1. Introduction
In dentistry, the introduction of technological advances such as digital flow and CAD/CAM (computer-aided design/computer-aided manufacturing) systems have enabled the fabrication of fixed dental prostheses using ceramic blocks (1). CAD/CAM blocks were introduced in the dental market in 1980 (2), while the production of restorations using zirconia blocks started in the late 1990s (3).
After the production and purification process, pure zirconia can be presented in 3 phases due to its chemical structure: monoclinic, tetragonal and cubic. The cubic phase crystallizes at a temperature of 2680°C and transforms at 2370°C into the tetragonal phase. At a temperature of 1170°C it transforms to monoclinic, with a volume increase of approximately 4-5 %. The addition of yttrium oxide leads to the formation of the metastable tetragonal phase and also of the cubic portions of the structure simultaneously, maintaining the stability of the crystalline form at room temperature (4)(5). Thus, the different generations from yttria-stabilized tetragonal zirconia oxide (Y-TZP) appear: The first generation, 3Y-TZP, contains 3% in moles of yttrium and 0.25% in weight of aluminum oxide, being a more robust material, with a bending strength of up to 1200 MPa. The second generation, 3Y-TZP 3% in moles of yttrium and 0.05 wt.% of aluminum oxide, was created with the purpose of improving translucency, reducing the alumina content of the first generation, however, it was not yet suitable for aesthetic areas, having to be layered with ceramic (6).
In 2015, a new ceramic system was introduced to the market: the tetragonal zirconia polycrystal stabilized with 5% moles of yttrium improving translucency, thus developing the third generation of 5Y-TZP. Its cubic phase reaches approximately 50% of the structure, the size and number of crystals, which are larger than 3Y-TZP, favor light transmission, reducing the refraction effect and giving better translucency with better optical properties, but with lower fracture toughness. In 2017, the fourth generation appears containing tetragonal zirconia polycrystals stabilized with 4 % moles of yttrium, increasing fracture toughness and fracture toughness than the third generation and with higher translucency than the first generation (7). In general, it has been stated that increasing the yttrium content increases the translucency of the material but decreases the flexural strength of zirconia (8) (9).
The improved mechanical properties, its biocompatibility and greater resistance to corrosion are advantages of zirconia. Its challenge is to present esthetics similar to natural dentition (10). Currently, monolithic translucent zirconia merges fracture resistance and color enhancement (11), evolving from an original white and opaque appearance to translucent, chromatic and polychromatic (multilayer) forms, which combine the favorable properties of different zirconia generations (3Y-TZP, 4Y-TZP and 5Y-TZP) (12).
Monolithic zirconia restorations became popular with the development of new CAD/CAM technologies (13) (14). It appears that monolithic translucent restorations improve survival compared to porcelain veneers with lower fracture resistance. It is a simplified procedure to make monolithic total coronal restoration, and it is the first choice compared to layered restorations avoiding the risk of chipping (15). In addition, the mechanical properties of monolithic zirconia materials are superior to those of all-ceramic restorative materials (4). In in vitro studies, monolithic zirconia single crowns showed a higher fracture resistance than layered zirconia crowns and could withstand the stresses that occur in the molar region during mastication (between 441 and 981 N) (16) (17).
Zirconia restorations can be milled in a fully sintered state (hard-state material) or pre-sintered (soft-state material). (18) In addition, high-speed sintering allows the production of zirconia restorations in a single appointment using a chairside workflow. These new rapid sintering protocols do not show a negative influence on flexural strength (19). After milling, zirconia prostheses should be sintered to achieve higher density and maximum strength (20) (21).
Monolithic Zirconia
The first multilayer monolithic zirconia system had the same yttrium content and cubic fraction in the different layers of the material, with the only difference in the pigment composition, which caused differences in shade, but not in translucency (22). Modi-fications in composition, structure and fabrication method have resulted in multilayered and precolored monolithic zirconia discs considered universal, with a balance between flexural strength and translucency, presenting a wider range of indications for single anterior and posterior crowns up to plural fixed prostheses. The most versatile combination was achieved using 4Y-TZP (fourth generation zirconia) with a more intense chroma in the base or cervical layer and 5Y-TZP (third generation zirconia) more translucent in the upper or incisal layer (23).
Monolithic zirconia dioxide can be presented with various types of translucency: low, medium, high, super and ultra, achieving different gradients of color and translucency desired for each clinical case. The grain size influences these translucent presentations, grains up to 80 nm result in a translucency similar to dental porcelains (24). Therefore, monolithic zirconia minimizes the risk of restoration failure due to chipping and incompatibility between the veneering ceramic and the zirconia ceramic (25).
1.1. Zirconia Cercon HT Dentsply-Sirona (CDS)
According to its manufacturer, because of its mechanical and esthetic properties, CDS can be applied in multi-unit crowns and bridges with a maximum of two pontics between stacked crowns in anterior and posterior regions. It is composed of yttrium-stabilized zirconia (Y-TPZ). It can be used as a fully anatomical restoration or as a framework to be veneered with feldspathic ceramics. Due to their composition (
Table 1) they have high strength, corrosion resistance, biological compatibility and translucency (26).
1.2. Zirconia Zolid Gen-X Amann Girrbach (ZGX)
It is a highly translucent and highly resistant multilayer monolithic zirconia oxide material, with a chromatic transition that improves its efficiency and esthetics, blending well with natural teeth. It is virtually divided into four horizontal layers to adapt perfectly to the color gradient, simplifying the choice of material for its multiple indications such as fully anatomical crowns and bridges from 4 pieces and anatomically reduced crown structures (
Table 1).
Monolithic zirconia has been continuously developing and it is necessary to know properties such as fracture resistance of these new materials. Compared to other ceramic materials, monolithic zirconia significantly reduces the space required for the preparation of the restoration and, therefore, contributes to a prosthetic restoration that preserves the greatest amount of tooth structure (19). Therefore, the objectives of this research were to evaluate and compare the fracture resistance of two CAD-CAM materials, zirconia dioxide (CDS) and (ZGX), stating as null hypothesis that there would be no significant differences in fracture resistance between the zirconia dioxide restorations studied.
