1. Background
Vaccination is known to be the most effective means to prevent diseases. It has a high cost-effectiveness ratio and has notably led to the eradication of smallpox and lessened the burden of several vaccine-preventable diseases (VPDs) such as poliomyelitis,
Haemophilus influenza type b (Hib), and measles amongst others [
1,
2]. Despite the gains in global immunization coverage for children, an estimated 21.8 million infants worldwide are still not being reached by routine immunization services [
3]. Among the 19.7 million children worldwide who did not complete the diphtheria-tetanus-pertussis-containing vaccine (DTP-3) series in 2019, 70% (13.8 million) were zero-dose children, and 30% (5.9 million) started but did not complete the DTP series [
4].
Reaching zero-dose children and missed communities with routine immunization is a crucial goal of the Immunization Agenda 2030 and the Gavi Alliance’s 2021-2025 strategy. However, Cameroon’s sub-optimal access to childhood vaccination raises an important question of whether this central African country will achieve this goal. Indeed, Cameroon’s key immunization indicators have either stalled or are slipping backward. For instance, the DTP-1 vaccination coverage has dropped significantly, falling from 83% in 2017 to 76% in 2018, and has stalled around this level for the past four years [
5]. In 2019, Cameroon was among the top 10 countries contributing to 86% of the world’s 7.3 million estimated zero-dose children [
6]. Globally, the number of zero-dose children has also increased significantly due to the abrupt and rapid progression of the COVID-19 pandemic, which significantly disrupted essential health service delivery in many countries, reversing past efforts to improve health indicators, including childhood immunization [
7,
8,
9]. This is the case in Cameroon, where the number of zero-dose children is consistently rising. Administrative data suggest that between 2020 and 2021, Cameroon experienced an increase of almost 17,000 zero-dose children (ZD) - the number rose from 114,569 in 2020 to 130,978 in 2021. This low immunization coverage probably explains the recent frequent outbreaks of VPDs in Cameroon.
In order to reach the global coverage goals with vaccines recommended across the life course, we must place hard-to-reach and hard-to-vaccinate populations at the center of vaccination interventions [
10]. Manoka Health District (MHD) in the Littoral Region of Cameroon is one of such hard-to-reach communities with a high proportion of zero-dose children, low vaccination coverage (DPT-1 coverage of 19.8% in 2021), and several outbreaks of VPDs reported by the district health team. Indeed, in a previous study, we showed that over 90% of children in this district’s most populous health area had not received a single dose of any vaccine [
11]. Despite this high proportion, there is a paucity of data on the reasons why children in this district or other similar settings have not received a single dose of basic pediatric vaccines [
10,
12,
13,
14,
15]. In a previous study in this setting, quantitative data was used to characterize zero-dose children, which revealed that children born at home, children born to minority non-Christian and immigrant parents, and younger children had higher odds of being zero-dose children [
11]. This was quite useful in zero-dose identification and vaccination. However, as recommended in the previous study, there is a need for a qualitative study to understand why these children are zero-dose children; for instance, why are younger children likely to be unvaccinated compared to older children? Also, the previous study lacked sufficient information to paint a complete picture of supply and demand-side barriers to vaccination. This knowledge gap poses a significant challenge in informing policy and developing tailored interventions to vaccinate zero-dose children in hard-to-reach communities. Therefore, this study sought to delve into context-specific reasons why there are zero-dose children in MHD-Littoral Region, Cameroon.
2. Methodology
2.1. Study Design and study population
We used a qualitative study design to explore potential reasons for the high proportion of zero-dose children in MHD. The MHD is a remote island district found in the Littoral Region of Cameroon- about 20km from the port city of Douala. The district has a population of about 19,943 persons and an annual under -2 EPI target of about 1,732 children, which are unequally spread across 47 islets. Over 70% of the population are immigrants from neighboring Nigeria, and most of them lack residence permits, limiting their freedom to travel to other locations for essential health services. As a result, the inhabitants mostly rely on roadside drug vendors, private dispensaries, and traditional healers for their health care needs.
