1. Introduction
Asthma is a chronic inflammatory condition of the airways including mast cells, eosinophils, neutrophils (particularly in abrupt onset, deadly exacerbations, occupational asthma, and smokers), T lymphocytes, macrophages, and epithelial cells [
1]. In sensitive individuals, this inflammation causes repeated coughing, wheezing, dyspnea, and chest tightness. Widespread but mild airflow blockages can be reversed spontaneously or medically. Increases in asthma prevalence, morbidity and mortality have intensified public health concern [
2]. Clinical manifestations of asthma can be controlled with appropriate treatment. There should be only occasional symptoms and no serious asthma attacks. Patients with asthma who are hospitalized had a lower preference for decision-making autonomy [
3]. Delaying the commencement of appropriate therapy during acute severe attacks might potentially result in adverse asthma outcomes. This is a major cause for concern because patients are known to discontinue treatment unintentionally due to a lack of knowledge about the numerous treatment options [
4]. When a patient's conduct and attitudes are affected by fear, it's because they don't grasp the situation. Providing asthma patients with the education they need to manage their condition effectively is a top priority for healthcare providers. Noncompliance, insufficient severity assessment, and inadequate therapy all contribute to generally poor control [
5]. Only physicians have been offering asthma education for decades to patients, which supports the necessity for additional sectors including nongovernmental groups, the media, and health professionals to educate patients about asthma [
6]. Denial about having a chronic condition, poor knowledge of the disease process and medication use, as well as poor comprehension of how to utilize inhalers, are all variables that contribute to asthma morbidity [
5,
6].
An interactive learning experience that changes patients' knowledge and health behaviors through teaching, counseling, and behavior modification tactics enables patients to actively participate in their health care. Most experts believe asthma education improves patient understanding, but other health effects vary [
7]. Lacking these skills increases asthma-related hospitalizations and ER visits. Morbidity and education, knowledge, and sickness behaviors remain a mystery. Patients were taught about a disease's origin, treatments, and triggers [
8]. They'll all tell you that they're overwhelmed by the amount of information out there on asthma. Generally, asthma education programs teach participants how to manage their asthma with a doctor (self-management), or both [
9]. A comprehensive asthma self-management program is required. One of the simplest and most cost-effective ways to educate people about asthma is to simply provide them with information on the disease and how to treat it. Either a hospital or a community setting can easily undertake this study [
10]. An interactive or non-interactive method of delivering asthma information can be used. Lectures, audiovisual presentations, and group discussions are all examples of forms of interactive learning that may be used in either individual or group sessions with a teacher. Other examples include role-playing, project or assignment-based learning, participatory learning, and the case method for developing problem-solving skills [
11].
The Knowledge, attitude, and perception [
6] study sought to learn more about patients' knowledge of risk factors for developing asthma and worsening the disease, as well as ways to help those who suffer from it. These sessions should focus on improving patients' knowledge of asthma, reducing risk factors, and avoiding medication side effects [
4]. A study showed that both asthma knowledge and social support had a significant positive relationship with asthma self-management behaviors variability [
5]. This study aimed to assess the knowledge of asthmatic patients regarding bronchial asthma and proper education in terms of improving their knowledge regarding meaning, risk factors, signs and symptoms, diagnostic measures, management, and prevention of bronchial asthma.
2. Materials and Methods
2.1. Design and ethics
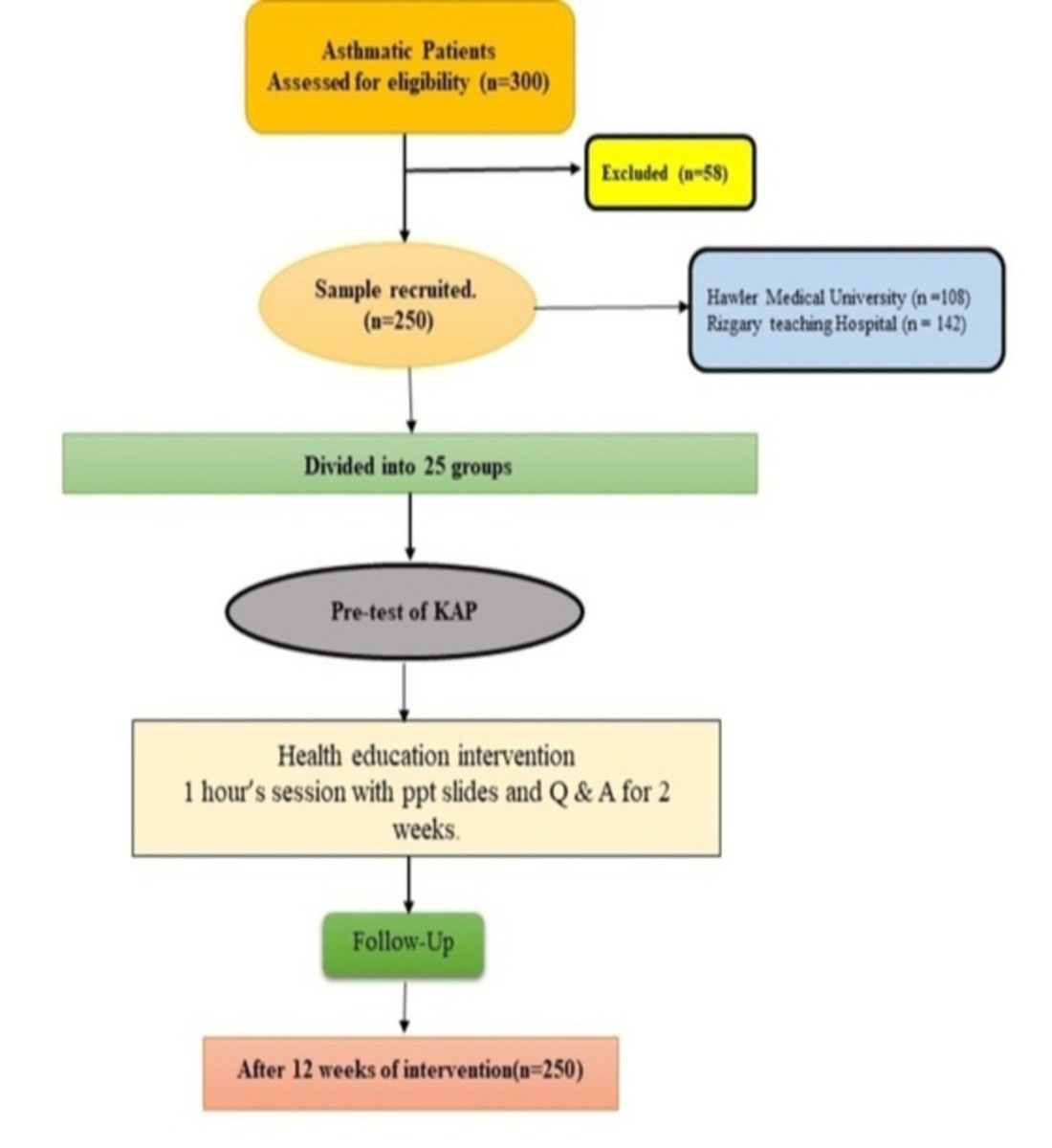
Using a questionnaire, we conducted a cross-sectional interventional survey of the KAP of patients with asthma in Erbil, Iraq. We used a validated study questionnaire based on the methodology of KAP studies conducted in other countries and adapted it to the Erbil situation and culture. The Ethics Committee for Research Involving Human Subjects at Universiti Sains Malaysia (USM) ,the Ministry of Health, Iraq's Ethics Committee for Research involving Human Subjects, and the administration of Rizgary Teaching Hospital and Hawler Medical University were also granted permission to conduct the study.
2.2. Participants
The study was conducted in the asthma clinics of two tertiary hospitals in Erbil city, Kurdistan region of Iraq. We selected 250 patients with asthma who presented at a hospital between from 1st October 2018 to 31st July 2019 and had been diagnosed with asthma for at least 3 months. The diagnoses must have conformed with the guidelines for the diagnosis and management of asthma by Ministry of Health, Iraq.
2.3. Questionnaire
Vallerand's technique [
13] validates the Gare's KAPQ across cultures [
14]. Seven steps: 1. Preparation of a preliminary version; 2. Evaluation and revision; 3. Pretest (verification of items clarity by the target population); 4. Concurrent and content validity; 5. Reliability; 6. Construct validity; 7. Concurrent validity, construct validity, reliability, and responsiveness to questionnaire design changes.
2.4. Preparation
The first draft of the Kurdish KAPQ was developed after the English version was translated by a professional translator with experience in the medical field. Kurdish speaking asthma specialists reviewed each item of the KAPQ to ensure that it contained the correct medical terminology. As a final step, a professional translator performed a back-translation to see how the two translations differed in the original language.
