1. Introduction
The ongoing pandemic of Coronavirus disease 2019 (COVID-19) has had a significant impact on various aspects of people’s lives for almost three years. [
1]. Not only does the disease itself pose a threat to individuals’ physical health, but misinformation and lack of trust in medical treatment and prevention methods can also contribute to increased uncertainty and stress. [
2,
3]. The lockdown measures implemented to slow the spread of the virus have also greatly affected people’s lifestyles, activities and mental health. [
4]. COVID-19 infection has been shown to have an adverse effect on the heart function of patients who survived the infection [
5]. A greater tendency to reduced left ventricular ejection fraction, end-diastolic volume, stroke volume was found. This can then negatively affect the physical activity of patients [
6]. Clinicians and psychologists are therefore searching for new coping strategies to address the mental health impacts of the pandemic. [
7]. It is also well known that COVID-19 can also affects the sleeping patterns and endurance of the patients and that is why mental health, sleeping and endurance are crucial concepts affected by COVID-19
A particularly difficult time in the lives of EAs and other people is the COVID-19 pandemic. EAs from Poland, Romania, and Slovakia had the highest level of mental stress during the fourth wave [
8]. EAs also adopted different coping strategies that affected mental health differently. Returning to regular training and physical fitness may not be easy due to mental aspects [
9]. Proper activity maintenance can prevent further stress related to the pandemic and lockdown [
10]. Physical activity has been shown to be associated with reduced hospitalization, intensive care unit admissions and mortality of COVID-19 patients. People who mainly perform resistance and endurance exercises are less likely to be hospitalized [
11]. It turns out that the diet before COVID-19 infection also influenced the development of the disease. The effectiveness of eating a high-quality diet, as well as a plant-based diet, had a positive effect on the risk of hospitalization [
12]. Not only the lockdown but also the COVID-19 disease had an impact on the adverse lifestyle changes and sports results achieved by EA [
13]. Coaches, medical doctors, and EA will try to counteract these problems to come to the previous competition level and fitness [
14]. Moreover, some may need rehabilitation [
15]. The mental health of patients 12 months after the disease presents symptoms of mental disorders, lack of concentration and focus, increasing with the severity of the infection [
16]. Significant improvement was noted 2 years after infection, which is reassuring, but it should be remembered that undergoing COVID-19 infection consequences for mental health can influence future health state of the EA [
17]. It was tested that the course of mental disorders related to COVID-19 depends on age and sex [
18,
19]. Commonly reported post-illness psychiatric symptoms are anxiety (6.5% to 63%), depression (4% to 31%), and post-traumatic stress disorder (12.1% to 46.9%), patients reported lower quality of life up to 3 months after illness [
20]. These data show that this is not a problem for individuals, but for a large group of patients, it can bother their everyday functioning and motivation.
Another aspect is the impact of the disease on patients’ sleep. It turns out that patients often report insomnia related to infection but is usually mild [
21]. Endurance athletes during the pandemic have been found to experience changes in their training, competition, and sleep patterns which can negatively affect their performance [
22]. Results from the study indicate that athletes who reported sleep disturbances had lower endurance performance, average marathon finishing times decreased during the pandemic. A meta-analysis shows the neurological and neuropsychiatric changes post-COVID-19, on average 31% of patients experience sleep disorders [
23]. This is a worrying phenomenon because sleep is a key aspect of the proper functioning of the body. This effect is especially challenging for EA, as sleep loss is associated with poorer athletic performance as well as exercise efficiency [
24].
The aim of our study is twofold: to understand how contracting COVID-19 affects sleep and mental health and to evaluate how a previous mild COVID-19 infection impacts results on endurance performance scores among EAs. These are aspects that we will struggle with during the pandemic, and EA will have to find solutions to counteract them until a fully effective vaccine or drug is found and the population shows a greater willingness to use vaccinations [
25].
2. Materials and Methods
2.1. General study information
We conducted a study that included: a double CPET assessment, and a mental health and sleep questionnaire. EAs underwent CPET before and after COVID-19 infection. During the second CPET, they also received the survey. Exercise tests were performed between June 2021 and December 2022 at the SportsLab sports diagnostics center (SportsLab, Warsaw, Poland). Participants underwent CPET before and after the disease with the same type (cycling or running). Interval between infection and both CPETs have been measured to control the effect of time elapsed and adjust analysis. The sample consists of amateur EAs at various fitness levels according to reference standards for VO
2max [
26,
27]. After infection and directly before the second CPET, each EA underwent a medical evaluation by a Physician (cardiology or internal medicine specialist) which consisted of taking their medical history, physical examination, 12-lead ECG, echocardiography, and complete blood count. EA have been screened for ongoing long-lasting COVID-19 (eg. respiratory and circulatory) consequences preventing them from performing CPET.
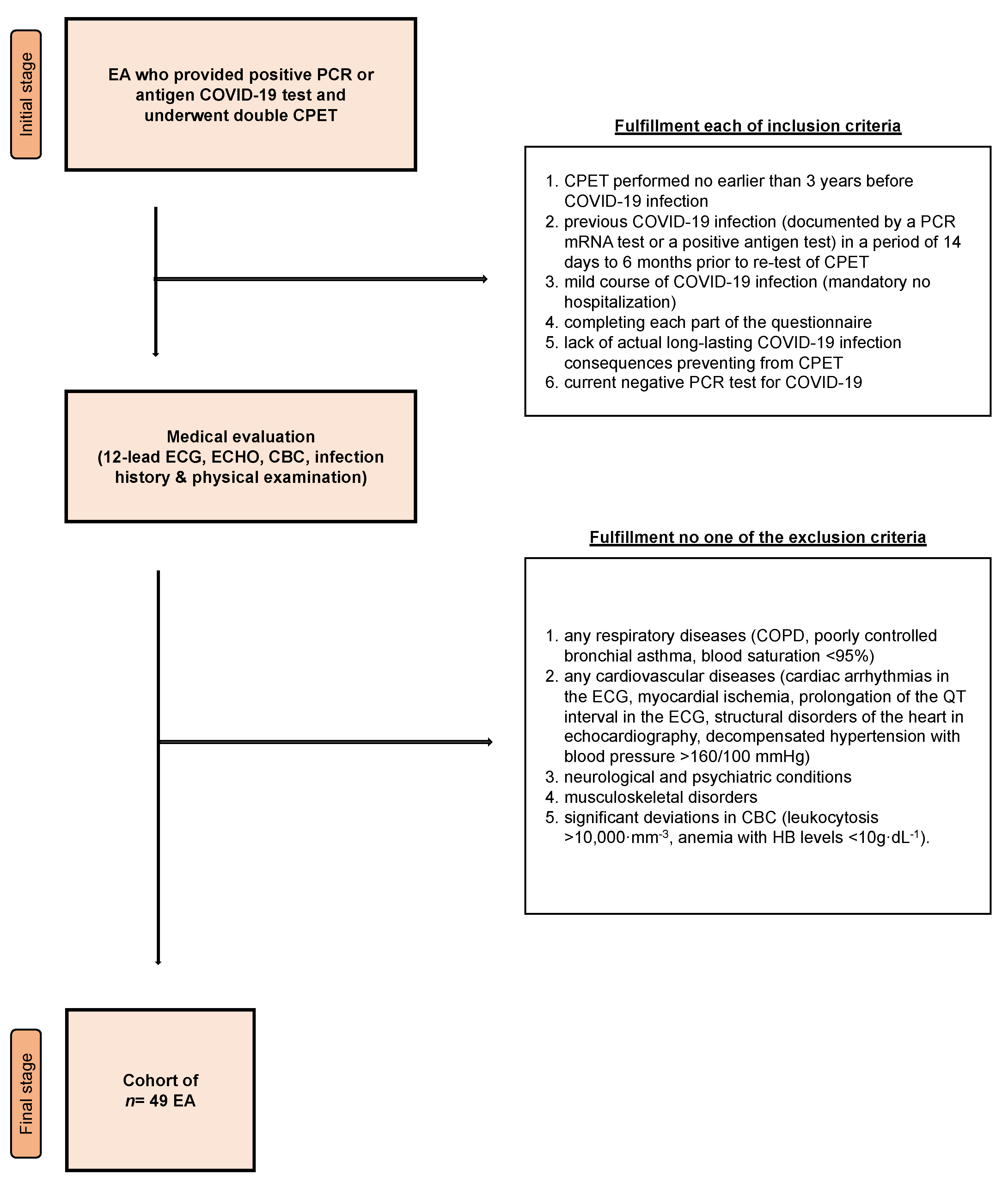
Inclusion criteria: the interval between the first CPET and COVID-19 infection <3 years, mild COVID-19 infection (which did not require hospitalization) confirmed by PCR or antigen test, participation in the survey, (4) no ongoing long-lasting COVID-19 consequences preventing from CPET (eg. related to circulatory and respiratory systems), and (5) present negative COVID-19 PCR or antigen test.