2.2. Sampling Methods and sample size
We used purposive sampling used to recruit participants from MHD for Key Informant Interviews (KII) with district healthcare workers based on their roles, availability, and willingness to participate. A snowballing approach served to recruit an intermixed population of caregivers composed of locals and immigrants for focused group discussions (FGD). Mothers of unvaccinated children, mothers of vaccinated children, and community leaders were recruited for separate FGD. The sample size depended on thematic saturation.
2.3. Data collection and analysis
Data collectors were trained on qualitative methods and how to handle sensitive topics with participants. Interview and FGD guides with open-ended questions were used for KII and FGDs, respectively. The data collectors collaborated with community liaisons to ease the moderation of FGDs. Tape recorders were used, and notes were taken where necessary.
Data from FGDs and KII were analyzed using thematic analysis. The audio recordings were transcribed, including translating from other interview languages to French. Coders independently coded each translated transcript and then reviewed it together to agree upon standard themes and codes for the analysis as we advanced, ensuring inter-coder reliability. The coders periodically debriefed on emergent themes to update the coding list throughout the analytical process until thematic saturation. For better analyses, the transcripts for In-depth interviews were first analyzed for exploratory reasons to learn more about vaccination hindrances and the general usage of health services. This approach helped to distill important preliminary issues regarding study themes. After this, transcripts from FGDs were analyzed to complement findings from KII. This approach helped to look at vaccine hindrances from a broader perspective, giving a more holistic explanation of low vaccination coverage by capturing the voices of women and community leaders who did not participate in the in-depth interviews and may have had a different perspective.
2.4. Ethical consideration:
Before data collection, we obtained ethical clearance from the Cameroon National Ethics Committee. Consent was obtained from each participant before they could join the study. Furthermore, the data were used solely for this study and not shared with any third party.
3. Results
Qualitative data was obtained through three FGDs involving an intermix of locals and the immigrant population. The FGDs involved Mothers of unvaccinated children (ten participants), mothers of vaccinated children (ten participants), and community leaders (seven participants), respectively. The four KII conducted targeted district and administrative level vaccine delivery coordinators. However, male caregivers were not interviewed because of failed attempts to meet fathers at home on several occasions, as they were mainly at sea for fishing. Female caregivers were found to be seemingly more expressive in a group discussion, even in the presence of a community relay agent.
The reason for the high zero-dose childhood immunization proportion in MHD can be summarized under four main themes:
3.1. Access barriers
MHD is an archipelago district with a single health facility serving 47 islets. Travel time to the lone health facility (primary healthcare facility) varies depending on the islets, from a couple of hours to 2 days (especially when persons need to sleep over in the nearest community to catch the boat the next day). The district is not viable enough to cover the cost of running frequent outreach vaccination sessions in most of the remote islets. Besides, the limited human resources (two general practitioners, two assistant nurses, one laboratory technician, and 12 active community health workers) further make routine vaccination service delivery an uphill task. The inhabitants therefore rely on national vaccination campaigns, supplementary immunization activities (SIA), and epidemic response activities to benefit from integrated vaccination services. Frequent community floods, bad weather, and sea turbulence-related risks pose a severe challenge to vaccination service delivery. For instance, one vaccine delivery coordinator noted that:
"During the planning of a vaccination campaign, you can consider going to the islets maybe on Thursday morning for sensitization, and in the morning, the sea waves are so violent to the point where you cannot dare to go."
Community leaders noted that this access challenge goes both ways:
"It is costly and risky for caregivers to take children to the lone health facility for vaccination. The lack of residence permits among the immigrant population makes it challenging for [them] to travel to vaccinate their children, especially when they must pass through other towns not within the MHD jurisdiction to get to the lone facility".
All participating community leaders (7/7) agreed it was a significant problem, so they preferred to wait and vaccinate their children during national campaigns and outreaches.
