1. Introduction
Patients with neuromuscular diseases such as muscular dystrophy and spinal muscular atrophy usually show progressive scoliosis called neuromuscular scoliosis (NMS). Some patients with NMS exhibit an impaired quality of life, including sitting difficulty, pulmonary dysfunction, and cardiac dysfunction, and usually require surgery [
1,
2]. Reportedly, posterior spinal correction and fusion surgery for NMS have good correction and clinical outcomes, including the inhibition of scoliosis progression and improvement in sitting difficulty [
2,
3]. However, many patients with NMS show pulmonary and cardiac dysfunction preoperatively, and several authors have reported high perioperative complication rates [
4,
5]. We also previously reported that 24% of patients with NMS showed perioperative complications, and patients with major perioperative complications exhibited severe restrictive ventilatory impairment preoperatively [
6]. Therefore, early intervention, including spinal fusion surgery, is recommended before pulmonary function impairment becomes severe.
However, some patients with NMS show severe scoliosis at the time of consultation and are difficult to treat. For the severe spinal deformity, posterior spinal fusion (PSF) surgery combined with anterior release, or/and intraoperative halo-femoral traction, or/and preoperative halo-gravity traction would be effective. However, surgery for patients with severe NMS is usually highly invasive, including a long duration of surgery and a high amount of blood loss. Especially, there are several concerns about these invasive procedures for patients with fragile condition. We performed PSF surgery without any anterior relase, pre and intraoperative traction in all NMS patients, even in patients with severe spinal deformity. This study aimed to evaluate the outcomes of PSF only surgery in patients with severe NMS with a Cobb angle > 100 °.
2. Materials and Methods
2.1. Patient population
A total of 30 patients (13 boys and 17 girls) who underwent PSF only surgery for scoliosis with a Cobb angle >100 ° from 2006 to 2020 at a minimum 1-year follow-up were included. The mean age at surgery was 13.8 years (range, 9–17 years), and the mean follow-up period was 57.9 months (range, 12–135 months). The diagnoses included 11 patients with spinal muscle atrophy, 8 patients with Duchenne type muscle dystrophy, and 11 patients with other types of atrophy, including Fukuyama type muscle dystrophy, Ulrich type muscle dystrophy, and central core disease. All the patients had a flaccid-type neuromuscular disease. Most patients could communicate without trouble; however, some had mental retardation. All patients underwent preoperative pulmonary function evaluation via spirometry and cardiac function evaluation via echocardiography. All patients experienced sitting difficulty and back pain due to NMS. None of the patients was excluded because of poor preoperative physical status.
2.2. Surgical procedure
All surgeries were performed under general anesthesia. Motor-evoked potentials were used to monitor the spinal cord function in all cases. In addition, we performed an autotransfusion as preoperative storage, while an intraoperative collection was performed during surgery. An incision was made in the midline of the back, and the spinal structure was exposed from the upper thoracic spine to the sacrum or pelvis. After removing all soft tissues, instrumentation was performed using pedicle screws, hooks, and sublaminar cables (Nesplon Cable System; Alfresa, Tokyo, Japan). Fusion levels ranged from T4 to L5 until May 2018 but were determined in individual cases based on curve flexibility or apex and physical status from June 2018. We then obtained local autograft bone from the spinous processes, lower facet joints, and transverse processes. Ponte osteotomy was performed on several segments (usually four or five) around the scoliosis apex to release the spinal structure and obtain curve flexibility. In all cases, spinal deformities were corrected using two combined techniques: a cantilever technique and a rod rotation technique. After correction, all laminae and facet joints were decorticated, and a local autograft bone mixed with bioresorbable bone graft was placed. Finally, the wound was sutured in three layers, and drainage tubes were placed. In all cases, we did not perform any anterior release surgery, preoperative and intraoperative traction. We attempted extubation as soon as possible after surgery when the patients could ventilate their lungs spontaneously to prevent respiratory dependency.
