health outcomes. Similarly, the rural healthcare system, specifically hospitals, require “medical” attention and targeting multifaceted treatment. As a results of COVID-19, rural healthcare systems nationwide were unprepared and unequipped to address a public health crisis of this magnitude. Community health centers or local health departments faced similar challenges as hospitals were limited in the amount of support available to the community, individuals, and families. Under the magnifying lens of the COVID-19 pandemic, the lack of available resources on rural Americans’ healthcare management, mental health status, and substance use continues to be exposed (
Table 1).
Table 1.
Characteristics of the included studies.
Table 1.
Characteristics of the included studies.
Furthermore, chronic illnesses such as heart disease, stroke, diabetes, respiratory diseases, and unintentional injuries are prevalent in rural communities. During the pandemic, many hospitals and clinics operated with limited capacity or closed entirely, while some home health services were suspended. Ultimately, populations who were already in a state of poor health were unable to receive adequate care, leaving rural Americans significantly more vulnerable compared to pre-pandemic conditions. The pandemic provided an opportunity to utilize telemedicine as a safe and reliable method to serve the rural patient population; however, the lack of available broadband internet access, infrastructure, and associated costs exacerbated an already complex challenge.
Substance abuse and mental health issues significantly increased during the pandemic. Individuals who reported abusing illicit drugs prior to the pandemic stated that they had increased their usage during the pandemic due to boredom or worry. Based on the unpredictability of the pandemic, anxiety and depression served as catalysts to substance abuse. A common theme of limited resources being a significant barrier in rural communities also was present regarding substance abuse use and mental health. A lack of psychologists and psychiatrists paired with limited telemedicine opportunities left many of these health concerns unaddressed (
Table 1).
Lastly, the health literacy issues faced by rural communities should not be overlooked when evaluating the effects of the COVID-19 pandemic. Many factors including poverty, lack of insurance coverage, low educational attainment, and limited English proficiency can influence health literacy. The research focus of the COVID-19 pandemic continues to be on the biological effects of the virus, its transmissibility, and the efficacy of the vaccines; however, in rural communities where health literacy is critically low, deciphering health information and understanding basic health implications is a significant challenge and roadblock for improving healthcare disparities. Moreover, the COVID-19 pandemic affirmed the need to improve health literacy, which could increase the likelihood of rural Americans and urban Americans to participate in preventative medicine and vaccinations.