3.2. Infrastructural and resource limitations
Due to the lack of electricity, the lone health facility with non-functional cold chain equipment (CCE) limits vaccination sessions to an ’on-spot’ service delivery approach upon receiving vaccines from the regional vaccine store. Therefore, achieving optimal vaccination coverage requires frequent vaccine collection and rapid vaccine roll-out while attempting to maintain recommended vaccine temperature range using icepacks for a few days. This delivery approach is resource-consuming, especially if it includes outreach and mobile vaccination strategies to reach the last mile. Despite these difficulties and the high expenses needed to carry out routine immunization in the entire district, there is limited financing. Routine vaccine delivery-related activities are financed and managed by the health district – this was easier when most of the funding came from a support fund offered by the ministry of public health (MOH). However, this support fund has been suspended since the introduction of the Performance-Based Financing (PBF) scheme in the district in 2018. Under this financing scheme, every health facility must self-finance and lobby funds for most activities. Subsequently, they receive some refund/financial reward based on the quantity and quality of services offered. However, raising funds for vaccination in this district is quite an uphill task due to the under-utilization of health services by the community.
3.3. Communication and community engagement challenges
Given that these islets are hard-to-reach communities, a well-thought-out communication plan is employed to maximize limited resources during campaigns and outreaches. After receiving official correspondence from the district team, community leaders, through their council of elders, pass vaccination-related information to the community using town criers while religious leaders circulate the information at worship places. Community health workers play an active role in under-2 children identification through door-to-door sensitization and mobilization sessions. Despite all the communication efforts, effective vaccination sessions require a mastery of the social dynamics of the population. As hinted by a vaccine delivery coordinator:
"During fishing or drying of fish, mothers do not allow their children to wander around, so the only way to vaccinate these children is to deliver the shots in their homes and sometimes in their fishing boats."
A significant communication drawback is that community health workers are not sufficient to cover all households across the 47 islets during their mobilization activities. Also, community leaders are sometimes informed late or unformed about upcoming vaccination campaigns, leading to a general lack of vaccination awareness.
3.4. Vaccine hesitancy
Although communication is key to identifying and mobilizing children for vaccination, vaccine delivery coordinators clarified that some families only accept vaccines if the head of their ethnic group approves. While at the household level, 80% (8/10) of mothers of vaccinated children during FGD indicated that they take the decision to vaccinate their children given the fact that their husbands spend most days and nights at sea fishing. In agreement with findings from FGD with community leaders, the other 20% (2/10) of mothers of vaccinated children explained that the decision to vaccinate a child in their community is usually based on a unanimous decision from both parents. However, mothers of unvaccinated children suggested that the fathers take the final decision on childhood vaccination uptake, as explained by an immigrant mother: "It is the fathers. If they refuse, we don’t vaccinate."
Although few family cultures are against using needles on their children, most vaccine hesitancies emanate from fear, stemming from unfounded rumors that vaccines cause ill health and sterility, hinder growth, and are a tool employed to ’wipe out the Black race.
All mothers of unvaccinated children confirmed that their principal reason for not vaccinating their children was post-vaccination fever. However, mothers of vaccinated children say that the benefits of vaccination outweigh the side effects, as summarized by a 37-year-old Cameroonian lady:
"Vaccination is good. It gives a fever, but after administering paracetamol, the child feels better. It helps to prevent diseases, and even if the child develops a disease, it is milder."
However, 60% (6/10) of mothers of unvaccinated children did not like the idea of vaccinating their children at home – as they feel their privacy is being invaded and would have preferred to vaccinate them in a health facility. Mothers of vaccinated children also prefer hospital-based routine immunization but are willing to accept home-based vaccination if there are no alternatives. As one of the women mentioned, "I prefer the hospital because, if something goes wrong, the doctor will know what to give the child there to calm his situation."
Another major issue that contributed to the observed hesitancy is the frequent postponement of vaccination schedules despite the hurdles experienced by caregivers to reach the distant lone vaccinating health facility. Also, since most women give birth at home, they are not versed with vaccination schedules and are likely to miss sessions even if they want to vaccinate their child.