2.3. Measurements
We reviewed age at surgery, preoperative %VC and FEV1.0 (%) for pulmonary function, preoperative ejection fraction (EF) for cardiac function, duration of surgery, blood loss, perioperative complications, upper instrumented vertebra (UIV), lower instrumented vertebra (LIV), and radiographic findings including Cobb angle and pelvic obliquity (PO) in the sitting position preoperatively, 1 month postoperatively, and at the final follow-up. The correction rates of Cobb angle and PO were calculated as follows:
In addition, the correction loss of the Cobb angle and PO were calculated as follows:
Correction loss (degrees) = angle at final follow-up - 1 month postoperative angle
2.4. Statistics
Repeated measures analysis of variance (ANOVA) was performed to compare the radiographic findings preoperatively, 1 month postoperatively, and at the final follow-up. Post hoc analysis was performed using Tukey’s test for multiple comparisons. Furthermore, we divided the patients into two groups: the LIV was an L5 group (L5), and the LIV was the pelvis group (pelvis). Age at surgery, preoperative %VC and FEV1.0 (%), preoperative EF, duration of surgery, blood loss, and radiographic findings, including Cobb angle and PO, were compared between the two groups. Leven's test was used to assess the equality of the variance of the variables of interest. The Mann–Whitney U test was applied to variables with unequal variances. For variables with equal variances, an unpaired t-test was used. Statistical significance was set at P < 0.05.
2.5. Ethics
Ethical approval from our institutional review board (IRB) was obtained for this study. This study was conducted in accordance with the ethical principles specified in the 1964 Declaration of Helsinki and its later amendments.
3. Results
The patient characteristics and surgical outcomes are described in Table 1. The mean preoperative %VC was 34.1%, FEV1.0 was 91.5%, and EF was 66.1%. Preoperative %VC in patients with severe NMS was extremely low, although preoperative FEV1.0 and EF were maintained. All patients reported difficulty sitting and back pain due to severe scoliosis preoperatively. For surgery, the UIV was T3 in 1 case, T4 in 25 cases, and T5 in four cases. The LIV was L5 in 24 cases and the pelvis in six cases. The preoperative and postoperative mean Cobb angles were 121.9 °and 63.8 °, respectively, and the mean correction rate was 