1. Introduction
Interventions in otorhinolaryngology (ORL), tracheal surgery, intensive care medicine, and thoracic surgery represent a specific situation for surgeons and anesthesiologists. Unlike in other surgical fields, in this case, the place of interest for both is the respiratory tract. The requirements of the performing physician for optimal access to the operative field are often in conflict with the requirements of the anesthesiologist to ensure patency of the airways and ventilation. Similarly, with tracheostomy and rigid or flexible bronchoscopy, the specialist's requirements are fairly specific [
1].
The choice of anesthesiologic approach and artificial lung ventilation (ALV) type in patients with airway or lung pathology, be it pneumonia, or COVID-19-associated ARDS (CARDS), largely depends on the pathological process in the respiratory tract. Also, on the traumatic changes in the airways, associated lung diseases (including COVID-19), and especially in oncologic patients when the airways are obstructed by a growing tumor. In addition, patients with bronchopneumonia have a risk of worsening the gas exchange in the lungs. In order to find an optimal solution, many different techniques were unsuccessfully used in the past: spontaneous ventilation and topical anesthesia, apneic oxygenation, intermittent apnea, and intubation with a thin endotracheal cannula. In the 1970s, high-frequency jet ventilation (HFJV) was developed [
2] to reduce the risk of aspiration of debris and blood, as well as to minimize vocal cord movements. Currently, the method of catheter high-frequency jet ventilation (C-HFJV) is often used.
Most of the studies so far have been focused on evaluating the effectiveness and safety of tracheotomies, whether according to Fantoni or puncture dilatation tracheotomy, bronchoscopy or in patients with pneumonia. Also, on evaluating patients with tumorous changes in the upper airways, or with traumatic changes of the trachea and bronchi. In this article, we present the positive effects of C-HFJV even with complications such as bacterial or viral pneumonia, including COVID-19. We offer recommendations for clinical practice obtained from a literature review as well as from our own rich clinical experience.
2. Materials and Methods
2.1. High-Frequency Jet Ventilation
The HFJV method is based on the application of small volumes of gas under high pressure through a specially adapted cannula (catheter), without sealing the airways with a balloon. Thus, leaving the airways with free communication with the surrounding environment or using a special multi-nozzle jet injector (MNJI) [
3]. In order to achieve adequate minute ventilation, it is necessary to ensure a high respiratory frequency with small applied volumes of gas [
3,
4].
2.1.1. Types of HFV Techniques
HFPPV (high-frequency positive pressure ventilation) - high-frequency ventilation with positive pressure using a frequency of up to 200 cycles/min
HFJV (high-frequency jet ventilation) - high-frequency ventilation using a nozzle to generate a jet stream with a frequency of up to 600 cycles/min
HFO (high-frequency oscillation) - high-frequency ventilation with a frequency above 600 cycles/min [
5]
From the technical implementation point of view, the ventilators are divided into:
classic ventilator with a higher breathing frequency (HFPPV)
ventilator with nozzle-type injector and receiving channel (HFJV)
special HF ventilators using piston, bubble, and membrane, to generate oscillation (HFO)
2.1.2. Methods of application – interface:
From the point of view of the ventilation circuit closure to the atmosphere, HFV can be divided into closed (hermetic) and open (non-hermetic) systems.
Methods of application of breathing gas, i.e. supply to the airways:
with a multi-nozzle jet injector connected to an endotracheal tube or laryngeal mask, tight or open
with a transtracheal needle or catheter
with a catheter inserted into the trachea (bronchus) with monitoring of airway pressure
with binasal cannula
with a face mask
Table 1.
Advantages and disadvantages of HFJV [
5].
Table 1.
Advantages and disadvantages of HFJV [
5].