4. Discussion
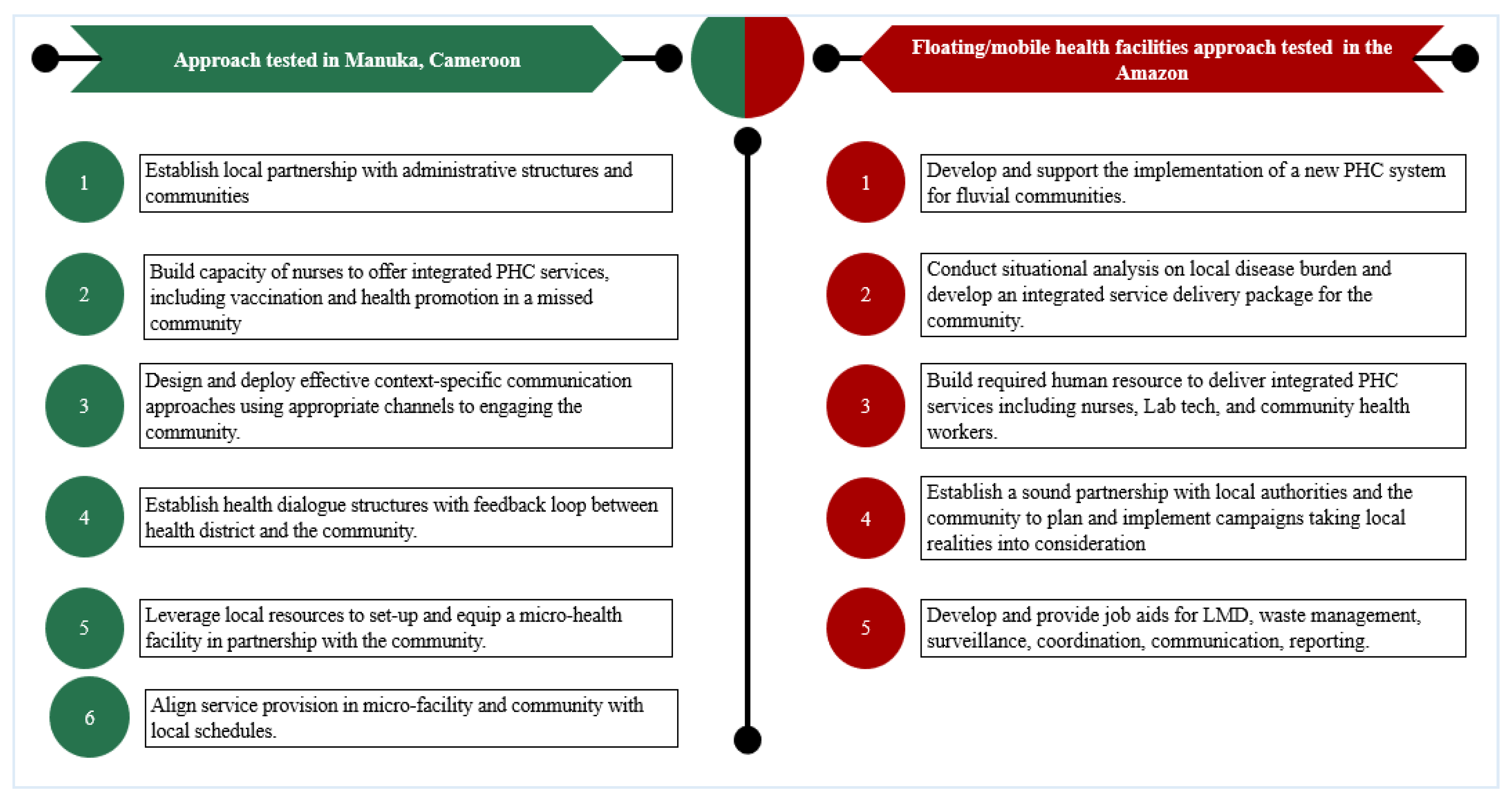
The characteristics of MHD revealed by this study are consistent with those of a vaccination hard-to-reach community based on a literature review conducted by Sachiko et al. in 2019 [
16]. The availability of only one vaccinating health facility with no functional cold chain equipment to cover 47 enclaved, distant, and poorly accessible islets; sea turbulence and the frequent diurnal floods in communities hamper vaccination service delivery. This finding is similar to those reported in remote rural municipalities in the Amazon – which are rarefied and highly dispersed populations living in conditions of social vulnerability[
17]. Planning routine outreach vaccination and campaigns in these communities need to consider these factors to maximize limited resources, as distance can significantly affect vaccine access and utilization [
16,
18]. In this setting, we have tested an approach that has helped to significantly raise vaccination coverage for all antigens. For instance, DTP-3 rose from 0% in 2019 to 73.4% in 2020 (unpublished data). This success story is similar to ones reported from settings in the Amazon in Latin America, where the authors adapted local policies and strategies that are different from those used in traditional settings, which enabled them to pay more emphasis on healthcare access rather than timing [
17,
19]. They used river vessels (which they called floating/ mobile health facilities) to offer intermittent horizontal preventive healthcare services for about 14 days per month in riverine communities. This approach greatly enhanced access to essential healthcare, including immunization, in remote rural areas in the Amazon [
19,
20]. A brief description of our approach as well as that used in the Amazon, is provided in
Figure 1.
