1. Introduction
Acute Appendicitis (AA) has an incidence of 1 new case per 100 people per year, and is the most common surgical emergency worldwide [
1]. The risk of AA in males is approximately 1.3 times higher than in females [
2], with peak incidence in the age range of 10 -19 years [
3]. Despite the absence of any known causative gene, its occurrence is roughly three times higher in people with a family history of appendicitis [
4]. AA may be caused due to obstruction of appendiceal lumen by fecolith, lymphoid hyperplasia, impacted stool, tumours or other mechanical aetiologies, and the causes vary in different age groups [
4]. Obstruction of appendiceal orifice results in an increase in intraluminal and intramural pressure which leads to vessel occlusion and lymphatic stasis. The obstructed appendix is then filled with mucus which further worsens the vascular compromise, facilitating the overgrowth of aerobic and anaerobic bacteria. The inflammation can potentially progress to localised ischemia, abscess, perforation and eventual peritonitis [
5]. The standard treatment procedure for AA is an emergency surgery, with a preference for laparoscopic appendectomy over open appendectomy. Although the procedures pose high success rates, the associated risks and complications such as need for reoperation, infection of the surgical site and bowel obstruction often follow [
6].
Appendix was previously believed to be a vestigial organ attached dorso - medially to the end of the caecum, with dubious functions due to its inferior size as compared to the homologues of other primates. However, recent studies have established the importance of the vermiform appendix and its immunological action, as the appendix acts as a reservoir of commensal intestinal flora and as a site for host - symbiotic bacteria interaction. The study also suggests a possibility that the appendix might have developed ahead of caecum, implying that the immunological importance was established before the digestive one [
7]. Thus, retaining the appendix might serve in replenishing the gut microbiota following its depletion due to causes such as antibiotic treatment, lifestyle changes and dietary imbalances.
During the global pandemic of COVID-19, a state of emergency led people across the world to stay at home to stop the spread of the virus. Further, people were advised to visit hospitals only in cases of COVID-19 related illnesses and non - COVID emergencies. Studies observed a decline in the number of patients visiting the hospitals due to the fear of COVID infection, leading to a significant rise in the number of complicated cases of appendicitis, and usage of non-surgical methods of intervention for various conditions, including antibiotic treatment for appendicitis [