Exclusion criteria: pulmonary condition (COPD, uncontrolled bronchial asthma, blood saturation <95%), cardiovascular disease (arrhythmia confirmed by ECG, ischemia of myocardium, QT prolongation confirmed by ECG, morphological heart abnormalities confirmed by echocardiography, uncontrolled hypertension >160/100 mmHg), [
28] present mental condition, (4) an orthopedic condition that prevents EA to perform CPET, (5) deviations in CBC (leukocytosis >10,000·mm
-3, anemia with blood hemoglobin <10g·dL
-1).
A visual representation of the recruitment procedure is provided in
Figure 1.
Figure 1.
Recruitment procedure. Abbreviations: EA, endurance athlete; PCR, polymerase chain reaction; COVID-19, coronavirus disease 2019; CPET, cardiopulmonary exercise test; ECG, 12-lead electrocardiogram; ECHO, echocardiography examination; CBC, complete blood count; COPD, Chronic obstructive pulmonary disease.
Figure 1.
Recruitment procedure. Abbreviations: EA, endurance athlete; PCR, polymerase chain reaction; COVID-19, coronavirus disease 2019; CPET, cardiopulmonary exercise test; ECG, 12-lead electrocardiogram; ECHO, echocardiography examination; CBC, complete blood count; COPD, Chronic obstructive pulmonary disease.
2.2. Questionnaire
We used the previously validated PaLS (Pandemic against LifeStyle) questionnaire [
29,
30,
31], which covered the following domains: basic information about the subjects, their training experience, health status, and infection details, mental health, coping strategies, and mood state (14 questions) and sleep habits (12 questions). The basic information part consisted of questions examining demographic data, primary sports discipline, training and competition experience, and any previous long-lasting COVID-19 consequences. We have added a point to each section in which the EAs rated on a scale of -5/0/+5 the impact of the COVID-19 pandemic, the restrictions introduced, the course of the disease, and the resulting lifestyle changes. Negative values represented a harmful effect, positive values a positive effect, and 0 meant no association. The scale allowed for adjusting to noticed changes in intensities.
2.2.1. Mental health part
Mental health was assessed by the original questions. EAs were asked about implemented methods: coping strategies (rapid return to work, neglecting or acceptance of the current condition, usage of stimulants and alcohol, looking for support among others, expanding knowledge about the virus, joking about the infection, usage of relaxation techniques), infection-related mood changes (concentrating on the situation, more often suffering negative emotions) and observed mental health disorders (giving up, more positive or more negative outlook on life, criticizing themselves, strong expressions of negative emotions). EAs could choose one of the following answers: “I did not try this method”, “I used it in my everyday life, but only to a small extent”, “I used this method often, or it was one of the basic methods to cope with COVID-19 induced stress”, “I used this method regularly”.
2.2.1. Sleep part
Sleep was assessed by the Athens Insomnia Scale [
32] and the three additional questions related to usual habits: hour of walking sleep (participants declared precise time when they walk into the bed), sleep time (described in hours and minutes), and time spent in front of the devices emitting blue light (also described in hours and minutes).
2.3. CPET procedure & somatic measurements
Each subject performed an intensity-adjusted, maximal effort–limited CPET either running (mechanical treadmill, h/p/Cosmos quasar, Germany) or cycling (cycle ergometer, RBM elektronik-automation GmbH, Leipzig, Germany). The selected modality was the same post-infection as pre-infection. During pre-infection CPET participants chose their modality based on their preferences and primary sport discipline. During examinations constant beath-by-breath gas exchange (Hans Rudolph V2 Mask, Hans Rudolph Inc, Shawnee, Kansas), blood lactate (Super GL2 analyzer, Müller Gerätebau GmbH, Freital, Germany), and cardiopulmonary (Cosmed Quark CPET device, Rome, Italy) monitoring were used. The cycling test began with 3-5 minutes of freewheel pedaling followed by a gradual increase in intensity (20 Watts/2 minutes for females and 30 Watts/2 minutes for males). The running protocol also started with a 3–5-minute warmup at a speed varying between 7-12 km per hour and a constant 1% inclination followed by a gradual increase in speed (1 km/2 minute both for females and males). CPET termination was obtained when the subject declared volitional exhaustion, and maximal effort was additionally confirmed by a heart rate (HR) or maximal oxygen uptake (VO
2max) plateau (lack of growth in exercise parameter with growing CPET resistance). Participants were verbally encouraged by the physiologist to achieve the maximum score. Anaerobic threshold (AT) and respiratory compensation point (RCP) were determined based on actually recommended guidelines [
33]. Before each exercise test, a body composition examination was performed (the Tanita body analyzer, Tanita, MC 718, Japan). The used multifrequency was 5 kHz/50 kHz/250 kHz. Obtained endpoints were weight, height, body mass index (BMI), lean mass, body fat percentage (BF), fat mass, VO
2, HR, pulmonary ventilation (VE), speed (for running CPET), power (for cycling CPET), breathing frequency (f
R), and blood lactate concentration (Lac).
