1. Introduction
There is now a fairly extensive literature examining cancer related cognitive dysfunction (CRCD) in cross-sectional designs [
1,
2,
3,
4,
5] as well as in prospective, longitudinal studies that report effects in short-interval follow-up assessments following treatment [
6,
7,
8,
9,
10,
11,
12]. Longitudinal studies also aim to examine whether cancer and cancer treatment alter biological and cognitive aging trajectories, potentially exacerbating the decline associated with normal cognitive aging. While suggestive, there are limitations to previous research examining these potential trajectories. Existing studies typically follow survivors with repeated testing over a relatively short window around the time of treatment and after (2-5 years) in which 1) little cognitive aging is expected, 2) practice effects due to repeated testing lead to the appearance of increasing cognitive performance with age, and 3) selective attrition, in which the most robust of the sample continue on study, obscures expected cognitive aging trends.
Long-term, there is evidence of persistent CRCD in cross-sectional studies at 5 [
13], 10 [
4], and 20 [
14] years post-treatment, although little is known regarding why or how cognition changes, i.e., the dynamics of the rate and magnitude of change, over developmentally meaningful intervals. This is an important gap since etiologies of cognitive dysfunction around the time of treatment may be distinct from potentially modifiable factors at longer intervals post-treatment. Aging trajectories may be influenced by multiple factors, with a growing body of research examining deficit accumulation and its effect. Deficit accumulation is characterized by comorbidity burden, polypharmacy, social detriments of disease (e.g., smoking, obesity), psychological disturbance, and functional limitations / declines in activities of daily living [
15]. A relationship between frailty and cognitive impairment has been reported in the geriatric literature [
16,
17,
18]. Cancer treatment is associated with an acceleration in the accumulation of other comorbidities and deficits over longer intervals [
19,
20,
21,
22], and recent work from our group has identified an association of deficit accumulation with cognitive function in breast cancer patients [
23,
24,
25]. In an earlier study, we found that comorbidity burden was higher in patients and associated with baseline cognitive function prior to adjuvant treatment.
23 In a study of longer-term survivors, survivors had higher deficit accumulation, and this exerted a greater effect on cognition compared to controls [
24]. In a recent study, we found that cognitive differences between older breast cancer survivors 5 to 15 years post treatment and non-cancer controls were largely mediated by increased deficit accumulation in survivors [
25]. This work focused on cognitive and deficit accumulation trajectories over a two-year interval and so was limited for the same reasons discussed above, i.e., repeated testing and short period of follow-up, and leaves open the dynamics of longer-term trajectories and association with deficit accumulation. Since deficit accumulation may be modifiable with appropriate preventative measures or managed with concurrent treatment, a better understanding of deficit accumulation and its long-term impact on cognition may improve outcomes for long-term survivors.
There are clear impediments to examining these longer-term outcomes longitudinally. Following survivors over a 10- to 20-year interval is logistically unfeasible and, like the limitations noted above in shorter interval studies, practice effects and selective attrition will distort the expected course of cognitive decline associated with age and survivorship. Practice effects are inherent in repeated cognitive testing [
26] and have a tendency to obscure age-related decline as a result of improving performance given previous experience with the measures [
27,
28]. The presence of practice effects may be especially problematic for the study of cognition in survivorship given our previous findings of initial learning and attention deficits in breast cancer survivors and evidence that repetition within and across testing sessions leads to steeper improvements in performance in survivors than in controls [
29]. As an alternative approach, the methods and analysis presented here stem from aging researchers, whose primary focus is on normal cognitive aging across the lifespan, that harnesses cross-sectional cognitive data to capture developmental changes over longer intervals. Previous work in normal cognitive aging has found that age-associated longitudinal and cross-sectional cognitive trajectories disagree, with the former exhibiting increases in performance with age and the latter exhibiting decreases [
27]. While the cross-sectional trend is intuitively more explicable, concerns have been raised about potential cohort effects in different age groups that may be confounded with age. These include early developmental variables, e.g., educational opportunities, nutritional access, acculturation, etc., that can result in differences in cognition between generational cohorts that confound the effects of age [
30] While a significant and robust finding in earlier work, there is increasing evidence that cohort effects, this pattern of increasing cognitive scores in successive generational cohorts over the 20
th century, has diminished as environmental factors have stabilized in developed countries [
31,
32], including the United States [
33]. Research from aging literature that disambiguates cohort and aging effects suggests that cohort effects have decreased [
27,
34] and with the inclusion of a non-cancer control group at matched ages any remaining cohort effect can be accounted for. Given the confounding effects of repeated longitudinal assessment on cognitive trajectories, selective attrition, and the logistical challenges in following individuals over aging intervals of interest (5-20 years), examining cross-sectional cognitive data across the lifespan and evaluating differences between survivors and controls may serve as a useful and accurate proxy indicator of how a history of cancer may alter cognitive aging trajectories.
The data reported here was collected as part of a collaboration between Memorial Sloan Kettering Cancer Center and City of Hope (PIs: Ahles; Hurria) that assessed cognition in controls and breast cancer survivors (age 60 or greater) who were all at least 5 years post-treatment and followed prospectively over 2 years with 4 timepoints at 8-month intervals [
35]. In this secondary analysis we examined data derived from the first time-point across a longer 5 to 15 year interval, in 4 quartiles, as a proxy indicator of how cognitive trajectories might be altered given a history of cancer and cancer treatment. We then compare these trends to longitudinally collected data over shorter intervals (2 years) to examine the potential distorting effects of repeated cognitive testing. Finally we examine the association of deficit accumulation with cognitive differences between survivors and non-cancer controls across the age span.