5. Conclusions
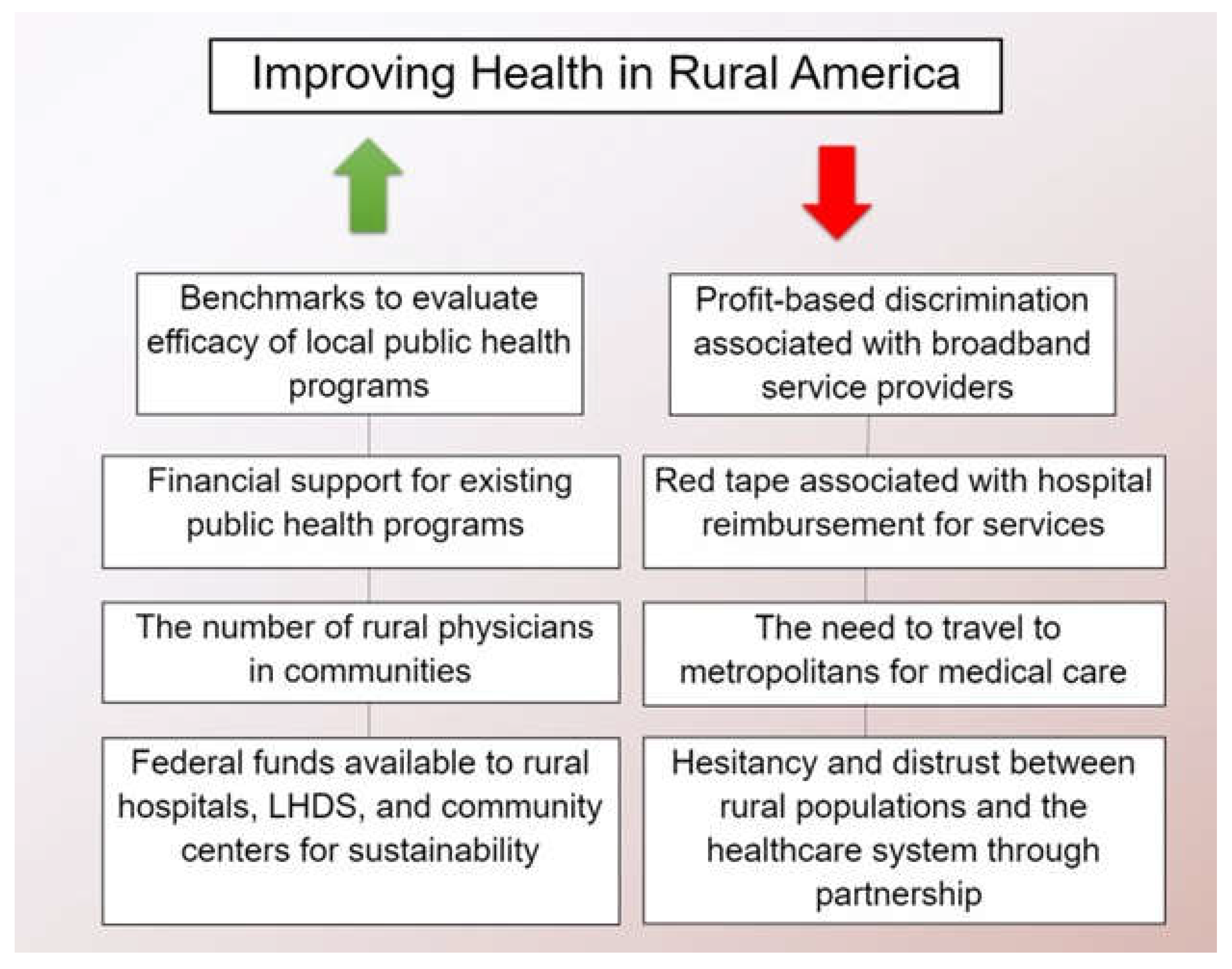
The complexity of rural healthcare in the U.S. is far-reaching. Focused state and federal funding to rural healthcare centers can sustain existing operations and effectively address the dire health needs of rural communities. In addition, addressing the physician and specialist shortage, increasing, and improving access to telemedicine, increasing physical access to healthcare are essential for improving rural health and decreasing overall healthcare costs in the U.S. (
Figure 4). In addition to focused funding, a multi-approach plan of action is essential to ensure ongoing funding and critical resources are available for staff, medical, and mental health professionals for the current pandemic and future public health crises. Frequent evaluation of benchmarks on the local and state level could help determine if programs targeted towards addressing social determinants of health have indeed led to improved health outcomes community wide. The COVID-19 pandemic has, in effect, emphasized the need for urgent change in rural healthcare as a microcosm for addressing loopholes and significant deficiencies for the goal of improving overall health outcomes in the U.S.
Author Contributions
BH provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; BH and VJ drafted the article or revised it critically for important intellectual content; VJ gave final approval of the version of the article to be published; all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hub, T. R. H. Rural Health Disparities. https://www.ruralhealthinfo.org/topics/rural-health-disparities Services, C. f. M. M. National Health Spending in 2020 Increases due to Impact of COVID-19 Pandemic. CMS.gov, 2021.
- Foutz, J. A., S.; Garfield, R. The Role of Medicaid in Rural America; https://www.kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/, 2017.
- Williams, D., Jr.; Holmes, M. Rural Health Care Costs: Are They Higher and Why Might They Differ from Urban Health Care Costs? N C Med J 2018, 79 (1), 51-55. https://doi.org/10.18043/ncm.79.1.51. [CrossRef]
- Waters, H. G., M. The Costs of Chronic Disease in U.S.; Milken Institute, 2018.
- Dobis, E. K., T.; Conley, K.; Sanders, A.; Ortiz, R. Rural America at a Glance: 2021 Edition; US Department of Agriculture, 2021. https://www.ers.usda.gov/webdocs/publications/102576/eib-230.pdf?v=1879.8.