8], [
9].
We present a case of AA associated with COVID 19, successfully managed with individualized classical homeopathy where complete resolution of the condition was observed.
2. Case report
This report describes the case of a 9 year and 10 months old female patient who developed AA.
2.1. Case Presentation
23 January 2022
The patient developed a fever of 39°C with chills (pulse unrecorded), headache at the root of the nose, barking cough, redness of both the cheeks, vertigo, and drowsiness.
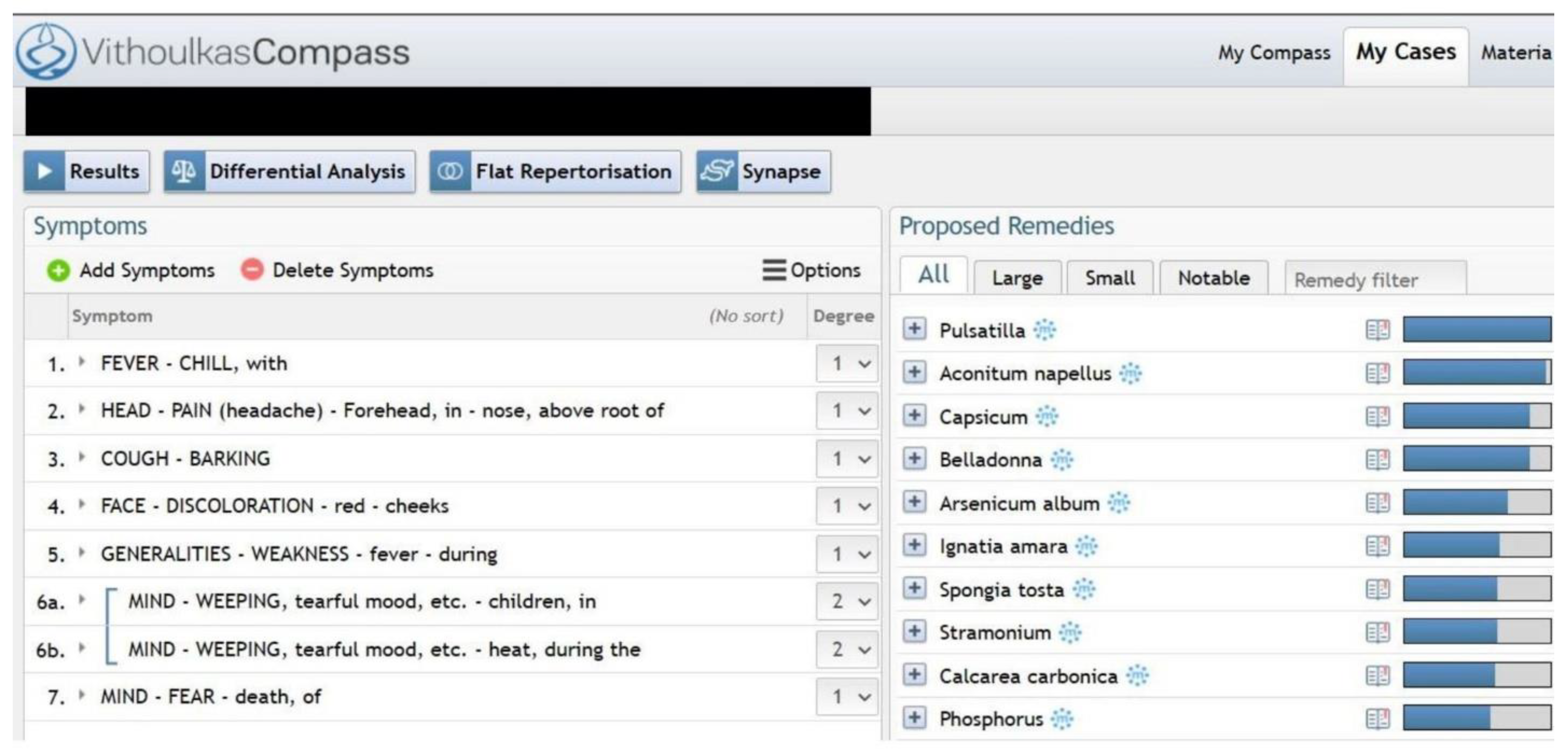
The child was in a teary mood and sought constant care and attention from her parents since the onset of the fever. When inquired about why she was teary, she explained that she was scared of dying. Homeopathic repertorisation of the case at first intake is presented in
Fig. 1.
2.1.1. Past medical history
An episode of acute bronchitis and pneumonia that required antibiotic and inhalant steroids at the age of 5 years, an episode of acute bronchitis at the age of 6 years. 4 – 5 episodes of febrile upper respiratory tract infections between the ages 4 -7 years, and recurrent styes between the ages 4-6 years.
2.1.2. Family history
The patient’s father had allergic bronchitis, and the mother had urticaria and allergic rhinitis. The maternal grandfather died of lung cancer; paternal grandfather had skin cancer and grandmother suffered from systemic lupus erythematosus and psoriatic arthritis.
2.2. Prescription:
Based on the totality of symptoms presented in the acute febrile illness, she was prescribed a single dose of Pulsatilla nigricans 200 CH.
2.4. 24 January 2022
The patient did not present any symptoms of febrile illness, and her mood was better. The fever did not recur.
2.5. 25 January 2022
The patient tested positive for COVID-19 when she was subjected to Reverse transcription polymerase chain reaction (RT-PCR) as per the protocol, as her parents tested positive for the same. The patient did not develop any fever, cough or other COVID related respiratory symptoms.
On the same day, she developed progressing pain in the right lower quadrant of the abdomen, associated with nausea at the sight of food, complete anorexia, and two episodes of projectile vomiting.
The child wanted to pass flatus or stools as she felt the pain would ameliorate by doing so but could not succeed despite exerting pressure. The mother, a paediatrician herself, examined the child at home.
Local examination: Local tenderness +, Guarding +, Rebound tenderness (Positive Blumberg sign) +.
2.6. Reports
Laboratory findings revealed white blood cell was 10150 cells/ uL (NV 4.5 - 11,000 cells/uL), Neutrophils - 88.8% (NV - 40 - 60%), Lymphocytes - 7.4%, N/L ratio - 12 (NV - 0.78 - 3.53). CRP was 4.85mg/dL (NV - <6mg/dL).