2.5. Evaluation and modification of content
Two other bilingual asthma specialists and a psychometric methodology expert evaluated the preliminary KAPQ, which was conducted by a committee of four researchers. Content validity was determined after two levels of evaluation. The committee first compared the original and back-translated English versions of each item to ensure that the meaning was consistent for each pair of items. Secondly, they checked the final Kurdish version (KAPQ) to make sure that there were no jargon-laden technical terms in it.
Pretest of the PAKQ
Kurdish-speaking asthmatics (n = 25) were invited sequentially to test the questionnaire to ensure that each item was clear, unambiguous, and written in a language they were familiar with before it was distributed to the general population. Random-probe interviews were used to accomplish this. The 42 questions were all found to be unambiguous, and it appears that patients had no difficulty deciphering their meaning. The original has not been altered in any way.
2.7. Validation
By conducting confirmatory factor analyses, we were able to determine the questionnaire's factorial structure. KAPQ found reliable with a high internal consistency (T0 = 0.84 and T1 = 0.92).
2.8. Health education program
A robust health education session was prepared with the help of the Asthma and Allergy Foundation America (AAFA) and the School of Pharmaceutical Sciences, Universiti Sains Malaysia. A PowerPoint presentation in Kurdish with a printout was used to deliver the health education program. PPT slide content and information were purchased with copyright from AAFA for patient education purposes. The presentation's contents were organized in the following order: common definition of asthma, causes, risk factors, diagnosis, treatment modalities, use of inhalers, preventive measures, and final message.
2.9. Intervention
Interview development used pre- and post-test designs. Before health education, asthmatics were questioned on their preventative knowledge, attitudes, and practices. Health education was provided for two weeks. 25 patients were grouped. Two sets of kids had a one-hour education session each morning and afternoon. Each ten-patient group had a PI-carrying respiratory physician assistant. The intervention was documented and communicated throughout. Every meeting ended with questions and replies for further discussion.