2. Materials and Methods
2.1. Materials
Two translucent monolithic zirconia dioxide materials (CDS and ZGX) were selected. A typodont was used with a preparation to make a full crown, following the following parameters: 2 mm occlusal reduction, 1.0 mm axial reduction, chamfered termination line, parallelism between axial walls of 6 degrees and rounded edges. A digital file of the preparation was obtained with a high power structured light scanner (PrimeScanTM, Dentsply-Sirona TM, New York, USA).
2.2. Digitalization of the model and design
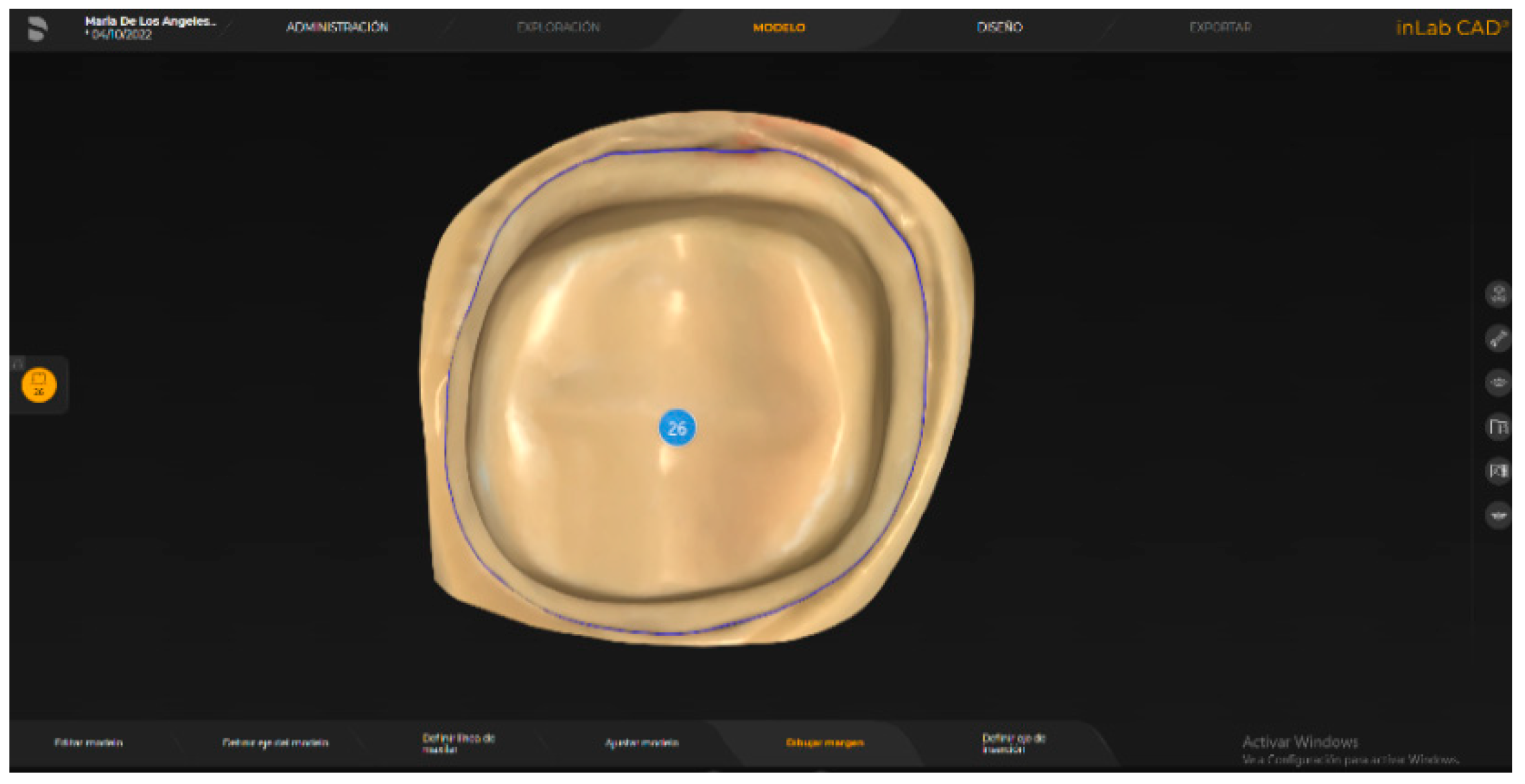
Once the model was digitized, the restoration was designed in an integrated design software (InLAB SW 22.0, Dentsply-Sirona
TM, Bensheim, Germany) (
Figure 1). For milling, the information was transferred to an integrated milling machine (CEREC InLab MCXL
TM, York, Pennsylvania, USA). Twenty restorations were made in two groups of 10 specimens for each material (
Figure 2).
2.3. Sinterization
Sintering of the zirconia dioxide restorations was carried out in a slow sintering furnace (InFire HTC, CEREC SpeedFire, Dentsply-Sirona, Bensheim, Germany) with a sintering time of 8 hours at a maximum temperature of 1500 °C on a preset pro-gram for the material.
