1. Introduction
The sacroiliac joint (SIJ) is recognized as a potent pain generator that can act as both a primary and a contributing source of chronically severe low back pain [
1,
2,
3]. Sacroiliitis can also manifest as adjacent segment disease secondary to lumbar spinal fusion surgery [
4,
5,
6]. When symptoms related to SIJ dysfunction become unresponsive to conservative care and impair normal physical function and quality of life, minimally-invasive SIJ arthrodesis is the preferred surgical option [
7]. Surgical fixation and stabilization of the SIJ to support bony fusion across the joint space can be accomplished using an array of surgical approaches [
8,
9,
10,]. While the surgical goal of all approaches is identical, the posterior approach utilizes a trajectory and easily identifiable landmarks that allow the surgeon to control the risk of violating important neuro-vascular structures [
11].
The minimally invasive, transfixing SIJ fusion procedure can employ numerous operative trajectories. To date, the most common trajectories utilized have been lateral and lateral-oblique trajectories. However, these operative trajectories come with certain risks and pitfalls; most commonly, implant breech of the neuroforamen or anterior sacral cortex [
12,
13,
14]. Furthermore, the implant location most associated with complication is placed in the superior aspect of the joint [
12]. In contrast, the postero-inferior trajectory allows implant placement in an ultra-safe operative corridor, originating at the inferior aspect of the joint, going through the ilium, across the sacroiliac joint space, and into the sacrum, transfixing the osseous confines of the ilium and sacrum across sub-chondral bone.
2. Materials and Methods
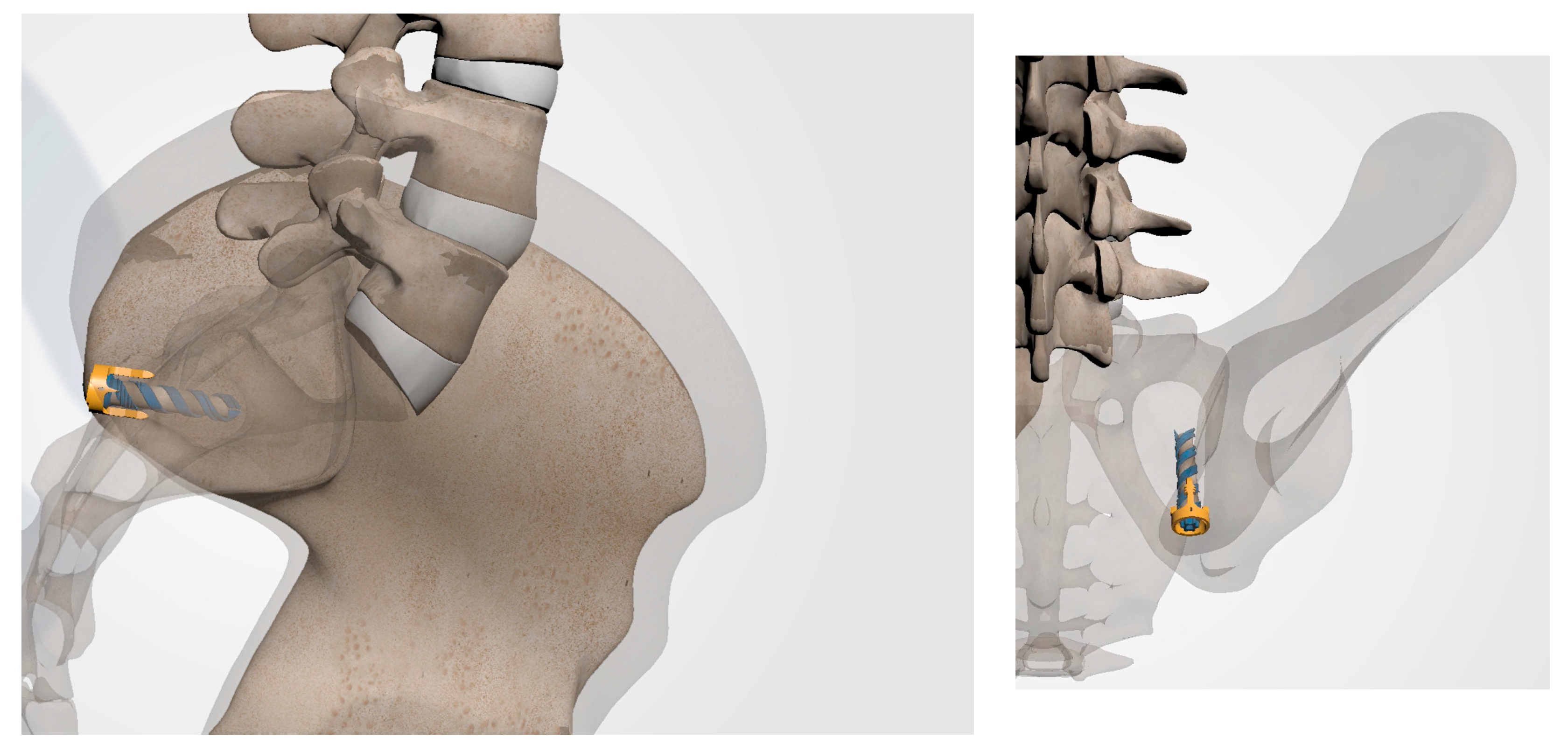
This paper details the surgical procedure associated with the postero-inferior operative trajectory (
Omnia postero-inferior approach) using the PsiF™DNA Sacroiliac Joint Fusion System [
15]. Included in this description will be a discussion of the biomechanical advantages of placing the Dorsal Nutation Anchor (DNA) in close proximity to the predominant rotational axis and utilizing natural joint architecture to stabilize the fusion construct.
3. Results
3.1. Structural Anatomy Overview
Figure 1 illustrates the important anatomical landmarks and features of the SIJ in perspective to the overall pelvic anatomy. Auricular-shaped surfaces encompass both the iliac and sacral joint aspects. As the primary structural connection between the axial and lower appendicular skeleton, the SIJ includes load transfer, weight-bearing and shock absorption characteristics, but has limited range of motion [
16].
3.2. Patient Selection
The PsiF™ Sacroiliac Joint Fusion System is intended for SIJ fusion for conditions including degenerative sacroiliitis and sacroiliac joint disruptions. Minimally-invasive fusion of the SIJ is considered medically necessary by most insurance plans when ALL of the following criteria are met:
Have moderate to severe pain with functional impairment and pain persists despite a minimum 6 months of intensive nonoperative treatment that must include medication optimization, activity modification, bracing, and active therapeutic exercise targeted at the lumbar spine, pelvis, SIJ and hip including a home exercise program.