2.10. Data collection
Pre-intervention evaluation questionnaires and a cover letter describing the study objective were issued initially. Two hospitals conducted two-day pre-testing. 142 Rizgary hospital and 100 Hawler hospital patients under Hawler Medical University completed pre-test questionnaires. Patients were briefed on the study and told not to discuss their questions or responses with others. They had consented to fill out a questionnaire for this study. Both universities' lecture halls hosted these events. The questionnaire might be completed in these well-lit, quiet places. Patients were encouraged to return questionnaires quickly. Patients could easily drop off completed questionnaires at any hall ward's main desk. Health education followed. Thus, patients receive PPT slides and printed documents. 25 groups received one-hour interventions over two weeks. Twelve weeks following health education, participants received similar questions. Patients were instructed to keep their issue private. Patients can drop off completed questionnaires at the front desk, just like in the pre-intervention assessment.
2.11. Analysis of data
Means and standard deviations were used as a measures of central tendency and dispersion, to describe the continuous variables like. For not normality distributed variables, the variables was described based on median and interquartile range. Categorical measured variables were described by used frequencies and percentages. Paired t-test was used for the comparison of the pre and post test score.
3. Results
3.1. Patients’ characteristics
Table 1 shows the socio-demographic characteristics of the respondent. The mean age of the respondent was 37.52±15.16. More than half of the participants were male (51.6%). Nearly two-third were married (72.4%), while 41.6 % were reported illiterate. Housewife (28.4%) were the most common occupations following worker 924.8%) and professionals (20.0%) like teacher, engineer, doctor, architecture etc. Only one-third of the respondents had smoking habit (26.9%). 48.7 % respondent having a positive family history of the asthma with a duration of 1-2 years (46.2%) following 0-12 months (39.8%).