48.5%. The preoperative and postoperative mean PO was 42.9 ° and 25.5 °, respectively, and the mean correction rate was 42.0%. In addition, the duration of surgery was 338.6 min, and blood loss was 1,441.1 mL, indicating the need for a highly invasive surgery (Table 1). Postoperatively, all patients showed improvement in sitting and back pain. There were 8 cases (24%) with perioperative complications, including pneumonia, CO2 narcosis, urinary tract infection, hemodynamic instability, and surgical site infection. Four of these 8 cases had respiratory complications (Table 2).
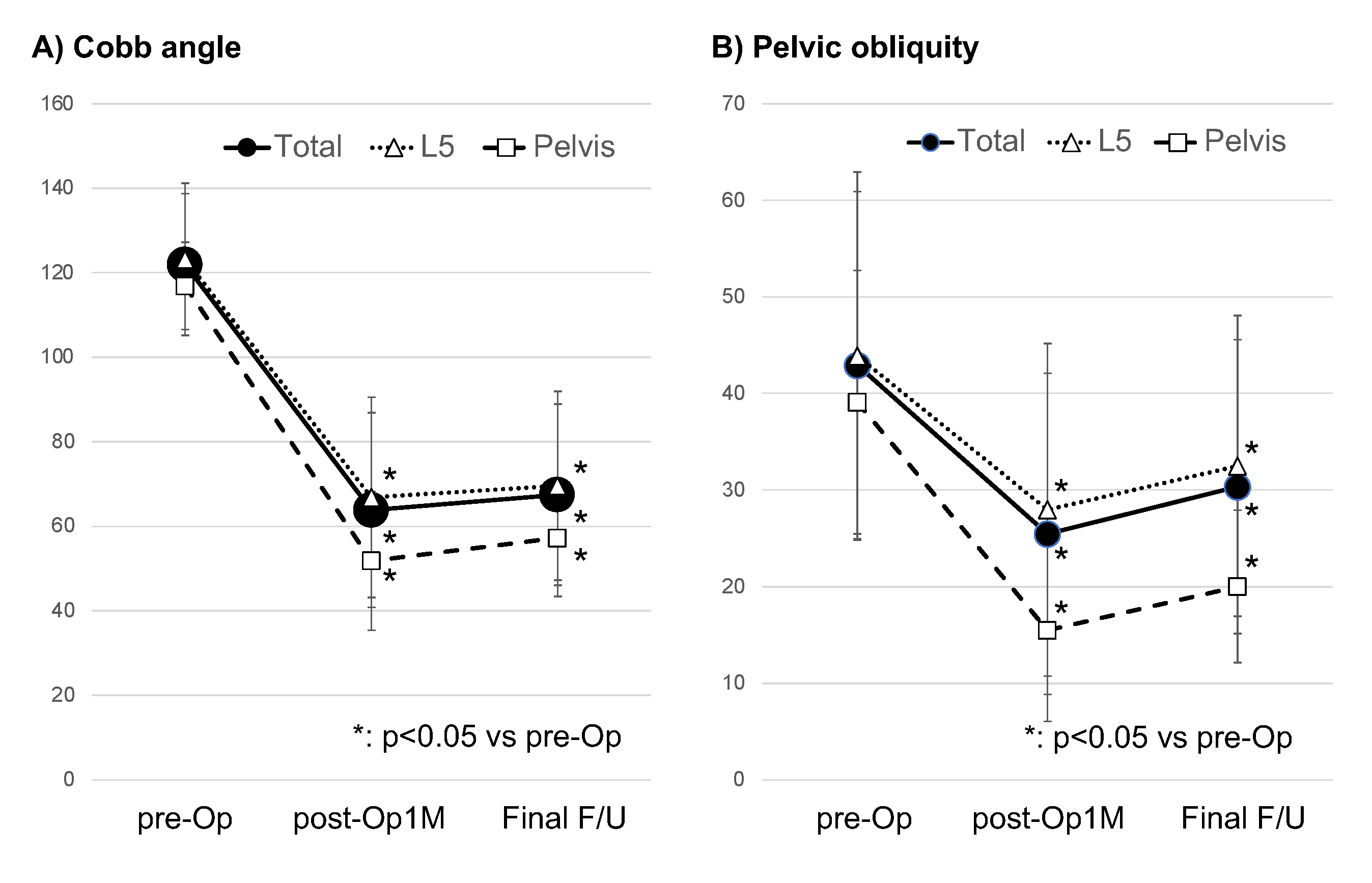
When we divided the patients into two groups, the L5 group and the pelvis group, the duration of surgery and PO correction rate in the pelvis group were significantly higher than that of the L5 group. Furthermore, correction loss of the Cobb angle and PO in the pelvis group was significantly lower than in the L5 group. However, there were no significant differences in age at surgery, preoperative %VC, preoperative FEV1.0, preoperative EF, preoperative Cobb angle, preoperative PO, blood loss, and correction rate of the Cobb angle between both groups (Table 3) (
Figure 1).
Figure 1.
A) Cobb angle and B) Pelvic obliquity preoperatively, 1 month postoperatively, and at the final follow-up in whole cases, or L5 groups, or pelvis group. pre-Op: preoperative, post-Op 1M: 1 month postoperative, Final F/U: at final follow up.
Figure 1.
A) Cobb angle and B) Pelvic obliquity preoperatively, 1 month postoperatively, and at the final follow-up in whole cases, or L5 groups, or pelvis group. pre-Op: preoperative, post-Op 1M: 1 month postoperative, Final F/U: at final follow up.
Table 1.
Patient characteristics and surgical outcomes.
Table 1.
Patient characteristics and surgical outcomes.
| |
mean |
SD |
| age (years) |
13.833 |
2.306 |
| %VC (%) |
34.108 |
20.535 |
| FEV1.0 (%) |
91.524 |
6.780 |
| EF (%) |
66.089 |
10.066 |
| pre-Op Cobb (°) |
121.910 |
16.792 |
| pre-Op PO (°) |
42.920 |
17.990 |
| Duration of surgery (min) |
338.600 |
74.289 |
| Blood loss (mL) |
1441.100 |
782.407 |
| post-Op1M Cobb (°) |
63.840 |
23.008 |
| post-Op1M PO (°) |
25.463 |
16.615 |
| CR of Cobb (%) |
48.513 |
13.404 |
| CR of PO (%) |
41.956 |
25.123 |
| CL of Cobb (°) |
4.430 |
7.311 |
| CL of PO (°) |
4.947 |
6.388 |
| F/U Duration (M) |
57.867 |
40.956 |
Table 2.
Perioperative complications.
Table 2.