Patient’s report of typically unilateral pain that is caudal to the lumbar spine (L5 vertebrae), localized over the posterior SIJ, and consistent with SIJ pain.
A thorough physical examination demonstrating localized tenderness with palpation over the sacral sulcus (Fortin’s point) in the absence of tenderness of similar severity elsewhere (e.g., greater trochanter, lumbar spine, coccyx) and that other obvious sources for their pain have been ruled out.
Positive response to a cluster of 3 provocative tests (e.g., thigh thrust test, compression test, Gaenslen’s test, distraction test, FABER test, posterior provocation test).
Absence of generalized pain behavior or generalized pain disorders (e.g., fibromyalgia) contributing to the SIJ-area pain.
-
Diagnostic imaging studies that include ALL of the following:
- -
Imaging (plain radiographs and a CT or MRI) of the SIJ that excludes the presence of destructive lesions (e.g., tumor, infection), fracture, traumatic SIJ instability, or inflammatory arthropathy that would not be properly addressed by percutaneous SIJ fusion.
- -
Imaging of the pelvis (AP plain radiograph) to rule out concomitant hip pathology.
- -
Imaging of the lumbar spine (CT or MRI) to rule out neural compression or other degenerative condition that can be causing low back or buttock pain.
Additionally, the patient should experience:
At least a 75 percent reduction in pain for the expected duration of a standard anesthetic agent, and the ability to perform previously painful maneuvers, following an image-guided, contrast-enhanced intra-articular SIJ injection.
A trial of at least two or more intra-articular SIJ injections, with at least one injection being therapeutic (i.e., corticosteroid injection).
3.3. Surgical Technique