*NV - Normal Value
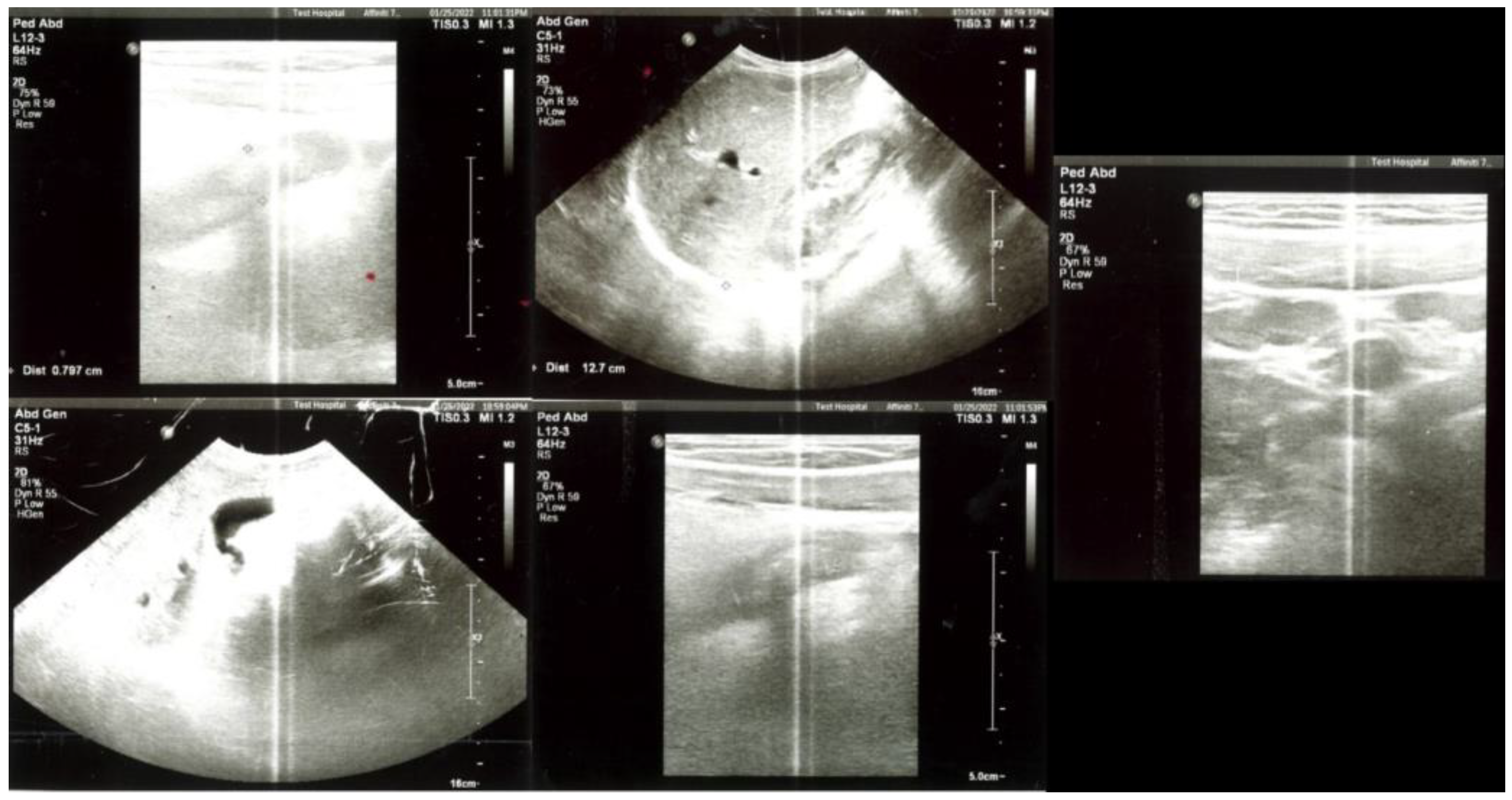
Abdominal Ultrasonography (USG) revealed an aperistaltic uncompressed segment reaching 7.6 mm in diameter in the peri-caecal area in the right lower quadrant of the abdomen, with an increase in echogenicity and minimal free fluid in the form of smearing in the adjacent omental tissue. Numerous well-circumscribed hypoechoic mesenteric lymph nodes, the largest of which was 15x9mm in size, were observed in the mesenteric area in the right lower quadrant of the abdomen (
Fig. 2).
