1. Introduction
Surgical ciliated cysts, also known as postoperative maxillary cysts, respiratory implantation cysts, or paranasal cysts are the collective term for a non-odontogenic cyst lined by respiratory epithelium because of traumatic implantation to the sinus or nasal mucosa [
1]. It occurs most commonly in the maxilla, but rarely in the mandible due to implantation of sinus epithelium by contaminated instruments or using nasal bone or cartilage with epithelium for augmentation genioplasty[2, 3]. Although this condition has been reported, its occurrence in the infratemporal fossa has not yet been reported.
Here, we present a case of a surgical ciliated cyst of the infratemporal fossa that was completely resolved using marsupialization via Le Fort I osteotomy.
2. Case Report
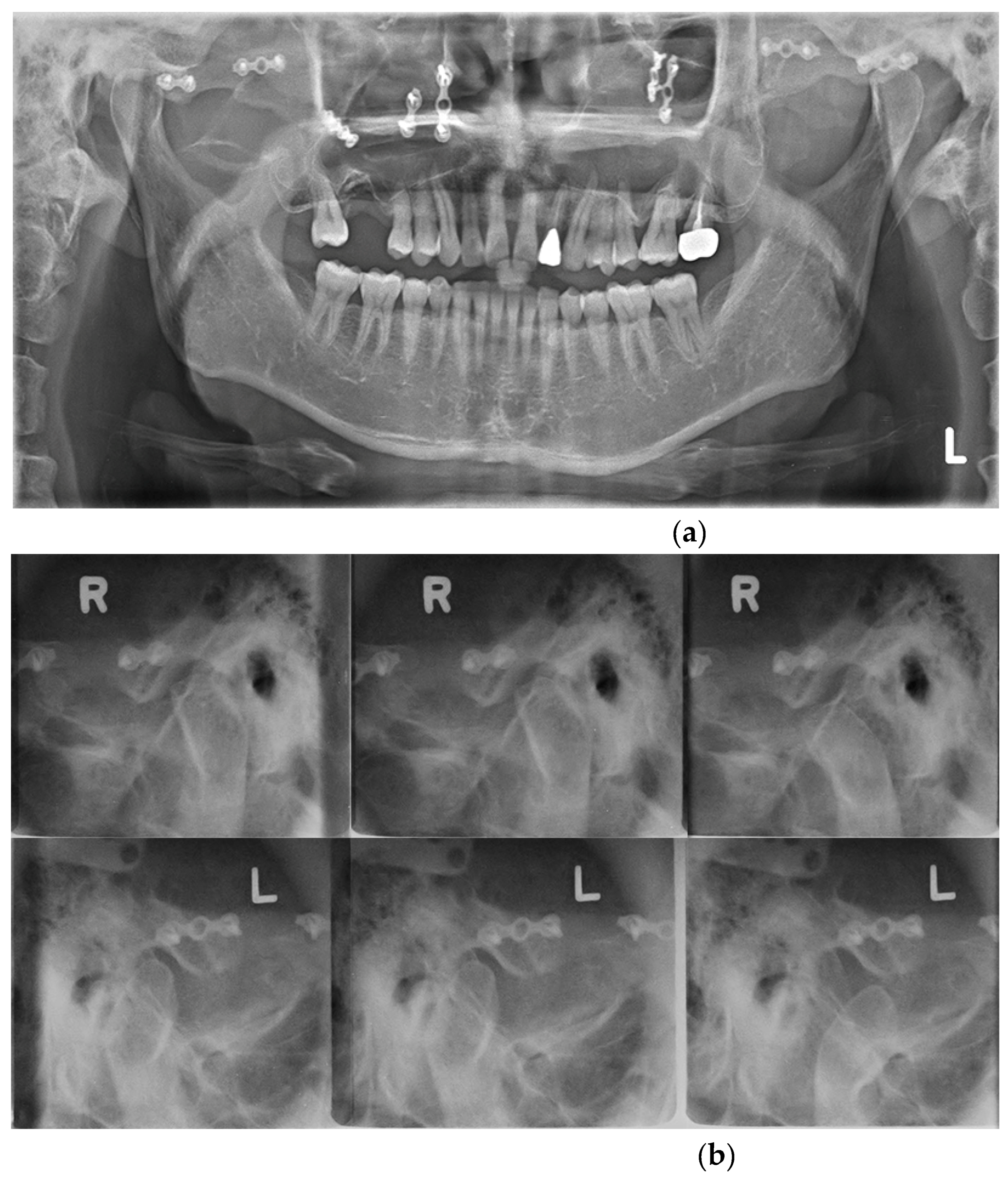