2.4. Fracture test
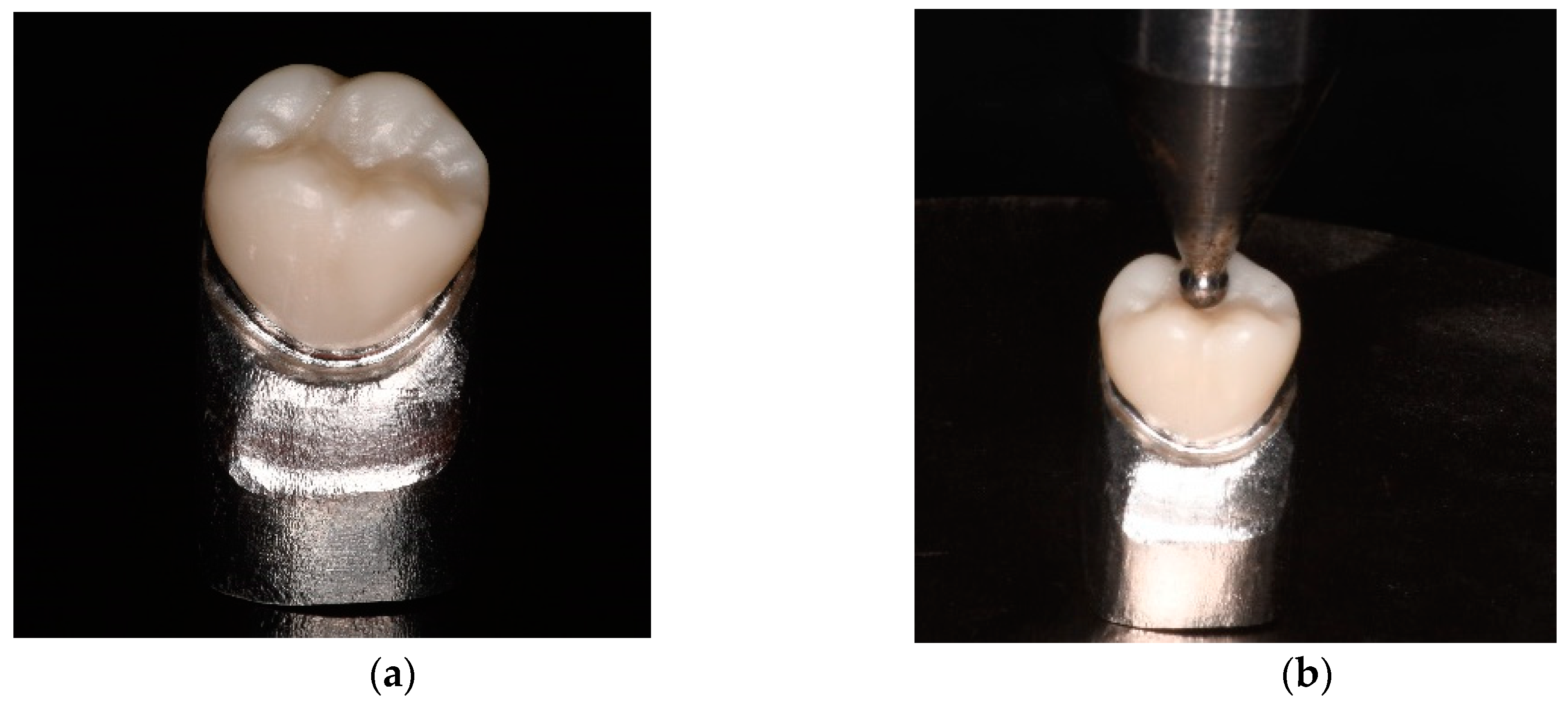
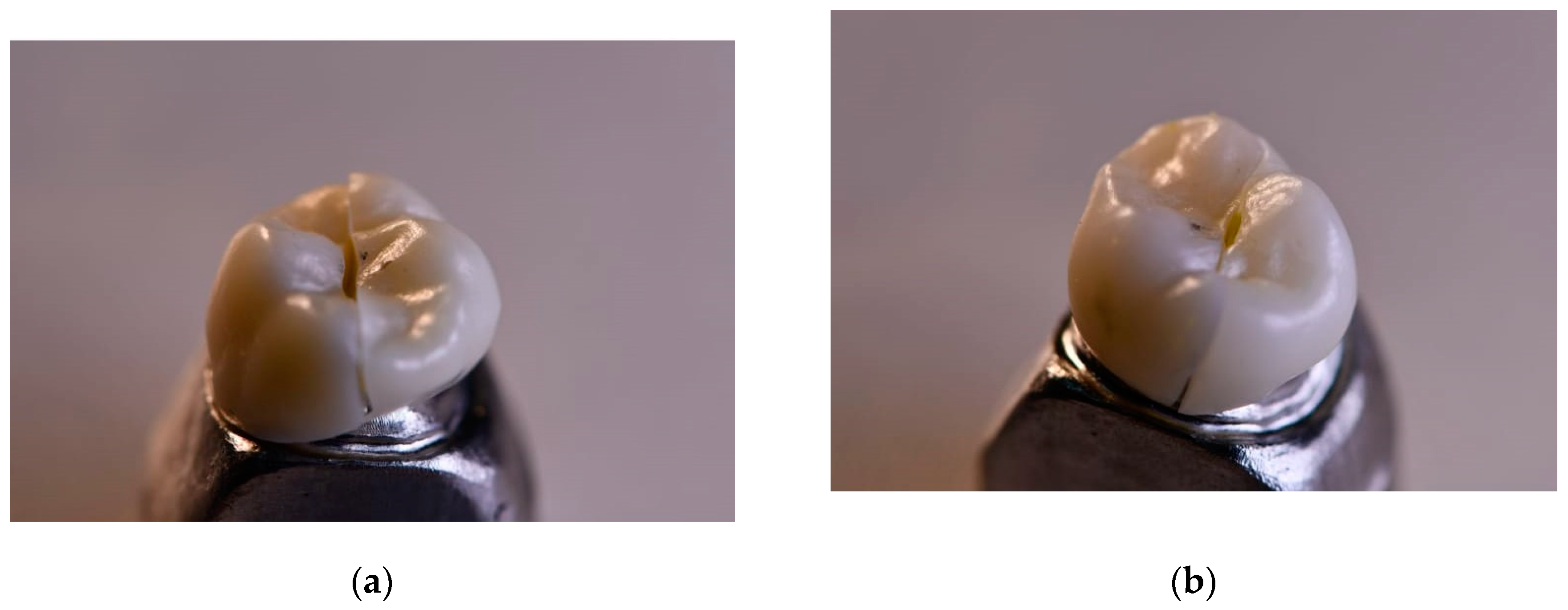
A cast metal master die (
Figure 3 [a]) was obtained from the initial scan of the original dowel type, suitable for load testing. The specimens were supported with non-cemented metal die and placed on the platform of the universal testing machine (Universal/Tensile Testing Machine, Autograph AGS-X Series).
