1. Introduction
Smoking is known as a risk factor for many cardiovascular and respiratory diseases: active and passive smoking increase morbidity and premature mortality from lung cancer, acute coronary syndrome and respiratory diseases [
1,
2]. Smoking-related diseases are the cause of premature mortality and account for 87% of the total mortality in Russia.
A growing body of evidence from different countries indicates that tobacco control (TC) regulations, including bans on smoking in public places, can reduce hospital admissions for acute cardiovascular disease [3-6] and respiratory diseases [7-9], along with affecting the incidence of lung cancer in the long term [
10,
11].
Several studies discovered a reduction in hospital admission rate for acute lower respiratory tract infections in children, following the introduction of smoking bans in public places and other TC regulations [12-15]. Evidence of the effect of TC provisions on respiratory diseases in the general population showed mainly a reduction in hospital admission rates for exacerbations of chronic bronchitis, COPD or asthma [
16], while very few studies did so in relation to the admissions for pneumonia in adults [ 17].
Existing studies primarily assessed the impact of smoking bans in indoor public places on hospital admission rates. However, other TC measures may also affect hospital admission rate for smoking-related acute conditions. Besides, all of these studies evaluated the direct impact of TC measures on the monthly rate of hospital admissions for smoking-related conditions [4,12-14] over one or two years after the introduction of such laws, making it difficult to verify the long-term effects of TC legislation. Finally, very few studies estimated the impact of national TC legislation at both countrywide and regional levels [4,12-14], and none of them have done so in relation to compliance with these regulations.
In 2013 Russia introduced one of the most comprehensive TC laws in Europe, aimed at protecting public health from the effects of tobacco smoke and the consequences of smoking. In accordance with the provisions of the WHO Framework Convention on Tobacco Control (FCTC), the Russian Tobacco Control Law (RTCL) introduced a complete ban on smoking in indoor and outdoor public places, workplaces and all public transport; a ban on advertising, promotion and sponsorship of tobacco products, including open display of tobacco products at points of sale; restrictions on the retail sale of tobacco products, e.g., near educational facilities; annual increase in excise taxes on tobacco products; information-communication measures to raise awareness of health risks associated with tobacco use and passive smoking; and measures to help smokers quit smoking. These regulations aim to reduce the prevalence of smoking as well as smoking-related morbidity and mortality in the population. Despite the notable progress made by Russia after ratification of the FCTC, the prevalence of smoking is still high at 27.3%: 46.4% in men and 14.6% in women in 2018. We should note the slowdown in the rate of decrease in smoking prevalence by only 3.5% as compared with 2013, i.e., after 5 years of RTCL implementation. However, both the prevalence of smoking and its changes varied across different regions of Russia.
Hence, we hypothesized that the effects of RTCL on prevalence of smoking and its impact on public health may depend on the degree of enforcement and implementation of these regulations in the regions of Russia. We evaluated the implementation of the law by measuring the compliance with the TC regulations. With this goal in mind, we conducted an evaluation survey in 2017-2018 based on a random sample of 11,625 participants in 10 constituent entities of the Russian Federation. Our Russian Tobacco Control Policy evaluation survey was representative both for the entire country and for the regions. This survey established different levels of compliance with TC measures across the 10 regions. This survey established different levels of compliance with TC measures across the 10 regions. In some of these regions, e.g., Chuvash Republic, the results of the survey showed high compliance with smoking bans, existence of tax and price policies, and comprehensive support of smoking cessation. In other regions, such as Arkhangelsk Oblast, these measures were implemented to a lesser extent. Using the scoring system of the Tobacco Control Scale by L. Joossens and M. Raw [
18] and the results of our Russian Tobacco Control Policy evaluation survey, we developed an original scale to assess the implementation of the most cost-effective existing TC measures (viz., the WHO MPOWER provisions) in the regions of Russia, and we have named it the Tobacco Control Implementation Scale (TCIS) [
19]. Our previous studies demonstrated a significant relationship between TCIS scores and changes in smoking prevalence in 10 regions over a 5-year period after the introduction of RTCL [
20].