Appendicitis Inflammatory Response (AIR) Score
: The AIR score based on the symptoms and laboratory findings were 9/12 [
10]
2.7. Diagnosis
U07.1 - COVID-19, virus identified; with
K35.8 - Acute appendicitis without mention of localized or generalized peritonitis. [
11]
Prescription
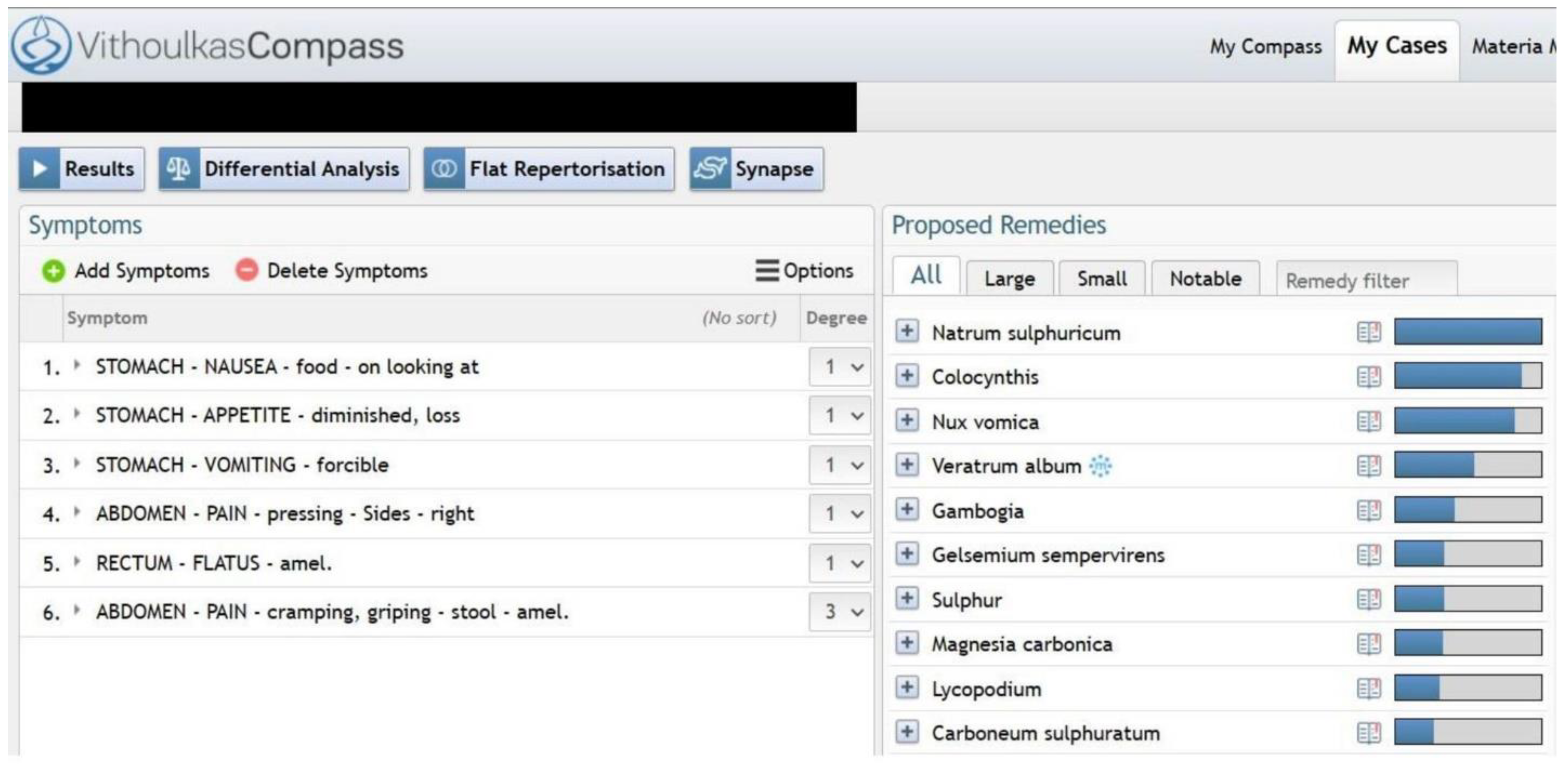
Based on the totality of the symptoms presented during the episode of appendicitis (repertorisation in
Fig. 3), she was prescribed
Natrum Sulphuricum 200CH, one dose.
