Submitted:
15 May 2023
Posted:
16 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Older Adults: Frailty Check Supporters and Participants
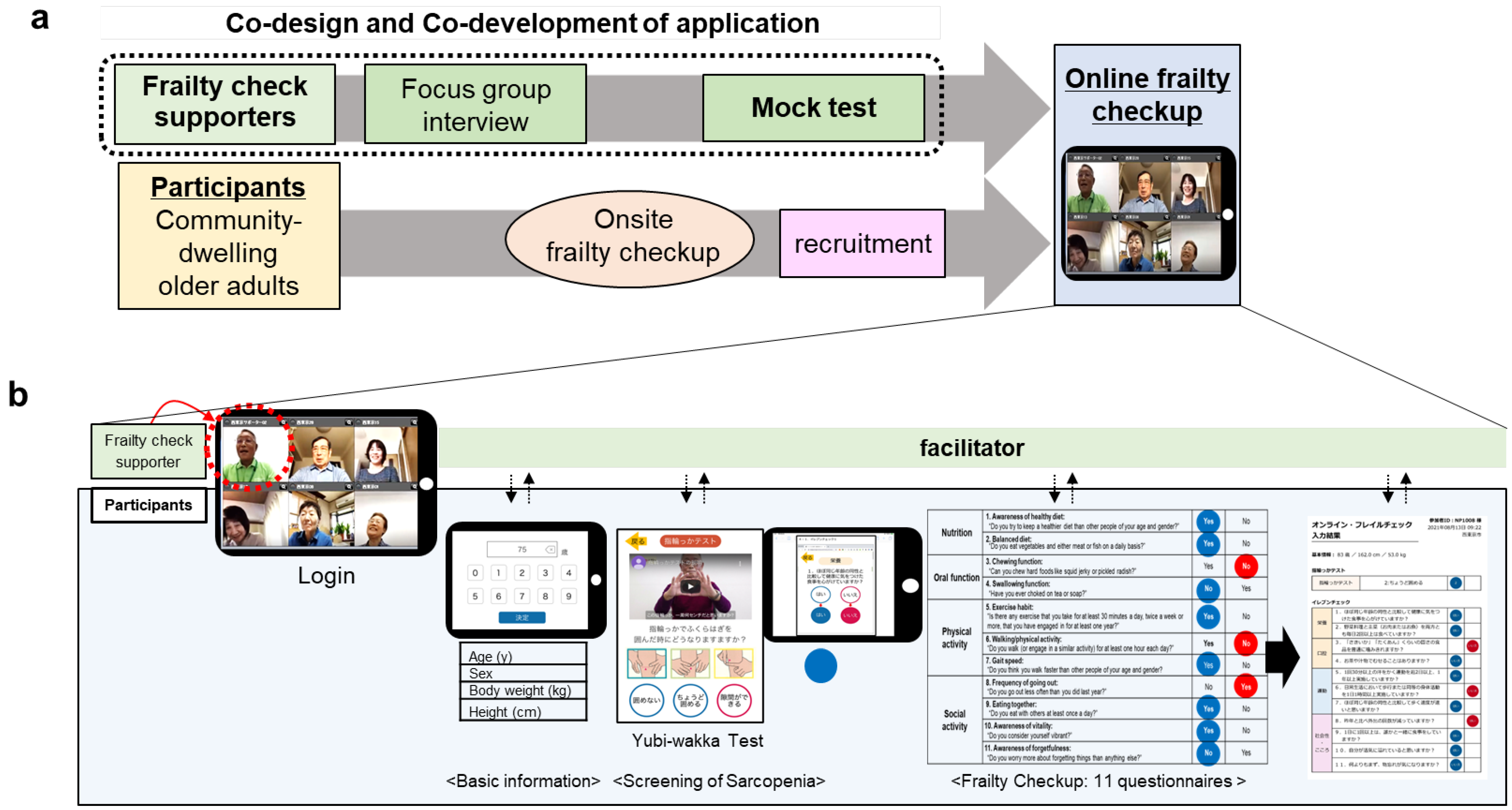
2.2. Study Design
2.2.1. Online Frailty Check Application: Device and Contents
2.2.2. Development and Refinement of Application; Participatory Action Research Method
2.3. Questionnaires
2.4. Analysis
3. Results
3.1. Frailty Check Supporters and Participants
3.2. Development and Refinement of the Application
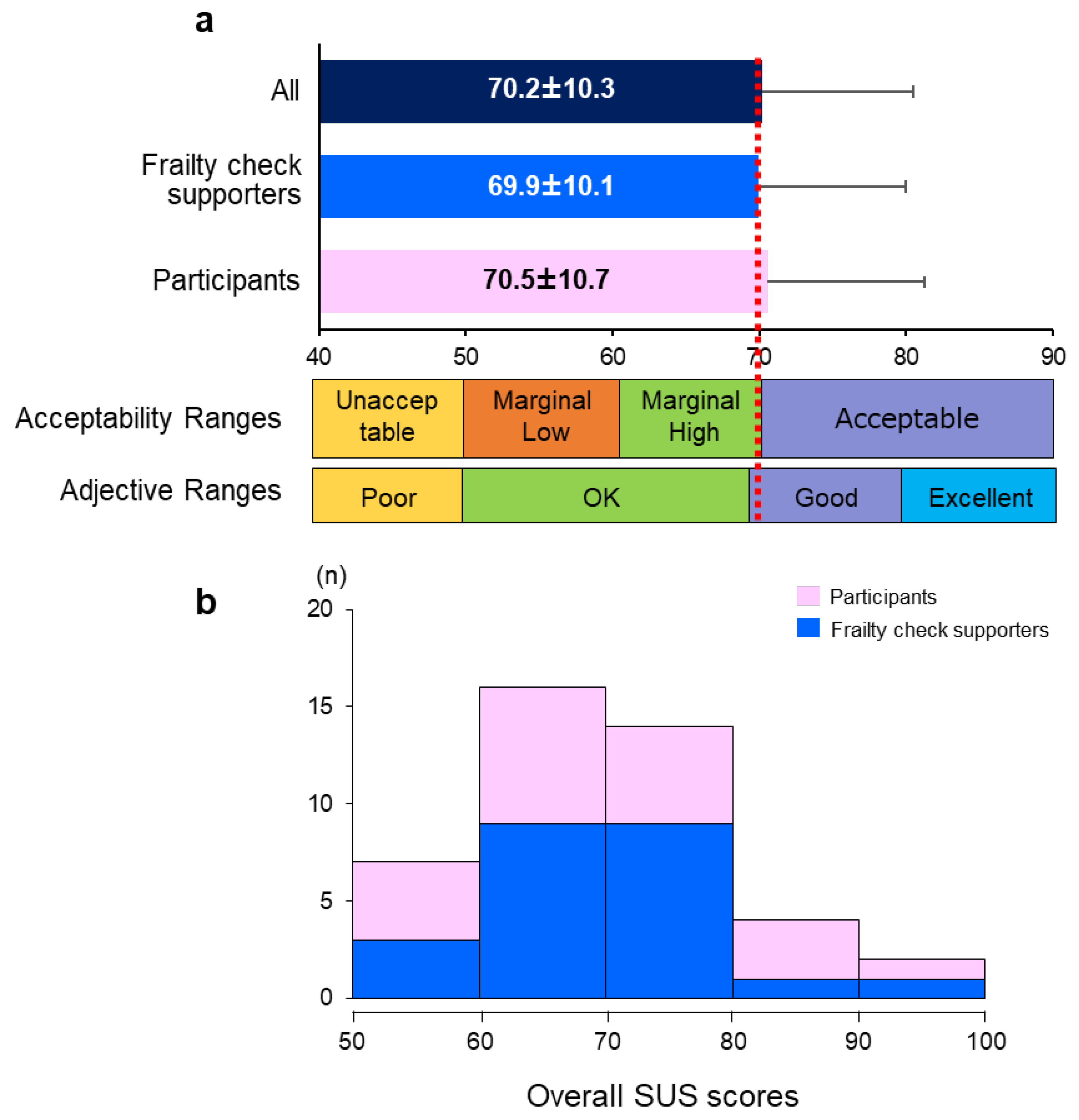
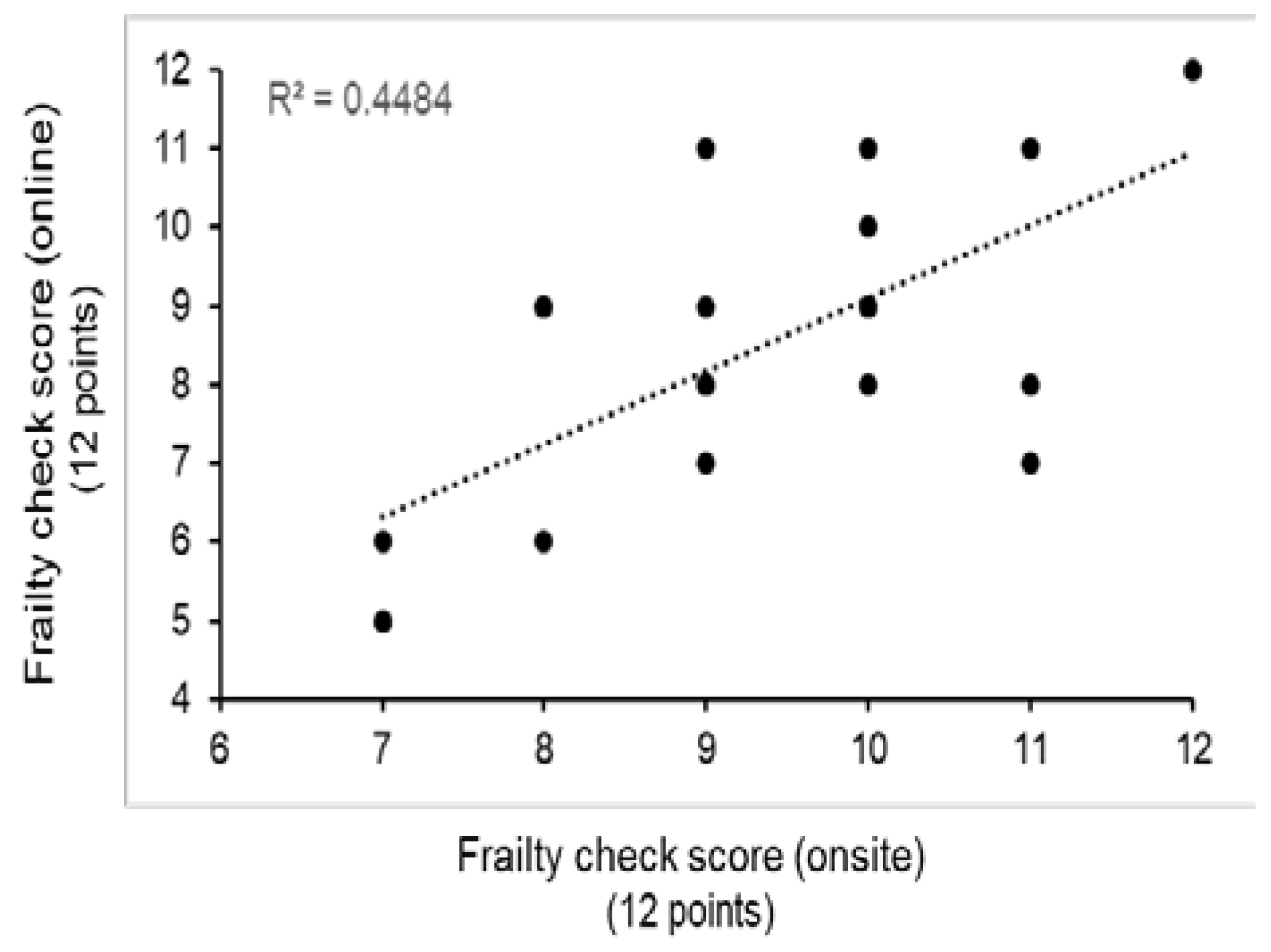
3.3. Self-efficacy of Frailty Check Supporters and Usability Evaluation
4. Discussion
4.1. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walston, J.; Hadley, E.C.; Ferrucci, L.; Guralnik, J.M.; Newman, A.B.; Studenski, S.A.; Ershler, W.B.; Harris, T.; Fried, L.P. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006, 54, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Ishii, S.; Tanaka, T.; Shibasaki, K.; Ouchi, Y.; Kikutani, T.; Higashiguchi, T.; Obuchi, S.P.; Ishikawa-Takata, K.; Hirano, H.; Kawai, H.; et al. Development of a simple screening test for sarcopenia in older adults. Geriatr Gerontol Int. 2014, 14, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Takahashi, K.; Akishita, M.; Tsuji, T.; Iijima, K. Yubi-wakka (finger-ring) test: a practical self-screening method for sarcopenia, and a predictor of disability and mortality among Japanese community-dwelling older adults. Geriatr Gerontol Int. 2018, 18, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Johnson, H.H.; Glascoff, M.A.; Lovelace, K.; Bibeau, D.L.; Tyler, E.T. Assessment of public health educator practice: health educator responsibilities. Health Promot Pract. 2005, 6, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Kalantar-Zadeh, K.; Anker, S.D. COVID-19: a major cause of cachexia and sarcopenia? J Cachexia Sarcopenia Muscle. 2020, 11, 863–865. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.B. Does COVID-19-related cachexia mimic cancer-related cachexia? Examining mechanisms, clinical biomarkers, and potential targets for clinical management. J Cachexia Sarcopenia Muscle. 