The specimen was load tested at a rate of 0.5 mm/min with a direction parallel to the major axis of the tooth with an initial preload of 10N (
Figure 3 b) equipped with a 20kN load cell. The load was applied through a hardened steel pilot punch with a radius of 3mm applied in the central pit of the crown until fracture occurred. The force/displacement of the specimens was determined using the built-in software (TRAPEZIUM LITE X Software). The results were expressed in newtons (N).
2.5. Evaluation of the fracture mode
The fracture surface of the samples after loading was observed and analyzed using a high-resolution stereomicroscope (Olympus; SZX7, USA).
3. Results
3.1. Descriptive Analysis
Table 2 shows the descriptive statistics of the fracture toughness of materials used in this study.
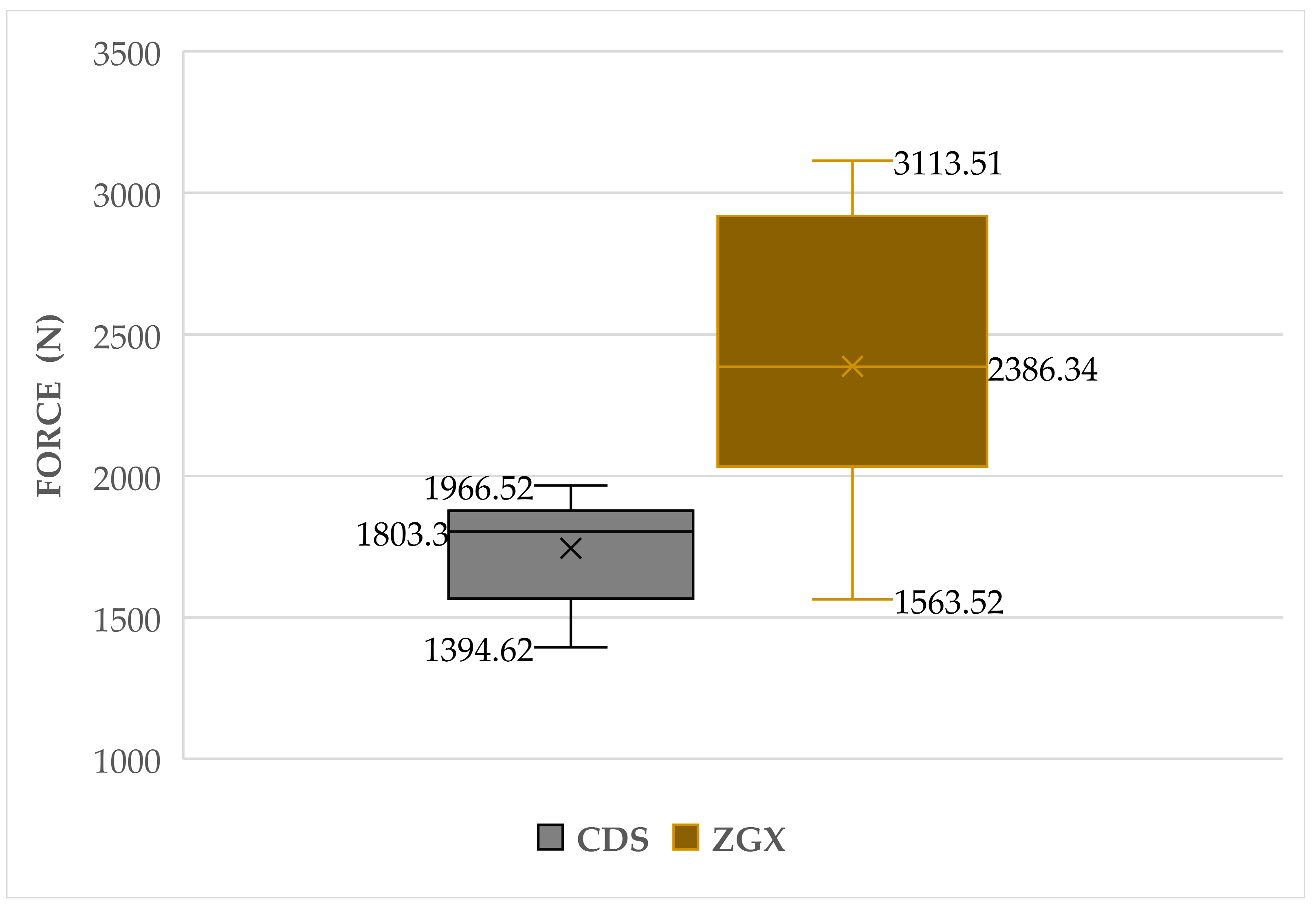
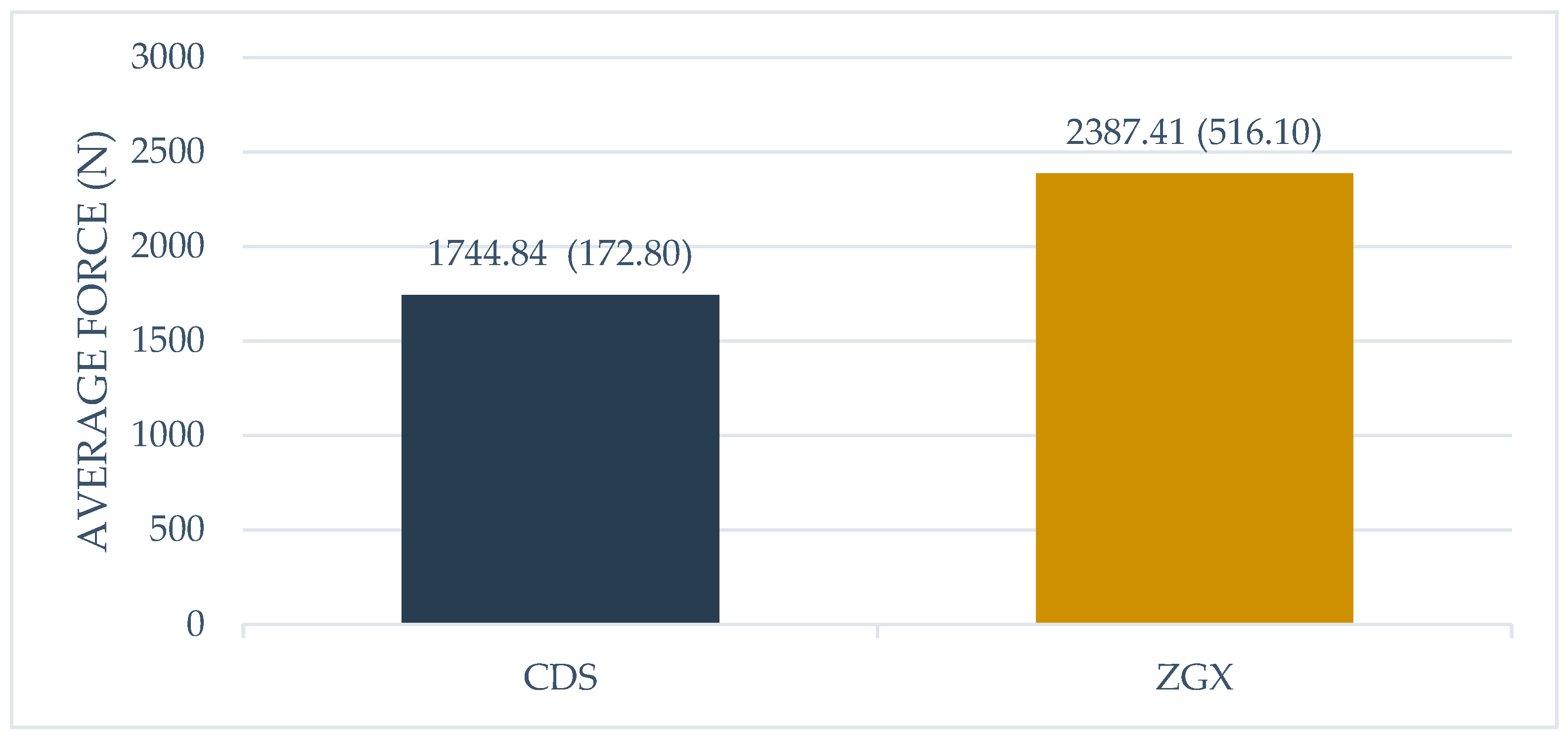
The ZGX material showed higher average fracture resistance with 2387.41 (SD = 516.10) N, the 95% confidence interval for the mean was (2018.23;2756.59) N, the coefficient of variation value indicated a mean dispersion (CV=21.9%), with a minimum and maximum strength of 1966.50 N and 3113.50 N, respectively. In comparison, the values reported with the CDS material yielded lower average fracture toughness with 1744.84 (SD = 172.80) N, the 95% confidence interval for the mean was (1628.75;1860.93) N, the dispersion was low (CV = 9.9%), and the observations were between Min = 1394.60 N and Max= 1563.50 N (
Table 2).
Figure 4 shows the quartiles, maximum and minimum values. From the comparison it was observed that the maximum value reached with the CDS material was lower than Quartile 1 (25%) of ZGX, showing a higher resistance.
Figure 5 shows the average fracture resistance of the materials. ZGX presented higher values than CDS.
3.2. Inferential analysis
With the results in
Table 3, the null hypothesis that the fracture toughness measurements are normally distributed was not rejected, with the Shapiro-Wilk statistic (p-value > 0.05), and the null hypothesis of equality of variances (p-value < 0.05) was rejected by Levene's test. Consequently, to evaluate the research hypothesis, the parametric test was used, with Student's t-statistic for independent samples assuming different variances.