Pre-operative planning for this procedure consists of lateral and oblique pelvic radiographs, as well as fluoroscopic inlet views (20° – 25° caudally) and AP/outlet views (35° outlet) to identify important SIJ anatomical landmarks.
For optimal intra-operative imaging, the fluoroscope should be equipped to rotate around the operating table 30° – 35° from vertical. Postero-inferior SIJ trans-fixation fusion surgery is performed minimally-invasively under fluoroscopic guidance, and the following provides the operative details on step-by-step basis:
3.3.1. Patient Positioning
Using a radiolucent table (flattop or Jackson table), the patient is placed in the prone position with the lumbar spine optimally flexed to minimize lumbar lordosis. 6” – 8” gel packs or a blanket roll under the umbilicus can be used to elevate the lumbar spine out of lordosis. This allows the hips to have approximately 15° – 20° of flexion. Positioning the patient to achieve a flat back helps to remove pelvic tilt and provides for key SIJ landmark identification under fluoroscopy. The procedure should be performed in a standard operative environment in a sterile surgical field.
3.3.2. Intraoperative Imaging
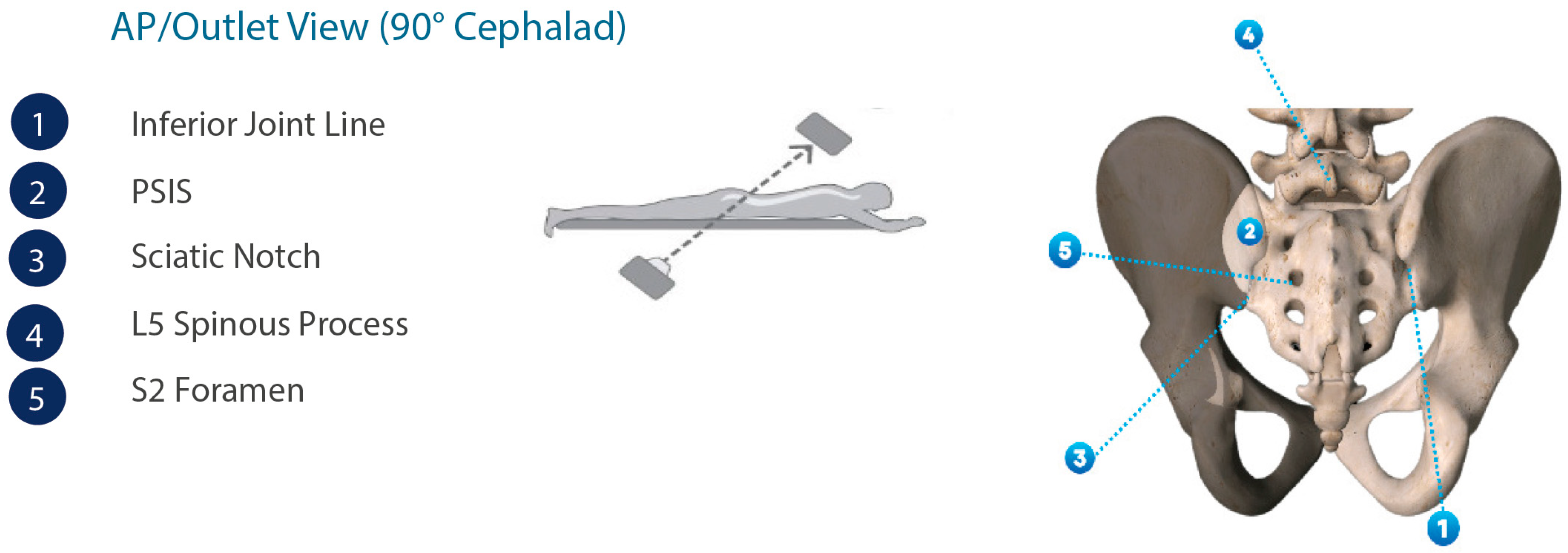
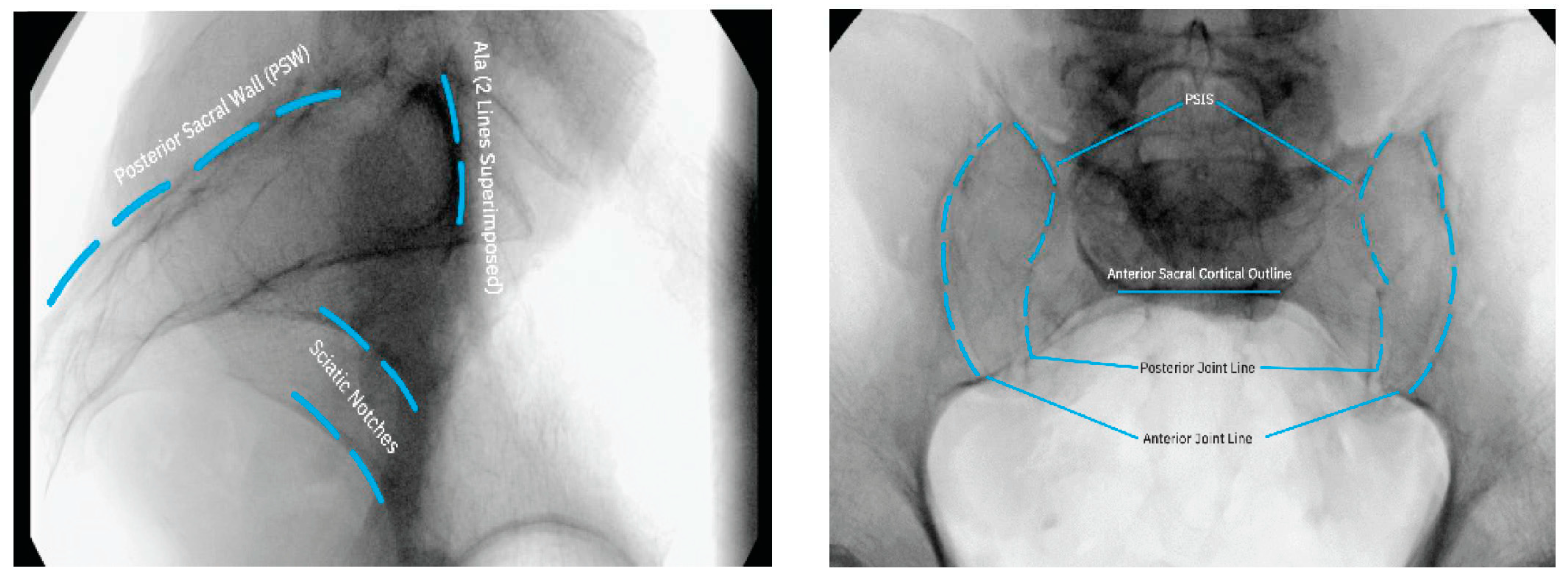
Once the patient is properly positioned, fluoroscopic imaging should be undertaken to obtain lateral, oblique, inlet, and AP/outlet views to identify the SIJ and its anatomical extent (
Figure 2).
3.3.3. Approach and Incision
The operative goal of postero-inferior SIJ fusion is to place the Dorsal Nutation Anchor Implant in a minimally invasive fashion, originating inferior to the posterior superior iliac spine on a trajectory that allows the implant to transfix the osseous confines of the ilium and sacrum, as closely adjacent to the sacral x axis as possible to allow for maximum fixation while minimizing the biomechanical forces on the implant [
