Submitted:
17 May 2023
Posted:
17 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Epidemiology
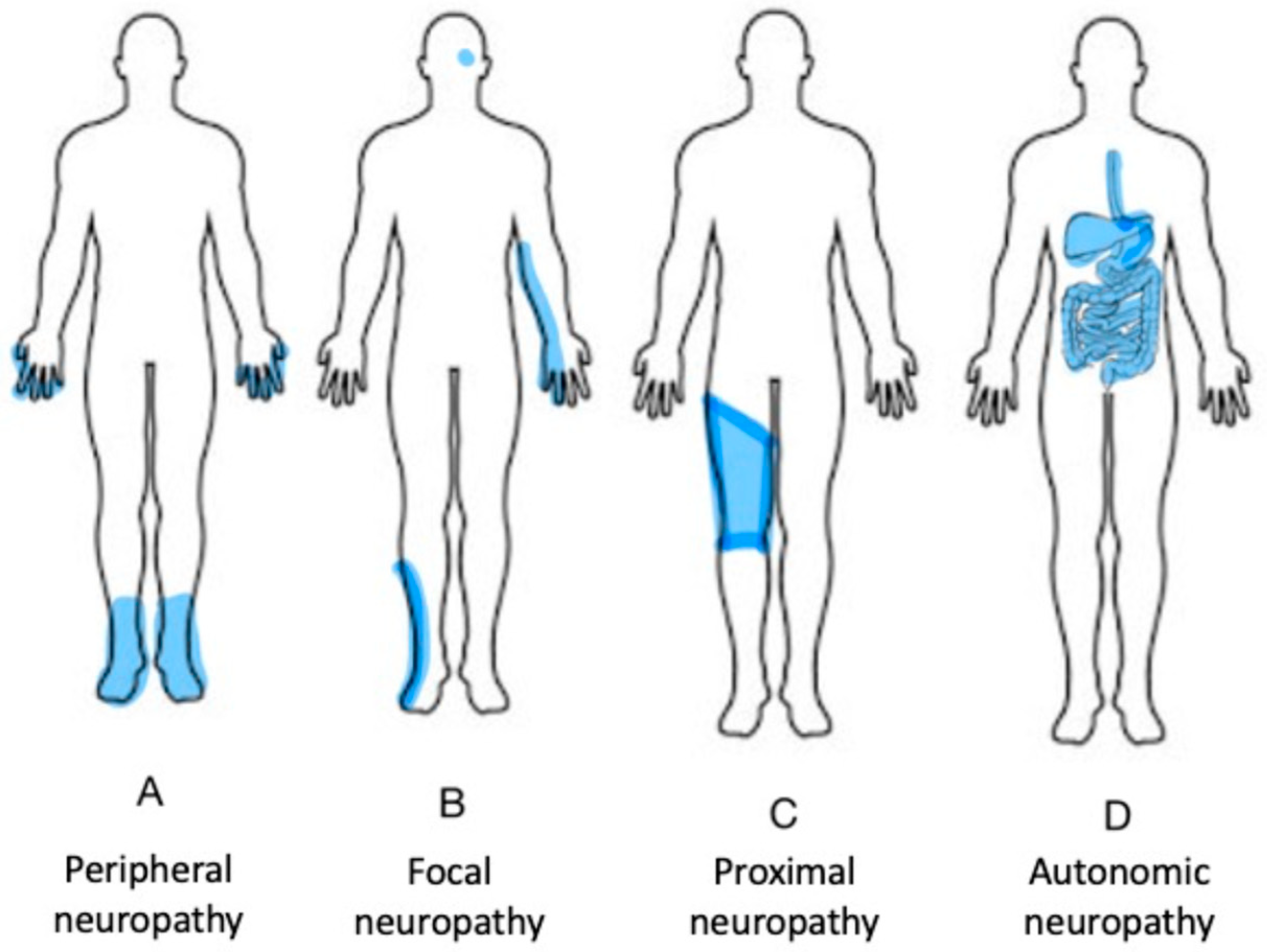
3. Patient Presentation
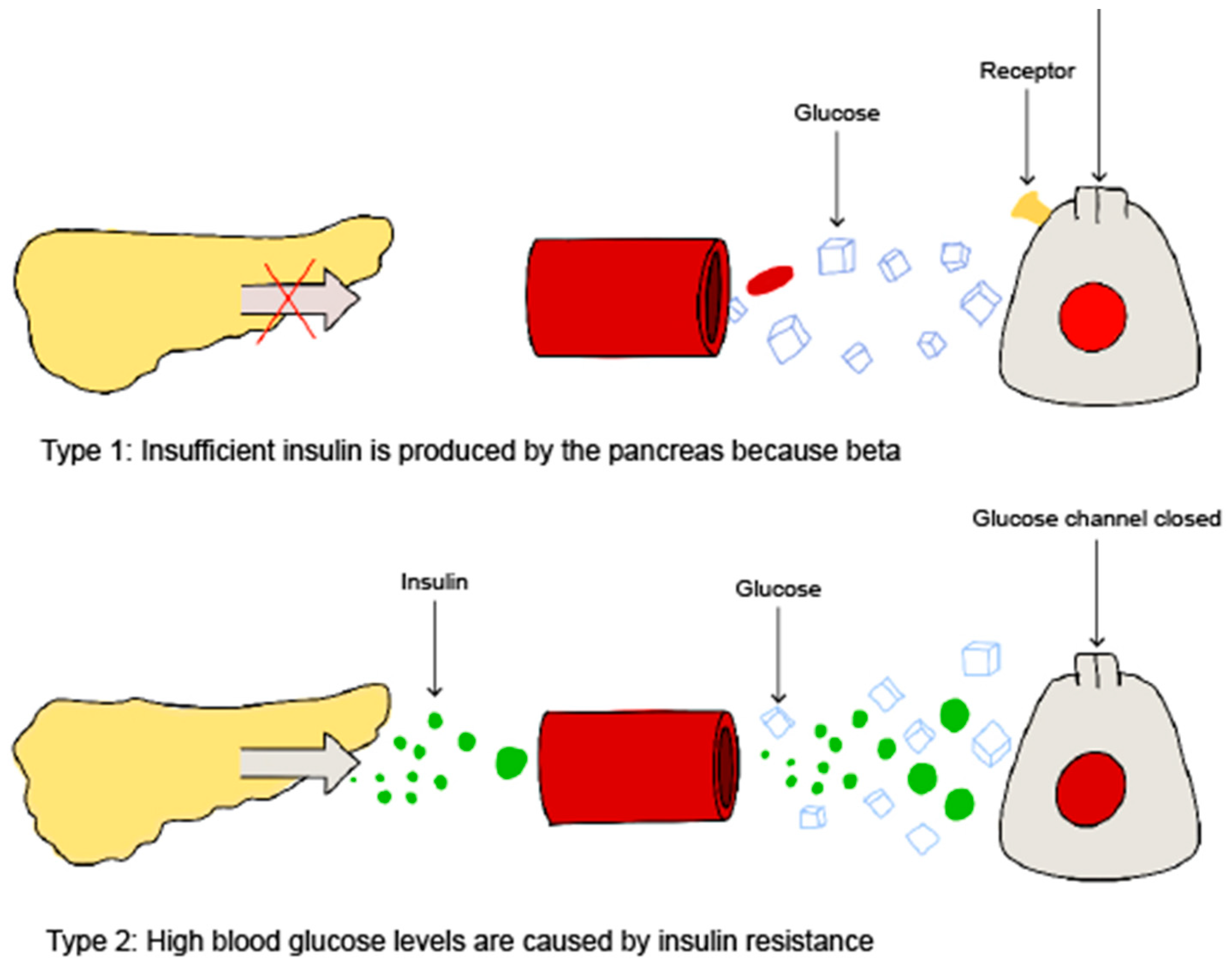
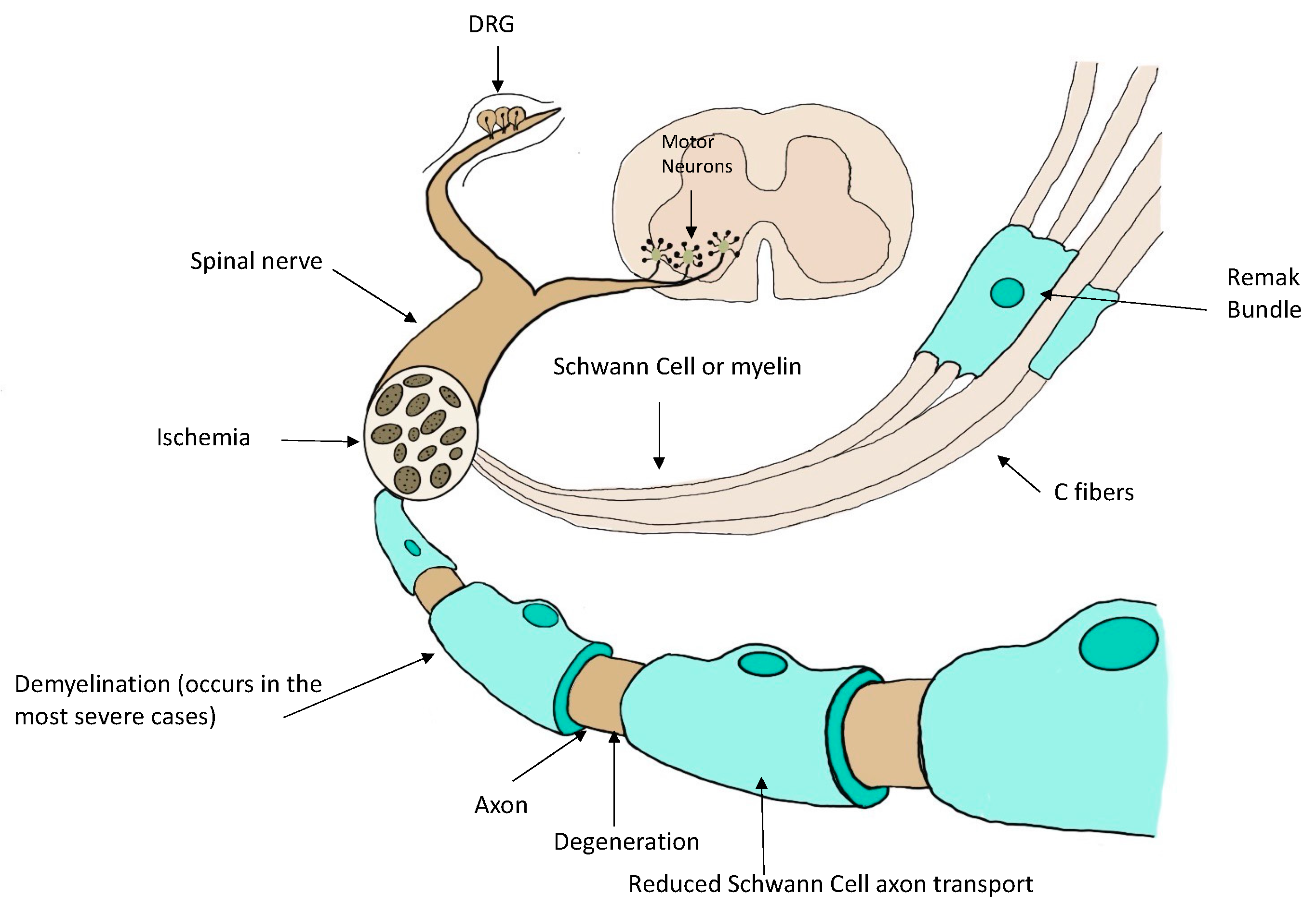
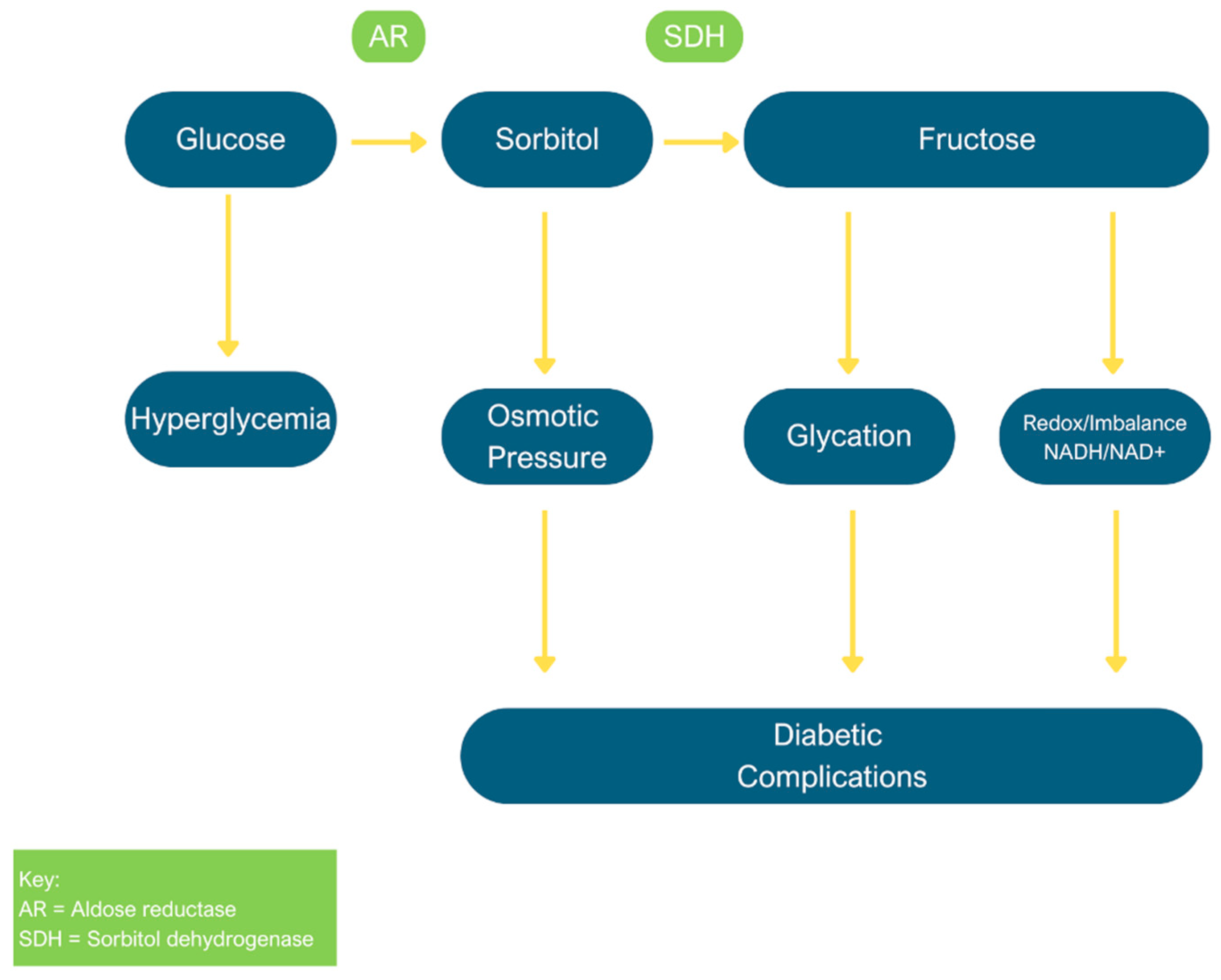
4. Pathophysiology
5. Treatments
6. Conclusion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
List of abbreviations
| ACT | Acceptance and commitment therapy |
| AGE | Advance glycation end product |
| DNP | Diabetic neuropathic pain |
| DPN | Diabetic peripheral neuropathy |
| DPNP | Diabetic peripheral neuropathic pain |
| INF | Intraneural facilitation |
| NCS | Nerve conduction studies |
| PNS | Peripheral nervous system |
| RAGE | Receptor for advanced glycation end |
| SCS | Spinal cord stimulation |
| T1D | Type 1 diabetes |
| T2D | Type 2 diabetes |
References
- Deli, G.; Bosnyak, E.; Pusch, G.; Komoly, S.; Feher, G. Diabetic neuropathies: Diagnosis and management. Neuroendocrinology. 2013, 98, 267. [Google Scholar] [CrossRef] [PubMed]
- Tabish, S.A. Is diabetes becoming the biggest epidemic of the twenty-first century? Int J Health Sci (Qassim). 2007, 1, V–VIII. [Google Scholar] [PubMed]
- Juster-Switlyk, K.; Smith, A.G. Updates in diabetic peripheral neuropathy. F1000Res. 2016, 5. [Google Scholar] [CrossRef]
- Salsali, A.; Nathan, M. A review of types 1 and 2 diabetes mellitus and their treatment with insulin. Am J There. 2006, 13, 349. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.L.; Vincent, A.M.; Cheng, H.T.; Feldman, E.L. Diabetic neuropathy: Mechanisms to management. Pharmacol Ther. 2008, 120, 1. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, D.C.; Blechschmidt, V.; Timmerman, H.; Wolff, A.; Treede, R.-D. Challenges of neuropathic pain: Focus on diabetic neuropathy. J Neural Transm (Vienna). 2020, 127, 589. [Google Scholar] [CrossRef] [PubMed]
- Calabek, B.; Callaghan, B.; Feldman, E.L. Therapy for diabetic neuropathy: An overview. Handb Clin Neurol. 2014, 126, 317. [Google Scholar]
- Oh, J. Clinical spectrum and diagnosis of diabetic neuropathies. Korean J Intern Med. 2020, 35, 1059. [Google Scholar] [CrossRef]
- Iqbal, Z.; Azmi, S.; Yadav, R.; Ferdousi, M.; Kumar, M.; Cuthbertson, D.J.; et al. Diabetic peripheral neuropathy: Epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018, 40, 828. [Google Scholar] [CrossRef]
- Yagihashi, S.; Mizukami, H.; Sugimoto, K. Mechanism of diabetic neuropathy: Where are we now and where to go? J Diabetes Investig. 2010, 2, 18. [Google Scholar] [CrossRef]
- Schreiber, A.K.; Nones, C.F.; Reis, R.C.; Chichorro, J.G.; Cunha, J.M. Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes. 2015, 6, 432. [Google Scholar] [CrossRef] [PubMed]
- Bansal, V.; Misra, U.K.; Kalita, J. Diabetic neuropathy. Postgrad Med J. 2006, 82, 95. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Selvin, E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep. 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, A.K. Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes. 2015, 6, 432. [Google Scholar] [CrossRef] [PubMed]
