Submitted:
25 April 2023
Posted:
26 April 2023
Read the latest preprint version here
Abstract
Keywords:
INTRODUCTION
METHODS
Study design
Health care setting
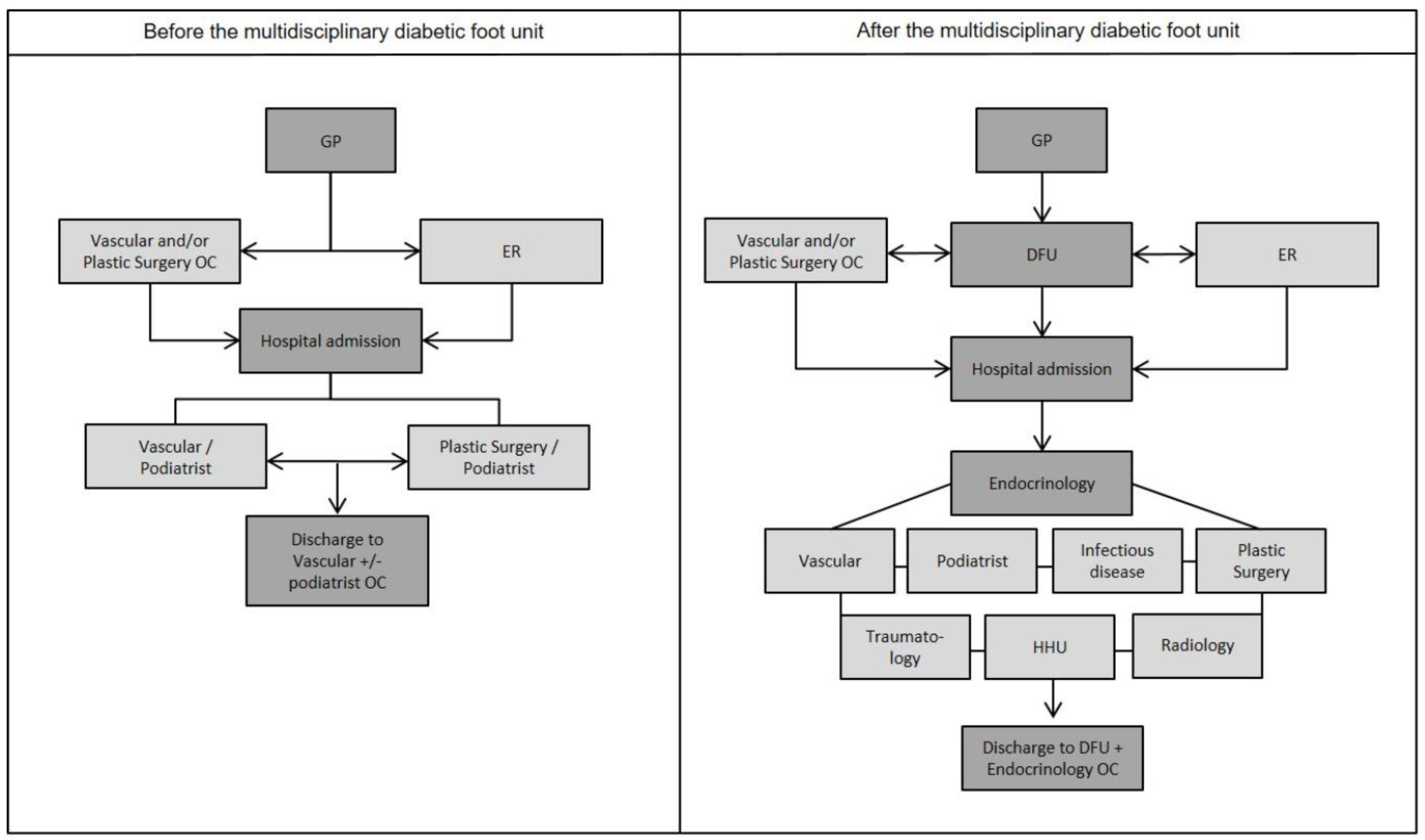
Circuit of a Diabetic Foot patient before and after the Multidisciplinary Diabetic Foot Clinic implementation
Cost analysis
RESULTS
Characteristics of amputee patients
In-hospital care characteristics
Estimation of direct and indirect costs
Total costs per patient
Sensitivity Analysis
DISCUSSION
Conclusions
Author Contributions
Source of Funding
Conflicts of Interest
References
- World Health Organization. (16 September 2022). Diabetes. https://www.who.int/news-room/fact-sheets/detail/diabetes. 16 September.
