1. INTRODUCTION
The COVID-19 pandemic has threatened the health and lives of millions of people across the globe. On 30th January 2020, the World Health Organization declared a public health emergency of international concern, and governments were urged to prepare for the global spread of Covid-19 from East Asia [
1]. There was a great confusion in understanding the disease in the beginning and due to which there was a huge number of deaths around the world. The primary focus has been on preventing transmission of the virus, finding the right treatment and developing a vaccine. At the beginning of the pandemic limited attention was given to the behavior and psychological changes [
2,
3] which is caused due to lock down, lack of social interactions, online work and education [
4]. This was one of the prominent effects on humans due to pandemic [
5]. The Covid infected respondents and their family members suffered more psychologically than the physical effect. These may range from the understandable anxiety related to health, life and global uncertainty [
6] to the effects of restrictions that have been placed on lives in the form of social distancing [
7], self-isolation and quarantine regimes [
8,
9]. Key workers, younger adults, those living in over-crowded house- holds, and individuals with health conditions (especially mental health conditions) have reported more daily stress. [
10]. According to Grover et.al [
11] more than two-fifths of the people experienced common mental disorders, due to lockdown and the COVID-19 pandemic and there is a need for psychological health services to everyone in the society [
12].
In addition, it is found that the masks and gloves used by the individuals infected by coronavirus keeps piling up. Infectious waste is characterized as any material that is suspected to contain pathogens (bacteria, viruses, parasites or fungi) in sufficient concentration or quantity to cause disease in susceptible hosts [
11,
13]. Millions of contaminated face masks, gloves and materials used in diagnosing, detecting and treating SARS-CoV-2 and other human pathogens are undergoing the irreversible process of becoming infectious waste. This causes environmental and health problems if they are stored, transported and handled improperly [
14,
15]. The quantity of daily face mask usage depends on the number of people residing in a certain country, urban population (per cent), face masks acceptance rate (per cent) and average daily face masks per capita [
16]. Hence there is a need to have a waste collection and safe disposal facility at the care center.
The main objective of this research is to discuss the psychological and behavioral impact on Humans due to outbreak of covid and other pandemics. Based on that, a person focus care center is outlined with the facilities to enhance the wellbeing of persons infected with infectious diseases like covid in addition to medical treatment. Also, it addresses the preventive and precautionary measures to control the transmission of diseases like Covid -19, its variants and other infectious diseases. Existing literature [
17,
18,
19,
20,
21] discusses the physical effects on the individual, but this paper focusses more on psychological effect on human life during the pandemic and lock down period. Based on surveys, interviews among stake holders (people affected with Covid, caretakers and family members of the Covid infected patient, doctors and nurses [
22] who treated Covid infected patients), it is recommended to set up a care center in each region with separate facilities to treat patients with different levels of infections and a counselling center to overcome psychological and behavior changes.
2. METHODOLOGIES
The qualitative and quantitative methods are used to achieve the objective of this research. The quantitate data is collected through surveys conducted in Saudi Arabia and India. Qualitative analysis is based on literature review, interviews and case studies. The research is divided into four different parts, the first part focuses mainly on surveys conducted among adults from 20 -60 years of old. The survey questionnaires were distributed among the audience through electronic media & the data was accumulated in the period from June 2020 to September 2020. This part of the research is to have a better understanding of the safety preferences and precautions of the individual during covid period.
The second part of the research includes extensive literature review to discuss the disposal of different infectious waste by the community and the methods of safe disposal of the infectious waste. In this paper the infectious waste refers to used masks and gloves which did not include the other medical wastes.
Third part of the research includes the results from the interviews conducted among different stakeholders which includes covid patients, and their family members, medical staffs such as doctors, nurses who treated Covid patients, to know the psychological effects and physical damage. The respondents of the interviews are residing in Saudi Arabia and India.
The last part of the research is to suggest the covid care center based on the results of surveys, interviews, case studies and literature. The design of the center focuses on segregation of patients, reduction of stress in patient, physicians, care takers, and the family members. It enhances over all well-being of the individuals and the community.
2.1. Design of questionare
A set of 15 questionnaire was prepared which included multiple-choice questions, opinion scales, questions with yes or no. Based on the choice of the respondents, other questions were linked to yes or no option. Some questions allow the respondents to choose more than one options. The survey was administered using the Google Forms platform from June 2020 to September 2020. The distribution of the questionnaire was conducted through the outreach of social media platforms, e-mail, and standard messaging services. The online survey questionnaire allows the respondents to describe their general demographics such as gender and age.
Information about the preventive measures, precautions, methods to increase immune system, preferential mode transport, types of masks and gloves used, Assessments of social gatherings, effect of stress in pandemic, and methods of disposal of used masks and gloves.
2.2. Statistical Analysis:
The surveys are conducted with the sample size of 283 persons of different age groups ranges from less than 20 to higher than 60 years residing in India and Saudi Arabia. The results of the survey analysis are depicted in the form of percentage. Mean, median, standard deviations and 95% confidence level are calculated using descriptive statistics of the data analysis tool bar in excel for the questionnaire on preventive measures to overcome the spread of infectious diseases, precautions during travel, habits of disposal of used masks and gloves, and measures taken to increase immune system during pandemic. One tail and two tail p values are calculated from t-test paired two samples for the selected above questions. A statistically significant value of P < 0.05 was considered.
2.3. Ethical considerations:
The participation in the surveys and interview is voluntary and the information included with the consent of participants. No personal details are enquired in the research study. There is no risk associated with conducted research.
3. PREVENTION AND PRECAUTIONARY MEASURES
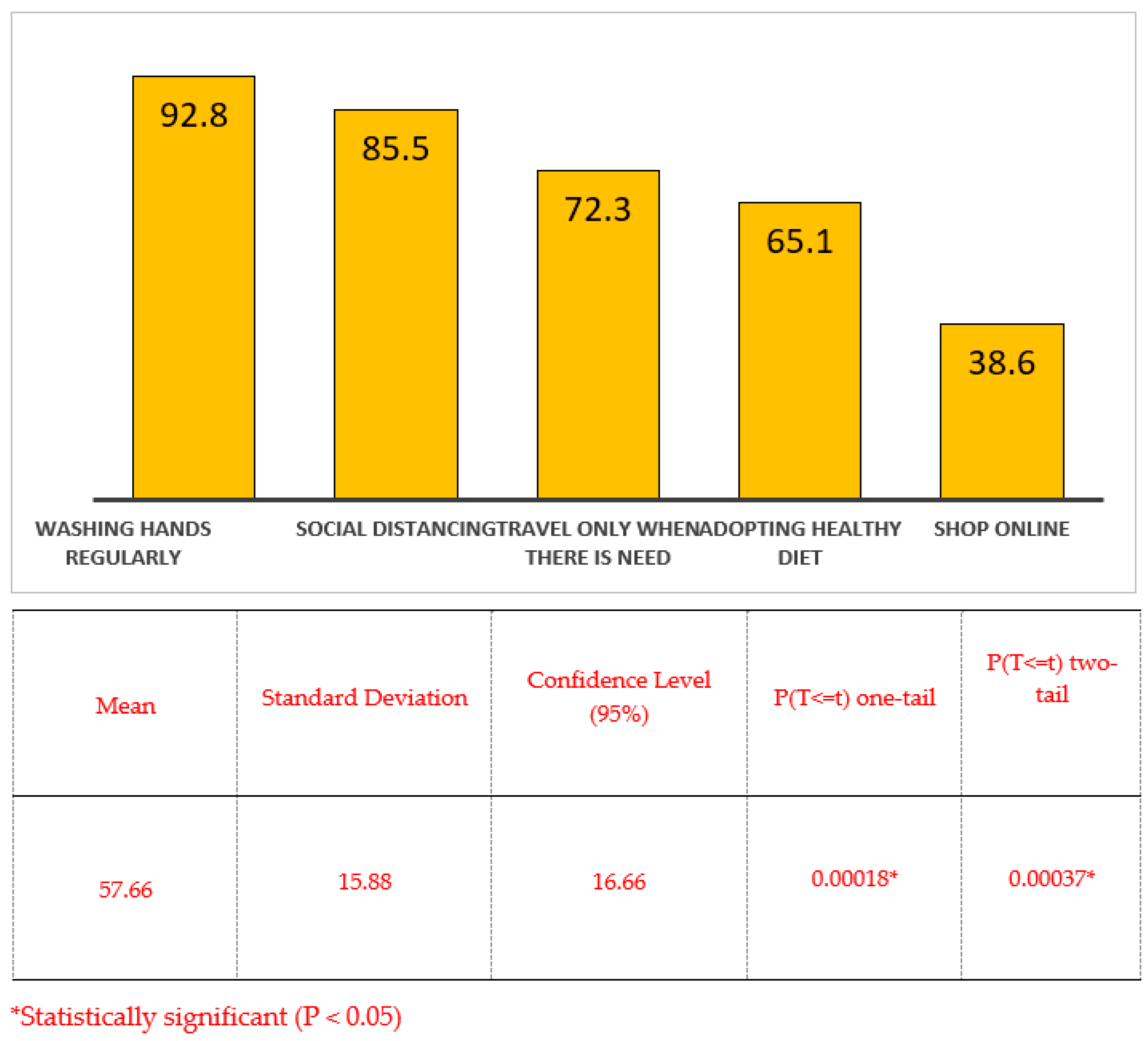
The survey is conducted among individuals in the age group of 20 to 60 years and 83 members participated in the survey in which 43% are male, 57% are female and majority of them are in the age group of 20 to 40 years. Based on the statistics of the survey conducted, the preventive measures preferred by the respondents to overcome the spread of infectious diseases are wash hands regularly, maintain social distancing, travel only when essential and preference to online shopping. (
Figure 1).