On the demand side, we identified that lack of a resident permit is one of the major factors that enormously contributes to affecting childhood vaccine uptake in our study community. This challenge limits their ability to access essential health services outside their current residence, rendering them depended on traditional healers, birth attendants, roadside drug vendors, and unregistered private dispensaries for their health needs. So, parents may be willing to vaccinate their children, but they have no choice but to wait for an outreach vaccination program since they cannot travel to get vaccines. This finding is consistent with a systemic review of studies in sub-Saharan Africa which revealed that migration is associated with low vaccination coverage [
21]. Also, comparatively lower vaccination coverage was found among immigrants in India compared to the locals because of a high prevalence of home births, lack of awareness of the location of health facility, mobility, child’s illness, fear of side effects, and vaccine distrust [
22]. In our study, there were similar reasons for non-vaccination, although we did not separate immigrants from locals during data collection and analysis.
The access challenges and infrastructural and resource constraints in MHD highlight the need for a proper communication and mobilization plan to optimize the use of limited resources to vaccinate children. However, a significant drawback is an insufficient number of community health workers to effectively carry out a door-to-door survey and the lack of a clear and practical approach to informing community leaders early enough before vaccination outreaches for community mobilization. Sound community leader engagement approaches are critical as the study revealed that some ethnic group leaders negatively influence parents’ decision to vaccinate their children. This finding is consistent with a cluster-randomized control trial in Nigeria, which demonstrated that improving traditional leaders’ knowledge of vaccines is highly beneficial in improving vaccination coverage [
23]. The question of which parent has the final say as to whether the child gets vaccinated stirred up an inconclusive debate that showed that at least both parents can influence childhood vaccination. Therefore, this study illustrates the importance of involving both parents in vaccination counseling and awareness sessions.
The preference for facility-based rather than home-based vaccination, the distance and risk of traveling to a lone facility, and frequent postponement of vaccination schedules negatively influenced this study’s parental decision on childhood vaccination. However, studies have shown that proper vaccination scheduling and notification can reduce vaccination delays and improve vaccination coverage [
24,
25,
26]. The fear of post-vaccination fever is among the major reasons for vaccine hesitancy among mothers of unvaccinated children. Like other vaccine side effects, post-vaccination fever, though a minor side effect, could cause excessive anxiety in parents and caregivers, leading to a possibility of vaccine hesitancy [
22,
27]. However, the study revealed that mothers of vaccinated children considered post-vaccination fever to be of concern but were still willing to vaccinate their children and use antipyretics when needed. This finding illustrates the relevance of proper vaccination education in reducing vaccine phobia due to fear of post-vaccination fever. Other contributing factors to vaccine hesitancy identified were rumors and distrust of vaccines. Although reasons for vaccine hesitancy are context-specific and vary across different cultures and contexts [
28], our results are consistent with findings from a systematic review of studies in sub-Saharan Africa that revealed some of the factors found in this study, including rumors and vaccine distrust [
21]. There is, therefore, a need for well-tailored communication plans to effectively address these hesitancies.