- Feldman, E.L.; Callaghan, B.C.; Pop-Busui, R.; Zochodne, D.W.; Wright, D.E.; Bennett, D.L.; et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J Diabetes. 2017, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Vase, L.; Wartolowska, K. Pain, placebo, and test of treatment efficacy: A narrative review. Br J Anaesth. 2019, 123, 254. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R. Diabetic neuropathy [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. U.S. Department of Health and Human Services; [cited 2022 Nov 18]. Available online: https://www.niddk.nih.gov/health information/diabetes/overview/preventingproblems/nerve-damage-diabeticneuropathies.
- Callaghan, B.C.; Price, R.S.; Feldman, E.L. Distal symmetric polyneuropathy. JAMA. 2015, 314, 2172. [Google Scholar] [CrossRef]
- Akamine, T.; Kusunose, N.; Matsunaga, N.; Koyanagi, S.; Ohdo, S. Accumulation of sorbitol in the sciatic nerve modulates circadian properties of diabetes induced neuropathic pain hypersensitivity in a diabetic mouse model. Biochem Biophys Res Commun. 2018, 503, 181. [Google Scholar] [CrossRef]
- Bodman, M.A.; Varacallo, M. Peripheral diabetic neuropathy. In: StatPearls.
- Lorenzi, M. The polyol pathway as a mechanism for diabetic retinopathy: Attractive, elusive, and resilient. Exp Diabetes Res. 2007, 2007. [Google Scholar] [CrossRef]
- Srikanth, K.K.; Orrick, J.A. Biochemistry, polyol or sorbitol pathways. In: StatPearls.
- Ishii, N.; Ikenaga, H.; Ogawa, Z.; Aoki, Y.; Saruta, T.; Suga, T. Effects of renal sorbitol accumulation on urinary excretion of enzymes in hyperglycemic rats. Ann Clin Biochem. 2001, 38, 391. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-M.; González, R.G. The effect of high glucose and oxidative stress on lens metabolism, aldose reductase, and senile cataractogenesis. Metabolism. 1986, 35 (4 Suppl 1), 10. [Google Scholar] [CrossRef]
