Submitted:
09 May 2023
Posted:
10 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
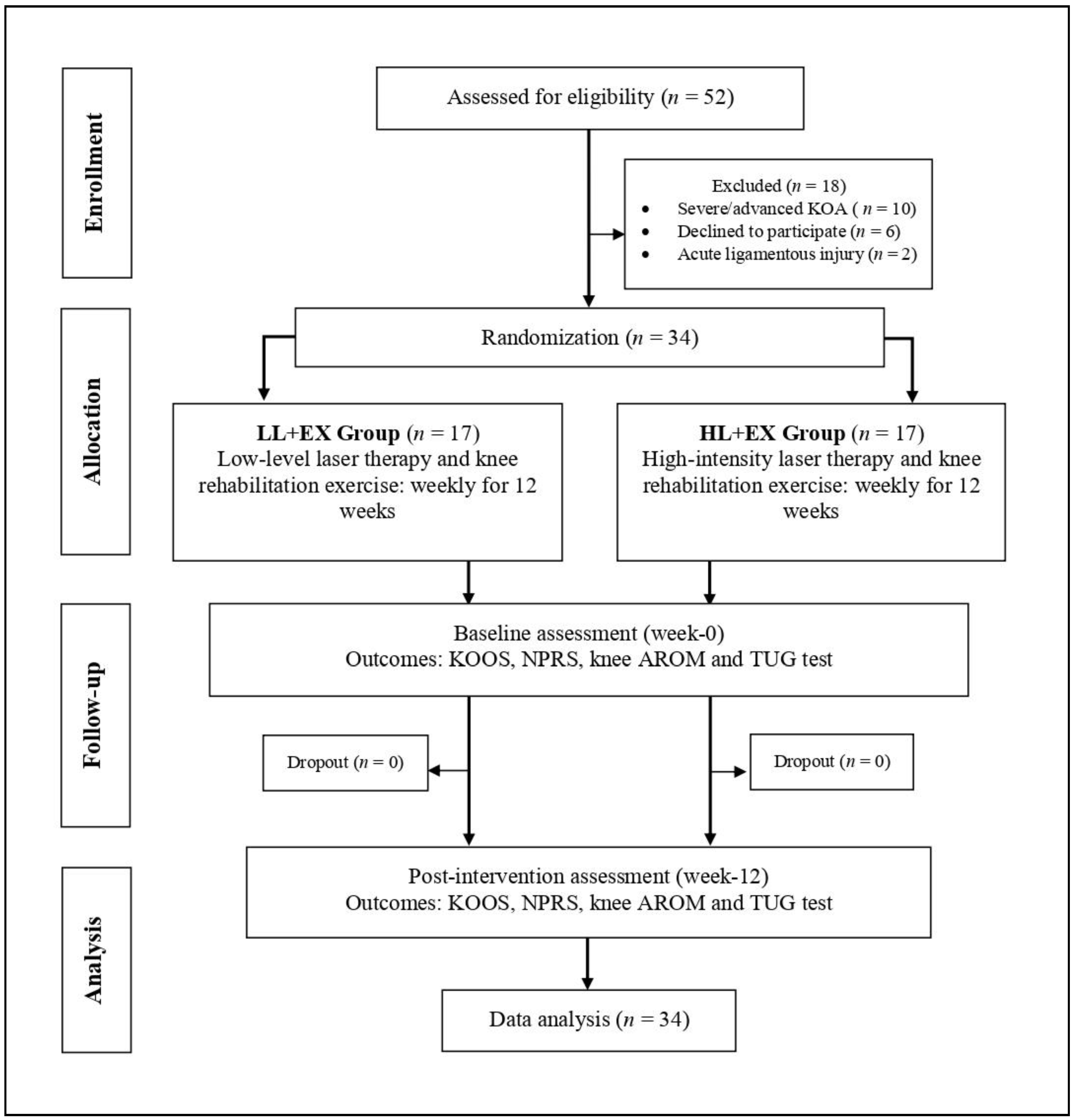
2.1. Study Design
2.2. Ethical Approval and Registration
2.3. Study Population and Setting
2.3.1. Inclusion
2.3.2. Exclusion
2.4. Sample Size Calculation
2.5. Procedures
2.5.1. Group LL+EX (n = 17)
2.5.2. Group HL+EX (n = 17)
2.6. Standardization and Blinding
2.7. Outcome Measures
2.8. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Baseline Comparability Analysis
3.3. Evaluation of Outcomes
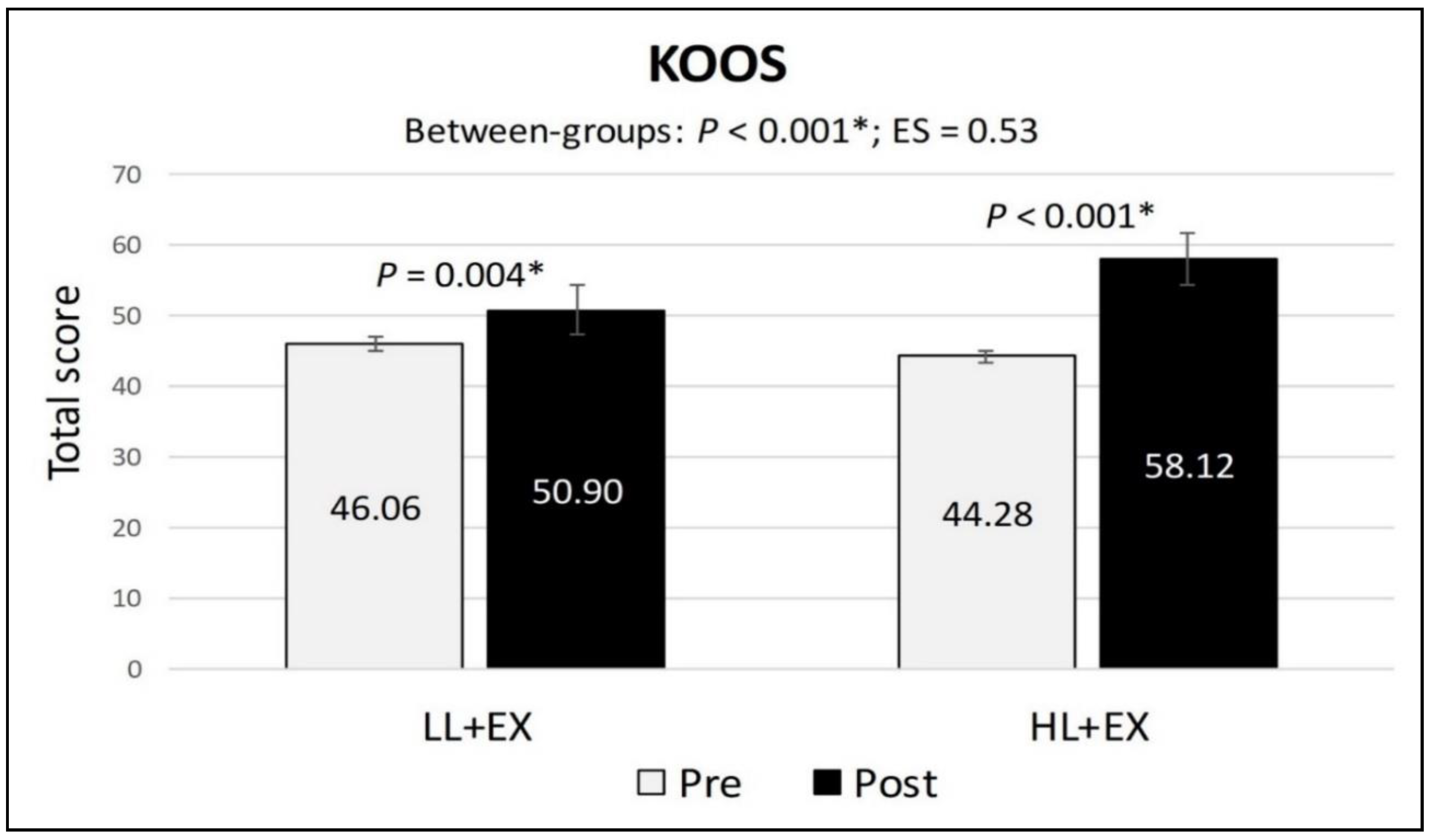
3.4. Changes in KOOS Scores
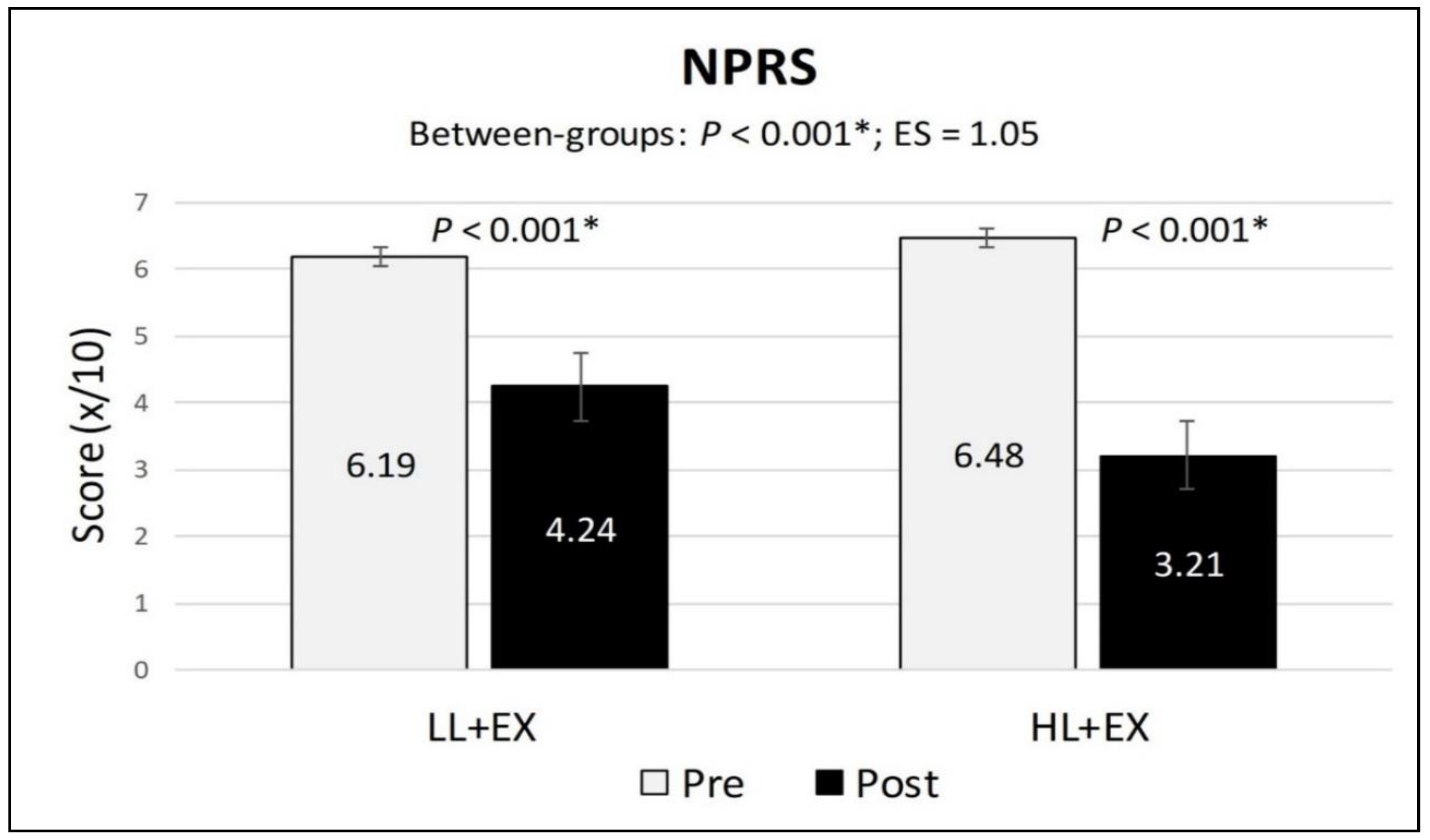
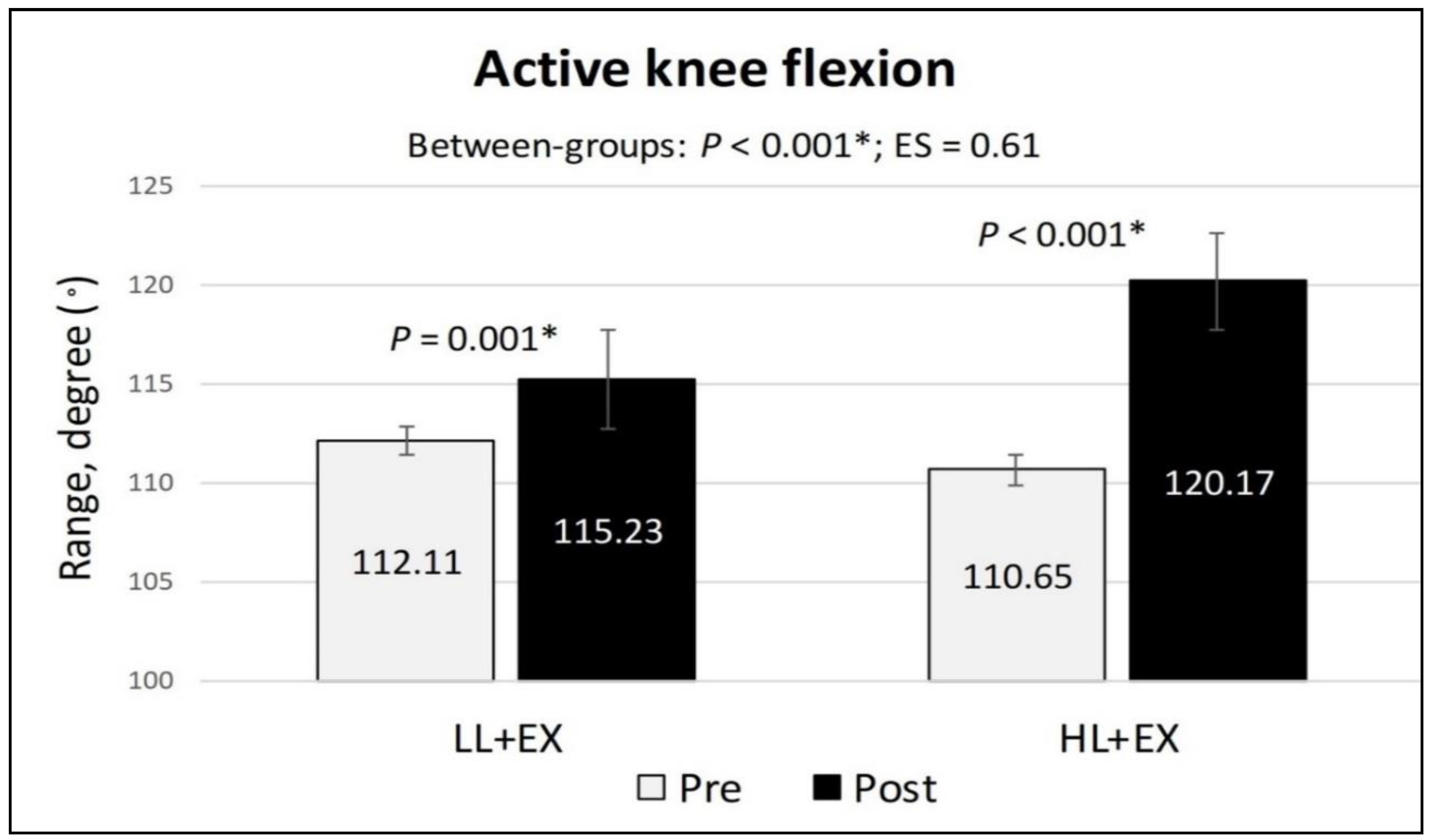
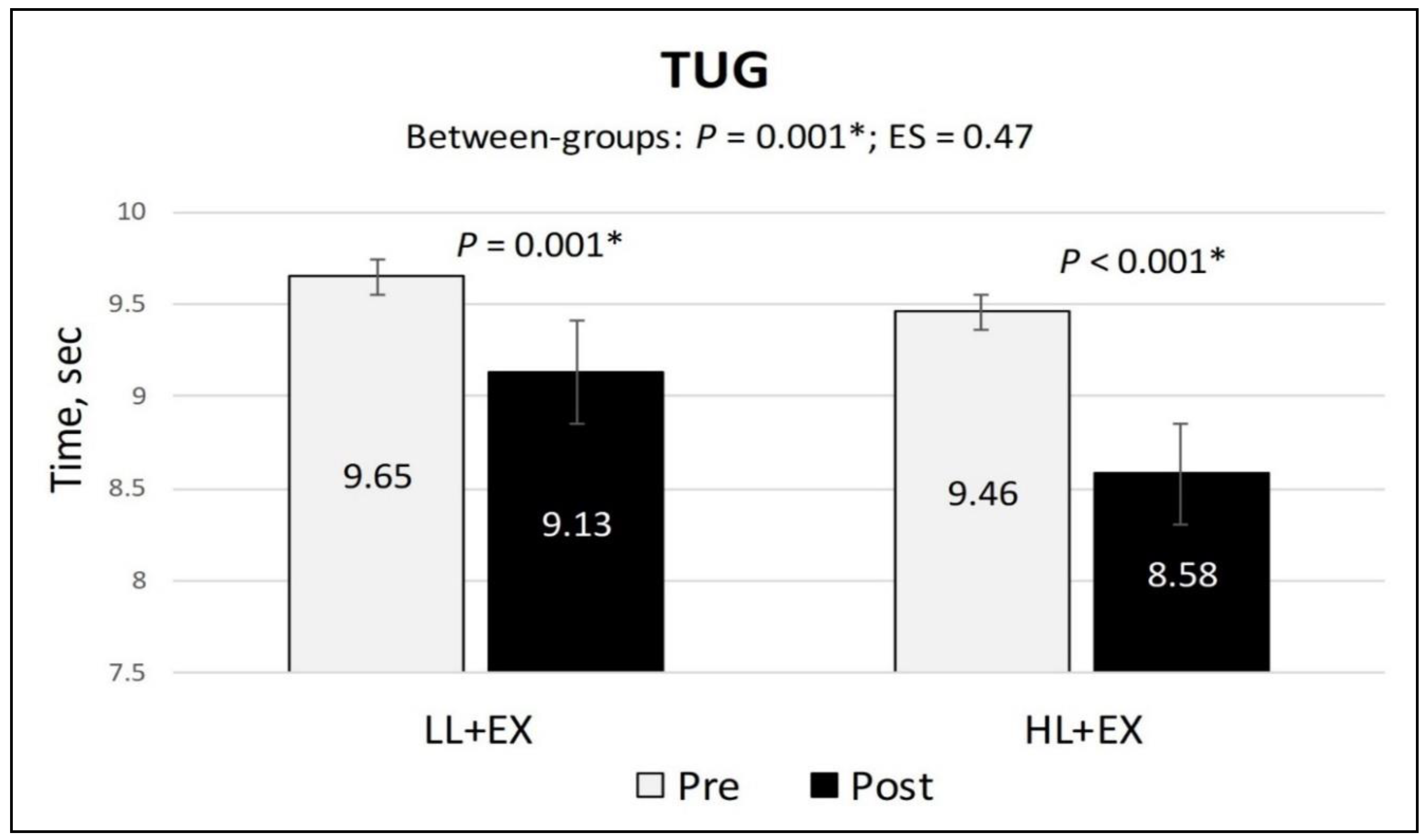
3.5. Changes in NPRS, Active Knee Flexion and TUG Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peat, G.; Thomas, M.J. Osteoarthritis year in review 2020: epidemiology & therapy. Osteoarthr. Cartil. 2020, 29, 180–189. [Google Scholar] [CrossRef]
- Singh, D.K.A. , Kamsan, S. S., Ahmad, M.A., Chien-Ying, A.N., Chua, W.Q., Padzil, F.M., Hendri, E.N.M. Knee associated problems and functional mobility among adults with knee osteoarthritis. Malay. J. Health. Sci. 2018, 16, 229–230. [Google Scholar]
- Kim, H.; Seo, J.; Lee, Y.; Park, K.; Perry, T.A.; Arden, N.K.; Mobasheri, A.; Choi, H. The current state of the osteoarthritis drug development pipeline: a comprehensive narrative review of the present challenges and future opportunities. Ther. Adv. Musculoskelet. Dis. 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Luan, L.; Pranata, A.; Witchalls, J.; Adams, R.; Bousie, J.; Han, J. Is high intensity laser therapy more effective than other physical therapy modalities for treating knee osteoarthritis? A systematic review and network meta-analysis. Front. Med. 2022, 9, 956188. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Chen, J.; Ma, J.; Shen, B.; Pei, F.; Kraus, V. Effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthr. Cartil. 