The preventive measure to overcome the spread of the infectious were statistically significant (p = 0.00018 for one tail test and 0.00037 for two tail test) as p value is less than 0.05. The median is found to be adopting healthy diet and travel when needed only. The mode is found to be washing hands regularly.
In the article of Bashforth [
23], Dr Micklewright stresses that “the pandemic is far from over. However, many aspects of our day-to-day lives have returned to the normal we knew prior to COVID-19, such as going to social gatherings and working back in the office. He says people would be forgiven for assuming the pandemic is non-existent now since schools and workplaces are open, stadiums are selling tickets again and international borders have opened. However, the decisions for these aspects of life to resume have been difficult, and careful planning was needed to ensure things opened back safely. while vaccines are helping to reduce intensity of infection and minimizes the deaths and spread of COVID-19, the virus is still present”. Now it is very evident, the virus is mutated to different form and more in near future. The muted Covid viruses are more infectious and spread faster than the original [
24].
“Face masks have been shown to prevent the spread of a number of airborne infections, including influenza and SARS," says Dr Micklewright[
23]. It is very clear, the spread of any airborne infection might be reduced by wearing a face mask such as common cold, whooping cough and mumps. Temsah et.al [
25] reported that the knowledge and adherence to personal hygienic practices reduces the anxiety towards covid 19.
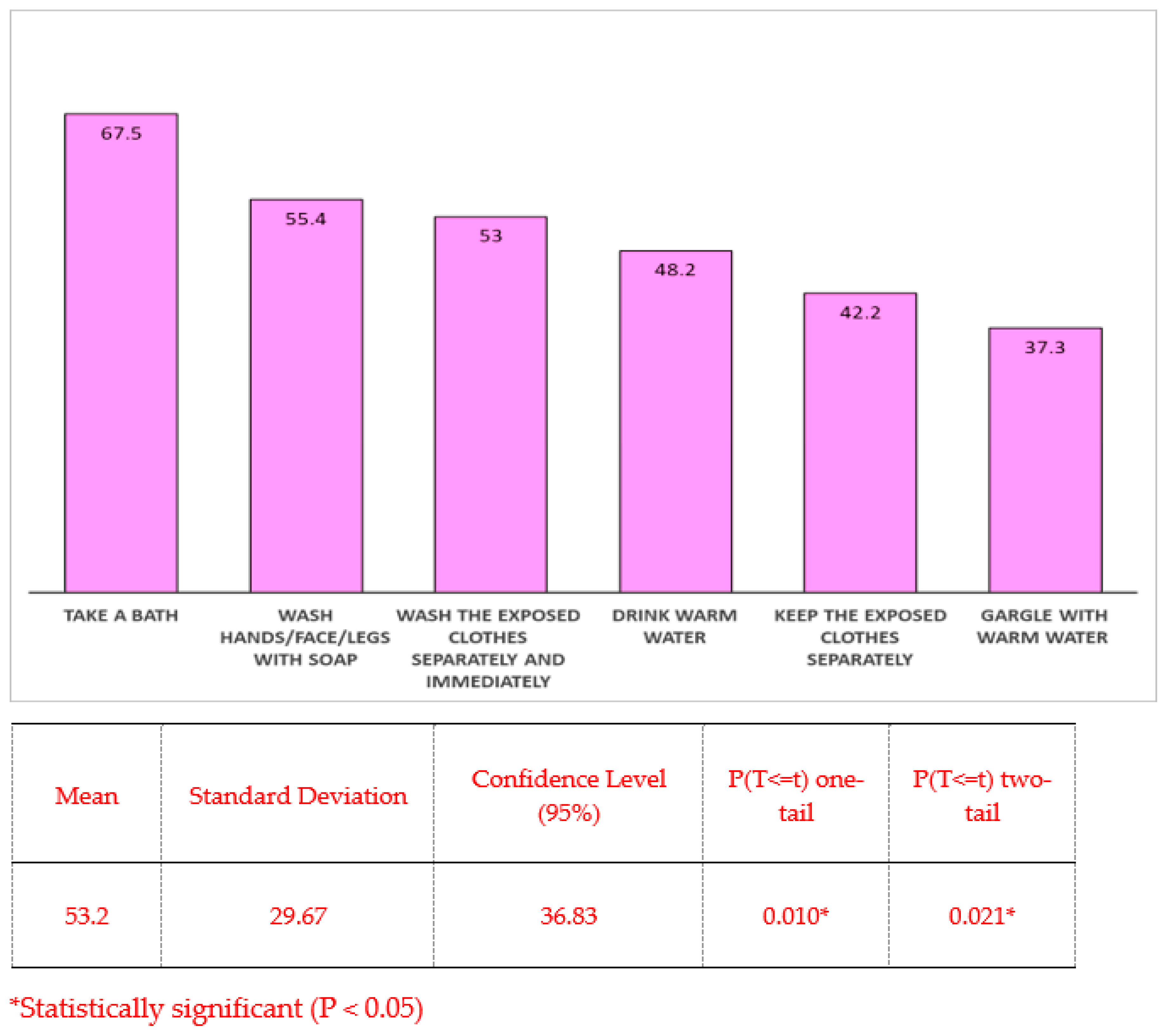
The survey results show most of the respondents follow precautionary measure such as wash the exposed body parts with soap or take bath, drink warm water and keep the exposed cloth separate, once returned from workplace or shopping (
Figure 2). As per Ong et.al., [
26] and Kampf et.al., [
27], 60 to 71 % ethanol sanitizers are effective to eliminate pathogens of infectious diseases such as MERS, SARS, SARS COV-2.
The precautionary measures adopted by the respondents were statistically significant (p = 0.010 for one tail test and 0.021 for two tail test) as p value is less than 0.05. The median of the survey questionnaire is applying sanitizer and most of the respondents prefer to wear mask face as precautionary measure based on the mode calculation.
3.1. Mode of transporation
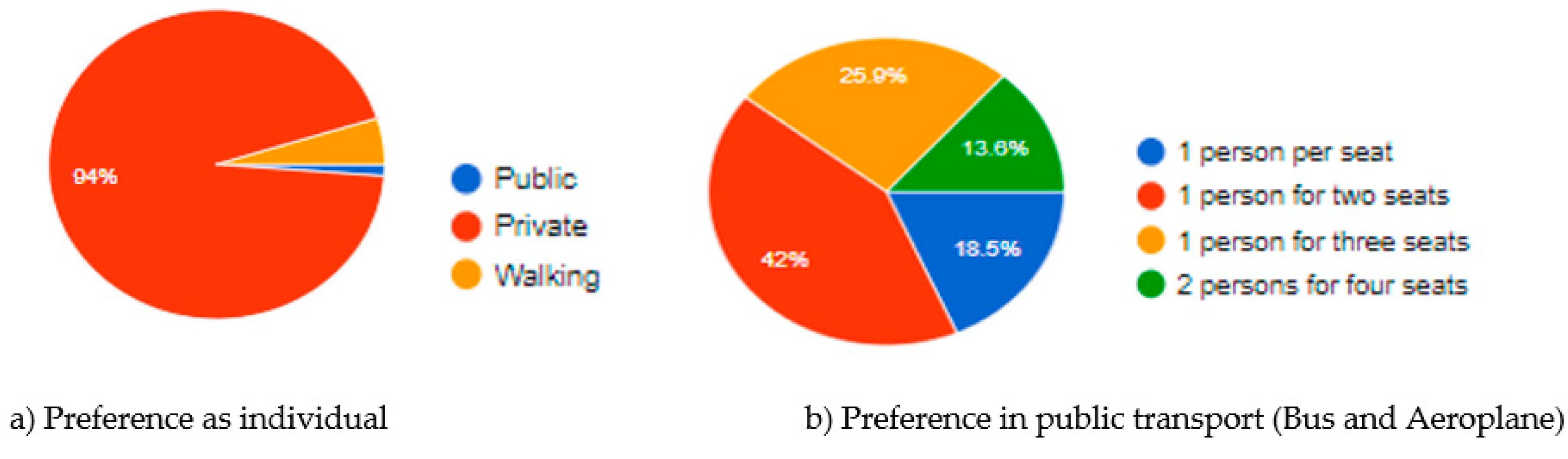
Preferences for mode of transportation results shows that 94% of the respondents prefer to use private vehicles (
Figure 3a) and the least presence is to public transport such as taxi, bus, train and airplane. In public transport the respondents prefer to travel alone whereas in private transport they prefer one person to accompany them. In case of air and bus travel 42%of people prefers one person for every two seats, 26% prefers one person per three seats as shown in
Figure 3 b.
The air quality showed improvement due to reduction in use of transport which is one of the positive effects of Covid.
