Background
Lumbar spinal stenosis (LSS) is evident radiographically in 19-47% of the population ≥60 years old[
1] and clinically symptomatic in about 10%[
2]. Decompression surgery is indicated for patients with moderate-to-severe symptoms refractory to conservative treatment[
3,
4].
Many surgical techniques for decompression are available ranging from traditional open complete laminectomy, through "mini-open" partial laminotomy, to different minimally invasive surgeries (MIS)[
5]. While the literature is not conclusive regarding the superiority of the MIS techniques versus the open techniques, there is an inclination towards the former due to less operative complications and better patient satisfaction[
5,
6,
7].
When performing decompression due to LSS, the main complications reported are; incidental Dural tear (4-9%)[
4,
8,
9]; deep wound infection (~1-2%)[
8,
10]; and neurological injury (<1%)[
3]. Some studies mention disc herniation as a post-decompression complication[
11,
12,
13,
14] but fail to distinguish its rate between the different surgical techniques. In our opinion, disc herniation, though rare, present a complication worthy of mention due to its clinical implications.
In open laminectomy/laminotomies, large portion of the posterior complex of the vertebra is being removed, as opposed to MIS techniques where an emphasis is put on preservation of the spinous process and its ligaments, along with other structures and surrounding musculature. Previous studies demonstrated lumbar spinal instability to occur in higher incidence after open laminectomy then MIS[
13,
15,
16,
17]. Since LSS is more prevalent in the elderly[
1,
2], the intervertebral disc of the operated level is already degenerated to some degree with weaker disc anulus. It is proposed that the combination of local instability and degenerated disc is more likely to result in disc herniation[
11].
We assume that performing lumbar spinal decompression using a tubular system with minimal bony and soft tissue removal will result in less disc herniations than open laminectomy. By conducting this study, we wish to compare the postoperative disc herniation rates of the "mini-open" laminectomy versus the tubular system decompression. Since no similar literature on this topic exist, this novel study is of important value.
Methods
Study design
A retrospective, comparative study was conducted. We performed an analysis of data of 563 patients who underwent primary lumbar spinal decompression in our institution between February 2015 until September 2020. The study was approved by our institutional ethical board.
Patient population
All patients who underwent lumbar spinal decompression for symptomatic LSS by the primary surgeon of this article in the spine surgery unit of our institution were candidates for this study. Preoperative CT and MRI of the lumbar spine was performed for all patients. We included all patients with intractable radicular pain or neurogenic claudication with disability related to LSS and symptoms duration of at least 6 months irresponsive to non-operative treatment. Few patients were included with rapid deterioration in daily function due to LSS. On MRI all patients had severe or extreme spinal stenosis as described by Schizas et al.[
18], light and moderate LSS patients are treated only with physiotherapy. Only patients with no other spinal pathology needing surgical intervention as seen in the preoperative MRI were included. A minimum of 12 months follow-up documented for all patients in study. We excluded all patients with previous spinal surgery or disc herniation at the operated level before surgery. Degenerative spondylolisthesis grade I was not a contraindication for decompression surgery without instrumentation if no signs of spinal instability on MRI/CT or dynamic flexion extension films seen. Patients were divided into two groups by surgical technique: group 1 underwent "mini-open" partial laminotomy via midline structures and group 2 underwent minimally invasive surgery (MIS) using tubular system without damaging the midline structures.
Surgical techniques
It is the senior author preference to always decompress bilaterally in cases of degenerative spinal stenosis even if symptoms are mainly unilateral.