Our two previous studies assessed changes in monthly hospitalization rates for acute coronary events (ACE) in three regions of Russia and annual hospital admission rates for ACE in the entire country and 10 regions of Russia [
21,
22]. The latter study [
22] showed a significant reduction in hospital admissions for both angina and myocardial infarction (16.6% [RR 0.83, 95% CI 0.74–0.93] and 3.5% [RR 0.96, 95% CI 0.96 -0.97], respectively) after the nationwide introduction of RTCL vs. the period before the adoption of this law, as well as effects of varying magnitude in 10 regions. Regions with better enforcement of the TC law experienced greater reductions in hospital admission rates for angina and myocardial infarction.
In this study, we sought to analyse the impact of Russian TC regulations on hospital admission rates for all-cause pneumonia in adults, which may be especially important in an era of the COVID-19 pandemic or other viral infections. Also, we intended to analyse the extent of these effects in various regions of Russia in connection with the implementation of TC legislative measures.
2. Materials and Methods
2.1. Study design and data sources
We analysed hospitalization rates for all-cause pneumonia to compare periods before and after the adoption of RTCL in 2013, adjusting for possible confounding factors and long-term trends. We used an interrupted time series analysis to quantify the change in hospital admissions for pneumonia after the adoption of RTCL vs. the preceding period. To demonstrate that immediate and gradual changes in hospitalisation rates for pneumonia were associated with RTCL, we also analysed asthma hospitalization rates for comparison. We assumed that since asthma has been routinely and legitimately monitored and controlled for many years at the outpatient level, the effect of RTCL on hospital admission rates for asthma should not be apparent. Besides we analysed hospitalization rates for rheumatic heart disease for comparison, (as a disease not associated with smoking), which should not be affected by TCL, and which also has been routinely controlled like asthma at outpatient level. The models were based on the time series of annual hospitalizations for all three diseases in the Russian Federation and 10 regions over the period of 2005–2019.
We also analysed the change in hospital admission rates after the adoption of RTCL, compared with the pre-law period in 10 regions of Russia, depending on the degree of enforcement of the TC regulations. To compare regions with different levels of compliance with RTCL, we used the TCIS developed in our previous study [
19].
Annual data on hospital admissions for pneumonia and bronchial asthma in the adult population that occurred in Russia and its 10 regions between 2005 and 2019 were obtained from the national official hospital discharge statistics database, which included the following information: the diagnosis at discharge, age category (0-17, including 0-1, and ≥18 years old), and region of residence. Respiratory outcomes were defined according to the International Classification of Diseases-10 codes for all-cause pneumonia (J12-18) and asthma (J45, J46).
We analysed the changes in the rate of hospitalization for pneumonia per 100,000 adult residents (aged ≥18 years) in the Russian Federation and its 10 constituent entities: the Chuvash Republic, Krasnodar and Primorsky Krais, and Arkhangelsk, Astrakhan, Belgorod, Novosibirsk, Orenburg, Samara and Tyumen Oblasts.
Smoking prevalence in years 2013, 2018 and 2019, was taken from the population surveys database of the Federal State Statistics Service; population data by age group (0-17 years and ≥18 years), as well as data on as hospital bed-population ratio were taken from the official statistics of Federal State Statistics Service [23-25].
2.2. Tobacco Control Implementation Scale
To compare changes in the hospital admission rate for pneumonia before and after the adoption of RTCL in different regions in terms of adherence to TC regulations, we used the scores of TCIS [
19]. The scale indicates how well the six MPOWER activities were implemented in each investigated region. Table 1 in
Appendix A shows how the scale applies to the 10 Russian regions, where the investigation was carried out and the ranks of the regions according to the scores of TCIS, characterising the performance of the MPOWER measures in each of the region.
The scores characterising the performance of the MPOWER package and each of its six measures were used as independent variables in the correlation and linear regression analyses [19-20].
2.3. Statistical data processing
We used standard methods for interrupted time series (ITS) to evaluate the effects of RTCL [
26]. The immediate effect was modelled as a step function including an indicator variable that changed after 2013, whereas the gradual effect was investigated via an interaction term between the RTCL impact and time. We employed generalized Poisson regression model with calculation of the incidence rate ratio (RR) and 95% confidence interval (95% CI) to estimate the immediate and long-term effects of RTCL.
