1. Introduction
Temporomandibular joint disorders (TMD) are a group of dysfunctions that appear to be of multifactorial origin, affecting the temporomandibular joint (TMJ), masticatory muscles, and adjacent structures [
1,
2]. Nowadays, TMD are considered the most frequent cause of chronic orofacial pain of non-dental origin and the third stomatological disorder leading to pain and disability. In addition, myofascial TMD is documented as the most frequent sub-type, followed by internal derangements such as disc displacement and arthralgia [
3,
4].
TMD affect a considerable part of the population. According to population-based studies, TMD can affect any populational group. The reported pain and dysfunction prevalence is significantly higher in women and younger subjects. However, TMD signs seem to increase with age [
1,
2,
5].
Psychosocial, environmental, biological, and neurophysiological factors are considered etiological entities significantly associated with TMD symptoms. Factors such as emotional stress (anxiety and depression), bruxism, occlusal disharmony, orthodontic treatment, masticatory dysfunction, and postural deviation are reported to increase the risk for TMD [
1,
4,
5].
The most prominent symptoms are restricted joint function with alteration of the mandibular physiological dynamics, muscular or articular pain that intensifies with mastication, headache, and TMJ noises. Limited mandibular range of motion, pain, crepitation, or clicking in TMJ palpation are all common signs of TMD assessed during a clinical examination [
1,
2].
This study attempts to evaluate and analyze the prevalence of TMD clinical signs and symptoms in a Portuguese TMD department and their association with various sociodemographic and individual factors such as age, gender, oral behaviors, risk factors and other comorbidities.
2. Materials and Methods
2.1. Database description
EUROTMJ is an online electronic medical database that allows data collection from patients with TMD (
Figure 1). The patient data is encrypted and only accessible through a password attributed to the clinician. The database works in the English language. EUROTMJ displays a tree format table content (
Figure 1). The database is constituted with different menus: general data (patient ID, employment status, comorbidities, daily medication, drug allergy); TMJ history (complaints, risk factors, past treatments, VAS Pain, TMJ click, Life impact/habits; clinical evaluation; exams, diagnosis, clinical resume, notes); questionnaires (SF-36, HADS, EQ-5D, OHIP-14, WHO, Fonseca, Pain Screener, GAD-2, PHQ-2); Treatments (Proposed treatments); Clinical Evaluation (evolution charts, evolution table).
2.2. Study Design and data collection
A 3-year prospective study was conducted in a Portuguese TMD department from the 1st of August 2019 to the 1st of August 2022. This study was approved by the Instituto Português da Face ethics committee (PT/IPFace//RCT/0822/01). All enrolled patients gave their informed consent in writing, following current legislation. The inclusion criteria were: (1) registration of all the variables under study in a first consultation; (2) clinical diagnosis of TMD. The exclusion criteria were: (1) severe medical problems or impaired cognitive capacity. All patients with inclusion criteria over these three years were included. Descriptive data and clinical outcomes were registered in EUROTMJ. Demographic data (date of birth and gender) was recorded. In the first consultation, patients were instructed to answer questions regarding their complaints (TMJ pain, TMJ clicking, TMJ crepitus, Limited Mouth Opening, Masticatory Muscles tension, Cervical Muscles Tension, Tinnitus, TMJ edema, Vertigo) and laterality (when applicable) and duration of the symptoms (<3M; 3M-1Y; 1Y-5Y >5Y). They were also asked about parafunctional habits in their daily life, such as bruxism and clenching. A clinical record registered other comorbidities and potential risk factors for TMD. The TMJ pain recording was accessed in the right and left joints through the Visual Analog Scale (VAS, 0-10, with 0 being no pain; 1-3:mild, 4-6: moderate, and 7-10 severe pain). The VASLIFE was accessed by asking: “If you could give a life impact score to your TMJ problem on a 0 to 10 scale, where 0 means no impact, and 10 means the maximum impact possible, what would be your score?”. In clinical evaluation, maximum mouth opening (MMO, mm), the presence of clicks, crepitus, arthralgia (right and left joint), and myalgia was recorded. MMO was accessed using a certified ruler between the incisor’s teeth (TheraBite Jaw ROM Scale). Limited mouth opening was defined as encountered when: (1) patients perceived a limitation in their mouth opening; (2) clinical observation in difficulty in mouth opening; (3) using the cut-off of MMO<40 mm [
6,
7]. Myalgia was diagnosed according to a positive clinical history for: (1) in the past 30 days, pain in the jaw, in front or directly in the ear, with confirmation of pain through palpation of the masticatory muscles by the examiner and (2) accompanied pain with jaw movement, function or parafunction and a positive clinical evaluation for palpation pressure (5 seconds/1kg pressure) in masseter and temporalis muscles as defined in DC/TMD [
6,
7]. Myalgia was graded accordingly with pain intensity in each muscle: 0 = No Pain/Pressure Only; 1 = Mild Pain; 2 = Moderate Pain; 3 = Severe Pain [
8]. Arthralgia was reported if verified: (1) history of pain in the TMJ area and (2) accompanied pain with jaw movement, function, or parafunction [
6,
7]. The level of TMJ arthralgia was registered through the pain on palpation of the lateral pole or around or pain on maximum unassisted or assisted opening, lateral or protrusive movements. The same clinician (D.F.A.) performed the clinical evaluation for all patients.
2.3. Statistical Analysis
Data were analyzed using GraphPad Prism (v9) and IBM SPSS (v26) software. The variables were expressed as the mean (± standard deviation (SD)) or frequency (%). The biserial correlation Pearson Test (rpb) assessed the variables’ correlation. The non-parametric Chi-square test (χ2 ) was used to determine the associations' presence, and its intensity was measured by Cramér's V Coefficient (φc). The significance level set was 5%. For a graphic representation of risk factors and other comorbidities, a percentage >1% was considered. P-value < 0.05 was considered statistically significant.
3. Results
A total of 595 patients were registered in the EUROTMJ database. The mean age was 38.20±15.73 years at the first visit, 479 (80.50 %) of whom were female gender (
Table 1). 86.39% of the patients presented symptoms bilaterally, while 6.89% and 6.72% presented only on the right and left, respectively.