"Mini-open" partial bilateral laminotomy (MOL): under general anesthesia, patients are placed prone on Jackson’s table. Surgical level is marked using fluoroscopy, then a 4-5 cm midline longitudinal incision performed, subperiosteal dissection using McCulloch retractor for soft tissue retraction until reaching the interlaminar gap. Using a Luer Rongeur or bone osteotome partial cutting of the spinous process with complete resection of the interspinous and supraspinous ligaments (ISL and SSL) at index level until lamina is exposed bilaterally. Surgical microscope deployed, and bilateral partial laminotomy is performed using a High-speed drill with diamond head of 4.5 mm or Kerrison Rongeur. The ligamentum flavum is than completely resected to expose the trans versing nerve roots. We assured that there is no pressure on the nerve root in the region of its shoulder, axilla or in the neuroforamen. Also, with a fine hook we check that there is no disc herniation compressing the nerve and that the nerve root is freely mobilized.
MIS using tubular system [METRx – Medtronic company, Minneapolis, Minnesota, USA]: the procedure was performed as described in detail by Alimi et al.[
19] with the exception of performing decompression of both sides using unilateral port – over the top decompression. Tube inserted on the most affected side of the patient and bilateral decompression was achieved via tilting of the operating table and angulation of the surgical microscope for contralateral decompression. On the affected side flavectomy and partial facetectomy performed as needed to remove all pressure from the nerve and on the contralateral side, if no pain, only flavectomy performed without bony work. We did not damage the Interspinous, Supraspinous or Spinous Process during the approach.
To clarify, only flavectomy and partial facetectomy were performed during the index surgery, no discectomy or anulotomy was done.
Study protocol