The following regression model was used:
where Yt — represents the outcome at time t.; T — is the time elapsed since the start of the study in with the unit representing the frequency with which observations are taken (year); Xt — a dummy variable indicating the pre-intervention period (coded 0) or the post-intervention period (coded 1); β
0 represents the baseline level at T= 0, β
1 is interpreted as the change in outcome associated with a time unit increase (representing the underlying pre-intervention trend), β
2 is the level change following the intervention and β
3 indicates the slope change following the intervention (using the interaction between time and intervention: TXt ).
Scaling corrections were applied to the model to avoid overdispersion and misestimation of standard errors. The models were also tested for autocorrelation.
To assess the relationship of between the relative change in hospital admission rates after the adoption of RTCL (%) and smoking prevalence rates in each region (dependent variable) and scores characterizing the degree of implementation of TC legislative measures (independent variable), we performed Spearman’s rank correlation analysis and linear regression analysis.
The analyses were carried out using the Stata v.11.2. statistical software.
3. Results
A total of 5,785,673 hospital admissions for pneumonia and 2,575,561 for bronchial asthma occurred among the Russian population during the study period. Of these, 2,395,953 cases of pneumonia and 865,994 cases of asthma were detected after the adoption of RTCL in 2013.
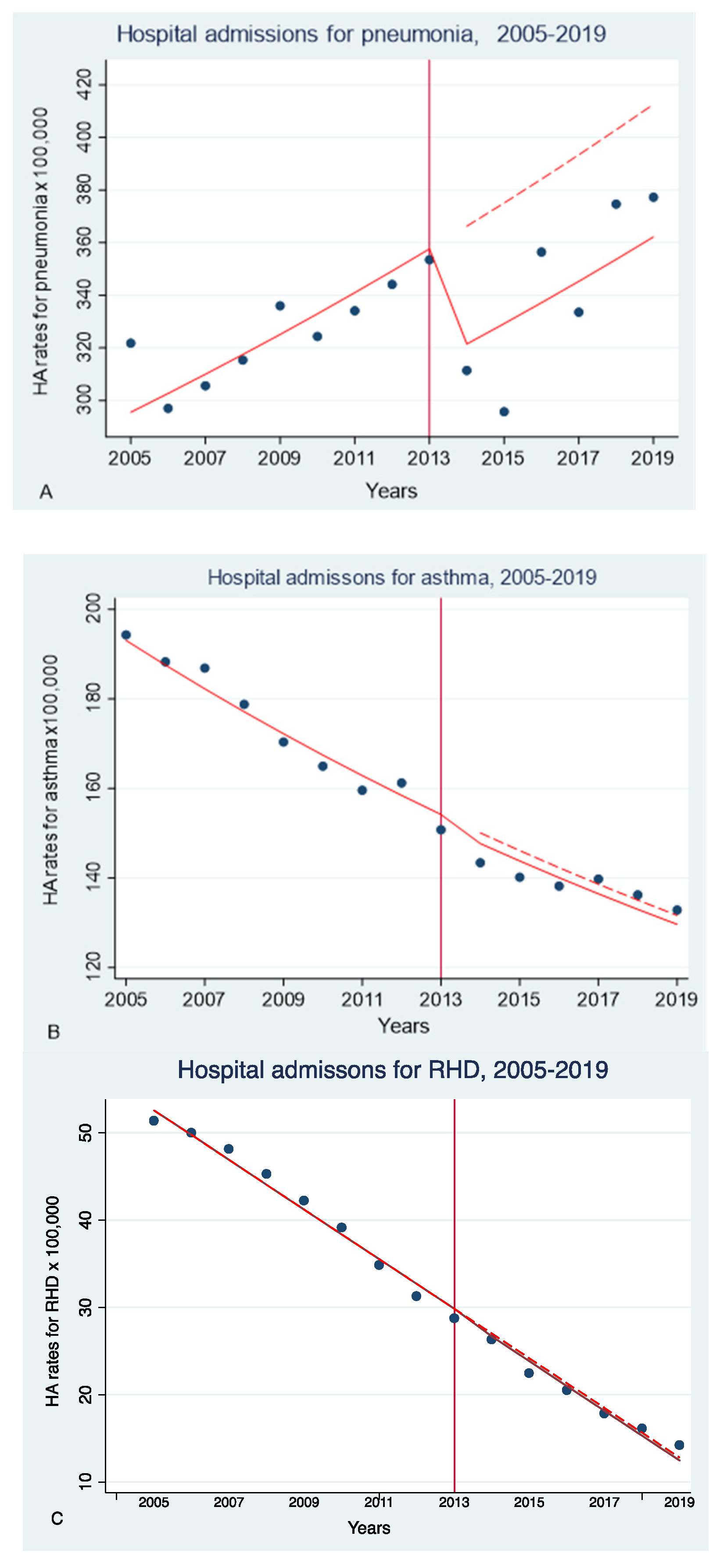
Figure 1 presents data on annual age-adjusted hospital admission rates for pneumonia, bronchial asthma and rheumatic heart disease per 100,000 residents from 2005 to 2019 in Russia. These data are shown in
Figure 1 by year, along with the predicted regression curves. The figure demonstrates the trends in annual hospital admission rates for pneumonia (1A) and asthma (1B) in the Russian Federation from 2005 to 2019, i.e., before and after the introduction of RTCL in 2013. Dynamics of hospitalization rates after the introduction of RTCL (solid line) in comparison with the predicted trend without TC measures (dashed line) is shown in
Figure 1 as well.