2015, 23, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Stausholm, M.B.; Naterstad, I.F.; Joensen, J.; Lopes-Martins, R. .B.; Sæbø, H.; Lund, H.; Fersum, K.V.; Bjordal, J.M. Efficacy of low-level laser therapy on pain and disability in knee osteoarthritis: systematic review and meta-analysis of randomised placebo-controlled trials. BMJ Open 2019, 9, e031142. [Google Scholar] [CrossRef] [PubMed]
- Wyszyńska, J.; Bal-Bocheńska, M. Efficacy of High-Intensity Laser Therapy in Treating Knee Osteoarthritis: A First Systematic Review. Photomed. Laser Surg. 2018, 36, 343–353. [Google Scholar] [CrossRef]
- Penberthy, W.T.; Vorwaller, C.E. Utilization of the 1064 nm Wavelength in Photobiomodulation: A Systematic Review and Meta-Analysis. J. Lasers Med Sci. 2021, 12, e86–e86. [Google Scholar] [CrossRef]
- Kim, E.-D.; Won, Y.H.; Park, S.-H.; Seo, J.-H.; Kim, D.-S.; Ko, M.-H.; Kim, G.-W. Efficacy and Safety of a Stimulator Using Low-Intensity Pulsed Ultrasound Combined with Transcutaneous Electrical Nerve Stimulation in Patients with Painful Knee Osteoarthritis. Pain Res. Manag. 2019, 2019, 1–10. [Google Scholar] [CrossRef]
- Samaan, S.S.R.R.; Sedhom, M.G.; Grace, M.O. A randomized comparative study between high-intensity laser vs low-intensity pulsed ultrasound both combined with exercises for the treatment of knee osteoarthritis. Int. J. Rheum. Dis. 2022, 25, 877–886. [Google Scholar] [CrossRef]
- White, P.F. , Alvir-Lazo, O. L., Yumul, R. Cold laser therapy for acute and chronic pain management: A comparison of low-level and high-intensity laser therapy devices. Anaesth. News. 2019, 13, 65–78. [Google Scholar]
- Kushibiki, T.; Ishihara, M. Biological Function of Low Reactive Level Laser Therapy (LLLT). In Photomedicine: Advances in Clinical Practice; Tanaka, Y., Ed.; IntechOpen: London, UK, 2017. [Google Scholar] [CrossRef]