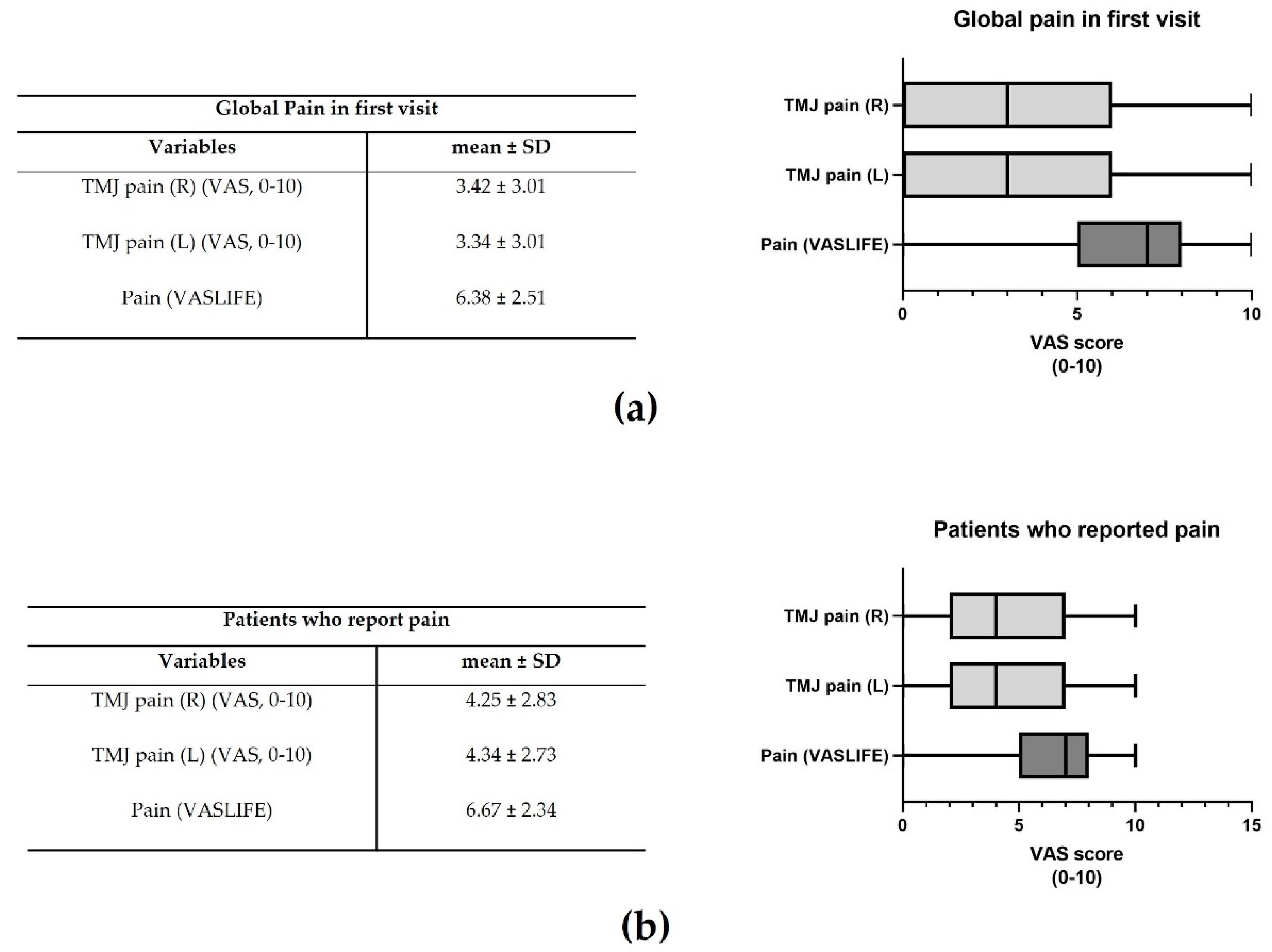
The mean global TMJ pain in the right and left joints was 3.42±3.01 and 3.34±3.01, respectively (
Figure 2a). The impact on life (VASLIFE) was 6.38±2.51 (
Figure 2a).
Considering only those patients who presented pain, pain right and left was 4.25±2.83 and 4.34±2.73, whereas VASLIFE was 6.67±2.34 (
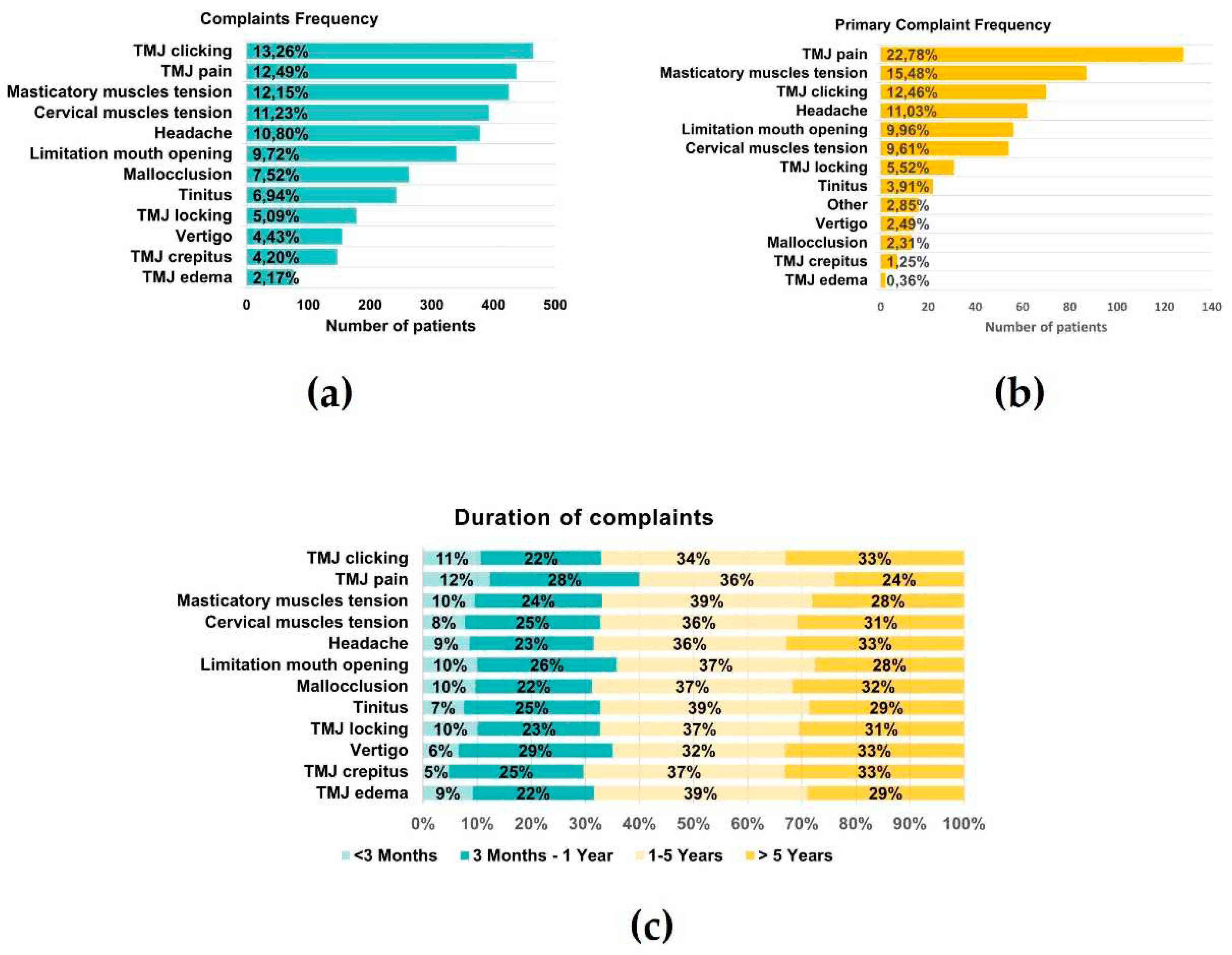
Figure 2b). The main complaints of the patients were TMJ clicking (13.26%), TMJ pain (12.49%), and masticatory muscle tension (12.15%), while the least frequent were vertigo (4.43%), crepitus (4.20%) and edema (2.17%) (
Figure 3a). However, considering the patient's main complaint, the one which presented the higher predominance was TMJ pain (22.78%) (
Figure 3b). There was also a high prevalence of symptom duration between 1-5 years (32%-39%) and over five years (24%-33%), while a low frequency of symptoms under 3 months was verified (5-12%) (
Figure 3c).