2.4. Data analysis
The results are shown as number (n) and percentage (%) for categorical variables and average with standard deviation for continuous variables. Data is shown in line with APA Guidelines (
https://apastyle.apa.org/; accessed on 16th March 2023). The Shapiro-Wilk test was used to evaluate the normal distribution. Relationships between CPET and somatic measures (weight, BMI, lean mass, BF, fat mass, VO
2, HR, VE, running speed, cycling power, f
R, and Lac) and questionnaire results (sleep and mental health outcomes) were assessed via Kruskal-Wallis rank’s ANOVA. Differences between pre-/post-COVID-19 results of exercise and somatic performance (weight, BMI, lean mass, BF, fat mass, VO
2, HR, VE, running speed, cycling power, f
R, and Lac) were obtained from Student’s t-test for independent means. The participant’s number was set before conducting recruitment procedures at the effective significant minimum using G∗Power (version 3.1.9.2; Germany). The p=0.05 was considered as a significance borderline. Data analysis was performed in STATISTICA (version 13.3, StatSoft Polska Sp. z o.o., Kraków, Poland) and SPSS (version 28; IBM SPSS, Chicago, IL, USA).
3. Results
3.1. Cohort description
Among 49 EAs who were recruited for this study, 87.8% (n=43) were males and 12.2 % (n=6) were females. Males were 40.7 (7.0) years old and 178.5 (6.8) cm in height, while females were 38.1 (6.4) years old and 178.4 (6.9) cm in height. There were 63.3% (n=31) running and 26.7% (n=18) cycling exercise examinations. Participants had to be prespecified in running or cycling, but also could add other supplemental trained disciplines. 30.6% (n=15) of participants declared additional disciplines which included triathlon, football and martial arts. 8.2% (n=4) of the cohort trained for 1-2 years, 28.6% (n=14) for 3-5 years, 38.8% (n=19) for 6-10 years, and 21.3% (n=12) had >10 years of training experience. 46.9% (n=23) of EAs withdrew from some type of competition due to undergoing COVID-19 infection. Individuals assessed their general health status on the -5/0/+5 scale as 4.8 (0.5) pre- and as 4.1 (0.5) post-COVID-19 infection, while 20.4% (n=10) of them declared suffering from COVID-19 consequences lasting longer than 2 weeks in the past. The time from the first to the second CPET was 591.7 (282.2) days. The period between pre-COVID-19 CPET and the termination of the infection (defined as negative PCR) was 436.4 (290.4) days, while the period between post-COVID-19 CPET and termination of the infection was 155.3 (82.52) days.
3.2. CPET performance
CPET performance stratified by infection status is presented in
Table 1. Between pre- and post-exercise tests, significant differences were found in key parameters, such as VO
2 at AT (35.0 (6.4) vs 32.4 (5.9) ml·kg·min
-1, p<0.001), RCP (43.9 (7.3) vs 40.5 (6.6) ml·kg·min
-1, p<0.001), and maximal (47.8 ((7.8) vs 45.0 (7.0) ml·kg·min
-1, p<0.001). VO
2 was higher before infection. We also observed a deterioration of HR at AT (145.1 (10.8) vs 141.1 (10.0) bpm, p<0.001) and RCP (168.8 (9.0) vs 165.1 (9.7) bpm, p<0.001). Other significantly different variables were running speed at AT (p=0.044) and RCP (p<0.001), VE at RCP (p<0.001), and Lac at RCP (p=0.013).
3.3. Sleep & mental health
A description of participants’ responses with mean rangs where applicable is presented in
Table 2 for sleep and
Table 3 for mental health. We are presenting only significant (p<0.05) results owing to a large amount of possible response-CPET variable combinations. Briefly, the mental health of our EAs showed a strong linkage to CPET performance. Awakenings during the night influenced HR at RCP (H(2)=7.2; p=0.028). EA who described it as a considerable problem also noticed the highest HR at RCP (mean rang= 99.9 vs 71.4 vs 55.1). Sufficient total sleep duration was linked with the highest VE at RCP compared to slightly and markedly insufficient (H(2)=8.7; p=0.013; mean rang= 30.4 vs 18.5 vs 29.7). Similar associations have been observed for f
R at RCP (H(2)=4.5; p=0.104) and Lac at RCP (H(2)=8.7; p=0.013). Sleep quality correlated with maximal power or speed, both relative and absolute VO
2 at RCP and maximal, VE at RCP and maximal, and maximal HR (each p<0.05). All precise results stratified by answer type and exercise variable have been shown in
Table 4, part A.
Interestingly, we found a much less significant relationship between self-reported mental health and sports performance. Briefly, our EA applied different coping strategies, and their habits to improve mental state varies significantly. Undertaking activities to improve one’s situation (e.g., by learning more about COVID-19) has been linked to lean body mass (H(3)=8.2; p=0.042). It is worth noting that, joking about the COVID-19 infection influenced up to five CPET variables: HR at AT (H(3)=8.2; p=0.042), absolute VO
2 at RCP (H(3)=9.1; p=0.029), VE at RCP (H(3)=8.3; p=0.041), maximal relative VO
2 (H(3)=8.0; p=0.047) and maximal absolute VO
2 (H(3)=10.6; p=0.014). Expressive negative emotions (e.g., by shouting loudly or arguing with others) correlated with VE at AT (H(3)=10.9; p=0.012), and EA who often used this method observed the highest VE (mean rang= 44.0 vs 42.0 vs 34.4 and 20.4). The use of relaxation techniques altered running speed or cycling power (H(2)=6.8; p=0.033), maximal relative VO
2 (H(2)=6.1; p=0.046), and maximal Lac (H(2)=6.2; p=0.045). We did not observe any other significant association between declared mental health state or habit and CPET performance. All Kruskal-Wallis H test scores from the mental health part are presented in
Table 4, part B.
4. Discussion
In our study, we showed the impact of EAs having mild COVID-19 on mental health and sleep, as well as their correlation with cardiopulmonary exercise test scores. The main findings were: episodes of awakening during sleep affected heart rate at the respiratory compensation point, sufficient total sleep duration compared to slightly and markedly insufficient was linked with the highest pulmonary ventilation at the respiratory compensation point, (4) quality of sleep correlated with maximal power or speed and maximal heart rate, (5) EAs adopted different strategies of coping with stress, which was associated with the influence on lean body mass, (6) cardiopulmonary exercise test parameters were influenced by EAs individual behaviors and habits (i.e.,. joking about the COVID-19 infection, expressive negative emotions and use of relaxation techniques). This paper focuses on outcomes of mild COVID-19 infection on sleep and mental health. Other possibly affecting covariables (including participants sex, age, CPET modality, nutrition, training regimen and previous sport experience) were analyzed in remaining CAESAR manuscripts [
34,
35].