- Kulchitskaya, D.B.; Konchugova, T.V.; E Fedorova, N. Comparative evaluation of the effects of high-intensity and low-intensity laser radiation on microcirculation among patients with knee arthritis. 2017, 826, 012015. [CrossRef]
- Jankaew, A.; You, Y.-L.; Yang, T.-H.; Chang, Y.-W.; Lin, C.-F. The effects of low-level laser therapy on muscle strength and functional outcomes in individuals with knee osteoarthritis: a double-blinded randomized controlled trial. Sci. Rep. 2023, 13, 1–9. [Google Scholar] [CrossRef]
- Siriratna, P.; Ratanasutiranont, C.; Manissorn, T.; Santiniyom, N.; Chira-Adisai, W. Short-Term Efficacy of High-Intensity Laser Therapy in Alleviating Pain in Patients with Knee Osteoarthritis: A Single-Blind Randomised Controlled Trial. Pain Res. Manag. 2022, 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.A.; Hamid, M.S.A.; Yusof, A. Effects of low-level and high-intensity laser therapy as adjunctive to rehabilitation exercise on pain, stiffness and function in knee osteoarthritis: a systematic review and meta-analysis. Physiotherapy 2021, 114, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Gur, A.; Cosut, A.; Sarac, A.J.; Cevik, R.; Nas, K.; Uyar, A. Efficacy of different therapy regimes of low-power laser in painful osteoarthritis of the knee: A double-blind and randomized-controlled trial. Lasers Surg. Med. 2003, 33, 330–338. [Google Scholar] [CrossRef] [PubMed]
- BTL-Corporate. High-Intensity Laser: Painless and non-surgical management. 2023 (, 2023). Available from: www.high-intensity-laser.com. 15 February.
- Kheshie, A.R.; Alayat, M.S.M.; Ali, M.M.E. High-intensity versus low-level laser therapy in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci. 2014, 29, 1371–1376. [Google Scholar] [CrossRef]