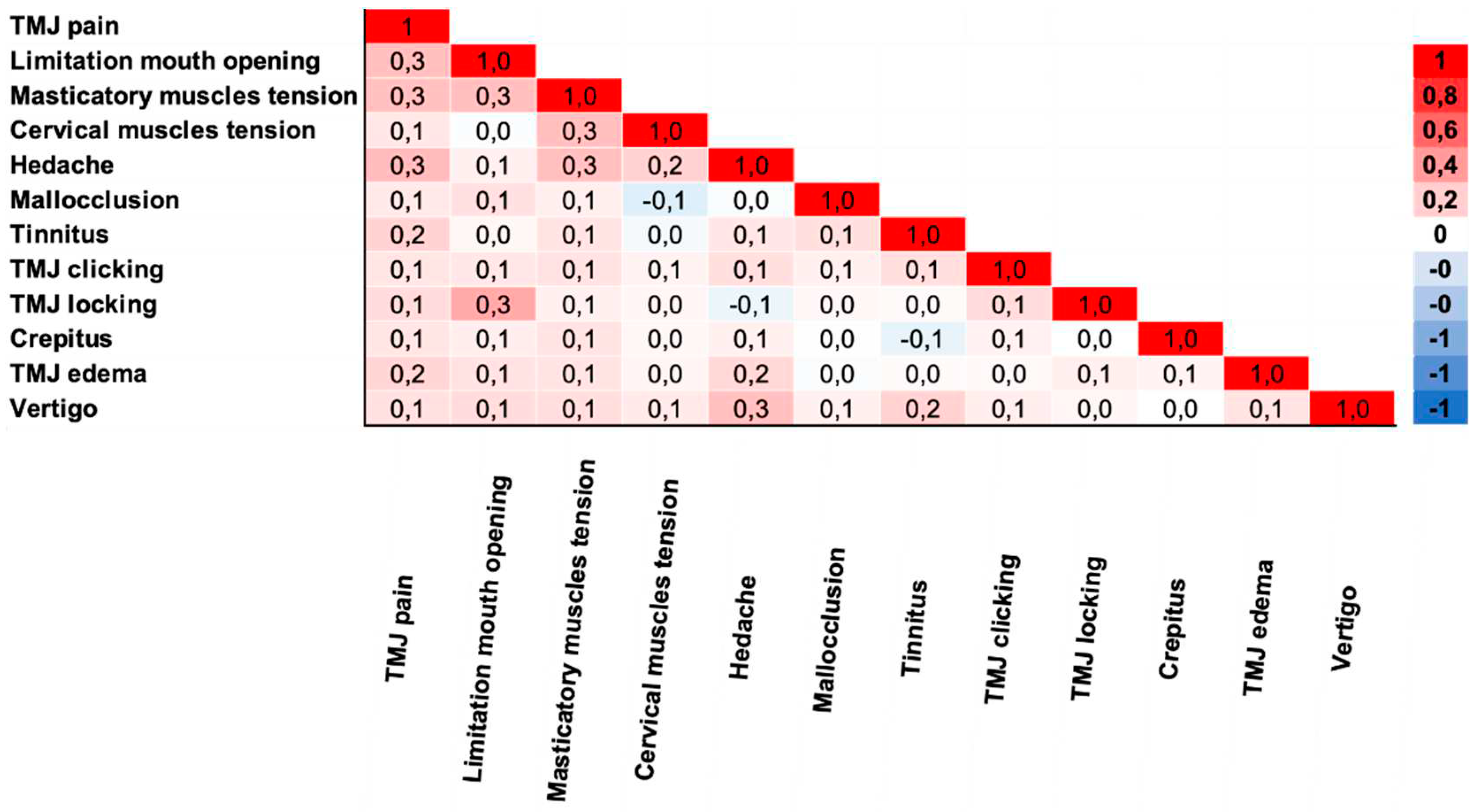
The correlation of complaints was analyzed in
Figure 4. TMJ pain was moderately correlated with limited mouth opening, masticatory muscle tension, and headache (rpb=0.3). TMJ pain also had a small correlation with other complaints (rpb=0.1-0.2). Limitation of mouth opening was moderately correlated with TMJ locking and masticatory muscle tension (rpb =0.3). Masticatory muscle tension was moderately correlated with headache and cervical muscle tension (rpb=0.3). Additionally, the headache was a moderate correlation with vertigo (rpb =0.3).
Regarding parafunctional habits, 180 (30%) of the patients answered that they perform bruxism, 138 (23%) at night, 35 (6%) at day and night, and 7(1%) during the day. On the other hand, 212 (36%) said that they do not perform, and 203 (34%) do not know (
Table 2). Regarding clenching, 359 (60%) of the patients answered that they do it, while 159 (27%) did not, and 77(13%) did not know.
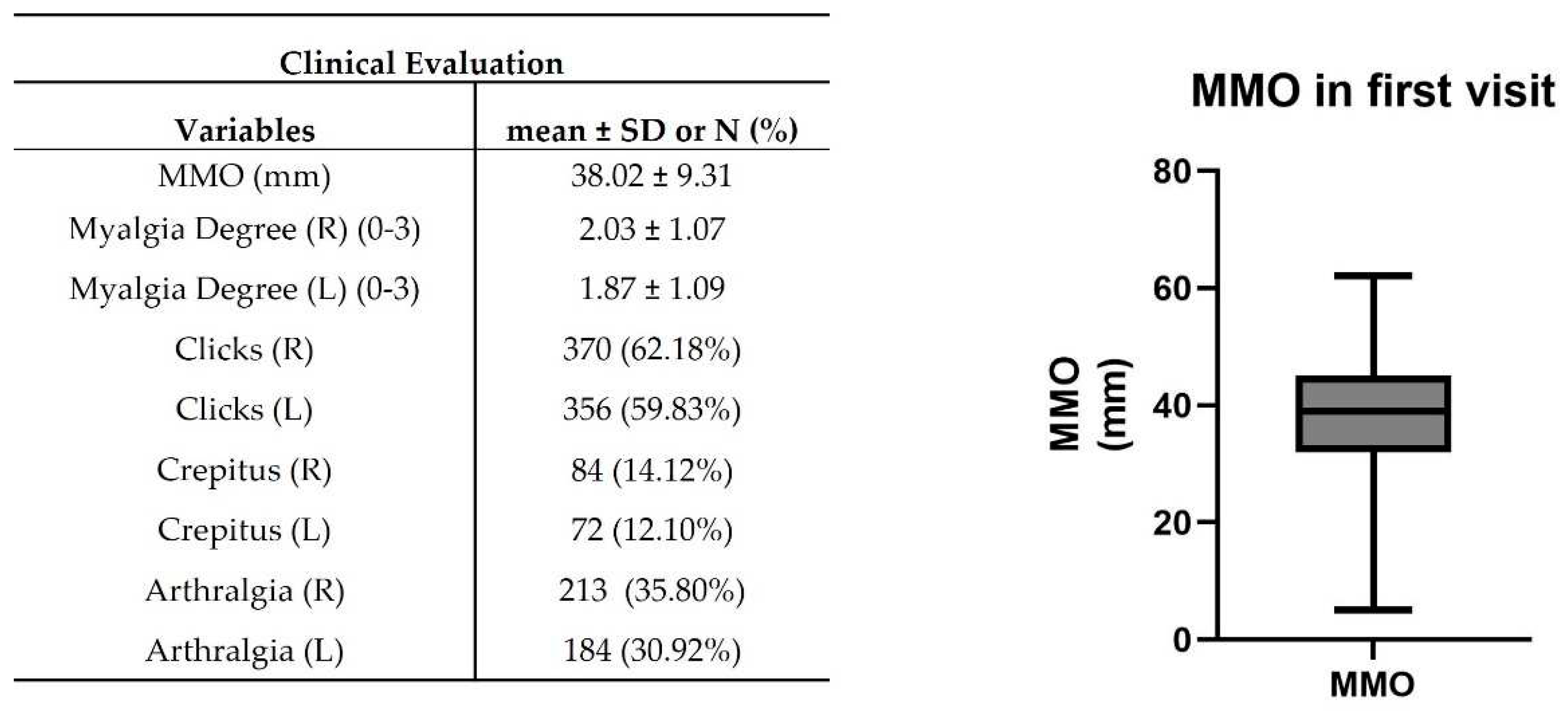
In clinical evaluation, patients presented 38±9.31 mm of MMO (
Figure 5). The mean myalgia degree was 2.03±1.07 and 1.87±1.09 on the right and left sides, respectively. 370 (~62%) and 356 (~60%) patients presented clicks in the right and left TMJ, while in 84 (~14%) and 72 (~12%) patients were verified crepitus (
Figure 5). A suggestive pain indicative of arthralgia was detected in 213 (~36%) and 184 (~31%) in the right and left TMJ (
Figure 5).
