Submitted:
17 March 2023
Posted:
22 March 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
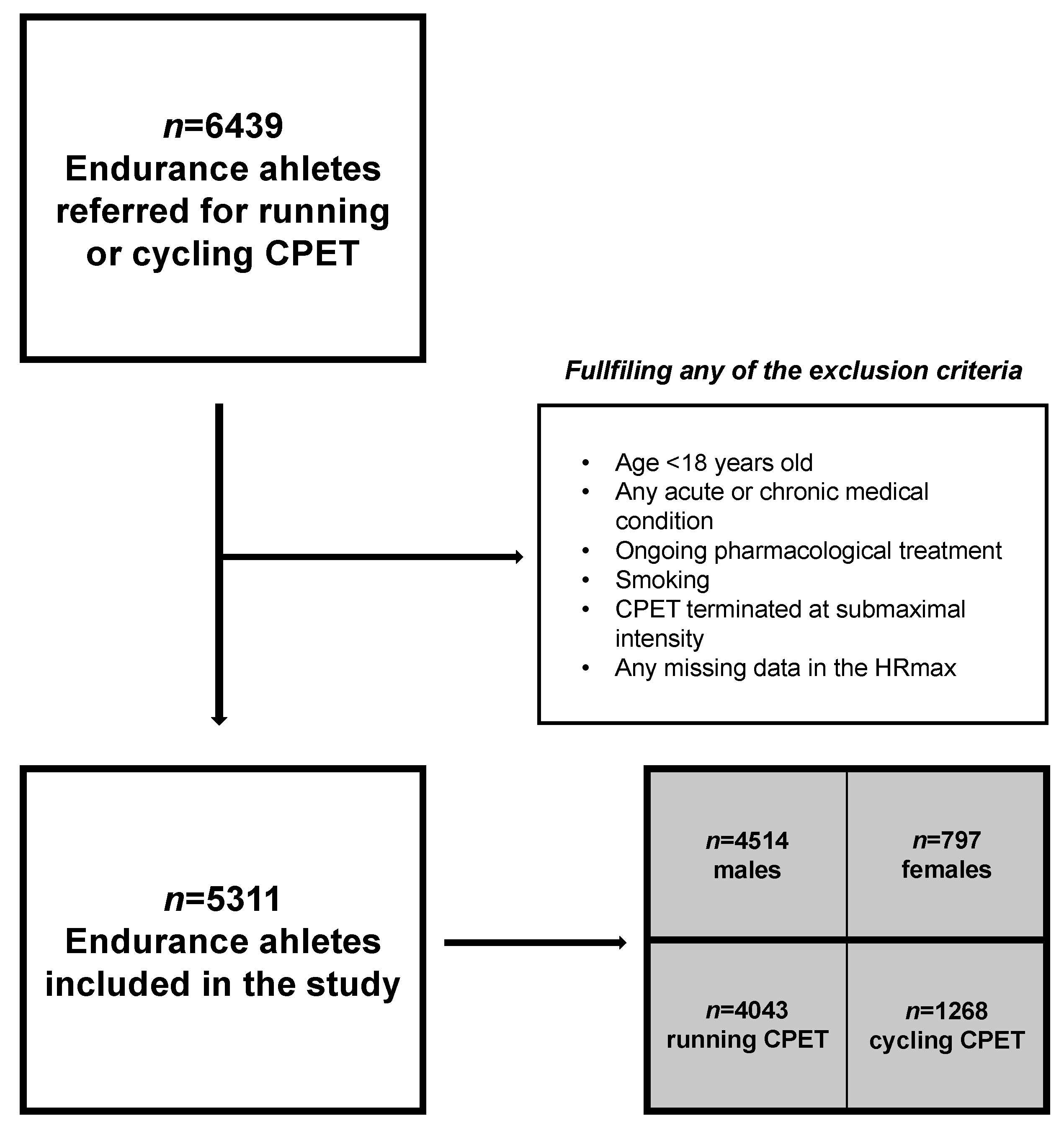
2. Materials and Methods
2.1. Study setting
2.2. Previously published HRmax prediction models
2.3. Cardiopulmonary exercise testing procedures
2.4. Data Analysis
3. Results
3.1. Athletes’ characteristics
3.2. Performance of selected prediction equations HRmax
| Reference | Equation | Performance in the athletic population | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predicted HRmax (beats·min−1) |
Difference from the observed HRmax (beats·min−1) |
MAPE | MAE (beats·min−1) | %MAE† | RMSE (beats·min−1) | %RMSE‡ | p-value | |||||
| Mean (SD) | CI | Mean (SD) | CI | |||||||||
| Part A. Running CPET | ||||||||||||
| Nes et al. | 211- 0.64 · age | 188.23 (5.20) | 188.07, 188.39 | 3.63 (8.98) | 3.35, 3.91 | 4.31 | 3.63 | 1.97 | 9.69 | 5.25 | <0.001 | |
| Machado et al. | 218- 0.8 · age | 189.54 (6.50) | 189.34, 189.74 | 4.94 (9.24) | 4.66, 5.23 | 4.69 | 4.94 | 2.68 | 10.47 | 5.67 | <0.001 | |
| Tanaka et al. | 208- 0.7 · age | 183.09 (5.68) | 182.92, 183.27 | -1.50 (9.06) | -1.78, -1.22 | 3.96 | 1.50 | 0.81 | 9.18 | 4.97 | <0.001 | |
| Fox et al. | 220- age | 184.42 (8.12) | 184.17, 184.67 | -0.18 (9.79) | -0.48, -0.12 | 4.25 | 0.18 | 0.10 | 9.79 | 5.13 | 0.38 | |
| Londeree et al. | 206.3- 0.711 · age | 181.00 (5.77) | 180.82, 181.18 | -3.59 (9.07) | -3.87, -3.31 | 4.17 | 3.59 | 1.95 | 9.76 | 5.29 | <0.001 | |
| Inbar et al. | 205.8- 0.685 · age | 181.43 (5.56) | 181.26, 161.60 | -3.17 (9.04) | -3.45, -2.89 | 4.10 | 3.17 | 1.72 | 9.58 | 5.19 | <0.001 | |
| Gellish et al. | 207- 0.7 · age | 182.09 (5.68) | 181.92, 182.27 | 2.50 (9.06) | 2.22, 2.78 | 4.03 | 2.50 | 1.36 | 9.40 | 5.09 | <0.001 | |
| Arena et al. | 209.3- 0.72 · age | 183.68 (5.85) | 183.50, 183.86 | -0.91 (9.09) | -1.19, -0.63 | 3.95 | 0.91 | 0.50 | 9.13 | 4.95 | <0.001 | |
| Part B. Cycling CPET | ||||||||||||
| Tanaka et al. | 208- 0.7 · age | 182.19 (6.32) | 181.84, 182.54 | -0.48 (9.24) | -0.99, -0.03 | 4.11 | 0.48 | 0.26 | 9.26 | 5.07 | 0.16 | |
| Fox et al. | 220- age | 183.12 (9.03) | 182.62, 183.62 | 0.46 (10.06) | -0.09, 1.01 | 4.41 | 0.46 | 0.25 | 10.07 | 5.52 | 0.23 | |