2021, 12, 519–522. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. The influence of the COVID-19 pandemic on physical activity and new incidence of frailty among initially non-frail older adults in Japan: a follow-up online survey. J Nutr Health Aging. 2021, 25, 751–756. [Google Scholar] [CrossRef]
- Shimokihara, S.; Maruta, M.; Hidaka, Y.; Akasaki, Y.; Tokuda, K.; Han, G.; Ikeda, Y.; Tabira, T. Relationship of decrease in frequency of socialization to daily life, social life, and physical function in community-dwelling adults aged 60 and over after the COVID-19 pandemic. Int J Environ Res Public Health. 2021, 18, 2573. [Google Scholar] [CrossRef]
- Son, B.K.; Imoto, T.; Inoue, T.; Nishimura, T.; Tanaka, T.; Iijima, K. Social detachment influenced muscle mass and strength during the COVID-19 pandemic in Japanese community-dwelling older women. J Frailty Aging. 2022, 11, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Sakano, Y.; Tohjoh, M. The general self-efficacy scale (GSES): scale development and validation. Jpn J Behav Ther. 1986, 12, 173–182. [Google Scholar]
- Parmanto, B.; Lewis, A.N. Jr.; Graham, K.M.; Bertolet, M.H. Development of the telehealth usability questionnaire (TUQ). Int J Telerehabil. 2016, 8, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J. SUS: a ‘quick and dirty’ usability scale. Usability Eval Ind. 1996, 189, 4–7. [Google Scholar]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An empirical evaluation of the system usability scale. Int J Hum-Comput Int. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J Epidemiol Community Health. 2006, 60, 854–857. [Google Scholar] [CrossRef] [PubMed]
- Hand, C.; Rudman, D.L.; McGrath, C.; Donnelly, C.; Sands, M. Initiating participatory action research with older adults: lessons learned through reflexivity. Can J Aging. 2019, 38, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Seino, S.; Tomine, Y.; Nishi, M.; Hata, T.; Fujiwara, Y.; Shinkai, S.; Kitamura, A. Effectiveness of a community-wide intervention for population-level frailty and functional health in older adults: a 2-year cluster nonrandomized controlled trial. Prev Med. 2021, 149, 106620. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Rodríguez, D.; Santillán García, A.; Montoro Robles, J.; Rodríguez Salvador, M.D.M.; Muñoz Ronda, F.J.; Arrogante, O. Increase in video consultations during the COVID-19 pandemic: healthcare professionals’ perceptions about their implementation and adequate management. Int J Environ Res Public Health. 2020, 17, 5112. [Google Scholar] [CrossRef] [PubMed]
- Pywell, J.; Vijaykumar, S.; Dodd, A.; Coventry, L. Barriers to older adults’ uptake of mobile-based mental health interventions. Digit Health. 2020, 6, 2055207620905422. [Google Scholar] [CrossRef] [PubMed]
- Askari, M.; Klaver, N.S.; van Gestel, T.J.; van de Klundert, J. Intention to use medical apps among older adults in the Netherlands: cross-sectional study. J Med Internet Res. 2020, 22, e18080. [Google Scholar] [CrossRef] [PubMed]
| Frailty check supporters |
Participants | p | |
| n | 32 | 20 | |
| Men/Women | 12/20 | 7/13 | 0.855 |
| Age (y) | 74.0 (67-86) | 82.0 (70-91) | 0.001 |
| Education level (longer than 14 years, %) |
23 (71.9%) | 7 (35.0%) | 0.009 |
| Resident period (years) | 40.5±16.0 | 35.3±17.2 | 0.277 |
| Living alone (%) | 7 (21.9%) | 6 (30.0%) | 0.752 |
| Subjective health (healthy status %) |
32 (100.0%) | 19 (95.0%) | 0.202 |
| Subjective well-being (10 points) |
8.0 (3.0-10.0) |
8.0 (5.0-10.0) |
0.854 |
| Subjective proficiency of ICT (10 points) |
5.5 (1.0-9.0) |
5.0 (0.0-10.0) |
0.082 |
| Category | Opinions (No. of opinions) | Example for opinions | Refinement |
|---|---|---|---|
| Reliability | Item entry (1) | “It is difficult for participants to enter the numbers unless FC supporters ask them verbally.” | Preparation of information to be entered before the test |
| Progress status (3) | “It would be better to have a display showing that other participants are still answering.” | Addition of a page to check the progress | |
| Final confirmation page (3) | “It would be better to be able to recognize which questions have not been answered at the end.” | Addition of confirmation page | |
| Homogeneity with onsite frailty check (3) |