According to
Table 4, the null hypothesis was not accepted (t=-3.75, p-value = 0.003<0.05). It was then determined, with a significance level of 5%, that there were significant differences between CDS and ZGX.
From the fractographic analysis, it is observed that the two materials under study present a brittle fracture. Once the critical stress value is reached, brittle materials present unstable cracks, that is, do not require an increase in stress for the spontaneous propagation of the crack and catastrophic failure occurs (
Figure 6).
4. Discussion
The all-ceramic crown is a common restorative method for a tooth that has lost much of its structure (27). Compared with the metal-ceramic crown, it has excellent biocompatibility and esthetic appearance, magnetic resonance imaging compatibility, and superior refractive index and transparency (28). Currently, materials used in all-ceramic crowns include mainly feldspathic, silica-based and yttria-stabilized tetragonal zirconia polycrystals (Y-TZP) ceramics (29). Full-contour zirconia restorations are gaining popularity in the market at the expense of multilayer systems (30). CAD/CAM applications offer a standardized fabrication process with a reliable and predictable workflow for single and complex restorations on teeth (31). Monolithic zirconia crowns have high flexural strength and fracture toughness (32). Mechanical properties such as fracture resistance would be affected by the different composition of each material. However, if these properties exceed the masticatory forces, they are clinically favorable for application in the posterior sector. Therefore, materials such as zirconium dioxide with high toughness, due to their fully crystalline microstructure and thanks to the presence of a resistive transformation mechanism, exhibit superior fracture toughness values in relation to other ceramic materials by preventing fracture propagation (33).