2.9. Follow up
2.9.1. 25 January 2022
After the remedy, the patient was able to sleep for about an hour, following which her appetite improved and she started to feel better. She was able to consume food without feeling nauseated, and the abdominal pain decreased.
On auscultation, bowel sounds had increased, and she was able to pass flatus with ease within three hours.
2.9.2. 26 January 2022
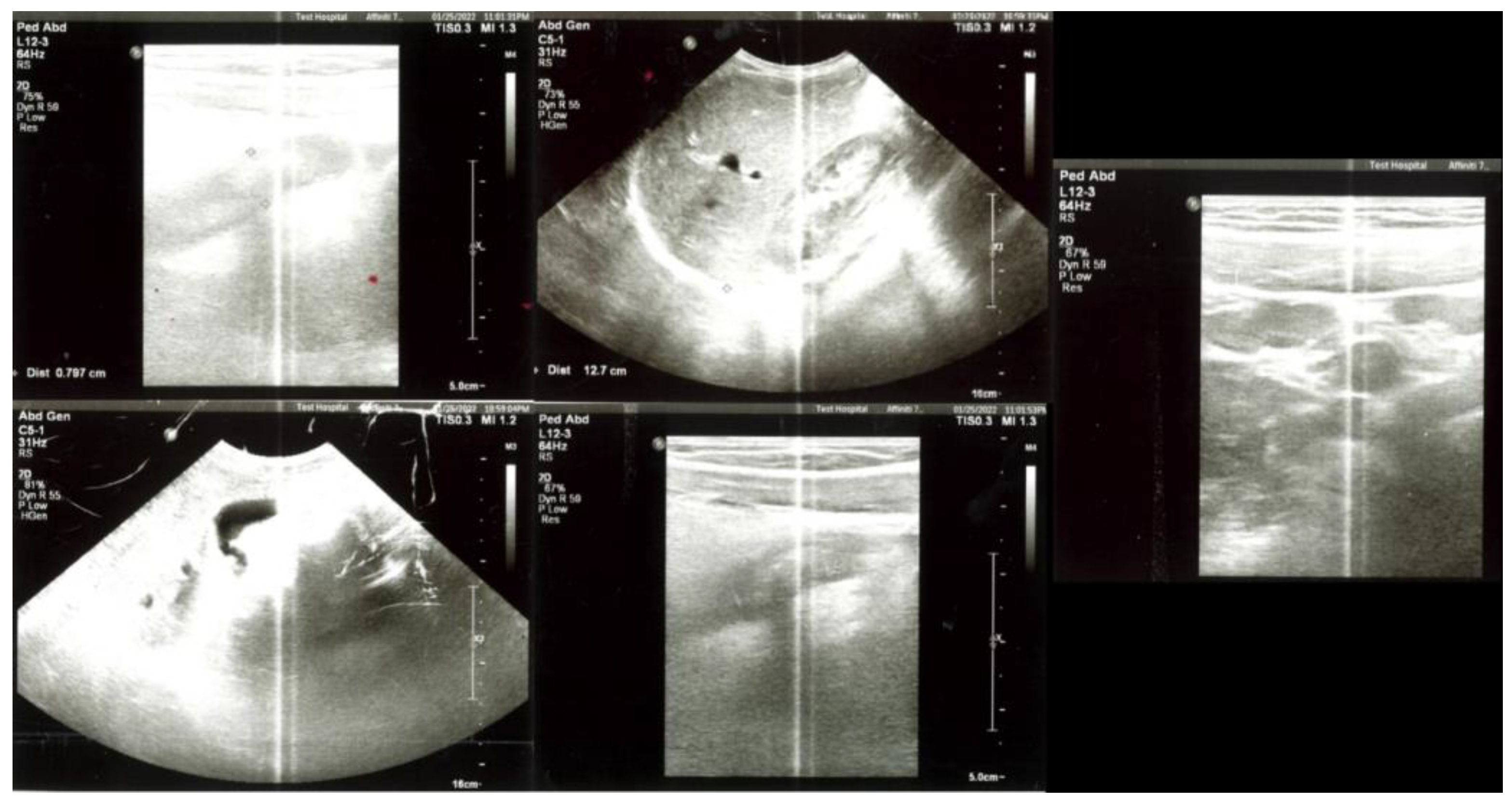
Abdominal USG revealed a hypoechoic tubular structure with a diameter of about 8.8 mm that does not change shape with compression, which is significant in terms of AA, as a diameter > 5.7 mm is an optimal criteria in diagnosing AA in children [
12]. A remarkable increase in inflammatory oedematous echo in adjacent mesenteric fat planes and free fluid was also noted in the right lower quadrant (
Fig. 4)
Laboratory reports revealed white blood cell - 5200 cells/ uL (NV 4.5 - 11,000 cells/uL), Neutrophils - 66.7% (NV - 40 - 60%), Lymphocytes - 25%, N/L ratio - 2.66 (NV - 0.78 - 3.53). CRP was 64.53mg/L (NV - <6 mg/dL).