17].
After the patient has been placed in the proper prone position, the initial surgical step is to draw a vertical line on the skin over the midline portion of the sacrum and position the C-arm of the fluoroscope over the sacrum in direct AP view to identify key landmarks such as the SIJ, sacral cornua, as well as the S1, S2 and S3 foramen. Next, a K-wire should be placed horizontal to the SIJ, directly over each sacral horn, and the skin should be marked on the vertical midline representing the sacral cornua. Skin marking should then be repeated for the S1, S2 and S3 foramen.
For unilateral procedures, the incision will start lateral to the apex of the posterior superior iliac spine, the incision should also be slightly lateral to the postero-inferior joint line. The incision should extend inferiorly to the inferior aspect of the SI joint. A knife and/or bovie should be used to dissect tissue down to the ilium and finger palpation may be used for blunt tissue dissection to the inferior aspect of the posterior superior iliac spine in order to confirm a clear path to the implantation site.
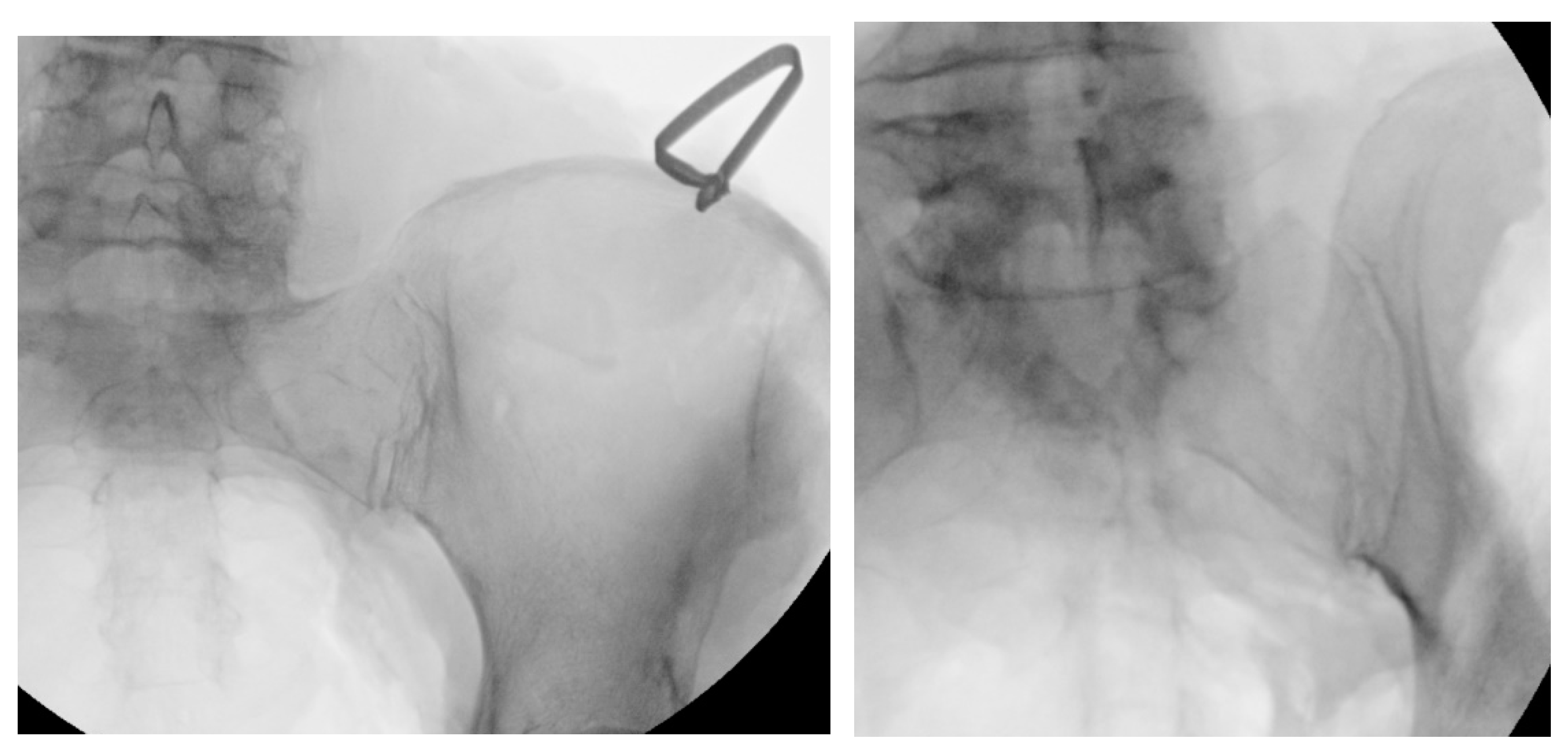
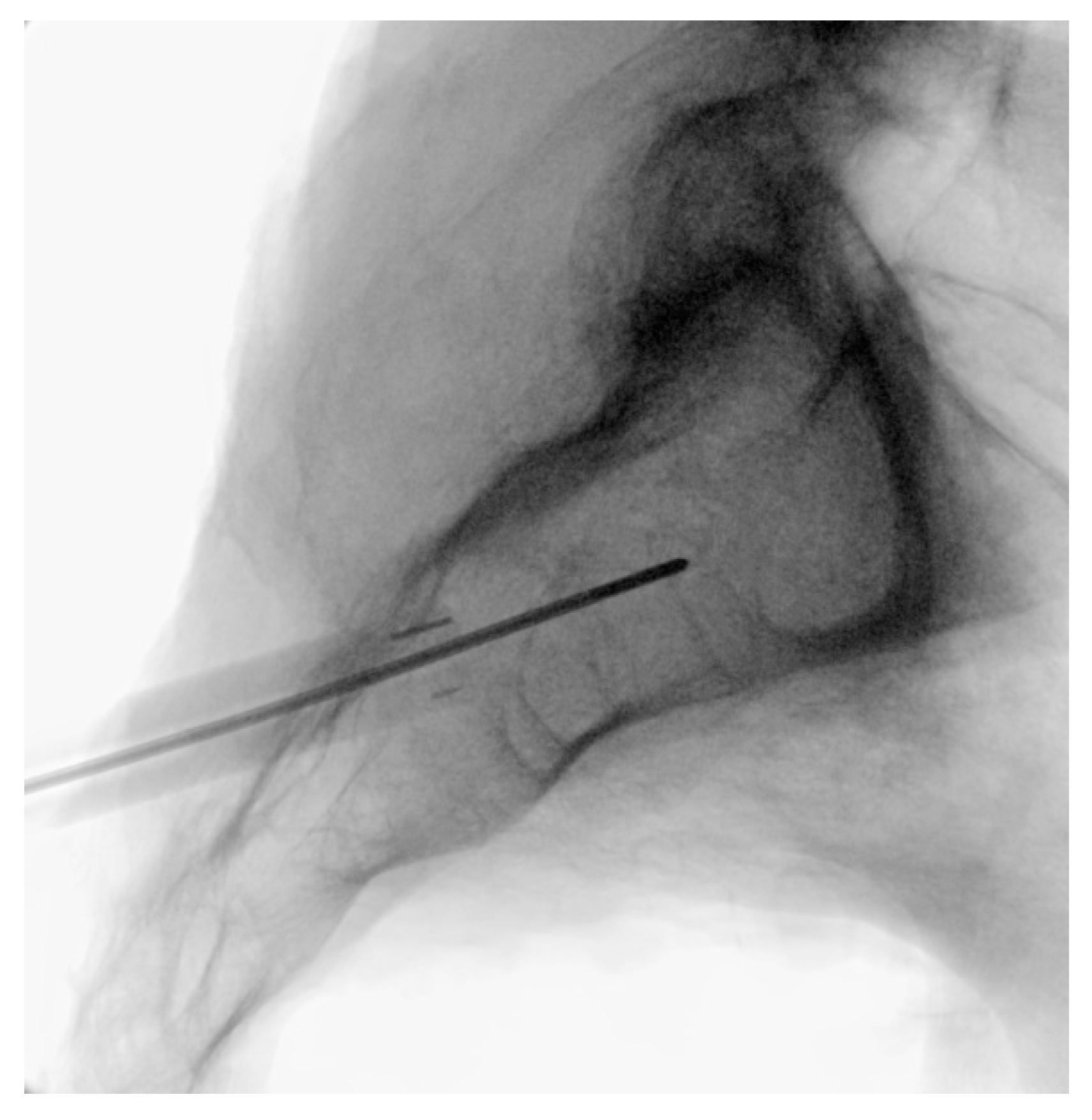
3.3.4. Steinman Pin Placement
Under fluoroscopic guidance using the inlet view, advance a Steinmann pin starting inferior, ventral, and lateral to the PSIS, and advancing superiorly, through the ilium across the SI joint into the sacrum. Finally, use a lateral fluoroscopic view to verify that the tip of the Steinmann pin has passed the posterior cortical outline of the sacrum, and is docked in the sacrum at or near center of the first sacral body (
Figure 3).