We observed a significant decrease in hospital admission rates for pneumonia by 14.3% after the adoption of RTCL (2014-2019), compared with the pre-law period (2005-2013): the RR was 0.88 (95% CI 0.79–1.00) (p=0.01).
We also revealed evidence of a gradual effect of RTCL: change in the main trend of hospital admission rate for pneumonia after 2013: RR=0.86 (95% CI 0.77-0.96) (p=0.006).
As for asthma and rheumatic heart disease, there was no statistically significant reduction in hospital admission rates after the adoption of RTCL vs. the preceding period: RR=1 (95% CI 0.97-1.1) (p=0.779) and RR=0.94 (95% CI 0.83-1.06) (p=0.332).
Secondary analyses conducted among the adult population in 10 constituent entities of Russia yielded similar effects of RTCL in different regions. However, these effects had different magnitudes, and the decrease in the hospital admission rates for pneumonia after the adoption of RTCL was statistically significant in only 4 out of 10 regions (Table 1).
Also, adjusting for factors potentially affecting hospital admission rates, such as hospital bed-population ratio, did not significantly change the results.
Table 1 demonstrates changes in hospital admission rates for pneumonia after the adoption of RTCL, compared with the preceding period, in 10 regions of the Russian Federation.
Table 1.
Changes in hospitalisation rates for all-cause pneumonia after the adoption of RTCL compared with the preceding period
Table 1.
Changes in hospitalisation rates for all-cause pneumonia after the adoption of RTCL compared with the preceding period
| Federal subjects of Russia |
IRR (95% CI) |
p |
Relative change IRR(%) |
| The Russian Federation |
0.88 (0.79-0.97) |
0.011 |
-14.3 |
| The Chuvash Republic |
0.75 (0.62-0.91) |
0.003 |
-27.5 |
| Krasnodar Krai |
0.98 (0.8-1.2) |
0.863 |
-4.0 |
| Primorskyi Krai |
1.01 (0.99-1.03) |
0.694 |
1.1 |
| Arkhangelsk Oblast |
0.88 (0.77-0.99) |
0.04 |
-14.7 |
| Astrakhan Oblast |
0.88 (0.72-1.08) |
0.224 |
-17.8 |
| Belgorod Oblast |
0.77 (0.6-0.98) |
0.033 |
-27.4 |
| Novosibirsk Oblast |
0.96 (0.79-1.16) |
0.681 |
-4.6 |
| Orenburg Oblast |
0.93 (0.76-1.14) |
0.512 |
-10.4 |
| Samara Oblast |
0.72 (0.63-0.82) |
0.000 |
-32.4 |
| Tyumen Oblast |
0.88 (0.67-1.2) |
0.353 |
-13.2 |
Thus, we hypothesized that the degree of reduction in hospital admission rates after the adoption of the RTCL vs. the preceding period in the regions may be related to the degree of this law enforcement.