Emergency appendectomy was advised for the patient, but as the pain and discomfort progressively decreased, the parents refused the surgical intervention. The child’s energy continued to increase, and she gained back her appetite. Defecation and flatulence ameliorated her complaints further, which she was able to perform with ease.
2.9.3. 28 January 2022
The patient had no complaints of abdominal pain, discomfort, constipation, or difficulty in passing flatus. Her appetite and energy were normal and she was able to perform her day-to-day activities with ease.
2.9.4. 26 February 2022
Control abdominal USG revealed an appendix of diameter 4.2 mm (NV 4.2–12.8 mm) [
13], and several lymph nodes in the mesenteric area, the largest of which is approximately 14mm in diameter, were observed (
Fig. 5). No inflammatory signs of the appendix were noted in the control abdominal USG.
3. Discussion
The CoVID-19 pandemic was deleterious to the global population, especially in terms of healthcare. Strict restriction policies were implemented to control the spread of the infection of SARS-CoV-2 virus, and it was encouraged that only cases with utmost severity seek emergency medical care. This led to a significant decline in the number of people visiting the hospital even for severe illnesses such as myocardial infarctions, cerebrovascular accidents, and surgical cases such as acute appendicitis due to fear of infection. Additionally, there was also a rise in the number of complications such as peritonitis and perforation in progressed appendicitis [
8].
There was a minority of patients who developed gastrointestinal manifestations associated with COVID-19 infection besides self-limiting symptoms such as nausea, vomiting, diarrhoea and anorexia, such as acute pancreatitis, AA, intestinal obstruction, bowel ischaemia, haemoperitoneum, and abdominal compartment syndrome. These manifestations were theorised to be due to - one: direct viral injury, two: cytokine storm, inflammatory immune responses, three: alteration in gut bacteria due to imbalance in gut secretions, acute hypoxia, and dysbiosis due to infection of the lung [
14]. Further, viral infections of the lung modify the gut microbiota composition and brings about a more pro-inflammatory state through actively functioning gut-lung axis. Such dysregulation is likely to make the patient susceptible to inflammatory diseases of the gut [
15].
In this case, the patient developed AA while she simultaneously tested positive for COVID-19 infection. Although she presented with fever two days prior to the development of abdominal pain and COVID–19, she did not have breathlessness, cough and other COVID related respiratory symptoms, which makes it difficult to confirm or deny the direct corelation between COVID infection and the development of acute appendicitis.
However, previous studies have shown the association between the two, as viral infections could cause lymphoid hyperplasia of the appendix, leading to appendix obstruction, ulceration of the mucosa, resulting in secondary bacterial infection of the appendix. Still, a relation between COVID-19 infection and development of AA is yet to be established [
16].
Initially, in this case, the patient’s blood report showed a high neutrophil-to-lymphocyte ratio (NLR) of 12 suggestive of a strong bacterial infective state, and less likely a viral infection [
17]. Considering that NLR > 8 is independently predictive of complicated appendicitis [
18], we can deduce that the girl is likely to have suffered from acute complicated bacterial appendicitis.