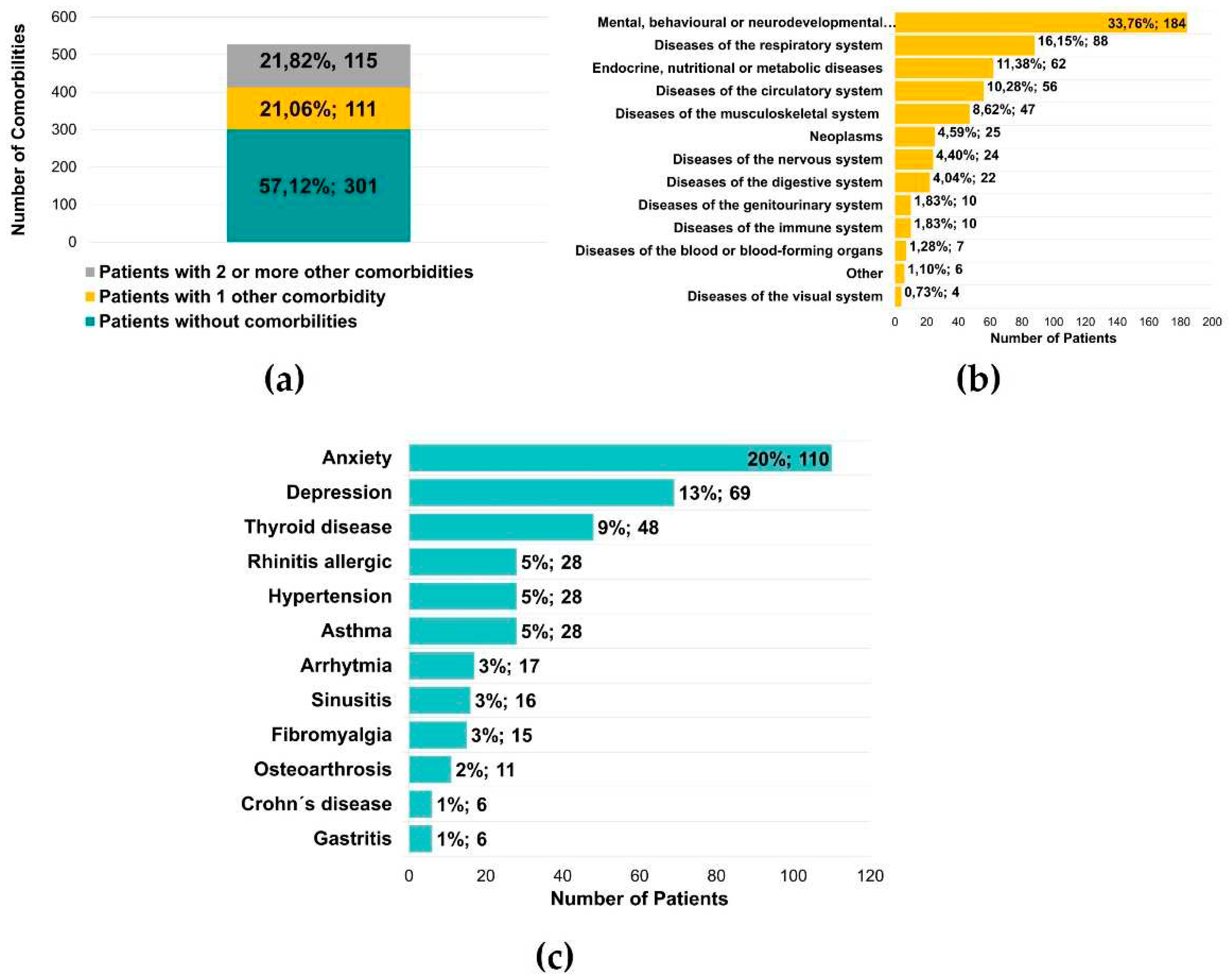
Five hundred twenty-seven patients were also questioned regarding the diagnosis of other diseases, and it was found that 226 (42.88%) of the patients had another illness, with 111 (21.06%) with one condition and 115 (21.82%) with two or more diseases (
Figure 6a). In 545 reported conditions, there was a significant predominance of mental, behavioral, or neurodevelopmental disorders (184 patients, 33.76%) (
Figure 6b). These values were supported by the diagnosis of anxiety and depression, verified in 110 (20%) and 69 (13%) patients, respectively (
Figure 6c). The authors observed an essential percentage of patients with respiratory and endocrine alterations, namely thyroid diseases (48 patients, 9%) (
Figure 6c).
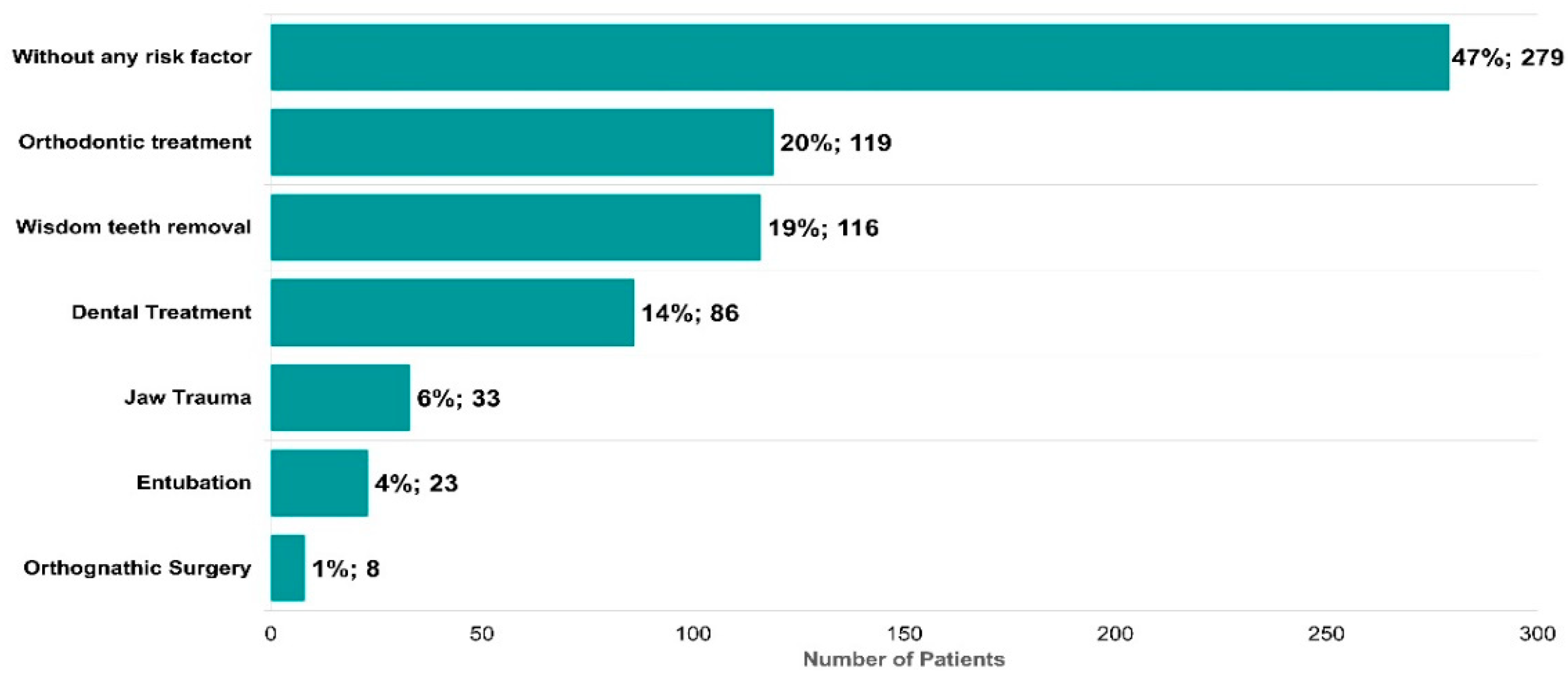
Potential risk factors described in the literature for triggering the onset of temporomandibular disorders were also identified (
Figure 7). 53% of the patients presented at least one risk factor (
Figure 7). Orthodontic treatment (119, 20%), wisdom tooth removal (116, 19%), dental treatment (86, 14%), jaw trauma (33, 6%), intubation (23, 4%), and orthognathic surgery (8, 1%) represent a large proportion of the risk factors identified (
Figure 7).