| Londeree et al. | 206.3- 0.711 · age | 180.08 (6.42) | 179.73, 180.43 | -2.58 (9.26) | -3.09, -2.07 | 4.31 | 2.58 | 1.41 | 9.61 | 5.26 | <0.001 | |
| Fairbarn et al. | 201- 0.63 · age | 177.77 (5.69) | 177.46, 178.08 | -4.90 (9.16) | -5.40, -4.40 | 4.68 | 4.90 | 2.68 | 10.38 | 5.68 | <0.001 | |
| Arena et al. | 209.3- 0.72 · age | 182.75 (6.50) | 182.39, 183.11 | 0.08 (9.28) | -0.43, 0.59 | 4.10 | 0.08 | 0.05 | 9.28 | 5.08 | 0.80 | |
4. Discussion
Perspective and further studies directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karvonen, J.; Vuorimaa, T. Heart rate and exercise intensity during sports activities. Practical application. Sports Med 1988, 5, 303-311. [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J Am Coll Cardiol 2001, 37, 153-156. [CrossRef]
- Guazzi, M.; Arena, R.; Halle, M.; Piepoli, M.F.; Myers, J.; Lavie, C.J. 2016 Focused Update: Clinical Recommendations for Cardiopulmonary Exercise Testing Data Assessment in Specific Patient Populations. Circulation 2016, 133, e694-711. [CrossRef]
- Iskandrian, A.S.; Heo, J.; Kong, B.; Lyons, E. Effect of exercise level on the ability of thallium-201 tomographic imaging in detecting coronary artery disease: analysis of 461 patients. J Am Coll Cardiol 1989, 14, 1477-1486. [CrossRef]
- Gianrossi, R.; Detrano, R.; Mulvihill, D.; Lehmann, K.; Dubach, P.; Colombo, A.; McArthur, D.; Froelicher, V. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation 1989, 80, 87-98. [CrossRef]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation 2010, 122, 191-225. [CrossRef]
- Kaminsky, L.A.; Arena, R.; Myers, J. Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing: Data From the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc 2015, 90, 1515-1523. [CrossRef]
- Millet, G.P.; Vleck, V.E.; Bentley, D.J. Physiological differences between cycling and running: lessons from triathletes. Sports Med 2009, 39, 179-206. [CrossRef]
- Price, S.; Wiecha, S.; Cieśliński, I.; Śliż, D.; Kasiak, P.S.; Lach, J.; Gruba, G.; Kowalski, T.; Mamcarz, A. Differences between Treadmill and Cycle Ergometer Cardiopulmonary Exercise Testing Results in Triathletes and Their Association with Body Composition and Body Mass Index. International Journal of Environmental Research and Public Health 2022, 19, 3557.