5. Conclusions
To effectively control vaccine-preventable diseases, there is a need to focus on and prioritize zero-dose children in underserved communities. Studies such as this, which explores context-specific childhood vaccination barriers, are essential in filling the knowledge gap and setting a foundation for proper routine vaccination roll-out plan in missed communities. As noted, the immigrant population, especially those without legal residence status, are vulnerable and traditionally miss routine childhood vaccination services. Dialogue structures with a feedback loop that links the community with the health district service will build trust, enhance communication and awareness, and improve vaccination coverage. Using effective resource mobilization to support culturally sensitive approaches to implementing SIA, vaccination campaigns, and outreaches as recommended by WHO will improve vaccination coverage in this context [
29,
30]. Also, investment in satellite micro-facilities in remote communities could significantly improve vaccine uptake, especially in underserved communities.
6. Limitations of the Study
Although our study design was thorough, like other qualitative studies, there is a problem of generalizability. However, findings are reflexive of challenges in vaccination uptake in similar hard-to-reach settings.
There was a risk of social desirability bias that may have occurred during FGDs [
31]. In this study, we tried to curb this by conducting different FGDs for mothers of unvaccinated and vaccinated children. However, this initial segregation was not done for community leaders.
In-depth interviews with mothers perhaps will have been influential in this research. However, during data collection, several interview attempts were very unrevealing. The women were not expressive because they were uncomfortable talking to strangers, even in the presence of a community liaison. They were more explicit in an FGD, so the data source for both mothers of vaccinated and unvaccinated children was FGDs.
Fathers were not involved in the qualitative study because of their unavailability. Three failed attempts to get an interview or FGD with fathers as they spend most of their time at sea, and their schedules are unpredictable since it depends wholly on the fish catch.
7. Research recommendation
The immigrant population has peculiarities different from the locals, which affects how they perceive and access childhood vaccination. It will be valuable to carry out a study that collects data from this population separate from the locals to understand their challenges and decision-making process on childhood vaccines.
The primary goal of vaccination is for every child to get the required vaccines – the timing is also important but secondary. This is especially true in remote rural settings where national vaccination policies and routine service delivery strategies seem alien. It might be more beneficial to have vaccination campaigns 3-4 times per year to vaccinate children in these islets, adhering to the minimum vaccination criteria even if the timing is off. Action research to establish the benefits of implementing such tailored policies and strategies could be valuable in achieving the WHO 2030 Immunization Agenda.
Author Contributions
conceptualization, Yauba Saidu, Pietro Mattei, Sangwe Nchinjoh, Adidja Amani, Shalom Ndoula, Owens Wiwa, Emanuele Montomoli, Sue Ann Clemens, Chen Stein Zamir, and Sveta Roberman; Data curation, Yauba Saidu, Sangwe Nchinjoh, Nkwain Muteh, Nadege Nnang, Shalom Ndoula and Songo Ancel; Formal analysis, Yauba Saidu and Sangwe Nchinjoh; Funding acquisition, Yauba Saidu and Pietro Mattei; Investigation, Yauba Saidu, Nadege Nnang, Andreas Njoh and Songo Ancel; Methodology, Yauba Saidu, Pietro Mattei, Sangwe Nchinjoh, Nkwain Muteh, Nadege Nnang, Andreas Njoh, Adidja Amani, Shalom Ndoula, Calvin Tonga, Owens Wiwa, Emanuele Montomoli, Sue Ann Clemens, Chen Stein Zamir, and Sveta Roberman; Project administration, Nkwain Muteh and Nadege Nnang; Supervision, Pietro Mattei, Nkwain Muteh, Andreas Njoh, Shalom Ndoula, Owens Wiwa, Emanuele Montomoli and Sue Ann Clemens; Validation, Yauba Saidu and Pietro Mattei; Writing – original draft, Yauba Saidu, Sangwe Nchinjoh, Adidja Amani, and Sveta Roberman; Writing – review & editing, Yauba Saidu, Pietro Mattei, Sangwe Nchinjoh, Nkwain Muteh, Nadege Nnang, Andreas Njoh, Adidja Amani, Songo Ancel, Calvin Tonga, Owens Wiwa, Emanuele Montomoli, Sue Ann Clemens, Chen Stein Zamir, and Sveta Roberman;
Funding
This research received no external funding.
Informed Consent Statement
formed consent was obtained from all subjects involved in the study.
Data used for this research is available from the corresponding author upon reasonable request.