- Askim, K.; Knardahl, S. The Influence of Affective State on Subjective-Report Measurements: Evidence From Experimental Manipulations of Mood. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Eckhard, L.; Munir, S.; Wood, D.; Talbot, S.; Brighton, R.; Walter, W.L.; Baré, J. Minimal important change and minimum clinically important difference values of the KOOS-12 after total knee arthroplasty. Knee 2021, 29, 541–546. [Google Scholar] [CrossRef]
- Alfredo, P.P.; Bjordal, J.M.; Dreyer, S.H.; Meneses, S.R.F.; Zaguetti, G.; Ovanessian, V.; Fukuda, T.Y.; Junior, W.S.; Martins, R. .B.L.; Casarotto, R.A.; et al. Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: a randomized double-blind study. Clin. Rehabilitation 2011, 26, 523–533. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; A Serdar, M. Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Medica 2021, 31, 27–53. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.; Hart, H.; Mills, K. Osteoarthritis year in review 2018: rehabilitation and outcomes. Osteoarthr. Cartil. 2019, 27, 378–391. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Iijima, H.; Tashiro, Y.; Kajiwara, Y.; Zeidan, H.; Shimoura, K.; Nishida, Y.; Bito, T.; Nakai, K.; Tatsumi, M.; et al. Home exercise therapy to improve muscle strength and joint flexibility effectively treats pre-radiographic knee OA in community-dwelling elderly: a randomized controlled trial. Clin. Rheumatol. 2018, 38, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Ponvel, P.; Singh, D.K.A.; Soon, M.S.; Kamsan, S.S.; Ahmad, M.A. Comparison of Physical Performance between Older Adult Fallers with and without Knee Osteoarthritis. J. Sains Kesihat. Malays. 2019, 17, 147–155. [Google Scholar] [CrossRef]
- Alfredo, P.P.; Bjordal, J.M.; Junior, W.S.; Lopes-Martins, R. .B.; Stausholm, M.B.; Casarotto, R.A.; Marques, A.P.; Joensen, J. Long-term results of a randomized, controlled, double-blind study of low-level laser therapy before exercises in knee osteoarthritis: laser and exercises in