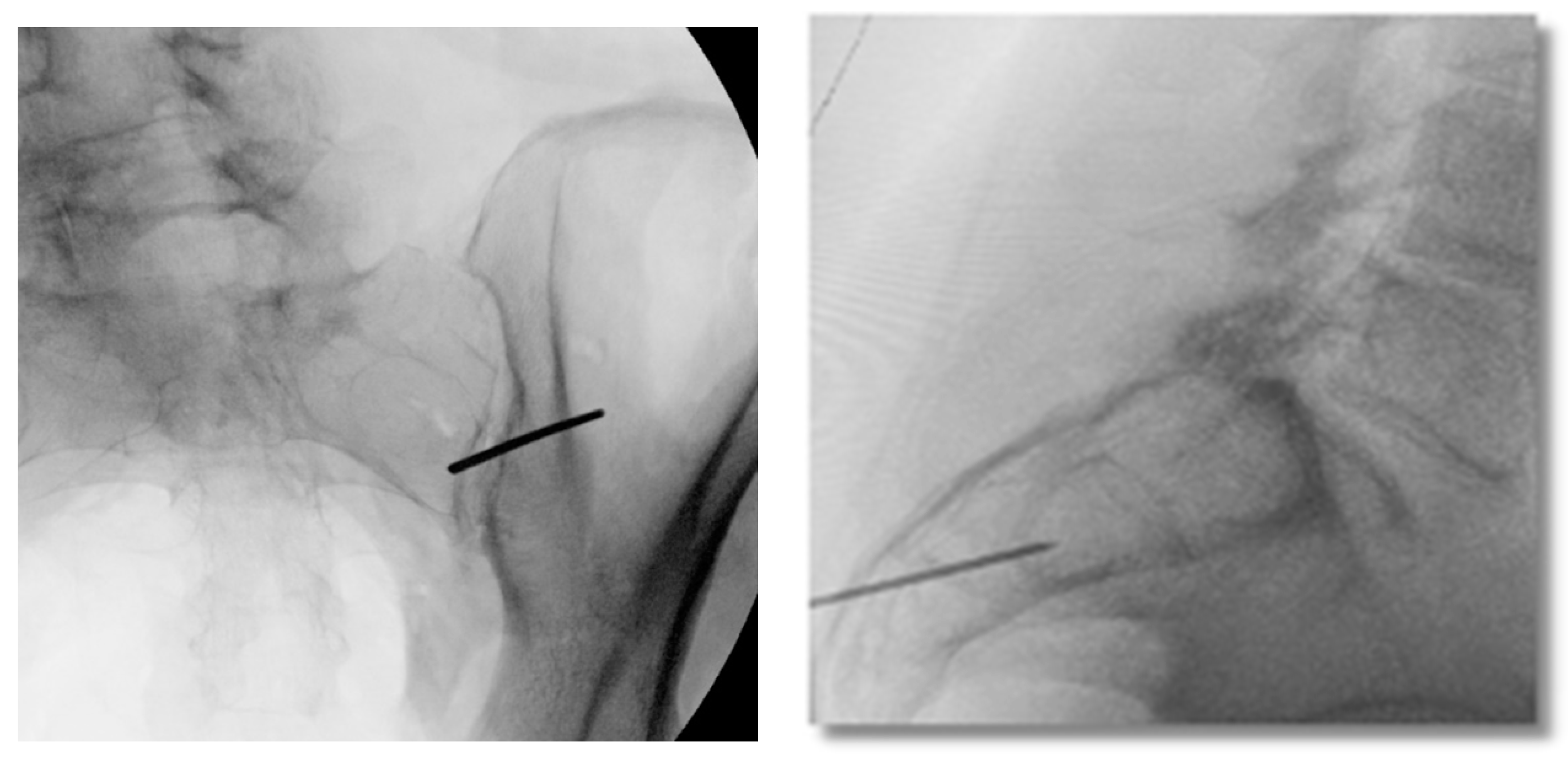
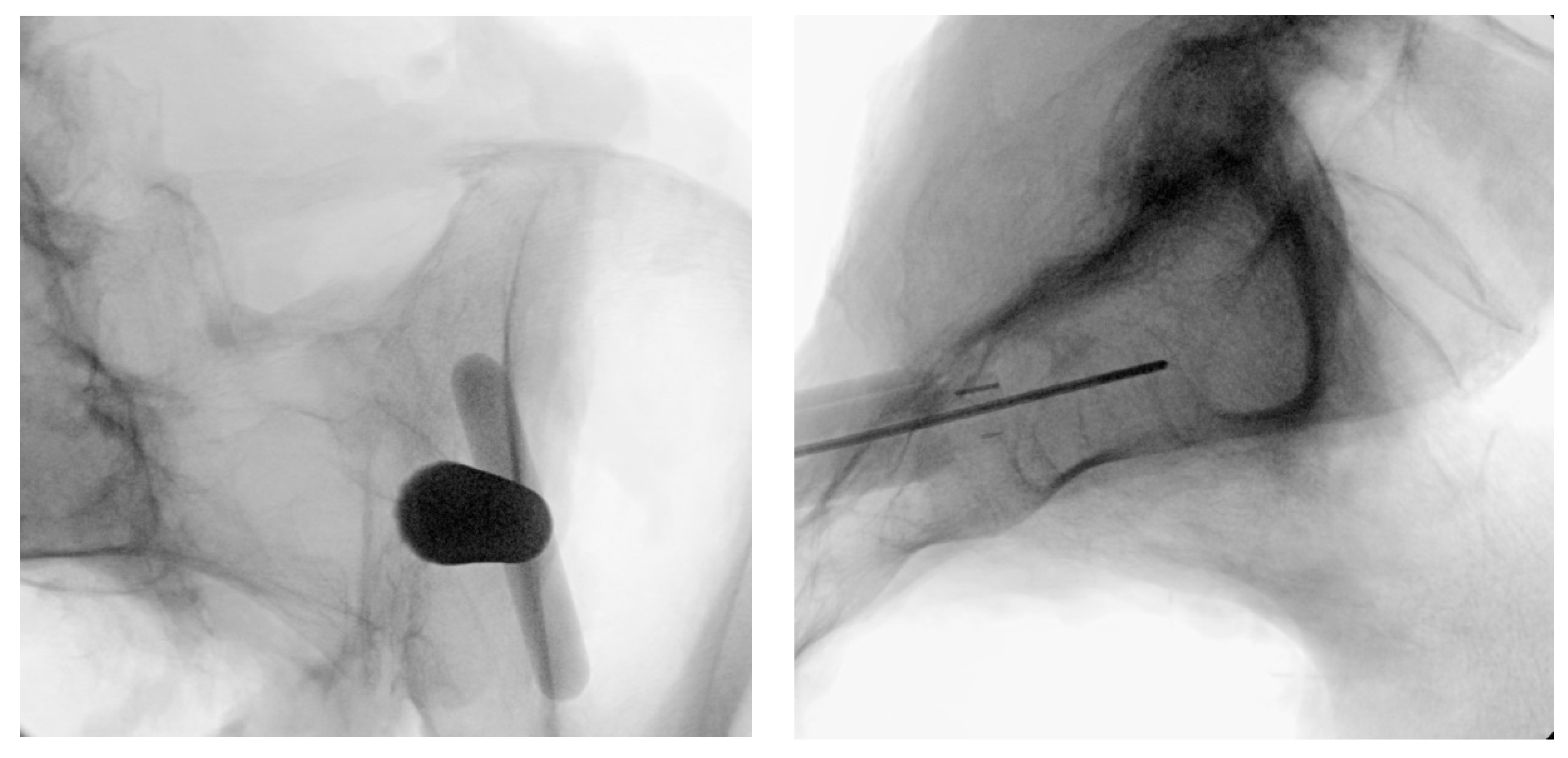
3.3.5. Tissue Dilation
With AP/outlet view visualization, a scalpel should be used to create a 2-3 cm skin vertical incision lateral to the postero-inferior joint line, at the apex of the posterior superior iliac spine, extending inferiorly to the inferior aspect of the joint line. The Initial Dilator instrument should be passed over the K-wire and, using a mallet, advanced until it docks inferior to the posterior superior iliac spine. Use an inlet view to confirm that the angle of the Initial Dilator is optimal for transfixation of the SIJ. To confirm proper placement, verify visually via lateral fluoroscopy that both corners of the Initial Dilator are past the posterior cortical outline and inferior aspect of the ilium (
Figure 4). Note: The Initial Dilator should be secure enough to stand on its own.