All patients underwent a full clinical evaluation including physical examination, CT, and MRI scan prior to the surgery. The same surgical techniques were used in all operations and performed by single senior surgeon (E.B). Postoperatively, all patients were allowed to mobilize as pain allowed. Most patients discharged less than 24 hours after surgery. Isometric strengthening and an exercise program were started 3-weeks following surgery. Patients were followed up in the outpatient clinic at 6-weeks, 6-months, and 1 year postoperatively. Clinical and demographic data (gender, age, BMI, affected level) were collected retrospectively from patient's medical records. As postoperative early radiculopathy is very rare if decompression performed properly, each patient suffering from postoperative radicular symptoms for more than three weeks and failed basic conservative treatment of 10 days anti-inflammatory and pain medication, underwent an MRI with contrast material.
Outcome measures
The primary outcome was comparison of post-decompression surgery, index level, disc herniation occurrence between the two study groups. Disc herniation diagnosis was confirmed by MRI examination.
Data analysis
Continuous parameters are presented as the means and standard deviations and categorical parameters as proportions. Continuous parameters (Age, BMI, etc.) were compared between the groups with independent two-tailed t test and categorical parameters (gender, affected level, etc.) were compared using the Fisher's exact test. All statistical analyses were performed using MedCalc Statistical Software version 19.7.2 (MedCalc Software Ltd, Ostend, Belgium). A p-value of <0.05 was considered significant
Results
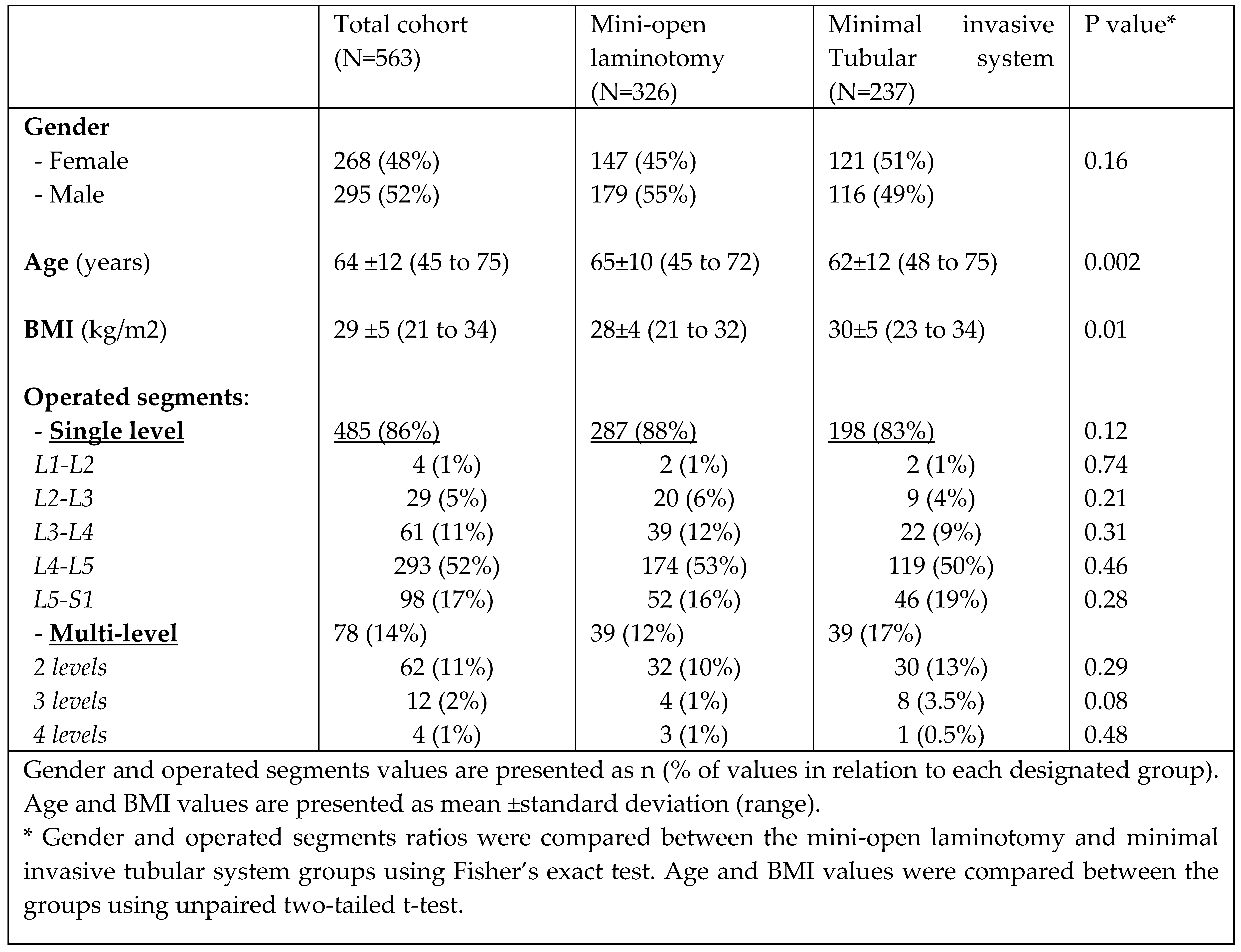
A total of 563 patients were included in this study: 326 underwent "Mini-open" laminotomy (MOL) and 237 underwent minimally invasive surgery using tubular system. In the MOL group 45% were females versus 51% in the minimally invasive group (p=0.16). Age was found statistically significant between the groups with patients aging 65±10 in the MOL group and 62±12 in the minimally invasive group (P=0.002). BMI was found statistically significant as well between the MOL and minimally invasive groups (28±4 versus 30±5 respectively, p=0.01).
No statistical difference was found between the groups regarding the number of segments operated nor among the segment's height as well (p>0.05). All demographics and clinical data are presented in
Table 1.