Perioperative complications.
| |
total |
L5 |
pelvis |
| Complications |
8 |
6 |
2 |
| Pneumonia |
3 |
2 |
1 |
| CO2 narcosis |
1 |
1 |
|
| Urinary tract infection |
2 |
1 |
1 |
| Hemodynamically unstable |
1 |
1 |
|
| surgical site infection |
1 |
1 |
|
Table 2.
Comparisons of patient characteristics and surgical outcomes between the L5 group and the pelvis group.
Table 2.
Comparisons of patient characteristics and surgical outcomes between the L5 group and the pelvis group.
| |
L5 |
pelvis |
p-value |
| |
mean |
SD |
mean |
SD |
| age (years) |
14.167 |
2.390 |
12.500 |
1.378 |
0.115 |
| %VC (%) |
31.904 |
19.386 |
51.333 |
25.007 |
0.125 |
| FEV1.0 (%) |
92.391 |
6.305 |
85.000 |
8.718 |
0.078 |
| EF (%) |
64.238 |
9.985 |
72.333 |
9.985 |
0.081 |
| pre-Op Cobb (°) |
123.167 |
18.004 |
116.883 |
10.319 |
0.422 |
| pre-Op PO (°) |
43.875 |
19.051 |
39.100 |
13.623 |
0.570 |
| Duration of surgery (min) |
323.042 |
71.289 |
400.833 |
53.124 |
0.019 |
| Blood loss (mL) |
1558.583 |
820.464 |
971.167 |
350.328 |
0.101 |
| post-Op1M Cobb (°) |
66.846 |
23.699 |
51.817 |
16.427 |
0.156 |
| post-Op1M PO (°) |
27.958 |
17.211 |
15.483 |
9.436 |
0.101 |
| CR of Cobb (%) |
46.736 |
12.997 |
55.621 |
13.758 |
0.150 |
| CR of PO (%) |
37.265 |
24.272 |
60.720 |
20.557 |
0.038 |
| CL of Cobb (°) |
5.275 |
7.968 |
1.050 |
0.903 |
0.013 |
| CL of PO (°) |
5.763 |
6.891 |
1.683 |
1.507 |
0.018 |
| F/U Duration (M) |
68.375 |
39.097 |
15.833 |
6.882 |
0.003 |
4. Discussion
In this study, patients with severe NMS had extremely low preoperative %VC. PSF surgery for severe NMS showed satisfactory outcomes, although they required highly invasive surgery with a high complication rate. PSF surgery to the pelvis showed a longer duration of surgery, higher PO correction rate, and lower correction loss of Cobb angle and PO compared to fusion surgery to L5.
Regarding the characteristics of patients with severe NMS in this study, patients with severe NMS with Cobb angle > 100 °showed extremely low %VC preoperatively. Several studies on idiopathic scoliosis patients have reported that progressing scoliosis and increasing Cobb angle were associated with pulmonary dysfunction, especially reduced %VC [
7,
8] . Furthermore, several studies on neuromuscular diseases have reported that patients with scoliosis showed low pulmonary function, especially restrictive ventilatory impairment [
6,
9,
10]. In their review of NMS patients, Mayer et al. reported altered respiratory mechanics due to scoliosis and decreased muscle strength due to neuromuscular diseases, leading to severe pulmonary dysfunction [
10]. These findings indicated that patients with severe NMS showed severe restrictive ventilatory impairment.
Regarding the surgery for severe NMS, patients with severe NMS required high invasive surgery with a longer duration of surgery and a high amount of blood loss, and the perioperative complication rate was 24% in this study. Moreover, many perioperative complications are also associated with pulmonary complications. Toombs et al. reported the following in their study of idiopathic scoliosis patients: Increased spinal curve magnitude might lead to a longer duration of surgery and more perioperative complications [
11]. No reports have elucidated the relationship between spinal curve magnitude and the invasiveness of surgery in patients with NMS. However, patients with NMS reportedly show pulmonary dysfunction, which might be a risk factor for NMS surgery [
6,
11,
12]. In addition, several authors have reported that the perioperative complication rate of NMS surgery was 24–68% [
4,
5,
6,
13,
14], similar to the results of this study. Previous reports also indicated that most perioperative complications are associated with respiration [
4,
6,
13], suggesting that patients with severe NMS require highly invasive surgery with a high complication rate. In particular, when treating patients with severe NMS, attention should be paid to perioperative respiratory complications.