3.2. Development of Immunity system
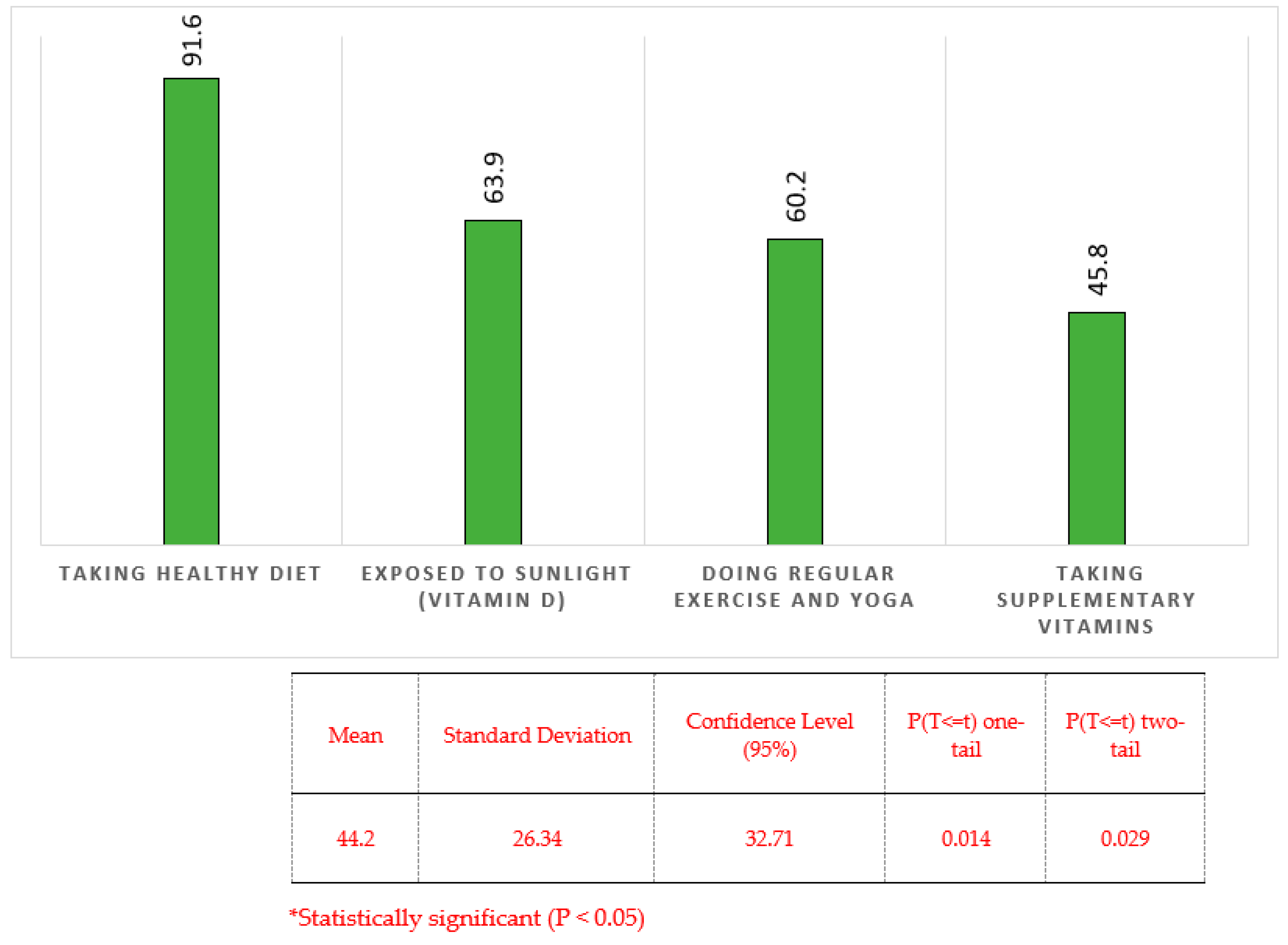
Most of the respondents prefer to take healthy diet, increase in vitamin C intake, regular exercise, steam inhalation, yoga and exposure to sunlight (
Figure 4) to increase their immunity. In one of the covid care centers in India the asymptotic patients, health workers and covid patients were treated using herbal concoction, breathing exercise, yoga. [
28]. The respondents used to take home-made healthy drink or immunity boaster on a periodic basis.
The precautionary measures adopted by the respondents were statistically significant (p = 0.014 for one tail test and 0.029 for two tail test) as p value is less than 0.05. Regular exercise is preferred by most of the respondents based on the statistical analysis.
4. INFECTIOUS WASTES
In this part of paper, study is carried out to find the preference of the people to use different types of personal protective equipment such as face masks and gloves and the awareness of the people about this protective equipment.
4.1. Types of Masks and Gloves
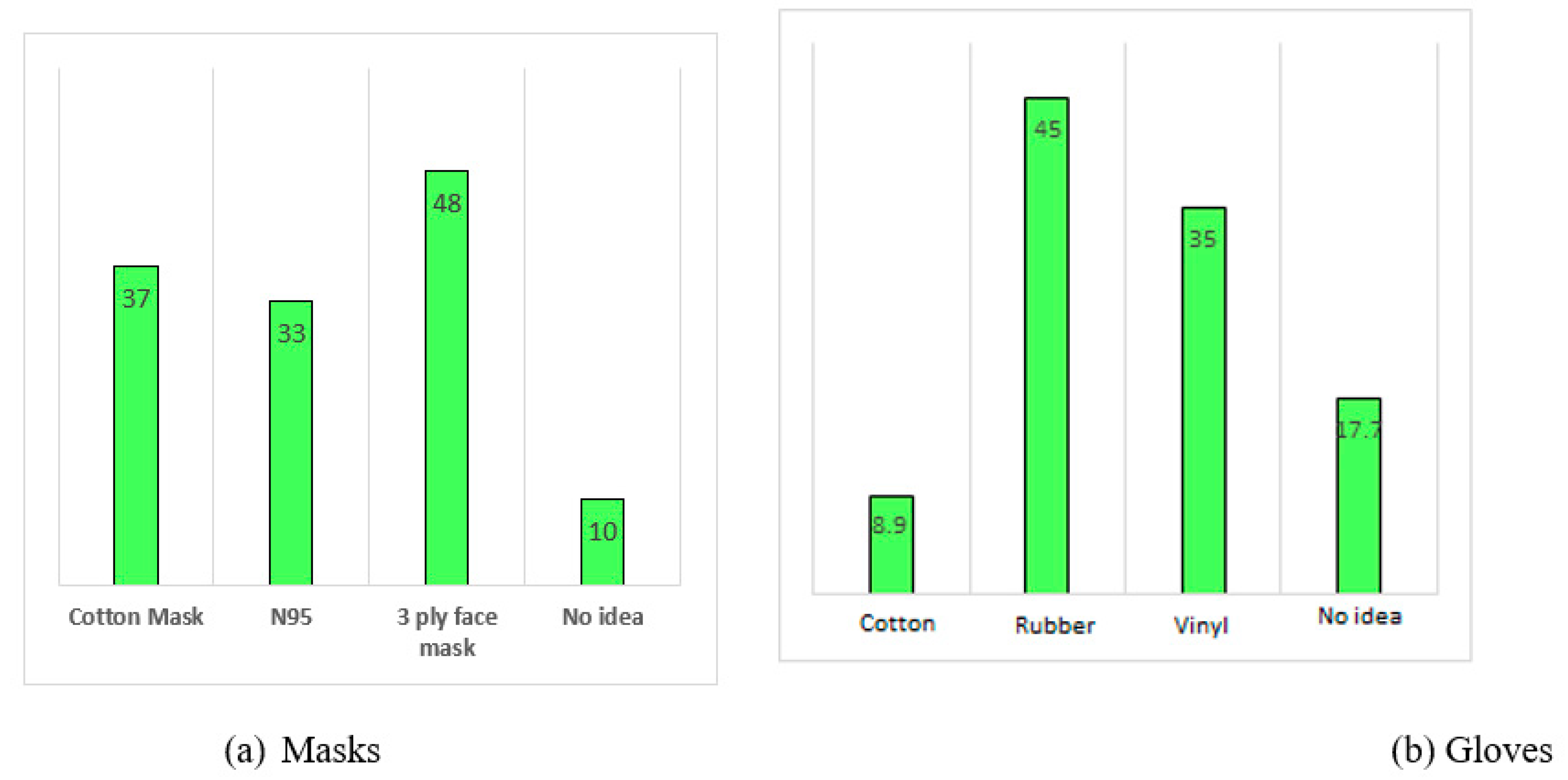
From the survey, it is found that 10-17 % of the respondents are unaware of the type of masks and gloves used by them. More number of people prefer to use 3 ply facemasks, followed by cotton masks and N95 masks as shown in
Figure 5 (a). Most of the respondents prefer to use rubber gloves as mentioned in
Figure 5b compare to the vinyl and cotton gloves. According to Tang [
29], surgical and N95 masks limit and redirect the projection of airborne droplets. Filtration efficiency of surgical masks is 80% against small particles in correlation with the contaminant. SET-C, 2020 [
30] mentioned that wearing masks reduces the spread of flu virus which is in aligned with Bashforth [
23].