To check this hypothesis, we measured the correlations and the associations between the relative changes of hospital admission rates for all three conditions and the TCIS scores characterising the extent of the implementation of TCL measures in the 10 regions by conducting Spearman’s correlation analysis and a linear regression analysis.
Table 2 presents the correlations of reduction in the rate of hospital admissions for pneumonia (RR%) with the degree of implementation of six MPOWER measures in 10 regions of Russia based on the TCIS scoring system (
Appendix A, Table 1).
We detected significant correlations between the reduction in hospital admission rates for pneumonia and TCIS scores for smoking ban rsp=-0.55 (95% CI -1.08, 0.02) (p=0.042) and for offering support in smoking cessation: rsp=-0.763 (95% CI -1.11, -0.41) (p<0.001).
An inverse correlation was also established between the decrease in hospital admission rate for pneumonia and the prevalence of smoking in 2019 in the regions: rsp=0.7 (95% CI -0.08, 2.25 (p<0.05).
Linear regression analysis yielded significant associations of the decrease in hospital admission rates for pneumonia (RR%) with the TCIS score for offering smoking cessation support (β=-4.21; 95% CI -7.61, -0.82; p=0.02), as well as with the prevalence of smoking in 2019 (β=2.40; 95% CI 0.34, 4.45; p=0.027). Both relationships were significant for pneumonia, but not for asthma (
Table 3).
We did not reveal any statistically significant correlations, or significant associations between the reduction in the rates of hospital admissions for asthma and rheumatic heart disease and the extent of implementation of either TCL measures or smoking prevalence in 10 regions of Russia.
4. Discussion
Our analysis, based on nearly six million hospital admissions, showed for the first time the long-term (over 15 years) trends of annual hospitalisation rates for all-cause pneumonia. We established a reduction in the rates of hospital admission for all-cause pneumonia among the adult population over the entire study period after the adoption of a comprehensive TC law in Russia. The observed decrease was similar across regions of Russia and was stronger in constituent entities with better compliance with TC regulations.
Our findings are consistent with several previously published studies demonstrating a reduction in hospital admissions for acute lower respiratory tract infections associated with adoption of a municipal or national smoking ban. A. Nyman et al. observed a 33% decrease in hospital admissions for respiratory diseases during a restaurant ban in Toronto [
16]. A study by J.-P. Humair et al. demonstrated that smoking bans resulted in a very significant reduction in hospitalizations for exacerbations of COPD and no significant changes in hospital admissions for pneumonia and acute asthma in the Canton of Geneva [
27]. However, changes in hospitalization rates in these studies were limited to the short period of smoking ban introduction and did not extend to the longer period after the ban. V. Ho et al. described the association of smoking bans, as well as higher excise taxes on cigarettes, with reduced rates of hospital admission for pneumonia in individuals 60 to 74 years of age in a nationwide study conducted in the USA [
17].
Unlike most previous studies on smoking bans, we measured the relationship between implementation of a comprehensive TC law and hospitalization rates nationwide. In addition, by analysing data on the implementation of RTCL in 10 constituent entities of the Russian Federation, we determined which of the TC measures had the greatest impact on reducing hospitalization rates for pneumonia among adults.
In our study, we assessed the gradual effect of reduced hospital admissions for pneumonia depending on the degree of enforcement of RTCL in 2017-2018. Our results implied that more effective implementation of anti-tobacco measures in the regions and the degree of their enforcement in 2017-2018 (assuming they were similar from the first year of RTCL adoption) could affect the change in rates of hospitalization for pneumonia.
Because we were looking at annual rather than monthly hospitalization rates, there was no need to adjust the models for seasonality. However, we adjusted the model for potential confounders, such as hospital bed-population ratio, which did not affect the results in any way.