2. Materials and Methods
Participants. Breast cancer survivors were identified through the survivorship clinics at Memorial Sloan Kettering Cancer Center (MSK) and City of Hope Comprehensive Cancer Center (COH), supplemented at each site by recruitment through the Army of Women. Survivors were eligible if they were diagnosed with stage 0-III breast cancer, treated at age 60 or above, were 5 to 15-year disease-free survivors at the time of enrollment and provided informed consent. Survivors were excluded based on the following criteria: score of 11 or greater (indicating risk of dementia) on the Blessed Orientation-Memory-Concentration (BOMC) Test, previous history of cancer (except non-melanoma skin cancer), treatment with chemotherapy for non-cancer conditions, neurobehavioral risk factors, including history of neurologic disorder (e.g., seizure or dementia), alcohol/substance abuse, head trauma requiring hospitalization or evidence of structural brain changes on imaging; and severe psychiatric disorder (e.g., schizophrenia, bipolar disorder). Female non-cancer controls who met the same inclusion criteria (except for diagnosis of cancer) and exclusion criteria were recruited through community advertisement and the Army of Women. Non-cancer controls were frequency matched on age and education. All methods and procedures were approved by the institutional review boards of MSK and COH. Toward the end of the study, the age at diagnosis was lowered to 55 to increase the number of survivors who had been treated with chemotherapy. Twenty-three participants who had been treated between 55-60 were recruited and thus contribute to the overall cohort of N=486 women.
Measures. Assessments occurred at enrollment and at 8, 16, and 24-month follow-ups. The assessment battery included standardized neuropsychological tests, self-report of cognitive function, and components of the Comprehensive Geriatric Assessment [
36] which were used to calculate the Deficit Accumulation Frailty Index (DAFI). The neuropsychological measures were categorized into domains based on previous studies [
36] and clinical judgment of the neuropsychologists involved with the study (JCR, ER, SP) informed by a factor analysis.
Each test score was first standardized (z-score) according to the healthy control group, and then a mean of standardized scores within the domain calculated for each participant. Individual test scores were checked for deviation from a normal distribution. For those that differed, the Box-Cox algorithm [
37] was used to determine a suitable power transformation prior to domain score calculations. Below are the tests administered categorized by domain:
Attention, Processing Speed, Executive Function: Digit Symbol [
38]; Trail Making A and B [
39]; DKEFS Color-Word Naming [
40]; NAB Digits Forward and Backward [
41]; NAB Driving Scenes [
41].
Learning and Memory: NAB List Learning [
41]: Trial 1, Semantic Clustering, List A Immediate, List A Delayed, Long Delay, List B Immediate, New Recognition Index; Logical Memory Part 1 and 2 [
42].
DAFI Score: Measures used to calculate the DAFI score assessed: 1)
Functional Status: Instrumental Activities of Daily Living (IADL) Subscale of the Multidimensional Functional Assessment Questionnaire [
43]; Medical Outcomes Study (MOS) Physical Health, Social Limitations, and Social Support Scales [
44]; Karnofsky Self-Reported Performance Status Scale [
45]; and Self-report of the number of falls in the last 6 months; 2)
Comorbidity: Physical Health Section Older American Resources & Services Questionnaire (OARS) [
43] and a single sum of the 14 items; 3)
Depression: Center for Epidemiological Study – Depression [
46]; 4)
Anxiety: Spielberger State Anxiety Inventory [
47]; and 5)
Fatigue: Fatigue Symptom Inventory [
48]. Finally the timed Up and Go test was administered [
49].
The DAFI score was quantified as a score ranging between zero and one based on up to 44 possible frailty indicators, as described by Cohen et.al. [
50]. For each indicator (e.g., limited ability to climb one flight of stairs, a diagnosis of arthritis) the participant scored a zero, one, or two based on whether the indicator showed absent, intermediate, or most adverse risk, respectively. The deficit accumulation frailty index (DAFI) score was then calculated as the sum of these individual indicator scores divided by the maximum possible score. In cases where an indicator variable was missing, the item was excluded from both numerator and denominator. The score was calculated for all participants for whom at least 35 indicators were assessed (2 participants were excluded). Continuous DAFI scores were than used to classify participants as robust (DAFI < 0.2), pre-frail (0.2 ≤ DAFI < 0.35), or frail (DAFI ≥ 0.35). Since we were interested in the relationship between deficit accumulation and cognition, self-report of cognitive function was not included as a frailty indicator. Additionally, to utilize the same criteria for survivors and controls, breast cancer history was not included as an indicator (3% of the sample had a history of another type of cancer (e.g., skin cancer), which was included as a frailty indicator).
Statistical Approach: We fitted what is known in the literature as a ‘varying-intercepts, varying-slopes’ model [
51] in a Bayesian framework. Briefly, the model is divided into two levels. In level 1, longitudinal assessments for the
ith person are first summarized as an intercept
and a slope
. In level 2, these varying intercepts and varying slopes are further analyzed. The intercepts are expressed as a quadratic function of chronological age at enrollment, as a continuous variable, centered at age 72.5 (average age of the entire sample), and the control and survivor cohorts follow two separate quadratic aging trends. The varying slopes are modeled as a function of 4 age quartiles at baseline. . We used the categorical age cohorts at enrollment to fit the varying slopes, rather than the continuous chronological age, because of specific research questions (i.e., whether practice over time differed between survivors and controls in these baseline age cohorts), and because we did not want to double count time (varying slopes were already fitted with time). Additional technical details on the model, including model equations are found in the Appendix, and a worked example with syntax codes can be found on an online data repository (
https://github.com/bayesnp/RandomSlopesIntcpts).
There are two noteworthy features in this model. First, the cross-sectional aging trend is modeled continuously over chronological age, which improves on the categorical age bins frequently used by aging researchers, and practice effects are modeled simultaneously, which improves on the separate analyses in Salthouse [
52]. Second, the covariance
allows slopes and intercepts to be correlated. For example, a positive correlation indicates that individuals who have a higher cross-sectional cognitive performance at enrollment also tend to show a greater practice effect over time. This correlation is not available when the cross-sectional and longitudinal data are analyzed separately.
Bayesian computation was done using the rstanarm package (version 2.21.3:
https://mc-stan.org/docs/reference-manual/index.html) in R version 4.2.2. Convergence of the simulations was evaluated by the
≤ 1.01 diagnostic metric [
53], achieved in all models with 4 chains of 60,000 iterations each, 10,000 of which omitted as warm up iterations and a thinning interval of 5. Parameter estimates and their 95% Highest Density Intervals (HDI) were sought. Source code files for model fitting and for plotting key figures are available at the online repository.