Regarding the surgical strategy for severe NMS, anterior release and posterior fusion surgery, intraoperative halo-femoral traction, and preoperative halo-gravity traction have been reported to be effective in severe scoliosis surgery, including NMS and idiopathic scoliosis [
15,
16,
17,
18,
19,
20,
21,
22,
23]. Auerbach et al. reported that good PO correction in patients with NMS with larger and less flexible curves could be achieved using anterior release and posterior fusion surgery [
21]. In contrast, several authors have reported that PSF surgery with intraoperative halo-femoral traction for scoliosis with spastic neuromuscular diseases, including cerebral palsy, was less invasive, including shorter operation time, smaller amount of blood loss, and lower frequency of respiratory complications than PSF surgery with anterior release[
22,
23]. According to these previous reports, PSF surgery with intraoperative halo-femoral traction for severe NMS is superior in efficacy and safety. However, there were concerns that intraoperative traction induces neuromonitoring signal changes and neurological deficit [
24]. Furthermore, in this study, PSF surgery without anterior release or intraoperative traction achieved acceptable scoliosis correction and improved clinical findings. Therefore, considering the results of this study, PSF only surgery for severe NMS might be sufficient.
For the fusion level of NMS surgery in this study, fusion surgery to the pelvis showed a longer duration of surgery, higher PO correction rate, and lower correction loss of Cobb angle and PO than fusion surgery to L5. We previously reported that fusion surgery to L5 for NMS showed satisfactory outcomes, including good correction and a high level of safety [
25,
26]. However, there were some limitations in ending instrumentation for NMS surgery at L5. We also reported that patients with a larger preoperative Cobb angle might not achieve adequate spinal and pelvic correction by fusion only to L5 [
27]. Tøndevold reported that pelvic fixation for NMS surgery showed good correction and decreased the risk of correction loss [
28]. According to these previous reports, pelvic fixation surgery would be superior in terms of good correction and low correction loss in patients with severe NMS. However, there were some concerns regarding pelvic fixation from a safety viewpoint. Hyun et al. reported that pelvic fixation requires extensive surgical exposure, associated with a high risk of blood loss and infection [
29]. These findings indicate that fixation to the pelvis in patients with severe NMS appears to have a longer operation duration, although good PO correction and low correction loss were observed. Furthermore, when treating patients with severe NMS, there is a need to balance efficacy and safety depending on patient characteristics, including preoperative pulmonary function, curve spinal flexibility, and neuromuscular disease (flaccid or spastic type). In addition, we considered an early intervention for NMS before it becomes a severe deformity requiring highly invasive surgery should be needed.
The study had some limitations. First, only a PSF surgery was performed. We did not have any data on findings from combined anterior release surgery or interoperative traction. Second, we could not evaluate the clinical findings using any questionnaire, although all patients showed improvement in sitting difficulty and back pain. Further studies are needed to evaluate the quality of life of these patients. Third, which is a critical issue, most previous reports of NMS targeted patients with spastic neuromuscular diseases, including cerebral palsy, or were included in each type of neuromuscular disease, whereas all the patients in this study had the flaccid-type neuromuscular disease. There might be some differences in surgical strategy and clinical outcomes between the spastic and flaccid types. Further studies targeting patients with only flaccid-type neuromuscular diseases are needed.
5. Conclusions
Patients with severe NMS demonstrated severe preoperative restrictive ventilatory impairments. PSF only surgery for severe NMS showed satisfactory outcomes, although highly invasive surgery was required. Instrumentation and fusion to the pelvis for severe scoliosis in patients with NMS showed good PO correction and low correction loss of Cobb angle and PO, but a longer duration of surgery.
Author Contributions
MM drafted the manuscript and conceived this study; WS, YM, NT, and TI participated in its design and coordination and drafted the manuscript; ES, KU, and TA helped to revise the manuscript and carried out statistical analysis; ShiI, AK, ShoI, and YY collected data from this study; AT revised the manuscript; MT and GI conceived the study and participated in its design and coordination. All the authors have read and approved the final manuscript.
Funding
This investigation was supported in part by the Intramural Research Grant (29-3) for Neurological and Psychiatric Disorders of NCNP..
Institutional Review Board Statement
Ethical approval from Institutional Review Board in Kitasato University was obtained for this study, which was conducted in accordance with the ethical principles specified in the 1964 Declaration of Helsinki and its later amendments. The approval code is #B16-236.