The association of clinical variables and TMJ pain with demographic data, parafunctional habits, risk factors, and other comorbidities were then studied (
Table S1).
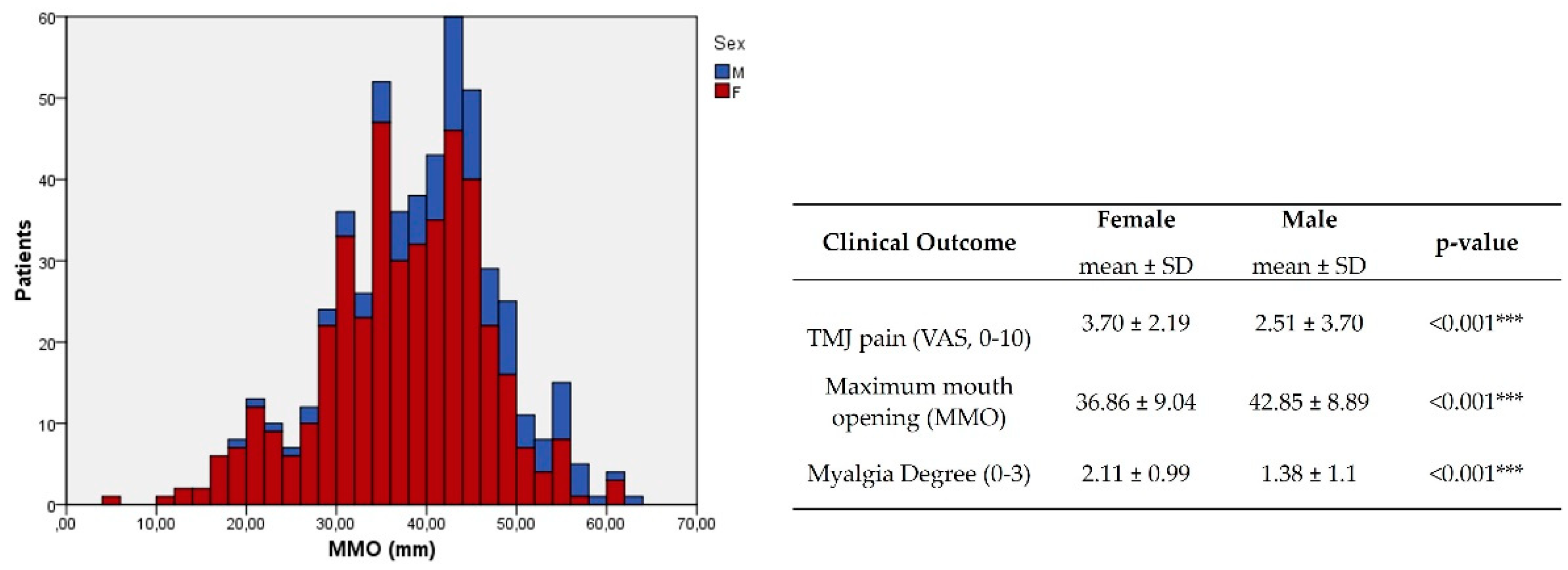
In demographic data, sex has a strong association with pain (P<0.001, φc=0.189,
Table 3) and limitation of mouth opening (P<0.001, φc=0.159,
Table 3) and a very strong association with the degree of myalgia (P<0.001, φc=0.277,
Table 3).
This association was corroborated by a higher degree of TMJ pain and myalgia and a lower MMO average in females (P<0.001,
Figure 8). At younger ages, the presence of clicks was more common (P=0.002, φc=0.177,
Table 3), while at older ages the presence of crepitus (P<0.001, φc=0.229,
Table 3).
Parafunctional habits have also been shown to have an association with the clinical variables: bruxism strongly associated with myalgia degree (P=0.006, φc=0.186,
Table 4); clenching strongly and moderately associated with myalgia degree and TMJ pain (P=0.008, φc=0.159 and P=0.035, φc=0.148,
Table 4).
Evaluating the association of risk factors with clinical variables revealed: past intubation was weakly related to limited mouth opening (P=0.047, φc=0.082,
Table 5), while past orthognathic surgery showed a moderate association with TMJ pain (P=0.011, φc=0.137,
Table 5); orthodontic treatment and wisdom teeth removal were weakly associated with TMJ clicks (P=0.026, φc=0.094; P=0.038, φc=0.088,
Table 5) and jaw trauma with TMJ crepitus (P=0.037, φc=0.093,
Table 5).
The presence of other comorbidities has been shown to have a strong association with the degree of TMJ pain and myalgia (P=0.002, φc=0.131 and P<0.001, φc=0.185,
Table 6). Within the identified disease classes, mental, behavioral, or neurodevelopmental disorders were strongly associated with the degree of myalgia and a moderate association with TMJ pain intensity (P<0.001, φc=0.202 and P=0.008, φc=0.142,
Table 6). Circulatory system diseases were moderately associated with the absence of TMJ clicks (P=0.003, φc=0.125,
Table 6).
4. Discussion
TMD are one of the principal causes of chronic facial pain, affecting a considerable part of the population [
9]. This 3-year prospective study provides a comprehensive and detailed characterization of the TMD population and demonstrates possible correlations with other comorbidities or risk factors. In this study, 80% of our patients were females with a mean age of 38 years. The age pattern and proportion of females were consistent with the results of other studies [
3,
10,
11]. Iodice, Cimino, Vollaro, Lobbezoo and Michelotti [
3] revealed that this phenomenon might result from the biological, behavioral, psychological, and/or social factors associated with the female gender [
3].
In our current study, the most common TMD symptom was TMJ clicking (13.26%), as reported in other studies [
3,
12,
13], followed by TMJ pain (12.49%) and masticatory muscle tension (12.15%). However, considering only the patient’s main complaint, we found that 22.78% referred to TMJ pain as their leading symptom. Additionally, in our study, the duration of complaints was mainly 1-5 and over 5 years, with a low occurrence of symptoms under 3 months. Therefore, we hypothesize that most patients take some time to associate the symptoms with TMD and find adequate medical opinion. This correlates with the fact that overall, the frequency of seeking treatment increases as the symptoms interfere with day-to-day activities. In addition, we also observed that TMD pain occurs as part of a group of symptoms rather than as a single entity [
3].
