1. Introduction
There are approximately 500,000 total NCAA college athletes who compete each year, and with competing comes vigorous training. Out of these 500,000 NCAA college athletes, about 190,000 of them are Division III athletes [
1]. Division III athletics have different rules concerning amount of practice time allotted and games played; however, the training can be just as intense as the Division I and II programs. A principal way that athletes complement sport-specific training is through high-intensity resistance training, to maximize their neuromuscular performance potential for training and competition. The American College of Sports Medicine (ACSM) has set guidelines for high intensity resistance training, characterized by performing exercises at ≥ 70% of a one-repetition maximum (1RM), which may induce significant physiological adaptations [
2]. When skeletal muscle is overloaded it stresses the myofibrils and extracellular matrix initiating a myogenic cascade, which leads to an increase in the amount of myofibrillar contractile proteins, thus increasing muscle cross sectional area (hypertrophy) and force production capacity [
3,
4]. However, the problem with a high-intensity resistance training regimen is that, along with sport training, it can potentially be mismanaged resulting in overuse or damage to the muscles and certain populations may not be able to participate due to risk factors [
5]. On the other hand, a lower risk training modality, low-intensity resistance training, does not increase muscle size and strength at the same rate as high-intensity resistance training without significantly increasing the repetitions or contraction time [
3]. The reason for this is thought to be an inadequate stimulus to cause metabolic stress to the muscle, thus little to no myogenic cascade, diminishing gains in hypertrophy and strength [
6]. Athletes could utilize low-intensity resistance training to decrease injury risk and reduce unnecessary stress on their bodies, and/or for rehabilitation purposes, but may need to be optimized.
A way to maximize low-intensity resistance training is by the addition of blood flow restriction (BFR). Blood flow restriction training (BFRT) is a newer exercise modality that has mainly been paired with low-intensity resistance training and has been previously shown to cause muscle hypertrophy and strength gains similarly to those observed with high-intensity resistance training [
7,
8,
9,
10,
11,
12,
13]. BFRT has also been reported to minimize muscle atrophy during periods of disuse and improve bone mineral density [
14,
15]. BFR works by reducing arterial blood flow to working muscles while also occluding venous return. This causes active muscles to encounter a relatively ischemic state, which imposes a greater metabolic stress on working muscles, without the need for heavy loads [
16,
17,
18,
19]. While BFRT has been extensively studied, there has been limited investigation into BFRT and its effects on muscle hypertrophy and strength gains in healthy male and female athletes when included as a supplemental part of a high-intensity resistance training regimen.
Accordingly, the purpose of this preliminary, ecological study was to investigate the effects of BFRT paired with low-intensity resistance training vs. traditional high-intensity resistance training on muscle size and strength in healthy, Division III, collegiate soccer athletes as part of their regularly scheduled strength training sessions in the off-season. It was hypothesized that similar gains in muscle hypertrophy and strength would occur for BFRT and high intensity resistance training, which could provide evidence of ecological validity to include low intensity BFRT as a supplement to their traditional high-intensity strength training.
2. Materials and Methods
Participants & General Procedures
Fifty-six college-aged Division III soccer players were recruited from the Skidmore College (Saratoga, NY, USA) men’s and women’s soccer teams to complete this study. Off-season athletes were chosen so as to not interfere with competition and primary on-field practice/training, and to optimize homogeneity soccer athletes were identified as a relatively large pool to recruit from, and limited to the home institution. Participants were included in the study as long as they were free of any chronic diseases or musculoskeletal injuries that would preclude them from resistance training and were non-smokers. This information was collected and reviewed via health history questionnaire. Further, participants were screened for appropriateness for BFRT using the AIS BFR pre-screening questionnaire
1. An answer of “no” to all of the contraindications would result in inclusion, and an answer of “yes” to any one of contraindications would result in exclusion. Any answer of “yes” to BFRT precautions were reviewed on a case-by-case basis by the investigative team, otherwise those reporting all “no” were readily included. Participants were asked to maintain a similar diet and sleep regimen throughout the duration of the study, and were asked to come to training and testing sessions as if prepared for training (hydrated and with recent nutrition), though this was not directly controlled. While participants were not required to alter their supplementation regiments, to maintain ecological validity of the research question, no participants reported use of supplements. All participants provided written informed consent prior to participation. This protocol was reviewed and approved by the Skidmore College Institutional Review Board (IRB#2201-1017), and was conducted in accordance with recent revisions to the Declaration of Helsinki.
Experimental Design
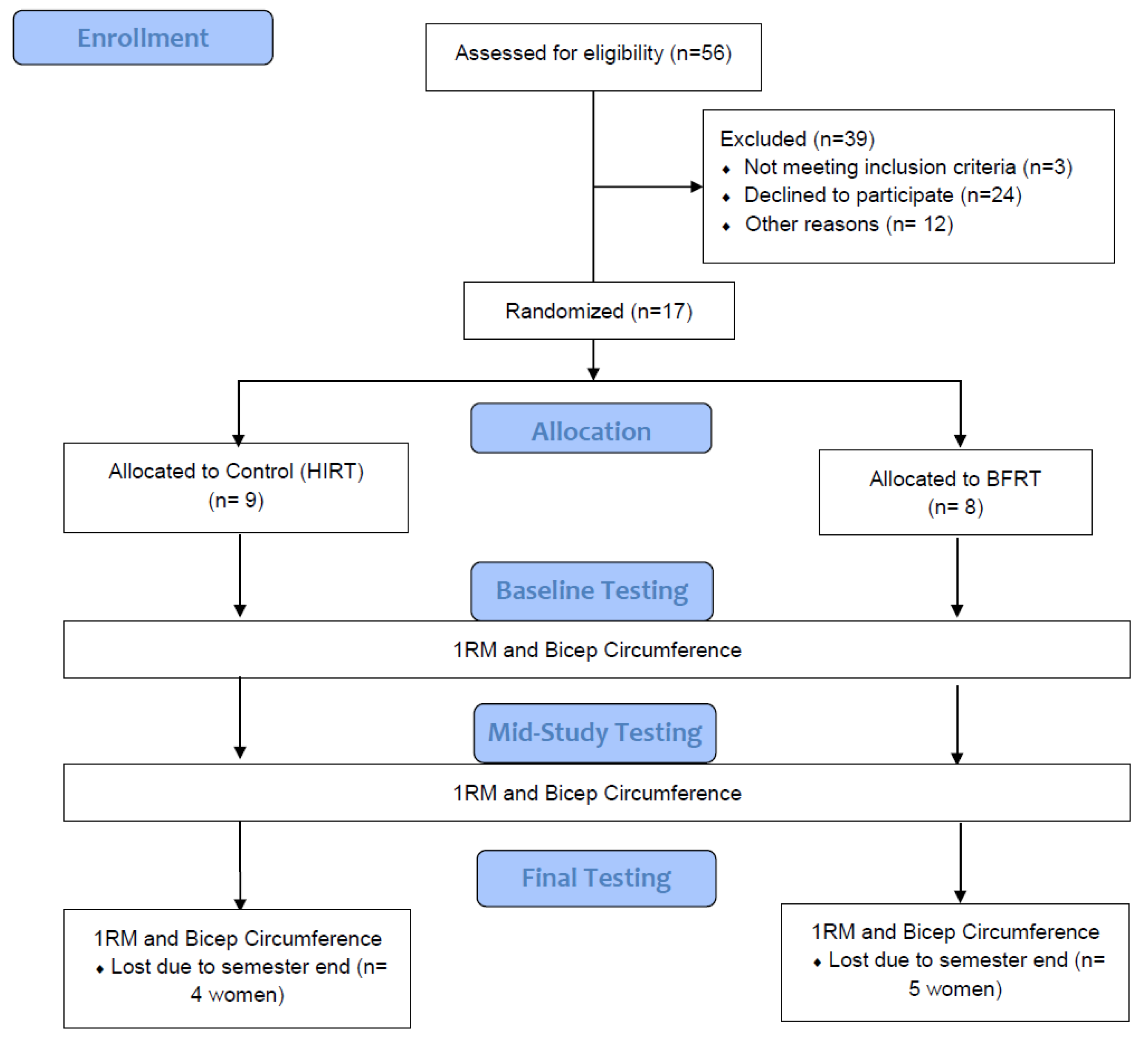
