Submitted:
30 April 2023
Posted:
04 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
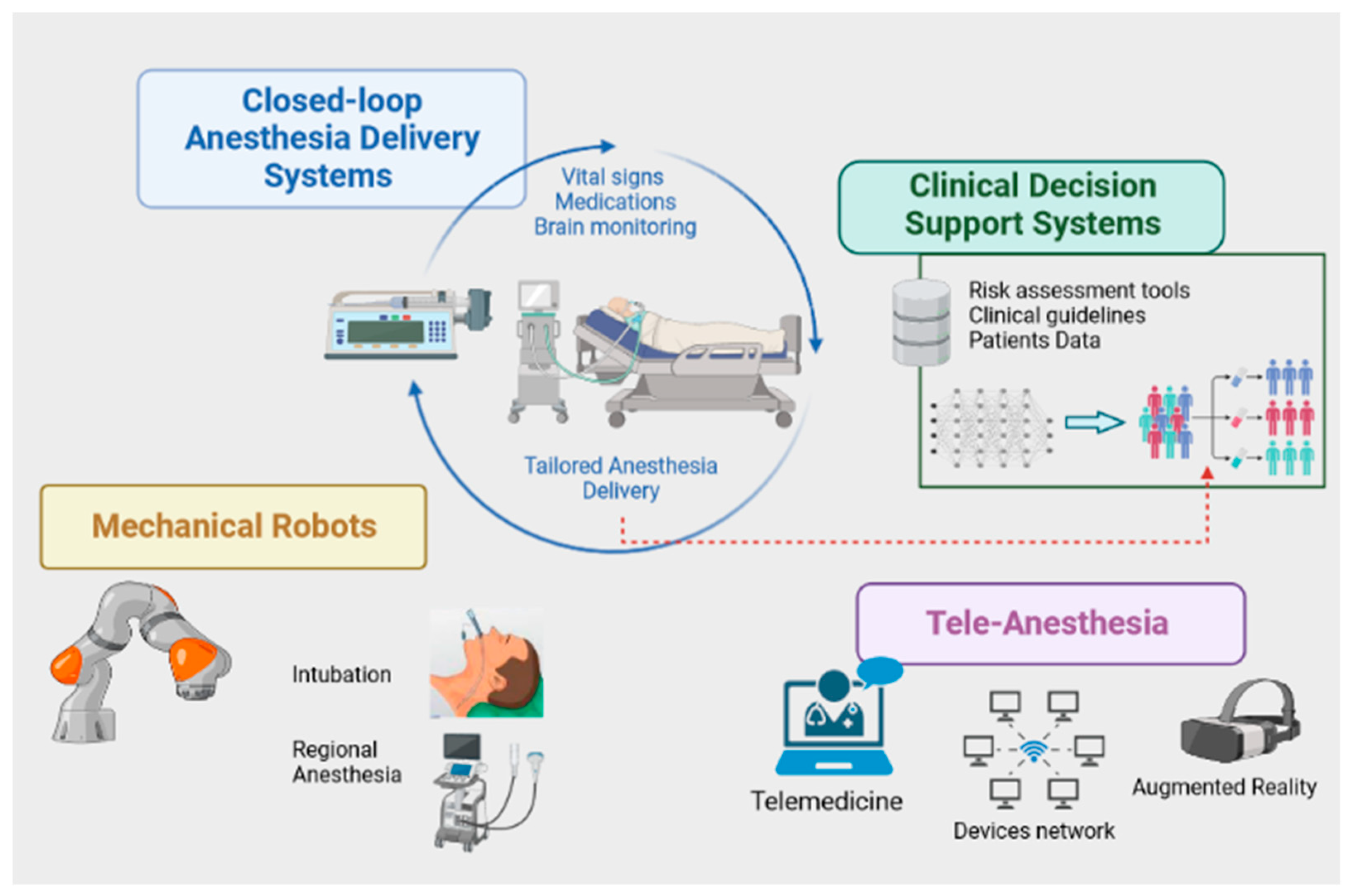
2. AI in Anesthesia
3. Ethical implications
Scientific Output, Ongoing Research, and Perspectives
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moon JS, Cannesson M. A Century of Technology in Anesthesia & Analgesia. Anesth Analg. 2022;135(2S Suppl 1):S48-S61. [CrossRef]
- Petermann H, Böhrer H, Witte W. Von der Äthernarkose zur „grünen“ Anästhesie : Herausforderungen in der Anästhesiologie der letzten 175 Jahre [From ether anesthesia to "green" anesthesia : Challenges in anesthesiology over the last 175 years]. Anaesthesist. 2021;70(10):832-842. German. [CrossRef]
- Stanfill MH, Marc DT. Health Information Management: Implications of Artificial Intelligence on Healthcare Data and Information Management. Yearb Med Inform. 2019;28(1):56-64. [CrossRef]
- Bellini V, Valente M, Gaddi AV, Pelosi P, Bignami E. Artificial intelligence and telemedicine in anesthesia: potential and problems. Minerva Anestesiol. 2022;88(9):729-734. [CrossRef]
- Bihorac A, Ozrazgat-Baslanti T, Ebadi A, Motaei A, Madkour M, Pardalos PM, Lipori G, Hogan WR, Efron PA, Moore F, Moldawer LL, Wang DZ, Hobson CE, Rashidi P, Li X, Momcilovic P. MySurgeryRisk: Development and Validation of a Machine-learning Risk Algorithm for Major Complications and Death After Surgery. Ann Surg. 2019;269(4):652-662. [CrossRef]
- Lee HC, Ryu HG, Chung EJ, Jung CW. Prediction of Bispectral Index during Target-controlled Infusion of Propofol and Remifentanil: A Deep Learning Approach. Anesthesiology. 2018;128(3):492-501. [CrossRef]
- Hofer IS, Lee C, Gabel E, Baldi P, Cannesson M. Development and validation of a deep neural network model to predict postoperative mortality, acute kidney injury, and reintubation using a single feature set. NPJ Digit Med. 2020;3:58. [CrossRef]
- Hewson DW, Bedforth NM. Closing the gap: artificial intelligence applied to ultrasound-guided regional anaesthesia. Br J Anaesth. 2023;130(3):245-247. [CrossRef]
- Solanki SL, Pandrowala S, Nayak A, Bhandare M, Ambulkar RP, Shrikhande SV. Artificial intelligence in perioperative management of major gastrointestinal surgeries. World J Gastroenterol. 2021;27(21):2758-2770. [CrossRef]