| |
Advantages |
Disadvantages |
| Physiological |
↓ peak pressure in airways |
Risk of barotrauma |
| ↑ cardiac output |
Inspired FiO2 inaccurate |
| ↓ ADH, fluid retention |
Gas exchange efficiency is less predictable in obesity or chronic obstructive pulmonary disease (COPD) |
| Surgical |
Minimal movement of the vocal cords |
Possibility of lower airways contamination during ORL surgery |
| Improving access to the surgical field |
| Lowering risk during laser surgery |
Contamination of expired air with operational debris |
| Minimizing the excursions of the respiratory system |
| Anesthesia |
Advangegous during respiratory tract operations and bronchoscopy |
Impossibility of inhalation anesthesia |
| Intermittent measurement of ETCO2
|
| Use in emergency situations, transtracheal approach |
Necessary humidification |
| Minor gas leak at broncho-pleural fistula surgery |
High gas flow |
| Measured airway pressure inaccurate |
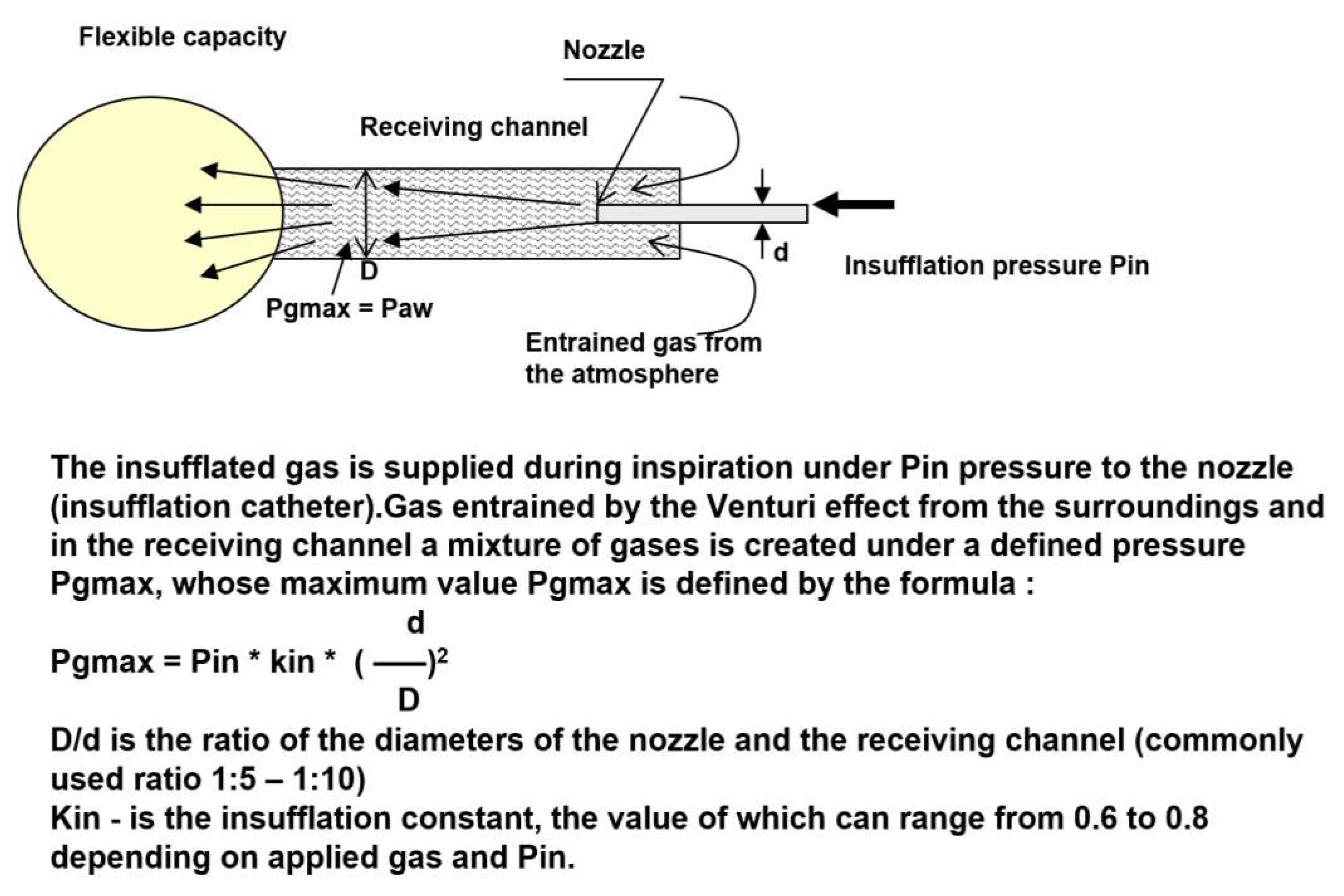
2.2. Basic physical principles of HFJV function
The principle of the HFJV function is based on the fact that the catheter introduced into the trachea represents a nozzle located in the receiving channel (trachea), i.e. a generator of gas kinetic power. During the flow of gases through the insufflation catheter, an overpressure is created at the distal end of the receiving channel, and the gas flowing through the nozzle creates a negative pressure at the proximal end of the generator by the Venturi effect, usually entraining gas from the surrounding atmosphere, which creates a total gas flow through the generator. Energy, i.e. pressure (Pg = Paw) and gas flow (Qi) depend on the driving pressure Pin and on the ratio of the diameters of the nozzle and the receiving channel (d, D). [
5]
For the clinical application, the maximum pressure of the generator PGmax is very important. This value determines the maximum pressure level that can be reached in the lungs at a given insufflation pressure Pin, which can range from 80 to 300 kPa. At the PGmax value, gas does not flow from the lungs or into the lungs, which means that the excess pressure in the lungs, the alveolar pressure (PAI), is equal to PGmax.
The value of PGmax is proportional to twice the value of the insufflation pressure and the square of the ratio of the diameter of the nozzle and the receiving channel (d/D). The constant Kin includes the pressure loss during the flow [
3].
Figure 1.
Scheme of the pressure and flow generator with the "nozzle-receiving channel" system.
Figure 1.
Scheme of the pressure and flow generator with the "nozzle-receiving channel" system.