“I want the answer page to be displayed similarly the onsite 11 self-reporting FC questionnaires page.” | Change to the similar design as the onsite questionnaire | |
| Change of display name (1) | “It would be better to be able to change the display name on the app.” | Indication of the participants' affiliation in their native language for easy understanding | |
| Need for training & practice (4) | “I think it would be preferable for supporters to work as a pair so that they could help each other.” | Conduction of self-directed learning activities by the supporters | |
| Encouragement (1) | “I thought I should support everyone by saying, ‘I couldn't do it either, but now I can.’” | Addition to cheering sound effect function | |
| Provision of frailty check results (2) | “In the onsite frailty check, participants can take home a paper of the results, but what about that during online frailty check?” “Can each participant receive their own data?” | Addition of a printing function and distribution of printed result to users | |
| Social interaction | Identification of speaker (3) | “I want a function/signal designed that allows me to recognize who the speaker is.” | Manualization of communication function |
| Tablet camera setting (2) | “My finger hits the camera when I hold the tablet.” | Manualization of setting and facilitating by the supporter | |
| Online communication (3) | “When we're online, we can't properly capture the other side's reaction, so we talk less often.” | Building intimacy through daily conversation before the measurement | |
| User-friendliness | Button (4) | “Buttons are small and difficult to touch with fingertips. I think it would be easier to do with a stylus.” | Use of a stylus |
| Touch screen sensitivity (2) | “Buttons do not respond when my fingers are dry.” | Use of a stylus | |
| Touch screen skills (4) | “I don't know how to press the button.” | Instruction provision, Addition of button pressing simulator | |
| Font (3) | “A larger font is better.” | Use of a larger font size | |
| Initialization function (1) | “It is better to design the question form so that the users can go back to the previous question.” | Manualization of operation method and clarification of troubleshooting | |