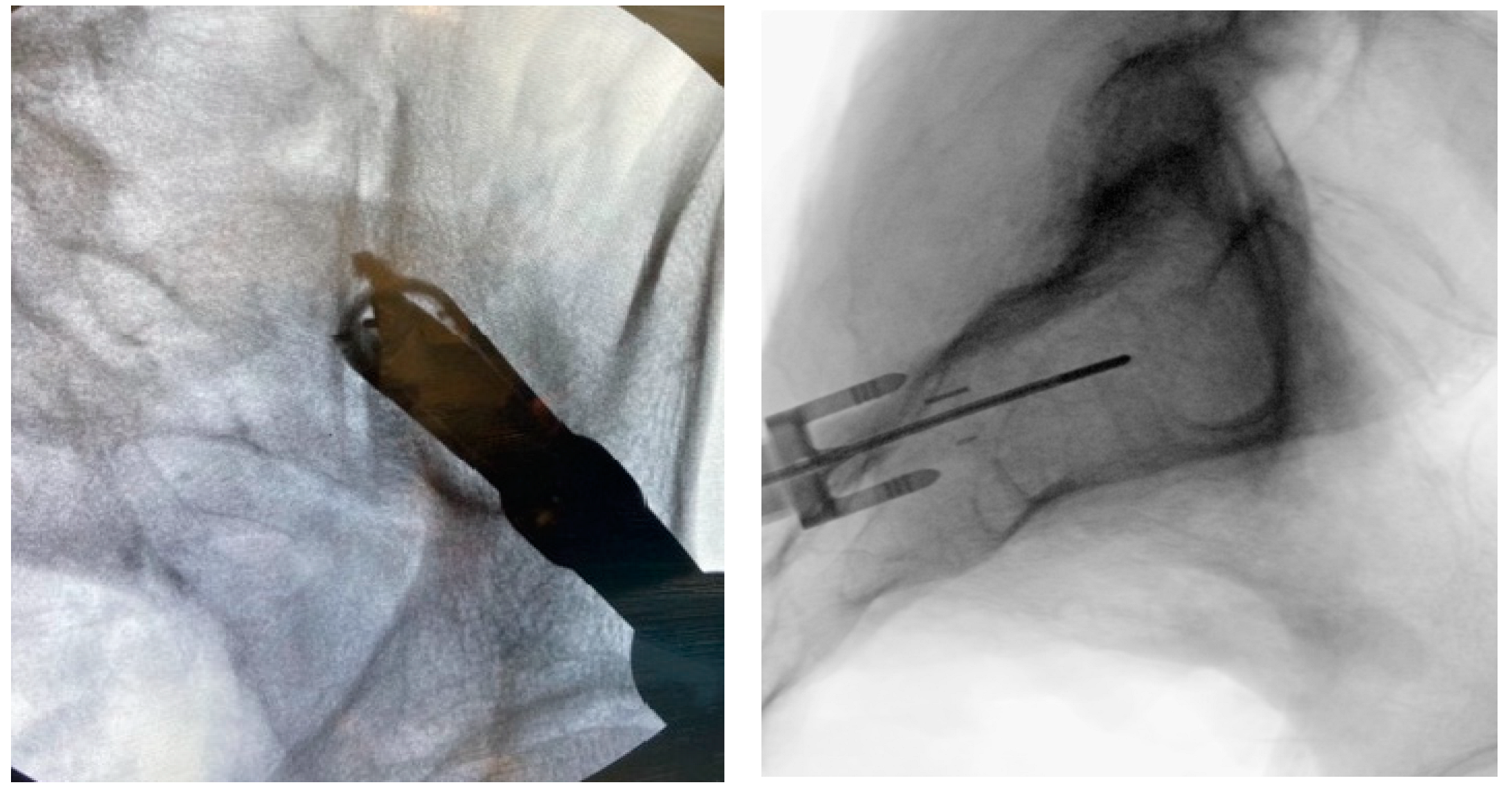
3.3.6. Implant Preparation
A mechanically solid implant construct is imperative to short-term stabilization of the joint. As such, a proper implant bed must be prepared for the construct, utilizing a Reamer-Drill. Oblique and inlet views should be used to confirm optimal trajectory of instrumentation. There must be adequate room ventral to the instrumentation to ensure that the Reamer-Drill does not violate the anterior border of the inferior joint line. (
Figure 5). Utilizing inlet and lateral views, an implant bed should be created by advancing the Reamer-Drill over the Initial Dilator and reaming down to the dense cortical bone of the ilium (
Figure 5). The tip of the Reamer-Drill should pass the posterior-inferior border of the ilium in lateral view to ensure that the implant bed is properly prepared.
3.3.7. Docking Washer Introduction
The Docking Washer should be introduced over the Initial Dilator and, using inlet and outlet views, should be advanced with a trajectory that allows for transfixation of the joint space by checking the angle of the approach (
Figure 6). To ensure safety, with an inlet view, the ventral aspect of the docking tangs should be observed to have adequate room on the ventral aspect of the joint (
Figure 6). Finally, using a lateral view, the Impact Cap should be attached and advanced using a mallet until the base of the Washer Tower is seated against the ilium (
Figure 6). To complete this step, the Impact Cap, Initial Dilator and Steinmann pin should be removed, leaving the Docking Washer Tower in place.