3.2. Knowledge of asthmatic patients regarding asthma before health education
The
Table 2 shows how much asthma patients knew about their condition before receiving health education. All survey takers were aware that asthma is an airway disease, but most had only a superficial understanding of how it manifests. Most responders had trouble differentiating between the many factors that worsened asthma-related respiratory issues. Air pollution (named by 80% of participants) and the common cold were both named by 100% of participants. In addition, everyone present was aware that smoking is a major contributor to the onset of asthma. Participants also demonstrated a lack of familiarity with asthma care recommendations and available treatments, according to the poll results.
Table 3 shows asthmatics' 2-week health education program results. A total of 91.2% who guessed correctly said asthma changes the lung and breathing tube. Wheezing (80%), time-varying (90.4%), and nighttime/morning (78.8%) asthma symptoms were correctly identified. Allergies (80%), air pollution (100%), colds (100%), exercise (100%), particular foods (68.4%), and incorrect notions such "living with asthma patients causes asthma" (100%). Patients received asthma management tools. Health education greatly increased patients' health knowledge.
Table 4 demonstrates asthmatic patients' asthma awareness after 12 weeks health education. Most patients forget asthma information after a while. 80.0% of respondents correctly recognized asthma etiology but misidentified asthma pathophysiology. Most respondents identified asthma symptoms and triggers.
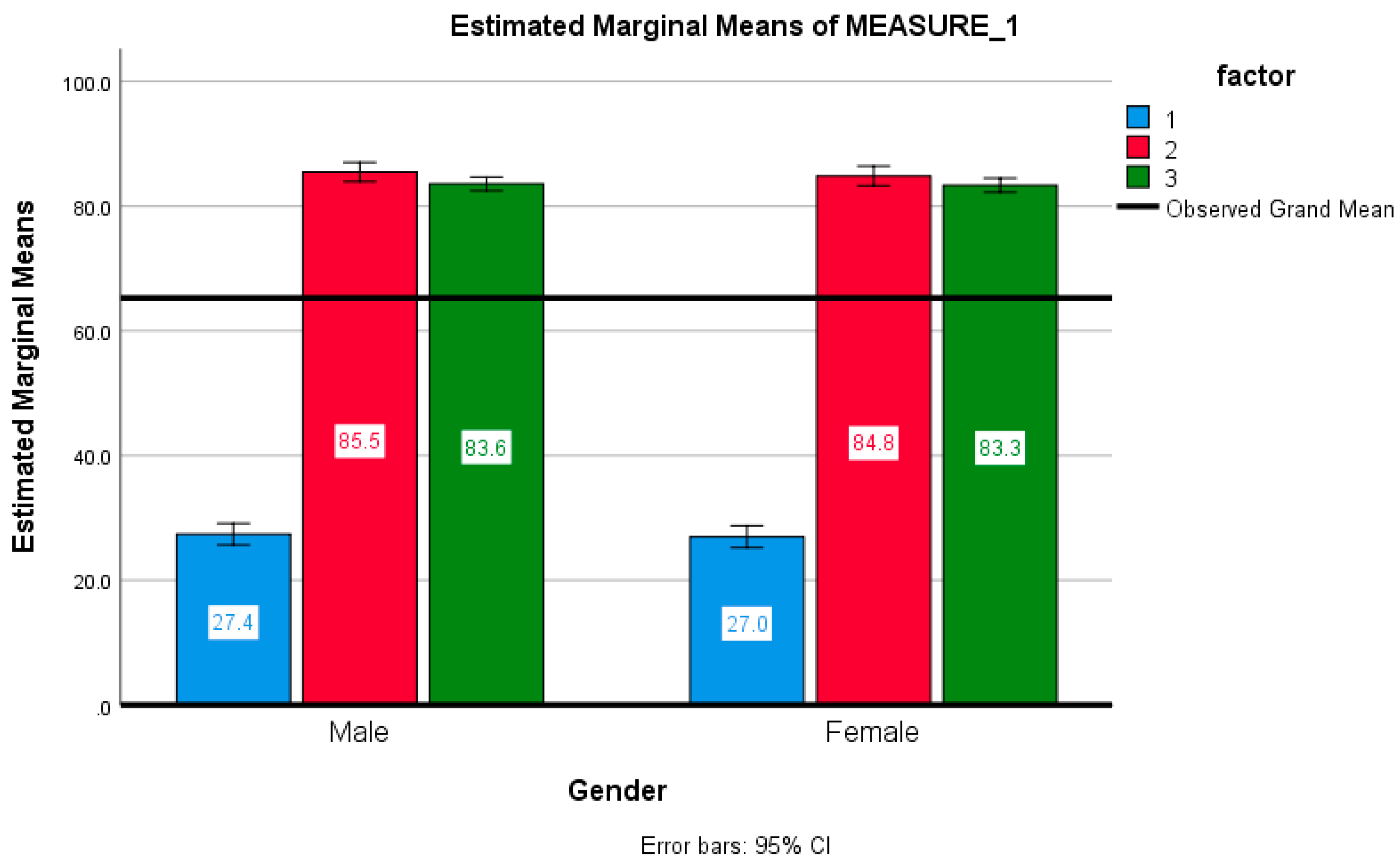
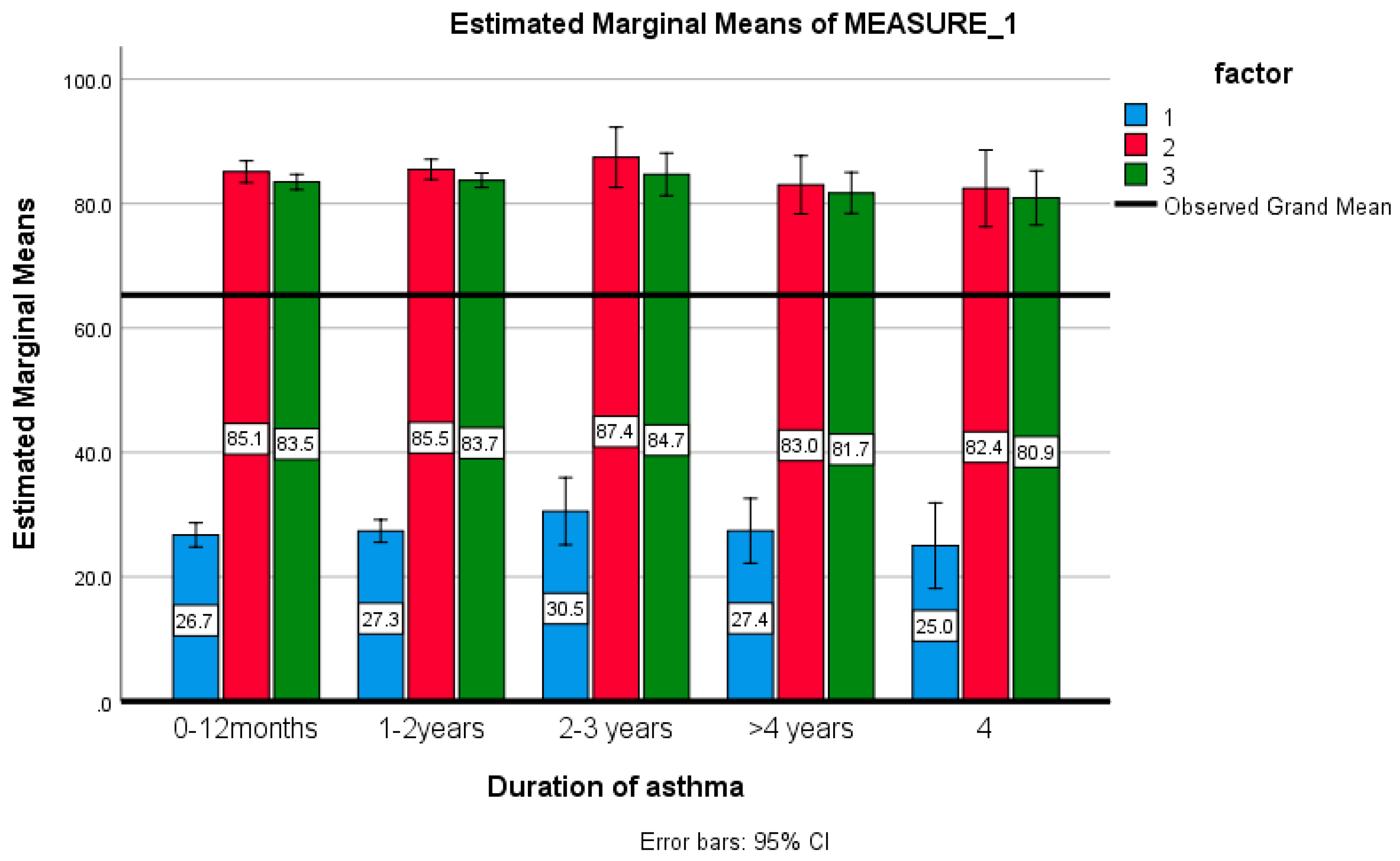
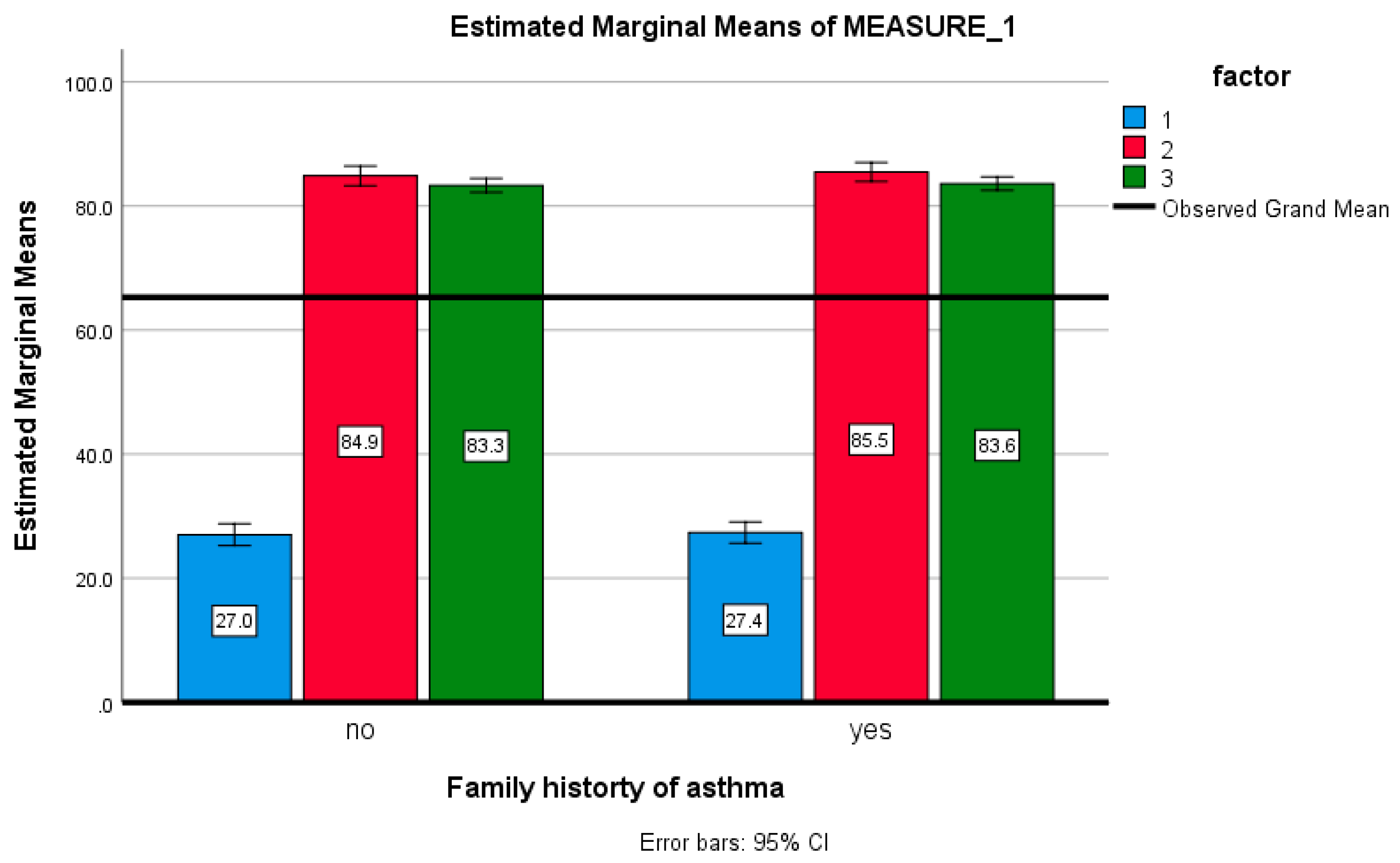
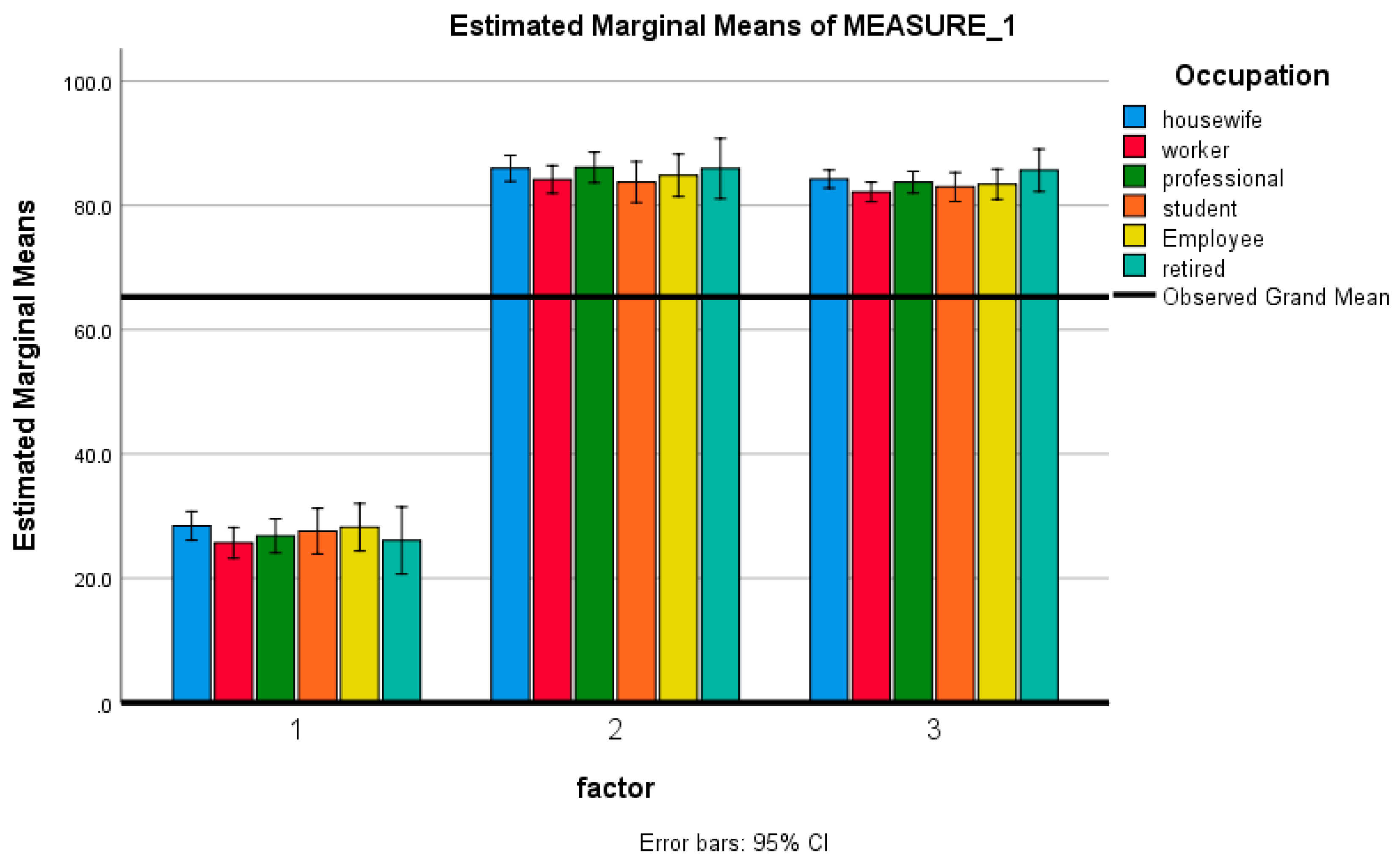
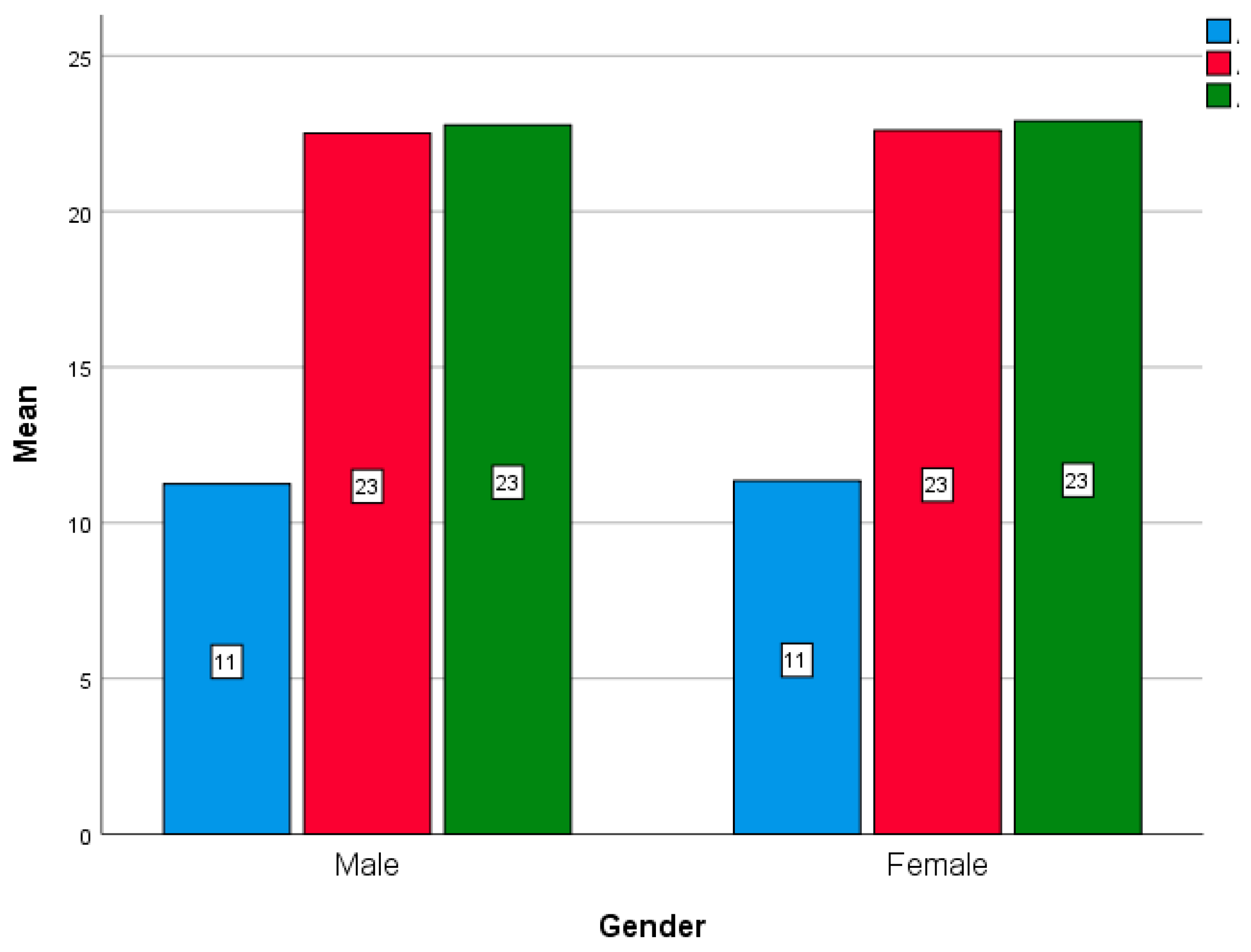
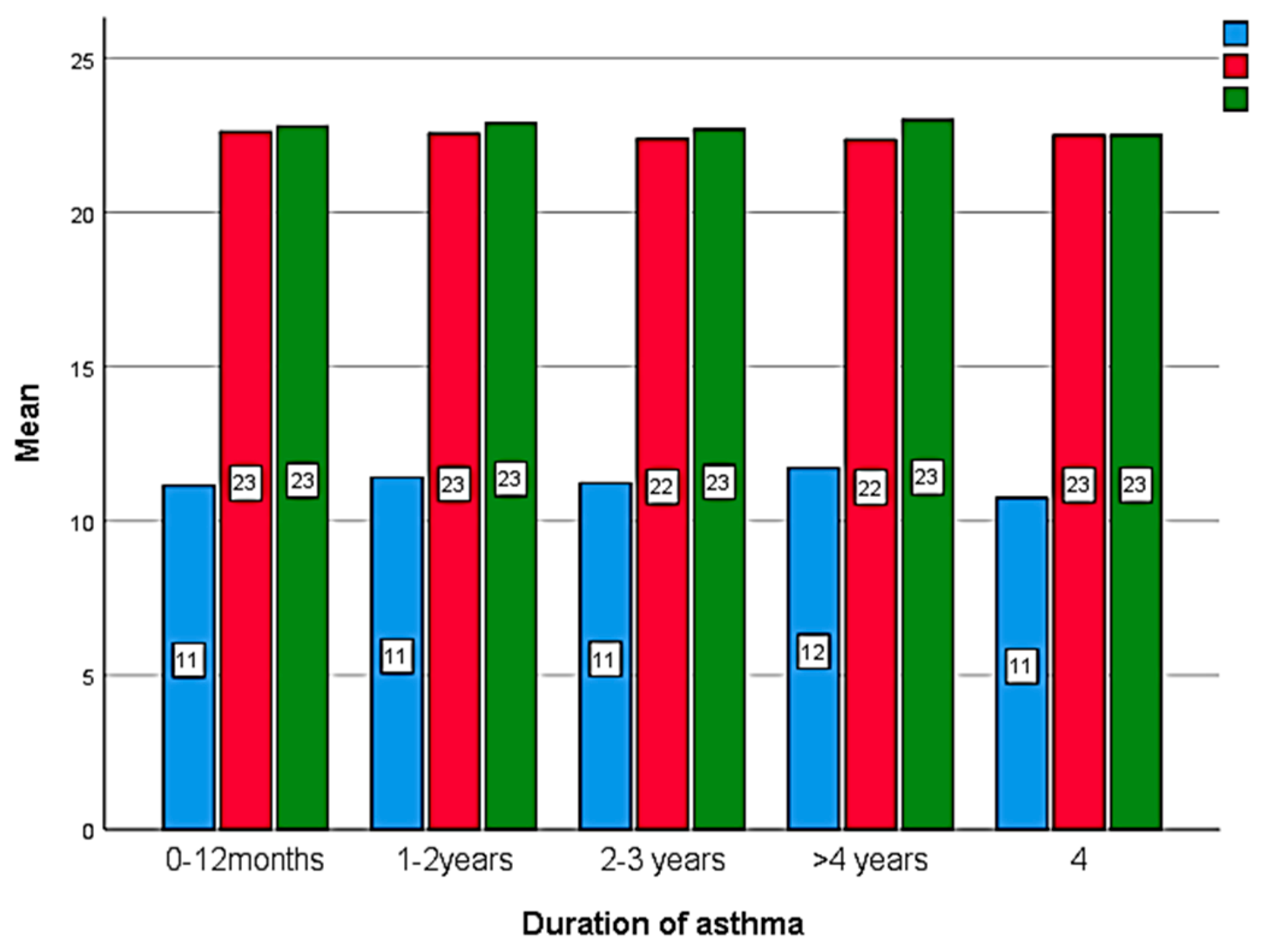
Table 5 shows the comparison of the knowledge score before and after health education intervention. After 2 weeks of health education intervention, respondent have a higher knowledge score compared to pre-education and after 12 weeks of education with a significant difference (
P <0.001). There were no significant association of the knowledge score with gender, education, family history and occupation (
P> 0.005) (
Figure 1,
Figure 2 and
Figure 3).