3. Results
Table 1 summarizes demographic and treatment characteristics of the sample. The analytic sample included 328 cancer survivors and 158 cancer controls as described previously [
25]. The sample was largely white (85%), non-Hispanic (88%), and had undergraduate education or greater (59%). Ages ranged from 60 to 89 years, with an average of 72.5 years. Recruitment was targeted so that approximately 50% had a history of treatment with chemotherapy or no chemotherapy. The majority of patients were ER positive (80%), PR positive (65%), and HER2 negative (88%) and had been treated with endocrine therapy (75%). Twenty-five percent of survivors were actively receiving endocrine therapy when enrolled in the study.
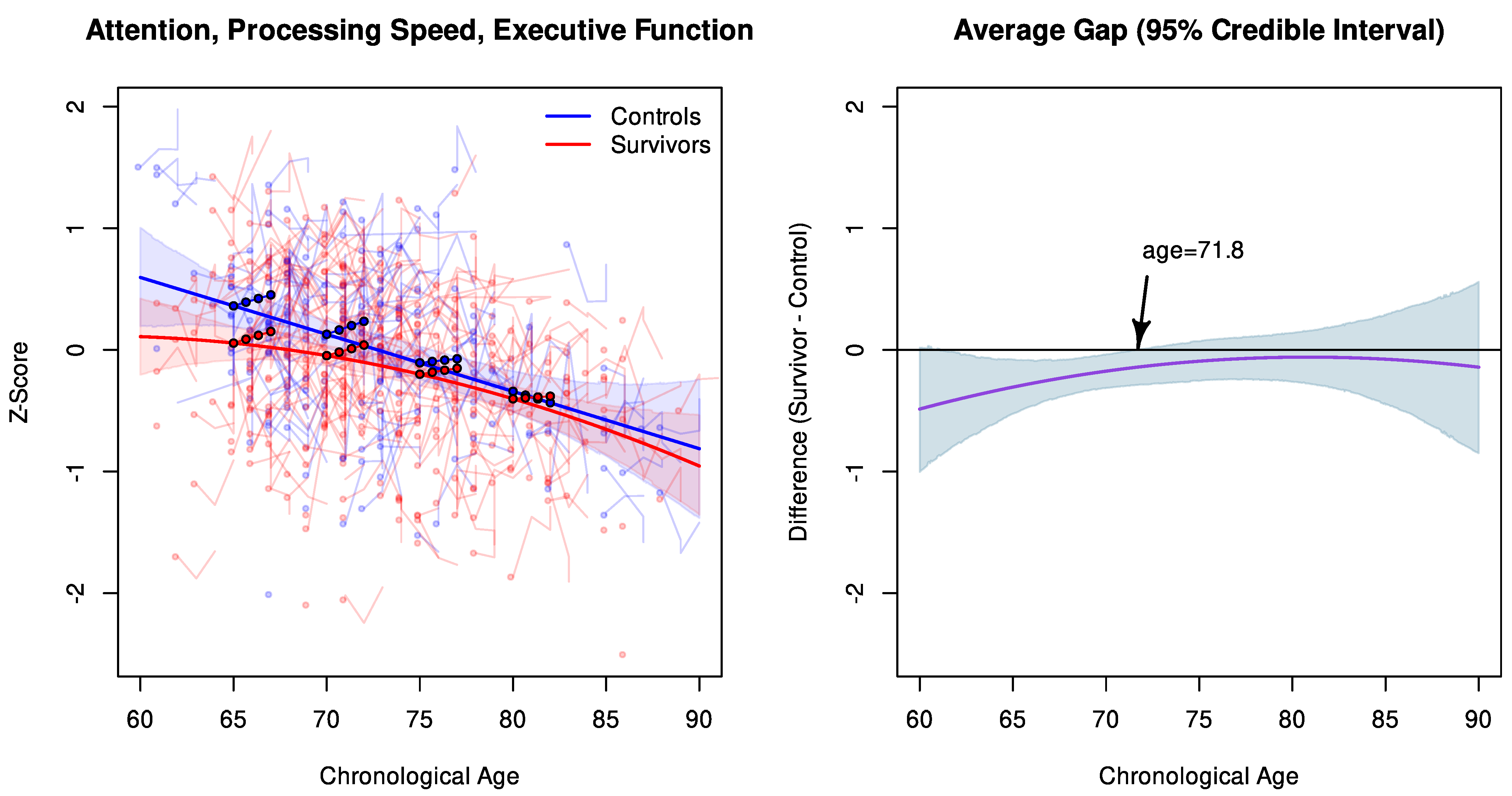
Table 2 summarizes the parameter estimates for the APE and LM models. For APE, there is a reliable linear term in chronological age at enrollment (
: -0.047, Bayesian 95% HDI: -0.065, -0.029), together with an average practice effect over months (
: 0.004, HDI: 0.0004, 0.007), and the oldest age quartile (77–89 year olds) showed a reliably lower longitudinal improvement as compared to the youngest age quartile (60–68 year olds). The age effect translates to a worsening APE in the control cohort by 0.47 z-scores per decade of aging, what Cohen would consider a ‘medium’ effect [
54] in psychological research. Survivors had slightly better aging linear term by 0.31 z-scores per decade of aging, although the difference between survivors and controls (
: 0.016, HDI: -0.006, 0.038) did not exclude the null. Survivors had a lower age intercept (
: -0.130, HDI: -0.279, 0.020), although the 95% HDI did not exclude the null. The random effect showed an estimated correlation of 0.16 between the random intercepts and slopes, indicating that a higher APE score at enrollment was associated with a greater longitudinal slope over 24 months.