- Hanson, N.J.; Scheadler, C.M.; Lee, T.L.; Neuenfeldt, N.C.; Michael, T.J.; Miller, M.G. Modality determines VO2max achieved in self-paced exercise tests: validation with the Bruce protocol. Eur J Appl Physiol 2016, 116, 1313-1319. [CrossRef]
- Moons, K.G.; Kengne, A.P.; Woodward, M.; Royston, P.; Vergouwe, Y.; Altman, D.G.; Grobbee, D.E. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio)marker. Heart 2012, 98, 683-690. [CrossRef]
- Moons, K.G.; Royston, P.; Vergouwe, Y.; Grobbee, D.E.; Altman, D.G. Prognosis and prognostic research: what, why, and how? BMJ 2009, 338, b375. [CrossRef]
- Wiecha, S.; Price, S.; Cieslinski, I.; Kasiak, P.S.; Tota, L.; Ambrozy, T.; Sliz, D. Transferability of Cardiopulmonary Parameters between Treadmill and Cycle Ergometer Testing in Male Triathletes-Prediction Formulae. International Journal of Environmental Research and Public Health 2022, 19. [CrossRef]
- Nes, B.M.; Janszky, I.; Wisloff, U.; Stoylen, A.; Karlsen, T. Age-predicted maximal heart rate in healthy subjects: The HUNT fitness study. Scand J Med Sci Sports 2013, 23, 697-704. [CrossRef]
- Gulati, M.; Shaw, L.J.; Thisted, R.A.; Black, H.R.; Bairey Merz, C.N.; Arnsdorf, M.F. Heart rate response to exercise stress testing in asymptomatic women: the st. James women take heart project. Circulation 2010, 122, 130-137. [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M.; members of the, T.g. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. Eur Urol 2015, 67, 1142-1151. [CrossRef]
- Takken, T.; Mylius, C.F.; Paap, D.; Broeders, W.; Hulzebos, H.J.; Van Brussel, M.; Bongers, B.C. Reference values for cardiopulmonary exercise testing in healthy subjects - an updated systematic review. Expert Review of Cardiovascular Therapy 2019, 17, 413-426. [CrossRef]
- Paap, D.; Takken, T. Reference values for cardiopulmonary exercise testing in healthy adults: a systematic review. Expert Rev Cardiovasc Ther 2014, 12, 1439-1453. [CrossRef]
- Samuel, M.F.a.J.P.N.a.W.L.H. Physical activity and the prevention of coronary heart disease. Annals of clinical research 1968, 3 6, 404-432.