The present study explored adding accessory upper body exercise BFRT or HIRT onto soccer players existing off-season strength and conditioning program. Subjects were randomly assigned to either a high-intensity resistance training group, which completed bicep curls at 80% of their one repetition maximum (1RM), or a low-intensity resistance training group with BFR, which performed bicep curls at 30% of their 1RM (
Figure 1). Both groups accessory training protocols consisted of 2 days/week, performing 4 sets of 5 repetitions of the bicep curls with their non-dominant arm, over a 6-week period, to ensure matching of volume. Two days/week was chosen to match the athletes already prescribed resistance training sessions with the college’s strength and conditioning coach. Thus, the only difference between groups was the single accessory exercise prescribed by the research team described above. The female participants only completed 3 weeks’ worth of training sessions (6 total sessions) due to scheduling conflicts and completion of team strength training sessions at semesters end, therefore only baseline and week 3 data are presented for the women, but are included for transparency and inclusivity purposes. Baseline measurements and 1 RM were taken during a baseline evaluation session prior to the first week of the supplemental training, as described below. After the 3-week mark, a separate re-evaluation session was conducted on a rest day, at least 48 hours after the last training session, to retest 1 RM and retake bicep circumference measurements. For the female participants, this was their final evaluation session. The male participants continued the study and their final evaluation session occurred on an off day after Week 6 of training, again at least 48 hours after the last training session. Each training session lasted for approximately 1 hour; each training session included their normal high-intensity resistance training workout designed and implemented by the Certified Strength and Conditioning Coach at Skidmore College, paired with the supplemental biceps curls either BFR with low-intensity resistance training or high-intensity resistance training through bicep curls. It was required that each participant attended at least 75% of the training sessions. The arm was selected because most of the programmed strength and conditioning was expectedly lower body oriented and thus the bicep curl was easy to isolate and wouldn’t interfere with, or result in overuse in, core weight lifting efforts. A single exercise was chosen to minimize participant burden and maximize compliance.
Procedures
After consenting to the study participants were asked to report to the Human Performance Research Laboratory for assessment of height, weight, BMI, and body fat percentage. Participants were asked to self-reported their age, dominant hand, and, if applicable any dietary supplementation (e.g. vitamins, sports supplements (e.g. creatine), etc.). All of the participants were right hand dominant, and no participants consistently took any supplements that would impact our results. A stadiometer was used to assess height, a standard scale was used to measure weight, and a bioelectrical impedance test was done to determine body composition (BMI and body fat percentage) (Tanita, Arlington Heights, IL, USA). Bicep circumference measurements were taken with the subjects standing in a neutral position with their arms relaxed at their sides. Their non-dominant (left) bicep was measured, using a Gulick tape in three spots: right above the crease of the elbow, at the thickest part of the bicep, and right below the deltoid process [
21]. These numbers were added together to achieve a total “Bicep Circumference Score”. Then, a Smart Cuff® blood flow restriction cuff was placed proximal to the thickest part of the participant’s biceps (SmartCuffs PRO®, Smart Tools, Strongsville, OH, USA). The SmartCuff® pump was programmed to determine 40% of each participants’ total limb occlusion pressure, and the pressures were used to partially occlude the blood flow of the participants' arms that were involved in the BFRT group.
To conclude the baseline evaluation session, the subjects reported to the weight room, and they were instructed to begin a warmup consisting of biking for 3-5 mins on a cycle ergometer, followed by 10 light-weight bicep curls (RPE 3-4) with their non-dominant arm. Subjects then began testing for their one 1RM by increasing the load by 5 pounds after each successful repetition performed until failure. Once the subject was unable to perform a repetition with proper form, the weight of the last successful repetition was recorded as their 1RM. Throughout the 1RM testing, proper form was monitored by the researchers and was characterized by subjects’ backs being flat against the wall, elbows in contact with their side and the wall simultaneously, and the arm becoming flexed to 45º. The research team were working under the Colleges Strength and Conditioning coach, and thus had experience in working with the athletes and in administering testing and training.
Statistical Analysis
A two-way repeated measures analysis of variance (ANOVA) was carried out using open-source software (JASP, v 0.15, Amsterdam, Netherlands) to detect significant differences in muscle strength and muscle size between groups over time. Tests of normality were performed and if a significant violation was found an appropriate adjustment to degrees of freedom was made. Significance was set at p < 0.05 and appropriate measures of effect size were used to complement the p values. Data are presented as means ± SD, unless stated otherwise.
3. Results
3.1. Subject Characteristics
The subject characteristics for all 17 participants are shown in
Table 1. The female participants were only able to complete 3 weeks’ worth of training sessions (6 total sessions) due to scheduling conflicts and completion of team strength training sessions at semesters end, therefore only baseline and week 3 data are presented for the women, but are included for transparency and inclusivity purposes.