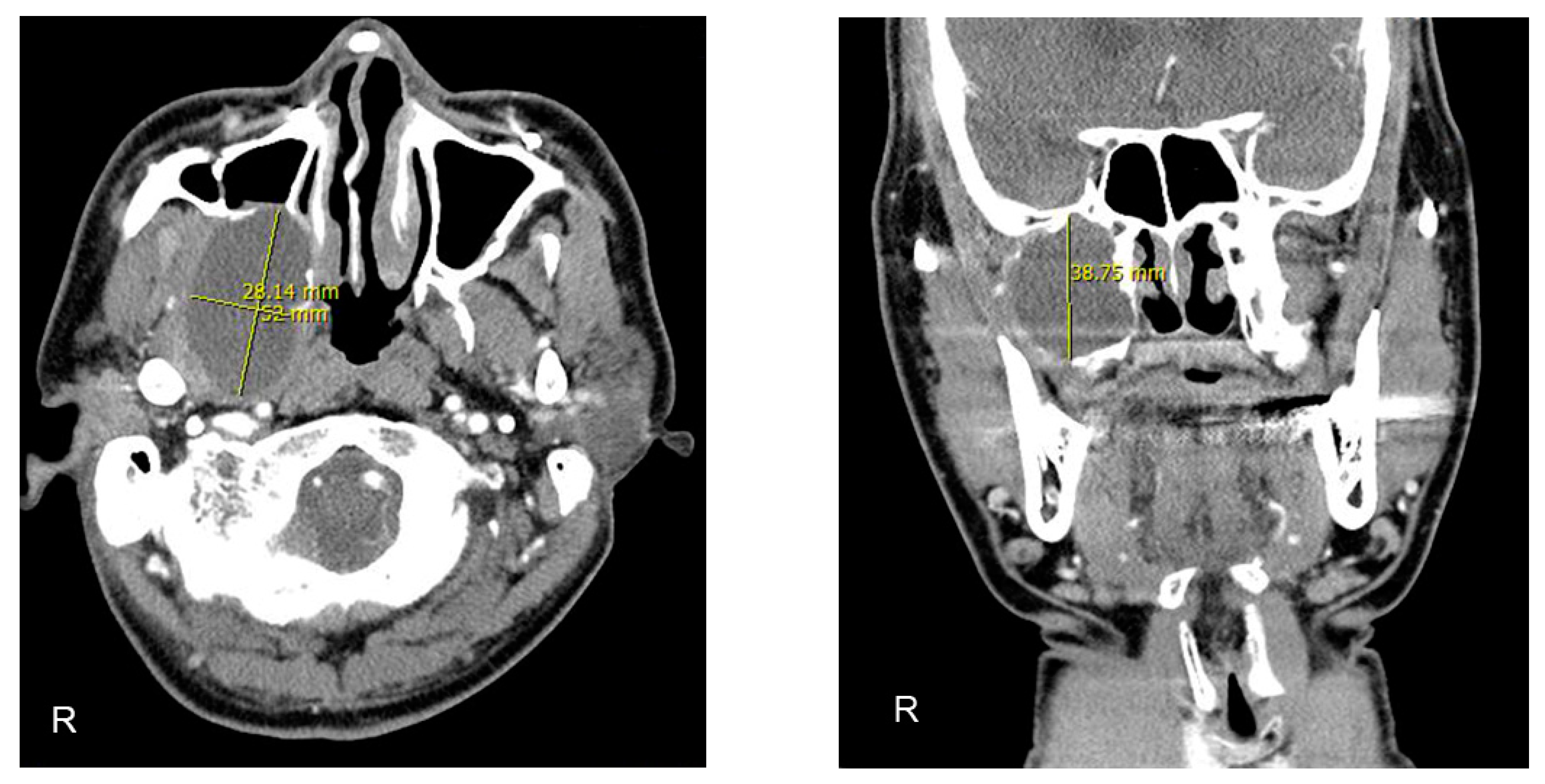
A 40-year-old man was referred to the Department of Oral and Maxillofacial Surgery with mandibular pain and limited mouth opening. Symptoms had started a year previously and gradually deteriorated. He was otherwise healthy but had experienced a facial bone fracture 25 years ago. On initial clinical examination, the maximum mouth opening was 26mm because of pain. Radiographic investigations included Panorex imaging (Fig. 1-a), transcranial view of temporomandibular joint (Fig. 1-b), computed tomography (CT) with contrast (Fig. 2-a, b), and magnetic resonance imaging (MRI) (Fig. 2-c, d). The studies confirmed a well-defined large osteolytic lesion 2.8 × 5.2 × 3.8 cm in the right infratemporal fossa with extension into the maxillary sinus and foramen ovale.