The effect of sleep deprivation and sleep duration on athletic performance, reaction time, accuracy, strength, and endurance in EAs has been proven in many studies [
36]. EAs in our study who reported insufficient sleep time had significant changes in parameters such as pulmonary ventilation, breathing frequency and blood lactate concentration at the respiratory compensation point;Lactate changes are mainly influenced by sleep deprivation at the end of the night [
37]. In contrast, increasing sleep time or introducing naps could improve reaction time, alertness, vigor and mood, as well as prevent fatigue [
38]. For EAs, the sleep of the correct quality and length is essential because it affects physical and mental regeneration, which is necessary to achieve high sports results [
39]. The reduction in endurance parameters may be partially linked to poor sleep hygiene, so it is important to follow it. Among young EAs, up to 41% do not comply with the rules of sleep hygiene [
40]. They exhibit behaviors such as exposure to blue light before falling asleep, extended wake-up time, and eating meals before falling asleep. Delayed onset and awakening after falling asleep and the presence of sleep phases unaffected by varying training severity suggest a questionable recovery in athletes after intense training [
41]. The quality of sleep among EAs surveyed in our study changed parameters such as speed, power, oxygen uptake, absolute oxygen uptake, pulmonary ventilations at the respiratory compensation point and maximal oxygen uptake, absolute maximal oxygen uptake, maximal heart rate, maximal pulmonary ventilation compared to the results before getting sick with COVID-19.
The COVID-19 also affected the mental health of endurance athletes. 22.2% reported mood deterioration or symptoms of depression during the COVID-19 pandemic. Comparably, only 3.8% reported such signs when asked about the pre-pandemic period [
42]. This is an alarming result considering that mental health affects CPET scores in EAs. Moreover, as the pandemic continues, this condition is getting worse. Comparing the results from 2020 to 2021, despite better access to possibilities of training, mental problems increased from 36% to 80% [
43]. Among young EAs whose activity level decreased during the pandemic, an improvement in the quality of mental life was noticed after returning to regular activity [
44]. Mood, stress levels, and overall mental health among EAs may be lowered at even 8 weeks after COVID-19 infection [
45], which consequently adversely affects athletic performance and attitude to training. It is worth underlining, that people who have recovered from COVID-19 are at risk of memory loss, anxiety, depression and even post-traumatic stress disorder (PTSD) compared to individuals who have not had the disease [
46]. This paper was directed at the impact of the disease on asymptomatic and mildly symptomatic EAs. As claimed by Petek et al. this was the most common course of COVID-19 infection in the athletic population [
47]. Even non-hospitalized EAs are more likely to develop anxiety, trauma- and stress-related disorders, or fatigue [
48]. Augustin et al. investigated that up to 14% of patients report fatigue at 7 months follow up and females are considered as a higher risk group [
49]. EAs incorporate various treatment strategies. Briefly, progressive muscle relaxation techniques have a positive impact on anxiety and sleep quality during the ongoing COVID-19 disease [
50]. Thus, it is worth considering strategy for EA during and after the disease. It is important to provide EAs with comprehensive care and assistance in recovering from COVID-19 and later returning to sports competition under stressful circumstances [
51,
52].
Declared negative emotions were correlated with VE at AT. This result may be influenced by the fact that stressful circumstances can enhance the response of EAs to exertion and mobilize them to higher performance [
53]. The impact of the relaxation techniques on the Lac among EAs is confirmed by a study conducted on runners [
54]. Athletes using meditation or autogenic training after six months had significantly reduced Lac after exercise compared to the control group. Although, changes in VO
2max were not significant. Findings provided by Solberg et al. may be extrapolated to the post-pandemic period because mindfulness techniques could improve performance, endurance, and cognitive functions [
55]. Finally, we found that joking about the disease affected HR, VO
2, and VE, however, the basic mechanism remains unclear. We underline, that the primary goal of this paper is not to investigate the causative mechanisms, but to draw attention of linkages between CPET changes, well-being, and underwent COVID-19 infection in the athletic population. Thus, we recommend further studies to examine the physiologic reasons for the above-described results.
Limitations
The survey results were based on self-reported answers and may not accurately reflect participants’ actual habits. The time gap between the pre- and post-infection CPET tests may have an impact on the results due to variations in fitness levels among participants. It is important to exercise caution when applying the findings to other situations and to conduct additional research to confirm the conclusions about the effects of mild COVID-19 infection on exercise performance, sleep, and mental health.
5. Conclusions
The quality of sleep and mental health is greatly impacted by both the ongoing pandemic and contracting COVID-19. It is essential for EAs to have access to professional medical and psychological support. Adopting effective coping strategies can aid in the treatment and prevention of mental health issues. There is also a connection between mental health and sleep habits and athletic performance. The course of COVID-19 infection and the lifestyle of athletes have an impact on cardiorespiratory capacity and CPET test results. Therefore those working with EAs, such as coaches, clinicians, and psychologists, should be aware of the potential effects of mild COVID-19 infection and take steps to protect their health, including providing appropriate treatment recommendations.