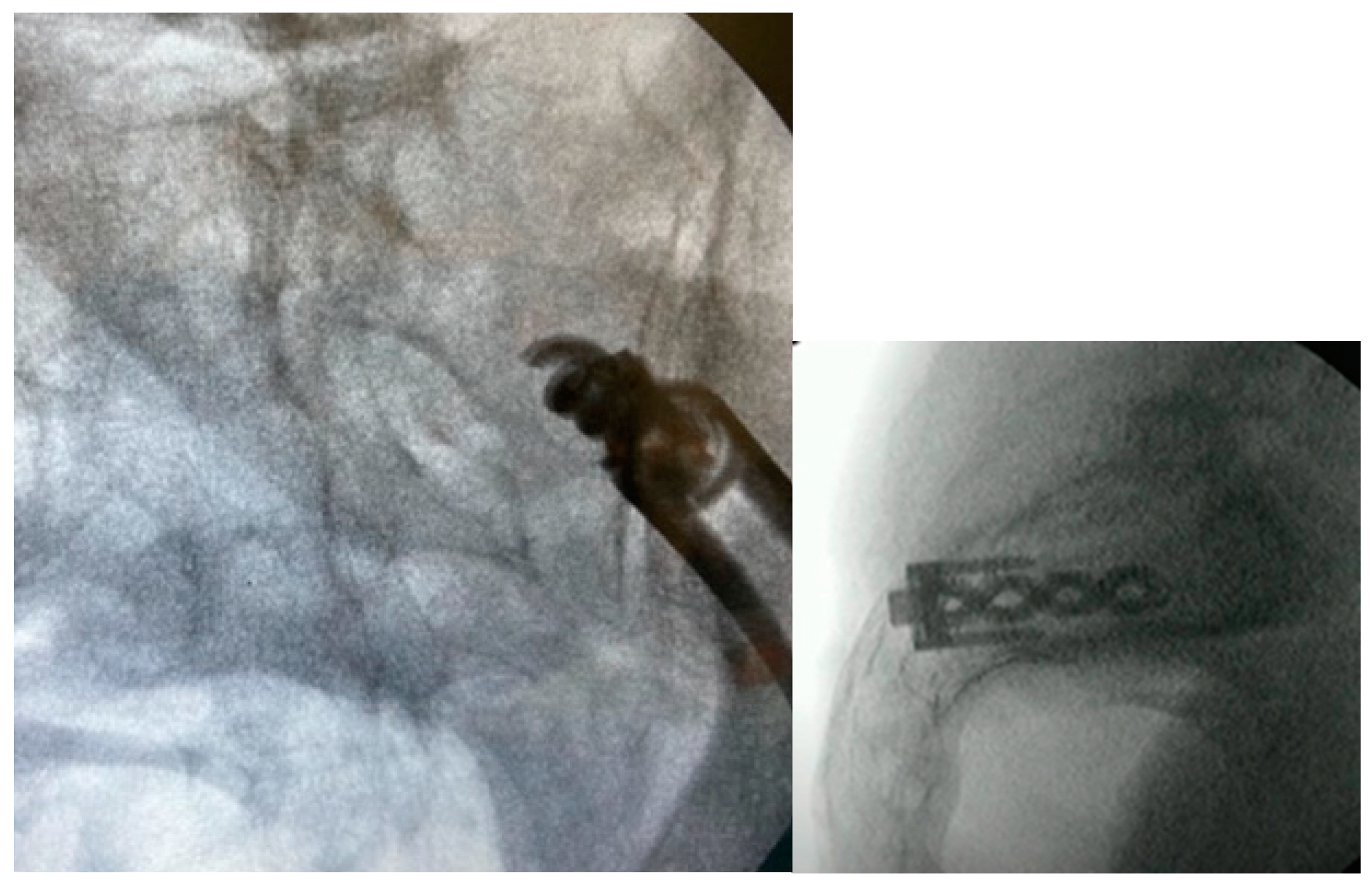
3.3.8. Implant Insertion
Once the Docking Washer has been firmly seated in the inferior aspect of the ilium and proper trajectory has been obtained, the PsiF™DNA implant is inserted down the Docking Washer Tower. Once the distal tips of the implant make contact with the ilium, ventral pressure is applied as the inserter is turned clockwise. The self-tapping, autograft harvesting implant will advance through the ilium, across the SI joint and into the sacrum (
Figure 7). When final placement is achieved, the base of the implant will lock in the Docking Washer. The base of the Docking Washer provides added safety from foraminal and ventral cortical breech.
3.3.9. Final Implant Placement
Once the PsiF™DNA implant is optimally placed to provide transfixation and stabilization, the tabs of the docking washer tower can be easily detached from the implant construct. All instrumentation can be removed and final imaging can be conducted (
Figure 8). The final implant placement should show the implant securely within the osseous confines of the ilium and sacrum, with the proximal end of the implant and Docking Washer docked firmly in the ilium and the distal end of the implant in the sacrum. The incision should be closed in a routine manner.
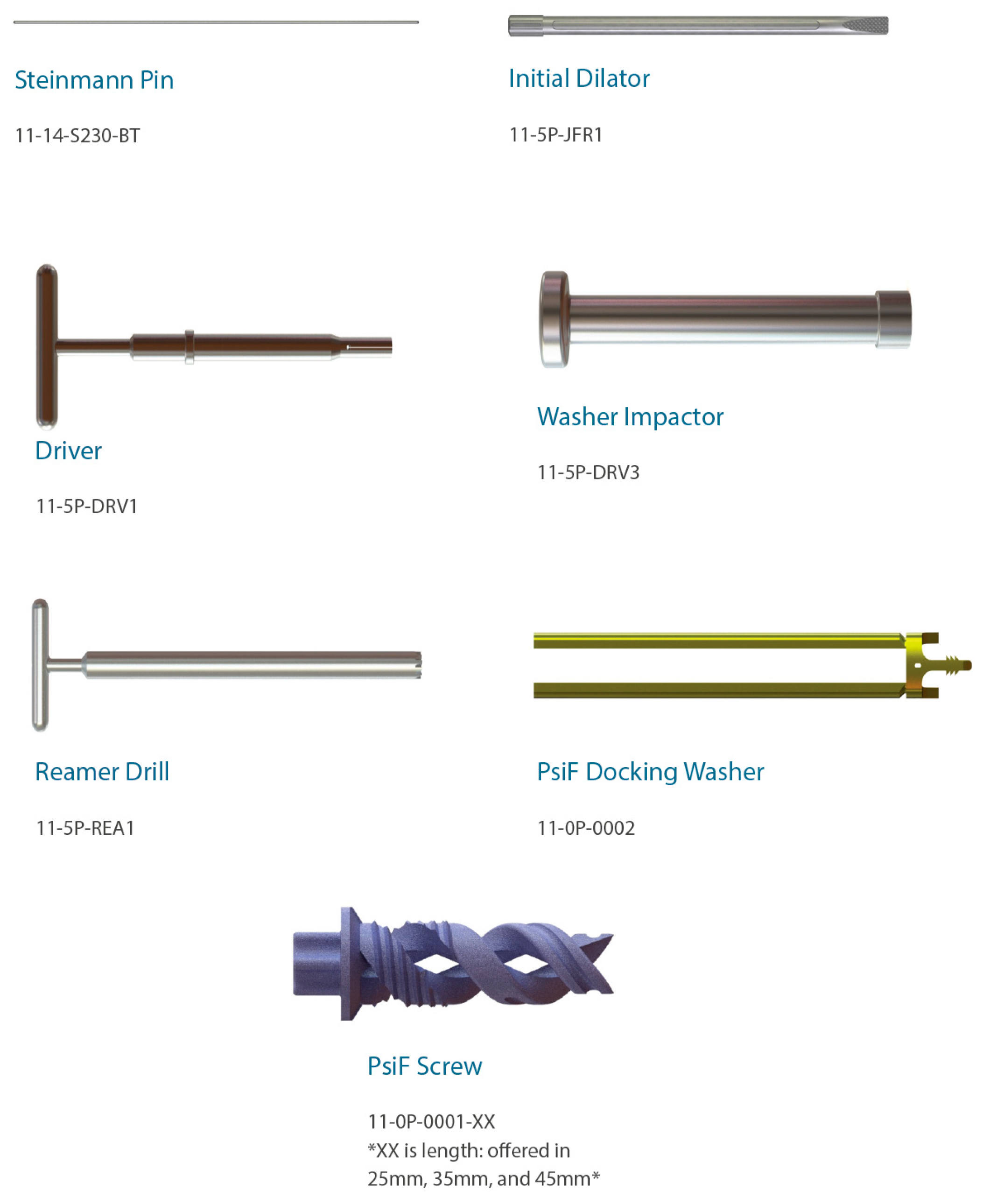
Figure 9 provides a visual guide of all instrumentation used in this minimally-invasive SIJ fusion procedure.