Figure 1.
Plain radiographs taken at first visit. (a) Panorex showing old miniplates and screws on the midface area; (b) In the transcranial view of the temporomandibular joint, no significant bony changes of the condyles were observed, but the movement of both condyles appeared to be restricted.
Figure 1.
Plain radiographs taken at first visit. (a) Panorex showing old miniplates and screws on the midface area; (b) In the transcranial view of the temporomandibular joint, no significant bony changes of the condyles were observed, but the movement of both condyles appeared to be restricted.
Figure 2.
Preoperative computed tomography (CT) with contrast and magnetic resonance imaging (MRI) scans showing a well-defined osteolytic 2.8 × 5.2 × 3.8 cm lesion extended into the right maxillary sinus and pterygoid plate. (a) Axial view of CT. (b) Coronal view of CT. (c) Axial view of T1-weighted MRI. (d) Axial view of T2-weighted MRI.
Figure 2.
Preoperative computed tomography (CT) with contrast and magnetic resonance imaging (MRI) scans showing a well-defined osteolytic 2.8 × 5.2 × 3.8 cm lesion extended into the right maxillary sinus and pterygoid plate. (a) Axial view of CT. (b) Coronal view of CT. (c) Axial view of T1-weighted MRI. (d) Axial view of T2-weighted MRI.
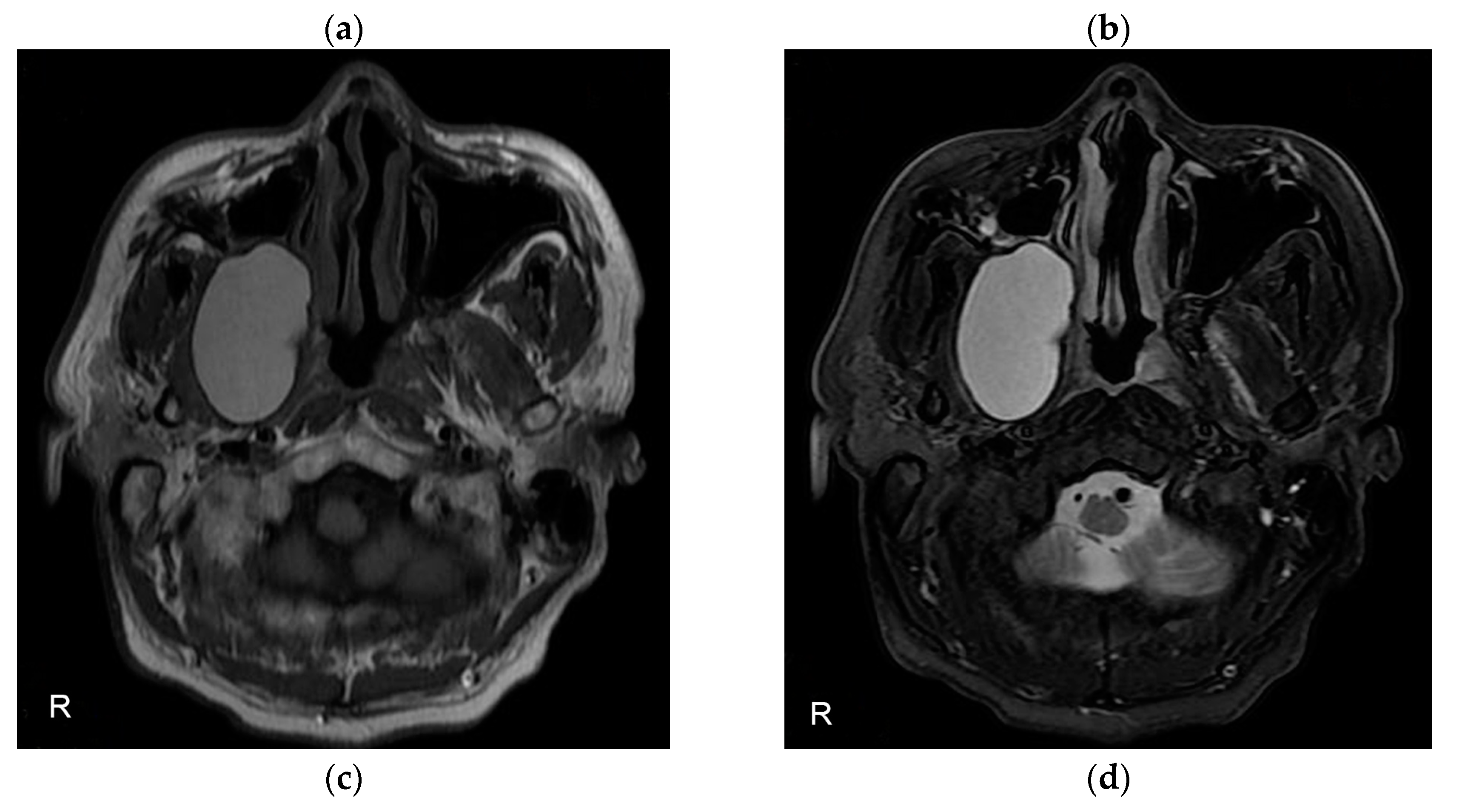
Under general anesthesia, old plates and screws on the anterior maxilla were removed, and a standard Le Fort I osteotomy was performed. After the downfracture, the lesion was carefully dissected and visualized. Aspiration was performed to confirm the lesion was a cyst, and slightly yellow, serous fluid was withdrawn. Partial excision of an ovoid shape of the cystic wall (0.8 × 2.4 × 0.3 cm) was made for a histopathologic exam. After repositioning the maxilla, a 1 x 1 cm sized bony window was made on the canine fossa area. The 10-cm Penrose drain tube was inserted at the end of the cyst through the anterior bony window. The drain was secured in place with a 3-0 non-absorbable suture to the anterior vestibular mucosa. The operative course was uneventful, and the patient was discharged on the third postoperative day. Before discharge, the patient was instructed to independently irrigate the wound with saline using a syringe after each meal. Histopathologic evaluation showed a pseudostratified ciliated columnar epithelium and focally squamous epithelium compatible with the diagnosis of a surgical ciliated cyst (Fig. 3).
Figure 3.
Histopathological features of pseudostratified epithelial lining with papillary arrangement (hematoxylin and eosin, original magnification ×200).
Figure 3.
Histopathological features of pseudostratified epithelial lining with papillary arrangement (hematoxylin and eosin, original magnification ×200).