TC regulations aim to reduce the prevalence of smoking and smoking-related morbidity and mortality in the long term. L. Palmieri et al. demonstrated a reduction in smoking prevalence in Italy from 31.7% to 21.8% between 1980 and 2000, which led to a decrease in mortality from coronary heart disease [
28]. Smoking is a risk factor for developing pneumonia. A meta-analysis by V. Baskaran et al. showed that current smokers and ex-smokers were 2.7 and 1.5 times, respectively, more likely to develop community-acquired pneumonia, compared to ‘never smokers’ [
29]. Their other finding was that current heavy smokers had a significantly higher risk of developing pneumonia than light smokers.
Our study suggests that greater relative changes in smoking prevalence over the 5-year period of RTCL implementation (2013-2018) and lower smoking prevalence in 2019 may be associated with lower hospitalization rates for pneumonia and better RTCL enforcement.
There are some strengths and limitations of the study that should be mentioned.
Among the strengths of this study, we should mention its large sample size encompassing all nationwide hospital admissions for pneumonia over a 15-year period. It explored the immediate and long-term impact of comprehensive tobacco control legislation on all-cause pneumonia in adults, which were not previously studied. In addition, relationships between the impact of comprehensive RTCL and individual legislative measures on hospitalization rates and the degree of implementation of these measures in different regions, based on large representative survey data, were investigated, which increased the strength of our study as well.
The limited number of investigated regions can be seen as a limitation of the study in terms of its ability to explore possible relationships in correlation and linear regression analyses. However, despite the limited number of regions, we still revealed statistically significant relationships.
Another limitation of our study is related to the data of a representative survey of the population assessing the Russian Tobacco Policy in 10 constituent entities of the Russian Federation. We assumed that the degree of compliance with anti-tobacco regulations, measured in 2017-2018 in 10 regions of Russia, was similar over the entire study period starting from the first year of RTCL adoption.
5. Conclusions
The results of this study conducted on a large population sample over a long follow-up period suggest that a comprehensive tobacco control policy can lead to an immediate reduction in hospital admission rate for all-cause pneumonia with a gradual effect. This finding has important public health implications, especially in the era of the COVID-19 pandemic and/or other viral infections. Smoking regulations represent a simple, effective and inexpensive way to prevent respiratory diseases, and the degree of compliance with the regulations can be important for the prevention of these ailments.
Author Contributions
Conceptualization, M.G. and A.K.; methodology, M.G. and A.K..; formal analysis, M.G.; investigation, M.G.; resources, A.K.; writing—original draft preparation, M.G.; writing—review and editing, M.G. and A.K.; supervision, O.D.; project administration, A.K.; O.D.; funding acquisition, O.D.
Funding
This research received no external funding.
Institutional Review Board Statement
The study did not require ethical approval.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the Russian Tobacco Control Evaluation Survey, the results of which are used in this study. The database on hospital admissions do not contain personal data.
Data Availability Statement
Data on annual hospital admissions are not public: they are obtainable from the official national official hospital discharge statistics database at the Data centre the Russian Research Institute of Health. For this study, hospital admission data were provided by the Russian Research Institute of Health upon official request. Data on smoking prevalence for years 2013, 2018 and 2019 were obtained from Population Surveys of the Federal State Statistics Service, provided upon request. Population data, by age group (0-17 years and ≥18 years), data on hospital bed-population ratio were taken from the Federal State Statistics Service official database available on the website of the Federal State Statistics Service:
https://gks.ru/bgd/regl/b20_14p/Main.htm
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Table 1.
Ranking of 10 Russian federal subjects by the Tobacco Control Implementation Scale.
Table 1.
Ranking of 10 Russian federal subjects by the Tobacco Control Implementation Scale.