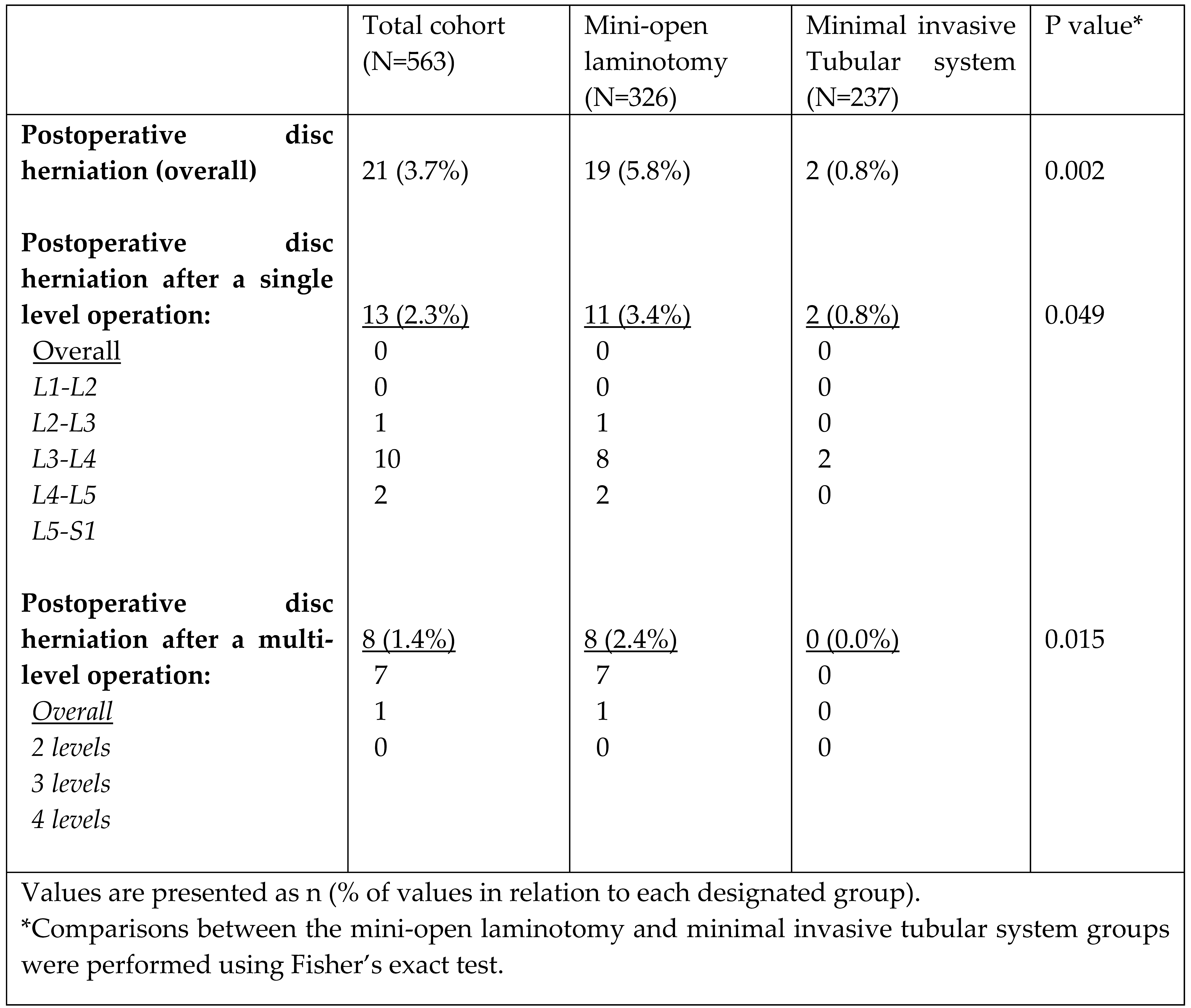
Postoperative disc herniation was found to be significantly higher in the "Mini-open" group with 19 cases (5.8%) versus 2 cases (0.8%) in the minimally invasive group (p=0.002). Postoperative disc herniation was also found to be significantly higher in multi-level operation, 8 out of 78 cases (10.2%) compared with single level operation, 13 out of 485 cases (2.7%), (p=0.0043). When comparing between surgical techniques, minimally invasive has significantly lower rates of postoperative disc herniation compared to "Mini-open" both in single level and multi-level operations, 2 versus 11 (p=0.049) and 0 versus 8 (p=0.015) respectively (
Table 2). As seen in
Table 2, most postoperative disc herniations following a single level operation, 10 out of 13 (76.9%), occurred after an operation at the level of L4-L5.