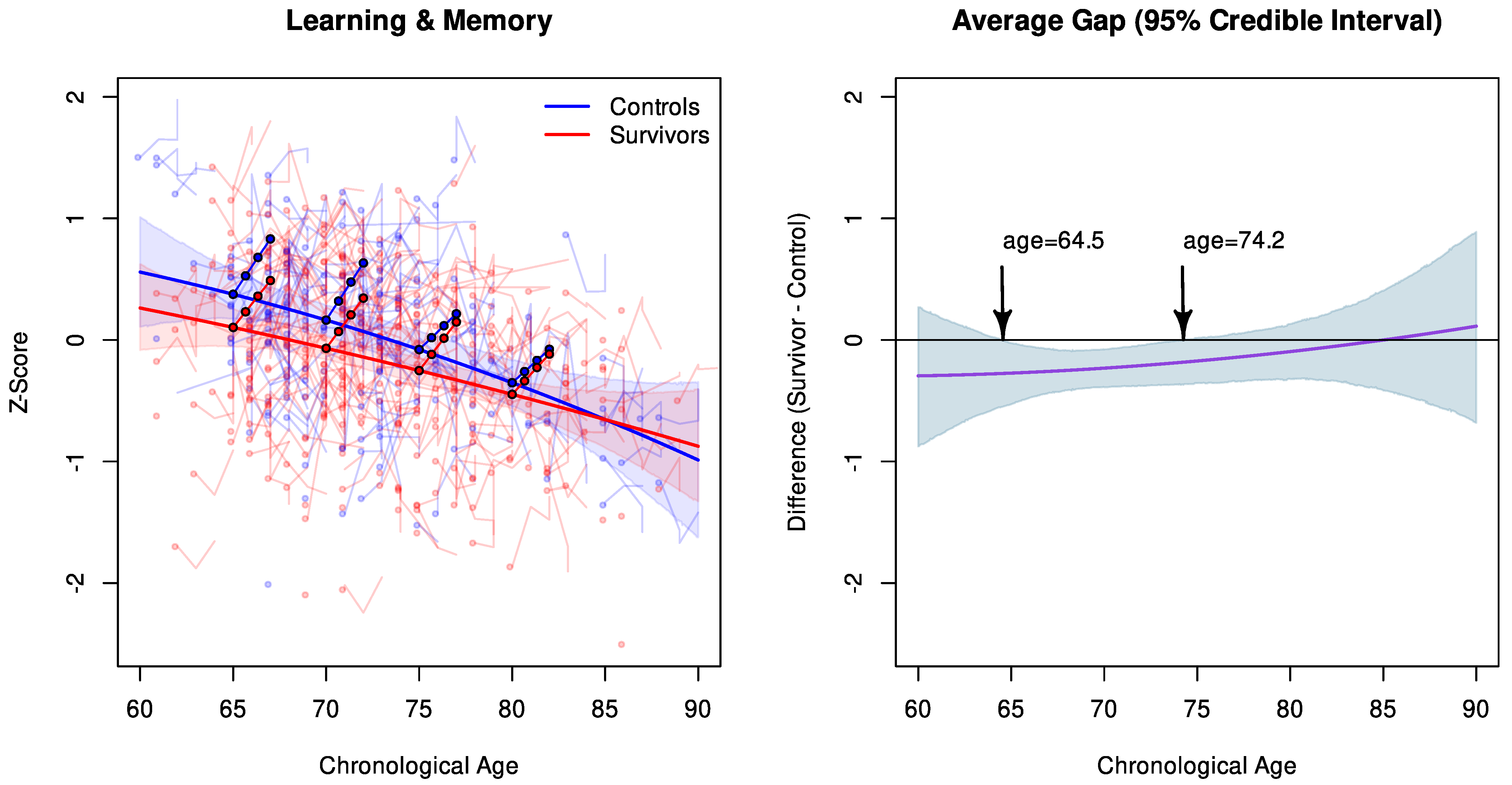
A similar pattern was observed in the Learning and Memory domain scores, where reliable fixed effects were found in the age linear term (-0.048, HDI: -0.069, -0.028) and longitudinal changes over months (0.019, HDI: 0.013, 0.025). The age effect translates to a worsening Learning & Memory score by 0.48 z-scores in the control cohort per decade of aging, comparable to the 0.47 in APE. Survivors had a lower age intercept that excluded the null (-0.205, HDI: -0.376, -0.034). There was a 0.27 correlation between the random intercepts and slopes, slightly greater than the 0.16 correlation in the APE domain.
Figure 1 provides a visual explanation for the APE model, where the model-estimated APE scores are plotted over chronological age. In the left panel, solid lines represent the model-estimated cross-sectional APE scores for survivors and controls. Superimposed on the solid lines are filled circles, which represent the model-estimated longitudinal changes over 24 months in the age quartiles. Added in opaque colors are the 95% credible intervals for the solid lines and the observed APE scores for each study participant over the course of up to 24 months. As demonstrated by the solid curves, survivor and control performance is discrepant in individuals younger than (approximately) 72 years of age, beyond which the credible intervals begin to converge. To further examine this gap, we plot on the right panel the average difference between survivors and controls (in solid line) at baseline and its 95% credible intervals (shaded areas). At age 65, survivors are estimated to have reliably lower APE performance than controls by 0.31 z-scores (95% HDI: -0.52, -0.08). The arrow shows that the shaded credible intervals begin to cross the null at age 71.8, where group contrasts are no longer significant.