- Li YY, Wang JJ, Huang SH, Kuo CL, Chen JY, Liu CF, Chu CC. Implementation of a machine learning application in preoperative risk assessment for hip repair surgery. BMC Anesthesiol. 2022;22(1):116. [CrossRef]
- Chiew CJ, Liu N, Wong TH, Sim YE, Abdullah HR. Utilizing Machine Learning Methods for Preoperative Prediction of Postsurgical Mortality and Intensive Care Unit Admission. Ann Surg. 2020;272(6):1133-1139. [CrossRef]
- Corey KM, Kashyap S, Lorenzi E, Lagoo-Deenadayalan SA, Heller K, Whalen K, Balu S, Heflin MT, McDonald SR, Swaminathan M, Sendak M. Development and validation of machine learning models to identify high-risk surgical patients using automatically curated electronic health record data (Pythia): A retrospective, single-site study. PLoS Med. 2018;15(11):e1002701. [CrossRef]
- Neckebroek M, Ionescu CM, van Amsterdam K, De Smet T, De Baets P, Decruyenaere J, De Keyser R, Struys MMRF. A comparison of propofol-to-BIS post-operative intensive care sedation by means of target controlled infusion, Bayesian-based and predictive control methods: an observational, open-label pilot study. J Clin Monit Comput. 2019;33(4):675-686. [CrossRef]
- Härkänen M, Haatainen K, Vehviläinen-Julkunen K, Miettinen M. Artificial Intelligence for Identifying the Prevention of Medication Incidents Causing Serious or Moderate Harm: An Analysis Using Incident Reporters' Views. Int J Environ Res Public Health. 2021;18(17):9206. [CrossRef]
- Syrowatka A, Song W, Amato MG, Foer D, Edrees H, Co Z, Kuznetsova M, Dulgarian S, Seger DL, Simona A, Bain PA, Purcell Jackson G, Rhee K, Bates DW. Key use cases for artificial intelligence to reduce the frequency of adverse drug events: a scoping review. Lancet Digit Health. 2022;4(2):e137-e148. [CrossRef]
- Hashimoto DA, Witkowski E, Gao L, Meireles O, Rosman G. Artificial Intelligence in Anesthesiology: Current Techniques, Clinical Applications, and Limitations. Anesthesiology. 2020;132(2):379-394. [CrossRef]
- Nagireddi JN, Vyas AK, Sanapati MR, Soin A, Manchikanti L. The Analysis of Pain Research through the Lens of Artificial Intelligence and Machine Learning. Pain Physician. 2022;25(2):E211-E243.