- Chapman, K. A.; Machado, S. S.; van der Merwe, K.; Bryson, A.; Smith, D. Exploring Primary Care Non-Attendance: A Study of Low-Income Patients. Journal of Primary Care & Community Health 2022, 13, 21501319221082352. [CrossRef]
- Rural Poverty & Well-Being. U.S Department of Agriculture.
- Hotez, P.J. Neglected infections of poverty in the United States of America. PLoS Negl Trop Dis 2008, 2(6), e256. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J. Supplemental Nutrition Assistance Program and Rural Households; Center for Rural Affairs, 2014.
- Commission, M. a. C. P. a. A. Medicaid and Rural Health; 2021.
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011, 155(2), 97–107. [Google Scholar] [CrossRef]
- Neter, E.; Brainin, E. eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 2012, 14(1), e19. [Google Scholar] [CrossRef]
- Eng, T. R.; Maxfield, A.; Patrick, K.; Deering, M. J.; Ratzan, S. C.; Gustafson, D. H. Access to health information and support: a public highway or a private road? JAMA 1998, 280(15), 1371–1375. [Google Scholar] [CrossRef]
- Kelley, M. S.; Su, D.; Britigan, D. H. Disparities in Health Information Access: Results of a County-Wide Survey and Implications for Health Communication. Health Commun 2016, 31(5), 575–582. [Google Scholar] [CrossRef]
- Chen, X.; Orom, H.; Hay, J. L.; Waters, E. A.; Schofield, E.; Li, Y.; Kiviniemi, M. T. Differences in Rural and Urban Health Information Access and Use. J Rural Health 2019, 35(3), 405–417. [Google Scholar] [CrossRef] [PubMed]
- Pollard, K. M., M. Digital Divide in High-Speed Internet Access Leaves Rural Areas Behind. 2021.
- Zahnd, W. E.; Bell, N.; Larson, A. E. Geographic, racial/ethnic, and socioeconomic inequities in broadband access. J Rural Health 2022, 38(3), 519–526. [Google Scholar] [CrossRef] [PubMed]
- Reddick, C. G.; Enriquez, R.; Harris, R. J.; Sharma, B. Determinants of broadband access and affordability: An analysis of a community survey on the digital divide. Cities 2020, 106, 102904. [Google Scholar] [CrossRef]
- Prieger, J. E. The Supply Side of the Digital Divide: Is There Equal Availability in the Broadband Internet Access Market? Economic Inquiry 2003, 41(2), 346–363. [Google Scholar] [CrossRef]
- Roberts, L. W.; Battaglia, J.; Epstein, R. S. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv 1999, 50(4), 497–503. [Google Scholar] [CrossRef]
- NHRA. Workforce Series: Rural Behavioral Health; 2008.
- Brenes, G. A.; Danhauer, S. C.; Lyles, M. F.; Hogan, P. E.; Miller, M. E. Barriers to Mental Health Treatment in Rural Older Adults. Am J Geriatr Psychiatry 2015, 23(11), 1172–1178. [Google Scholar] [CrossRef]
- GoodTherapy. GoodTherapy. https://www.goodtherapy.org/blog/faq/how-much-does-therapy-cost.