3.3. Attitudes of the asthmatic patients before and after health education intervention
Table 6,
Table 7 and
Table 8 shows the comparison of the attitude’s responses with score (
Table 9) before health education, 2 weeks after and 12 weeks after health education. There is a significant difference found between the time interval with a better positive attitude after health education (P < 0.005). Although there is no significant score difference observed between gender (
Figure 5), duration of asthma (
Figure 6).
3.4. Practice of the asthmatic patients before and after health education
Table 10 shows the practice of the asthmatic patients regarding asthma before, after 2 weeks and 12 weeks of health education intervention [
8]. After 2 weeks, visiting of physician was practiced by 92%, while after 12 weeks its reduced to 81.9%. Nasal spray used also increased after HEI at 2 weeks and 12 weeks. Before HEI, 99.6% of the patients were used to buy over the counter drug without physician advice, which completely zeroed after education. Although a total of 36.1% again buying over the counter drug without physician advice after 12 weeks. After HEI, almost 88.0% of patients avoid house dust and smoke and also follow doctor advice strictly. Physical exercise also increases after HEI, which help them in their daily life activities. A total of 87.6% patients didn’t forget to take medication in last two weeks after 2 weeks of HEI, 37.2% reported that they forgot after 12 weeks. A total 74.8 -80.8% patients reported that they are changing medication if asthma worse with consulting proper channel. After HEI, patients were more concern to avoid smoke dust by removing them by fan or more cautiously use deodorant to avoid sudden asthma attack.
4. Discussion
The Global Initiative for Asthma [
9] and the asthma guidelines for prevention and treatment written by an expert panel from the National Heart, Lung, and Blood Institute emphasize the importance of promoting a standardized classification of asthma treatment [
15]. In this analysis of the KAP of Erbil patients with asthma, a wide gap was observed between recommended and actual practices, and their overall asthma-related knowledge was insufficient at baseline. Furthermore, asthma-related knowledge was associated with deficiencies in the care process. After successful implementation health education program, overall KAP is improved. The importance of asthmatic habits in controlling the disease cannot be overstated [
16]. This research was carried out in Erbil with the purpose of determining the levels of knowledge, attitudes, and practices held by adult patients who suffer from asthma. The questionnaire was based on knowledge of the fundamental pathophysiology of the disease, symptoms, triggering factors, precipitating causes, medication, and management of asthma, all of which are crucial to know by individuals who have chronic asthma. In addition to that, it evaluated the behaviors that patients need to follow in order to reduce the likelihood of future asthma exacerbations.
Our study found that all participants knew asthma is an airway illness. However, most didn't know asthma's causes, symptoms, or triggers. Asthma guidelines and treatment alternatives were unfamiliar to survey respondents. This study found that prior asthma education does not improve asthma control or quality of life. This matches prior studies [
17]. Comparing asthma information gained from personal experience to that gained through active education. Meyer et al. observed that personal asthma knowledge differed more than active education [
18]. However, knowledge still reduces asthma morbidity and mortality. Other studies also found a correlation between asthma knowledge and asthma severity [
19].
Asthma attitudes and beliefs that promote excellent health and medication compliance for effective disease management were also considered [
20]. This ensured optimum illness management. Most asthmatics know little about the disease and its treatments. Higher patient education may have affected their knowledge. After health education, the time intervals with a more positive attitude differed statistically (P < 0.005). Due to the majority of participants not having completed secondary education, it is suggested. However, college-educated people understood their ailment and treatment better. Our findings reflect prior data suggesting better education is strongly connected with asthma knowledge [
21].
Asthma control improved quality of life. Effective asthma management may benefit from non-educational asthma control methods. Health education raised patients' knowledge significantly. After two weeks of health education intervention, respondents had a significantly higher knowledge score than before and after 12 weeks (P < 0.001). After two weeks of health education, 91.2% could identify asthma pathogenesis. 100% of participants also knew the causes that worsen asthmatic episodes. Health care providers should empower asthmatics to manage their own health and have confidence in doing so. Patients should help establish a self-management approach [
22]. Health education teaches people how to handle symptoms and well-being. Patients' asthma and treatment knowledge will rise. If health practitioners consider patients' beliefs and goals to meet their needs, such programs will gain credibility. College-educated patients had this compared to non-graduated patients [
23]. A recent comprehensive study found that patients still trust doctors more than social media and the internet for health information [
24].
Many patients had misperceptions about asthma and related illnesses before receiving health education. This is another impediment to proper information, along with illiteracy and ignorance. Sodhi and colleagues researched Bronchial asthma patients share knowledge, attitudes, and behaviors. (In terms of asthma beliefs, 64% of patients were uninformed of the etiology of their disease; 16.3% thought it was caused by allergens; 8.7% thought it was genetics; and 3.6% thought it was a curse from God) . Kumar et al. found that several patient characteristics affected asthma knowledge [
25]. Despite prior studies, there was a significant age-related difference in patient knowledge. We postulate that younger age groups have less life experience with asthma, while elderly patients (those older than 60 years) have less asthma knowledge due to forgetfulness and memory impairment [
26]. Inhaled medications are misunderstood. Most asthmatics use inhalers, but some say pills work better. This misperception may make asthma medication compliance harder. It is also associated to the shift away from inhaler medicines to other treatments [
27].
The international asthma guidelines recommend collaboration between asthmatics and their health care providers [
28]. This method should give patients the knowledge, confidence, and abilities to manage their asthma. Self-management has been shown to lower asthma morbidity. However, misperceptions regarding asthma and inhaled medicine may lead to poor self-control [
29]. These guidelines also prescribe regular preventive inhaled medicine and bronchodilator therapy to prevent and treat chronic asthma [
30]. In impoverished countries, inhaled corticosteroids reduce hospital admissions and ER visits by up to 80% [
31,
32]. Some research from other territories supports our findings on adult asthma practice and this session's variables. Higher-educated patients can read asthma instructions and execute better self-care. Higher-income patients have easier access to health services. Experienced asthmatics can also better manage their symptoms. It also reduces asthma exacerbations, which is consistent with earlier study [
33]. Patients who receive asthma education from their healthcare providers and community pharmacists have better asthma management [
34]. Patients who can self-manage and have a high quality of life have fewer asthma attacks and can manage their disease more efficiently and easily than those who cannot [
35].
Despite recognizing symptoms and trigger points, some individuals lose asthma expertise after twelve weeks. A recent study suggests that patients should continue health education for long-term asthma control [
36]. Education boosts patients' and providers' confidence and competence, and it improves practice [
37]. Our study clearly links patient education to results. Asthma management may benefit from brochures, books, and self-practice cards [34, 35].
5. Conclusions
Health education programs led to considerable improvements in asthmatic patients' knowledge, attitudes, and practices regarding their condition. After receiving health education for a period of two weeks, the majority of the participants answered correctly regarding asthma, its causes, and the elements that trigger asthma attacks. There is a statistically significant difference (P < 0.001) between the respondents' knowledge scores before and after receiving health education for a period of 12 weeks, but after receiving health education for only two weeks, respondents' knowledge scores are significantly higher, and their positive attitudes are significantly improved.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, All the supplementary file were submitted to the MDPI. English and Kurdish questionnaire, ethics permission was submitted to the journal.