In our study, TMD signs are more frequent than symptoms [
2,
14]. This can partly be explained by the difference between the prevalence of TMJ clicking as a complaint (13.26%) or clinical signs during the medical evaluation. Despite being a TMD symptom, TMJ clicking can also be a sign of TMD. Nevertheless, the most common TMD sign was TMJ sounds (~62% and ~60% clicking in the right and left TMJ; ~14% and ~12 crepitus in the right and left TMJ). Suggestive pain indicative of possible TMJ arthralgia (~36% and ~31% in the right and left TMJ), masticatory muscles myalgia (2.03±1.07 and 1.87±1.09 on right and left sides, respectively), and MMO (38±9.31 mm) was also evaluated. This data suggests that an expert clinical evaluation can sometimes valorize signs that patients are unaware. Previous studies correlate the association between TMD signs and symptoms with age, gender, and TMD diagnosis. TMJ clicking has been shown to be common in younger subjects, while TMJ crepitation showed a stronger association with higher age [
3,
15]. This result is in accordance with our study, as our population was mainly younger subjects and the predominant clinical sign was TMJ clicking. At the same time, crepitus was more prevalent in older patients. This result is in agreement that the presence of crepitus is related to the diagnosis of osteoarthritis, which is more common in older patients [
16]. Also, TMJ pain and myalgia were significantly higher in females, while MMO was significantly lower. This result shows that besides the prevalence of the disease in women, the symptoms are also more exacerbated. Correlation between signs and symptoms can contribute to an appropriate TMD diagnosis. Previous studies demonstrate that muscle pain and tenderness may indicate myofascial disorders, while TMJ pain on palpation and Limited Mouth Opening (LMO) can suggest intra-articular conditions. In our research, this was observed in pain indicative of arthralgia (~36% and ~31% in the right and left TMJ) and a mean MMO of 38±9.31 mm, encountering a limitation of mouth opening as a cut-off of MMO<40 mm was defined in our study.
Furthermore, TMJ pain was moderated correlated with LMO, while masticatory muscle tension had a moderate correlation with headache and cervical muscle tension. LMO was moderately associated with TMJ locking. On the other hand, TMJ clicking is considered a potential sign of disc displacement with reduction. Otherwise, limited mouth opening (LMO) can be a typical sign of disc displacement without reduction [
2]. In the present study, ~62% and ~60% of the patients presented TMJ clicking in the right and left TMJ, respectively, and the mean of MMO measured was 38±9.31mm. By analyzing these results, we observed that over one-half of the patients evaluated had signs of disc displacement with reduction. However, on average, the majority of the patients presented LMO. Previous studies support these findings as they linked LMO with other entities besides disc displacement without reduction, such as myalgia and degenerative joint disease associated with the normal aging process, possibly explaining the high percentage of individuals with LMO in this study [
13]. In addition, some authors described disc displacement without reduction with the absence of LMO, while acute disease with the presence of LMO [
17,
18].
The most frequent possible causes for TMD described by the patients included: (1) parafunctional habits: clenching (60%), bruxism (30%); (2) previous orthodontic treatment (20%); (3) wisdom tooth removal (19%), (4) general dental treatment (14%), (5) jaw trauma (6%), (6) tracheal intubation (4%), and (7) orthognathic surgery (1%). Our study shows a strong association between clenching and bruxism with the degree of myalgia and a moderate association between clenching and TMJ pain. In addition, previous tracheal intubation, orthognathic surgery, and wisdom tooth removal were positively associated with a limited mandibular range of motion, TMJ pain, and TMJ clicking, respectively. These findings are in accordance with previous studies, as Marklund and Wänman [
19] that performed a 2-year prospective observational study and concluded that biomechanical factors, such as bruxism, mandibular instability, and malocclusion, were linked to the incidence and persistence of TMJ signs and symptoms. Moreover, trauma and long-standing load may also contribute to the development and course of TMD [
19,
20].
Regarding other comorbidities, it is unclear to which extent TMD may reflect symptoms or manifestations of underlying diseases. In the current study, although most of the patients evaluated had no comorbidities (57.12%), 42.88% of TMD have other conditions: 21.06% presented only one disease. In comparison, 21.82% of the patients referred two or more diseases.
Almost one-third of these patients reported mental behavior and neurodevelopmental diseases, a pertinent factor for many patients with TMD. A total of 20% had positive results for anxiety and 13% for depression. This study shows a correlation between mental behavioral and neurodevelopmental diseases with TMJ pain and myalgia. This result is consistent with other studies that demonstrated significant associations between stress, anxiety, depression, and TMD [
21,
22]. Previous and present results strongly support such an association and should be aware that specialists to keep psychosocial modulators as possible treatment-associated modalities. In addition, other chronic diseases summarized in
Figure 6, such as respiratory and endocrine alterations, might be related to TMD. This is corroborated in other population studies as there is evidence for an association between impaired general health and TMD, suggesting that TMD symptoms may share characteristics with other chronic conditions [
23,
24].
One of the strengths of this study was the consistency of a questionnaire and clinical examination to obtain reliable results for TMJ signs and symptoms in the first appointment. In addition, the validated EUROTMJ database allows the collection of data and evaluation of TMD-related symptoms, correlating the findings with TMD signs. This can be a valuable, and applicable platform for TMD screening and treatment decisions. Also, only one specialist examined all the patients in a TMD-specialized appointment, making it an advantage of this study. However, as with most studies, the present analysis has limitations. Firstly, the questionnaire is not validated; also, the information bias might be present since the parameters evaluated using the VAS scale could be over or underestimated by the patients. Additionally, the evaluation of the correlation between TMD signs and symptoms and TMJ diagnosis and proposed treatment was not included in this study, making it a limitation. Moreover, this study is single-center, which should be reproduced in a multi-center study.
5. Conclusions
TMD are a group of dysfunctions that affect a considerable part of the population nowadays, mainly younger female patients. This study demonstrates that TMD represent a group of disorders with a broad spectrum of clinical manifestations, pathophysiology, and associated comorbid conditions. Significant associations between TMD signs and symptoms with intrinsic characteristics, such as age and gender, and parafunctional habits, such as clenching and bruxism, have been made. Positive correlations were also made with mental behavior and neurodevelopmental diseases, such as anxiety and depression, and other comorbidities, such as respiratory and endocrine alterations. Interestingly, risk factors such as wisdom tooth removal, orthodontic treatment, jaw trauma, tracheal intubation, and orthognathic surgery may increase the susceptibility to develop TMD clinical symptoms. However, more studies are needed to understand such associations. We believe this data will serve as a milestone in providing helpful information for researchers and healthcare providers treating patients with TMD.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Relative frequency (%) of the TMJ pain and clinical variables.