- Cascella M, Montomoli J, Bellini V, Bignami EG. Integrating data science and neural architecture techniques for automatic pain assessment in critically ill patients. Anaesth Crit Care Pain Med. 2023;42(4):101220. [CrossRef]
- Cobianchi L, Piccolo D, Dal Mas F, Agnoletti V, Ansaloni L, Balch J, Biffl W, Butturini G, Catena F, Coccolini F, Denicolai S, De Simone B, Frigerio I, Fugazzola P, Marseglia G, Marseglia GR, Martellucci J, Modenese M, Previtali P, Ruta F, Venturi A, Kaafarani HM, Loftus TJ; Team Dynamics Study Group. Surgeons' perspectives on artificial intelligence to support clinical decision-making in trauma and emergency contexts: results from an international survey. World J Emerg Surg. 2023;18(1):1. [CrossRef]
- McCoy A, Das R. Reducing patient mortality, length of stay and readmissions through machine learning-based sepsis prediction in the emergency department, intensive care unit and hospital floor units. BMJ Open Qual. 2017;6(2):e000158. [CrossRef]
- Loftus TJ, Vlaar APJ, Hung AJ, Bihorac A, Dennis BM, Juillard C, Hashimoto DA, Kaafarani HMA, Tighe PJ, Kuo PC, Miyashita S, Wexner SD, Behrns KE. Executive summary of the artificial intelligence in surgery series. Surgery. 2022;171(5):1435-1439. [CrossRef]
- O'Connor S, ChatGPT. Open artificial intelligence platforms in nursing education: Tools for academic progress or abuse? Nurse Educ Pract. 2023;66:103537. [CrossRef]
- Cascella M, Montomoli J, Bellini V, Bignami E. Evaluating the Feasibility of ChatGPT in Healthcare: An Analysis of Multiple Clinical and Research Scenarios. J Med Syst. 2023;47(1):33. [CrossRef]
- Bellini V, Cascella M, Cutugno F, Russo M, Lanza R, Compagnone C, Bignami EG. Understanding basic principles of Artificial Intelligence: a practical guide for intensivists. Acta Biomed. 2022;93(5):e2022297. [CrossRef]
- Hassan AM, Rajesh A, Asaad M, Nelson JA, Coert JH, Mehrara BJ, Butler CE. A Surgeon's Guide to Artificial Intelligence-Driven Predictive Models. Am Surg. 2023;89(1):11-19. [CrossRef]
- Freundlich RE, Ehrenfeld JM. Anesthesia information management: clinical decision support. Curr Opin Anaesthesiol. 2017 Dec;30(6):705-709. [CrossRef]
- Olsen RM, Aasvang EK, Meyhoff CS, Dissing Sorensen HB. Towards an automated multimodal clinical decision support system at the post anesthesia care unit. Comput Biol Med. 2018;101:15-21. [CrossRef]
- Wingert T, Lee C, Cannesson M. Machine Learning, Deep Learning, and Closed Loop Devices-Anesthesia Delivery. Anesthesiol Clin. 2021;39(3):565-581. [CrossRef]
- Wehbe M, Arbeid E, Cyr S, Mathieu PA, Taddei R, Morse J, Hemmerling TM. A technical description of a novel pharmacological anesthesia robot. J Clin Monit Comput. 2014;28(1):27-34. [CrossRef]
- Hemmerling TM, Wehbe M, Zaouter C, Taddei R, Morse J. The Kepler intubation system. Anesth Analg. 2012;114:590–4. [CrossRef]
- O'Donnell BD, O'Sullivan O, Gal-lagher AG, Shorten GD. Robotic assistance with needle guidance. Br J Anaesth. 2015;114(4):708-9. [CrossRef]
- Cobianchi L, Verde JM, Loftus TJ, Piccolo D, Dal Mas F, Mascagni P, Garcia Vazquez A, Ansaloni L, Marseglia GR, Massaro M, Gallix B, Padoy N, Peter A, Kaafarani HM. Artificial Intelligence and Surgery: Ethical Dilemmas and Open Issues. J Am Coll Surg. 2022;235(2):268-275. [CrossRef]
- Cascella M, Montomoli J, Bellini V, Vittori A, Biancuzzi H, Dal Mas F, Bignami EG. Crossing the AI Chasm in Neurocritical Care. Computers. 2023;12(4):83. [CrossRef]
- Panch T, Mattie H, Atun R. Artificial intelligence and algorithmic bias: implications for health systems. J Glob Health. 2019;9(2):010318. [CrossRef]
- Bellini V, Petroni A, Palumbo G, Bignami E. Data quality and blockchain technology. Anaesth Crit Care Pain Med. 2019;38(5):521-522. [CrossRef]
- Raimundo R, Rosário A. The Impact of Artificial Intelligence on Data System Security: A Literature Review. Sensors (Basel). 2021;21(21):7029. [CrossRef]
- Harvey HB, Gowda V. Regulatory Issues and Challenges to Artificial Intelligence Adoption. Radiol Clin North Am. 2021;59(6):1075-1083. [CrossRef]
- Nifakos S, Chandramouli K, Nikolaou CK, Papachristou P, Koch S, Panaousis E, Bonacina S. Influence of Human Factors on Cyber Security within Healthcare Organisations: A Systematic Review. Sensors (Basel). 2021;21(15):5119. [CrossRef]
- Health Insurance Portability and Accountability Act of 1996 (HIPAA). Available at: https://www.cdc.gov/phlp/publications/topic/hipaa.html. Last Accessed: April 20, 2023.