Discussion
Lumbar spinal stenosis (LSS) is a common diagnosis in the general population with increasing incidence correlated to increasing age[
1,
2]. General recommendations are to perform decompression surgery on patients whose symptoms are moderate-to-severe and refractory to conservative treatment for more than 3 months[
3,
4,
8,
20]. With many previous studies comparing between open decompression and minimally invasive techniques, there is yet no conclusive preference on either and no technique has been abandoned. Still, there in an inclination towards the MIS techniques due to less blood loss, shorter operative duration, shorter hospital stays, fewer opiate use, and higher patient satisfaction[
5,
7,
20,
21].
Like in any other operation, lumbar spinal decompression carry risks of general surgical complication (reaction to anesthesia, blood clots, bleeding, etc.) but other risks are notably mentioned like; incidental Dural tear (4-10%)[
4,
8,
9]; deep wound infection (~1-2%)[
8,
10]; and neurological injury (<1%)[
3]. When performing spinal decompression, the main purpose is to alleviate pain and prevent future neural deterioration. When an intervertebral disc herniates after decompressive procedure, it may lead to return of symptoms and patient complaints. Lurie et al.[
22] performed a long-term (8-years) comparison of the outcomes of patients from the SPORT study. They found the reoperation rate due to restenosis to be 10% after lumbar decompression but no complication of disc herniation was mentioned. In this study we describe disc herniation as a short-term complication after different decompressive surgery.
While the literature tried to compare the complication rate between open and MIS decompression techniques, there is no reference comparing post-decompressive lumbar disc herniation (PDLDH) rates between the different techniques. Takenaka et al.[
11] provides a table which summarizes 12 studies between the years 1993-2016, including their own, of lumbar spinal decompression procedures and following PDLDH rates. As Takenaka et al. mentioned, the incidence of PDLDH was lower for the MIS procedures. However, some of the studies included patients with an already herniated disc or preformed fusion during primary operation, and none of them made a comparison between the two techniques. This study is the first to compare the rates between different decompressive techniques and we show the PDLDH rate to be lower in the MIS technique using tubular system then in the "mini-open" laminotomy.
Our study found 21 cases (3.7% from the total cohort) of new disc herniation after decompressive surgery. 19 cases of disc herniation (comprising 5.8% of the "mini-open" group) occurred if posterior elements were damaged during surgery and 2 cases (comprising 0.8% of the MIS group) occurred if posterior elements kept intact.
In this study we performed a "mini-open" procedure as described in the methods section. Even with the utilization of a surgical microscope and only 4-cm skin incision, the procedure can still be considered as rather aggressive due to the removal of the spinous process and ligaments. Spinal instability is broadly discussed in previous studies[
13,
15,
16,
17,
21,
23,
24,
25]. Removal of the ISL and SSL as well as the spinous process results in spinal instability, most notably in flexion-extension motion[
11,
13,
15,
23]. This instability transfers much of the force to the same-level disc[
24,
25]. Since LSS is common among the elderly[
1,
2], the intervertebral disc of the operated level is relatively degenerated. In a degenerated disc, the annular ring is more frail, easier to bulge or tear, and the nucleus pulposus, even if dried out, may herniate. It is proposed that the combination of local instability and degenerated disc is more likely to result in disc herniation[
11]. Rao et al.[
24] compared spinal stability after laminotomy and laminectomy by comparing postsurgical range of motion, furthermore, they calculated pressure loads upon the intervertebral disc in each procedure and motion. They demonstrated significantly larger motion of the spine in flexion, extension, and lateral rotation after laminectomy rather than laminotomy. In addition, they found an 130% increase in stress upon the disc annulus after laminectomy compared with only 20% after laminotomy. Zander et al.[
25] demonstrated as well, an increase in pressure upon posterior annulus while standing and increased pressure in the anterior part while forward bending after facetectomy. Rao et al. also mentioned in their study that the increase in pulposus pressure was insignificant after both procedures[
24].