3. Results
3.1. Catheter form of HFJV with the original jet catheter
3.1.1. History of catheter HFJV
In 1967, Sanders developed alternative ventilation to conventional ventilation during microlaryngoscopy [
6]. During passive expiration, the gas was applied above the vocal cords through the application cannula fixed to the laryngoscope. Since at that time, several application systems have been developed to provide subglottic, supraglottic, and transtracheal high-frequency ventilation, using different catheters and ventilation frequencies. In 1994 Hunsaker introduced a fluoroplastic, laser-resistant catheter, allowing subglottic ventilation and measurement of airway pressure and end-tidal CO
2 concentration (ETCO
2) [
7].
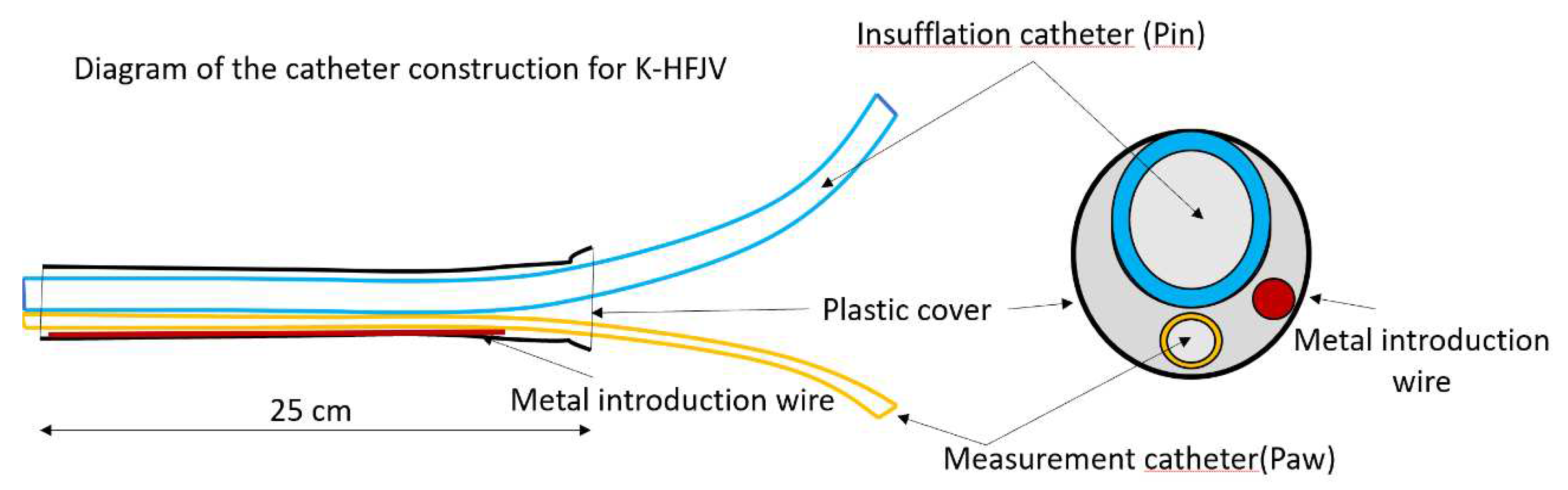
3.2. The present form of catheter HFJV - using the original double-lumen ventilation catheter (DVK) Figure 2
In this form of ALV, a ventilation catheter, which consists of an insufflation catheter, a measuring catheter, and a soft metal guidewire used to strengthen the shape of the catheter, covered in the plastic material package, is inserted into the trachea. The catheter, in its original construction, has an outer diameter of approximately 5.5 mm and a length of 27-28 cm.
Figure 2.
Scheme of the ventilation catheter.
Figure 2.
Scheme of the ventilation catheter.
The catheter is inserted into the trachea, either nasotracheally or orotracheally, usually under direct laryngoscopy. In cases where C-HFJV is applied in thoracic surgery, mainly for procedures on the trachea and bronchi, an insufflation catheter with a diameter of 1.5 mm is usually used for selective ventilation of the lungs. The insufflation catheter serves to apply gas from the ventilator under a pressure of 100-250 kPa, which generates kinetic energy of gases (flow and pressure) during inspiration (expiration is passive). The measuring catheter serves the purpose of measuring the pressure in the airways. At the same time, it is an active element in the prevention of barotrauma, which in rare cases can put the patient on C-HFJV at risk (e.g. laryngospasm) [
5]. The ventilator monitors the pressure in the airways and when the set limit is exceeded, it turns off the ventilator and stops the flow of gases through the Qi insufflation catheter, thus cutting off the flow to the alveolar compartment [
8]. The ventilation frequency is usually 120 c/min, which is a relatively optimal setting in terms of gas exchange.