| Tutorial function (1) | “It would be good to have a button-pressing practice function. Elderly people can't learn it in one session.” | Addition of button pressing simulator | |
| Visual design (2) | “I want the design to be relevant to frailty check and the elderly.” | Improvement of layout | |
| Social interaction & Reliability |
Timing to watch the Yubi-wakka tutorial video (2) | “Some participants think the video starts automatically, so they need to be verbally informed.” | Addition of step-by-step tutorial video |
| Calling attention (1) | “To prevent accidents, appropriate explanations such as ‘Please sit in a chair during the examination’ are needed.” | Emphasizing in the step-by-step tutorial video, with verbal reminders by the supporter | |
| Frailty check procedures (1) | “I think it would be easier for participants to 11 self-reporting FC questionnaires, if the supporters read the questions one by one.” | Checking the progress by calling participant's name | |
| Announcement for ending (1) | “It would be better to all say goodbye and then guide participants to press the exit button.” | Instruction manual and verbal reminder | |
| Reliability & User-friendly |
Answer format (1) | “It would be better for all participants to answer each question simultaneously.” | Converting one page forms to one question per page form |
| Backward function (1) | “On all pages, I want a button to go back to the previous page.” | Addition of backward function | |
| Display of the test tutorial video (5) | “Please consider making an Yubi-wakka test explanation video in advance and showing it during the check.” | Verbal guidance on how to play the tutorial video |
| General Self-Efficacy Scale | Before | After | p | |
|---|---|---|---|---|
| Self-efficacy (total score, points/ 16 points) | 12.0 (5.0-16.0) |
13.0 (6.0-16.0) |
0.498 | |
| Positive behavior ( points/ 7 points) | 6.0 (1.0-7.0) |
6.0 (0.0-7.0) |
0.952 | |
| Q1 | I am confident when I do something. (yes, %) | 77.8 | 77.8 | 0.375 |