In MIS procedure, using tubular system, and performing a unilateral laminotomy for bilateral decompression (ULBD), as described in the methods section, the spinous process, ISL, SSL and surrounding musculature are kept intact. The lamina is trimmed to the minimum required as well as the facet joint. Based on the above studies, we believe the tubular system provide a better technique for lumbar decompression by keeping the spine as stable as possible and still accomplish its purpose. This can be seen by the significantly lower rates of PDLDH in the MIS groups compared with the "mini-open" group. Additionally, it was found in our study that multi-level operation resulted in more postoperative disc herniation compared with single level operation (10.2% vs. 2.7%, p=0.0043). To our understanding, the difference between multi and single level operation PDLDH derives from the proportion of soft and bony tissues removed (more tissue damage in multi-level operations) thus creating far more instability in the operated area and leading to the aforementioned results.
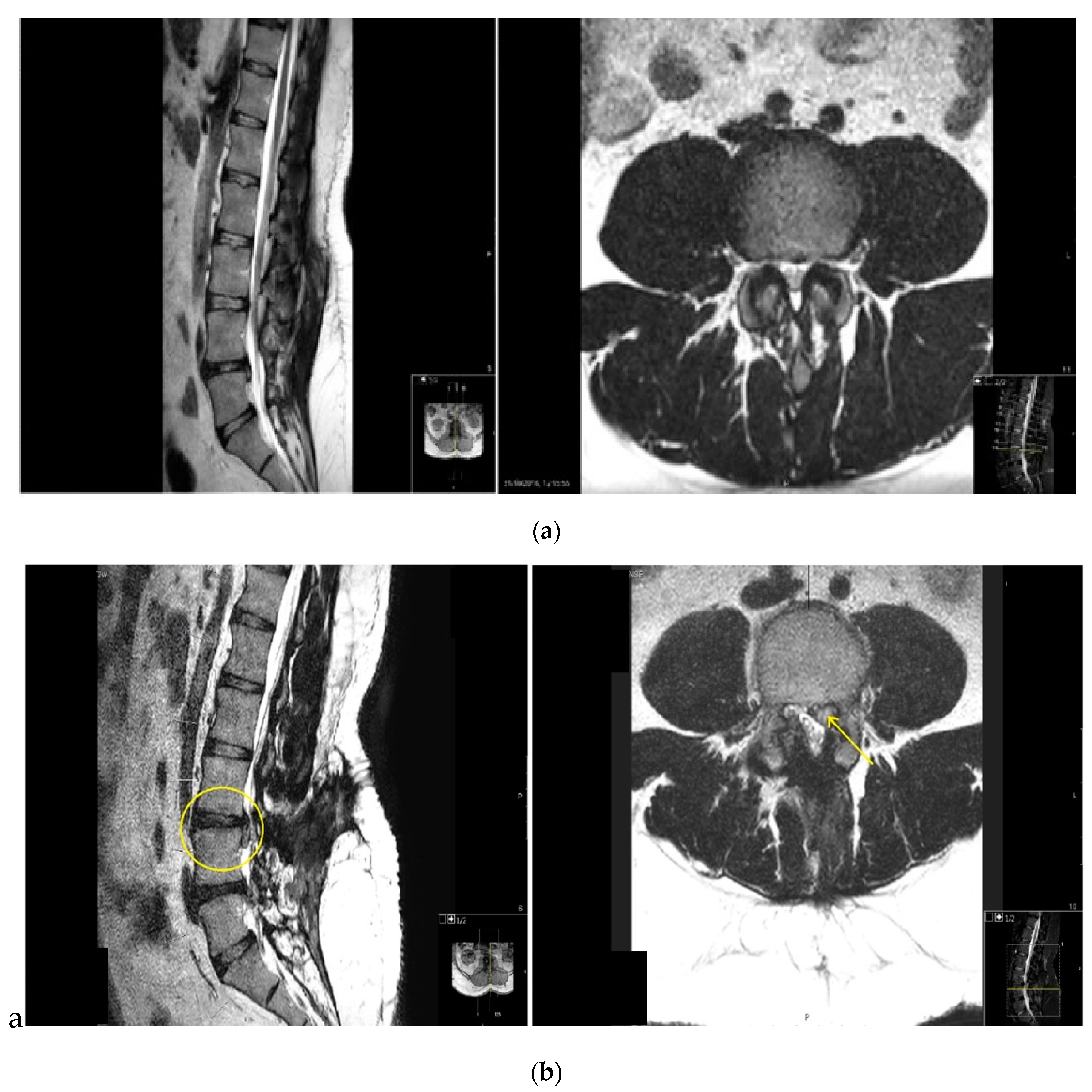
Of the 21 postoperative disc herniation (
Figure 1), 6 underwent further discectomy surgery in which the herniated disc was removed with resolution of radicular pain.