Author Contributions
Conceptualization, Syed Azhar Syed Sulaiman and Amer Hayat Khan; Data curation, Karwan Maulood; Formal analysis, Karwan Maulood and Mohammad Khan; Investigation, Karwan Maulood; Methodology, Karwan Maulood, Mohammad Khan, Syed Azhar Syed Sulaiman and Amer Hayat Khan; Software, Mohammad Khan; Supervision, Syed Azhar Syed Sulaiman and Amer Hayat Khan; Validation, Mohammad Khan and Syed Azhar Syed Sulaiman; Visualization, Mohammad Khan; Writing – original draft, Karwan Maulood and Mohammad Khan; Writing – review & editing, Syed Azhar Syed Sulaiman and Amer Hayat Khan.
Funding
This research received no external funding.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki and approved by the the Ethics Committee for Research Involving Human Subjects at Universiti Sains Malaysia (USM), the Ministry of Health, Iraq's Ethics Committee for Research involving Human Subjects, and the administration of Rizgary Teaching Hospital and Hawler Medical hospital under Hawler Medical University were also granted permission to conduct the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
All data were available upon request to the corresponding authors.
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflict of interest.
References
- San Ko, F.W.; Fleming, L. Advancement of asthma management in the past decade. Lancet Respir. Med. 2023, 11, 15–17. [Google Scholar]
- Salmanpour, F.; Kian, N.; Samieefar, N.; Khazeei Tabari, M.A.; Rezaei, N. Asthma and vitamin d deficiency: Occurrence, immune mechanisms, and new perspectives. J. Immunol. Res. 2022, 2022. [Google Scholar] [CrossRef] [PubMed]
- Buckey, T.M.; Morales, K.H.; Apter, A.J. Understanding Autonomy in Patients with Moderate to Severe Asthma. J. Clin. Immunol. 2022, 10, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Gagné, M.; Cheung, J.L.S.; Kouri, A.; FitzGerald, J.M.; O’Byrne, P.M.; Boulet, L.P.; Gupta, S. A patient decision aid for mild asthma: Navigating a new asthma treatment paradigm. Res. Med. 2022, 201, 106568. [Google Scholar] [CrossRef] [PubMed]
- Eassey, D.; Reddel, H.K.; Ryan, K.; Smith, L. The impact of severe asthma on patients’ autonomy: A qualitative study. Health Expect. 2019, 22, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Gualano, M.R.; Bert, F.; Passi, S.; Stillo, M.; Brescia, V.; Scaioli, G.; Siliquini, R. Could share decision making affect staying in hospital? A cross-sectional pilot studies. BMC Health Serv. Res. 2019, 19, 1–8. [Google Scholar] [CrossRef]
- Singh, H.K.; Kennedy, G.A.; Stupans, I. Pharmacist health coaching in Australian community pharmacies: What do pharmacy professionals think? Health Soc Care Community 2020, 28, 1190–1198. [Google Scholar] [CrossRef]
- Mitchell, I.; Govias, G.; Mitchell, I.; Govias, G. Teaching the Person with Asthma. Asthma Education: Principles and Practice for the Asthma Educator 2021, 515–568. [Google Scholar]
- Gardner, E.A.; Kaplan, B.M.; Collins, P.; Zahran, H. Breathe Well, Live Well: Implementing an Adult Asthma Self-Management Education Program. Health Promot. Pract. 2022, 22, 702–713. [Google Scholar] [CrossRef]
- Gibson, P.G.; FS Ram, and H. Powell, Asthma education. Res. Med., 2003, 97, 1036–1044. [Google Scholar] [CrossRef]
- Bateman, E.D.; et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J., 2008, 31, 143–178. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Pinnock, H.; Dowrick, A.; Steed, L. Generational perspective on asthma self-management in the Bangladeshi and Pakistani community in the United Kingdom: A qualitative study. Health Expect. 2022, 25, 2534–2547. [Google Scholar] [CrossRef]
- Chamarro, A.; Penelo, E.; Fornieles, A.; Oberst, U.; Vallerand, R.J.; Fernández-Castro, J. Psychometric properties of the Spanish version of the Passion Scale. Psicothema 2015, 27, 402–409. [Google Scholar] [PubMed]
- Gare, M.B.; Godana, G.H.; Zewdu, B. Knowledge, attitude, and practice assessment of adult asthmatic patients towards pharmacotherapy of asthma at Jimma university specialized hospital. EC Pul. Res. Med. 2020, 9, 1–10. [Google Scholar]
- Brown, A.G.; Hyams, T.; Brown, A.N.; Nicastro, H.; Pratt, C.A. News from NHLBI: nutrition research at the National Heart, Lung, and Blood Institute and future opportunities. J. Nutr. 2021, 151, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.H.; Huang, J.L.; Yeh, K.W.; Tsai, Y.F. The stress of caring for children with asthma: a qualitative study of primary caregivers. J. Nur. Res. 2015, 23, 298–307. [Google Scholar] [CrossRef]
- Rhee, H.; Love, T.; Mammen, J. Comparing asthma control questionnaire (ACQ) and national asthma education and prevention program (NAEPP) asthma control criteria. Ann. Allergy Asthma Immunol. 2019, 122, 58–64. [Google Scholar] [CrossRef]
- Meyers, D.A.; Bleecker, E.R.; Holloway, J.W.; Holgate, S.T. Asthma genetics and personalised medicine. Lancet Respir. Med., 2014, 2, 405–415. [Google Scholar] [CrossRef]
- Kattan, M. Inner City Asthma: Strategies to Reduce Mortality and Morbidity. Pediatr Allergy Immunol. 2015, 303. [Google Scholar]
- Kosse, R.C.; Koster, E.S.; Kaptein, A.A.; de Vries, T.W.; Bouvy, M.L. Asthma control and quality of life in adolescents: the role of illness perceptions, medication beliefs, and adherence. J. Asthma 2020, 57, 1145–1154. [Google Scholar] [CrossRef]
- Drummond, D.; Monnier, D.; Tesnière, A.; Hadchouel, A. A systematic review of serious games in asthma education. Pediatr Allergy Immunol. 2017, 28, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Holley, S.; Walker, D.; Knibb, R.; Latter, S.; Liossi, C.; Mitchell, F.; Roberts, G. Barriers and facilitators to self-management of asthma in adolescents: an interview study to inform development of a novel intervention. Clin. Exp. Allergy 2018, 48, 944–956. [Google Scholar] [CrossRef] [PubMed]
- Dabholkar, Y.G.; Wadhwa, A.; Deshmukh, A. A study of knowledge, attitude and practices about otitis media in parents in Navi-Mumbai. J. Otol. 2021, 16, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Credibility of health information and digital media: New perspectives and implications for youth, 2008, (pp. 123-154). MacArthur Foundation Digital Media and Learning Initiative.
- Kumar, N.; Kamdar, S.; Karnani, R.K. Assessment of knowledge regarding asthma & breathing exercises among bronchial asthma patients. Int. J. Med. Educ. 2018, 5, 269–274. [Google Scholar]
- Hanania, N.A.; King, M.J.; Braman, S.S.; Saltoun, C.; Wise, R.A.; Enright, P.; Ledford, D.K. Asthma in the elderly: current understanding and future research needs—a report of a National Institute on Aging (NIA) workshop. J. Allergy Clin. Immunol. 2011, 128, S4–S24. [Google Scholar] [CrossRef]
- George, M. Adherence in asthma and COPD: new strategies for an old problem. Respir. Care 2018, 63, 818–831. [Google Scholar] [CrossRef]
- Sony, A.E.; Mohammad, Y. Asthma in the Eastern Mediterranean Region. Int J Tuberc Lung Dis 2022, 26, 48–55. [Google Scholar]
- Zainol, A.H.; Ismail, A.F.; Taib, F.; Norsa’adah, B. Treatment adherence, knowledge, attitude and quality of life of adolescents with asthma in northeastern Malaysia. Bangladesh J. Medical Sci. 2020, 19, 73–82. [Google Scholar] [CrossRef]
- Levy, M.L.; Bacharier, L.B.; Bateman, E.; Boulet, L.P.; Brightling, C.; Buhl, R.; Reddel, H.K. Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update. NPJ Prim. Care Respir. Med. 2023, 33, 7. [Google Scholar] [CrossRef]
- Kligler, S.K.; Vargas-Torres, C.; Abbott, E.E.; Lin, M. Inhaled Corticosteroids Rarely Prescribed At Emergency Department Discharge In Spite Of Low Rates Of Follow-Up Care. J. Emerg. Med. 2023.