| |
Tax and price measures in tobacco control |
Protection from tobacco smoke |
Information and communication measures |
Rising awareness about tobacco advertising and promotion |
Warning signs |
Offering help for smoking cessation |
All measures |
| Maximum possible score |
30 |
22 |
15 |
13 |
10 |
10 |
100 |
| All regions |
17.0 |
19.6 |
12.7 |
11.2 |
7.7 |
5.8 |
73.9 |
| The Chuvash Republic |
28.9 |
21.1 |
14.25 |
13.0 |
6.4 |
9.5 |
93.1 |
| Astrakhan Oblast |
25.2 |
20.7 |
12.9 |
11.9 |
7.5 |
7.5 |
85.8 |
| Orenburg Oblast |
16.4 |
18.2 |
14.3 |
11.0 |
8.3 |
4.8 |
73.0 |
| Primorskyi Krai |
19.1 |
19.3 |
11.5 |
11.2 |
7.7 |
3.7 |
72.5 |
| Krasnodar Krai |
15.9 |
17.8 |
13.8 |
11.0 |
8.4 |
5.3 |
72.3 |
| Novosibirsk Oblast |
17.0 |
20.6 |
11.0 |
11.3 |
7.4 |
4.6 |
71.9 |
| Samara Oblast |
15.6 |
18.4 |
12.5 |
10.2 |
7.6 |
7.3 |
71.6 |
| Belgorod Oblast |
14.2 |
21.5 |
12.2 |
9.7 |
8.3 |
5.1 |
70.8 |
| Arkhangelsk Oblast |
17.2 |
18.0 |
13.1 |
10.4 |
7.7 |
3.9 |
70.3 |
| Tyumen Oblast |
9.6 |
20.7 |
13.5 |
11.7 |
7.7 |
6.4 |
69.5 |
References
- Carreras G, Lugo A, Gallus S, et al. Burden of disease attributable to second-hand smoke exposure: A systematic review. Prev Med. 2019; 129105833. [CrossRef]
- Goodchild M, Nargis N, Tursan d'Espaignet E. Global economic cost of smoking-attributable diseases. Tob Control. 2018 Jan;27(1):58-64. [CrossRef]
- Christensen TM, Møller L, Jørgensen T, Pisinger C. The impact of the Danish smoking ban on hospital admissions for acute myocardial infarction. Eur J Prev Cardiol. 2014 Jan;21(1):65-73. [CrossRef]
- Séguret F, Ferreira C, Cambou JP, Carrière I, Thomas D. Changes in hospitalization rates for acute coronary syndrome after a two-phase comprehensive smoking ban. Eur J Prev Cardiol. 2014 Dec;21(12):1575-82. [CrossRef]
- Cox B, Vangronsveld J, Nawrot TS. Impact of stepwise introduction of smoke-free legislation on population rates of acute myocardial infarction deaths in Flanders, Belgium. Heart. 2014 Sep 15;100(18):1430-5. [CrossRef]
- Barone-Adesi F, Gasparrini A, Vizzini L, Merletti F, Richiardi L. Effects of Italian smoking regulation on rates of hospital admission for acute coronary events: A country-wide study. PLoS One. 2011; 6(3): e17419. [CrossRef]
- Kent BD, Sulaiman I, Nicholson TT, Lane SJ, Moloney ED. Acute pulmonary admissions following implementation of a national workplace smoking ban. Chest. 2012;142(3):673–679. [CrossRef]
- Humair JP, Garin N, Gerstel E, Carballo S, Carballo D, Keller PF, Guessous I. Acute respiratory and cardiovascular admissions after a public smoking ban in Geneva, Switzerland. PLoS One. 2014 Mar 5;9(3):e90417. [CrossRef]
- Galán I, Simón L, Flores V, Ortiz C, Fernández-Cuenca R, Linares C, Boldo E, Medrano MJ, Pastor-Barriuso R. Assessing the effects of the Spanish partial smoking ban on cardiovascular and respiratory diseases: methodological issues. BMJ Open. 2015 Dec, 1;5(12):e008892. [CrossRef]
- Kabir Z, Caputi TOP89 The impact of smoke-free legislation in ireland on lung cancer incidence and mortality. J Epidemiol Community Health. 2019;73:A44;. [CrossRef]
- Gredner T, Mons U, Niedermaier T, et al. Impact of tobacco control policies implementation on future lung cancer incidence in Europe: An international, population-based modeling study. The Lancet Regional Health – Europe. 2021;4. [CrossRef]
- Been JV, Millett C, Lee JT, van Schayck CP, Sheikh A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections. Eur Respir J. 2015 Sep;46(3):697-706. [CrossRef]
- Been JV, Szatkowski L, van Staa TP, Leufkens HG, van Schayck OC, Sheikh A, de Vries F, Souverein P. Smoke-free legislation and the incidence of paediatric respiratory infections and wheezing/asthma: interrupted time series analyses in the four UK nations; [CrossRef]