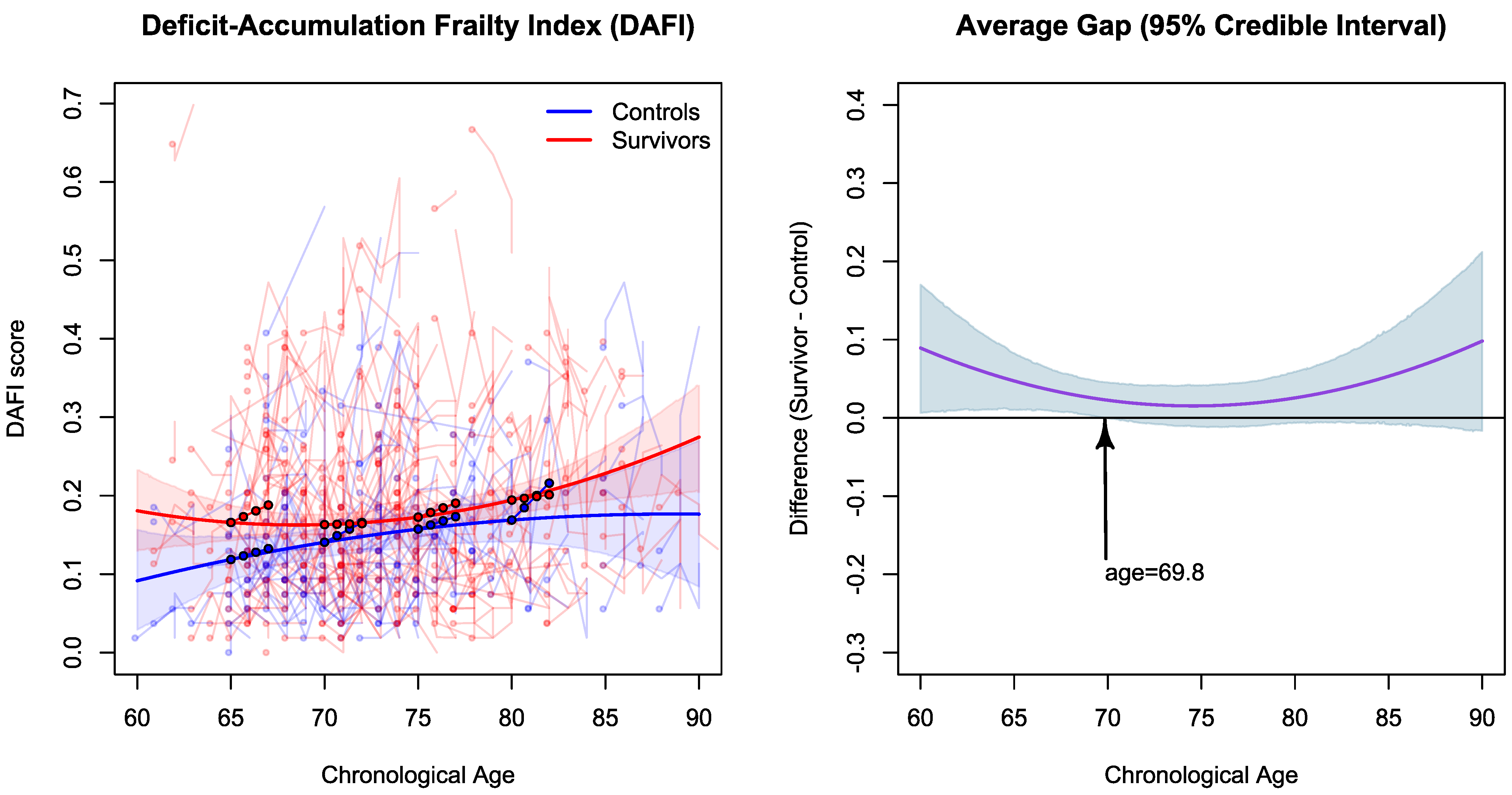
Figure 2 shows a similar overall pattern in Learning & Memory, where cross-sectional cognitive performance declines with chronological age. The longitudinal slopes in the filled circles have a visibly pronounced upward increase for all age cohorts, and they appear steeper than those in APE, and even the oldest age quartile retain a steep slope. The right panel shows that, between 64.5 and 74.2 years of age, a discernible gap at 95% posterior confidence is found between survivors and controls, indicating significantly lower survivor performance than controls over this age range; similar to the APE analysis, performance between groups begins to overlap as individuals age, indicating no significant difference between survivors and controls. The credible interval is somewhat wide for age 64.5 and younger, in part because of relatively sparse data from 16 controls and 27 survivors.
Figure 3 shows the same model applied to scores on Deficit-Accumulation and Frailty Index (DAFI). The plot on the left shows that cancer survivors have a greater deficit accumulation than non-cancer controls across the chronological age span. Similar to the pattern seen in
Figure 1 and
Figure 2, the gap in deficit accumulation at enrollment appears to be primarily in younger age, and the plot on the right shows that its credible interval crosses the null at age 69.8. Deficit accumulation also appears to be greater in older cancer survivors. However, the average gap plot indicates that the difference is not statistically discernible at 95%, in part due to the relatively small number of older participants. Filled circles show that survivors in the youngest age quartile continue to accumulate deficits over the 24 months duration of the study, while deficit accumulation appears to subside in the older survivor quartile groups. Interestingly, controls in the oldest age quartile continue to accumulate deficits.
4. Discussion
In this analysis, we examined baseline, cross-sectional performance differences between survivors and controls over a 30-year age span as a proxy indicator of how cancer and cancer treatment might affect cognitive aging trajectories. We have taken this approach to sample potential cognitive aging trends over meaningful aging intervals absent the effects of practice and selective attrition in repeated testing, as well as to demonstrate the distorting effects of repeated longitudinal testing on cognitive trajectories.
As expected, longitudinal trajectories suggest improving cognitive performance at each successive timepoint, driven by practice effects due to repeated test exposure, in contrast to cross-sectional, baseline trends that indicate an inverse association of age and cognition. Longitudinal analysis results in two counterintuitive findings regarding age and deficit accumulation and their effect on cognition: increasing age and increasing deficit accumulation, accurately reflecting increasing deficits over time, become artifactually associated with improving cognition. Both associations are at odds with what is known of the influence of age and deficit accumulation on cognition. Aging literature indicates that advancing age is one of the most robustly negative effects on cognition [
52]. Likewise, deficit accumulation and frailty also demonstrate an inverse association with cognition in older adults [
16,
17,
18]. Repeated testing obscures both expected cognitive aging trajectories and associated mediators of cognitive aging, in this case deficit accumulation. The argument could be made that any practice effects would be shared equally between groups and that in contrasts of survivors and controls these effects are subtracted away, leaving the expected effects of cancer and cancer treatment. We note that that practice effects are not equal between domains or age bands and in previous work we have found that survivors benefit more from repeated exposure both within and across assessment time-points [
29]. In this analysis, for LM, a strong practice effect is notable across all age bands, in contrast to a weaker and declining practice effect for APE with increasing age. Our analysis also found a significant association of baseline performance with magnitude of practice effect. This heterogeneity between domains, ages and baseline performance effects suggests that attempts to model or account for practice effects in any analysis will be methodologically difficult, as this would require baseline, age and domain specific modeling of practice.