knee osteoarthritis. Clin. Rehabilitation 2017, 32, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Nazari, A. , Moezy, A. , Nejati, P., Mazaherinezhad, A., et al. Efficacy of high-intensity laser therapy in comparison with conventional physiotherapy and exercise therapy on pain and function of patients with knee osteoarthritis: A randomised controlled trial with 12-week follow up. Lasers Med. Sci. 2019, 34, 505–516. [Google Scholar]
- Al Rashoud, A.; Abboud, R.; Wang, W.; Wigderowitz, C. Efficacy of low-level laser therapy applied at acupuncture points in knee osteoarthritis: a randomised double-blind comparative trial. Physiotherapy 2014, 100, 242–248. [Google Scholar] [CrossRef]
- Multanen, J.; Honkanen, M.; Häkkinen, A.; Kiviranta, I. Construct validity and reliability of the Finnish version of the Knee Injury and Osteoarthritis Outcome Score. BMC Musculoskelet. Disord. 2018, 19, 155. [Google Scholar] [CrossRef]
- Collins, N.J.; Misra, D.; Felson, D.T.; Crossley, K.M.; Roos, E.M. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. 2011, 63, S208–S228. [Google Scholar] [CrossRef]
- Phatama, K.Y.; Aziz, A.; Bimadi, M.H.; Oktafandi, I.G.N.A.A.; Cendikiawan, F.; Mustamsir, E. Knee Injury and Osteoarthritis Outcome Score: Validity and Reliability of an Indonesian Version. Ochsner J. 2021, 21, 63–67. [Google Scholar] [CrossRef]
- Zulkifli, M. M, Kadir, A. A., Elias, A., Bea, K.C., Sadagatullah, A.N. Psychometric properties of the malay language version of knee injury and osteoarthritis outcome score (KOOS) questionnaire among knee osteoarthritis patients: a confirmatory factor analysis. Malay. Orthop. J. 2017, 11, 7–14. [Google Scholar]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthr. Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, ume 11, 851–856. [Google Scholar] [CrossRef]