- Bouchard, C.; An, P.; Rice, T.; Skinner, J.S.; Wilmore, J.H.; Gagnon, J.; Perusse, L.; Leon, A.S.; Rao, D.C. Familial aggregation of VO(2max) response to exercise training: results from the HERITAGE Family Study. J Appl Physiol (1985) 1999, 87, 1003-1008. [CrossRef]
- Wiecha, S.; Kasiak, P.S.; Cieslinski, I.; Takken, T.; Palka, T.; Knechtle, B.; Nikolaidis, P.; Malek, L.A.; Postula, M.; Mamcarz, A.; et al. External validation of VO2max prediction models based on recreational and elite endurance athletes. PLoS One 2023, 18, e0280897. [CrossRef]
- Scherr, J.; Wolfarth, B.; Christle, J.W.; Pressler, A.; Wagenpfeil, S.; Halle, M. Associations between Borg's rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol 2013, 113, 147-155. [CrossRef]
- Damen, J.A.A.; Moons, K.G.M.; van Smeden, M.; Hooft, L. How to conduct a systematic review and meta-analysis of prognostic model studies. Clin Microbiol Infect 2022. [CrossRef]
- Stensvold, D.; Sandbakk, S.B.; Viken, H.; Zisko, N.; Reitlo, L.S.; Nauman, J.; Gaustad, S.E.; Hassel, E.; Moufack, M.; Bronstad, E.; et al. Cardiorespiratory Reference Data in Older Adults: The Generation 100 Study. Medicine and Science in Sports and Exercise 2017, 49, 2206-2215. [CrossRef]
- Lach, J.; Wiecha, S.; Sliz, D.; Price, S.; Zaborski, M.; Cieslinski, I.; Postula, M.; Knechtle, B.; Mamcarz, A. HR Max Prediction Based on Age, Body Composition, Fitness Level, Testing Modality and Sex in Physically Active Population. Frontiers in Physiology 2021, 12, 695950. [CrossRef]
- Machado, F.A.; Kravchychyn, A.C.P.; Peserico, C.S.; da Silva, D.F.; Mezzaroba, P.V. A new age-based equation for predicting maximum heart rate in endurance-trained runners. Revista Brasileira de Ciências do Esporte 2018, 40, 100-105. [CrossRef]
- McGregor, G.; Powell, R.; Begg, B.; Birkett, S.T.; Nichols, S.; Ennis, S.; McGuire, S.; Prosser, J.; Fiassam, O.; Hee, S.W.; et al. High-intensity interval training in cardiac rehabilitation (HIIT or MISS UK): A multi-centre randomised controlled trial. Eur J Prev Cardiol 2023. [CrossRef]
- Kostis, J.B.; Moreyra, A.E.; Amendo, M.T.; Di Pietro, J.; Cosgrove, N.; Kuo, P.T. The effect of age on heart rate in subjects free of heart disease. Studies by ambulatory electrocardiography and maximal exercise stress test. Circulation 1982, 65, 141-145. [CrossRef]
- Arena, R.; Myers, J.; Kaminsky, L.A. Revisiting age-predicted maximal heart rate: Can it be used as a valid measure of effort? Am Heart J 2016, 173, 49-56. [CrossRef]
- Magri, D.; Piepoli, M.; Gallo, G.; Corra, U.; Metra, M.; Paolillo, S.; Filardi, P.P.; Maruotti, A.; Salvioni, E.; Mapelli, M.; et al. Old and new equations for maximal heart rate prediction in patients with heart failure and reduced ejection fraction on beta-blockers treatment: results from the MECKI score data set. Eur J Prev Cardiol 2022, 29, 1680-1688. [CrossRef]