Author Contributions
Conceptualization, Ângelo D.F., Sanz D., Mota B and Cardoso H.J.; methodology, Ângelo D.F., São João R. and Cardoso H.J.; validation, Ângelo D.F, Sanz D. and Mota B formal analysis, São João R. and Cardoso H.J.; investigation, Ângelo D.F., Sanz D., Mota B, São João R. and Cardoso H.J.; resources, Ângelo D.F., Sanz D; data curation, São João R. and Cardoso H.J.; writing—original draft preparation, Ângelo D.F., Mota B and Cardoso H.J.; writing—review and editing, Ângelo D.F., Sanz D., Mota B, São João R. and Cardoso H.J..; supervision, Ângelo D.F.; project administration, Ângelo D.F. and Cardoso H.J. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Research Grant SORG 2019 assigned to David Ângelo (M.D, PhD) - project: "EUROTMJ – recording TMJ outcomes in a central database.” We also thank the sub-group created by the European Society of TMJ Surgeons (ESTMJS) for their contribution to the creation of the database, namely to: Florencio Monje (M.D, PhD); Raúl González-García (M.D, PhD); Vladimir Machoň (M.D); Mattias Ulmner (M.D, PhD); Niall McLeod (M.D); Jacinto Fernández Sanromán (M.D, PhD). The funding for publication is supported by CEAUL – Centro de Estatística e Aplicações, Faculdade de Ciências, Universidade de Lisboa, Portugal financed by national funds through FCT – Fundação para a Ciência e a Tecnologia under the project UIDB/00006/2020.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Instituto Português da Face ethics committee (PT/IPFace//RCT/0822/01).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Chaurasia, A.; Ishrat, S.; Katheriya, G.; Chaudhary, P.K.; Dhingra, K.; Nagar, A. Temporomandibular disorders in North Indian population visiting a tertiary care dental hospital. Natl J Maxillofac Surg 2020, 11, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Qvintus, V.; Sipilä, K.; Le Bell, Y.; Suominen, A.L. Prevalence of clinical signs and pain symptoms of temporomandibular disorders and associated factors in adult Finns. Acta odontologica Scandinavica 2020, 78, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Iodice, G.; Cimino, R.; Vollaro, S.; Lobbezoo, F.; Michelotti, A. Prevalence of temporomandibular disorder pain, jaw noises and oral behaviours in an adult Italian population sample. J Oral Rehabil 2019, 46, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Kmeid, E.; Nacouzi, M.; Hallit, S.; Rohayem, Z. Prevalence of temporomandibular joint disorder in the Lebanese population, and its association with depression, anxiety, and stress. Head & face medicine 2020, 16, 19. [Google Scholar] [CrossRef]
- Johansson, A.; Unell, L.; Carlsson, G.E.; Söderfeldt, B.; Halling, A. Risk factors associated with symptoms of temporomandibular disorders in a population of 50- and 60-year-old subjects. J Oral Rehabil 2006, 33, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.L.; Ohrbach, R.; Truelove, E.L.; Tai, F.; Anderson, G.C.; Pan, W.; Gonzalez, Y.M.; John, M.T.; Sommers, E.; List, T.; et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 2010, 24, 63–78. [Google Scholar] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. Journal of oral & facial pain and headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Goiato, M.C.; Zuim, P.R.J.; Moreno, A.; Dos Santos, D.M.; da Silva, E.V.F.; de Caxias, F.P.; Turcio, K.H.L. Does pain in the masseter and anterior temporal muscles influence maximal bite force? Archives of oral biology 2017, 83, 1–6. [Google Scholar] [CrossRef]
- Kothari, K.; Jayakumar, N.; Razzaque, A. Multidisciplinary management of temporomandibular joint ankylosis in an adult: journey from arthroplasty to oral rehabilitation. BMJ case reports 2021, 14. [Google Scholar] [CrossRef]
- Gesch, D.; Bernhardt, O.; Alte, D.; Schwahn, C.; Kocher, T.; John, U.; Hensel, E. Prevalence of signs and symptoms of temporomandibular disorders in an urban and rural German population: results of a population-based Study of Health in Pomerania. Quintessence international (Berlin, Germany : 1985) 2004, 35, 143–150. [Google Scholar]
- Feteih, R.M. Signs and symptoms of temporomandibular disorders and oral parafunctions in urban Saudi Arabian adolescents: a research report. Head & face medicine 2006, 2, 25. [Google Scholar] [CrossRef]
- Gonçalves, D.A.; Dal Fabbro, A.L.; Campos, J.A.; Bigal, M.E.; Speciali, J.G. Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain 2010, 24, 270–278. [Google Scholar] [PubMed]
- Mobilio, N.; Casetta, I.; Cesnik, E.; Catapano, S. Prevalence of self-reported symptoms related to temporomandibular disorders in an Italian population. J Oral Rehabil 2011, 38, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Könönen, M.; Waltimo, A.; Nyström, M. Does clicking in adolescence lead to painful temporomandibular joint locking? Lancet (London, England) 1996, 347, 1080–1081. [Google Scholar] [CrossRef]
- Lamot, U.; Strojan, P.; Šurlan Popovič, K. Magnetic resonance imaging of temporomandibular joint dysfunction-correlation with clinical symptoms, age, and gender. Oral surgery, oral medicine, oral pathology and oral radiology 2013, 116, 258–263. [Google Scholar] [CrossRef]
- Abrahamsson, A.K.; Kristensen, M.; Arvidsson, L.Z.; Kvien, T.K.; Larheim, T.A.; Haugen, I.K. Frequency of temporomandibular joint osteoarthritis and related symptoms in a hand osteoarthritis cohort. Osteoarthritis and cartilage 2017, 25, 654–657. [Google Scholar] [CrossRef]
- Al-Baghdadi, M.; Durham, J.; Araujo-Soares, V.; Robalino, S.; Errington, L.; Steele, J. TMJ Disc Displacement without Reduction Management: A Systematic Review. Journal of dental research 2014, 93, 37s–51s. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Sousa, R.; Pinto, I.; Sanz, D.; Gil, F.M.; Salvado, F. Early magnetic resonance imaging control after temporomandibular joint arthrocentesis. Ann Maxillofac Surg 2015, 5, 255–257. [Google Scholar] [CrossRef]
- Marklund, S.; Wänman, A. Risk factors associated with incidence and persistence of signs and symptoms of temporomandibular disorders. Acta odontologica Scandinavica 2010, 68, 289–299. [Google Scholar] [CrossRef]
- Johansson, A.; Unell, L.; Carlsson, G.; Söderfeldt, B.; Halling, A.; Widar, F. Associations between social and general health factors and symptoms related to temporomandibular disorders and bruxism in a population of 50-year-old subjects. Acta odontologica Scandinavica 2004, 62, 231–237. [Google Scholar] [CrossRef]
- De La Torre Canales, G.; Câmara-Souza, M.B.; Muñoz Lora, V.R.M.; Guarda-Nardini, L.; Conti, P.C.R.; Rodrigues Garcia, R.M.; Del Bel Cury, A.A.; Manfredini, D. Prevalence of psychosocial impairment in temporomandibular disorder patients: A systematic review. J Oral Rehabil 2018, 45, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Rauch, A.; Hahnel, S.; Kloss-Brandstätter, A.; Schierz, O. Patients referred to a German TMD-specialized consultation hour-a retrospective on patients without a diagnosis according to RDC/TMD decision trees. Clinical oral investigations 2021, 25, 5641–5647. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, S.F.; Huggins, K.H.; LeResche, L.; Von Korff, M.; Howard, J.; Truelove, E.; Sommers, E. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. Journal of the American Dental Association (1939) 1990, 120, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, R.G.; Kotchen, J.M.; Kotchen, T.A.; Cowley, T.; Dasgupta, M.; Cowley, A.W., Jr. Temporomandibular disorders and associated clinical comorbidities. The Clinical journal of pain 2011, 27, 268–274. [Google Scholar] [CrossRef]
Figure 1.
EUROTMJ database screen.
Figure 1.
EUROTMJ database screen.
Figure 2.
Global pain in the first visit (a) and Visual Analogue Score (VAS) in the patients that reported pain (b). The representative median VAS values in the range [Q1-1.5IQR;Q3+1.5IQR] are shown in the right graphs where IQR=interquartile range and Q1 and Q3 are, respectively, the 1st and 3rd quartiles (N=595).
Figure 2.
Global pain in the first visit (a) and Visual Analogue Score (VAS) in the patients that reported pain (b). The representative median VAS values in the range [Q1-1.5IQR;Q3+1.5IQR] are shown in the right graphs where IQR=interquartile range and Q1 and Q3 are, respectively, the 1st and 3rd quartiles (N=595).
Figure 3.
Global Complaints. (A) Complaints frequency; (B) Primary complaint frequency; (C) Duration of each complaint (N=595).
Figure 3.
Global Complaints. (A) Complaints frequency; (B) Primary complaint frequency; (C) Duration of each complaint (N=595).
Figure 4.
Correlation matrix of complaints obtained by biserial correlation Pearson Test. N=595 p-value<0.05*.
Figure 4.
Correlation matrix of complaints obtained by biserial correlation Pearson Test. N=595 p-value<0.05*.
Figure 5.