- Lambert, D.; Gale, J. A.; Hartley, D. Substance abuse by youth and young adults in rural America. J Rural Health 2008, 24(3), 221–228. [Google Scholar] [CrossRef]
- Oser, C. B.; Leukefeld, C. G.; Tindall, M. S.; Garrity, T. F.; Carlson, R. G.; Falck, R.; Wang, J.; Booth, B. M. Rural drug users: factors associated with substance abuse treatment utilization. Int J Offender Ther Comp Criminol 2011, 55(4), 567–586. [Google Scholar] [CrossRef] [PubMed]
- Bond Edmond, M.; Aletraris, L.; Roman, P. M. Rural substance use treatment centers in the United States: an assessment of treatment quality by location. Am J Drug Alcohol Abuse 2015, 41(5), 449–457. [Google Scholar] [CrossRef]
- Calcaterra, S. L.; Bach, P.; Chadi, A.; Chadi, N.; Kimmel, S. D.; Morford, K. L.; Roy, P.; Samet, J. H. Methadone Matters: What the United States Can Learn from the Global Effort to Treat Opioid Addiction. J Gen Intern Med 2019, 34(6), 1039–1042. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M. C.; Rossen, L. M.; Bastian, B.; Faul, M.; Dowling, N. F.; Thomas, C. C.; Schieb, L.; Hong, Y.; Yoon, P. W.; Iademarco, M. F. Potentially Excess Deaths from the Five Leading Causes of Death in Metropolitan and Nonmetropolitan Counties - United States, 2010-2017. MMWR Surveill Summ 2019, 68(10), 1–11. [Google Scholar] [CrossRef] [PubMed]
- Okobi, O. E.; Ajayi, O. O.; Okobi, T. J.; Anaya, I. C.; Fasehun, O. O.; Diala, C. S.; Evbayekha, E. O.; Ajibowo, A. O.; Olateju, I. V.; Ekabua, J. J.; et al. The Burden of Obesity in the Rural Adult Population of America. Cureus 2021, 13(6), e15770. [Google Scholar] [CrossRef]
- Buettner-Schmidt, K.; Miller, D. R.; Maack, B. Disparities in Rural Tobacco Use, Smoke-Free Policies, and Tobacco Taxes. West J Nurs Res 2019, 41(8), 1184–1202. [Google Scholar] [CrossRef] [PubMed]
- Doogan, N. J.; Roberts, M. E.; Wewers, M. E.; Stanton, C. A.; Keith, D. R.; Gaalema, D. E.; Kurti, A. N.; Redner, R.; Cepeda-Benito, A.; Bunn, J. Y.; et al. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev Med 2017, 104, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M. C.; Gauthreaux, N.; Hermstad, A.; Arriola, K. J.; Mickens, A.; Ditzel, K.; Hernandez, C.; Haardorfer, R. Inequities in Physical Activity Environments and Leisure-Time Physical Activity in Rural Communities. Prev Chronic Dis 2022, 19, E40. [Google Scholar] [CrossRef]
- Cacari Stone, L.; Roary, M. C.; Diana, A.; Grady, P. A. State health disparities research in Rural America: Gaps and future directions in an era of COVID-19. J Rural Health 2021, 37(3), 460–466. [Google Scholar] [CrossRef]
- Association, A. H. Rural Report; 2019. https://www.giaging.org/issues/rural-aging/.
- Callaghan, T.; Lueck, J. A.; Trujillo, K. L.; Ferdinand, A. O. Rural and Urban Differences in COVID-19 Prevention Behaviors. J Rural Health 2021, 37(2), 287–295. [Google Scholar] [CrossRef]
- Sood, L.; Sood, V. Being African American and Rural: A Double Jeopardy From COVID-19. J Rural Health 2021, 37(1), 217–221. [Google Scholar] [CrossRef]
- Snowden, L. R.; Graaf, G. COVID-19, Social Determinants Past, Present, and Future, and African Americans' Health. J Racial Ethn Health Disparities 2021, 8(1), 12–20. [Google Scholar] [CrossRef]
- Leider, J. P.; Meit, M.; McCullough, J. M.; Resnick, B.; Dekker, D.; Alfonso, Y. N.; Bishai, D. The State of Rural Public Health: Enduring Needs in a New Decade. Am J Public Health 2020, 110(9), 1283–1290. [Google Scholar] [CrossRef] [PubMed]
- Dugani, S. B.; Mielke, M. M.; Vella, A. Burden and management of type 2 diabetes in rural United States. Diabetes Metab Res Rev 2021, 37(5), e3410. [Google Scholar] [CrossRef] [PubMed]
- Kurani, S. S.; Lampman, M. A.; Funni, S. A.; Giblon, R. E.; Inselman, J. W.; Shah, N. D.; Allen, S.; Rushlow, D.; McCoy, R. G. Association Between Area-Level Socioeconomic Deprivation and Diabetes Care Quality in US Primary Care Practices. JAMA Netw Open 2021, 4(12), e2138438. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A. G.; Nordberg, C. M.; Bandeen-Roche, K.; Pollak, J.; Poulsen, M. N.; Moon, K. A.; Schwartz, B. S. Urban-Rural Differences in Health Care Utilization and COVID-19 Outcomes in Patients With Type 2 Diabetes. Prev Chronic Dis 2022, 19, E44. [Google Scholar] [CrossRef] [PubMed]
- Prevention, C. f. D. C. a. Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals. 2023.