- Hao, W.; Tashiro, S.; Hasegawa, T.; Sato, Y.; Kobayashi, T.; Tando, T.; et al. Hyperglycemia promotes Schwann cell de-differentiation and de-myelination via sorbitol accumulation and IGF1 protein down-regulation. J Biol Chem. 2015, 290, 17106. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, K.; Yasujima, M.; Yagihashi, S. Role of advanced glycation end products in diabetic neuropathy. Curr Pharm Des. 2008, 14, 953. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.M.; Russell, J.W.; Low, P.; Feldman, E.L. Oxidative stress in the pathogenesis of diabetic neuropathy. Endocr Rev. 2004, 25, 612. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R.; Ang, L.; Boulton, A.; Feldman, E.; Marcus, R.; Mizokami-Stout, K.; et al. Diagnosis and treatment of painful diabetic peripheral neuropathy. ADA Clinical Compendia. 2022, 2022, 1. [Google Scholar] [CrossRef]
- Fang, X.-X.; Wang, H.; Song, H.-L.; Wang, J.; Zhang, Z.-J. Neuroinflammation involved in diabetes-related pain and itch. Front Pharmacol. 2022, 13. [Google Scholar] [CrossRef]
- Sloan, G.; Alam, U.; Selvarajah, D.; Tesfaye, S. The treatment of painful diabetic neuropathy. Curr Diabetes Rev. 2022, 18, e070721194556. [Google Scholar] [CrossRef]
- Khdour, M.R. Treatment of diabetic peripheral neuropathy: A review. J Pharm Pharmacol. 2020, 72, 863. [Google Scholar] [CrossRef]