Similar problems were encountered by researchers studying normal aging and cognition – repeated testing that aimed to establish cognitive trajectories associated with age led to the appearance of improvement in cognition with age. When a quasi-longitudinal (same cohort/different age) design was used, trajectories associated with aging followed the expected cross-sectional trends of declining cognition with age that cannot be explained by a generational cohort effect [
27]. The contrast of longitudinal and cross-sectional data from that work is strikingly similar to longitudinal and cross-sectional trends that we see here – longitudinal improvements versus cross-sectional declines. Examining the first timepoint cross-sectionally across age allows us to see cognitive differences with age in both groups, as well as differences in these trends specific to survivors and controls. In both LM and APE plots, survivors experience an early decline in cognition at a younger age range and exhibit a declining but flatter slope than controls with increasing age. Survivors and control slopes finally meet and continue to overlap from approximately age 70 through to the highest age range. This pattern, while a proxy for true longitudinal trends associated with aging and survivorship, was unexpected given previously theorized trajectories associated with cancer and cancer treatment. Both a phase shift trajectory, in which deficits persist but parallel cognitive decline in women without a cancer history, and an accelerated aging trajectory, in which there is a steeper slope of cognitive decline with age, have been hypothesized [
55]. The phase shift trajectory would be expected if the primary effect on cognition is assumed to be cancer development and treatment, with little recovery in the near- and long-term, creating a new baseline that now parallels similarly aged individuals with no cancer history, both declining equally with age. In contrast, an accelerated aging trajectory might be expected if either a) the initial effect of cancer treatment leads to a cascade of biologic events, i.e., deficit accumulation, that cause continued cognitive decline with aging, or b) if a given treatment may not be sufficient to immediately affect cognitive function but may produce a delayed effect as aging continues. Instead, our analysis found evidence of early decline in younger survivors with controls approaching similar declines in cognition at older ages. While we have demonstrated cognitive differences between survivors and controls in this sample as a whole in previous work [
35], the data examined here suggests that it is the younger survivors who contribute most to these observed cognitive differences.
Gaps in deficit accumulation also appear to be greatest for survivors younger than 70. This suggests that perhaps gaps in cognition are associated with gaps in deficit accumulation, and cancer and cancer treatment contribute to the additional deficits in younger cancer survivors as compared to controls. We have previously established a mediating role of deficit accumulation in cognitive dysfunction in survivors in the sample as a whole [
25]. To the extent that this pattern is driven by deficit accumulation, this may suggest that younger survivors experience an early increase in deficits associated with cancer and treatment, i.e., comorbidity burden, polypharmacy, social detriments of disease (e.g., smoking, obesity), psychological disturbance, and functional limitations / declines in activities of daily living, compared to individuals without a history of cancer, that in turn lead to an early decline in cognition. At younger ages, survivors may be most unique from controls for the fact of cancer diagnosis, treatment and associated deficits. As controls age, comorbidities and functional limitations accrue related to normal aging and other etiologies outside of cancer and treatment. With time, and with the normal process of aging and deficit accumulation absent a history of cancer, older controls accrue deficits at similar levels to those of younger and older survivors, with cognitive performance now converging as a result. This may partly explain why neither a phase shift nor accelerated aging trend was found. Survivors accrue deficits earlier, but the slope of accumulation is relatively more flat, in contrast to controls who steadily accrue increasing deficits with age, converging with survivors.
As with any research, this report is subject to limitations. This is a secondary analysis that was not originally intended in the original proposed study. That proposal intended to examine altered cognitive trajectories using the longitudinal timepoints over a two-year period. Given the difficulties imposed by repeated testing and the relatively short timeframe proposed, this secondary analysis sought to estimate aging trends from only baseline cognitive performance over a longer interval. While we note that generational cohort effects are of less concern given evidence that these effects have diminished, we cannot rule out an effect of cohort on our analysis as a whole. With the addition of control data from equivalent ages/cohorts, we can, however, control for any cohort effects that would influence differences in cognition between survivors and controls. Additionally, work from Salthouse et al found little effect of cohort effects on cognition, with quasi-longitudinal and cross-sectional trends returning similar trajectories over age.
5. Conclusions
This analysis highlights the distorting effects of longitudinal cognitive testing on expected cognitive trajectories as a result of repeated exposure to cognitive measures. We have introduced an analysis informed by normal cognitive aging research using cross-sectional data as a proxy indicator of cognitive aging more generally, and in this case of differences in cognitive aging associated with a history of cancer and cancer treatment. The additional analysis of deficit accumulation reveals similar trends in deficit accumulation and cognition, and suggests a potential link between the two specifically in younger survivors. To the extent that deficit accumulation is implicated in cognitive decline in survivorship, this would suggest one potentially modifiable risk factor to be identified for monitoring, prevention and intervention.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Detailed statistical approach.
Author Contributions
Conceptualization, T.A.A. and J.C.R.; Methodology, T.A.A. and J.C.R.; Formal Analysis, Y.L. and E.S.; Investigation, T.A.A.; Resources, T.A.A.; Data Curation, Y.L. and E.S.; Writing – Original Manuscript Preparation, J.C.R. and T.A.A.; Writing – Review and Editing, J.C.R., T.A.A., Y.L., E.S., S.P., I.O., T.T.; Visualization, Y.L.; Supervision, T.A.A.; Project Administration, T.A.A.; Funding Acquisition, T.A.A..
Funding
This research was supported by grants from the National Cancer Institute (TA: R01 CA172119, U54 CA137788, P30 CA008748), the American Cancer Society (SKP: RSG-17-023-01-CPPB), and Internal MSK grants (IO: Society of MSK, Brain Tumor Center Award).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Memorial Sloan Kettering Cancer Center (10-079; 7/21/2010).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be made available in response to all reasonable requests.
Conflicts of Interest
The authors declare no conflict of interest.
References
- van Dam, F.S.; Schagen, S.B.; Muller, M.J.; Boogerd, W.; vd Wall, E.; Droogleever Fortuyn, M.E.; Rodenhuis, S. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst 1998, 90, 210-218. [CrossRef]
- Schagen, S.B.; van Dam, F.S.; Muller, M.J.; Boogerd, W.; Lindeboom, J.; Bruning, P.F. Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer 1999, 85, 640-650. [CrossRef]
- Ahles, T.A.; Saykin, A.J.; Furstenberg, C.T.; Cole, B.; Mott, L.A.; Skalla, K.; Whedon, M.B.; Bivens, S.; Mitchell, T.; Greenberg, E.R.; et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol 2002, 20, 485-493.