4.2. Safe disposal of Infectious waste
Wearing masks has become a global requirement and it has become part of the dress code but the public is mostly not aware of safe disposal of used face masks and gloves and the serious consequences of this waste. Jones [
31] reported that the used face masks are seen on roads, in front of shopping malls, parks, even on beaches These are made of TNT material which is a non-woven fabric and takes many years approximately 400-450 years to decompose. If they are not disposed of properly, it may result in spread of disease, threat to aquatic, terrestrial and atmospheric environments. A surgical mask has the potential to release thousands of microscopic fibers in a marine environment [
32].
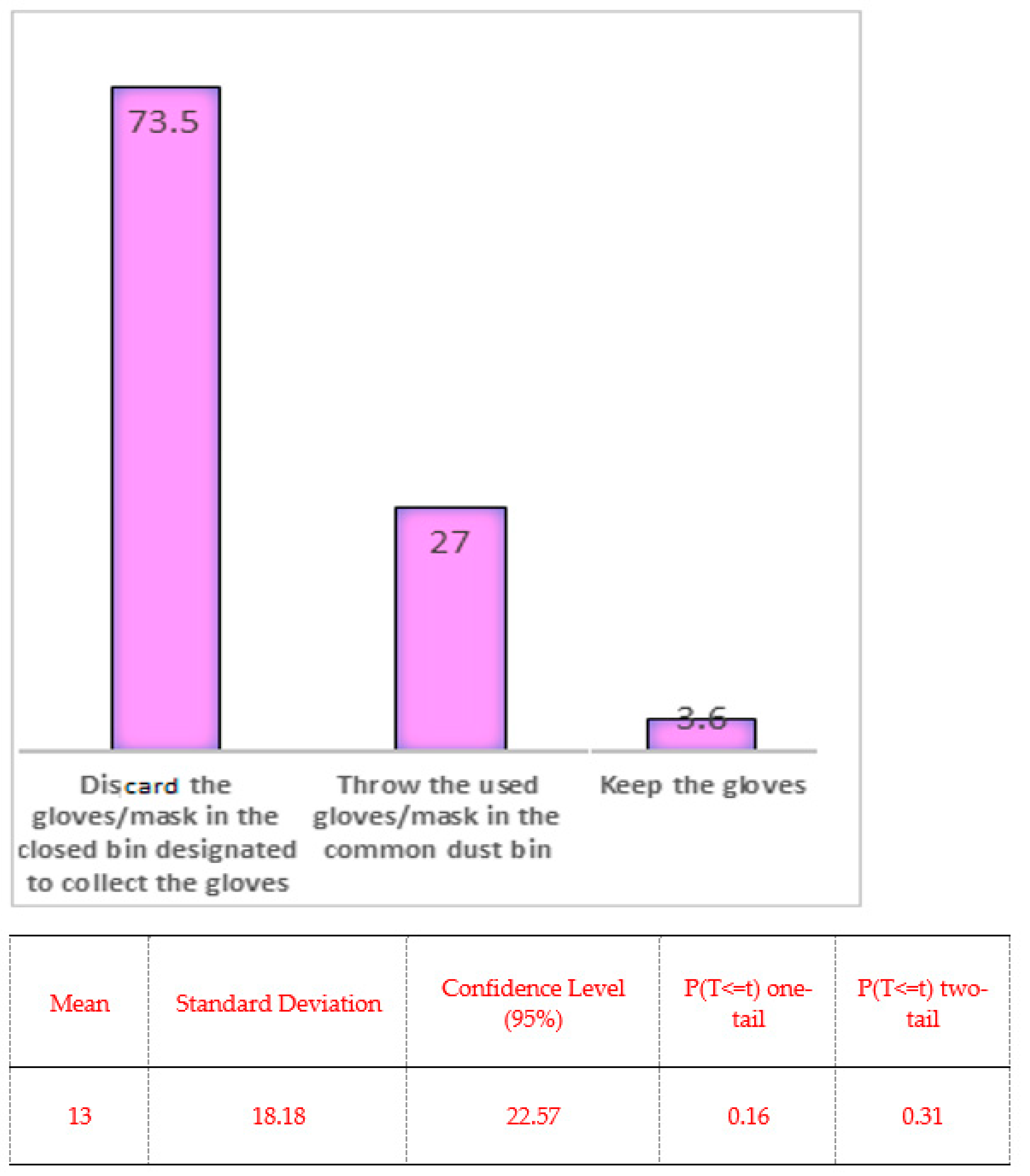
People discard the used gloves and masks either in the closed bin or the one designated for collection (
Figure 6) for effective disposal. An action is required for storage, transportation and safe disposal of used masks. Used masks should be collected in the smart trash cans such as touchless sensor trash cans with double layered waste bags. The persons handling and transporting these waste bags must wear PPE, gloves and follow other precautionary measures as suggested by UNEP [
33]. The used masks can be disposed by dumping in landfills which are separate from the municipal waste landfills and covered with the soil immediately.
Based on the statistically analysis, preference to dispose the used mask and gloves were not statistically significant (p = 0.16 for one tail test and 0.31 for two tail test) as p value is greater than 0.05. The median and mode is disposing the used mask and gloves in the common bin.
5. PSYCHOLOGICAL AND BEHAVIOR CHANGES IN HUMAN
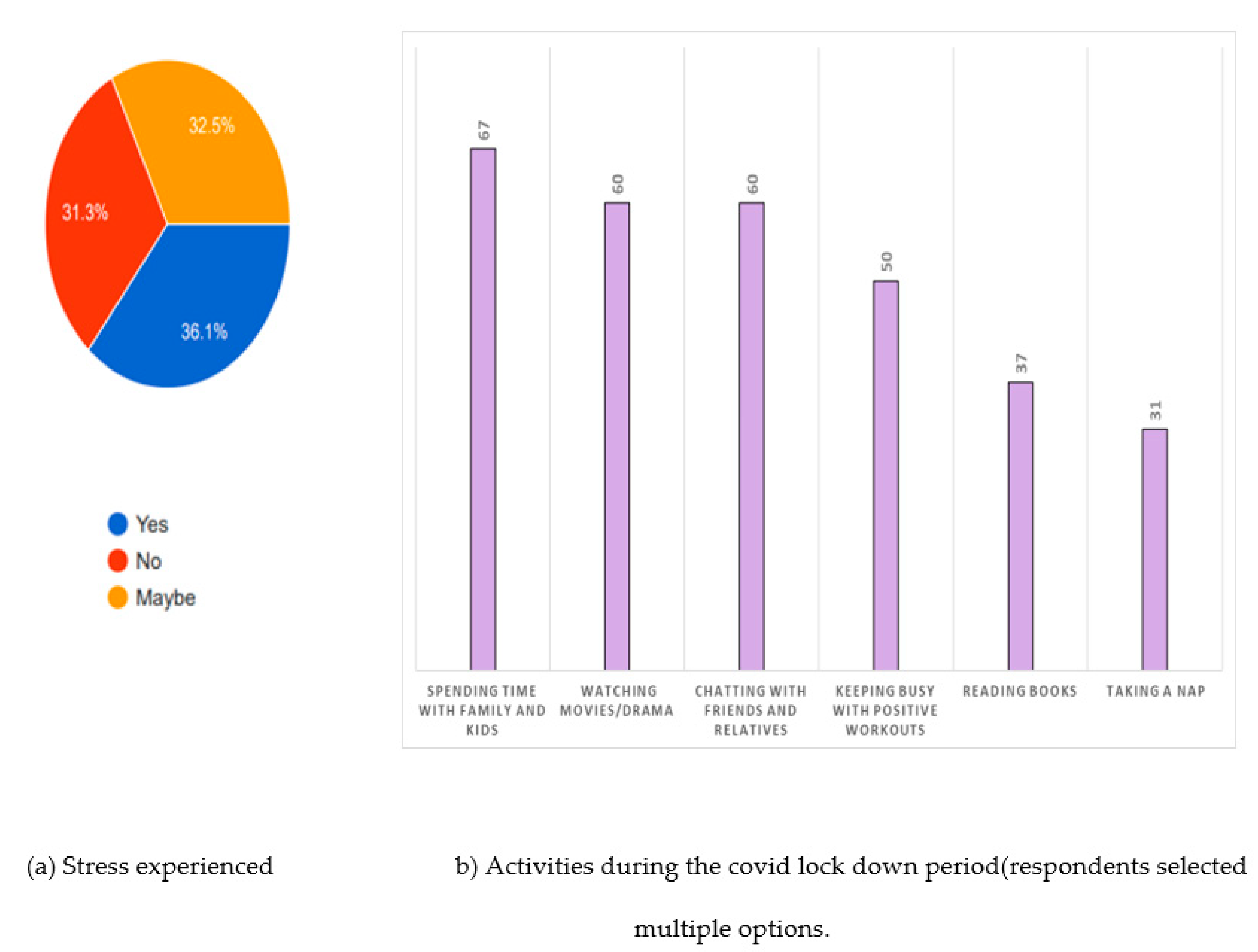
The survey conducted among different stakeholders (during the period of June 2020 till September 2020), it is found that 36% of the respondents are sure that they are subjected to stress during the lockdown period and 32% are not able to sure whether they went through any psychological stability and this indicates that alone 68% of the respondents felt some changes in their behavior and they tried to overcome the stress by different ways. The survey results show that 67% prefer to spend qualitative time with family, 60 % prefer to watch movies or drama, chat with friends and relative through social media.50% prefer to keep themselves busy with positive work out, 37% prefer to read books and 31% prefer to relax by taking nap (
Figure 7b). The above preferences show that the Covid period helps to strengthen the family bonds, which is a positive effect during Covid lock down and restrictions.