3.2. The Impact of 6-Weeks of BFRT vs. HIRT in Male Soccer Players
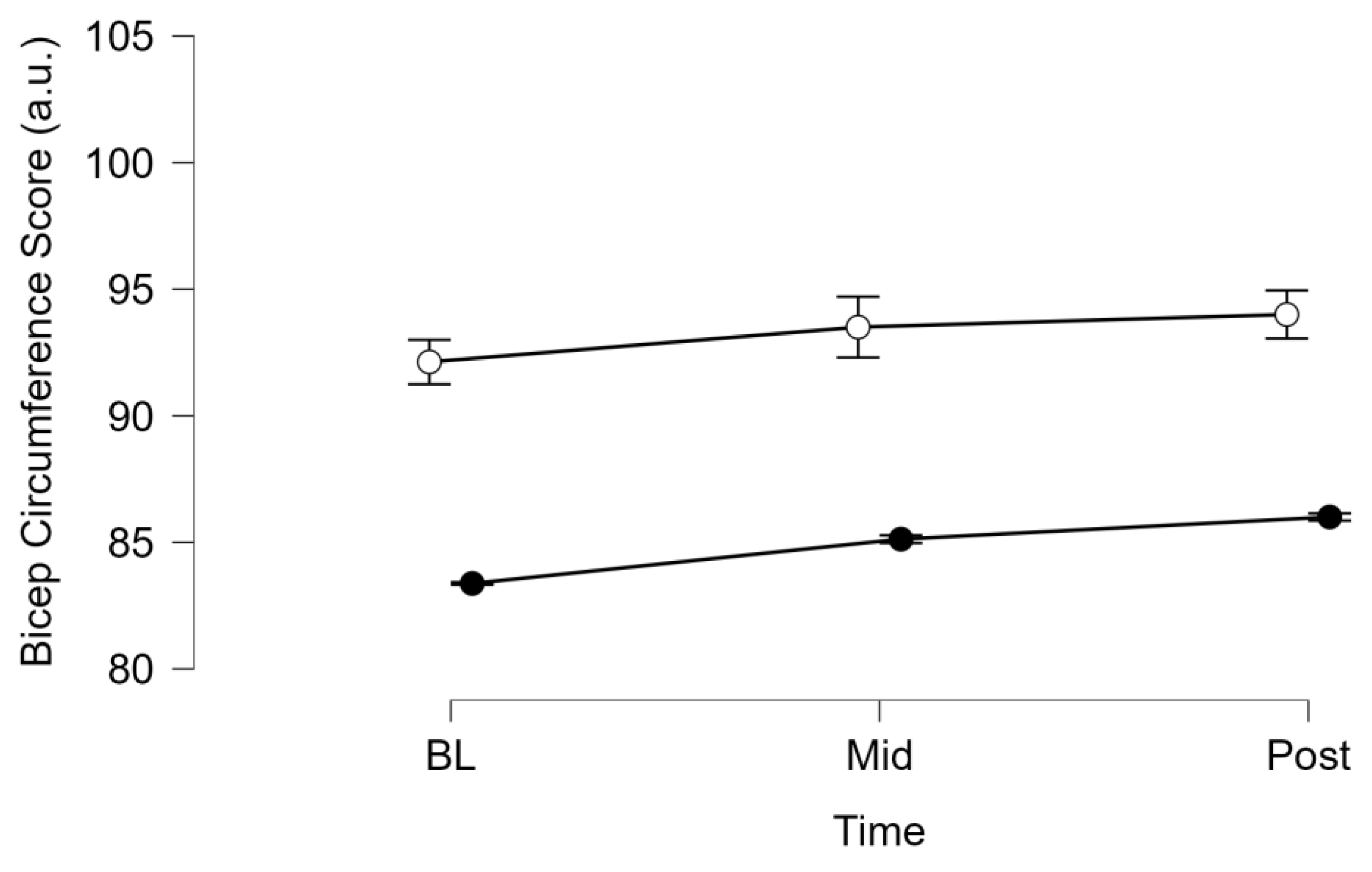
There was no significant interaction between time and condition (BFR vs Control) for male bicep circumference score (p = 0.877, η2p = 0.022,
Figure 2). There was a significant effect of the condition on male bicep circumference score (p = 0.024, η2p = 0.600,
Figure 2). There was a significant effect of time on male bicep circumference score (p = 0.026, η2p = 0.456,
Figure 2).
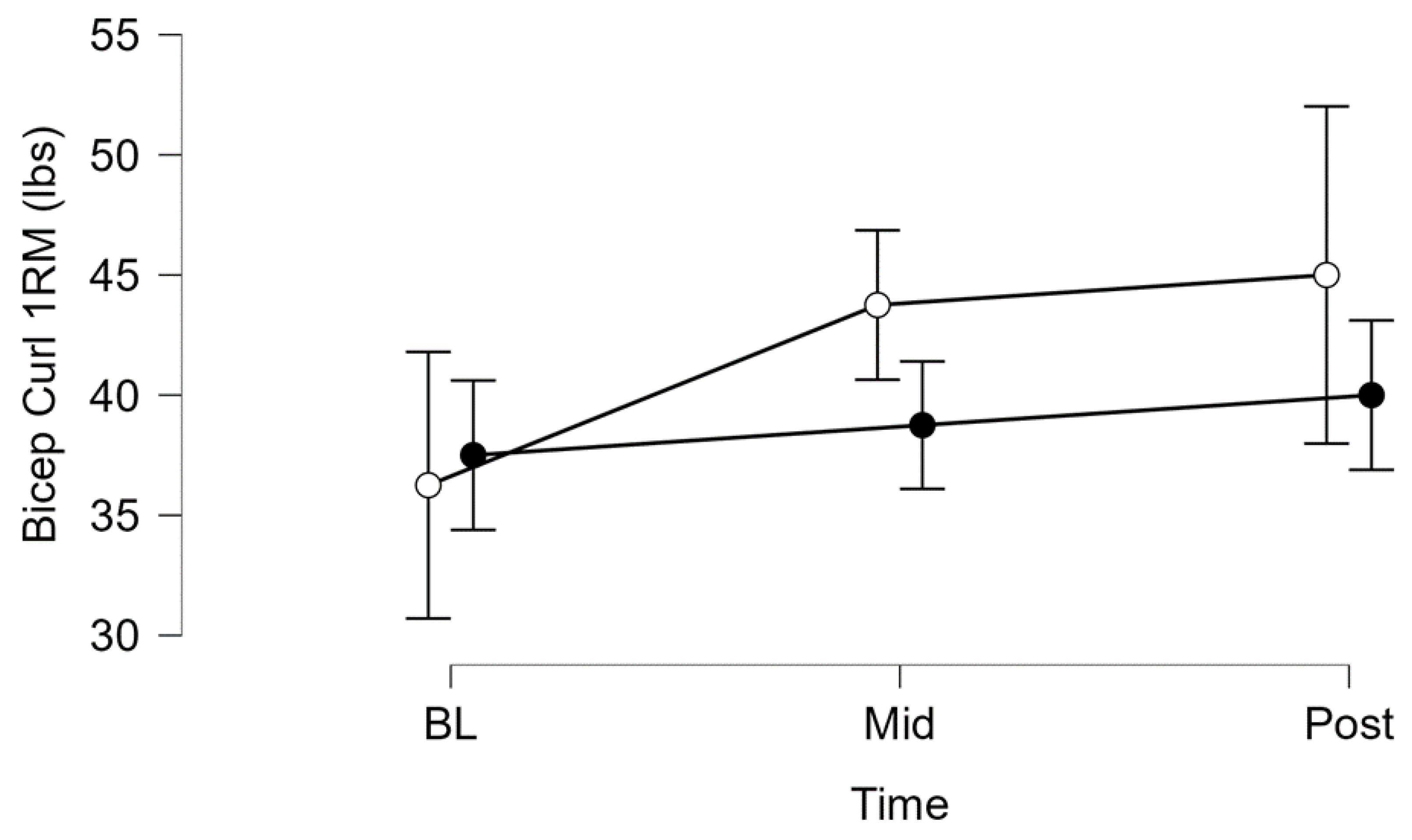
There was no significant interaction between time and condition (BFR vs Control) for male 1RM (p = 0.067, η2p = 0.362,
Figure 3). There was no significant effect of condition on male 1 RM (p = 0.598, η2p = 0.049,
Figure 3). There was a significant effect of time on male 1 RM (p = 0.004, η2p = 0.604,
Figure 3).