- Kearns, N.; Maijers, I.; Harper, J.; Beasley, R.; Weatherall, M. Inhaled corticosteroids in acute asthma: a systemic review and meta-analysis. J Allergy Clin Immunol Pract. 2020, 8, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Aziz, D.A.; Abbas, A.; Viquar, W.; Hussain, A.M. Association of vitamin D levels and asthma exacerbations in children and adolescents: Experience from a tertiary care center. Monaldi Arch Chest Dis 2023, 93. [Google Scholar] [CrossRef] [PubMed]
- Makhinova, T.; Barner, J.C.; Brown, C.M.; Richards, K.M.; Rascati, K.L.; Rush, S.; Nag, A. Examination of barriers to medication adherence, asthma management, and control among community pharmacy patients with asthma. J. Pharm. Pract. 2021, 34, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Roberts, G.; Vazquez-Ortiz, M.; Knibb, R.; Khaleva, E.; Alviani, C.; Angier, E.; Timmermans, F. EAACI Guidelines on the effective transition of adolescents and young adults with allergy and asthma. Allergy 2020, 75, 2734–2752. [Google Scholar] [CrossRef]
- Bridgeman, M.B.; Wilken, L.A. Essential role of pharmacists in asthma care and management. J. Pharm. Pract. 2021, 34, 149–162. [Google Scholar] [CrossRef]
- McCabe, E.M.; McDonald, C.; Connolly, C.; Lipman, T.H. A review of school nurses’ self-efficacy in asthma care. J. Sch. Nurs. 2019, 35, 15–26. [Google Scholar] [CrossRef]
Figure 1.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education between the gender (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 1.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education between the gender (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 2.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education between the duration of asthma (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 2.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education between the duration of asthma (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 3.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education with family history (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 3.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education with family history (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 4.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education with occupation (1 : baseline; 2: after 2 weeks; 3 : after 12 weeks).
Figure 4.
Comparison of the knowledge score before, after 2 weeks and 12 weeks of health education with occupation (1 : baseline; 2: after 2 weeks; 3 : after 12 weeks).
Figure 5.
Comparison of the attitudes score before, after 2 weeks and 12 weeks of health education between the genders (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 5.
Comparison of the attitudes score before, after 2 weeks and 12 weeks of health education between the genders (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 6.
Comparison of the attitudes score before, after 2 weeks and 12 weeks of health education between the duration of asthma (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Figure 6.
Comparison of the attitudes score before, after 2 weeks and 12 weeks of health education between the duration of asthma (Blue : baseline; Red: after 2 weeks; Green : after 12 weeks).
Table 1.
Characteristics of the respondents.
Table 1.
Characteristics of the respondents.
| Variable |
Frequency, N (%) |
| Age* |
37.52±15.16 |
| Gender |
|
| Male |
129(51.6) |
| Female |
121(48.4) |
| Marital status |
|
| Married |
181 (72.4) |
| Single |
69 (27.6) |
| Educational qualification |
|
| Illiterate |
104(41.6) |
| Primary/secondary |
83 (33.2) |
| College /University |
63 (25.2) |
| Occupation |
|
| Housewife |
71 (28.4) |
| Worker |
62 (24.8) |
| Professionals |
50 (20.0) |
| Students |
28 (11.2) |
| Employee |
26 (10.4) |
| Retried |
13 (5.2) |
| Smoking habit |
|
| Yes |
67 (26.9) |
| No |
182 (73.1) |
| Duration of asthma |
|
| 0-12 months |
99 (39.8) |
| 1-2 years |
115 (46.2) |
| 2-3 years |
13 (5.2) |
| >4 years |
22 (8.8 |
| Family history |
|
| Yes |
129 (48.7) |
| No |
121 (45.7) |
| *Mean [6] |
Table 2.
Knowledge of asthmatic patients regarding asthma before health education.
Table 2.
Knowledge of asthmatic patients regarding asthma before health education.
| Item variable |
Agree |
Disagree |
No opinion |
| Asthma is a chronic inflammatory disorder of airways. |
100(100) |
0(0.0) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to mucus (sputum) collection |
0(0.0) |
101(40.4) |
149 (59.6) |
| In asthma breathing tubes in lungs become narrow due to tightening of muscles around them |
176(70.4) |
74(29.6) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to swelling of their walls |
49(19.6) |
82(32.8) |
119(47.6) |
| Symptom of asthma are breathing difficulty with wheezing sound |
0(0.0) |
127 (50.8) |
123(49.2) |
| Asthma symptoms vary time to time, less at some times and more at other times |
45(18.0) |
151(60.4) |
54(21.6) |
| Asthma symptoms more likely to occur at night or early morning |
73(29.2) |
52(20.8) |
125(50.0) |
| Asthma symptoms can be caused by: |
- a)
Allergy |
76(30.4) |
174(69.6) |
0(0.0) |
- b)
Air pollution(dust) |
200(80.0) |
26(10.4) |
24(9.6) |
- c)
Living with asthma patient |
200(80.0) |
0(0.0) |
50(20.0) |
- d)
Common cold |
250(100.0) |
0(0.0) |
0(0.0) |
- e)
Exercise |
25(10.0) |
101(40.4) |
124(49.6) |
- f)
Certain food |
0(0.0) |
132(52.8) |
118(47.2) |
- g)
Without obvious reason |
105(42.0) |
0(0.0) |
145(58.0) |
| Smoking make asthma worse |
250(100.0) |
0(0.0) |
0(0.0) |
| Asthma medicine can be given a tablet/syrup/inhalers |
7(2.8) |
118(47.2) |
125(50.0) |
| The best way to take asthma medicine is inhalation |
32(12.8) |
50(20.0) |
168(67.2) |
| Asthma medicine are usually of two types- one to give immediate relief and other to prevent symptoms |
7(2.8) |
0(0.0) |
243(97.2) |
| Most effective drugs for controlling asthma are called steroids |
102(40.8) |
0(0.0) |
148(59.2) |
| Inhalers are free from significant side effects |
169(67.6) |
51(20.40 |
30(2.0) |
| Asthma medicine has to be taken till symptom persist then can be stopped |
0(0.0) |
107(42.8) |
143(57.2) |
| Asthma medicine has to be taken even after symptoms are no longer there, till your doctor advise you to stop |
50(20.0) |
50(20.0) |
150(60.0) |
Table 3.
Knowledge of asthmatic patients regarding asthma after 2 weeks of health education.
Table 3.
Knowledge of asthmatic patients regarding asthma after 2 weeks of health education.
| Item variable |
Agree |
Disagree |
No
opinion |
| Asthma is a chronic inflammatory disorder of airways. |
250(100.0) |
0(0.0) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to mucus (sputum) collection |
0(0.0) |
228(91.2) |
22(8.8) |
| In asthma breathing tubes in lungs become narrow due to tightening of muscles around them |
0(0.0) |
198(79.2) |
52(20.8) |
| In asthma breathing tubes in lungs become narrow due to swelling of their walls |
228(91.2) |
0(0.0) |
22(8.8) |
| Symptom of asthma are breathing difficulty with wheezing sound |
200(80.0) |
50(20.0) |
0(0.0) |
| Asthma symptoms vary time to time, less at some times and more at other times |
226(90.4) |
24(9.6) |
0(0.0) |
| Asthma symptoms more likely to occur at night or early morning |
197(78.8) |
53(21.2) |
0(0.0) |
| Asthma symptoms can be caused by: |
- a)
Allergy |
200(80.0) |
50(20.0) |
0(0.0) |
- b)
Air pollution(dust) |
250(100) |
0(0.0) |
0(0.0) |
- c)
Living with asthma patient |
0(0.0) |
250(100.0) |
0(0.0) |
- d)
Common cold |
250(100.0) |
0(0.0) |
0(0.0) |
- e)
Exercise |
250(100.0) |
0(0.0) |
0(0.0) |
- f)
Certain food |
171(68.4) |
79(31.6) |
0(0.0) |
- g)
Without obvious reason |
0(0.0) |
250(100.0) |
0(0.0) |
| Smoking make asthma worse |
250(100.0) |
0(0.0) |
0(0.0) |
| Asthma medicine can be given a tablet/syrup/inhalers |
250(100.0) |
0(0.0) |
0(0.0) |
| The best way to take asthma medicine is inhalation |
248(99.2) |
2(0.8) |
0(0.0) |
| Asthma medicine are usually of two types- one to give immediate relief and other to prevent symptoms |
249(99.6) |
0(0.0) |
1(0.4) |
| Most effective drugs for controlling asthma are called steroids |
177(70.8) |
73(29.2) |
0(0.0) |
| Inhalers are free from significant side effects |
0(0.0) |
199(79.6) |
51(20.4) |
| Asthma medicine has to be taken till symptom persist then can be stopped |
0(0.0) |
130(52.0) |
120(48.0) |
| Asthma medicine has to be taken even after symptoms are no longer there, till your doctor advise you to stop |
224(89.6) |
26(10.4) |
0(0.0) |
Table 4.
Knowledge of asthmatic patients regarding asthma after 12 weeks health education.
Table 4.