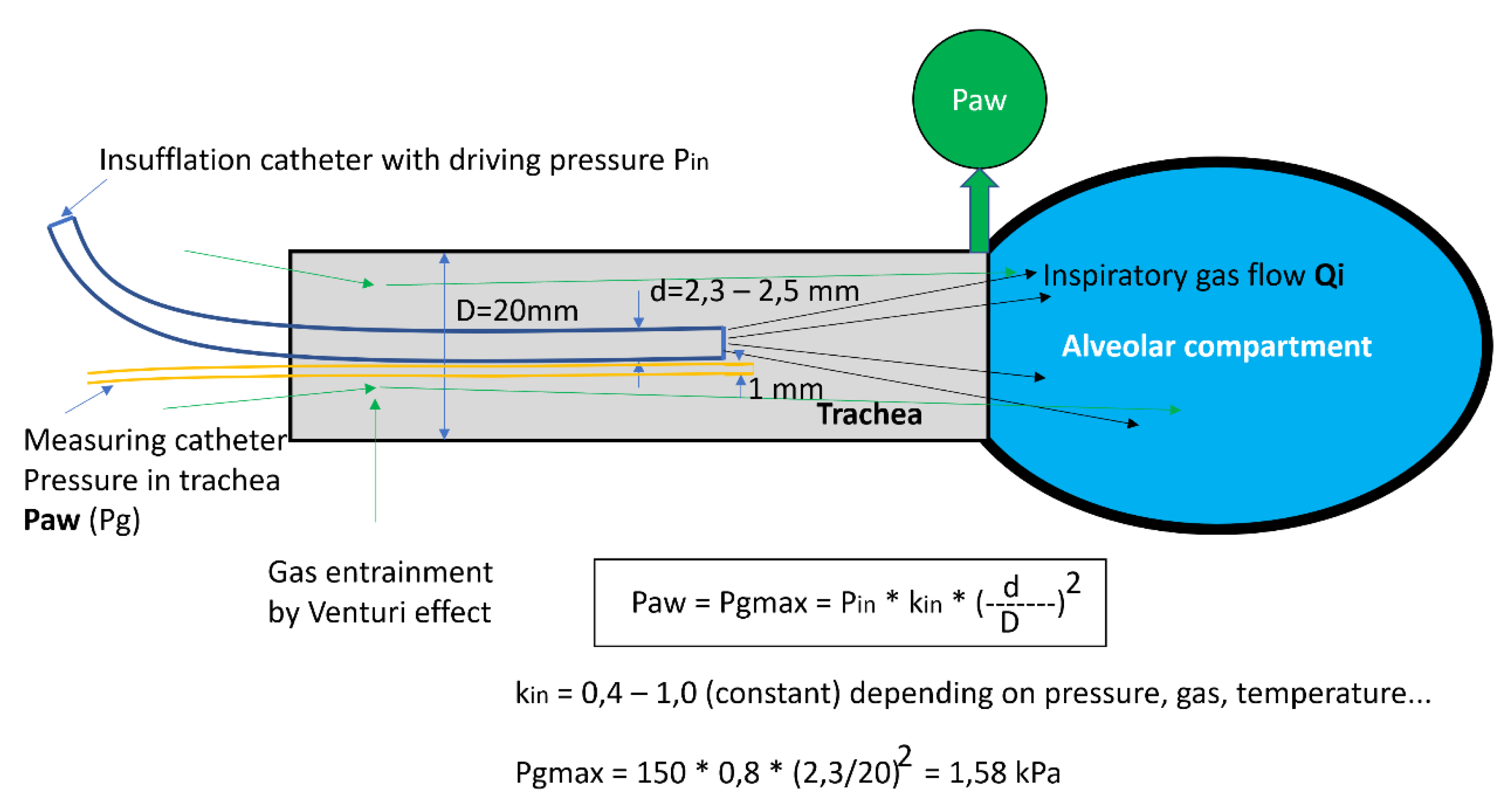
Figure 3.
Principles of catheter function in C-HFJV. Paw - pressure in the airways, Pin - insufflation pressure, kin - flow constant, d - diameter of the catheter, D - diameter of the receiving channel (trachea).
Figure 3.
Principles of catheter function in C-HFJV. Paw - pressure in the airways, Pin - insufflation pressure, kin - flow constant, d - diameter of the catheter, D - diameter of the receiving channel (trachea).
3.2.1. Advantages of catheter HFJV
ensures adequate exchange of blood gases
free operating field or bronchoscope view
prevention of aspiration - the Klein effect (positive pressure in the space under the tip of the catheter and the flow of gases is continuous during expiration and inspiration from the airways to the atmosphere).