Regular follow-up visits were scheduled every other month for Penrose drain adjustments. The drain was shortened by 1 cm monthly. A follow-up CT scan performed 2 months after surgery showed a decreasing bony defect and regenerating bone around the drain. The drain was fully removed 5 months after surgery. CT taken 3 years postoperatively showed evidence of complete bony regeneration without recurrence (Fig. 4-a, b).
Figure 4.
CT scan 3 years after surgery showing complete resolution without recurrence. (a) Axial view of CT; (b) Coronal view of CT.
Figure 4.
CT scan 3 years after surgery showing complete resolution without recurrence. (a) Axial view of CT; (b) Coronal view of CT.
3. Discussion
The infratemporal fossa is a rectangular posterior maxillary space located deep in the skull base that contains important neurovascular structures such as the pterygoid muscle, mandibular nerve, tympanic cord, middle meningeal artery, internal maxillary artery and vein, and pterygoid venous plexus[
4]. The foramen ovale is just posterior to the junction of the lateral pterygoid plate with the body of the sphenoid, and the foramen spinosum is located a few millimeters posterolaterally[
5]. The classic approaches to the infratemporal fossa can be categorized into anterior, lateral, and transcranial pathways[
6]. Because of the significant morbidities associated with invasive surgery of the infratemporal fossa, less invasive alternatives are recommended[
7].
Le Fort I osteotomy was neglected as a surgical approach for decades before regaining popularity in the late 1980s, especially for the removal of tumors at the base of the skull and midface[8, 9]. The major advantage of this procedure is that it provides a wide surgical field of view in the maxillary sinus, and nasopharynx, allowing large cysts such as those described in this article to be easily exposed without needing an otherwise extended and unacceptable resection of the maxillary bone. Disadvantages are related to the classic intra- and perioperative complications associated with maxillary osteotomies, such as anatomic deviation, hemorrhage, infection, malocclusion, nonunion or pseudoarthrosis, maxillary sinusitis, and maxillary bone necrosis, which are rare[
10].
For the treatment of surgical ciliated cysts, most previous studies have recommended a Caldwell-Luc operation consisting of complete removal of the cyst lining, together with nasal antrostomy[11-13]. Primary closure or open packing yielded equally effective results, and marsupialization may be indicated for the treatment of unilocular cysts with a thin cystic wall and extensive bony perforation or when cysts are located in an inaccessible location[
14].