Author Contributions
Conceptualization, Daniel Śliż, Szczepan Wiecha and Marcin Lewandowski; Methodology, Daniel Śliż and Przemysław Seweryn Kasiak; Validation, Daniel Śliż and Szczepan Wiecha; Formal analysis, Daniel Śliż, Jakub S. Gąsior and Przemysław Seweryn Kasiak; Investigation, Daniel Śliż, Szczepan Wiecha, Marcin Lewandowski and Artur Mamcarz; Resources, Daniel Śliż, Szczepan Wiecha and Marcin Lewandowski; Data curation, Daniel Śliż, Szczepan Wiecha, Przemysław Seweryn Kasiak and Katarzyna Ulaszewska; Writing – original draft, Daniel Śliż, Przemysław Seweryn Kasiak and Katarzyna Ulaszewska; Writing – review & editing, Daniel Śliż, Szczepan Wiecha, Jakub S. Gąsior, Przemysław Seweryn Kasiak and Katarzyna Ulaszewska; Visualization, Daniel Śliż, Szczepan Wiecha, Jakub S. Gąsior and Przemysław Seweryn Kasiak; Supervision, Daniel Śliż, Szczepan Wiecha and Artur Mamcarz; Project administration, Daniel Śliż, Szczepan Wiecha and Artur Mamcarz; Funding acquisition, Daniel Śliż, Marcin Lewandowski and Marcin Barylski. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the Medical University of Warsaw (approval no. KB/50/21 from 19th April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to not obtaining consent from respondents to publish the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tagliabue, F.; Galassi, L.; Mariani, P. The “Pandemic” of Disinformation in COVID-19. SN Compr Clin Med 2020, 2, 1287-1289. [CrossRef]
- Makowska, M.; Boguszewski, R.; Podkowińska, M. Trust in Medicine as a Factor Conditioning Behaviors Recommended by Healthcare Experts during the COVID-19 Pandemic in Poland. Int J Environ Res Public Health 2022, 19. [CrossRef]
- Sharif, N.; Alzahrani, K.J.; Ahmed, S.N.; Dey, S.K. Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front Immunol 2021, 12, 714170. [CrossRef]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res 2020, 293, 113429. [CrossRef]
- Rahmati, M.; Koyanagi, A.; Banitalebi, E.; Yon, D.K.; Lee, S.W.; Il Shin, J.; Smith, L. The effect of SARS-CoV-2 infection on cardiac function in post-COVID-19 survivors: A systematic review and meta-analysis. J Med Virol 2023, 95, e28325. [CrossRef]
- Gielen, S.; Laughlin, M.H.; O’Conner, C.; Duncker, D.J. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog Cardiovasc Dis 2015, 57, 347-355. [CrossRef]
- Belen, H. Fear of COVID-19 and Mental Health: The Role of Mindfulness in During Times of Crisis. Int J Ment Health Addict 2022, 20, 607-618. [CrossRef]
- Makarowski, R.; Predoiu, R.; Piotrowski, A.; Görner, K.; Predoiu, A.; Oliveira, R.; Pelin, R.A.; Moanță, A.D.; Boe, O.; Rawat, S.; et al. Coping Strategies and Perceiving Stress among Athletes during Different Waves of the COVID-19 Pandemic-Data from Poland, Romania, and Slovakia. Healthcare (Basel) 2022, 10. [CrossRef]
- Mulcahey, M.K.; Gianakos, A.L.; Mercurio, A.; Rodeo, S.; Sutton, K.M. Sports Medicine Considerations During the COVID-19 Pandemic. Am J Sports Med 2021, 49, 512-521. [CrossRef]
- Fiorilli, G.; Buonsenso, A.; Davola, N.; Di Martino, G.; Baralla, F.; Boutious, S.; Centorbi, M.; Calcagno, G.; di Cagno, A. Stress Impact of COVID-19 Sports Restrictions on Disabled Athletes. Int J Environ Res Public Health 2021, 18. [CrossRef]
- Rahmati, M.; Shamsi, M.M.; Khoramipour, K.; Malakoutinia, F.; Woo, W.; Park, S.; Yon, D.K.; Lee, S.W.; Shin, J.I.; Smith, L. Baseline physical activity is associated with reduced mortality and disease outcomes in COVID-19: A systematic review and meta-analysis. Rev Med Virol 2022, 32, e2349. [CrossRef]
- Rahmati, M.; Fatemi, R.; Yon, D.K.; Lee, S.W.; Koyanagi, A.; Il Shin, J.; Smith, L. The effect of adherence to high-quality dietary pattern on COVID-19 outcomes: A systematic review and meta-analysis. J Med Virol 2023, 95, e28298. [CrossRef]
- Fikenzer, S.; Fikenzer, K.; Laufs, U.; Falz, R.; Pietrek, H.; Hepp, P. Impact of COVID-19 lockdown on endurance capacity of elite handball players. J Sports Med Phys Fitness 2021, 61, 977-982. [CrossRef]
- Toresdahl, B.G.; Asif, I.M. Coronavirus Disease 2019 (COVID-19): Considerations for the Competitive Athlete. Sports Health 2020, 12, 221-224. [CrossRef]
- Wiśniowski, P.; Cieśliński, M.; Jarocka, M.; Kasiak, P.S.; Makaruk, B.; Pawliczek, W.; Wiecha, S. The Effect of Pressotherapy on Performance and Recovery in the Management of Delayed Onset Muscle Soreness: A Systematic Review and Meta-Analysis. J Clin Med 2022, 11. [CrossRef]
- Colizzi, M.; Peghin, M.; De Martino, M.; Bontempo, G.; Gerussi, V.; Palese, A.; Isola, M.; Tascini, C.; Balestrieri, M. Mental health symptoms one year after acute COVID-19 infection: Prevalence and risk factors. Rev Psiquiatr Salud Ment 2022. [CrossRef]
- Pan, J.; Zhou, K.; Wang, J.; Zheng, Y.; Yu, D.; Kang, H.; Zhang, Y.; Peng, S.; Tung, T.H.; Shen, B. Quality of Life and Mental Health Status in Recovered COVID-19 Subjects at Two Years after Infection in Taizhou, China: A Longitudinal Cohort Study. Brain Sci 2022, 12. [CrossRef]
- Price, S.; Wiecha, S.; Cieśliński, I.; Śliż, D.; Kasiak, P.S.; Lach, J.; Gruba, G.; Kowalski, T.; Mamcarz, A. Differences between Treadmill and Cycle Ergometer Cardiopulmonary Exercise Testing Results in Triathletes and Their Association with Body Composition and Body Mass Index. Int J Environ Res Public Health 2022, 19. [CrossRef]
- Guo, L.; Lin, J.; Ying, W.; Zheng, C.; Tao, L.; Ying, B.; Cheng, B.; Jin, S.; Hu, B. Correlation Study of Short-Term Mental Health in Patients Discharged After Coronavirus Disease 2019 (COVID-19) Infection without Comorbidities: A Prospective Study. Neuropsychiatr Dis Treat 2020, 16, 2661-2667. [CrossRef]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-Arimi, S. Physical and mental health complications post-COVID-19: Scoping review. J Psychosom Res 2021, 147, 110525. [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J Affect Disord 2022, 299, 118-125. [CrossRef]
- Scheer, V.; Valero, D.; Villiger, E.; Rosemann, T.; Knechtle, B. The Impact of the COVID-19 Pandemic on Endurance and Ultra-Endurance Running. Medicina (Kaunas) 2021, 57. [CrossRef]
- Premraj, L.; Kannapadi, N.V.; Briggs, J.; Seal, S.M.; Battaglini, D.; Fanning, J.; Suen, J.; Robba, C.; Fraser, J.; Cho, S.M. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J Neurol Sci 2022, 434, 120162. [CrossRef]
- Fullagar, H.H.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med 2015, 45, 161-186. [CrossRef]
- Ulaszewska, K.; Jodczyk, A.M.; Dlugolecki, P.; Emerla, S.; Stanska, W.; Kasiak, P.S.; Gasior, J.S.; Parol, D.; Mamcarz, A.; Sliz, D. Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population-A Cross-Sectional Survey. Vaccines (Basel) 2022, 10. [CrossRef]
- Kaminsky, L.A.; Arena, R.; Myers, J. Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing: Data From the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc 2015, 90, 1515-1523. [CrossRef]
- Boraita, A.; Díaz-Gonzalez, L.; Valenzuela, P.L.; Heras, M.E.; Morales-Acuna, F.; Castillo-García, A.; Lucia, M.J.; Suja, P.; Santos-Lozano, A.; Lucia, A. Normative Values for Sport-Specific Left Ventricular Dimensions and Exercise-Induced Cardiac Remodeling in Elite Spanish Male and Female Athletes. Sports Med Open 2022, 8, 116. [CrossRef]
- Pluhar, E.; McCracken, C.; Griffith, K.L.; Christino, M.A.; Sugimoto, D.; Meehan, W.P., 3rd. Team Sport Athletes May Be Less Likely To Suffer Anxiety or Depression than Individual Sport Athletes. J Sports Sci Med 2019, 18, 490-496.