Therefore, the objective of this research was to compare, through an in vitro study, the fracture resistance of zirconium oxide crowns of two different commercial brands (CDS and ZGX). The null hypothesis was rejected, and it was concluded that there are differences in average fracture resistance between both CAD/CAM materials. In addition, mean fracture strengths of 1744.84 ± 172.8 N were observed for CDS and a higher strength of 2387.41 ± 516.1 N for ZGX, This differs from that reported in a study, where they compared the fracture load of four brands of zirconia, whose reported mean fracture loads were, 4804.94 ± 70.12 N, 3317.76 ± 199.80 N, 3086.54 ± 441.74 N and 2921.87 ± 349.67 N for Cercon HT, Cercon XT, Zolid Gen X and Vita YZ XT, respectively, the crowns were sandblasted before cementing to increase bond strength. Zolid Gen X had the most cracks overall, while Cercon HT crowns had the fewest cracks. Concluding that, Cercon HT presented the best strength properties, the highest fracture load and no visible cracks and that Zolid Gen X presented the lowest strength properties (34). In contrast to our study the crowns were not cemented; in a study by Sorrentino et al. who cemented the restorations with a dual-curing self-adhesive universal resin cement to simulate a real clinical situation, the formation of an adhesive layer probably contributed to increase the fracture toughness, allowing the cement to act as an elastic stress adsorbent and compensating the stiffness of the zirconia core, this could strengthen the restoration, allowing to dissipate occlusal loads over the entire surface of the crowns.(35)
Bulut in his study concluded that the occlusal thickness and the type of cement significantly affected the fracture resistance of the crowns, but the occlusal thickness was more significant. Samples of 0.5, 1.0 and 1.5 mm were made, the 1.5 mm crowns cemented with a resin cement showed higher fracture resistance compared to the other thicknesses however no significant differences were found therefore posterior zirconia crowns can withstand physiological occlusal forces even with a thickness as low as 0.5 mm (36). Corroborating with this, Sorrentino et al. similarly suggested that the occlusal thickness could be reduced to 0.5 mm without affecting fracture resistance, the crowns exhibited high fracture resistance at this 0.5 mm thickness, with a fracture load of 1400 NW being clinically acceptable. In a literature review on zirconium dioxide-based restorations, the results showed a performance similar to that of this study in terms of fracture resistance, being a resistant material suitable for this purpose both in areas with high functional load, as well as in esthetic areas of the patient (37).
An important aspect to mention is that the production of the restorations in this study involved several stages such as milling and sintering, therefore, some self-report certain limitations of the material as the production of the restorations involves several processing steps that could cause defects in the finished product (38). Therefore, there are currently studies that analyze whether variables in the production process could affect the clinical success of monolithic zirconia crowns (39) (40) (41).
An in vitro study by Kauling (42) evaluated the properties of 3-unit zirconia monolithic fixed dental prostheses (FPD) after rapid sintering and compared the properties with conventional sintering. They found that the fast-sintering FPDs had a better marginal and occlusal fit than the conventionally sintered FPDs. In addition, no significant differences in fracture load values were found due to the sintering procedure, but artificial aging was found to significantly affect the fracture load values. In general, fast sintering FPDs had equal and better values for fracture set and fracture load than conventional sintering FPDs. However, other authors concluded that there was no significant difference between the two groups, and the mechanical strength of the material was not affected, which would imply clinical and laboratory time savings when performing rapid sintering on translucent monolithic zirconium dioxide restorations. However, rapidly sintered restorations have limited reliability depending on the case (43).
In another study, the flexural strength of different kinds of multilayered zirconia in enamel and dentin layers was evaluated. The strength was similar for that of both layers and the multilayer restoration accumulated the highest strength, followed by the translucent super multilayer and the ultra-translucent multilayer. However, the strength of the transverse multilayer was lower than that of the enamel or dentin layers due to weak interfaces. In addition, it was mentioned that, when measuring strength by bending, there may be errors due to friction and accuracy in determining the distances of the loading spans (44). The result of resistance to fracture shown with CDS in this research was similar to that obtained in a study where they compared the resistance to fracture between a group of crowns made to measure and a group of prefabricated crowns, both made of Cercon HT Dentsply-Sirona Zirconia (34); yielding an average resistance of 1987.38 ± 414.88 N for the crowns made to measure and 1793.54 ± 423.82 N for the prefabricated ones, finding no significant differences between the two. According to Ottawa: (Canadian Agency for Drugs and Technologies in Health) the average resistance to initial fracture shown with Zolid Gen-X was 2634 ± 106.2 N and after aging in a chewing simulator it was 2087 ± 126.1 N, showing similar values to those reported in the present investigation (27).
It should be noted that, during the load test that was performed in the first instance, a printed resin die was used and during the process the initial failure was of the die, so it was chosen to perform it in a more resistant material. In this case, a cast metal cobalt-chromium die with higher elastic modulus and fracture resistance, however a natural tooth could have replicated the clinical environment more accurately if it had been chosen as an abutment, however natural teeth have different sizes, shapes and qualities, and therefore the preparation material would be difficult to standardize (45).
Laboratory tests apply static loads until the material breaks by means of a universal machine, representing its behavior in a force-displacement curve and recording the maximum load applied. These tests provide information on the strength of the material, the potential risk of failure and the deformation of the material. However, they cannot sufficiently predict the long-term performance of dental restorations. Badawy et al. (46) mentioned in their study the importance of knowing the fracture toughness of dental ceramics, which by nature are brittle and have an increased susceptibility to fracture under stress. A restorative material with high fracture toughness presents better fracture resistance and longevity. Being an in-vitro study, one of the limitations of this research is that the behavior of these materials under cyclic fatigue was not analyzed. Fracture toughness testing, using a single unidirectional compressive load, provides only limited insight into clinically relevant mechanisms of crown damage under forces with different directions and cyclic loading. (43) Future research needs to analyze the cyclic fatigue and clinical behavior of this material over time, as well as to analyze the material cemented with different adhesive techniques. Therefore, experimental settings that reproduce situations similar to intraoral conditions are needed. More evidence from long-term clinical studies is needed to verify the fracture performance of monolithic zirconia CAD/CAM materials for indirect full-coverage restorations.