15 were treated conservatively with selective nerve root injection, physiotherapy, and anti-inflammatory medication with an improvement of their symptoms at the final follow-up. We think the relatively low reoperation rate even with proven large disc herniation is due to the laminotomy performed in the decompression operation, with the enlargement of the canal the nerve root has more space to avoid the compressive pressure of the disc herniation, causing less severe radicular pain, pain that could be managed with conservative treatments rather than surgery until herniated disc absorbed over time.
This study shows a 3.7% of new disc herniation after lumbar decompression surgery. This complication prevalence is second only to durotomy and more common than infection or neurological injury. Therefore, in our opinion, the knowledge of disc herniation as short-term complication of decompressive surgery must be transferred to our patients pre-operatively when signing a consent form.
Limitations and strengths
As a retrospective study our study holds some inherent limitations. However, any selection bias or confounders are minimized due to the large sample size in this study. Our study holds some strengths as all operations in this study were performed by one senior surgeon, experienced in both techniques, lowering by that the chance for different surgical outcomes by different surgical techniques. It is worth mentioning that we performed postoperative MRI studies only on symptomatic patients, meaning disc herniation after lumbar decompression surgery occurrence might be even higher than 3.7% reported by us. Still, case-control, prospective study is required for these results to be more definitive.
Conclusion
This study found 3.7% risk of disc herniation after lumbar decompressive surgery, a complication that is significant and second only to durotomy as short period complication. This study found higher rate of disc herniation if posterior elements are damaged. Minimally invasive surgery using tubular system for lumbar spinal decompression is shown to result in significantly lower rates of post-decompressive lumbar disc herniation than "mini-open" partial laminectomy.
Author Contributions
OU and LA are responsible for the conception of the study. EB, YF and AM are responsible for the acquisition of the data. WS and IP analyzed and interpretate the data. All authors took part in drafting the manuscript and approved its final draft.
Funding
The authors declare that no funding was received for this study.
Ethics approval and consent to participate
This study was approved by our institutional ethical board (0124-21-HYMC).