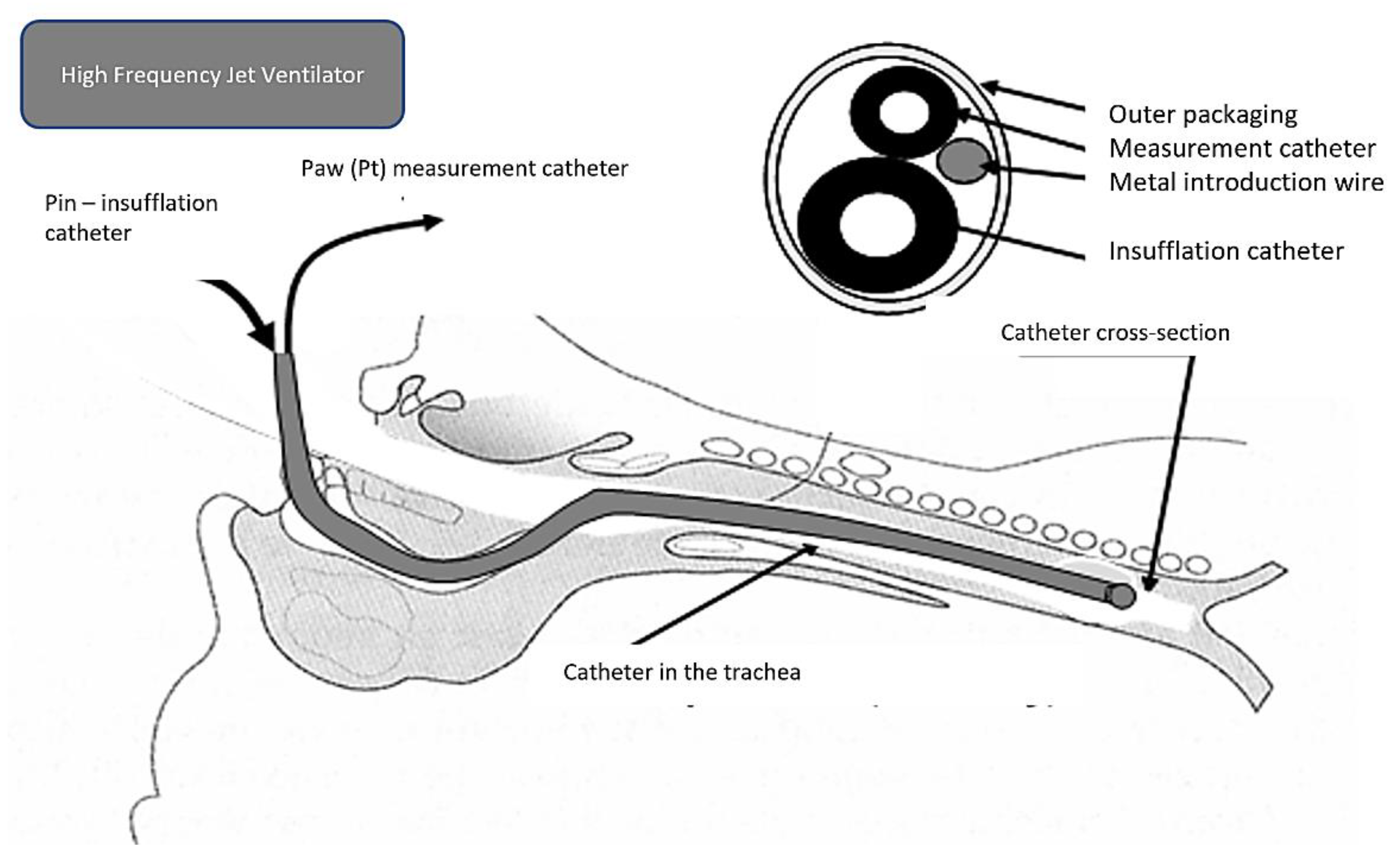
3.2.2. Placement of ventilation catheter:
supraglottic (during surgery in the area above the vocal cords)
transtracheal (very rare, usually as a life-saving procedure)
subglottic (introduced to a depth of 6-8 cm below the vocal cords or 3-4 cm above the carina)
The advantage of subglottic placement is the provision of ventilation independent of the instrumentation of the doctor performing the treatment or diagnostic procedure. Better gas exchange is ensured by the deeper placement of the cannula.