3.2. The Impact of 3-Weeks of BFRT vs. HIRT in Female Soccer Players
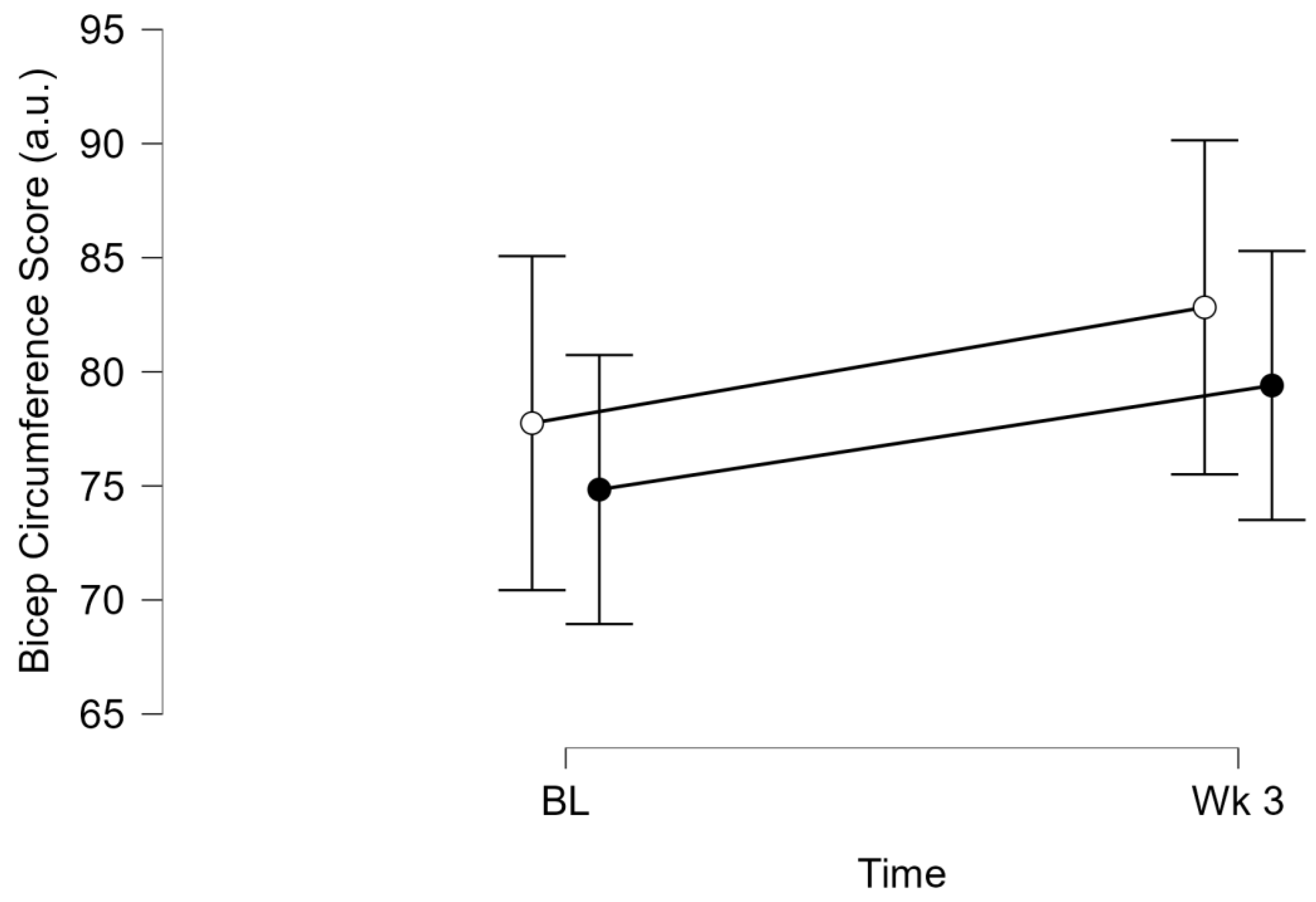
There was no significant interaction between time and condition (BFR vs Control) for female bicep circumference score (p=0.911, η2p=0.002,
Figure 4). There was no significant effect of condition on female bicep circumference score (p=0.494, η2p=0.069,
Figure 4). There was a significant effect of time on female bicep circumference score (p=0.067, η2p=0.402,
Figure 4).