- Verdejo, H. E.; Ferreccio, C.; Castro, P. F. Heart Failure in Rural Communities. Heart Fail Clin 2015, 11(4), 515–522. [Google Scholar] [CrossRef] [PubMed]
- Khan, M. S.; Kumar, P.; Sreenivasan, J.; Khan, S. U.; Nasir, K.; Mehra, M. R.; C, O. D.; Warraich, H. J. Rural-Urban Differences in Mortality From Ischemic Heart Disease, Heart Failure, and Stroke in the United States. Circ Cardiovasc Qual Outcomes 2021, 14(4), e007341. [Google Scholar] [CrossRef] [PubMed]
- Stack, E.; Leichtling, G.; Larsen, J. E.; Gray, M.; Pope, J.; Leahy, J. M.; Gelberg, L.; Seaman, A.; Korthuis, P. T. The Impacts of COVID-19 on Mental Health, Substance Use, and Overdose Concerns of People Who Use Drugs in Rural Communities. J Addict Med 2021, 15(5), 383–389. [Google Scholar] [CrossRef]
- Summers-Gabr, N. M. Rural-urban mental health disparities in the United States during COVID-19. Psychol Trauma 2020, 12 (Suppl. S1), S222–S224. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhu, L.; Li, S.; Huang, J.; Ye, Z.; Wei, Q.; Du, C. Rural-urban disparities in knowledge, behaviors, and mental health during COVID-19 pandemic: A community-based cross-sectional survey. Medicine (Baltimore) 2021, 100(13), e25207. [Google Scholar] [CrossRef] [PubMed]
- IHME. New Global Burden of Disease analyses show depression and anxiety among the top causes of health loss worldwide, and a significant increase due to the COVID-19 pandemic.
- Twitter. 2021.
- NRHA. About Rural Health Care. https://www.ruralhealth.us/about-nrha/about-rural-health-care#:~:text=Ease%20of%20access%20to%20a,the%20health%20of%20the%20population.
- Mueller, J. T.; McConnell, K.; Burow, P. B.; Pofahl, K.; Merdjanoff, A. A.; Farrell, J. Impacts of the COVID-19 pandemic on rural America. Proc Natl Acad Sci USA 2021, 118. [Google Scholar] [CrossRef]
- McElfish, P. A.; Willis, D. E.; Shah, S. K.; Bryant-Moore, K.; Rojo, M. O.; Selig, J. P. Sociodemographic Determinants of COVID-19 Vaccine Hesitancy, Fear of Infection, and Protection Self-Efficacy. J Prim Care Community Health 2021, 12, 21501327211040746. [Google Scholar] [CrossRef] [PubMed]
- Julien, H. M.; Eberly, L. A.; Adusumalli, S. Telemedicine and the Forgotten America. Circulation 2020, 142(4), 312–314. [Google Scholar] [CrossRef] [PubMed]
- Hirko, K. A.; Kerver, J. M.; Ford, S.; Szafranski, C.; Beckett, J.; Kitchen, C.; Wendling, A. L. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc 2020, 27(11), 1816–1818. [Google Scholar] [CrossRef]
- Schmidt, E. READING THE NUMBERS: 130 MILLION AMERICAN ADULTS HAVE LOW LITERACY SKILLS, BUT FUNDING DIFFERS DRASTICALLY BY STATE. 2022.
- Mitchell, A. J., M.; Oliphant, B.; Shearer, E. Three Months In, Many Americans See Exaggeration, Conspiracy Theories and Partisanship in COVID-19 News. Pew Rsearch Center: 2020.
- Harris, J. K.; Beatty, K.; Leider, J. P.; Knudson, A.; Anderson, B. L.; Meit, M. The Double Disparity Facing Rural Local Health Departments. Annu Rev Public Health 2016, 37, 167–184. [Google Scholar] [CrossRef]
- Dauner, K. N.; Loomer, L. A qualitative assessment of barriers and facilitators associated with addressing social determinants of health among members of a health collaborative in the rural Midwest. BMC Health Serv Res 2021, 21(1), 867. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).