- Yamada, T.H.; Denburg, N.L.; Beglinger, L.J.; Schultz, S.K. Neuropsychological outcomes of older breast cancer survivors: cognitive features ten or more years after chemotherapy. J Neuropsychiatry Clin Neurosci 2010, 22, 48-54. [CrossRef]
- Wouters, H.; Baars, J.W.; Schagen, S.B. Neurocognitive function of lymphoma patients after treatment with chemotherapy. Acta Oncol 2016, 55, 1121-1125. [CrossRef]
- Fan, H.G.; Houede-Tchen, N.; Yi, Q.L.; Chemerynsky, I.; Downie, F.P.; Sabate, K.; Tannock, I.F. Fatigue, menopausal symptoms, and cognitive function in women after adjuvant chemotherapy for breast cancer: 1- and 2-year follow-up of a prospective controlled study. J Clin Oncol 2005, 23, 8025-8032. [CrossRef]
- Shilling, V.; Jenkins, V.; Morris, R.; Deutsch, G.; Bloomfield, D. The effects of adjuvant chemotherapy on cognition in women with breast cancer--preliminary results of an observational longitudinal study. Breast 2005, 14, 142-150, doi:S0960-9776(04)00215-2 [pii]. [CrossRef]
- Schagen, S.B.; Muller, M.J.; Boogerd, W.; Mellenbergh, G.J.; van Dam, F.S. Change in cognitive function after chemotherapy: a prospective longitudinal study in breast cancer patients. J Natl Cancer Inst 2006, 98, 1742-1745, doi:98/23/1742 [pii]. [CrossRef]
- Hermelink, K.; Untch, M.; Lux, M.P.; Kreienberg, R.; Beck, T.; Bauerfeind, I.; Munzel, K. Cognitive function during neoadjuvant chemotherapy for breast cancer: results of a prospective, multicenter, longitudinal study. Cancer 2007, 109, 1905-1913. [CrossRef]
- Ahles, T.A.; Li, Y.; McDonald, B.C.; Schwartz, G.N.; Kaufman, P.A.; Tsongalis, G.J.; Moore, J.H.; Saykin, A.J. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: the impact of APOE and smoking. Psychooncology 2014, 23, 1382-1390. [CrossRef]
- Janelsins, M.C.; Heckler, C.E.; Peppone, L.J.; Mohile, S.G.; Mustian, K.M.; Ahles, T.; Palesh, O.; O'Mara, A.M.; Minasian, L.M.; Williams, A.; et al. Longitudinal assessment of cancer-related cognitive impairment (CRCI) up to six-months post-chemotherapy with multiple cognitive testing methods in 943 breast cancer (BC) patients and controls. Journal of Clinical Oncology 2017, 35, 10014-10014. [CrossRef]
- Mandelblatt, J.S.; Small, B.J.; Luta, G.; Hurria, A.; Jim, H.; McDonald, B.C.; Graham, D.; Zhou, X.; Clapp, J.; Zhai, W.; et al. Cancer-Related Cognitive Outcomes Among Older Breast Cancer Survivors in the Thinking and Living With Cancer Study. J Clin Oncol 2018, JCO1800140. [CrossRef]
- Kreukels, B.P.; van Dam, F.S.; Ridderinkhof, K.R.; Boogerd, W.; Schagen, S.B. Persistent neurocognitive problems after adjuvant chemotherapy for breast cancer. Clin Breast Cancer 2008, 8, 80-87. [CrossRef]
- Koppelmans, V.; Breteler, M.M.; Boogerd, W.; Seynaeve, C.; Gundy, C.; Schagen, S.B. Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J Clin Oncol 2012, 30, 1080-1086. [CrossRef]
- Searle, S.D.; Rockwood, K. Frailty and the risk of cognitive impairment. Alzheimer's research & therapy 2015, 7, 54. [CrossRef]
- Avila-Funes, J.A.; Amieva, H.; Barberger-Gateau, P.; Le Goff, M.; Raoux, N.; Ritchie, K.; Carriere, I.; Tavernier, B.; Tzourio, C.; Gutierrez-Robledo, L.M.; et al. Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: the three-city study. J Am Geriatr Soc 2009, 57, 453-461. [CrossRef]
- Buchman, A.S.; Schneider, J.A.; Leurgans, S.; Bennett, D.A. Physical frailty in older persons is associated with Alzheimer disease pathology. Neurology 2008, 71, 499-504. [CrossRef]
- Buchman, A.S.; Yu, L.; Wilson, R.S.; Boyle, P.A.; Schneider, J.A.; Bennett, D.A. Brain pathology contributes to simultaneous change in physical frailty and cognition in old age. J Gerontol A Biol Sci Med Sci 2014, 69, 1536-1544. [CrossRef]
- Hurria, A.; Jones, L.; Muss, H.B. Cancer Treatment as an Accelerated Aging Process: Assessment, Biomarkers, and Interventions. Am Soc Clin Oncol Educ Book 2016, 35, e516-522. [CrossRef]
- Keating, N.L.; Norredam, M.; Landrum, M.B.; Huskamp, H.A.; Meara, E. Physical and mental health status of older long-term cancer survivors. J Am Geriatr Soc 2005, 53, 2145-2152. [CrossRef]
- Pinder, M.C.; Duan, Z.; Goodwin, J.S.; Hortobagyi, G.N.; Giordano, S.H. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol 2007, 25, 3808-3815. [CrossRef]
- Eastell, R.; Adams, J.E.; Coleman, R.E.; Howell, A.; Hannon, R.A.; Cuzick, J.; Mackey, J.R.; Beckmann, M.W.; Clack, G. Effect of anastrozole on bone mineral density: 5-year results from the anastrozole, tamoxifen, alone or in combination trial 18233230. J Clin Oncol 2008, 26, 1051-1057. [CrossRef]
- Mandelblatt, J.S.; Stern, R.A.; Luta, G.; McGuckin, M.; Clapp, J.D.; Hurria, A.; Jacobsen, P.B.; Faul, L.A.; Isaacs, C.; Denduluri, N.; et al. Cognitive impairment in older patients with breast cancer before systemic therapy: is there an interaction between cancer and comorbidity? J Clin Oncol 2014, 32, 1909-1918. [CrossRef]
- Ahles, T.A.; Schofield, E.; Li, Y.; Ryan, E.; Root, J.C.; Patel, S.K.; McNeal, K.; Gaynor, A.; Tan, H.; Katheria, V.; et al. Relationship between cognitive functioning and frailty in older breast cancer survivors. J Geriatr Oncol 2021. [CrossRef]