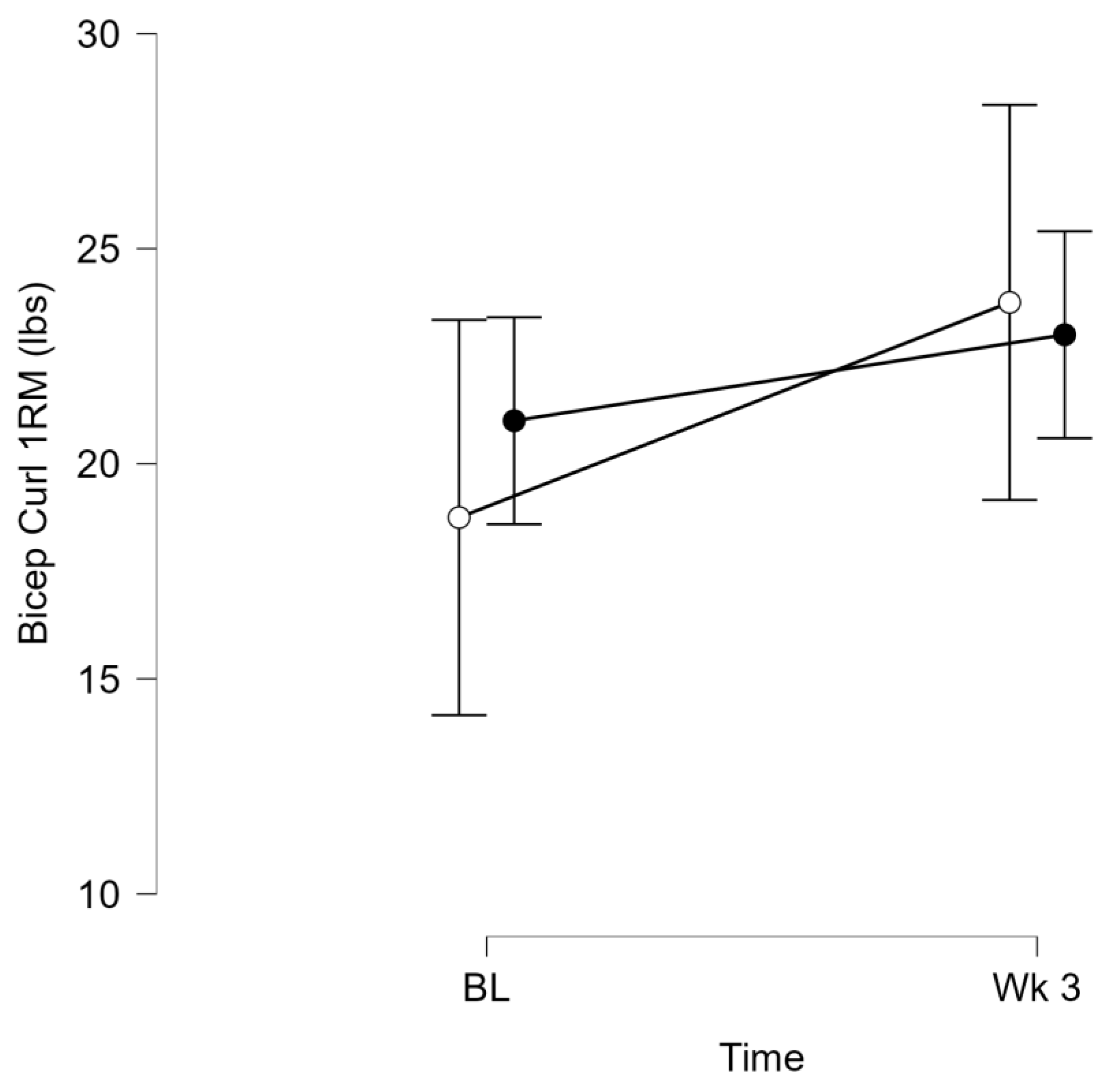
There was no significant interaction between time and condition (BFR vs Control) for female 1 RM (p = 0.227, η2p = 0.200,
Figure 5). There was no significant effect of condition on female 1 RM (p = 0.741, η2p = 0.017,
Figure 5). There was a significant effect of time on female 1 RM (p = 0.018, η2p = 0.576,
Figure 5).
4. Discussion
The purpose of this preliminary ecological study was to investigate the effects of blood flow restriction training on muscle size and strength in healthy, Division III collegiate soccer players when added to a currently prescribed off-season high intensity resistance training regimen. The primary finding of the present study was that blood flow restriction training produced improvements in muscular size and strength of the biceps similarly to HIRT in both male and female soccer players. This finding suggests that using blood flow restriction training (BFRT) may be a viable supplemental training method to continue strength and hypertrophy improvements while perhaps minimizing risk of injury or accumulated fatigue. This can also be a valuable tool and training strategy to implement during times of a competitive season in which high intensity resistance training is not feasible, desirable, or practical due to a busy competitive schedule and limited recovery times. Future work needs to explore the efficacy of BFRT to determine if outcomes are similar on core lifts in the collegiate strength and conditioning setting.
Currently, the American College of Sports Medicine recommends that in order to optimize muscular hypertrophy and strength improvements, resistance training intensity should be set above 70% of one rep max (1RM) [
2,
22]. By implementing high-intensity resistance training programs, the skeletal muscle is overloaded. This stimulus leads to stress on the myofibrils and extracellular matrix, initiating a myogenic cascade. This cascade results in an increase in the size (hypertrophy) and amount of myofibrillar contractile proteins, as well as the number of sarcomeres. This results in an increase in muscle cross sectional area as well as an increase in the amount of force the muscle can produce [
4,
23]. Adaptations to muscle size or strength are not commonly observed when implementing a low-intensity resistance training program, unless there is a significant increase in repetitions or contraction times [
24]. It is believed that intensities below 70% of 1RM provide an inadequate stimulus to cause metabolic stress to the muscle, resulting in little to no myogenic cascade, and minimal improvements in hypertrophy and strength [
6]
. However, this intensity may not be appropriate for everyone and low-intensity training programs may need to be utilized for various reasons amongst various different populations.
One way low-intensity resistance training can be utilized to increase muscle size and strength is through BFRT. A low-intensity resistance training protocol paired with BFR can elicit similar improvements in muscle size and strength when compared to a HIRT protocol [
12,
13,
25,
26,
27,
28]. The current study observed non-significant differences between the control group (HIRT) and BFRT group when comparing Bicep Circumference Score pre and post training as well as 1RM values (
Figure 2,
Figure 3,
Figure 4 and
Figure 5). Although, we did observe increases over time, which may have contributed, at least in part, to the increases in 1RM, as previous studies have documented increases in muscle cross-sectional area and strength even after 2-4 weeks, although neuromuscular changes may be more instrumental in meditating the strength changes and edema may influence such early increases in measures of muscle size [
29]. Further, in the men while a significant group effect was found, this is reflecting baseline differences between groups as the interaction was not significant.
It’s possible that the improvement in muscle size and strength are a result of rapid increases in plasma growth hormone following BFRT. Takarada et al. [
30], examined plasma concentrations of a variety of hormones and observed acute increases in growth hormone, norepinephrine, and lactate following the use of BFRT when compared to exercise of the same intensity but without BFRT. Although plasma hormone levels were not measured in this study it is possible that the utilization of BFRT resulted in similar hormonal changes post-exercise as HIRT, promoting a myogenic cascade. BFRT has also been reported to stimulate the mTORC1 pathway, increase S6K1 phosphorylation and increase levels of IGF-1 all resulting in an increase in muscle protein synthesis and demonstrating that the myogenic cascade necessary for muscular hypertrophy appears to occurs with BFRT [
8,
31,
32]. The repeated exposure to these anabolic hormonal changes and the myogenic cascade likely resulted in the cumulative effect of muscular hypertrophy and strength improvements, similarly to what is observed with consistent HIRT.
It is also possible that the addition of blood flow restriction to low intensity resistance training provides enough stimuli to produce metabolic stress, resulting in the recruitment of Type II muscle fibers and initiating the myogenic cascade that results in improvements in strength and muscular hypertrophy [
9,
12,
17,
33]. It has been demonstrated that placing the muscle in an ischemic state does alter the metabolic profile and metabolite content of muscle [
16,
18]. Moritani et al., [
34] examined integrated electromyogram (EMG) activity of the muscles of the forearm while training with blood flow restriction and light loads (20% maximal voluntary contraction) and observed increased motor unit activity. This is supported by the fact that EMG activity and motor unit recruitment were low when light loads were used without blood flow restriction. Similarly, Moore et al., [
33] observed an increase in EMG activity with BFRT when compared to low intensity resistance training without BFR. The authors of both of these papers speculate that the recruitment of additional motor units was a result of the changing metabolic conditions and buildup of metabolites within the muscle as a result of the occlusion from BFRT. This led to accelerated muscular fatigue which then necessitated an increase in motor unit recruitment. These additional motor units were likely larger motor units consisting of Type II muscle fibers, which are more susceptible to hypertrophy and typically recruited at higher intensities, according to the size principle. The changing metabolic conditions within the muscle that occur with BFRT and low intensity may result in the recruitment of Type II muscle fibers, which typically does not occur with low intensity resistance training in the absence of occlusion [
17].