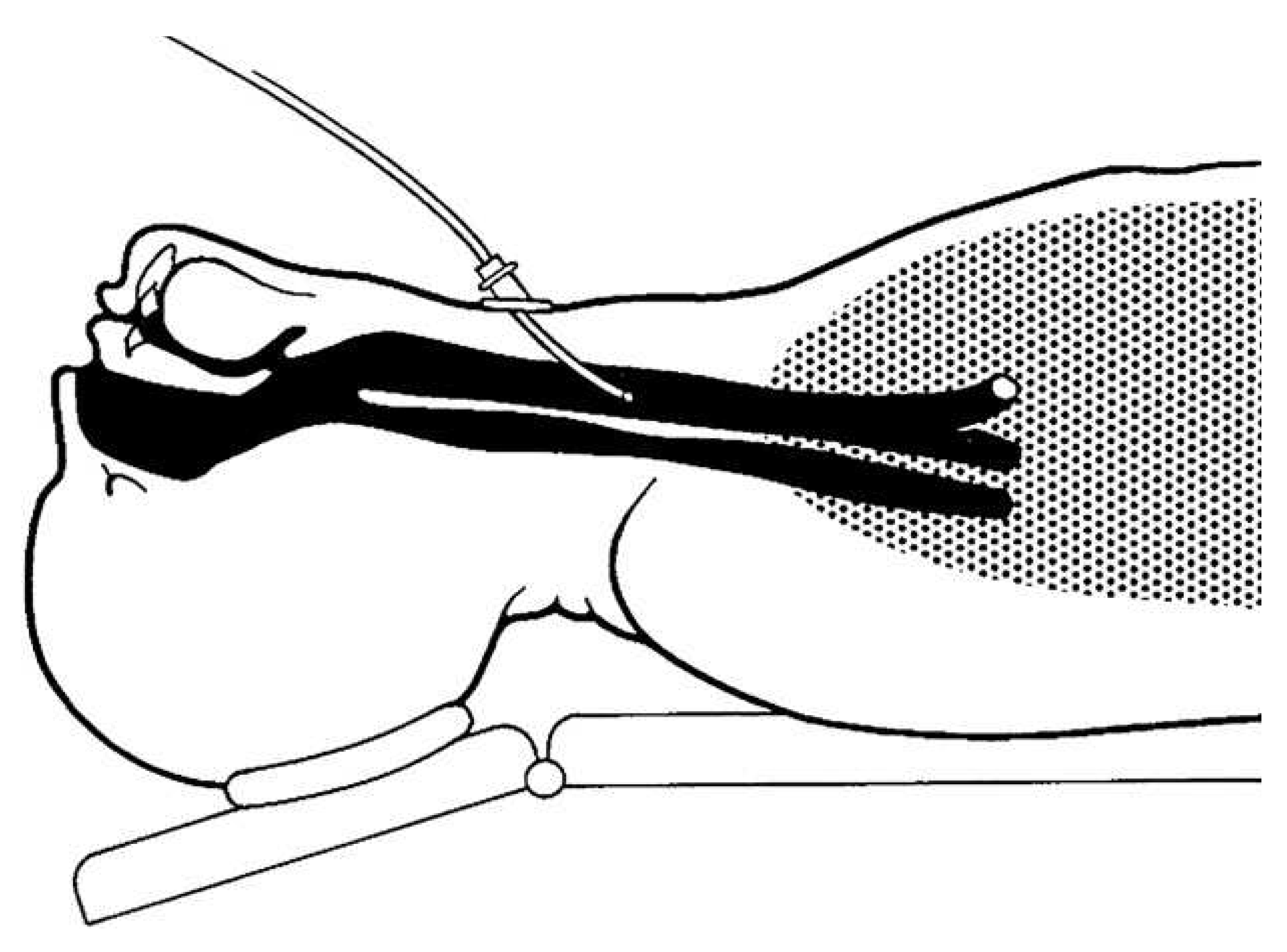
Figure 4.
Subglottic placement of the ventilation catheter.
Figure 4.
Subglottic placement of the ventilation catheter.
However, there is a risk of air trapping in the case of a sudden closure of the vocal cords, therefore it is not recommended to insert a catheter if the vocal fold is narrowed by more than 50% of the diameter. In this case, it is necessary to place the catheter proximal to the obstruction. In addition to greater safety in cases of airway obstruction, a supraglottically placed catheter ensures ventilation while maintaining a free glottis [
9]. The disadvantage is the lower efficiency of ventilation, which can be compensated by increasing the insufflation pressure. In urgent situations, e.g. impossibility of intubation or ventilation, it is possible to transtracheally place a thin (1 mm), single-lumen catheter subglottically through the cricothyroid ligament. For HFJV applied in this way, it is essential that the airways are free, without obstruction in the larynx and airways (
Figure 5).
3.2.3. Contraindications for the use of C-HFJV
There are no absolute contraindications for the use of C-HFJV. However, in some cases, it can be a problem to maintain sufficient oxygenation and CO
2 elimination. These are patients with morbid obesity, with present obstructive or restrictive lung diseases. [
4].
Insufficient oxygenation, manifested by a serious rise in lactate [
11], can be corrected by increasing FiO
2 and subsequently by increasing the insufflation pressure. The next step is to increase the inspiratory pressure, prevent respiratory entrainment of air during inspiration, and possibly insert the catheter more distally into the airway.
Insufficient elimination of CO2 occurs mainly in patients with COPD and in obese patients. The solution is to increase the inspiratory pressure to the maximum tolerable level (4.0 - 4.5 kPa).
3.3. Ventilator settings
HFJV is a form of time-cycled, pressure-limited ventilation (similar to pressure-controlled PCV ventilation). If the ventilator settings are constant, in the case of a decrease in compliance of the lungs and chest, minute ventilation is reduced. The elimination of CO2 depends more on the setting of the insufflation pressure than on the frequency of the ventilator.
Tidal volume is not adjustable but is a function of insufflation pressure, lung mechanics, inspiratory time, and physical properties of the catheter. The answer to adjusting the settings can be contradictory. Increasing the rate will cause hypercapnia by decreasing tidal volume if insufflation pressure and inspiratory time remain constant.
