Submitted:
18 May 2023
Posted:
19 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
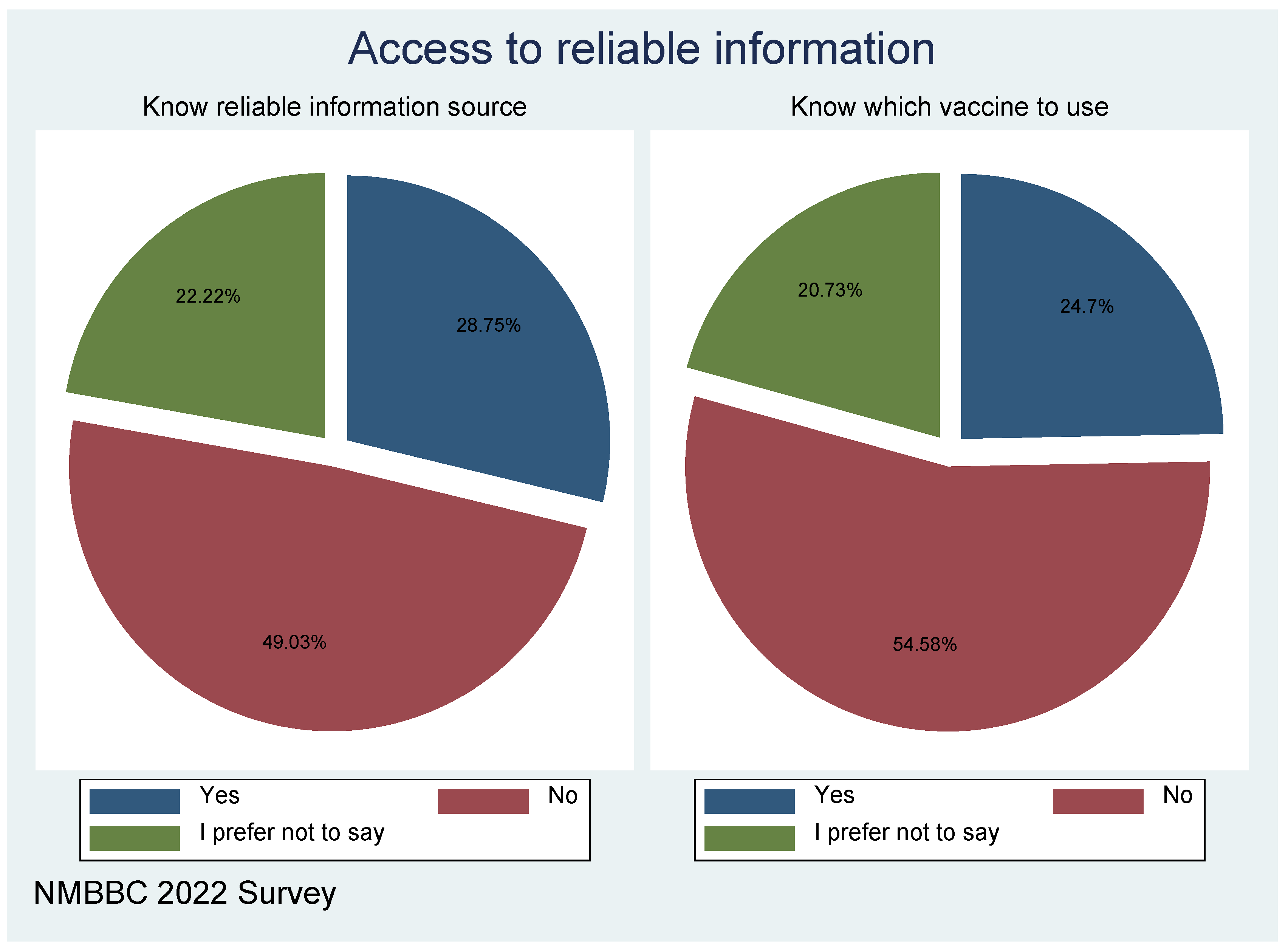