- Jodczyk, A.M.; Gruba, G.; Sikora, Z.; Kasiak, P.S.; Gebarowska, J.; Adamczyk, N.; Mamcarz, A.; Sliz, D. PaLS Study: How Has the COVID-19 Pandemic Influenced Physical Activity and Nutrition? Observations a Year after the Outbreak of the Pandemic. International Journal of Environmental Research and Public Health 2021, 18. [CrossRef]
- Jodczyk, A.M.; Kasiak, P.S.; Adamczyk, N.; Gebarowska, J.; Sikora, Z.; Gruba, G.; Mamcarz, A.; Sliz, D. PaLS Study: Tobacco, Alcohol and Drugs Usage among Polish University Students in the Context of Stress Caused by the COVID-19 Pandemic. International Journal of Environmental Research and Public Health 2022, 19. [CrossRef]
- Gruba, G.; Kasiak, P.S.; Gebarowska, J.; Adamczyk, N.; Sikora, Z.; Jodczyk, A.M.; Mamcarz, A.; Sliz, D. PaLS Study of Sleep Deprivation and Mental Health Consequences of the COVID-19 Pandemic among University Students: A Cross-Sectional Survey. International Journal of Environmental Research and Public Health 2021, 18. [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res 2000, 48, 555-560. [CrossRef]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A NEW METHOD FOR DETECTING ANAEROBIC THRESHOLD BY GAS-EXCHANGE. Journal of Applied Physiology 1986, 60, 2020-2027. [CrossRef]
- Sliz, D.; Wiecha, S.; Gasior, J.S.; Kasiak, P.S.; Ulaszewska, K.; Postula, M.; Malek, L.A.; Mamcarz, A. The Influence of Nutrition and Physical Activity on Exercise Performance after Mild COVID-19 Infection in Endurance Athletes-CESAR Study. Nutrients 2022, 14. [CrossRef]
- Sliz, D.; Wiecha, S.; Ulaszewska, K.; Gasior, J.S.; Lewandowski, M.; Kasiak, P.S.; Mamcarz, A. COVID-19 and athletes: Endurance sport and activity resilience study-CAESAR study. Front Physiol 2022, 13, 1078763. [CrossRef]
- Vitale, K.C.; Owens, R.; Hopkins, S.R.; Malhotra, A. Sleep Hygiene for Optimizing Recovery in Athletes: Review and Recommendations. Int J Sports Med 2019, 40, 535-543. [CrossRef]
- Mejri, M.A.; Yousfi, N.; Mhenni, T.; Tayech, A.; Hammouda, O.; Driss, T.; Chaouachi, A.; Souissi, N. Does one night of partial sleep deprivation affect the evening performance during intermittent exercise in Taekwondo players? J Exerc Rehabil 2016, 12, 47-53. [CrossRef]
- Kamdar, B.B.; Kaplan, K.A.; Kezirian, E.J.; Dement, W.C. The impact of extended sleep on daytime alertness, vigilance, and mood. Sleep Med 2004, 5, 441-448. [CrossRef]
- Doherty, R.; Madigan, S.; Warrington, G.; Ellis, J. Sleep and Nutrition Interactions: Implications for Athletes. Nutrients 2019, 11. [CrossRef]
- Rebello, L.J.; Roberts, A.W.; Fenuta, A.M.; Cote, A.T.; Bodner, M.E. Sleep Quality and Sleep Behaviors in Varsity Athletes: A Pilot Study. Front Sports Act Living 2022, 4, 906663. [CrossRef]
- Knufinke, M.; Nieuwenhuys, A.; Geurts, S.A.E.; Coenen, A.M.L.; Kompier, M.A.J. Self-reported sleep quantity, quality and sleep hygiene in elite athletes. J Sleep Res 2018, 27, 78-85. [CrossRef]
- Roche, M.; Sainani, K.; Noordsy, D.; Fredericson, M. The Impacts of COVID-19 on Mental Health and Training in US Professional Endurance Athletes. Clin J Sport Med 2022, 32, 290-296. [CrossRef]
- Tamm, A.L.; Parm, Ü.; Aluoja, A.; Tomingas, T. Changes in the Mental Health Indicators and Training Opportunities for Estonian Elite Athletes Compared to the COVID-19 Isolation Period. Sports (Basel) 2022, 10. [CrossRef]
- Watson, A.; Haraldsdottir, K.; Biese, K.; Schwarz, A.; Hetzel, S.; Reardon, C.; Brooks, M.A.; Bell, D.R.; McGuine, T. Impact of COVID-19 on the physical activity, quality of life and mental health of adolescent athletes: a 2-year evaluation of over 17 000 athletes. Br J Sports Med 2022. [CrossRef]
- Wagemans, J.; Catteeuw, P.; Vandenhouten, J.; Jansen, J.; de Corte, X.; Ceusters, C.; Vissers, D. The Impact of COVID-19 on Physical Performance and Mental Health-A Retrospective Case Series of Belgian Male Professional Football Players. Front Sports Act Living 2021, 3, 803130. [CrossRef]
- Daugherty, S.E.; Guo, Y.; Heath, K.; Dasmariñas, M.C.; Jubilo, K.G.; Samranvedhya, J.; Lipsitch, M.; Cohen, K. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. Bmj 2021, 373, n1098. [CrossRef]
- Petek, B.J.; Moulson, N.; Baggish, A.L.; Kliethermes, S.A.; Patel, M.R.; Churchill, T.W.; Harmon, K.G.; Drezner, J.A.; Investigators, O. Prevalence and clinical implications of persistent or exertional cardiopulmonary symptoms following SARS-CoV-2 infection in 3597 collegiate athletes: a study from the Outcomes Registry for Cardiac Conditions in Athletes (ORCCA). Br J Sports Med 2022, 56, 913-918. [CrossRef]
- Al-Aly, Z.; Xie, Y.; Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021, 594, 259-264. [CrossRef]
- Augustin, M.; Schommers, P.; Stecher, M.; Dewald, F.; Gieselmann, L.; Gruell, H.; Horn, C.; Vanshylla, K.; Cristanziano, V.D.; Osebold, L.; et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg Health Eur 2021, 6, 100122. [CrossRef]
- Liu, K.; Chen, Y.; Wu, D.; Lin, R.; Wang, Z.; Pan, L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract 2020, 39, 101132. [CrossRef]
- Lindsay, R.K.; Wilson, J.J.; Trott, M.; Olanrewaju, O.; Tully, M.A.; López-Sánchez, G.F.; Shin, J.I.; Pizzol, D.; Allen, P.; Butler, L.T.; et al. What are the recommendations for returning athletes who have experienced long term COVID-19 symptoms? Ann Med 2021, 53, 1935-1944. [CrossRef]
- Kasiak, P.S.; Adamczyk, N.; Jodczyk, A.M.; Kaproń, A.; Lisowska, A.; Mamcarz, A.; Śliż, D. COVID-19 Pandemic Consequences among Individuals with Eating Disorders on a Clinical Sample in Poland-A Cross-Sectional Study. Int J Environ Res Public Health 2022, 19. [CrossRef]
- Selimbegović, L.; Dupuy, O.; Terache, J.; Blandin, Y.; Bosquet, L.; Chatard, A. Evaluative Threat Increases Effort Expenditure in a Cycling Exercise: An Exploratory Study. J Sport Exerc Psychol 2020, 1-8. [CrossRef]
- Solberg, E.E.; Ingjer, F.; Holen, A.; Sundgot-Borgen, J.; Nilsson, S.; Holme, I. Stress reactivity to and recovery from a standardised exercise bout: a study of 31 runners practising relaxation techniques. Br J Sports Med 2000, 34, 268-272. [CrossRef]
- Nien, J.T.; Wu, C.H.; Yang, K.T.; Cho, Y.M.; Chu, C.H.; Chang, Y.K.; Zhou, C. Mindfulness Training Enhances Endurance Performance and Executive Functions in Athletes: An Event-Related Potential Study. Neural Plast 2020, 2020, 8213710. [CrossRef]
Table 1.