Insufflation pressure on the ventilator is set in the range of 120 - 300 kPa. In adults, Pin is initially set to a value of 150 kPa. By increasing the insufflation pressure, the tidal volume increases, the pressure in the airways increases, and CO2 decreases. However, a large increase in insufflation pressure at a high frequency will cause CO2 retention because of a short expiratory time. Thus, there is no linear relationship between insufflation pressure and gas exchange.
Ventilation frequency, i.e. the number of ventilator cycles per minute, represents the span of 12 - 300 c/min. A higher frequency makes it possible to generate smaller volumes, which results in a smaller amplitude of movement of the vocal cords. The disadvantage of a too-high frequency is the insufficient elimination of CO2 and the occurrence of auto-PEEP (positive end-expiratory pressure). For C-HFJV, the cycle frequency is usually set to f = 120 c/min
Auto-PEEP is a significant component of HFJV, depends on expiratory time, and increases with frequency and shorter expiratory time. This increases the air volume in areas of the lungs with a long time constant and a shorter expiration time [
5].
Spontaneous respiratory activity in HFJV. The patient can breathe spontaneously (if muscle relaxants are not used) because HFJV does not interfere with spontaneous ventilation. This also enables a smooth transition from HFJV to spontaneous ventilation without the need to intubate the patient or apply some form of an assistor.
Inspiratory time is the time between active insufflation and passive expiration. It is defined as a ratio (percentage) of the insufflation time to the total respiratory cycle, usually set to 50%. Changing the inspiratory time will immediately affect the tidal volume. The shortening results in an increase in auto-PEEP and other difficult-to-estimate changes in gas exchange.
Inspiratory oxygen concentration (FiO2) is the result of mixing insufflated oxygen with entrained air. It ranges between 0.4 - 1.0. Increased oxygen concentrations can be dangerous for laser surgery applications, so FiO2 should not exceed 40%. With C-HFJV, the average FiO2 = 0.5 - 0.6. (60%).
4. Discussion
A patient undergoing procedures that require a different way of securing the airways, or the use of another interface between the ventilator and the patient is problematic or impossible. It requires a specific approach and is often a challenge for the anesthesiologist. This area allows you to choose from multiple techniques/approaches and replace the routine procedure of conventional ventilation (CV) with C-HFJV. The decision to use C-HFJV presupposes extensive knowledge of the principles of its operation, consistent selection of suitable patients, and the ability to promptly solve the complications that arise. At the same time, in addition to theoretical knowledge, the anesthesiologist is required to have manual skills, the ability to foresee, have a backup plan, deal with critical situations, and have a sense of teamwork.
Several studies have compared different options for ventilation of patients undergoing surgical procedures in the area of the larynx, bronchoscopy, dilatation tracheostomy, Fantoni tracheostomy, and thoracic surgery with the aim of finding the optimal technique for maintaining airway patency, ensuring safe and effective ventilation with optimal access to the operative field [
1,
5]. But these studies were mostly aimed at evaluating safety and effectiveness [
7]. During bronchoscopic treatment of airways in hypoxic patients (bronchopneumonia, CARDS, etc.), the risk of further hypoxia during this type of instrumental procedure is reduced.
Among the most common complications in the past was barotrauma, which was common, especially in the early days of using high-frequency ventilation. It occurs as a result of airway obstruction and blockage of free gas expiration [
12]. Unlike manual ventilators, the automatic high-frequency jet ventilator has a "total stop" automatic shutdown system in case of exceeding the set pressure limit in the airways, therefore it is necessary to monitor the pressure in the airways with a measuring catheter. The safety of patients with C-HFJV during the procedure was ensured by the use of adequate monitoring of vital functions [
5]. However, the possibility of air contamination by virus-infected cells during C-HFJV still remains under discussion.
The thin insufflation catheter enables much better visualization of the space compared to the endotracheal cannula (diameter 6.5-7.5 mm - internal dimension). Repeated insertion of a Kleinsasser catheter can be avoided, compared to the endotracheal tube. This is especially important in the case of oncologic surgery, where good orientation and uninterrupted surgical performance are essential for the excision of the tumor and its edges free of tumorous cells.
The basic requirement for an anesthesiologist is to ensure high-quality hypnosis, analgesia, amnesia, and muscle relaxation (for surgical procedures). They also require control of the airways, safe ventilation of the lungs, and high-quality monitoring of vital functions. The consumption of anesthetics is usually higher in the C-HFJV group compared to the group of intubated patients, due to the effort to ensure deep anesthesia and relaxation as a prevention of laryngospasm. As a result, the duration of anesthesia is usually longer in patients ventilated with C-HFJV [
1].
Recommendations for the practice
Based on our clinical experience, simulations of the lungs model as well as the results of studies, we would like to provide some recommendations for work with C-HFJV for practice:
The C-HFJV method is safe and preferred by surgeons, even in the case of airway obstruction of various degrees and locations.