- Saeedi, P., Petersohn, I., Salpea, P., Malanda, B., Karuranga, S., Unwin, N., ... & IDF Diabetes Atlas Committee. (2019). Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes research and clinical practice, 157, 107843. [CrossRef]
- Nieto-Gil, P., Ortega-Avila, A. B., Pardo-Rios, M., Cobo-Najar, M., Blasco-Garcia, C., & Gijon-Nogueron, G. (2018). Hospitalisation cost of patients with diabetic foot ulcers in valencia (Spain) in the period 2009–2013: a retrospective descriptive analysis. International journal of environmental research and public health, 15(9), 1831. [CrossRef]
- Schaper, N. C., van Netten, J. J., Apelqvist, J., Bus, S. A., Hinchliffe, R. J., Lipsky, B. A., & IWGDF Editorial Board. (2020). Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews, 36, e3266. [CrossRef]
- Zhang, P., Lu, J., Jing, Y., Tang, S., Zhu, D., & Bi, Y. (2017). Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Annals of medicine, 49(2), 106-116. [CrossRef]
- Syed, M. H., Salata, K., Hussain, M. A., Zamzam, A., de Mestral, C., Wheatcroft, M., ... & Al-Omran, M. (2020). The economic burden of inpatient diabetic foot ulcers in Toronto, Canada. Vascular, 28(5), 520-529. [CrossRef]
- González, P., Faure, E., & Del Castillo, A. (2006). Coste de la diabetes mellitus en España. Medicina clínica, 127(20), 776-784.
- Wang, C., Mai, L., Yang, C., Liu, D., Sun, K., Song, W., ... & Yan, L. (2016). Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC endocrine disorders, 16(1), 1-8. [CrossRef]
- Cahn, A., Elishuv, O., & Olshtain-Pops, K. (2014). Establishing a multidisciplinary diabetic foot team in a large tertiary hospital: a workshop. Diabetes/Metabolism Research and Reviews, 30(5), 350-353. [CrossRef]
- Joret, M. O., Osman, K., Dean, A., Cao, C., van der Werf, B., & Bhamidipaty, V. (2019). Multidisciplinary clinics reduce treatment costs and improve patient outcomes in diabetic foot disease. Journal of vascular surgery, 70(3), 806-814. [CrossRef]
- Husereau, D., Drummond, M., Petrou, S., Carswell, C., Moher, D., Greenberg, D., ... & Loder, E. (2013). Consolidated health economic evaluation reporting standards (CHEERS) statement. International journal of technology assessment in health care, 29(2), 117-122. [CrossRef]
- López Seguí, F., Vidal-Alaball, J., Sagarra Castro, M., García-Altés, A., & García Cuyàs, F. (2020). General practitioners’ perceptions of whether teleconsultations reduce the number of face-to-face visits in the Catalan public primary care system: retrospective cross-sectional study. Journal of medical Internet research, 22(3), e14478. [CrossRef]
- Generalitat de Catalunya. Ordre SLT/71/2020, de 2 de juny, per la qual es regulen els supòsits i conceptes facturables i s'aproven els preus públics corresponents als serveis que presta l'Institut Català de la Salut. 2020. Available at: https://cido.diba.cat/legislacio/10263520/ordre-slt712020-de-2-de-juny-per-la-qual-es-regulen-els-suposits-i-conceptes-facturables-i-saproven-els-preus-publics-corresponents-als-serveis-que-presta-linstitut-catala-de-la-salut-departament-de-salut . Accessed 13 Dec 2022.
- Idescat. Annual indicators. Annual gross salary. By sex and age groups. 2019. (2021, July 5). https://www.idescat.cat/indicadors/?id=anuals&n=10400&t=201900.
- Idescat. Indicators of the economic situation. Activity, employment and unemployment rates. By sex and age groups. Q4/2019. (2020, January 28). https://www.idescat.cat/indicadors/?id=conj&n=10218&t=201904. 28 January.
- Prompers, L., Huijberts, M., Schaper, N., Apelqvist, J., Bakker, K., Edmonds, M., ... & Tennvall, G. R. (2008). Resource utilisation and costs associated with the treatment of diabetic foot ulcers. Prospective data from the Eurodiale Study. Diabetologia, 51, 1826-1834. [CrossRef]
- Jafary, M. R., Amini, M. R., Sanjari, M., Aalaa, M., Goudarzi, Z., Najafpour, Z., & Mohajeri Tehrani, M. R. (2020). Comparison home care service versus hospital-based care in patients with diabetic foot ulcer: an economic evaluation study. Journal of Diabetes & Metabolic Disorders, 19, 445-452. [CrossRef]
- Vallejo-Torres, L., García-Lorenzo, B., & Serrano-Aguilar, P. (2018). Estimating a cost-effectiveness threshold for the Spanish NHS. Health economics, 27(4), 746-761.
- Vallejo-Torres, L., García-Lorenzo, B., Rivero-Arias, O., & Pinto-Prades, J. L. (2020). The societal monetary value of a QALY associated with EQ-5D-3L health gains. The European Journal of Health Economics, 21(3), 363-379. [CrossRef]
- Generalitat de Catalunya. Departament de Salut. (2016). Pla de Salut de Catalunya 2016-2020: Un sistema centrat en la persona: públic, universal i just. https://www.salutweb.gencat.cat/url/pladesalut.