- Hancock, G.E.; Hepworth, T.; Wembridge, K. Accuracy and reliability of knee goniometry methods. J. Exp. Orthop. 2018, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.; Anwer, S.; Brismée, J.-M. The reliability and minimal detectable change of Timed Up and Go test in individuals with grade 1 – 3 knee osteoarthritis. BMC Musculoskelet. Disord. 2015, 16, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Barry, D. Sarcopenia: Textbook of Natural Medicine. In. Joseph E. Pizzorno, Michael T. Murray (Fifth Edition): Churchill Livingstone 2020.
- Maldaner, N.; Sosnova, M.; Ziga, M.; Zeitlberger, A.M.; Bozinov, O.; Gautschi, O.P.; Weyerbrock, A.; Regli, L.; Stienen, M.N.M. External Validation of the Minimum Clinically Important Difference in the Timed-up-and-go Test After Surgery for Lumbar Degenerative Disc Disease. Spine 2021, 47, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain 2004, 8, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Probst, P. , Grummich, K. , Heger, P., Zaschke, S., Knebel, P., Ulrich, A., et al. Blinding in randomised controlled trials in general and abdominal surgery: Protocol for a systematic review and empirical study. Sys. Rev. 2016, 5, 48–54. [Google Scholar]
- Delkhosh, C.T. , Fatemy, E. , Ghorbani, R., Mohammadi, R. Comparing the immediate and long-term effects of low and high power laser on the symptoms of knee osteoarthritis. J. Maz. Univ. Med. Sci. 2018, 28, 69–77. [Google Scholar]
- Braghin, R.d.M.B.; Libardi, E.C.; Junqueira, C.; Rodrigues, N.C.; Nogueira-Barbosa, M.H.; Renno, A.C.M.; de Abreu, D.C.C. The effect of low-level laser therapy and physical exercise on pain, stiffness, function, and spatiotemporal gait variables in subjects with bilateral knee osteoarthritis: a blind randomized clinical trial. Disabil. Rehabilitation 2018, 41, 3165–3172. [Google Scholar] [CrossRef]