- Coppola L, Cianflone A, Grimaldi AM, Incoronato M, Bevilacqua P, Messina F, Baselice S, Soricelli A, Mirabelli P, Salvatore M. Biobanking in health care: evolution and future directions. J Transl Med. 2019;17(1):172. [CrossRef]
- Amann J, Blasimme A, Vayena E, Frey D, Madai VI; Precise4Q consortium. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020;20(1):310. [CrossRef]
- Arbelaez Ossa L, Starke G, Lorenzini G, Vogt JE, Shaw DM, Elger BS. Re-focusing explainability in medicine. Digit Health. 2022 Feb 11;8:20552076221074488. [CrossRef]
- Koski E, Murphy J. AI in Healthcare. Stud Health Technol Inform. 2021;284:295-299. [CrossRef]
- Banja, J. How Might Artificial Intelligence Applications Impact Risk Management? AMA J Ethics. 2020;22(11):E945-951. [CrossRef]
- Keskinbora, KH. Medical ethics considerations on artificial intelligence. J Clin Neurosci. 2019;64:277-282. [CrossRef]
- Alexander JC, Romito BT, Çobanoğlu MC. The present and future role of artificial intelli-gence and machine learning in anesthesiology. Int Anesthesiol Clin. 2020 Fall;58(4):7-16. [CrossRef]
- Cascella M, Perri F, Ottaiano A, Cuomo A, Wirz S, Coluccia S. Trends in Research on Artificial Intelligence in Anesthesia: A VOSviewer -Based Biblio-metric Analysis. Inteligencia Artificial 2022;25(70):126-137. [CrossRef]
- Miyaguchi N, Takeuchi K, Kashima H, Morita M, Morimatsu H. Predicting anesthetic infusion events using machine learning. Sci Rep. 2021;11(1):23648. [CrossRef]
- Zhao H, You J, Peng Y, Feng Y. Machine Learning Algorithm Using Electronic Chart-Derived Data to Predict Delirium After Elderly Hip Fracture Surgeries: A Retrospective Case-Control Study. Front Surg. 2021;8:634629. [CrossRef]
- Walczak S, Velanovich V. Prediction of perioperative transfusions using an artificial neural network. PLoS One. 2020;15(2):e0229450. [CrossRef]
- Afshar S, Boostani R, Sanei S. A Combinatorial Deep Learning Structure for Precise Depth of Anesthesia Estimation From EEG Signals. IEEE J Biomed Health Inform. 2021; 25(9): 3408-3415. [CrossRef]
- Cuendet GL, Schoettker P, Yüce A, Sorci M, Gao H, Perruchoud C, et al. Facial Image Analysis for Fully Automatic Prediction of Difficult Endotracheal Intubation. IEEE Trans Biomed Eng. 2016; 63(2):328-39. [CrossRef]
- Joosten A, Alexander B, Duranteau J, Taccone FS, Creteur J, Vincent JL, et al. Feasibility of closed-loop titration of norepinephrine infusion in patients undergoing moderate- and high-risk surgery. Br J Anaesth. 2019; 123(4): 430-438. [CrossRef]
- Connor, CW. Artificial Intelligence and Machine Learning in Anesthesiology. Anesthesiology. 2019; 131(6): 1346-1359. [CrossRef]
- Lee M, Sanz LRD, Barra A, Wolff A, Nieminen JO, Boly M, et al. Quantifying arousal and awareness in altered states of consciousness using interpretable deep learning. Nat Commun. 2022;13(1):1064. [CrossRef]
- Lonsdale H, Jalali A, Gálvez JA, Ahumada LM, Simpao AF. Artificial Intelligence in Anesthesiology: Hype, Hope, and Hurdles. Anesth Analg. 2020;130(5):1111-1113. [CrossRef]
- Singh M, Nath G. Artificial intelligence and anesthesia: A narrative review. Saudi J Anaesth. 2022;16(1):86-93. [CrossRef]
- Stradolini F, Tuoheti A, Kilic T, Ntella SL, Tamburrano N, Huang Z, De Micheli G, Demarchi D, Carrara S. An IoT Solution for Online Monitoring of Anesthetics in Human Serum Based on an Integrated Fluidic Bioelectronic System. IEEE Trans Biomed Circuits Syst. 2018;12(5):1056-1064. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions, and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |
| Application | Strategy | [Ref.] |
|---|---|---|
| Presurgical evaluation | Preoperative management and planning. | [9,10,11,12] |
| Anesthetic Dosage Optimization | AI algorithms can analyze a patient's medical history, physiological data, and other factors to determine the most appropriate anesthetic dose, which can improve patient safety and minimize complications. | [6,13] |