Additionally, an increase in blood lactate has been observed following the use of BFRT resulting in changes in venous blood pH [
32,
35]. It is hypothesized that this increase in lactate production and alteration in venous blood pH levels results in stimulation of group III and IV afferent nerves, impacted muscle activation during exercise with occlusion present [
35]. The changing internal conditions of partial ischemic muscle results in an increased reliance on nonoxidative metabolic pathways, resulting in an accumulation of lactate. This accumulation alters muscle fiber recruitments patterns and mimics muscle activation we typically observe with HIRT. We can then expect to see similar improvements in muscular strength and hypertrophy using BFRT as we would with HIRT, which may have been what was observed in this study.
Limitations
In the current study, a Gulick tape measure was used to measure bicep circumference in three different locations (upper, middle, lower) and was summed to create a Bicep Circumference Score [
21]. Unfortunately, there was not a more accurate measure of assessing muscle hypertrophy available, such as a DEXA, MRI, or ultrasound which would allow a more accurate assessment of muscle growth. Another limitation to the current study is the female subjects only completed 3 weeks of testing due to time conflict issues between the researchers and the participants. Diets were not controlled for either group, which may impact results due to varying amounts of calories and different macronutrient distributions, although given the randomization of athletes and recruitment from a similar group of athletes at a singular institution, we don’t expect that chance differences in diet would have explained the current findings. Finally, while seeking to maintain homogeneity we focused on a single off-season sport, at a single institution, thus limiting the pool of participants, thus this preliminary ecological study should be completed with larger numbers (e.g. across institutions and/or sports), but will likely add variability due to differences in training programs.
Future Directions
Blood flow restriction training has shown promising results in previous studies, as well as in the current study, because it caused increases in muscle size and strength when paired with a low intensity resistance training protocol. These results are both intriguing and exciting as injured, postoperative, chronically diseased, and elderly populations can participate in this type of training when certain contraindications prevent them from performing high intensity resistance training. However, limited knowledge by health practitioners on how to appropriately apply this training modality has prevented its broad adoption into clinical practice [
36]. BFRT gives the populations mentioned, as well as healthy populations, an alternate, potentially safer, training modality to use to increase muscle strength and size. Future research should focus on an expanded training period, beyond 6 weeks to examine if improvements in muscular strength and hypertrophy continue to happen at the same rate for both training modalities or if one produces a more favorable result. To enhance the precision of muscular hypertrophy analysis, it's imperative to utilize more accurate methodologies that enable researchers to precisely measure the extent of muscular growth between the two training techniques. There are also conflicting reports on how BFRT impacts muscular power output when compared to HIRT. Some studies have reported a decrement in power output while others have reported improvements [
37,
38,
39]. Future research may want to focus on not just muscular strength and hypertrophy following extended periods of BFRT but should also examine the impact this training modality has on power output and rate of force development.
5. Conclusions
Using an ecologically valid model of performing BFRT (light load + BFR) or traditional HIRT for a single accessory resistance exercise performed after an off-season team weight lifting session, this preliminary study reveals that BFRT induced similar increases in muscle strength and muscle size as HIRT in male and female soccer players. These results suggest that BFRT could be incorporated into collegiate athlete training, but further work is needed, especially during core lifts, in athletes recovering from injury or during in season training.
Author Contributions
Conceptualization, K.J., C.M., M.W., K.W. and S.J.I.; methodology, K.J., C.M., M.W., K.W. and S.J.I.; validation, K.J., C.M., M.W., K.W. and S.J.I.; formal analysis, K.J., C.M., M.W., K.W., J.F., and S.J.I.; investigation, K.J., C.M., M.W., K.W. and S.J.I.; resources, S.J.I.; data curation, K.J., C.M., M.W., K.W. and S.J.I..; writing—original draft preparation, K.J., C.M., M.W., K.W., J.F. and S.J.I. writing—review and editing, K.J., C.M., M.W., K.W., J.F. and S.J.I.; visualization, K.J., C.M., M.W., K.W., J.F. and S.J.I.; supervision, S.J.I.; project administration, S.J.I.; funding acquisition, S.J.I.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding, but the authors would like to acknowledge modest funding from the HHPS Department at Skidmore college.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Skidmore College (protocol #2201-1017, approved 02/23/2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and intellectual property concerns.
Acknowledgments
We would like to acknowledge the athletes who participated in this study and crucially the Skidmore College Strength and Conditioning coach, Matt Chatham for his support and patience in completing this project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- National Strength and Conditioning Association The College Divisions Explained (D1 vs. D2 vs. D3) | NCSA Available online: https://www.ncsasports.org/recruiting/how-to-get-recruited/college-divisions (accessed on 24 March 2023).
-
ACSM’s Guidelines for Exercise Testing and Prescription; American College of Sports Medicine, Liguori, G., Feito, Y., Fountaine, C., Roy, B., Eds.; Eleventh edition.; Wolters Kluwer: Philadelphia, 2021; ISBN 978-1-975150-22-8.
- Ikezoe, T.; Kobayashi, T.; Nakamura, M.; Ichihashi, N. Effects of Low-Load, Higher-Repetition vs. High-Load, Lower-Repetition Resistance Training Not Performed to Failure on Muscle Strength, Mass, and Echo Intensity in Healthy Young Men: A Time-Course Study. J. Strength Cond. Res. 2020, 34, 3439. [CrossRef]
- Schoenfeld, B.J. The Mechanisms of Muscle Hypertrophy and Their Application to Resistance Training. J. Strength Cond. Res. 2010, 24, 2857–2872.