The insufflation catheter must be inserted deep enough (6-7 cm below the vocal cords) and well fixed, usually in the corner of the mouth.
It is necessary to maintain a sufficient depth of anesthesia and sufficient relaxation to prevent cough and laryngospasm, and regularly check the position of the catheter.
Catheter insertion must take place under visual control, as blind insertion can result in dislocation into the esophagus and its injury.
The position of the catheter should be checked regularly, especially when handling surgical instruments.
Before the insertion, in the period when there is no diagnostic, or surgical instrument present, it is necessary to ensure the free passage of expired gases by using an airline.
The catheter must contain a measurement channel for measuring airway pressure, as well as a "total stop" system, i.e. the ventilator is stopped when the maximum pressure in the airways, chosen by the doctor, is exceeded.
The methodology requires the cooperation of an experienced anesthesiologist and surgeon.
5. Conclusions
Catheter methods of HFJV ventilation have proven to be very effective ALV methods in technical experimental conditions as well as in clinical applications. Our aim was to assess and clarify application methodologies of catheter HFJV ventilation, its biophysical principles of function, as well as solutions to prevent barotrauma. Using C-HFJV with a double-lumen ventilation catheter for diagnostic procedures as well as surgical procedures can be applied with several HGJV ventilators, such as Paravent PATe, Paravent V from Kalas Medical, s.r.o., or Monsoon from Acutronic. Despite the fact that many patients suffer from preoperative mild hypoxia and hypercapnia, C-HFJV is able to largely eliminate this pathology even in patients with bronchopneumonia caused by "classic" microorganisms, as well as by COVID-19 or other viruses. In conclusion, double-lumen catheter ventilation brings a significant contribution to clinical practice.
Author Contributions
Conceptualization, P.M. and S.H..; methodology, L.K and P.T.; validation, D.M., P.T. and L.K..; formal analysis, M.P..; resources, D.M..; writing—original draft preparation, P.T..; writing—review and editing, M.P and S.H..; project administration, P.K..; funding acquisition, P.M. All authors have read and agreed to the published version of the manuscript.
Funding
This publication was created with the help of the operational program: Integrated infrastructure for the project "Technological adaptation of the high-frequency jet ventilator PARAVENT V for the improvement of the existing parameters of pulmonary ventilation for the therapy of patients suffering from the disease COVID-19", ITMS 313011AUL1, acronym PARAVENT-V-COVID, co-financed from the resources of the European fund of regional development.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- PAULÍKOVÁ M.: Catheter high-frequency nozzle lung ventilation and its use in ORL surgery / Katétrová vysokofrekvenčná dýzová ventilácia pľúc a jej použitie v ORL chirurgii. Anestéziologia a intenzívna medicína 2017;6:46-49.
- KLAIN M., SMITH RB.: High frequency percutaneous transtracheal jet ventilation. Crit Care Med. 1977;6:280-287.
- BRYCHTA O. : High Frequency Ventilation Research Final Report / Záverečná správa z výskumu vysokofrekvenčnej ventilácie. Konštrukta Trenčín. 1985.
- BIRO, P. : Carbon dioxide elimination during high-frequency jet ventilation for rigid bronchoscopy, British Journal of Anaesthesia 2000 84:635-7. [CrossRef]
- TÖRÖK, P. A KOL.: Theoretical and clinical foundations of high-frequency nozzle ventilation of the Czech-Slovak type and methods and techniques of artificial lung ventilation derived from it / Teoretické a klinické základy vysokofrekvenčnej dýzovej ventilácie česko-slovenského typu a od nej odvodených spôsobov a techník umelej ventilácie pľúc, Osveta 2013.
- SANDERS RD.: Two ventilating attachments for bronchoscopes, Del Med J 1967; 178-80.
- DAVIES JM. et al: The Hunsaker Mon-Jet tube with jet ventilation is effective for microlaryngeal surgery, Can J Anest 2009;56:284-290. [CrossRef]
- PATEL C, DIBA A.: Measuring tracheal airway pressures during transtracheal jet ventilation: an observational study. Anaesthesia 2004;59:248-51. [CrossRef]
- PATEL A, RUBIN JS.: The difficult airway: the use of subglottic jet ventilation for larynge-al surgery. Logoped Phoniatr Vocol 2008;33:22-24. [CrossRef]
- BIRO, P. : Jet ventilation for surgical interventions in the upper airway, Anesthesiolo¬gyClin 2010;28:397-409. [CrossRef]
- RYBÁR, D. : Lactate and its clearance as a marker of shock after cardiac surgery / Laktát a jeho klírens ako marker šoku po kardiochirurgických výkonoch. Anestéziológia a intenzívna medicína 2016; (5), 2, str.
- GALMÉN K, HARBUT P, FREEDMAN J, JAKOBSSON JG.: The use of high-frequency ventilation during general anaesthesia: An update. F1000 Research. 2017;6:756. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).