| Preventing Drug Errors | AI-powered systems can help prevent drug administration errors by verifying medication orders, drug interactions, and dosages. | [14,15] |
| Early detection of complications | AI can be used to analyze various data streams in real-time to detect patterns or anomalies that may indicate a potential complication such as hypoxia and hypotension. | [4,16] |
| Predicting Patient Outcomes | Machine learning algorithms can be used to predict the likelihood of complications or adverse outcomes during surgery, allowing anesthesiologists to make more informed decisions about patient care. | [10] |
| Predicting Postsurgical ICU Admission | Various machine learning algorithms can be employed to develop predictive models from data such as patient demographics, medical history, surgical procedures, vital signs, laboratory values, and other clinical factors. | [11] |
| Automated Monitoring | AI-powered monitoring systems can continuously track a patient's vital signs, such as heart rate, blood pressure, and oxygen saturation, and alert the anesthesiologist to any potential problems. | [16] |
| Automated Anesthesia Dosing | AI can help tailor anesthesia delivery and optimize closed-loop systems based on patient data. | [4,6] |
| Pain Management | AI can help adjust the dosage and administering of drugs to achieve optimal postoperative pain control. | [17,18] |
| Real-Time Decision Support | AI algorithms can provide real-time decision support to anesthesiologists during surgery, such as recommending alternative drug options if a patient is not responding to the initial anesthetic. | [19] |
| Postoperative Monitoring | AI can help monitor patients postoperatively, predicting and detecting any adverse events that might occur, and giving alerts and recommendations to physicians. | [20] |
| Resource Allocation | AI algorithms can help optimize the use of anesthesia resources by identifying the best candidates for specific procedures and reducing unnecessary anesthesia use. | [21] |
| Training and Education | AI can be used to simulate scenarios and train anesthesiologists to handle challenging situations, such as unexpected complications during surgery. | [22,23] |
| Image recognition | AI algorithms can analyze medical images to identify anatomical structures and guide the placement of regional anesthesia techniques. | [8] |
| Research and Analysis | AI can help analyze vast amounts of data from anesthesia records, patient charts, and other sources to identify patterns, trends, and insights that could help improve patient outcomes and safety. | [24,25] |
| Issue | Notes | [Ref.] |
|---|---|---|
| Bias and discrimination | AI systems may perpetuate biases and discrimination if they are trained on biased data. | [34,35,36] |
| Privacy and security | It is mandatory to establish robust security protocols | [38,39,40] |
| Accountability and transparency | Model explainability is the ability of AI and machine learning models to provide clear and interpretable explanations of their decision-making process | [41,42] |
| Access to healthcare | AI systems may exacerbate existing disparities in access to healthcare, as the use of AI may require expensive technology or specialized training that is not available to all healthcare providers. | [43] |
| Regulatory processes | Governments and other stakeholders must define technical standards for ensuring the accuracy, reliability, and safety of AI systems, as well as guidelines for the ethical use of AI. | [37] |
| Biorepositories | Ethical guidelines and protocols as well as uniform methodological approaches and international standards are required. | [40] |
| Ethicists involvement | Ethicists should be involved in AI projects from the beginning. | [44,45] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