CPET Performance.
Table 1.
CPET Performance.
| Variable |
Pre-COVID-19 |
Post-COVID-19 |
p-value |
| Weight (kg) |
76.6 (10.0) |
76.7 (10.9) |
0.951 |
| BMI (kg·m-2) |
24.0 (2.5) |
24.0 (2.7) |
0.931 |
| Lean mass (kg) |
63.4 (7.6) |
63.5 (8.0) |
0.774 |
| BF (%) |
17.1 (4.7) |
16.9 (5.1) |
0.604 |
| Fat mass (kg) |
13.3 (4.7) |
13.2 (5.2) |
0.848 |
| VO2AT (ml·kg·min-1) |
35.0 (6.5) |
32.4 (6.0) |
<0.001 |
| VO2Ata (ml·min-1) |
2650.0 (470.9) |
2446.1 (400.3) |
<0.001 |
| HRAT (beats·min-1) |
145.1 (10.9) |
141.1 (10.1) |
0.001 |
| VEAT (l·min-1) |
70.8 (18.7) |
68.1 (14.7) |
0.090 |
| SAT (km·h-1) |
11.4 (1.4) |
11.1 (1.3) |
0.044 |
| PAT (Watts) |
162.8 (25.9) |
154.8 (25.9) |
0.066 |
| fRAT (breaths·min-1) |
32.1 (9.0) |
32.1 (8.1) |
0.706 |
| LacAT (mmol·L-1) |
2.0 (0.9) |
2.1 (0.9) |
0.630 |
| VO2RCP (ml·kg·min-1) |
43.9 (7.4) |
40.5 (6.7) |
<0.001 |
| VO2RCPa (ml·min-1) |
3324.3 (512.9) |
3063.7 (440.1) |
<0.001 |
| HRRCP (beats·min-1) |
168.8 (9.2) |
165.1 (9.8) |
<0.001 |
| VERCP (l·min-1) |
106.8 (21.7) |
98.9 (18.3) |
<0.001 |
| SRCP (km·h-1) |
14.3 (1.9) |
13.8 (1.5) |
<0.001 |
| PRCP (Watts) |
245.2 (42.0) |
232.2 (39.7) |
0.061 |
| fRRCP (breaths·min-1) |
41.3 (8.7) |
40.1 (8.9) |
0.876 |
| LacRCP (mmol·L-1) |
4.9 (1.4) |
4.3 (1.1) |
0.013 |
| VO2max (ml·kg·min-1) |
47.8 (8.0) |
45.0 (7.1) |
<0.001 |
| VO2maxa (ml·min-1) |
3623.5 (552.1) |
3406.0 (474.5) |
<0.001 |
| HRmax (beats·min-1) |
180.8 (10.1) |
179.8 (10.0) |
0.273 |
| VEmax (l·min-1) |
143.0 (26.9) |
138.50 (23.9) |
0.068 |
| Smax (km·h-1) |
16.6 (1.6) |
16.4 (1.7) |
0.264 |
| Pmax (Watts) |
310.0 (37.2) |
312.2 (49.1) |
0.811 |
| fRmax (breaths·min-1) |
58.9 (14.4) |
57.3 (11.0) |
0.959 |
| Lacmax (mmol·L-1) |
9.7 (2.3) |
9.6 (2.4) |
0.880 |
| VO2AT (ml·kg·min-1) |
35.0 (6.5) |
32.4 (6.0) |
<0.001 |
Table 2.
Results of answers to questions related to sleep.
Table 2.
Results of answers to questions related to sleep.
| Question |
Answer type |
Lack of answer |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
| >Sleep induction |
No problem |
Slightly delayed |
Markedly delayed |
Very delayed or did not sleep at all |
2 (4.1) |
| 22 (44,9) |
16 (32.7) |
7 (14.3) |
2 (4.1) |
| >Awakenings during the night |
No problem |
Minor problem |
Considerable problem |
Serious problem or did not sleep at all |
2 (4.1) |
8 (16.3)
71.4 for HRRCP
|
27 (55.1)
55.1 for HRRCP
|
12 (24.5)
99.9 for HRRCP
|
0 (0.0) |
| >Final awakening |
Not earlier |
A little earlier |
Markedly earlier |
Much earlier or did not sleep at all |
3 (6.1) |
| 28 (57.1) |
15 (30.6) |
3 (6.1) |
0 (0.0) |
| >Total sleep duration |
Sufficient |
Slightly insufficient |
Markedly insufficient |
Very insufficient or did not sleep at all |
2 (4.1) |
19 (38.8)
30.4 for VERCP
29.2 for fRRCP
24.9 for LacRCP
|
25 (51.0)
18.5 for VERCP
20.4 for fRRCP
13.9 for LacRCP
|
3 (6.1)
29.7 for VERCP
21.3 for fRRCP
18.0 for LacRCP
|
0 (0.0) |
| >Sleep quality |
Satisfactory |
Slightly unsatisfactory |
Markedly unsatisfactory |
Very unsatisfactory or did not sleep at all |
2 (4.1) |
22 (44.9)
27.2 for SRCP/PRCP
29.4 for VO2RCPa
29.2 for VO2RCP
29.1 for VERCP
27.6 for VO2max
27.5 for VO2maxa
27.3 for HRmax
25.9 for VEmax
|
22 (44.9)
19.3 for SRCP/PRCP
17.6 for VO2RCPa
18.0 for VO2RCP
18.3 for VERCP
18.8 for VO2max
18.6 for VO2maxa
19.4 for HRmax
19.8 for VEmax
|
3 (6.1)
35.3 for SRCP/PRCP
31.3 for VO2RCPa
28.7 for VO2RCP
28.7 for VERCP
35.3 for VO2maxa
38.0for VO2maxa
33.8 for HRmax
40.7 for VEmax
|
0 (0.0) |
| >Well-being during the day |
Normal |
Slightly decreased |
Markedly decreased |
Very decreased |
2 (4.1) |
28 (57.1)
27.8 for SRCP/PRCP
28.3 for Smax/Pmax
|
19 (38.8)
18.5 for SRCP/PRCP
17.6 for Smax/Pmax
|
0 (0.0) |
0 (0.0) |
| >Functioning capacity during the day |
Normal |
Slightly decreased |
Markedly decreased |
Very decreased |
3 (6.1) |
| 26 (53.1) |
19 (38.8) |
1 (2.0) |
0 (0.0) |
| >Sleepiness during the day |
None |
Mild |
Considerable |
Intense |
2 (4.1) |
| 5 (10.2) |
28 (57.1) |
13 (26.5) |
1 (2.0) |
| What hour did you usually get out of bed in the morning |
7.1 (2.5) |
4 (8.2) |
| Hours of actual sleep per night |
6.8 (1.0) |
|
| Hours spend in front of the screen of devices emitting blue light per day |
7.0 (2.9) |
3 (6.1) |
| Self-assessed impact of COVID-19 pandemic and imposed restrictions sleep (in -5/0/+5 scale) |
0.4 (1.3) |
2 (4.1) |
Table 3.