- Várkonyi, T.; Kempler, P. Diabetic neuropathy: New strategies for treatment. Diabetes Obes Metab. 2008, 10, 99. [Google Scholar] [CrossRef]
- Max, M.B.; Lynch, S.A.; Muir, J.; Shoaf, S.E.; Smoller, B.; Dubner, R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med. 1992, 326, 1250. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, M.; Ansari, M.; Basiri, K.; Shaigannejad, V. The effects of intradermal botulinum toxin type a injections on pain symptoms of patients with diabetic neuropathy. J Res Med Sci. 2014, 19, 106. [Google Scholar] [PubMed]
- Tesfaye, S.; Sloan, G.; Petrie, J.; White, D.; Bradburn, M.; Julious, S.; et al. Comparison of amitriptyline supplemented with pregabalin, pregabalin supplemented with amitriptyline, and duloxetine supplemented with pregabalin for the treatment of diabetic peripheral neuropathic pain (option DM): A multicentre, double-blind, randomised crossover trial. Lancet. 2022, 400, 680. [Google Scholar] [PubMed]
- Park, J.H.; Park, H. Botulinum toxin for the treatment of neuropathic pain. Toxins (Basel). 2017, 9. [Google Scholar] [CrossRef]
- Wiffen, P.J.; Derry, S.; Bell, R.F.; Rice, A.S.C.; Töll, T.R.; Phillips, T.; et al. Gabapentin for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017, 6, CD007938. [Google Scholar] [CrossRef] [PubMed]
- Chao, M.T.; Schillinger, D.; Nguyen, U.; Santana, T.; Liu, R.; Gregorich, S.; et al. A randomized clinical trial of group acupuncture for painful diabetic neuropathy among diverse safety net patients. Pain Med. 2019, 20, 2292. [Google Scholar] [CrossRef] [PubMed]