Informed Consent Statement
Opt-out consent were obtained in the current study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank Motoki Makabe for their assistance with this study.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- Chong, H.S.; Moon, E.S.; Kim, H.S.; Ankur, N.; Park, J.O.; Kim, J.Y.; Kho, P.A.; Moon, S.H.; Lee, H.M.; Seul, N.H. Comparison between Operated Muscular Dystrophy and Spinal Muscular Atrophy Patients in terms of Radiological, Pulmonary and Functional Outcomes. Asian Spine J 2010, 4, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Takaso, M.; Nakazawa, T.; Imura, T.; Okada, T.; Toyama, M.; Ueno, M.; Fukushima, K.; Saito, W.; Minatani, A.; Miyajima, G.; et al. Two-year results for scoliosis secondary to Duchenne muscular dystrophy fused to lumbar 5 with segmental pedicle screw instrumentation. J Orthop Sci 2010, 15, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Hahn, F.; Hauser, D.; Espinosa, N.; Blumenthal, S.; Min, K. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J 2008, 17, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Modi, H.N.; Suh, S.W.; Yang, J.H.; Cho, J.W.; Hong, J.Y.; Singh, S.U.; Jain, S. Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis 2009, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Bendon, A.A.; George, K.A.; Patel, D. Perioperative complications and outcomes in children with cerebral palsy undergoing scoliosis surgery. Paediatr Anaesth 2016, 26, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Miyagi, M.; Saito, W.; Imura, T.; Inoue, G.; Nakazawa, T.; Shirasawa, E.; Uchida, K.; Akazawa, T.; Takahira, N.; et al. Perioperative Complications in Posterior Spinal Fusion Surgery for Neuromuscular Scoliosis. Spine Surg Relat Res 2018, 2, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Kearon, C.; Viviani, G.R.; Kirkley, A.; Killian, K.J. Factors determining pulmonary function in adolescent idiopathic thoracic scoliosis. Am Rev Respir Dis 1993, 148, 288–294. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Zavala, D.C.; Ponseti, I.V. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am 1981, 63, 702–712. [Google Scholar] [CrossRef]
- Merlini, L.; Granata, C.; Bonfiglioli, S.; Marini, M.L.; Cervellati, S.; Savini, R. Scoliosis in spinal muscular atrophy: natural history and management. Dev Med Child Neurol 1989, 31, 501–508. [Google Scholar] [CrossRef]
- Mayer, O.H. Scoliosis and the impact in neuromuscular disease. Paediatr Respir Rev 2015, 16, 35–42. [Google Scholar] [CrossRef]
- Toombs, C.; Lonner, B.; Fazal, A.; Boachie-Adjei, O.; Bastrom, T.; Pellise, F.; Ramadan, M.; Koptan, W.; ElMiligui, Y.; Zhu, F.; et al. The Adolescent Idiopathic Scoliosis International Disease Severity Study: Do Operative Curve Magnitude and Complications Vary by Country? Spine Deform 2019, 7, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.R.; Suh, S.W.; Lee, I.O. Preoperative predictors of postoperative pulmonary complications in neuromuscular scoliosis. J Orthop Sci 2011, 16, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Sarwahi, V.; Sarwark, J.F.; Schafer, M.F.; Backer, C.; Lee, M.; King, E.C.; Aminian, A.; Grayhack, J.J. Standards in anterior spine surgery in pediatric patients with neuromuscular scoliosis. J Pediatr Orthop 2001, 21, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Benson, E.R.; Thomson, J.D.; Smith, B.G.; Banta, J.V. Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine (Phila Pa 1976) 1998, 23, 2308–2317. [Google Scholar] [CrossRef] [PubMed]
- Delman, C.; Cage, J.M.; Lausé, G.; Roberto, R.; Gupta, M.C.; Klineberg, E. Anterior and Posterior Fusion for Large, Rigid Idiopathic Scoliosis: Does Implant Density Matter? World Neurosurg 2020, 134, e37–e45. [Google Scholar] [CrossRef] [PubMed]