Clinical evaluation in the first visit. Maximum mouth opening (MMO), muscle tenderness, clicks, crepitus, and arthralgia were registered. The right graph shows the representative median MMO value in the range [Q1-1.5IQR; Q3+1.5IQR] where IQR=interquartile range and Q1 and Q3 are, respectively, the 1st and 3rd quartiles (N=595).
Figure 5.
Clinical evaluation in the first visit. Maximum mouth opening (MMO), muscle tenderness, clicks, crepitus, and arthralgia were registered. The right graph shows the representative median MMO value in the range [Q1-1.5IQR; Q3+1.5IQR] where IQR=interquartile range and Q1 and Q3 are, respectively, the 1st and 3rd quartiles (N=595).
Figure 6.
Other comorbidities identified in patients with temporomandibular disorders. (A) Number of patients without or with at least 1 or 2 comorbidities (N=527) (B) Number of patients for a group of comorbidities (N=545) (C) Number of patients with specific comorbidities (N=545).
Figure 6.
Other comorbidities identified in patients with temporomandibular disorders. (A) Number of patients without or with at least 1 or 2 comorbidities (N=527) (B) Number of patients for a group of comorbidities (N=545) (C) Number of patients with specific comorbidities (N=545).
Figure 7.
Risk factors identified in patients with symptoms of the temporomandibular disease (N=595).
Figure 7.
Risk factors identified in patients with symptoms of the temporomandibular disease (N=595).
Figure 8.
Distribution of maximum mouth opening (MMO) and statistical difference between TMJ pain, MMO, and myalgia degree by sex. F-female; M-male. ****P<0.001.
Figure 8.
Distribution of maximum mouth opening (MMO) and statistical difference between TMJ pain, MMO, and myalgia degree by sex. F-female; M-male. ****P<0.001.
Table 1.
Demographic data and side of the TMJ symptoms.
Table 1.
Demographic data and side of the TMJ symptoms.
| Variables |
N (%), or mean±SD |
| Number of patients |
595 |
|
| Sex |
Female |
479 (80.50 %) |
| Male |
116 (19.50 %) |
| Age |
38.20±15.73 |
|
| |
|
|
| Side of the joint with symptoms |
Only Right |
41 (6.89 %) |
| Only Left |
40 (6.72 %) |
| Bilateral |
514 (86.39 %) |
Table 2.
Parafunctional habits. Frequency of Clenching and bruxism habits. N=595.
Table 2.
Parafunctional habits. Frequency of Clenching and bruxism habits. N=595.
| Parafunctional Habits |
|---|
| Variables |
|
N (%) |
| Bruxism |
Day |
7 (1%) |
| Night |
138 (23%) |
| Day and Night |
35 (6%) |
| No |
212 (36%) |
| Does not know |
203 (34%) |
| Clenching |
Yes |
359 (60%) |
| No |
159 (27%) |
| Does not know |
77 (13%) |
Table 3.
Association table with demographic data and TMJ pain and clinical variables. Significant values are in bold.
Table 3.
Association table with demographic data and TMJ pain and clinical variables. Significant values are in bold.
| TMJ Pain and Clinical Variables |
|---|
| Demographic Data |
TMJ Pain |
Open Mouth Limitation |
Myalgia Degree |
TMJ Clicks |
TMJ Crepitus |
Arthralgia |
| p-value, Cramer’s V |
| Sex |
<0.001, 0.189 |
<0.001, 0.154 |
<0.001, 0.277 |
0.698, 0.016 |
0.179, 0.060 |
0.143, 0.064 |
| Age |
0.889, 0.060 |
0.543, 0.072 |
0.456, 0.088 |
0.002, 0.177 |
<0.001, 0.229 |
0.032, 0.142 |
Table 4.
Association table with parafunctional habits and TMJ pain and clinical variables. Significant values are in bold.
Table 4.
Association table with parafunctional habits and TMJ pain and clinical variables. Significant values are in bold.
| TMJ Pain and Clinical Variables |
|---|
| Parafunctional Habits |
TMJ Pain |
Open Mouth Limitation |
Myalgia Degree |
TMJ Clicks |
TMJ Crepitus |
Arthralgia |
| P-value, Cramer’s V |
| Clenching |
0.203, 0.094 |
0.340, 0.042 |
0.008, 0.159 |
0.760, 0.013 |
0.571, 0.026 |
0.677, 0.020 |
| Bruxism |
0.035, 0.148 |
0.732, 0.017 |
0.006, 0.186 |
0.890, 0.012 |
0.496, 0.036 |
0.364, 0.048 |
Table 5.
Association table with risk factors and TMJ pain and clinical variables. Significant values are in bold.
Table 5.
Association table with risk factors and TMJ pain and clinical variables. Significant values are in bold.
| Global Pain and Clinical Variables |
|---|
| Risk Factors |
TMJ Pain |
Open Mouth Limitation |
Myalgia Degree |
TMJ Clicks |
TMJ Crepitus |
Arthralgia |
| P-value, Cramer’s V |
| Dental treatment |
0.343, 0.075 |
0.168, 0.057 |
0.891, 0.035 |
0.698, 0.016 |
0.270, 0.049 |
0.065, 0.080 |
| Orthodontic treatment |
0.419, 0.069 |
0.116, 0.064 |
0.386, 0.077 |
0.026, 0.094 |
0.238, 0.053 |
0.523, 0.028 |
| Entubation |
0.489, 0.064 |
0.047, 0.082 |
0.323, 0.082 |
0.169, 0.058 |
0.135, 0.067 |
0.731, 0.015 |
| Orthognathic surgery |
0.011, 0.137 |
0.234, 0.049 |
0.286, 0.086 |
0.858, 0.008 |
0.313, 0.045 |
0.524, 0.028 |
| Wisdom teeth removal |
0.537, 0.060 |
0.115, 0.065 |
0.879, 0.036 |
0.038, 0.088 |
0.824, 0.010 |
0.729, 0.015 |
| Jaw trauma |
0.216, 0.087 |
0.326, 0.040 |
0.179, 0.098 |
0.732, 0.014 |
0.037, 0.093 |
0.201, 0.056 |
Table 6.
Association table of other comorbidities and TMJ pain and clinical variables. Significant values are in bold.
Table 6.
Association table of other comorbidities and TMJ pain and clinical variables. Significant values are in bold.
| TMJ pain and Clinical Variables |
|---|
| Other Comorbidities |
TMJ Pain |
Open Mouth Limitation |
Myalgia Degree |
TMJ Clicks |
TMJ Crepitus |
Arthralgia |
| P-value, Cramer’s V |
| N (no, 1, ≥2) |
0.002, 0.131 |
0.354, 0.059 |
<0.001, 0.185 |
0.125, 0.086 |
0.490, 0.054 |
0.786, 0.030, |
| Group of other Comorbidities |
|
|
|
|
|
|
| |
|
|
|
|
|
| Mental, behavioral or neurodevelopmental disorders |
0.008, 0.142 |
0.678, 0.017 |
<0.001, 0.202 |
0.708, 0.016 |
0.677, 0.019 |
0.645, 0.020 |
| Diseases of the respiratory system |
0.492, 0.064 |
0.475, 0.029 |
0.138, 0.103 |
0.381, 0.037 |
0.236, 0.053 |
0.835, 0.009 |
| Endocrine, nutritional or metabolic diseases |
0.154, 0.094 |
0.798, 0.011 |
0.195, 0.096 |
0.264, 0.047 |
0.370, 0.040 |
0.487, 0.030 |
| Diseases of the circulatory system |
0.990, 0.014 |
0.679, 0.017 |
0.956, 0.025 |
0.003, 0.125 |
0.066, 0.083 |
0.416, 0.035 |
| Diseases of the musculoskeletal system |
0.228, 0.085 |
0.584, 0.022 |
0.719, 0.051 |
0.979, 0.001 |
0.125, 0.069 |
0.253, 0.050 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).