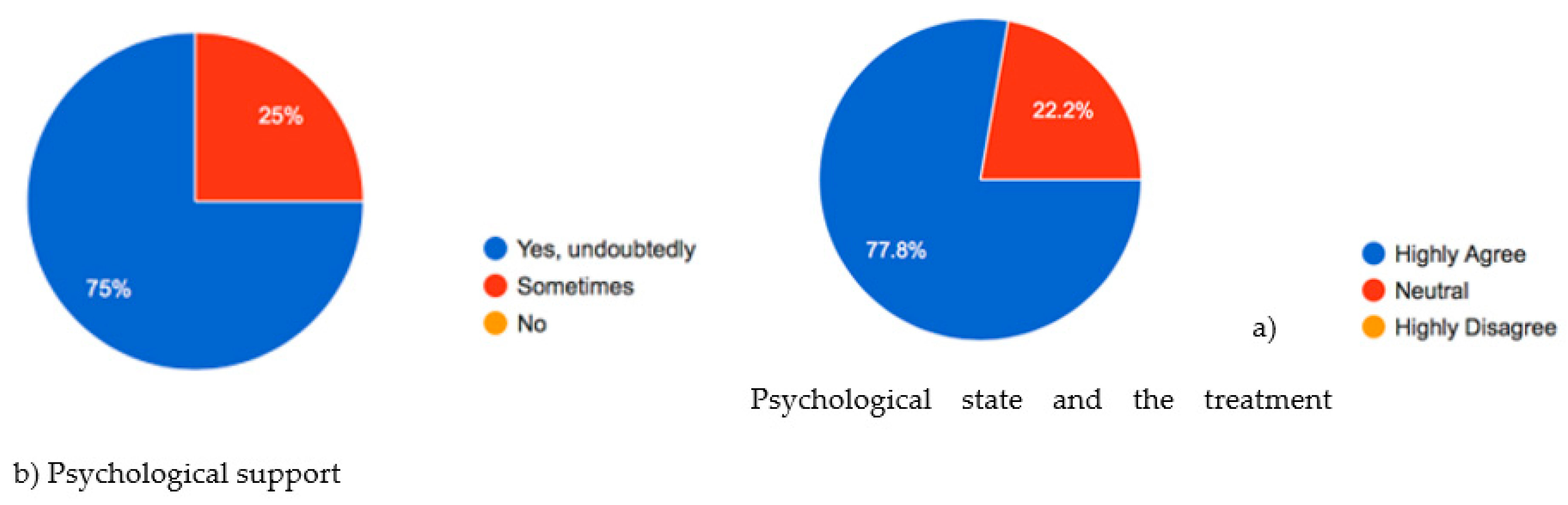
The question is posing to the respondents whether they felt is there any relationship with the treatment and psychological state of the patients and 75% of the respondents think that treatment of the covid or any disease depends on the psychological wellbeing of the patients (
Figure 8a) and all the respondents agree that psychological support can be given to patients to overcome the effects of the disease (
Figure 8b).
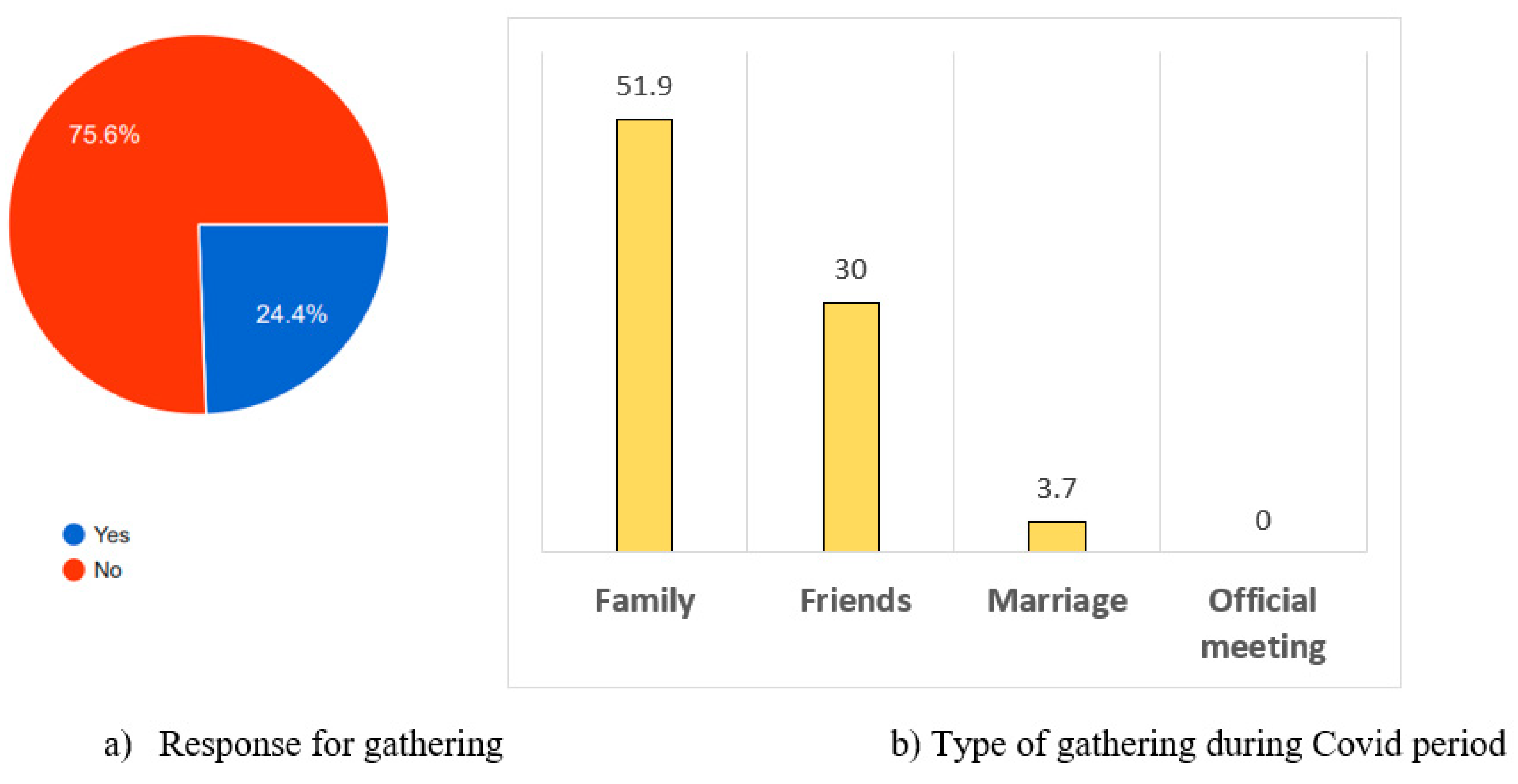
The survey results given in figure 9a shows that 76% of the respondents are against social gatherings during the period of Jan 2020 till Sep 2020. 51.9 % prefers family gatherings, 30% friends’ gatherings ,3.7 % prefers to attend marriage gatherings and none prefers official meetings. which shows less preference to gatherings (
Figure 9b). From the study it is concluded that most of the respondents prefer to avoid official meeting or social gathering during the covid period or during the spread of any infectious diseases.
The results of the interviews conducted among covid affected individuals, their family members/ and care takers are summarized below.
The covid infected respondents and their family members suffered more psychologically than the physical damage. The psychological effects on care takers are different from the patients and the family members as they suffer more physically due to over work, sleepless night and not able to give time to the family. The common psychological effects noticed are depression, anxiety and loneliness in patients and their family members. Some of the physical damages in covid patients are loss of weight, appetite, damage of taste buds, sense of smell, fatigue, dizziness and breathlessness and the extreme damage is the loss of the life. Tesmsah et al., [
25] reported, quarantine people experienced numerous emotional outcomes, including stress, depression, irritability, insomnia, fear, confusion, anger, frustration, boredom, and stigma associated with quarantine, some of which persisted even after end of the quarantine. Also, the family care givers were isolated from social network which creates substantial pressure on their mental health. The guidance to people was not clear and the instructions kept changing during the covid -19 pandemic that increases the confusion, anxiety and stress. There were rumors in the social media which has increased the psychological impact on the people. Humans are social species prefer to live in a community to survive and thrive [
34] when they get disconnected from the society, they will go into depression and the same is reflected during the covid period
Participants from developing countries especially from India, mentioned that due to fear of ostracization with the neighbors and society, forced them not to disclose about the infection to others that has increased the transmission of disease and number of casualties. Also, most of the respondents accepted that their children are most affected physically and psychologically due to pandemic. Lack of physical activity has increased obesity and continuous use of mobile phones, ipod’s or watching TV affected vision. Also, this pandemic greatly affected the cognitive and interpersonal skills of the children. It is noticed, there was a lack of interest in their studies, reduction in social interaction, minimal verbal and non-verbal communication, isolation, lack of team work and collaboration with peers.