Knowledge of asthmatic patients regarding asthma after 12 weeks health education.
| Item variable |
Agree |
Disagree |
No opinion |
| Asthma is a chronic inflammatory disorder of airways. |
250(100.0) |
0(0.0) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to mucus (sputum) collection |
203(81.2) |
47(18.8) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to tightening of muscles around them |
101(40.4) |
149(59.6) |
0(0.0) |
| In asthma breathing tubes in lungs become narrow due to swelling of their walls |
218(87.2) |
32(12.8) |
0(0.0) |
| Symptom of asthma are breathing difficulty with wheezing sound |
200(80.0) |
24(9.6) |
26(10.4) |
| Asthma symptoms vary time to time, less at some times and more at other times |
156(62.4) |
46(18.4) |
48(19.2) |
| Asthma symptoms more likely to occur at night or early morning |
175(70.0) |
0(0.0) |
75(30.0) |
| Asthma symptoms can be caused by: |
- a)
Allergy |
202(80.4) |
25(10.0) |
23(9.2) |
- b)
Air pollution(dust) |
250(100.0) |
0(0.0) |
0(0.0) |
- c)
Living with asthma patient |
25(10.0) |
200(80.0) |
25(10.0) |
- d)
Common cold |
250(100) |
0(0.0) |
0(0.0) |
- e)
Exercise |
175(70.0) |
49(19.6) |
26(10.4) |
- f)
Certain food |
199(79.6) |
0(0.0) |
51(20.4) |
- g)
Without obvious reason |
106(42.4) |
119(47.6) |
25(10.0) |
| Smoking make asthma worse |
243(97.2) |
5(2.0) |
2(0.8) |
| Asthma medicine can be given a tablet/syrup/inhalers |
245(98.0) |
1(0.4) |
4(1.6) |
| The best way to take asthma medicine is inhalation |
200(80.0) |
43(17.2) |
7(2.8) |
| Asthma medicine are usually of two types- one to give immediate relief and other to prevent symptoms |
184(73.6) |
0(0.0) |
66(26.4) |
| Most effective drugs for controlling asthma are called steroids |
207(82.4) |
43(17.2) |
0(0.0) |
| Inhalers are free from significant side effects |
0(0.0) |
177(70.8) |
73(29.2) |
| Asthma medicine has to be taken till symptom persist then can be stopped |
142(56.8) |
108(43.2) |
0(0.0) |
| Asthma medicine has to be taken even after symptoms are no longer there, till your doctor advise you to stop |
175(70.0) |
75(30.0) |
0(0.0) |
Table 5.
Comparison of the knowledge score before, after 2weeks and 12 weeks of the health education.
Table 5.
Comparison of the knowledge score before, after 2weeks and 12 weeks of the health education.
| Variable |
Mean |
95% CI |
Χ2[df] |
F[df] |
P value |
| lower |
upper |
| Pre score |
27.19±9.83 |
25.96 |
28.41 |
175(1,63) |
9283.6(1,249) |
<0.001 |
| After 2 weeks |
85.18±8.8 |
84.08 |
86.28 |
| After 12 weeks |
83.4±6.25 |
82.68 |
84.24 |
| Chi-square test and RMANOVA test were carried out. |
Table 6.
Attitudes of the asthmatic patients before health education intervention.
Table 6.
Attitudes of the asthmatic patients before health education intervention.
| Variable |
Strongly Agree |
Agree |
Neutral |
Disagree |
Strongly Disagree |
| If one person has asthma, then all of the families are likely to have asthma as well |
43(17.2) |
139(55.6) |
38(27.2) |
0(0.0) |
0(0.0) |
| Asthma is contagious |
139(55.6) |
141(44.4) |
0(0.0) |
0(0.0) |
0(0.0) |
| People with asthma cannot do as much physical exercise as other people |
0(0.0) |
50(20.0) |
200(80.0) |
0(0.0) |
0(0.0) |
| Asthma can be cured |
68(27.2) |
68(27.2) |
71(28.4) |
43(17.2) |
0(0.0) |
| Asthma can’t be controlled |
43(17.2) |
136(54.4) |
71(28.4) |
0(0.0) |
0(0.0) |
Table 7.
Attitudes of the asthmatic patients after 2 weeks of health education intervention.
Table 7.
Attitudes of the asthmatic patients after 2 weeks of health education intervention.
| Variable |
Strongly Agree |
Agree |
Neutral |
Disagree |
Strongly
Disagree |
If one person has
asthma, then all of the families are likely to have asthma as well |
0(0.0) |
0(0.0) |
0(0.0) |
182(72.8) |
68(27.2) |
| Asthma is contagious |
0(0.0) |
0(0.0) |
0(0.0)) |
182(72.8) |
68(27.2) |
| People with asthma cannot do as much physical exercise as other people |
0(0.0) |
0(0.0) |
0(0.0)) |
182(72.8) |
68(27.2) |
| Asthma can be cured |
71(28.4) |
179(71.6) |
0(0.0)) |
0(0.0) |
0(0.0) |
| Asthma can’t be controlled |
0(0.0)) |
0(0.0)) |
0(0.0)) |
43(17.2) |
207(82.8) |
Table 8.
Attitudes of the asthmatic patients after 12weeks of health education intervention.
Table 8.
Attitudes of the asthmatic patients after 12weeks of health education intervention.
| Variable |
Strongly Agree |
Agree |
Neutral |
Disagree |
Strongly Disagree |
| If one person has asthma, then all of the families are likely to have asthma as well |
0(0.0)) |
0(0.0)) |
0(0.0)) |
68(27.2) |
182(72.8) |
| Asthma is contagious |
0(0.0)) |
0(0.0)) |
0(0.0)) |
182(72.8) |
68(27.2) |
| People with asthma cannot do as much physical exercise as other people |
0(0.0)) |
0(0.0)) |
0(0.0)) |
182(72.8) |
68(27.2) |
| Asthma can be cured |
139(55.6) |
111(41.9) |
0(0.0)) |
0(0.0)) |
0(0.0)) |
| Asthma can’t be controlled |
0(0.0)) |
0(0.0)) |
|
68(27.2) |
182(72.8) |
Table 9.
Comparison of the attitudes score before, after 2weeks and 12 weeks of the health education.
Table 9.
Comparison of the attitudes score before, after 2weeks and 12 weeks of the health education.
| Variable |
Mean |
95% CI |
Χ2[df] |
F[df] |
P value |
| lower |
upper |
| Pre score |
11.3±1.56 |
11.10 |
11.49 |
250.0(1,3) |
14471.7(2,248) |
<0.001 |
| After 2 weeks |
22.6±0.51 |
22.49 |
22.62 |
| After 12 weeks |
22.4±0.84 |
22.73 |
22.96 |
| Chi-square test and RMANOVA test were carried out. |
Table 10.
Practice of the asthmatic patients regarding asthma before and after health education.
Table 10.
Practice of the asthmatic patients regarding asthma before and after health education.
| Variable |
|
Pre |
After 2weeks |
After 12 weeks |
| Do you usually visit physician when developing symptoms? |
Yes |
67(26.9) |
229(92.0) |
204(81.9) |
| No |
182(73.1) |
20(8.0) |
45(18.1) |
| Do you use nasal spray? |
Yes |
69(27.7) |
203(81.5) |
203(81.5) |
| No |
180(72.3) |
46(18.5) |
46(18.5) |
| Do you buy over the counter drugs without consulting a physician? |
Yes |
249(99.6) |
0(0.00) |
90(36.1) |
| No |
1(0.4) |
250(100) |
160(63.9) |
| Do you avoid house dust and smoke? |
Yes |
109(43.6) |
220(88.0) |
219(87.6) |
| No |
141(56.4) |
30(12.0) |
31(12.4) |
| Do you strictly follow the doctors’ instruction? |
Yes |
78(31.2) |
202(80.8) |
190(76.0) |
| No |
172(68.8) |
48(19.2) |
60(24.0) |
| Have you done physical work or exercise in the last two weeks? |
Yes |
110(44.0) |
141(56.4) |
156(62.4) |
| No |
140(56.0) |
109(43.6) |
94(37.6) |
| Many people tend to forget taking medication. Have you forgotten in the last two weeks? |
Yes |
158(63.2) |
31(12.4) |
93(37.2) |
| No |
92(36.8) |
219(87.6) |
157(62.8) |
| If the asthma symptoms getting worse, I change my medication |
Yes |
125(50.0) |
63(25.2) |
48(19.2) |
| No |
125(50.0) |
187(74.8) |
202(80.8) |
| Do you use a fan to remove smoke and steam during cooking? |
Yes |
107(42.8) |
235(94.0) |
220(88.0) |
| No |
143(57.3) |
15(6) |
30(12.0) |
| Do you use deodorants or perfumes? |
Yes |
250(100.0) |
141(56.4) |
220(88.0) |
| No |
0.(00) |
109943.60 |
30(12.0) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).