- Zavorsky, G.S. Evidence and possible mechanisms of altered maximum heart rate with endurance training and tapering. Sports Med 2000, 29, 13-26. [CrossRef]
- Miller, W.C.; Wallace, J.P.; Eggert, K.E. Predicting max HR and the HR-&OV0312;2 relationship for exercise prescription in obesity. Medicine & Science in Sports & Exercise 1993, 25. [CrossRef]
- Wiecha, S.; Kasiak, P.S.; Cieslinski, I.; Maciejczyk, M.; Mamcarz, A.; Sliz, D. Modeling Physiological Predictors of Running Velocity for Endurance Athletes. J Clin Med 2022, 11. [CrossRef]
- Sliz, D.; Wiecha, S.; Gasior, J.S.; Kasiak, P.S.; Ulaszewska, K.; Postula, M.; Malek, L.A.; Mamcarz, A. The Influence of Nutrition and Physical Activity on Exercise Performance after Mild COVID-19 Infection in Endurance Athletes-CESAR Study. Nutrients 2022, 14. [CrossRef]
- Sliz, D.; Wiecha, S.; Ulaszewska, K.; Gasior, J.S.; Lewandowski, M.; Kasiak, P.S.; Mamcarz, A. COVID-19 and athletes: Endurance sport and activity resilience study-CAESAR study. Front Physiol 2022, 13, 1078763. [CrossRef]
| Variable | Running CPET | Cycling CPET | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| All [n=4043] | Males [n=3377] | Females [n=666] | All [n=1268] | Males [n=1137] | Females [n=131] | ||||
| Age [years] | 33.58 (8.12) | 33.96 (8.15) | 33.66 (7.67) | 36.88 (9.03) | 37.30 (9.11) | 33.19 (7.37) | <0.001 | ||
| Weight [kg] | 74.87 (11.18) | 77.68 (9.38) | 60.60 (8.36) | 76.99 (10.76) | 78.81 (9.53) | 61.18 (7.30) | <0.001 | ||
| Height [cm] | 177.52 (7.84) | 179.55 (6.24) | 167.22 (7.00) | 178.77 (7.26) | 180.01 (6.38) | 168.05 (5.41) | <0.001 | ||
| BMI [kg·m−2] | 23.66 (2.54) | 24.06 (2.41) | 21.65 (2.18) | 24.04 (2.65) | 24.32 (2.56) | 21.63 (2.11) | <0.001 | ||
| BF [%] | 16.47 (5.17) | 15.48 (4.52) | 21.48 (5.33) | 16.75 (5.07) | 16.09 (4.68) | 22.46 (4.66) | 0.09 | ||
| FFM [kg] | 62.45 (9.27) | 65.40 (6.44) | 47.49 (6.55) | 63.93 (8.17) | 65.86 (6.02) | 47.23 (4.40) | <0.001 | ||
| HRmax [beats·min−1] | 184.60 (9.79) | 184.47 (9.88) | 185.22 (9.33) | 182.67 (10.27) | 182.46 (10.30) | 184.38 (9.97) | <0.001 | ||
| RERmax | 1.12 (0.04) | 1.12 (0.04) | 1.12 (0.04) | 1.13 (0.04) | 1.13 (0.05) | 1.12 (0.03) | <0.001 | ||
| VE/VCO2max | 31.75 (3.89) | 31.70 (3.83) | 32.02 (4.22) | 29.39 (4.18) | 29.33 (4.17) | 29.92 (4.28) | <0.001 | ||
| fR [breaths·min−1] | 57.22 (9.11) | 57.57 (9.22) | 55.44 (8.31) | 56.37 (9.32) | 56.51 (9.47) | 55.18 (7.92) | 0.004 | ||
| VO2max [mL·min−1·kg−1] | 53.24 (7.12) | 54.09 (6.92) | 48.90 (6.54) | 51.67 (7.86) | 51.95 (7.96) | 49.21 (6.53) | <0.001 | ||
| O2pulsemax [mL·beat−1] | 21.58 (4.03) | 22.69 (3.24) | 15.95 (2.73) | 21.66 (3.62) | 22.28 (3.18) | 16.31 (2.67) | 0.53 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