- Teixeira da Silva, L.E.; de Barros, A.G.; de Azevedo, G.B. Management of severe and rigid idiopathic scoliosis. Eur J Orthop Surg Traumatol 2015, 25 Suppl 1, S7–12. [Google Scholar] [CrossRef]
- Takeshita, K.; Lenke, L.G.; Bridwell, K.H.; Kim, Y.J.; Sides, B.; Hensley, M. Analysis of patients with nonambulatory neuromuscular scoliosis surgically treated to the pelvis with intraoperative halo-femoral traction. Spine (Phila Pa 1976) 2006, 31, 2381–2385. [Google Scholar] [CrossRef] [PubMed]
- Tøndevold, N.; Bari, T.J.; Andersen, T.B.; Gehrchen, M. Intraoperative traction in neuromuscular scoliosis surgery improves major curve correction when fusing to L5. Spine Deform 2021, 9, 769–776. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, G.; Guo, C.; Liu, J.; Tang, M. Analysis of the corrective contribution of strong halo-femoral traction in the treatment of severe rigid nonidiopathic scoliosis. J Orthop Surg Res 2020, 15, 567. [Google Scholar] [CrossRef]
- Mejabi, J.O.; Sergeenko, O.M.; Ryabykh, S.O. Correction using Halo Gravity Traction for Severe Rigid Neuromuscular Scoliosis: A Report of Three Cases. Malays Orthop J 2019, 13, 49–53. [Google Scholar] [CrossRef]
- Auerbach, J.D.; Spiegel, D.A.; Zgonis, M.H.; Reddy, S.C.; Drummond, D.S.; Dormans, J.P.; Flynn, J.M. The correction of pelvic obliquity in patients with cerebral palsy and neuromuscular scoliosis: is there a benefit of anterior release prior to posterior spinal arthrodesis? Spine (Phila Pa 1976) 2009, 34, E766–774. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.J.; Yaszay, B.; Pahys, J.M.; Singla, A.; Miyanji, F.; Shah, S.A.; Sponseller, P.D.; Newton, P.O.; Flynn, J.M.; Cahill, P.J. Intraoperative Traction May Be a Viable Alternative to Anterior Surgery in Cerebral Palsy Scoliosis ≥100 Degrees. J Pediatr Orthop 2018, 38, e278–e284. [Google Scholar] [CrossRef] [PubMed]
- Keeler, K.A.; Lenke, L.G.; Good, C.R.; Bridwell, K.H.; Sides, B.; Luhmann, S.J. Spinal fusion for spastic neuromuscular scoliosis: is anterior releasing necessary when intraoperative halo-femoral traction is used? Spine (Phila Pa 1976) 2010, 35, E427–433. [Google Scholar] [CrossRef] [PubMed]
- LaMothe, J.M.; Al Sayegh, S.; Parsons, D.L.; Ferri-de-Barros, F. The Use of Intraoperative Traction in Pediatric Scoliosis Surgery: A Systematic Review. Spine Deform 2015, 3, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Takaso, M.; Nakazawa, T.; Imura, T.; Ueno, M.; Saito, W.; Shintani, R.; Takahashi, K.; Yamazaki, M.; Ohtori, S.; Okamoto, M.; et al. Can the caudal extent of fusion in the surgical treatment of scoliosis in Duchenne muscular dystrophy be stopped at lumbar 5? Eur Spine J 2010, 19, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Takei, S.; Miyagi, M.; Saito, W.; Imura, T.; Inoue, G.; Nakazawa, T.; Shirasawa, E.; Uchida, K.; Akazawa, T.; Takahira, N.; et al. Safety and Efficacy of Treatment for Scolios Is Secondary to Spinal Muscular Atrophy Fused to Lumbar 5 Level. Spine Surg Relat Res 2018, 2, 294–298. [Google Scholar] [CrossRef]
- Saito, W.; Inoue, G.; Shirasawa, E.; Imura, T.; Nakazawa, T.; Miyagi, M.; Kawakubo, A.; Uchida, K.; Kotani, T.; Akazawa, T.; et al. Limitations of posterior spinal fusion to L5 for flaccid neuromuscular scoliosis focusing on pelvic obliquity. Spine Deform 2021, 9, 559–565. [Google Scholar] [CrossRef]
- Tøndevold, N.; Lastikka, M.; Andersen, T.; Gehrchen, M.; Helenius, I. Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Joint J 2020, 102-b, 261–267. [Google Scholar] [CrossRef]
- Hyun, S.J.; Rhim, S.C.; Kim, Y.J.; Kim, Y.B. A mid-term follow-up result of spinopelvic fixation using iliac screws for lumbosacral fusion. J Korean Neurosurg Soc 2010, 48, 347–353. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).