Acknowledgments
our gratitude to Gavi for funding the conduct of this study, the Staff of the Expanded Program on Immunization for their oversights, and the Staff of the Manoka Health District for coordinating the data collection process. We are also grateful to the local authorities, including the Mayor of Manoka, the Village Head of Cap-Cameroon, the various religious leaders, and the people who took part in the FGDs and in-depth interviews.
Conflicts of Interest
The authors declare no conflict of interest.
is study was conducted in compliance with the Helsinki Declaration and all applicable national laws and institutional rules and has been approved by the author’s institutional review board. Ethical approval was granted by the Cameroon National Ethics Committee for Human Health Research with the reference 2019/07/1174/CE/CNERSH/SP on 12TH of July 2019.
Ethics approval and Consent to Participate
is study was conducted in compliance with the Helsinki Declaration and all applicable national laws and institutional rules and has been approved by the author’s institutional review board. Ethical approval was granted by the Cameroon National Ethics Committee for Human Health Research with the reference 2019/07/1174/CE/CNERSH/SP on 12TH of July 2019.
Availability of data and materials
Data used for this research is available from the corresponding author upon reasonable request.
References
- Fokoun C. Strategies implemented to address vaccine hesitancy in France: A review article. Hum Vaccines Immunother 2018;14:1580–90. [CrossRef]
- Nathanson N, Kew OM. From Emergence to Eradication: The Epidemiology of Poliomyelitis Deconstructed. Am J Epidemiol 2010;172:1213–29. [CrossRef]
- Global Vaccine Action Plan n.d. https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/global-vaccine-action-plan (accessed December 25, 2020).
- Chard AN, Gacic-Dobo M, Diallo MS, Sodha SV, Wallace AS. Routine Vaccination Coverage — Worldwide, 2019. Morb Mortal Wkly Rep 2000;69:1706–10. [CrossRef]
- WHO Immunization Data portal n.d. https://immunizationdata.who.int/pages/profiles/cmr.html (accessed August 27, 2022).
- WHO. WHO 2021. Framework for the implementation of the 2030 immunization program in the WHO African Region: Secretariat Report 2021.
- Mansour Z, Arab J, Said R, Rady A, Hamadeh R, Gerbaka B, et al. Impact of COVID-19 pandemic on the utilization of routine immunization services in Lebanon. PLOS ONE 2021;16:e0246951. [CrossRef]
- Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: An analysis of provincial electronic immunization registry data. Vaccine 2020;38:7146–55. [CrossRef]
- Desta AA, Woldearegay TW, Gebremeskel E, Alemayehu M, Getachew T, Gebregzabiher G, et al. Impacts of COVID-19 on essential health services in Tigray, Northern Ethiopia: A pre-post study. PLOS ONE 2021;16:e0256330. [CrossRef]
- Russo G, Miglietta A, Pezzotti P, Biguioh RM, Mayaka GB, Sobze MS, et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12-23 months in Dschang, West Region, Cameroon: a cross-sectional survey during a polio outbreak. BMC Public Health 2015;15:1–11. [CrossRef]
- Nchinjoh SC, Saidu Y, Agbor VN, Mbanga CM, Jude Muteh N, Njoh AA, et al. Factors Associated with Zero-Dose Childhood Vaccination Status in a Remote Fishing Community in Cameroon: A Cross-Sectional Analytical Study. Vaccines 2022;10:2052. [CrossRef]
- Ateudjieu J, Yakum MN, Goura AP, Tembei AM, Ingrid DK, Bita’a Landry B, et al. EPI immunization coverage, timeliness and dropout rate among children in a West Cameroon health district: a cross sectional study. BMC Public Health 2020;20:1–11. [CrossRef]
- Ebile Akoh W, Ateudjieu J, Nouetchognou JS, Yakum MN, Djouma Nembot F, Nafack Sonkeng S, et al. The expanded program on immunization service delivery in the Dschang health district, west region of Cameroon: a cross sectional survey. BMC Public Health 2016;16:801. [CrossRef]