The doctors who treated the Covid patients mentioned that the psychological balance is more important for the well-being of the individuals. The persons suffering from major health problems such as hypertension, cardiovascular diseases, diabetes mellitus, Chronic obstructive pulmonary disease (COPD), renal failure, chronic kidney and liver diseases, cancer patients and organ transplant cases suffer from more complications during the SAR COV-2.
6. DESIGN DETAILS OF THE CARE CENTER
The problems faced during the pandemics are insufficient hospitals, inadequate facilities to handle the patients, lack of skills and no preparation to handle such situations. There is a need to set up person centered care to overcome the psychological and behavioral effects on humans. The factors to be consider for design of care center includes type of patients, level of infection, level of care, type of facilities, mobility, complexity of required care and risks presented to the patient and care takers. The care center suggested in this paper has seven units with person centered approach. Angela and Denita [
35,
36] also suggested person centered approach is important in treatment of covid cases and not just hospital focus treatment. The bubble diagram or in other words relationship diagram is a diagrammatic representation of initial planning of the care center with different design aspects and facilities and it is shown in
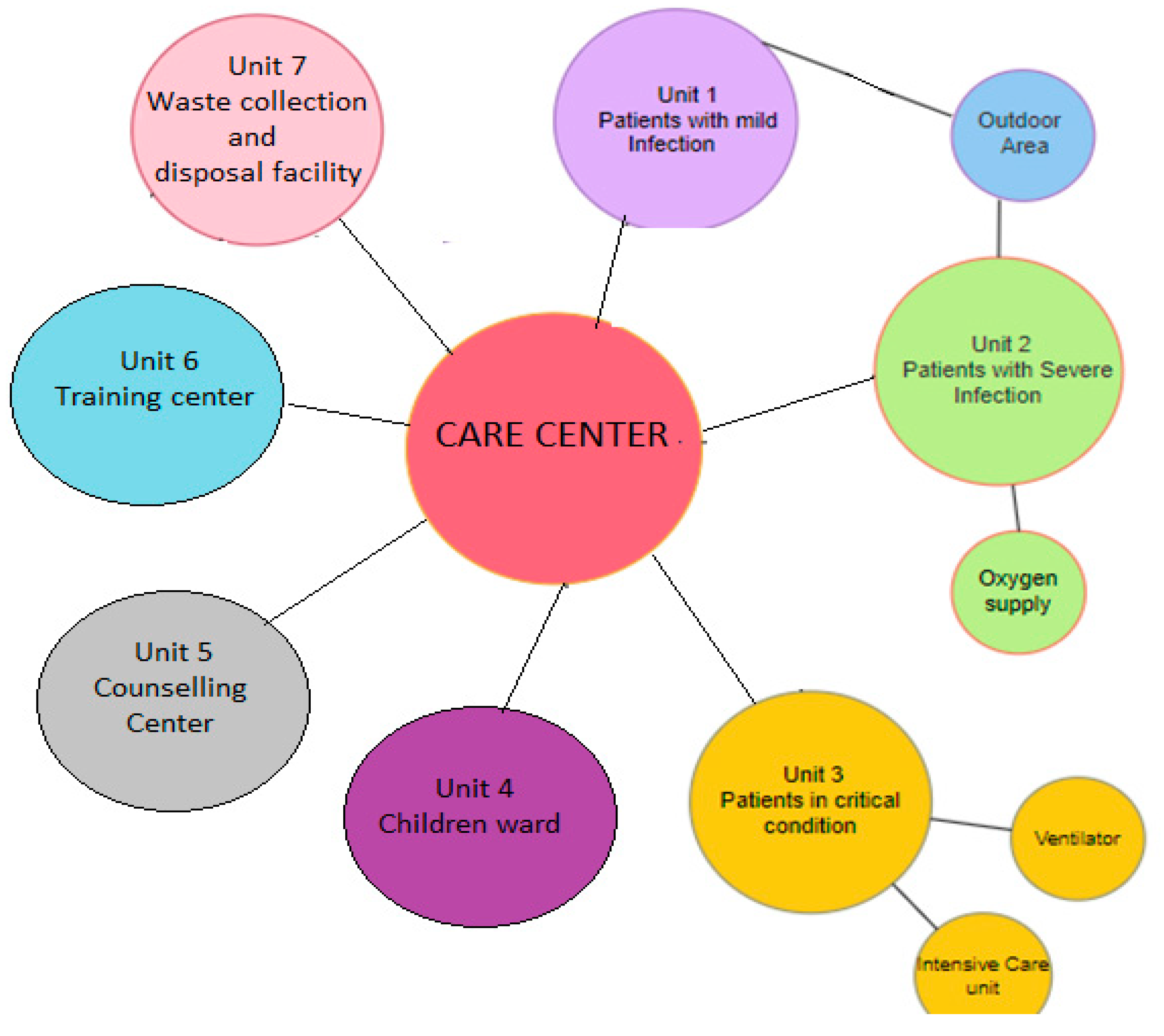
Figure 10.
The care center has seven unit: unit 1 has facilities to treat people suffering from mild infection, provided they don’t have enough space to quarantine themselves in their house. Unit 2 is assigned for patients suffering from severe infection like breathing difficulty. Unit 3 is for critically ill patients who requires ventilator and life support treatment. Unit 4 is specifically design to handle children with different levels of infection and unit 3 and 4 have separate entrances. Unit 5 is incorporated for psychosocial wellbeing of patients, family members and care takers. Unit 6 is the training center for family and voluntary care givers and it is separated from treatment facilities. Unit 7 is for collection and safe disposal of the used masks, gloves, PPE and other such wastes with restricted and separate access from the other end of the care center.
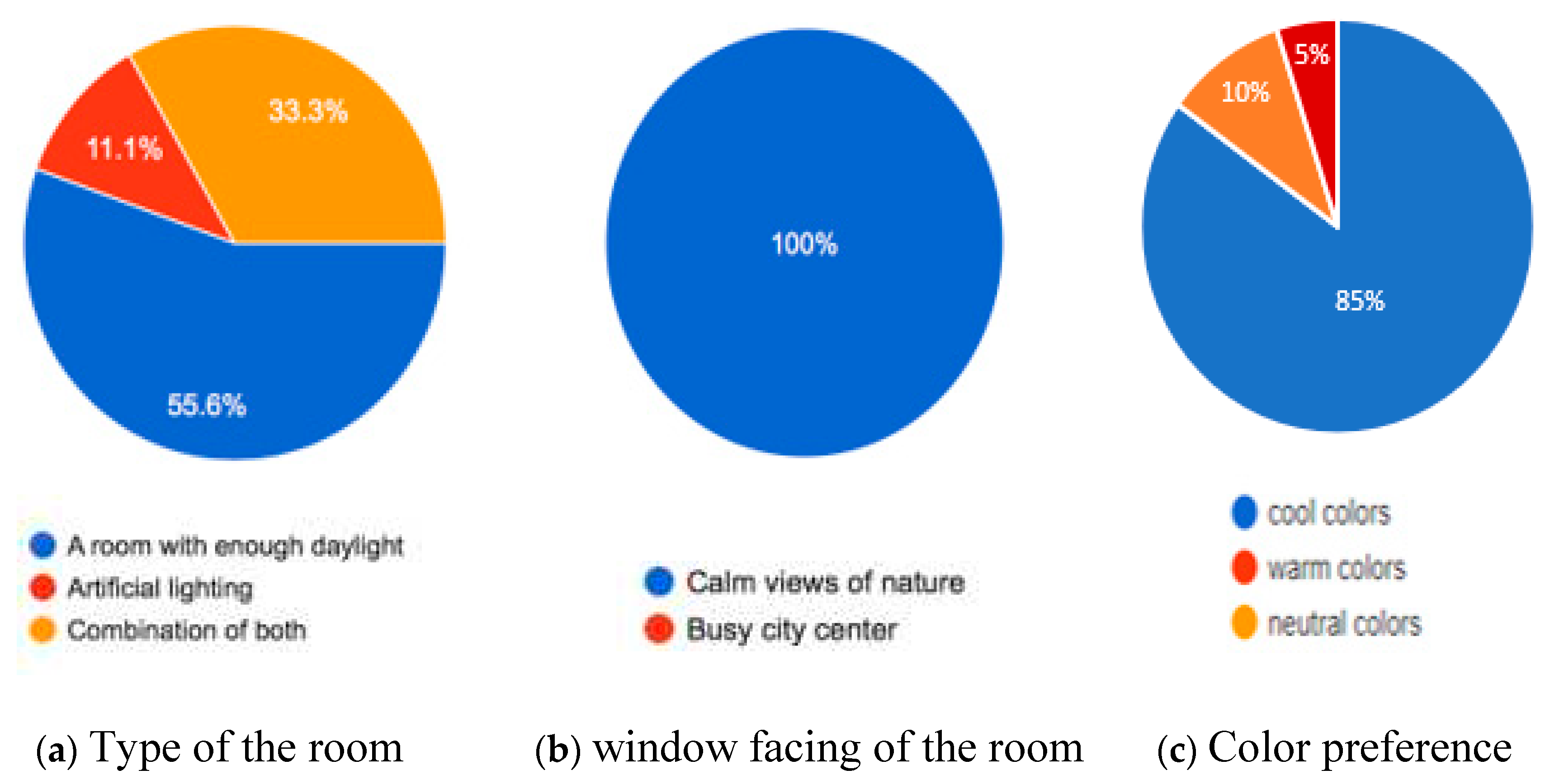
6.1. Design consideration of the room
Patients prefer to have large windows that allows adequate daylight which offers a glimpse of the landscape and eradicate boredom experienced by them (
Figure 11a and b). Most patients stated that indoor plants were essential as they bring the feeling of the outside environment. The caretakers feel that care center need more breathable space as they felt suffocated in small and confined spaces. Most of the patients voted for dim artificial lighting as it does not cause glare or eye irritation as based on previous experience. Moreover, patients have shown an interest in exercising and moving about in their rooms. The design of the person-centered care center includes open court yard, indoor and outdoor garden. The windows in the patients’ room facing the garden and open spaces. There is more response for cool colors than warm and neutral color (
Figure 11c). Cool colors enhance the positive psychological effect. The green color in psychology represents health. It is the most restful color because the eye lens focuses green on the retina, symbolically represents nature and life and is considered the most natural calming, balancing, and relaxing color [
37].