5. Conclusions
- -
It was found that the ZGX material, obtained higher fracture resistance compared with the CDS.
- -
The crown fracture loads of the two materials were in the acceptable range. In comparison with the maximum bite force, the materials showed an acceptable load-to-fracture value.
- -
The monolithic zirconia crowns showed a favorable mechanical property to withstand the occlusal load at 0.5 mm thickness.
Author Contributions
Conceptualization, C.A.; methodology, C.A., C.A.P., J.F.,A.U., C.A.P. and J.I.F.; software, C.P. J.I.F.; validation, C.A., J.I.F.; formal analysis, A.U. and A.P.; investigation, C.A., A.U., C.A.P. and J.I.F.; resources, C.A.; C.A.P., A.U., A.P. and J.I.F.; data curation, A.U. and A.P.; writing—original draft preparation, C.A.; C.A.P., A.U., A.P. and J.I.F.; writing—review and editing, C.A.; A.U., C.A.P. and J.I.F.; visualization, C.A.; C.A.P.;J.I.F.; supervision, C.A.; C.A.P. and J.I.F.; project administration, C.A. All authors have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Spitznagel FA, Boldt J, Gierthmuehlen PC. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J Dent Res. September 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- Mörmann, WH. The evolution of the CEREC system. J Am Dent Assoc, 1939. September 2006;137 Suppl:7S–13S.
- Luthardt RG, Sandkuhl O, Reitz B. Zirconia-TZP and alumina--advanced technologies for the manufacturing of single crowns. Eur J Prosthodont Restor Dent. december 1999, 7, 113–119. [Google Scholar]
- Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int Berl Ger 1985. 2017, 48, 369–380. [Google Scholar]
- Čokić SM, Cóndor M, Vleugels J, Meerbeek BV, Oosterwyck HV, Inokoshi M, et al. Mechanical properties-translucency-microstructure relationships in commercial monolayer and multilayer monolithic zirconia ceramics. Dent Mater Off Publ Acad Dent Mater. may 2022, 38, 797–810. [Google Scholar]
- Özkurt-Kayahan, Z. monolithic-zirconia-a-review-of-the-literature. Biomed Res. 2016, 27. [Google Scholar]
- Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int Berl Ger 1985. 2017, 48, 441–450. [Google Scholar]
- Güth JF, Stawarczyk B, Edelhoff D, Liebermann A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int Berl Ger 1985. 2019, 50, 512–520.
- Ghodsi S, Jafarian Z. A Review on Translucent Zirconia. Eur J Prosthodont Restor Dent. may 2018, 26, 62–74. [Google Scholar]
- Zhang Y, Lawn BR. Novel Zirconia Materials in Dentistry. J Dent Res. february 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. july 2018, 120, 132–137. [Google Scholar] [CrossRef]
- Rinke S, Metzger A, Ziebolz H. Multilayer Super-Translucent Zirconia for Chairside Fabrication of a Monolithic Posterior Crown. Case Rep Dent. 2022, 2022, 4474227. [Google Scholar]
- Flinn BD, Raigrodski AJ, Mancl LA, Toivola R, Kuykendall T. Influence of aging on flexural strength of translucent zirconia for monolithic restorations. J Prosthet Dent. february 2017, 117, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, TF. The effect of extended aging on the optical properties of different zirconia materials. J Prosthodont Res. july 2017, 61, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Silva LH da, Lima E de, Miranda RB de P, Favero SS, Lohbauer U, Cesar PF. Dental ceramics: a review of new materials and processing methods. Braz Oral Res. august 2017, 31, e58. [Google Scholar]
- Lameira DP, Buarque e Silva WA, Andrade e Silva F, De Souza GM. Fracture Strength of Aged Monolithic and Bilayer Zirconia-Based Crowns. BioMed Res Int. 2015, 2015, 418641. [Google Scholar]
- Johansson C, Kmet G, Rivera J, Larsson C, Vult Von Steyern P. Fracture strength of monolithic all-ceramic crowns made of high translucent yttrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontol Scand. february 2014, 72, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Jansen JU, Lümkemann N, Letz I, Pfefferle R, Sener B, Stawarczyk B. Impact of high-speed sintering on translucency, phase content, grain sizes, and flexural strength of 3Y-TZP and 4Y-TZP zirconia materials. J Prosthet Dent. october 2019, 122, 396–403. [Google Scholar]
- Ahmed WM, Troczynski T, McCullagh AP, Wyatt CCL, Carvalho RM. The influence of altering sintering protocols on the optical and mechanical properties of zirconia: A review. J Esthet Restor Dent Off Publ Am Acad Esthet Dent Al. september 2019, 31, 423–430. [Google Scholar]
- Kolakarnprasert N, Kaizer MR, Kim DK, Zhang Y. New multi-layered zirconias: Composition, microstructure and translucency. Dent Mater Off Publ Acad Dent Mater. may 2019, 35, 797–806. [Google Scholar]
- Cardoso KV, Adabo GL, Mariscal-Muñoz E, Antonio SG, Arioli Filho JN. Effect of sintering temperature on microstructure, flexural strength, and optical properties of a fully stabilized monolithic zirconia. J Prosthet Dent. november 2020, 124, 594–598. [Google Scholar] [CrossRef]
- Optical properties of translucent zirconia: A review of the literature [Internet]. march 2023. Disponible : https://sciendo.com/article/10.2478/ebtj-2019-0005. 2478.