- Ahles, T.A.; Schofield, E.; Li, Y.; Ryan, E.; Orlow, I.; Patel, S.K.; Traina, T.; Root, J.C. Cognitive function is mediated by deficit accumulation in older, long-term breast cancer survivors. J Cancer Surviv 2023. [CrossRef]
- Calamia, M.; Markon, K.; Tranel, D. Scoring higher the second time around: meta-analyses of practice effects in neuropsychological assessment. Clin Neuropsychol 2012, 26, 543-570. [CrossRef]
- Salthouse, T.A. Trajectories of normal cognitive aging. Psychol Aging 2019, 34, 17-24. [CrossRef]
- Salthouse, T.A. Influence of age on practice effects in longitudinal neurocognitive change. Neuropsychology 2010, 24, 563-572. [CrossRef]
- Gaynor, A.M.; Ahles, T.A.; Ryan, E.; Schofield, E.; Li, Y.; Patel, S.K.; McNeal, K.; Traina, T.; Root, J.C. Initial encoding deficits with intact memory retention in older long-term breast cancer survivors. J Cancer Surviv 2022, 16, 940-947. [CrossRef]
- Shenk, D. What is the Flynn Effect, and how does it change our understanding of IQ? Wiley Interdiscip Rev Cogn Sci 2017, 8. [CrossRef]
- Bratsberg, B.; Rogeberg, O. Flynn effect and its reversal are both environmentally caused. Proc Natl Acad Sci U S A 2018, 115, 6674-6678. [CrossRef]
- Dutton, E.; van der Linden, D.; Lynn, R. The negative Flynn effect: A systematic literature review. Intelligence 2016, 59, 163-169. [CrossRef]
- Platt, J.M.; Keyes, K.M.; McLaughlin, K.A.; Kaufman, A.S. The Flynn effect for fluid IQ may not generalize to all ages or ability levels: a population-based study of 10,000 US adolescents. Intelligence 2019, 77. [CrossRef]
- Kaufman, A. Clinical applications II: Age and intelligence across the adult life span. . In Essentials of WAIS IV Assessment, Lichtenberg, Kaufman, Eds.; 2013.
- Ahles, T.A.; Orlow, I.; Schofield, E.; Li, Y.; Ryan, E.; Root, J.C.; Patel, S.K.; McNeal, K.; Gaynor, A.; Tan, H.; et al. The impact of APOE and smoking history on cognitive function in older, long-term breast cancer survivors. J Cancer Surviv 2022. [CrossRef]
- Mandelblatt, J.S.; Zhou, X.; Small, B.J.; Ahn, J.; Zhai, W.; Ahles, T.; Extermann, M.; Graham, D.; Jacobsen, P.B.; Jim, H.; et al. Deficit Accumulation Frailty Trajectories of Older Breast Cancer Survivors and Non-Cancer Controls: The Thinking and Living with Cancer Study. J Natl Cancer Inst 2021. [CrossRef]
- Box, G.E.P.; Cox, D.R. An Analysis of Transformations. Journal of the Royal Statistical Society. Series B (Methodological) 1964, 26, 211-252.
- Wechsler, D. Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) Pearson: San Antonio, TX, 2008.
- Reitan, R.M. Trail Making Test: manual for adminstration and scoring. Reitan Neuropsychological Laboratory: Tuscon, AZ, 1971.
- Delis, D.C.; Kaplan, E.; Kramer, J.H. Delis-Kaplan Executive Function System; Pearson: San Antonio, TX, 2001.
- Stern, R.A.; White, T. Neuropsychological Assessment Battery; WPS: 2003.
- Weintraub, S.; Salmon, D.; Mercaldo, N.; Ferris, S.; Graff-Radford, N.R.; Chui, H.; Cummings, J.; DeCarli, C.; Foster, N.L.; Galasko, D.; et al. The Alzheimer's Disease Centers' Uniform Data Set (UDS): the neuropsychologic test battery. Alzheimer disease and associated disorders 2009, 23, 91-101. [CrossRef]
- Fillenbaum, G.G.; Smyer, M.A. The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J Gerontol 1981, 36, 428-434. [CrossRef]
- Stewart, A.L.; Ware, J.E. Measuring functioning and well-being: The Medical Outcomes Study approach; Duke University Press: Durham NC, 1992.
- Karnofsky D.A., B., J.H. The clinical evaluation of chemotherapeutic agents in cancer. In Evaluation of chemotherapeutic agents, MacLeod, C.M., Ed.; Columbia University Press: New York, 1949; pp. 191-205.
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied psychological measurement 1977, 1.
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.G. Manual for the State-Trait Anxiety Inventory for Adults. 1983.
- Hann, D.; Jacobsen, P.; Azzarello, L.; Martin, S.; Curran, S.; Fields, K.; Greenberg, H.; Lyman, G. Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Quality of Life Research 1998, 7, 301-310. [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991, 39, 142-148. [CrossRef]
- Cohen, H.J.; Smith, D.; Sun, C.L.; Tew, W.; Mohile, S.G.; Owusu, C.; Klepin, H.D.; Gross, C.P.; Lichtman, S.M.; Gajra, A.; et al. Frailty as determined by a comprehensive geriatric assessment-derived deficit-accumulation index in older patients with cancer who receive chemotherapy. Cancer 2016, 122, 3865-3872. [CrossRef]
- Gelman, A.; Hill, J. Data analysis using regression and multilevel/hierarchical models; Cambridge University Press: New York, 2007.
- Salthouse, T.A. Do cognitive interventions alter the rate of age-related cognitive change? Intelligence 2015, 53, 86-91. [CrossRef]
- Gelman, A.; Rubin, D.B. Inference from iterative simulation using multiple sequences. Statistical Science 1992, 7, 457 -- 472.
- Cohen, J. A power primer. Psychol Bull 1992, 112, 155-159.
- Ahles, T.A.; Root, J.C.; Ryan, E.L. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol 2012, 30, 3675-3686. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).