Results of answers to questions related to mental health.
Table 3.
Results of answers to questions related to mental health.
| Question |
Answer type |
Lack of answer |
| I did not try this method |
I used it in my everyday life, but only to a small extent |
I used this method often, or it was one of the basic methods to cope with COVID-19 induced stress |
I used this method regularly |
|
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
| I wanted to return to work and duties as soon as possible to stop thinking about my illness |
24 (49.0) |
8 (16.3) |
4 (8.2) |
11 (22.4) |
2 (4.1) |
| I was concentrating very hard on the situation I found myself in |
27 (55.1) |
11 (22.4) |
0 (0.0) |
8 (16.3) |
3 (6.1) |
| I told myself „It can’t be true that I am infected with COVID-19” |
41 (83.7) |
4 (8.2) |
0 (0.0) |
1 (2.0) |
0 (0.0) |
| I used alcohol or other stimulants to improve my mood |
37 (75.5) |
7 (14.3) |
1 (2.0) |
1 (2.0) |
3 (6.1) |
| I gave up after trying to cope with the whole situation |
42 (85.7) |
1 (2.0) |
3 (6.1) |
0 (0.0) |
3 (6.1) |
| I was looking for support from family, friends and other people |
33 (67.3) |
8 (16.3) |
1 (2.0) |
4 (8.2) |
3 (6.1) |
| I undertook activities to improve my situation by expanding my knowledge about COVID-19 |
17 (34.7)
24.9 for lean mass |
13 (26.5)
15.4 for lean mass |
3 (6.1)
35.0 for lean mass |
13 (26.5)
27.2 for lean mass |
3 (6.1) |
| I was looking for positives in the situation I found myself in |
12 (24.5) |
7 (14.3) |
8 (16.3) |
19 (38.8) |
3 (6.1) |
| I criticized myself for not taking precautions enough, which resulted in COVID-19 infection |
40 (81.6) |
6 (12.2) |
0 (0.0) |
0 (0.0) |
3 (6.1) |
| I tried to joke about the COVID-19 infection |
18 (36.7)
27.7 for HRAT
25.6 for VO2RCP
27.3 for VERCP
24.9 for VO2max
26.3 for VO2maxa
|
11 (22.4)
23.5 for HRAT
28.5 for VO2RCP
22.5for VERCP
28.6 for VO2max
28.0 for VO2maxa
|
4 (8.2)
41.5 for HRAT
30.3 for VO2RCP
34.3 for VERCP
30.3 for VO2max
31.3 for VO2maxa
|
13 (26.5)
15.2 for HRAT
14.3 for VO2RCP
15.8 for VERCP
15.1 for VO2max
13.5 for VO2maxa
|
3 (6.1) |
| I quickly accepted the state I was in |
3 (6.1) |
7 (14.3) |
20 (40.8) |
16 (32.7) |
3 (6.1) |
| I expressed my negative emotions expressively by screaming loudly or arguing with others |
37 (75.5)
20.4 for VEAT
|
7 (14.3)
34.4 for VEAT
|
1 (2.0)
44.0 for VEAT
|
1 (2.0)
42.0 for VEAT
|
3 (6.1) |
| I tried to improve my mood through religious practices or meditation relaxation techniques |
35 (71.4)
22.3 for Smax/Pmax
23.0 for VO2max
13.7 for Lacmax
|
6 (12.2)
35.8 for Smax/Pmax
34.2 for VO2max
21.7 for Lacmax
|
0 (0.0) |
5 (10.2)
17.2 for Smax/Pmax
14.4 for VO2max
7.8 for Lacmax
|
3 (6.1) |
| Self-assessed impact of COVID-19 pandemic and imposed restrictions mental health (in -5/0/+5 scale) |
0.6 (1.8) |
2 (4.1) |
Table 4.
Relationships between sleep, mental health and CPET performance.
Table 4.
Relationships between sleep, mental health and CPET performance.
| CPET variable |
Survey question |
p-value |
| Part A. Sleep |
| HRRCP
|
Awakenings during the night |
0.028 |
| VERCP
|
Total sleep duration |
0.013 |
| fRRCP
|
Total sleep duration |
0.010 |
| LacRCP
|
Total sleep duration |
0.013 |
| SRCP/PRCP
|
Sleep quality |
0.046 |
| VO2RCPa
|
Sleep quality |
0.011 |
| VO2RCP
|
Sleep quality |
0.018 |
| VERCP
|
Sleep quality |
0.027 |
| VO2max
|
Sleep quality |
0.034 |
| VO2maxa
|
Sleep quality |
0.019 |
| HRmax
|
Sleep quality |
0.070 |
| VEmax
|
Sleep quality |
0.032 |
| SRCP/PRCP
|
Well-being during the day |
0.023 |
| Smax/Pmax
|
Well-being during the day |
0.007 |
| Part B. Mental health |
| Lean mass |
Undertaking activities to improve one’s situation |
0.042 |
| HRAT
|
Joking about the COVID-19 infection |
0.042 |
| VO2RCP
|
Joking about the COVID-19 infection |
0.029 |
| VERCP
|
Joking about the COVID-19 infection |
0.041 |
| VO2max
|
Joking about the COVID-19 infection |
0.047 |
| VO2maxa
|
Joking about the COVID-19 infection |
0.014 |
| VEAT
|
Expressing negative emotions expressively |
0.012 |
| Smax/Pmax
|
Improving mood through religious practices or meditation relaxation techniques |
0.033 |
| VO2max
|
Improving mood through religious practices or meditation relaxation techniques |
0.046 |
| Lacmax
|
Improving mood through religious practices or meditation relaxation techniques |
0.045 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).