Homeopathic interventions have previously been recorded to be beneficial in treating chronic and debilitating conditions, but a little to no scientific studies are available on treating AA. The studies available on treating COVID-19 associated appendicitis are minimal, and have recorded the usage on conventional therapies for treating the same [
14,
17,
19]. Conventionally, the symptoms of malaise, tiredness and sickness-related-depression are given little to no consideration in terms of treatment, despite studies proving that they are not symptoms caused due to the infection per-se, but is a strategically organized effort of the neuroendocrine system to combat the infection [
20]. In contrast, homeopathy considers symptoms of the illness presented on mental, emotional and physical planes, thus providing a wholistic approach at sickness and health [
21]. Apart from complete resolution of the initial fever, or the appendicitis that followed, the child was also relieved of alteration of her emotional state during the fever. Additionally, a significant decline in the NLR (2.66) was observed, and the follow-up abdominal USG were also suggestive of complete resolution of acute appendicitis. Although, in this case, the patient was in contact care of a paediatrician, and an early detection and timely intervention worked in the favour of resolution of AA without its due progression to further complications.
It is noteworthy that AA was managed without any conventional medicinal intervention.
The Modified Naranjo Criteria for Assessing Causal Attribution of Clinical Outcome to Homeopathic Intervention (MONARCH) score was assessed to be 8 [
22]. (Table 1)
| The Modified Naranjo Criteria for Homeopathy (MONARCH) |
Y |
N |
Not sure/NA |
Score in case |
| 1. Was there an improvement in the main symptom or condition for which the homeopathic medicine was prescribed? |
2 |
-1 |
0 |
2 |
| 2. Did the clinical improvement occur within a plausible time frame relative to drug intake? |
1 |
-2 |
0 |
1 |
| 3. Was there an initial aggravation of symptoms? |
1 |
0 |
0 |
0 |
| 4. Did the effect encompass more than the main symptom or condition, i.e., were other symptoms ultimately improved or changed? |
1 |
0 |
0 |
1 |
| 5. Did overall well-being improve? |
1 |
0 |
0 |
1 |
| 6. (A) Direction of cure: did some symptoms improve in the opposite order of the development of symptoms of the disease? |
1 |
0 |
0 |
0 |
| 6. (B) Direction of cure: did at least two of the following aspects apply to the order of improvement of symptoms:–from organs of more importance to those of less importance? –from deeper to more superficial aspects of the individual? –from the top downwards? |
1 |
0 |
0 |
0 |
| 7. Did “old symptoms” (defined as non-seasonal and non-cyclical symptoms that were previously thought to have resolved) reappear temporarily during the course of improvement? |
1 |
0 |
0 |
0 |
| 8. Are there alternate causes (other than the medicine) that—with a high probability— could have caused the improvement? (Consider known course of disease, other forms of treatment, and other clinically relevant interventions) |
-3 |
1 |
0 |
1 |
| 9. Was the health improvement confirmed by any objective evidence? (e.g., laboratory test, clinical observation, etc.) |
2 |
0 |
0 |
0 |
| 10. Did repeat dosing, if conducted, create similar clinical improvement? |
1 |
0 |
0 |
0 |
| total |
|
|
|
8 |
5. Conclusions
Individualised classical homeopathy was beneficial in managing acute appendicitis associated with COVID-19 infection in a girl of 9 years. The condition, though exhibiting signs of severe infection resolved in 2 days avoiding the need for the otherwise recommended surgical excision. Further scientific studies, especially in hospital set ups are needed to investigate the role of individualised classical homeopathy in treating similar severe acute infections.
Author Contributions
Conceptualization, S.M., and M.M; resources, E.E., and M.M.; data curation, P.D.; writing—original draft preparation, P.D.; writing—review and editing, P.D., S.M.; supervision, G.V.; project administration, G.V, S.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient’s guardian to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix B
Figure 1: Homeopathic repertorisation of symptoms as on 23, January 2022
Figure 2: USG abdomen as on 25, January 2022.
Figure 3: Homeopathic repertorisation of symptoms as on 25, January 2022
Figure 4: USG abdomen as on 26, January 2022.
Figure 5: Control abdominal USG taken on 26 February 2022
Table 1: Modified Naranjo Criteria for Assessing Causal Attribution of Clinical Outcome to Homeopathic Intervention
References
- P. Téoule, J. de Laffolie, U. Rolle, and C. Reissfelder, “Acute Appendicitis in Childhood and Adulthood,” Dtsch Arztebl Int, vol. 117, no. 45, pp. 764–774, Nov. 2020. [CrossRef]
- M. Albahadili, “Study of the effect of age, gender and seasonal variation on appendicitis in Azizyah-Iraq,” vol. 8, Jul. 2016.