- Magliano, D., & Boyko, E. J. (2021). IDF Diabetes Atlas (10.a ed.). International Diabetes Federation.
- Rinkel, W. D., Luiten, J., van Dongen, J., Kuppens, B., Van Neck, J. W., Polinder, S., ... & Coert, J. H. (2017). In-hospital costs of diabetic foot disease treated by a multidisciplinary foot team. Diabetes research and clinical practice, 132, 68-78. [CrossRef]
- Mata, M., Antoñanzas, F., Tafalla, M., & Sanz, P. (2002). El coste de la diabetes tipo 2 en España: El estudio CODE-2. Gaceta Sanitaria, 16, 511-520. [CrossRef]
- Nason, G. J., Strapp, H., Kiernan, C., Moore, K., Gibney, J., Feeley, T. M., ... & Tierney, S. (2013). The cost utility of a multi-disciplinary foot protection clinic (MDFPC) in an Irish hospital setting. Irish journal of medical science, 182, 41-45. [CrossRef]
| Resource | Cost | Unit |
|---|---|---|
| Emergency room | €194 | Per visit |
| Outpatient clinic | €77 | Per visit |
| DFC | €77 | Per visit |
| Hospitalization | €674 | Per staying day |
| ICU | €1,037 | Per visit |
| Amputation | €2,950 | Per intervention |
| Median gross patient salary | €71 | Per staying day |
| Antibiotic | €1,197 | Per hospital stay |
| QALY | 0.29 units | Per amputation |
| General | pre-MDFU (n=150) | MDFU (n=82) | p | |
|---|---|---|---|---|
| Age (ye ars, SD) | 71.4 (10.7) | 70.6 (11.12) | 70 (9.98) | 0.673 |
| Men (%) | 68.1 | 62.7 | 78 | 0.024 |
| BMI (kg/m2) (N, SD) | 28.14 (6.01) | 28.81 (6.39) | 27.22 (5.38) | 0.206 |
| T2D (%) | 95.9 | 96.7 | 94.3 | 0.649 |
| Time of evolution of T2D (years, SD) | 13.4 | 12 (8.21) | 15.7 (9.80) | 0.043 |
| HbA1c (%, SD) | 6.85 (1.27) | 6.55 (1.02) | 6.95 (1.34) | 0.259 |
| Nephropathy (%) | 67.2 | 63.5 | 73.9 | 0.186 |
| Retinopathy (%) | 65.1 | 65.5 | 64.3 | 0.982 |
| Diabetic Foot (%) | 71.3 | 72.6 | 70 | 0.843 |
| Ischemic heart disease (%) | 37 | 38.1 | 35.1 | 0.764 |
| Stroke (%) | 21.9 | 22.5 | 20.8 | 0.897 |
| Peripheral arterial disease (%) | 95.4 | 94.4 | 97.4 | 0.491 |
| Charcot foot (%) | 0.9 | 0.7 | 1.3 | 0.759 |
| Oral antidiabetic agents (%) | 65.9 | 71.2 | 56 | 0.037 |
| Insulin (%) | 77.8 | 73.8 | 85.3 | 0.076 |
| Oral antidiabetic agents + insulin (%) | 44.7 | 45.7 | 42.7 | 0.776 |
| Hypertension (%) | 93.1 | 91.4 | 96.1 | 0.297 |
| Dyslypidemia (%) | 73.2 | 71.9 | 75.3 | 0.706 |
| Expected value before MDFC | % of total | Expected value after MDFC | % of total | ||
|---|---|---|---|---|---|
| Direct costs | Antibiotic | €874 | 5.92% | €407 | 6.80% |
| Emergency room | €116 | 0.79% | €78 | 1.30% | |
| Outpatient clinic | €31 | 0.21% | €15 | 0.25% | |
| Hospitalization | €8,979 | 60.80% | €2,733 | 45.66% | |
| ICU | €0 | 0.00% | €27 | 0.45% | |
| DFC | €0 | 0.00% | €31 | 0.51% | |
| Amputation | €1,164 | 7.88% | €709 | 11.85% | |
| Total direct costs per patient | €11,164 | 75.60% | €3,999 | 66.82% | |
| Indirect costs | Loss of productivity during admission | €744 | 5.04% | €244 | 4.07% |
| Loss of mobility due to amputation | €2,860 | 19.37% | €1,742 | 29.10% | |
| Total indirect costs per patient | €3,604 | 24.41% | €1,986 | 33.17% | |
| Total costs per patient | €14,768 | 100% | €5,985 | 100% | |
| Total savings per patient with MDFC | €8,783 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