- Wickenheisser, V.A.; Zywot, E.M.; Rabjohns, E.M.; Lee, H.H.; Lawrence, D.S.; Tarrant, T.K. Laser Light Therapy in Inflammatory, Musculoskeletal, and Autoimmune Disease. Curr. Allergy Asthma Rep. 2019, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kamsan, S.S.; Singh, D.K.A.; Tan, M.P.; Kumar, S. The knowledge and self-management educational needs of older adults with knee osteoarthritis: A qualitative study. PLOS ONE 2020, 15, e0230318. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.A. , Singh, D. K.A., Qing, C.W., Rahman, N.N.A., Padzil, F.M. Knee osteoarthritis and its related issues: Patients’ perspective. Malay. J. Health Sci. 2018, 16, 171–177. [Google Scholar]
- Shori, G.; Kapoor, G.; Talukdar, P. Effectiveness of home-based physiotherapy on pain and disability in participants with osteoarthritis of knee: an observational study. J. Phys. Ther. Sci. 2018, 30, 1232–1236. [Google Scholar] [CrossRef]
- Turner, M.N.; Hernandez, D.O.; Cade, W.; Emerson, C.P.; Reynolds, J.M.; Best, T.M. The Role of Resistance Training Dosing on Pain and Physical Function in Individuals With Knee Osteoarthritis: A Systematic Review. Sports Heal. A Multidiscip. Approach 2019, 12, 200–206. [Google Scholar] [CrossRef]
| Variables | LL+EX (n = 17) |
HL+EX (n = 17) |
p-value |
| Age (years) | 57.94 (10.56) | 51.18 (9.79) | 0.062 |
| Gender (male/female) | 5/12 | 3/14 | 0.344 |
| Body mass index (kg/m²) | 27.57 (4.47) | 30.58 (5.43) | 0.088 |
| KOA duration (months) | 38.35 (28.26) | 39.88 (39.11) | 0.897 |
| Affected side (uni/bilateral) | 5/12 | 2/15 | 0.199 |
| K-L grade (I/II/III) | 0/5/12 | 0/9/8 | 0.142 |
| Mobility aid (yes/no) | 14/3 | 14/3 | 0.672 |
| KOOS (total score) | 46.06 (9.47) | 44.28 (12.41) | 0.642 |
| NPRS (score) | 6.19 (1.45) | 6.48 (1.21) | 0.537 |
| Active knee flexion (degree) | 112.11 (11.87) | 110.65 (9.73) | 0.697 |
| TUG (time, sec) | 9.65 (1.51) | 9.46 (0.75) | 0.639 |
| Outcomes | LL+EX (n = 17) |
HL+EX (n = 17) |
Between-groups (analysis of covariance) |
||