- Been JV, Mackay DF, Millett C, Soyiri I, van Schayck CP, Pell JP, Sheikh A. Smoke-free legislation and paediatric hospitalisations for acute respiratory tract infections: National quasi-experimental study with unexpected findings and important methodological implications. Tob Control. 2018 Oct;27(e2):e160-e166. [CrossRef]
- Turner S, Mackay D, Dick S, Semple S, Pell JP. Associations between a smoke-free homes intervention and childhood admissions to hospital in Scotland: An interrupted time-series analysis of whole-population data. Lancet Public Health. 2020 Sep;5(9):e493-e500. [CrossRef]
- Naiman A, Glazier RH, Moineddin R. Association of anti-smoking legislation with rates of hospital admission for cardiovascular and respiratory conditions. CMAJ. 2010 May 18;182(8):761-7. [CrossRef]
- Ho V, Ross JS, Steiner CA, Mandawat A, Short M, Ku-Goto MH, Krumholz HM. A Nationwide assessment of the association of smoking bans and cigarette taxes with hospitalizations for acute myocardial infarction, heart failure, and pneumonia. Med Care Res Rev. 2017 Dec; 74(6): 687–704. [CrossRef]
- Joossens L., Raw M. The Tobacco Control Scale: A new scale to measure country activity. Tobacco Control. 2006;15:247–253. [CrossRef]
- Gambaryan MG, Drapkina OM. Integrated scale for assessing the implementation of the Federal Tobacco Control Law in the Russian regions. The Russian Journal of Preventive Medicine. 2020;23(6):50-9. (In Russ.). [CrossRef]
- Gambaryan MG, Drapkina OM. The effectiveness of implementing tobacco control legislative measures in relation to the smoking prevalence in 10 constituent entities of the Russian Federation from 2013 to 2018. The Russian Journal of Preventive Medicine. 2021;24(2):44-51. (In Russ.). [CrossRef]
- Kontsevaya AV, Agishina TA, Gambaryan MG, et al. Impact of anti-tobacco policy measures on hospitalization rates for acute myocardial infarction and unstable angina in three Russian regions. Human Ecology. 2020;5:37-44. (In Russ.);. [CrossRef]
- Gambaryan MG, Kontsevaya AV, Agishina TA, Drapkina OM.Assessing the effectiveness of legislative measures for tobacco control in relation to reducing in-hospital incidence of angina pectoris and myocardial infarction in the Russian Federation and its 10 constituent entities. Cardiovascular Therapy and Prevention. 2021;20(6):2911. (In Russ.). [CrossRef]
- Federal State Statistics Service. Regions of Russia. Socioeconomic indicators — 2020. (In Russ.) https://gks.ru/bgd/regl/ b20_14p/Main.htm. https://gks.ru/bgd/regl/b20_14p/Main.htm.
- Federal State Statistics Service. The results of selective observation of behavioural factors affecting the health of the population in 2013 and 2018. (In Russ.); https://www.gks.ru/free_doc/new_site/ZDOR/Factors2018_2812/index.html.
- Federal State Statistics Service. Results of selective monitoring for the health status of the population in 2019. (In Russ.); https://gks.ru/free_doc/new_site/ZDOR/Sdp2013.Bfs.Publisher/index.html, https://gks.ru/free_doc/new_site/ZDOR/2019/PublishSite/index.html.
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Internat J Epidemiol. 2017;46(1):348-55. [CrossRef]
- Humair J-P, Garin N, Gerste E, et al. Acute respiratory and cardiovascular admissions after a public smoking ban in Geneva, Switzerland. PLoS One. 2014; 9(3): e90417. [CrossRef]
- Palmieri L, Bennett K, Giampaoli S, Capewell S. Explaining the decrease in coronary heart disease mortality in Italy between 1980 and 2000. Am J Public Health. 2010; 100: 684–692;. [CrossRef]
- Baskaran V, Murray RL, Hunter A, Lim WS, McKeever TM. Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PLoS One, 2019; 14(7): e0220204. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).