- Spada, T.C.; Silva, J.M.R.D.; Francisco, L.S.; Marçal, L.J.; Antonangelo, L.; Zanetta, D.M.T.; Yu, L.; Burdmann, E.A. High Intensity Resistance Training Causes Muscle Damage and Increases Biomarkers of Acute Kidney Injury in Healthy Individuals. PLOS ONE 2018, 13, e0205791. [CrossRef]
- Androulakis-Korakakis, P.; Michalopoulos, N.; Fisher, J.; Keogh, J.; Loenneke, J.; Helms, E.; Wolf, M.; Nuckols, G.L.; Steele, J. The Minimum Effective Training Dose Required to Increase 1RM Strength in Powerlifters; SportRxiv, 2021;
- Abe, T.; Beekley, M.D.; Hinata, S.; Koizumi, K.; Sato, Y. Day-to-Day Change in Muscle Strength and MRI-Measured Skeletal Muscle Size during 7 Days KAATSU Resistance Training: A Case Study. Int. J. KAATSU Train. Res. 2005, 1, 71–76. [CrossRef]
- Abe, T.; Yasuda, T.; Midorikawa, T.; Sato, Y.; Kearns, C.F.; Inoue, K.; Koizumi, K.; Ishii, N. Skeletal Muscle Size and Circulating IGF-1 Are Increased after Two Weeks of Twice Daily “KAATSU” Resistance Training. Int. J. KAATSU Train. Res. 2005, 1, 6–12. [CrossRef]
- Amani-Shalamzari, S.; Rajabi, S.; Rajabi, H.; Gahreman, D.E.; Paton, C.; Bayati, M.; Rosemann, T.; Nikolaidis, P.T.; Knechtle, B. Effects of Blood Flow Restriction and Exercise Intensity on Aerobic, Anaerobic, and Muscle Strength Adaptations in Physically Active Collegiate Women. Front. Physiol. 2019, 10, 810. [CrossRef]
- Cook, S.B.; Clark, B.C.; Ploutz-Snyder, L.L. Effects of Exercise Load and Blood-Flow Restriction on Skeletal Muscle Function. Med. Sci. Sports Exerc. 2007, 39, 1708–1713. [CrossRef]
- Takarada, Y.; Sato, Y.; Ishii, N. Effects of Resistance Exercise Combined with Vascular Occlusion on Muscle Function in Athletes. Eur. J. Appl. Physiol. 2002, 86, 308–314. [CrossRef]
- Takarada, Y.; Takazawa, H.; Sato, Y.; Takebayashi, S.; Tanaka, Y.; Ishii, N. Effects of Resistance Exercise Combined with Moderate Vascular Occlusion on Muscular Function in Humans. J. Appl. Physiol. 2000, 88, 2097–2106.
- Yasuda, T.; Loenneke, J.P.; Thiebaud, R.S.; Abe, T. Effects of Blood Flow Restricted Low-Intensity Concentric or Eccentric Training on Muscle Size and Strength. PloS One 2012, 7, e52843. [CrossRef]
- Beekley, M.D.; Sato, Y.; Abe, T. KAATSU-Walk Training Increases Serum Bone-Specific Alkaline Phosphatase in Young Men. Int. J. KAATSU Train. Res. 2005, 1, 77–81. [CrossRef]
- Takarada, Y.; Takazawa, H.; Ishii, N. Applications of Vascular Occlusion Diminish Disuse Atrophy of Knee Extensor Muscles. Med. Sci. Sports Exerc. 2000, 32, 2035–2039. [CrossRef]
- Burgomaster, K.A.; Moore, D.R.; Schofield, L.M.; Phillips, S.M.; Sale, D.G.; Gibala, M.J. Resistance Training with Vascular Occlusion: Metabolic Adaptations in Human Muscle: Med. Sci. Sports Exerc. 2003, 35, 1203–1208. [CrossRef]
- Loenneke, J.P.; Fahs, C.A.; Wilson, J.M.; Bemben, M.G. Blood Flow Restriction: The Metabolite/Volume Threshold Theory. Med. Hypotheses 2011, 77, 748–752. [CrossRef]
- Sahlin, K.; Katz, A. Hypoxaemia Increases the Accumulation of Inosine Monophosphate (IMP) in Human Skeletal Muscle during Submaximal Exercise. Acta Physiol. Scand. 1989, 136, 199–203. [CrossRef]
- Tanimoto, M.; Ishii, N. Effects of Low-Intensity Resistance Exercise with Slow Movement and Tonic Force Generation on Muscular Function in Young Men. J. Appl. Physiol. 2006, 100, 1150–1157. [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMC Med. 2010, 8, 18. [CrossRef]
- Avila, M.L.; Ward, L.C.; Feldman, B.M.; Montoya, M.I.; Stinson, J.; Kiss, A.; Brandao, L.R. Normal Values for Segmental Bioimpedance Spectroscopy in Pediatric Patients. PLoS ONE 2015, 10. [CrossRef]
- Panissa, V.L.G.; Fukuda, D.H.; de Oliveira, F.P.; Parmezzani, S.S.; Campos, E.Z.; Rossi, F.E.; Franchini, E.; Lira, F.S. Maximum Strength Development and Volume-Load during Concurrent High Intensity Intermittent Training Plus Strength or Strength-Only Training. J. Sports Sci. Med. 2018, 17, 623–632.
- Grgic, J. The Effects of Low-Load vs. High-Load Resistance Training on Muscle Fiber Hypertrophy: A Meta-Analysis. J. Hum. Kinet. 2020, 74, 51–58. [CrossRef]
- Bowman, E.N.; Elshaar, R.; Milligan, H.; Jue, G.; Mohr, K.; Brown, P.; Watanabe, D.M.; Limpisvasti, O. Proximal, Distal, and Contralateral Effects of Blood Flow Restriction Training on the Lower Extremities: A Randomized Controlled Trial. Sports Health 2019, 11, 149–156. [CrossRef]
- Abe, T.; Kawamoto, K.; Yasuda, T.; Kearns, C.F.; Midorikawa, T.; Sato, Y. Eight Days KAATSU-Resistance Training Improved Sprint but Not Jump Performance in Collegiate Male Track and Field Athletes. Int. J. KAATSU Train. Res. 2005, 1, 19–23. [CrossRef]
- Abe, T.; Sakamaki, M.; Fujita, S.; Ozaki, H.; Sugaya, M.; Sato, Y.; Nakajima, T. Effects of Low-Intensity Walk Training with Restricted Leg Blood Flow on Muscle Strength and Aerobic Capacity in Older Adults. J. Geriatr. Phys. Ther. 2001 2010, 33, 34–40.
- Loenneke, J.P.; Wilson, J.M.; Wilson, G.J.; Pujol, T.J.; Bemben, M.G. Potential Safety Issues with Blood Flow Restriction Training - Loenneke - 2011 - Scandinavian Journal of Medicine & Science in Sports - Wiley Online Library. Scand. J. Med. Sci. Sports 2011, 21, 510–528.
- Yasuda, T.; Ogasawara, R.; Sakamaki, M.; Ozaki, H.; Sato, Y.; Abe, T. Combined Effects of Low-Intensity Blood Flow Restriction Training and High-Intensity Resistance Training on Muscle Strength and Size. Eur. J. Appl. Physiol. 2011, 111, 2525–2533. [CrossRef]
- Hughes, D.C.; Ellefsen, S.; Baar, K. Adaptations to Endurance and Strength Training. Cold Spring Harb. Perspect. Med. 2018, 8, a029769. [CrossRef]
- Takarada, Y.; Nakamura, Y.; Aruga, S.; Onda, T.; Miyazaki, S.; Ishii, N. Rapid Increase in Plasma Growth Hormone after Low-Intensity Resistance Exercise with Vascular Occlusion. J. Appl. Physiol. 2000, 88, 61–65.