| Q2 | I am worried compared to people. (no, %) | 55.6 | 51.9 | 0.312 |
| Q3 | I decide without hesitation when I decide something. (yes, %) | 63.0 | 55.6 | 0.250 |
| Q4 | I think I am a shy person. (no, %) | 70.4 | 70.4 | 0.375 |
| Q5 | I think it's better to work proactively even in jobs where the results are uncertain. (yes, %). | 85.2 | 88.9 | 0.500 |
| Q6 | I am a person who is willing to do anything. (yes, %) | 66.7 | 77.8 | 0.125 |
| Q7 | I am a person who are not good at actively working. (no, %) | 85.2 | 85.2 | 0.500 |
| Non-anxiety about failure ( points/ 5 points) | 4.0 (2.0-5.0) |
5.0 (1.0-5.0) |
0.582 | |
| Q1 | I often feel dark remembering the mistakes and unpleasant experiences I made in the past. (no, %) |
81.5 | 85.2 | 0.375 |
| Q2 | I often feel that I have failed, after finishing work. (no, %) | 92.6 | 92.6 | 0.500 |
| Q3 | I'm often worried that it won't work when to do something. (no, %) | 77.8 | 74.1 | 0.375 |
| Q4 | I often can't get to work since I couldn't decide what to do. (no, %) | 92.6 | 88.9 | 0.312 |
| Q5 | I am concerned all the time for small failure than others(no, %) | 63.0 | 77.8 | 0.094 |
| Social positioning of ability ( points/ 4 points) | 2.0 (1.0-4.0) |
3.0 (0.0-4.0) |
0.593 | |
| Q1 | I have better ability than friends(yes, %) | 40.7 | 55.6 | 0.063 |
| Q2 | I have better memory than humans. (yes, %) | 44.4 | 51.9 | 0.234 |
| Q3 | there are areas where I have a particularly good knowledge than friends(yes, %) | 55.6 | 74.1 | 0.031* |
| Q4 | I think I have the power to contribute to the world. (yes, %) | 85.2 | 88.9 | 0.375 |
| SUS score | p | |
|---|---|---|
| Age | -0.319* | 0.037 |
| Sex | -0.153 | 0.328 |
| Education | 0.376* | 0.013 |
| ICT proficiency | 0.376* | 0.013 |
| Reliability | 0.312* | 0.042 |
| Interaction | 0.309* | 0.044 |
| Model 1 | Model 2 | Model 3 | |||||||
| b | 95% CI | p | b | 95% CI | p | b | 95% CI | p | |
| Reliability | 0.228 | -0.343-1.591 | 0.200 | 0.326* | 0.004-1.782 | 0.049 | 0.400* | 0.243-1.951 | 0.013 |
| Interaction | 0.178 | -0.408-1.244 | 0.313 | 0.196 | -0.289-1.206 | 0.222 | 0.139 | -0.389-1.038 | 0.362 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