4. Discussion
The primary surgical objective of all minimally-invasive SIJ fusion procedures is to provide immediate fixation and stabilization across the joint space to support osseous consolidation and the development of a mechanically solid arthrodesis [
18]. This can be accomplished via several different surgical approaches. This paper provides surgical and procedural details regarding the postero-inferior approach which utilizes an operative trajectory that significantly limits the risk of violating the critical neuro-vascular structures by utilizing the ultra-safe corridor of dense cortical bone across the purely articular portion of the SIJ. With reduced peri-operative injury risk, this minimally-invasive approach offers a straightforward technique for a physician to learn.
The postero-inferior approach also takes advantage of the natural SIJ architecture by positioning the implant perpendicular to the S1 endplate, inferior and ventral to the PSIS and near the sacral axis of rotation. This allows for the establishment of a natural “pivot point” around the implant that acts to attenuate the mechanical forces associated with sacral rotation and flexion-extension.
This procedure is accomplished completely under fluoroscopic guidance with minimal tissue disruption. Total procedural time can vary depending on whether the procedure is unilateral or bilateral and the number of implants. Further observational data from real-world clinical use are encouraged to further validate this procedure as the surgical preference for minimally-invasive SIJ fusion.
Author Contributions
Conceptualization, J.E.B.; methodology, J.E.B.; software, J.E.B.; validation, J.E.B.; formal analysis, J.E.B.; investigation, J.E.B.; resources, J.E.B.; data curation, J.E.B.; writing—original draft preparation, J.E.B.; writing—review and editing, U.F., P.J.H., G.T., L.A.G., I.M.S. and J.E.B.; visualization, J.E.B.; supervision, J.E.B.; project administration, J.E.B.; funding acquisition, J.E.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
J.E.B. is an independent advisor to Omnia Medical (Morgantown, WV, USA). J.E.B. received remuneration for manuscript development. U.F., P.J.H., G.T., L.A.G. and I.M.S. received no funding for this study and report no other conflicts of interest.
References
- Ou-Yang, D.C.; York, P.J.; Kleck, C.J.; Patel, V.V. Diagnosis and Management of Sacroiliac Joint Dysfunction. J Bone Joint Surg Am 2017, 99, 2027–2036. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, A.C.; Aprill, C.N.; Bogduk, N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995, 20, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Vleeming, A.; Schuenke, M.D.; Masi, A.T.; Carreiro, J.E.; Danneels, L.; Willard, F.H. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 2012, 221, 537–567. [Google Scholar] [CrossRef] [PubMed]
- DePalma, M.J.; Ketchum, J.M.; Saullo, T.R. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med 2011, 12, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Liliang, P.C.; Lu, K.; Liang, C.L.; Tsai, Y.D.; Wang, K.W.; Chen, H.J. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med 2011, 12, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Maigne, J.Y.; Planchon, C.A. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J 2005, 14, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.T.; Haase, L.; Lender, P.A.; Polly, D.W. Minimally Invasive Sacroiliac Joint Fusion: The Current Evidence. Int J Spine Surg 2020, 14, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Belanger, T.A.; Dall, B.E. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: a new technique. J Spinal Disord 2001, 14, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Edinoff, A.N.; Scoon, L.; Youn, S.; Farrell, K.J.; Kaye, A.J.; Shah, R.J.; Cornett, E.M.; Chami, A.A.; Dixon, B.M.; et al. Novel Interventional Techniques for Chronic Pain with Minimally Invasive Arthrodesis of the Sacroiliac Joint: (INSITE, iFuse, Tricor, Rialto, and others). Rheumatol Ther 2021, 8, 1061–1072. [Google Scholar] [CrossRef] [PubMed]
- Wise, C.L.; Dall, B.E. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008, 21, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Cross, W.W.; Delbridge, A.; Hales, D.; Fielding, L.C. Minimally Invasive Sacroiliac Joint Fusion: 2-Year Radiographic and Clinical Outcomes with a Principles-Based SIJ Fusion System. Open Orthop J 2018, 12, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Rahl, M.D.; Weistroffer, J.; Dall, B.E. Analysis of Complications in Sacroiliac Joint Fusions Using FDA 510(k) Cleared Devices. Clin Spine Surg 2022, 35, E363–E367. [Google Scholar] [CrossRef] [PubMed]
- Schoell, K.; Buser, Z.; Jakoi, A.; Pham, M.; Patel, N.N.; Hsieh, P.C.; Liu, J.C.; Wang, J.C. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J 2016, 16, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Shamrock, A.G.; Patel, A.; Alam, M.; Shamrock, K.H.; Al Maaieh, M. The Safety Profile of Percutaneous Minimally Invasive Sacroiliac Joint Fusion. Global Spine J 2019, 9, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Lynch, P.J.; Tubic, G.; Foster, J.M.; Puri, S.; Burnette, C.A.; Block, J.E. Minimally Invasive Inferior Intra-Articular Sacroiliac Joint Fusion: Successful Application of Osseous Stabilization Using Allograft Bone. Orthop Res Rev 2022, 14, 429–435. [Google Scholar] [CrossRef]
- Kiapour, A.; Joukar, A.; Elgafy, H.; Erbulut, D.U.; Agarwal, A.K.; Goel, V.K. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg 2020, 14, 3–13. [Google Scholar] [CrossRef] [PubMed]
- DonTigny, R.L. Function and pathomechanics of the sacroiliac joint. A review. Phys Ther 1985, 65, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Patterson, D.G.; Sayed, D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int J Spine Surg 2021, 15, 514–524. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).