- Fry, C.S.; Glynn, E.L.; Drummond, M.J.; Timmerman, K.L.; Fujita, S.; Abe, T.; Dhanani, S.; Volpi, E.; Rasmussen, B.B. Blood Flow Restriction Exercise Stimulates MTORC1 Signaling and Muscle Protein Synthesis in Older Men. J. Appl. Physiol. 2010, 108, 1199–1209. [CrossRef]
- Fujita, S.; Abe, T.; Drummond, M.J.; Cadenas, J.G.; Dreyer, H.C.; Sato, Y.; Volpi, E.; Rasmussen, B.B. Blood Flow Restriction during Low-Intensity Resistance Exercise Increases S6K1 Phosphorylation and Muscle Protein Synthesis. J. Appl. Physiol. 2007, 103, 903–910. [CrossRef]
- Moore, D.R.; Burgomaster, K.A.; Schofield, L.M.; Gibala, M.J.; Sale, D.G.; Phillips, S.M. Neuromuscular Adaptations in Human Muscle Following Low Intensity Resistance Training with Vascular Occlusion. Eur. J. Appl. Physiol. 2004, 92, 399–406. [CrossRef]
- Moritani, T.; Sherman, W.M.; Shibata, M.; Matsumoto, T.; Shinohara, M. Oxygen Availability and Motor Unit Activity in Humans. Eur. J. Appl. Physiol. 1992, 64, 552–556. [CrossRef]
- Yasuda, T.; Abe, T.; Brechue, W.F.; Iida, H.; Takano, H.; Meguro, K.; Kurano, M.; Fujita, S.; Nakajima, T. Venous Blood Gas and Metabolite Response to Low-Intensity Muscle Contractions with External Limb Compression. Metabolism. 2010, 59, 1510–1519. [CrossRef]
- Mills, N.; Elder, M.; Boyce, M.; Evdokas, M.; Ives, S. The Knowledge and Use of Blood Flow Restriction Therapy in a Sample of Physical Therapists in the United States. Res. Directs Health Sci. 2021, 1. [CrossRef]
- Behringer, M.; Behlau, D.; Montag, J.C.K.; McCourt, M.L.; Mester, J. Low-Intensity Sprint Training With Blood Flow Restriction Improves 100-m Dash. J. Strength Cond. Res. 2017, 31, 2462–2472. [CrossRef]
- Cleary, C.J.; Cook, S.B. Postactivation Potentiation in Blood Flow–Restricted Complex Training. J. Strength Cond. Res. 2020, 1. [CrossRef]
- Faller, J.; Sotir, S.; Ouellette, K.; Paolone, V.J.; Thompson, B. Exercise with Blood Flow Restriction and Power Development of the Lower Body. Med. Sci. Sports Exerc. 2018, 50, 17. [CrossRef]
Figure 1.
Overview of Study Design using CONSORT diagram [
20].
Figure 1.
Overview of Study Design using CONSORT diagram [
20].
Figure 2.
Bicep Circumference Score at Baseline, 3 Weeks, and 6 Weeks with BFRT (open circle ○, n = 4) or Without (Control, HIRT, filled circle ●, n = 4) in Male Division III Soccer Players (n = 8). Data are expressed as means ± 95% confidence interval. Interaction p = 0.877, Group: p = 0.024, Time: p = 0.026.
Figure 2.
Bicep Circumference Score at Baseline, 3 Weeks, and 6 Weeks with BFRT (open circle ○, n = 4) or Without (Control, HIRT, filled circle ●, n = 4) in Male Division III Soccer Players (n = 8). Data are expressed as means ± 95% confidence interval. Interaction p = 0.877, Group: p = 0.024, Time: p = 0.026.
Figure 3.
Bicep Curl 1 Repetition Maximum (1 RM) at Baseline, 3 Weeks, and 6 Weeks with BFRT (open circle ○, n=4) or Without (Control, HIRT, filled circle ●, n=4) in Male Division III Soccer Players (n = 8). Data are expressed as means ± 95% confidence interval. Interaction p = 0.067, Group: p = 0.60, Time: p = 0.004.
Figure 3.
Bicep Curl 1 Repetition Maximum (1 RM) at Baseline, 3 Weeks, and 6 Weeks with BFRT (open circle ○, n=4) or Without (Control, HIRT, filled circle ●, n=4) in Male Division III Soccer Players (n = 8). Data are expressed as means ± 95% confidence interval. Interaction p = 0.067, Group: p = 0.60, Time: p = 0.004.
Figure 4.
Bicep Circumference Score at Baseline and 3 Weeks with BFRT (open circle ○, n = 4) or Without (Control, HIRT, filled circle ●, n = 5) in Female Division III Soccer Players (n = 9). Data are expressed as means ± 95% confidence interval. Interaction p = 0.911, Group: p = 0.494, Time: p = 0.067.
Figure 4.
Bicep Circumference Score at Baseline and 3 Weeks with BFRT (open circle ○, n = 4) or Without (Control, HIRT, filled circle ●, n = 5) in Female Division III Soccer Players (n = 9). Data are expressed as means ± 95% confidence interval. Interaction p = 0.911, Group: p = 0.494, Time: p = 0.067.
Figure 5.
Bicep Curl 1 Repetition Maximum (1 RM) at Baseline and 3 Weeks with BFRT (open circle ○, n=4) or Without (Control, HIRT, filled circle ●, n = 5) in Female Division III Soccer Players (n = 9). Data are expressed as means ± 95% confidence interval. Interaction p = 0.227, Group: p = 0.741, Time: p = 0.018.
Figure 5.
Bicep Curl 1 Repetition Maximum (1 RM) at Baseline and 3 Weeks with BFRT (open circle ○, n=4) or Without (Control, HIRT, filled circle ●, n = 5) in Female Division III Soccer Players (n = 9). Data are expressed as means ± 95% confidence interval. Interaction p = 0.227, Group: p = 0.741, Time: p = 0.018.
Table 1.
Subject Characteristics (n = 17), data are presented as mean ± SD.
Table 1.
Subject Characteristics (n = 17), data are presented as mean ± SD.
| Characteristic |
Men (n = 8) |
Women (n = 9) |
| Age (years) |
20 ± 1 |
20 ± 1 |
| Height (cm) |
182 ± 8 |
165 ± 4 |
| Weight (kg) |
76 ± 11 |
63 ± 6 |
| Body Mass Index (kg/m2) |
23.4 ± 1.5 |
23.1 ± 1.5 |
| Body Fat (%) |
13.3 ± 1.9 |
23 ± 2.5 |
| 1. |
https://www.ais.gov.au/position_statements/best_practice_content/blood-flow-restriction-training-guidelines |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).