| Mean (SD) | Mean (SD) | p-value | Effect size | ||
| KOOS (Total score) |
Pre | 46.06 (9.47) | 44.28 (12.41) | p = 0.001* | 0.53 |
| Post | 50.90 (13.92) | 58.12 (13.25) | |||
| MD; 95% CI; p | 4.84; 1.74 to 7.94; p = 0.004* | 13.84; 9.83 to 17.85; p < 0.001* | |||
| Symptoms | Pre | 10.87 (3.83) | 11.75 (2.65) | p = 0.002* | 0.14 |
| Post | 9.73 (3.83) | 8.32 (1.60) | |||
| MD; 95% CI; p | -1.12; -1.94 to -0.32; p = 0.009* | -3.43; -4.61 to -2.25; p < 0.001* | |||
| Pain | Pre | 18.32 (5.70) | 20.14 (6.38) | p < 0.001* | 1.04 |
| Post | 15.86 (5.50) | 11.09 (3.39) | |||
| MD; 95% CI; p | -2.46; -3.97 to -0.94; p = 0.003* | -9.05; -11.68 to -6.40; p < 0.001* | |||
| ADL | Pre | 36.73 (9.28) | 32.51 (11.48) | p = 0.014* | 0.26 |
| Post | 39.34 (8.33) | 41.90 (11.44) | |||
| MD; 95% CI; p | 2.60; 0.41 to 4.80; p = 0.023* | 9.40; 5.03 to 13.78; p < 0.001* | |||
| Sports | Pre | 3.92 (1.97) | 3.86 (3.31) | p < 0.001* | 0.64 |
| Post | 4.40 (2.16) | 6.55 (4.24) | |||
| MD; 95% CI; p | 0.48; 0.14 to 0.82; p = 0.007* | 2.69; 1.65 to 3.74; p < 0.001* | |||
| QOL | Pre | 4.67 (2.59) | 4.01 (2.43) | p = 0.002* | 0.66 |
| Post | 5.32 (2.88) | 7.24 (2.90) | |||
| MD; 95% CI; p | 0.65; 0.29 to 1.01; p = 0.002* | 3.24; 2.39 to 4.09; p < 0.001* | |||
| NPRS | Pre | 6.19 (1.45) | 6.48 (1.21) | p < 0.001* | 1.05 |
| Post | 4.24 (1.16) | 3.21 (0.75) | |||
| MD; 95% CI; p | -1.95; -2.3 to -1.53; p < 0.001* | -3.28; -3.78 to -2.76; p < 0.001* | |||
| Active knee flexion | Pre | 112.11 (11.87) | 110.65 (9.73) | p < 0.001* | 0.61 |
| Post | 115.23 (10.69) | 120.17 (4.26) | |||
| MD; 95% CI; p | 3.12; 1.56 to 4.68; p = 0.001* | 9.53; 5.57 to 13.49; p < 0.001* | |||
| TUG | Pre | 9.65 (1.51) | 9.46 (0.75) | p = 0.001* | 0.47 |
| Post | 9.13 (1.54) | 8.58 (0.61) | |||
| MD; 95% CI; p | -0.53; -0.64 to -0.41; p < 0.001* | -0.88; -1.04 to -0.72; p < 0.001* | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