- Lopez-Suarez C, Rodriguez V, Pelaez J, Agustin-Panadero R, Suarez MJ. Comparative fracture behavior of monolithic and veneered zirconia posterior fixed dental prostheses. Dent Mater J. november 2017, 36, 816–821. [Google Scholar] [CrossRef]
- Sarıkaya I, Hayran Y. Effects of dynamic aging on the wear and fracture strength of monolithic zirconia restorations. BMC Oral Health. august 2018, 18, 146. [Google Scholar]
- Habibi Y, Dawid MT, Waldecker M, Rammelsberg P, Bömicke W. Three-year clinical performance of monolithic and partially veneered zirconia ceramic fixed partial dentures. J Esthet Restor Dent Off Publ Am Acad Esthet Dent Al. june 2020, 32, 395–402. [Google Scholar]
- El Shahawy OI, Azab MM. Fracture resistance of prefabricated versus custom-made zirconia crowns after thermo-mechanical aging: an in-vitro study. BMC Oral Health. december 2022, 22, 587. [Google Scholar]
- J. Mech Behav Biomed MaterPorcelain-Fused-to-Metal Crowns versus All-ceramic Crowns: A Review of the Clinical and Cost-Effectiveness [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2015 [march 2023]. (CADTH Rapid Response Reports). Disponible en: http://www.ncbi.nlm.nih.gov/books/NBK304693/. 3046.
- Barão VAR, Gennari-Filho H, Goiato MC, dos Santos DM, Pesqueira AA. Factors to achieve aesthetics in all-ceramic restorations. J Craniofac Surg. november 2010, 21, 2007–2012. [Google Scholar] [CrossRef] [PubMed]
- Harada K, Shinya A, Gomi H, Hatano Y, Shinya A, Raigrodski AJ. Effect of accelerated aging on the fracture toughness of zirconias. J Prosthet Dent. february 2016, 115, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis I, Trikka D, Gasparatos S, Mitsias ME. Clinical Outcomes of Monolithic Zirconia Crowns with CAD/CAM Technology. A 1-Year Follow-Up Prospective Clinical Study of 65 Patients. Int J Environ Res Public Health. 12 de november 2018, 15, 2523.
- Yang SW, Kim JE, Shin Y, Shim JS, Kim JH. Enamel wear and aging of translucent zirconias: In vitro and clinical studies. J Prosthet Dent. march 2019, 121, 417–425. [Google Scholar] [CrossRef]
- Candido LM, Miotto LN, Fais L, Cesar PF, Pinelli L. Mechanical and Surface Properties of Monolithic Zirconia. Oper Dent. 2018, 43, E119–E128. [Google Scholar] [CrossRef]
- Scherrer SS, Lohbauer U, Della Bona A, Vichi A, Tholey MJ, Kelly JR, et al. ADM guidance-Ceramics: guidance to the use of fractography in failure analysis of brittle materials. Dent Mater Off Publ Acad Dent Mater. june 2017, 33, 599–620. [Google Scholar]
- Kongkiatkamon S, Booranasophone K, Tongtaksin A, Kiatthanakorn V, Rokaya D. Comparison of Fracture Load of the Four Translucent Zirconia Crowns. Mol Basel Switz. 1 de september 2021, 26, 5308.
- Sorrentino R, Triulzio C, Tricarico MG, Bonadeo G, Gherlone EF, Ferrari M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J Mech Behav Biomed Mater. august 2016, 61, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Bulut AC, Atsü SS. Occlusal Thickness and Cement-Type Effects on Fracture Resistance of Implant-Supported Posterior Monolithic Zirconia Crowns. Int J Oral Maxillofac Implants. 2021, 36, 485–491. [Google Scholar] [CrossRef]
- Tekin YH, Hayran Y. Fracture resistance and marginal fit of the zirconia crowns with varied occlusal thickness. J Adv Prosthodont. october 2020, 12, 283–290. [Google Scholar] [CrossRef]
- Denry, I. How and when does fabrication damage adversely affect the clinical performance of ceramic restorations? Dent Mater Off Publ Acad Dent Mater. january 2013, 29, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Hallmann L, Mehl A, Ulmer P, Reusser E, Stadler J, Zenobi R, et al. The influence of grain size on low-temperature degradation of dental zirconia. J Biomed Mater Res B Appl Biomater. february 2012, 100, 447–456. [Google Scholar]
- Pereira GKR, Guilardi LF, Dapieve KS, Kleverlaan CJ, Rippe MP, Valandro LF. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J Mech Behav Biomed Mater. september 2018, 85, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Kim HK, Kim SH, Lee JB, Han JS, Yeo IS. Effect of polishing and glazing on the color and spectral distribution of monolithic zirconia. J Adv Prosthodont. august 2013, 5, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Elisa Kauling A, Güth JF, Erdelt K, Edelhoff D, Keul C. Influence of speed sintering on the fit and fracture strength of 3-unit monolithic zirconia fixed partial dentures. J Prosthet Dent. september 2020, 124, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Ordoñez Balladares A, Abad-Coronel C, Ramos JC, Martín Biedma BJ. Fracture Resistance of Sintered Monolithic Zirconia Dioxide in Different Thermal Units. Mater Basel Switz. march 2022, 15, 2478. [Google Scholar]
- Kaizer MR, Kolakarnprasert N, Rodrigues C, Chai H, Zhang Y. Probing the interfacial strength of novel multi-layer zirconias. Dent Mater Off Publ Acad Dent Mater. january 2020, 36, 60–67. [Google Scholar]
- Giner S, Bartolomé JF, Gomez-Cogolludo P, Castellote C, Pradíes G. Fatigue fracture resistance of titanium and chairside CAD-CAM zirconia implant abutments supporting zirconia crowns: An in vitro comparative and finite element analysis study. J Prosthet Dent. march 2021, 125, e1–e503. [Google Scholar]
- Badawy R, El-Mowafy O, Tam LE. Fracture toughness of chairside CAD/CAM materials - Alternative loading approach for compact tension test. Dent Mater Off Publ Acad Dent Mater. july 2016, 32, 847–852. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).