- M. Wagner, D. J. Tubre, and J. A. Asensio, “Evolution and Current Trends in the Management of Acute Appendicitis,” Surg Clin North Am, vol. 98, no. 5, pp. 1005–1023, Oct. 2018. [CrossRef]
- Bhangu, K. Søreide, S. Di Saverio, J. H. Assarsson, and F. T. Drake, “Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management,” Lancet, vol. 386, no. 10000, pp. 1278–1287, Sep. 2015. [CrossRef]
- M. W. Jones, R. A. Lopez, and J. G. Deppen, “Appendicitis,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2022. Accessed: Jan. 29, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK493193/.
- J. J. López, K. J. Deans, and P. C. Minneci, “Nonoperative management of appendicitis in children,” Curr Opin Pediatr, vol. 29, no. 3, pp. 358–362, Jun. 2017. [CrossRef]
- A. Kooij, S. Sahami, S. L. Meijer, C. J. Buskens, and A. A. te Velde, “The immunology of the vermiform appendix: a review of the literature,” Clin Exp Immunol, vol. 186, no. 1, pp. 1–9, Oct. 2016. [CrossRef]
- G. Orthopoulos et al., “Increasing incidence of complicated appendicitis during COVID-19 pandemic,” Am J Surg, vol. 221, no. 5, pp. 1056–1060, May 2021. [CrossRef]
- “Changes in appendicitis treatment during the COVID-19 pandemic – A systematic review and meta-analysis - PMC.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8539829/ (accessed Jan. 29, 2023).
- B. VON-MÜHLEN, O. FRANZON, M. G. BEDUSCHI, N. KRUEL, and D. LUPSELO, “AIR SCORE ASSESSMENT FOR ACUTE APPENDICITIS,” Arq Bras Cir Dig, vol. 28, no. 3, pp. 171–173, 2015. [CrossRef]
- “ICD-10 Version:2019.” https://icd.who.int/browse10/2019/en (accessed Jan. 29, 2023).
- N. H. Park, H. E. Oh, H. J. Park, and J. Y. Park, “Ultrasonography of normal and abnormal appendix in children,” World J Radiol, vol. 3, no. 4, pp. 85–91, Apr. 2011. [CrossRef]
- Willekens, E. Peeters, M. De Maeseneer, and J. de Mey, “The Normal Appendix on CT: Does Size Matter?,” PLoS One, vol. 9, no. 5, p. e96476, May 2014. [CrossRef]
- C. Kariyawasam, U. Jayarajah, R. Riza, V. Abeysuriya, and S. L. Seneviratne, “Gastrointestinal manifestations in COVID-19,” Trans R Soc Trop Med Hyg, p. trab042, Mar. 2021. [CrossRef]
- “The Gut-Lung Axis in Health and Respiratory Diseases: A Place for Inter-Organ and Inter-Kingdom Crosstalks - PMC.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7042389/ (accessed Jan. 29, 2023).
- V. E. Georgakopoulou et al., “COVID-19-associated acute appendicitis in adults. A report of five cases and a review of the literature,” Experimental and Therapeutic Medicine, vol. 24, no. 1, pp. 1–9, Jul. 2022. [CrossRef]
- Naess, S. S. Nilssen, R. Mo, G. E. Eide, and H. Sjursen, “Role of neutrophil to lymphocyte and monocyte to lymphocyte ratios in the diagnosis of bacterial infection in patients with fever,” Infection, vol. 45, no. 3, pp. 299–307, 2017. [CrossRef]
- S. Hajibandeh, S. Hajibandeh, N. Hobbs, and M. Mansour, “Neutrophil-to-lymphocyte ratio predicts acute appendicitis and distinguishes between complicated and uncomplicated appendicitis: A systematic review and meta-analysis,” Am J Surg, vol. 219, no. 1, pp. 154–163, Jan. 2020. [CrossRef]
- “Can COVID 19 present like appendicitis? - ScienceDirect.” https://www.sciencedirect.com/science/article/pii/S2214250920301682 (accessed Jan. 29, 2023).
- “Cytokine, Sickness Behavior, and Depression - PMC.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740752/ (accessed Jan. 29, 2023).
- S. Hahnemann, Organon of Medicine. B. Jain Publishers, 2002.
- C. D. Lamba et al., “Evaluation of the Modified Naranjo Criteria for Assessing Causal Attribution of Clinical Outcome to Homeopathic Intervention as Presented in Case Reports,” Homeopathy, vol. 109, no. 4, pp. 191–197, Nov. 2020. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).