- Taheri, A.A.; Foroughi, A.A.; Mohammadian, Y.; Ahmadi, S.M.; Heshmati, K.; Hezarkhani, L.A.; et al. The effectiveness of acceptance and commitment therapy on pain acceptance and pain perception in patients with painful diabetic neuropathy: A randomized controlled trial. Diabetes Ther. 2020, 11, 1695. [Google Scholar] [CrossRef]
- Smith, M. New LLUH research discovers treatment for diabetic neuropathy [Internet]. News;2022 [cited 2022 Nov 17]. Available online: https://news.llu.edu/research/new-lluh-research-discovers-treatment-fordiabetic-neuropathy.
- Petersen, E.A.; Stauss, T.G.; Scowcroft, J.A.; Brooks, E.S.; White, J.L.; Sills, S.M.; et al. Effect of high-frequency (10-KHz) spinal cord stimulation in patients with painful diabetic neuropathy. JAMA Neurol. 2021, 78, 687. [Google Scholar] [CrossRef]
- Saylor, J. New spinal cord stimulation diabetes treatment approved by FDA [Internet]. Corbin, KY:WYMNT;2022 [cited 2022 Nov 17]. Available online: https://www.wymt.com/2022/02/07/new-spinal-cord-stimulation-diabetes treatment-approved-by-fda/.
- Callaghan, B.C.; Gallagher, G.; Fridman, V.; Feldman, E.L. Diabetic neuropathy: What does the future hold? Diabetologia. 2020, 63, 891. [Google Scholar] [CrossRef]
- Balducci, S.; Iacobellis, G.; Parisi, L.; Di Biase, N.; Calandriello, E.; Leonetti, F.; et al. Exercise training can modify the natural history of diabetic peripheral neuropathy. J Diabetes Complications [Internet]. 2006, 20, 216. [Google Scholar] [CrossRef]
- Pfeifer, M.A.; Schumer, M.P. Clinical trials of diabetic neuropathy: Past, present, and future. Diabetes. 1995, 44, 1355. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