- Chiabi A, Nguefack FD, Njapndounke F, Kobela M, Kenfack K, Nguefack S, et al. vaccination of infants aged 0 to 11 months at the Yaounde Gynaeco-obstetric and pediatric hospital in Cameroon: how complete and how timely? BMC Pediatr 2017;17. [CrossRef]
- Pouth SFBB, Kazambu D, Delissaint D, Kobela M. Couverture vaccinale et facteurs associés à la non complétude vaccinale des enfants de 12 à 23 mois du district de santé de Djoungolo-Cameroun en 2012. Pan Afr Med J 2014;17. [CrossRef]
- Ozawa S, Yemeke T, Evans D, Pallas S, Wallace A, Lee B. Defining hard-to-reach populations for vaccination. Vaccine 2019;37. [CrossRef]
- Branco FLCC, Pereira TM, Delfino BM, Braña AM, Oliart-Guzmán H, Mantovani SAS, et al. Socioeconomic inequalities are still a barrier to full child vaccine coverage in the Brazilian Amazon: a cross-sectional study in Assis Brasil, Acre, Brazil. Int J Equity Health 2014;13:118. [CrossRef]
- Muathe EC, Kamau M, Rajula E. Exploring Strategies to Improve Adherence to Immunization Schedule: A Study among Children Attending Maternal and Child Health Clinic at Kenyatta National Hospital, Nairobi, Kenya. Int J Pediatr 2020;2020:e4730205. [CrossRef]
- Fausto MCR, Giovanella L, Lima JG, Cabral LM da S, Seidl H. Primary Health Care sustainability in rural remote territories at the fluvial Amazon: organization, strategies, and challenges. Ciênc Saúde Coletiva 2022;27:1605–18.
- Kadri MRE, Santos BS dos, Lima RT de S, Schweickardt JC, Martins FM. Floating Primary Health Center: a new approach to Primary Care in the Amazon, Brazil. Interface - Comun Saúde Educ 2019;23. [CrossRef]
- Bangura JB, Xiao S, Qiu D, Ouyang F, Chen L. Barriers to childhood immunization in sub-Saharan Africa: A systematic review. BMC Public Health 2020;20:1108. [CrossRef]
- Kusuma YS, Kaushal S, Sundari AB, Babu BV. Access to childhood immunisation services and its determinants among recent and settled migrants in Delhi, India. Public Health 2018;158:135–43. [CrossRef]
- Oyo-Ita A, Bosch-Capblanch X, Ross A, Oku A, Esu E, Ameh S, et al. Effects of engaging communities in decision-making and action through traditional and religious leaders on vaccination coverage in Cross River State, Nigeria: A cluster-randomised control trial. PLOS ONE 2021;16:e0248236. [CrossRef]
- Oyo-Ita A, Wiysonge CS, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database Syst Rev 2016;7:CD008145. [CrossRef]
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014;14:188. [CrossRef]
- Kazi AM, Ali M, Zubair K, Kalimuddin H, Kazi AN, Iqbal SP, et al. Effect of Mobile Phone Text Message Reminders on Routine Immunization Uptake in Pakistan: Randomized Controlled Trial. JMIR Public Health Surveill 2018;4:e7026. [CrossRef]
- Ahn SH, Zhiang J, Kim H, Chang S, Shin J, Kim M, et al. Postvaccination Fever Response Rates in Children Derived Using the Fever Coach Mobile App: A Retrospective Observational Study. JMIR MHealth UHealth 2019;7:e12223. [CrossRef]
- Ogundele O, Ogundele T, Beloved O. Vaccine hesitancy in Nigeria: Contributing factors – way forward. Niger J Gen Pract 2020;18:1. [CrossRef]
- Vijayaraghavan M, Martin RM, Sangrujee N, Kimani GN, Oyombe S, Kalu A, et al. Measles supplemental immunization activities improve measles vaccine coverage and equity: Evidence from Kenya, 2002. Health Policy Amst Neth 2007;83:27–36. [CrossRef]
- Sutter RW, Maher C. Mass Vaccination Campaigns for Polio Eradication: An Essential Strategy for Success. In: Plotkin SA, editor. Mass Vaccin. Glob. Asp. — Prog. Obstacles, Berlin, Heidelberg: Springer; 2006, p. 195–220. [CrossRef]
- Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant 2013;47:2025–47. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).