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
List of abbreviations
Lumbar spinal stenosis (LSS)
Minimally invasive surgeries (MIS)
"Mini-open" laminotomy (MOL)
Interspinous ligaments (ISL)
Supraspinous ligaments (SSL)
Post-decompressive lumbar disc herniation (PDLDH)
Unilateral laminotomy for bilateral decompression (ULBD)
References
- Kalichman L, Cole R, Kim DH, et al (2009) Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J 9:545–550. [CrossRef]
- Ishimoto Y, Yoshimura N, Muraki S, et al (2012) Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthr Cartil 20:1103–1108. [CrossRef]
- Costa F, Alves OL, Anania CD, et al (2020) Decompressive surgery for lumbar spinal stenosis: WFNS spine committee recommendations. World Neurosurgery: X 7:100076. [CrossRef]
- Weinstein JN, Tosteson TD, Lurie JD, et al (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358:794–810. [CrossRef]
- Phan K, Mobbs RJ (2016) Minimally Invasive Versus Open Laminectomy for Lumbar Stenosis: A Systematic Review and Meta-Analysis. Spine 41:E91–E100. [CrossRef]
- Overdevest GM, Jacobs W, Vleggeert-Lankamp C, et al (2015) Effectiveness of posterior decompression techniques compared with conventional laminectomy for lumbar stenosis. Cochrane Database Syst Rev CD010036. [CrossRef]
- Nerland US, Jakola AS, Solheim O, et al (2015) Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 350:h1603. [CrossRef]
- Weinstein JN, Tosteson TD, Lurie JD, et al (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 296:2441–2450. [CrossRef]
- McMahon P, Dididze M, Levi AD (2012) Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine 17:30–36. [CrossRef]
- Mueller K, Zhao D, Johnson O, et al (2019) The difference in surgical site infection rates between open and minimally invasive spine surgery for degenerative lumbar pathology: A retrospective single center experience of 1442 cases. Oper Neurosurg (Hagerstown) 16:750–755. [CrossRef]
- Takenaka S, Tateishi K, Hosono N, et al (2016) Preoperative retrolisthesis as a risk factor of postdecompression lumbar disc herniation. J Neurosurg Spine 24:592–601. [CrossRef]
- Hwang H-J, Park H-K, Lee G-S, et al (2016) Predictors of Reoperation after Microdecompression in Lumbar Spinal Stenosis. Korean J Spine 13:183–189. [CrossRef]
- Hopp E, Tsou PM (1988) Postdecompression lumbar instability. Clin Orthop Relat Res 227:143–151.
- Yüce İ, Kahyaoğlu O, Çavuşoğlu HA, et al (2019) Long-Term Clinical Outcome and Reoperation Rate for Microsurgical Bilateral Decompression via Unilateral Approach of Lumbar Spinal Stenosis. World Neurosurg 125:e465–e472. [CrossRef]
- Tai C-L, Hsieh P-H, Chen W-P, et al (2008) Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome - an experimental study in porcine model. BMC Musculoskelet Disord 9:84. [CrossRef]
- Hamasaki T, Tanaka N, Kim J, et al (2009) Biomechanical assessment of minimally invasive decompression for lumbar spinal canal stenosis: a cadaver study. J Spinal Disord Tech 22:486–491. [CrossRef]
- Lee MJ, Bransford RJ, Bellabarba C, et al (2010) The effect of bilateral laminotomy versus laminectomy on the motion and stiffness of the human lumbar spine: a biomechanical comparison. Spine 35:1789–1793. [CrossRef]
- Schizas C, Theumann N, Burn A, et al (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine 35:1919–1924. [CrossRef]
- Alimi M, Hofstetter CP, Pyo SY, et al (2015) Minimally invasive laminectomy for lumbar spinal stenosis in patients with and without preoperative spondylolisthesis: clinical outcome and reoperation rates. J Neurosurg Spine 22:339–352. [CrossRef]
- Watters WC, Baisden J, Gilbert TJ, et al (2008) Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J 8:305–310. [CrossRef]
- Postacchini F, Cinotti G, Perugia D, Gumina S (1993) The surgical treatment of central lumbar stenosis. Multiple laminotomy compared with total laminectomy. J Bone Joint Surg Br 75:386–392. [CrossRef]
- Lurie JD, Tosteson TD, Tosteson A, et al (2015) Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine 40:63–76. [CrossRef]
- Goel VK, Fromknecht SJ, Nishiyama K, et al (1985) The role of lumbar spinal elements in flexion. Spine 10:516–523. [CrossRef]
- Rao RD, Wang M, Singhal P, et al (2002) Intradiscal pressure and kinematic behavior of lumbar spine after bilateral laminotomy and laminectomy. Spine J 2:320–326. [CrossRef]
- Zander T, Rohlmann A, Klöckner C, Bergmann G (2003) Influence of graded facetectomy and laminectomy on spinal biomechanics. Eur Spine J 12:427–434. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).