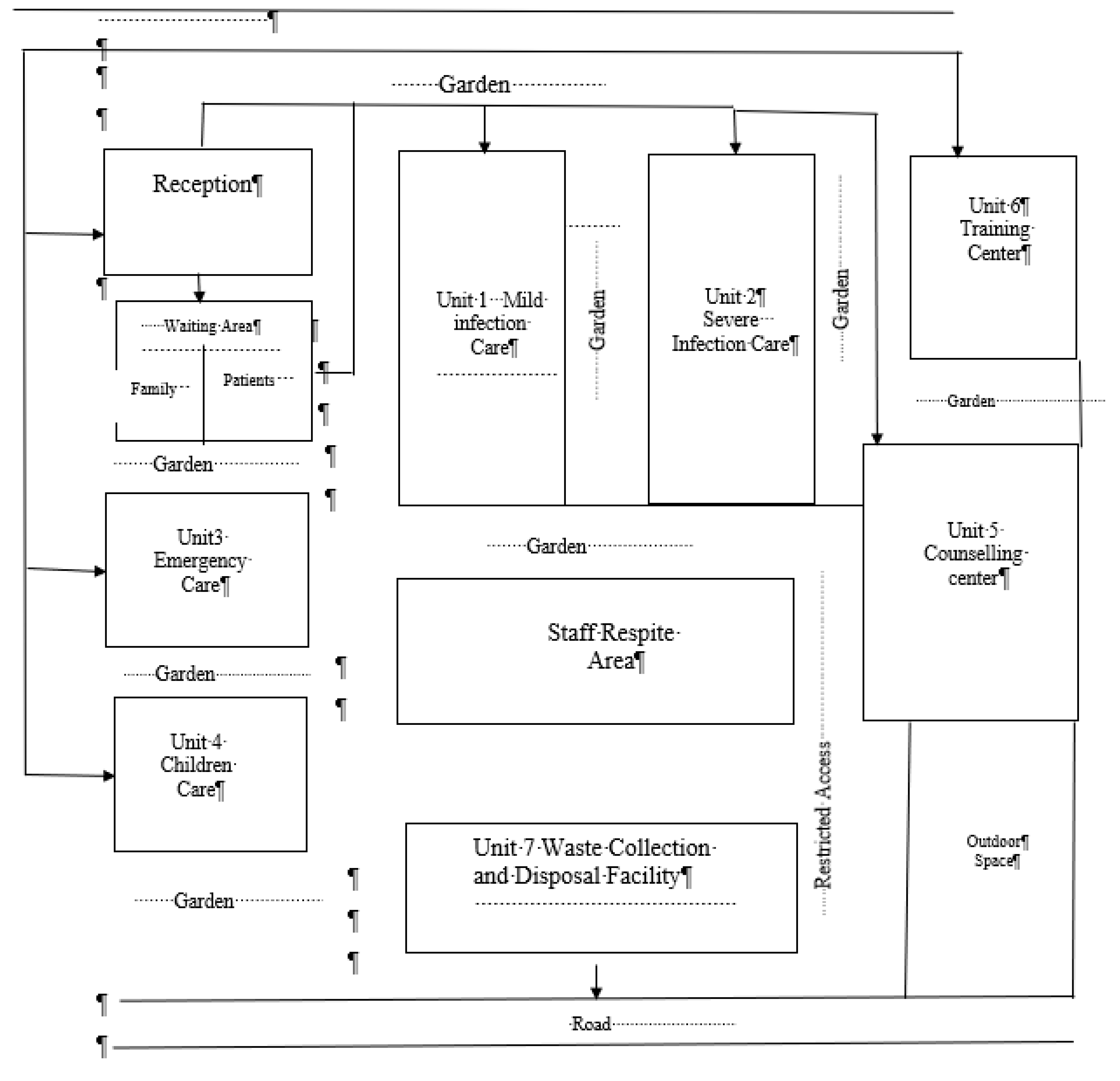
The conceptual diagram of the suggested care center gives more details of each unit with the optimum utilization of the space and it is depicted in figure 12 which has three main access to care center. The first access is to reception, emergency and child care. The second access is directed to the training center. The third access is for collection and disposal facility. Inclusion of family members in the care of vulnerable people involving patients in decisions about their care, make the treatment more effective and efficient. [
35]. So, the family caregivers play key role in the care of patients but the training for respite care was limited which can be overcome by the care center. A separate area should be assigned for registration, family waiting, staff respite. Doctors advocate for the increased size of the waiting rooms. Staff respite includes facilities to store their personnel belongings, change their personnel protective equipment with washroom and relaxing room with garden view. The care center inhouse restricted area for medical storage and preparation room with clear signs.
6.2. Building services in care center:
Controlled air condition is suggested for heating, cooling of the spaces and circulation, ventilation and filtration of air. It is recommended to use nonthermal-plasma reactors to filter the air, instead of the conventional mechanical filters, removes airborne particles through electrostatic capture in highly porous, dialectic media [
38]. Ventilation can be done by two principles: dilution and removal to mitigate the risk of infection. Clean air when added to room dilute the airborne contaminants present in the room, thus reduces the chances of spread of infection. The indoor air should be removed by exhaust fan or high efficiency particulate air filter [
39]. This reduces the pressure inside the patient’s room thus prevents airborne droplets to escape in corridors and other adjacent areas and decreases the transmission of virus.
Day light is important factor in controlling the viability of infectious pathogen due to UV component of the sunlight. It is recommended to provide large windows for the entry of day light and air circulation also the orientation of the windows facing the garden of the care center.
Patient ‘drop-off’ and pick up points have separate access. Drop off point is provided with walk-in facility and multiple screening stations to screen potentially contaminated patients. The exit and entry points for staff are separated from patients. Parking facilities for staff and other vehicles, EMT access, ambulance drop off and pick up is considered in the design. Areas housing medical supplies, hazardous materials, equipment mechanical space and other such places are secured with access to staff only. The security doors with smart lock system must be install to entry and egress in such facilities. The entire care center must be under CCTV surveillance.
The space provided for collection and disposal of medical, non-medical, infectious waste and hazardous waste is separate from main building and has restricted access. It provides facility to clean and disinfect the equipment.
The facilities in the care center are able to cater corona virus cases and also different emerging pathogens such as Ebola, Nipah, Zikah MERS-COV, SARS -COV- 2, H1N1 and so on. It is recommended to set up at least one care center in each region to handle future epidemics or pandemics due to various emerging pathogens.
7. LIMITATIONS
The limitations of this study are: the survey is conducted during specific period and there was no follow up period, the participants of the survey were residing in specific countries, number of samples are limited, voluntary participation and digital platform increases selection biased.
8. CONCLUSIONS
From the study it is evident that the pandemic affected the psychology and behavior of human which has changed the lifestyle of people. During the pandemic, hospitals and the requirements were insufficient to handle the patients. The stake holders were not sufficiently trained to face the situation. This led to the need of designing a care center which can cater the treatment and psychological support under one single umbrella. It is recommended to set up at least one care center in each region of the country with focus on person centered treatment. The recommended care center inhouse facilities for treatment, care, training, counselling for the psychological wellbeing of individuals and the care takers who serves the infected patients. The architectural design details of the space play an important role in the healing process of patients such as orientation of the windows, light, wall and furniture color, indoor plants, out -side view. Also, the design outlines the building services of the care center which includes lightning, mechanical and natural air circulation, air filtration and entry- exit access. For staff it includes training center, respite area for relaxation as well as outdoor space. The selection of the elements improves the physical and psychological state of the patients which enhances the recovery process. The separate road access with restricted entry for disposal of the used medical and non-medical infectious and hazardous waste.
References
- World Health Organization WHO Director-General’s statement on IHR emergency committee on novel coronavirus (2019-nCoV). https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) 2020 (Accessed on,09. June 2020). 20 June.
- Chaturvedi, Kunal, Dinesh Kumar Vishwakarma, and Nidhi Singh. 2021. COVID-19 and its impact on education, social life, and mental health of students: A survey. Children and Youth Services Review 121: 105866.