In our patient, based on the high T1/T2 signal on MRI, the lesion was suspected to be cystic. Some benign tumors, such as epidermal inclusion cysts, fibromas, and schwannomas may present with similar features in the infratemporal fossa. Differential diagnosis includes neurogenic tumors, lymphangioma dermoid/epidermoid cysts, and surgical ciliated cysts. Because the lesion was regarded as non-malignant, we considered surgical excision immediately without performing an incisional biopsy before surgery. During surgery, complete enucleation of the lesion without injury to the adjacent structures was considered impossible because of the thin cystic wall and extensive bone loss, and the lesion was marsupialized.
4. Conclusions
Surgical ciliated cysts occur as a delayed complication after radical surgical intervention and trauma in the maxillary sinus and rarely recur after appropriate surgical treatment. Surgical procedures are determined according to the location or aggressiveness of the lesion. This is the first report of the marsupialization via Le Fort I osteotomy of a surgical ciliated cyst in the deep infratemporal fossa. The risk of significant morbidity associated with an isolated surgical ciliated cyst of the infratemporal fossa can be minimized by proper diagnosis and less invasive surgery, including the most appropriate surgical approach.
Author Contributions
Conceptualization, D.-W.K. and M.-Y.K.; methodology, D.-W.K., J.H.Y. and M.-Y.K.; validation, D.-W.K., H.-S.P. and J.-H.L.; investigation, J.-H.L. and M.-Y.K.; resources, D.-W.K. and J.H.Y.; writing—original draft preparation, D.-W.K. and M.-Y.K.; writing—review and editing, E.-S.K., H.-S.P., J.-H.L. and M.-Y.K.; supervision, M.-Y.K.; funding acquisition, M.-Y.K. All authors have read and agreed to the published.
Funding
M.-Y.K. was supported by a National Research Foundation of Korea (NRF) grant funded by the Ministry of Science and ICT (2021R1C1C1008843), Priority Research Center Program provided by the Ministry of Education (2019R1A6A1A11034536) and Medical Research Center Program NRF (2021R1A5A2022318) and the Global Research Development Center Program (2018K1A4A3A01064257).
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mete O, Wenig BM: Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Overview of the 2022 WHO Classification of Head and Neck Neuroendocrine Neoplasms. Head and neck pathology 2022, 16(1):123-142.
- Bourgeois SL, Jr., Nelson BL: Surgical ciliated cyst of the mandible secondary to simultaneous Le Fort I osteotomy and genioplasty: report of case and review of the literature. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics 2005, 100(1):36-39.
- Amin M, Witherow H, Lee R, Blenkinsopp PJJoo, surgery m: Surgical ciliated cyst after maxillary orthognathic surgery: report of a case. 2003, 61(1):138-141.
- Joo W, Funaki T, Yoshioka F, Rhoton Jr ALJCA: Microsurgical anatomy of the infratemporal fossa. 2013, 26(4):455-469.
- Tiwari RJJoC-MS: Surgical landmarks of the infratemporal fossa. 1998, 26(2):84-86.
- Chung HJ, Moon IS, Cho H-J, Kim C-H, Sharhan SSA, Chang JH, Yoon J-H: Analysis of Surgical Approaches to Skull Base Tumors Involving the Pterygopalatine and Infratemporal Fossa. Journal of Craniofacial Surgery 2019, 30(2).
- Haidar H, Deveze A, Lavieille JP: Mini-invasive surgery of infratemporal fossa schwannomas. The Journal of Laryngology & Otology 2015, 129(2):187-193.
- Hopkins R, Seel D: The use of a Le Fort I osteotomy as a surgical approach. The British journal of oral surgery 1975, 13(1):27-32.
- Brown DH: The Le Fort I maxillary osteotomy approach to surgery of the skull base. The Journal of otolaryngology 1989, 18(6):289-292.
- Kramer F-J, Baethge C, Swennen G, Teltzrow T, Schulze A, Berten J, Brachvogel PJJoCS: Intra-and perioperative complications of the LeFort I osteotomy: a prospective evaluation of 1000 patients. 2004, 15(6):971-977.
- Basu MK, Rout PGJ, Rippin JW, Smith AJ: The post-operative maxillary cyst: Experience with 23 cases. International Journal of Oral and Maxillofacial Surgery 1988, 17(5):282-284.
- Iinuma T, Mizutani A, Miyakawa KJPO: Postoperative cysts of the maxilla: A review of 474 cases. 1974, 67:427-436.
- Gregory GJJoS: Surgical ciliated cysts of the maxilla: report of cases. 1958, 16:251-253.
- Yoshikawa Y, Nakajima T, Kaneshiro S, Sakaguchi M: Effective treatment of the postoperative maxillary cyst by marsupialization. Journal of Oral and Maxillofacial Surgery 1982, 40(8):487-491.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).