- Clair, Ruta, Maya Gordon, Matthew Kroon, and Carolyn Reilly. 2021. The effects of social isolation on well-being and life satisfaction during pandemic. Humanities & Social Sciences Communications 8: 28. [CrossRef]
- Elmer, Timon, Kieran Mepham, and Christoph Stadtfeld. 2020. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 15: e0236337. [CrossRef]
- Cao, Wenjun, Ziwei Fang, Guoquiang Hou, Mei Han, Xinrong Xu, Jiaxin Dong, and Jianzhong Zheng. 2020. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research 287: 112934. [CrossRef]
- Yao, J.U. ; Chen, Y. Xu. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020, 7 (4) 21. [CrossRef]
- Bedford, J.; Enria, D.; Giudecca.; Heymann, D. L.; Ihekweazu,C.;Kobinger, G.; Lane, H.C.; Memish,Z.; Oh.M.; Sall, A.A.; Schuchat, A.; Ungchusak, K.; Wieler, L.H. COVID-19: towards controlling of a pandemic. Lancet 2020, 395 (10229), 1015–1018. [CrossRef]
- Gold, R; Styra. Reynolds, J.R.; Garay, S.L.; Deamond, M.K.; Moran, W.; Gold, R; Styra. R.; Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2007, 136, 997–1007. [CrossRef]
- Memish, Z.A.; Ahmed, Q.A.; Schlagenhauf, P.; Doumbia, S.; Khan, A. No time for dilemma: mass gatherings must be suspended., Lancet. 2020, 395 (10231),1191–1192. [CrossRef]
- Fancourt, D.; Bu, F.; Van Mak, H.; Steptoe, A. 2020. Covid 19 Social Study. Results Release 1. University College, London. https://www.nuffieldfoundation.org/wp-content/uploads/2020/05/COVID-19-social-study-results-release-29-May-2020.pdf (Accessed 19 October 2022). 19 October.
- Eria - Economic Research Institute for ASEAN and East Asia. 2020. Strengthening Waste Management Policies to Mitigate the COVID-19 Pandemic. https://www.eria.org/uploads/media/policy-brief/Strengthening-Waste-Management-Policies-to-Mitigate-the-COVID19-Pandemic-.pdf (Accessed 19 October 2022). 19 October.
- Grover, S.; Sahoo, S.;, Mehra, A.; Avasthi, A.; Tripathi, A.; Subramanyan, A.; Pattojoshi, A.; Rao, G.P.; Saha, G.; Mishra, K.K.; Chakraborty, K. .; Rao, N.P.; Vaishnav, M.; Singh, O.P.; Dalal, P.K.; Chadda, R.K.; Gupta, R.; Gautam, S.; Sarkar, S.; Rao, T.S.S.; Kumar, V.; Reddy, Y.C.J. Psychological impact of COVID-19 lockdown: An online survey from India. Indian J Psychiatry. 2020 Jul-Aug;62(4):354-362. Epub 2020 Jul 27. PMCID: . [CrossRef] [PubMed Central]
- Mihai, F.C. Assessment of COVID-19 waste flows during the emergency State in Romania and related public health and environmental concerns. Int. J. Environ. Res. Publ. Health. 2020, 17(15), 5439. [CrossRef]
- Nzediegwu, C.; Chang, S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020,161,104947. [CrossRef]
- Singh, N.; Tang, Y.; Zhang, Z.; Zheng, C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020, 163,105071. 2020; 163, 105071. [CrossRef]
- Sangkham, S. Face mask and medical waste disposal during the novel COVID-19 pandemic in Asia, Case Studies in Chemical and Environmental Engineering, 2020, 2,100052. [CrossRef]
- Pretto, C. R., Morais, K. C. P. de, Mendes, V. C., Paiva, A. L., Silva, R. M. da, & Beck, C. L. C. (2022). The Impact of COVID-19 on the Physical Well-being of Nursing and Medical Personnel: An Integrative Review. Aquichan, 22(2), e2225. [CrossRef]
- Bentlage, E., Ammar, A., How, D., Ahmed, M., Trabelsi, K., Chtourou, H., et al. (2020). Practical recommendations for maintaining active lifestyle during the COVID-19 pandemic: a systematic literature review. Int. J. Environ. Res. Public Health 17:6265. [CrossRef]
- Bourdas, D. I., and Zacharakis, E. D. (2020). Impact of COVID-19 lockdown on physical activity in a sam-ple of greek adults. Sports 8:139. [CrossRef]
- Hanke, A. A., Sundermeier, T., Boeck, H. T., Schieffer, E., Boyen, J., Braun, A. C., et al. (2020). Influence of officially ordered restrictions during the first wave of COVID-19 pandemic on physical activity and quality of life in patients after kidney transplantation in a telemedicine based aftercare program—A KTx360° sub study. Int. J. Environ. Res. Public Health 17:9144. [CrossRef]
- Lesser, I. A., and Nienhuis, C. P. (2020). The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int. J. Environ. Res. Public Health 17:3899. [CrossRef]
- Shaukat, N., Ali, D.M. & Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 13, 40 (2020). [CrossRef]
- Bashforth, E. Should you wear a face mask if you have a cold this winter? Article in Patient Health Information.2021 https://patient.info/news-and-features/should-you-wear-a-face-mask-if-you-have-a-cold-this-winter (Accessed 9, October 2022). 20 October.
- Miller, J.K.; Elenberg, K.; Dubrawski, A. Forecasting emergence of COVID-19 variants of concern. PLos one . 2022, 17(2): e0264198. [CrossRef]
- Temsah, M.H.; Alhuzaimi, A. N.; Alamro, N.; Alrabiaah,A.; Al-Sohime,F.; Alhasan, K.1.;Kari, J.A.; Almaghlouth, I.; Aljamaan, F.; Jamal, A.; Al Amri,M.; Barry, S.A.; Somily,A.M.; Al-Zamil, F. Knowledge, attitudes and practices of healthcare workers during the early COVID-19 pandemic in a main, academic tertiary care center in Saudi Arabia. Epidemiology and Infection,2020 148, e203, 1–9. [CrossRef]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA, 2020, 323(16),1610-1612.
- Kampf, G. Efficacy of ethanol against viruses in hand disinfection. J Hosp Infect. 2018, 98 (4), 331–338. [CrossRef]
- Newspaper Article, Mint, retrieved from https://www.livemint.com/news/india/nearly-6-000-covid-patients-cured-through-siddha-medicine-in-tamil-nadu-11597051467504.html (assessed 10 Aug, 2022).
- Tang, J.W.; Liebner, T.J.; Craven, B.A.; Settles, G.S.A. Schlieren optical study of the human cough with and without wearing masks for aerosol infection control. J. R. Soc. Interface6 (Suppl 6), 2009, S727–S736. [CrossRef]
- SET-C Science in Emergencies Tasking – COVID-19 Face masks and coverings for the general public: Behavioural knowledge, effectiveness of cloth coverings and public messaging. The Royal Society, London, UK (2020). https://royalsociety.org/-/media/policy/projects/set-c/set-c-facemasks.pdf.
- Jones, M. A. Report on More than 1.56 billion face masks could end up polluting oceans, CIV news, Dec 7, 2020 https://www.ctvnews.ca/sci-tech/more-than-1-56-billion-face-masks-could-end-up-polluting-oceans-report-1.5221239.
- Francesco, S.; Veronelli, M.; Raguso, C.; Barana,D.; Galli, P.; Lasagni,M. The release process of microfibers: from surgical face masks into the marine environment, Environmental advance 2021, 4, 100042. [CrossRef]
- UNEP, Waste Management during the COVID-19 pandemic. Ministry of Environment (MOE), Government of Japan through United Nations Environment Programme International Environmental Technology Centre (UNEP- IETC).2020 http://wedocs.unep.org/bitstream/handle/20.500.11822/33416/WMC-19.pdf?sequence= 1&isAllowed=y. (Accessed 9 October 2022). 9 October.
- The cooperative human, Nature Human Behavior, Editorial Publication, 2018, 2, 427–428. [CrossRef]
- Coulter, A.; Richards,T. Care during covid-19 must be humane and person centred, BMJ 2020,370:m3483. [CrossRef]
- Cepiku,D.; Giordano,P.; Bovaird, T.; Loeffler, E. New development: Managing the Covid-19 pandemic—from a hospital-centered model of care to a community co-production approach, Public Money & Management, 2021, 41(1), 77- 80. [CrossRef]
- Jonauskaite, D., Tremea, I., Bürki, L., Diouf, C. N., & Mohr, C. (2020). To see or not to see: importance of color perception to color therapy. Color Research & Application, 45(3), 450-464.
- Bergeron, V.; Reboux, G.; Poirot, J.L.; Laudinet, N. Decreasing airborne contamination levels in high-risk hospital areas using a novel mobile air-treatment unit. Infect Control Hosp Epidemiol. 2007,28(10):1181-6. Epub 2007 Aug 3. [CrossRef] [PubMed]
- Dietz, L.; Horve, P.F.; Coil, D.A.; Fretz, M.; Eisen, J.A.; Den, V.; Wymelenberg, K. Novel Coronavirus (COVID-19) Pandemic: Built Environment Considerations To Reduce Transmission. mSystems. 2020 Apr 7;5(2): e00245-20. https://doi.org/ 10.1128/mSystems.00245-20. Erratum in: mSystems. 2020, 5(3). [CrossRef] [PubMed] [PubMed Central]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).