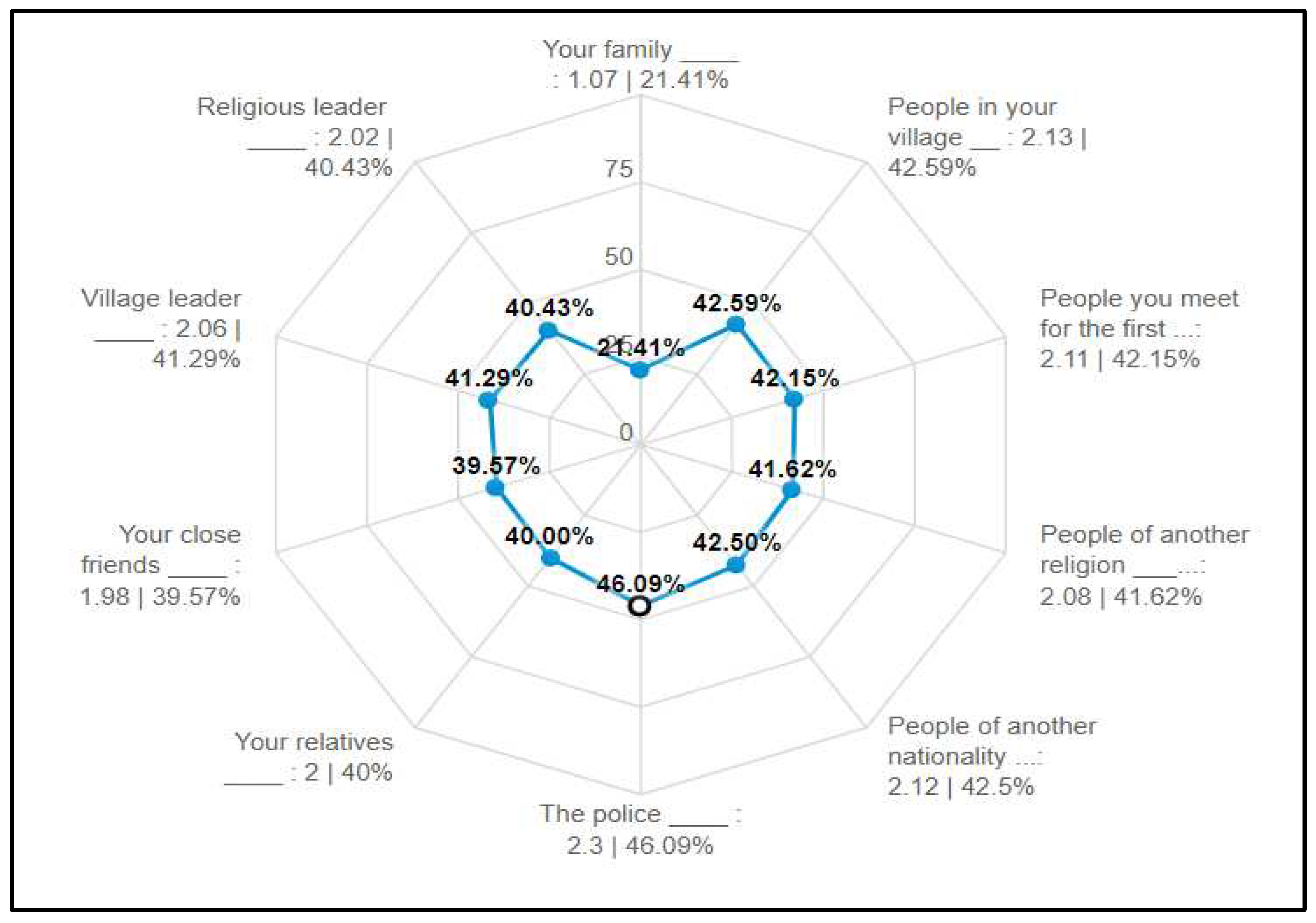
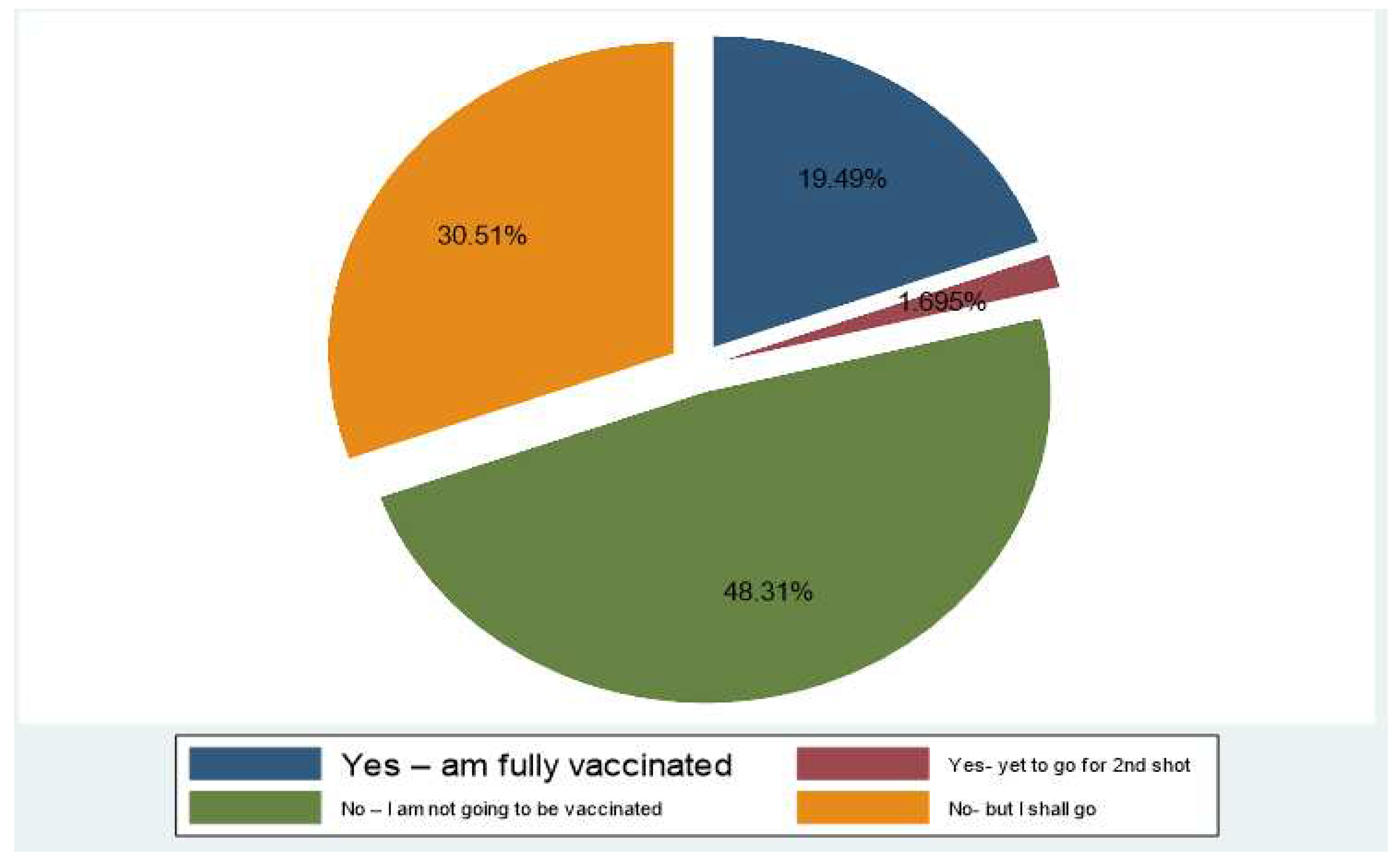
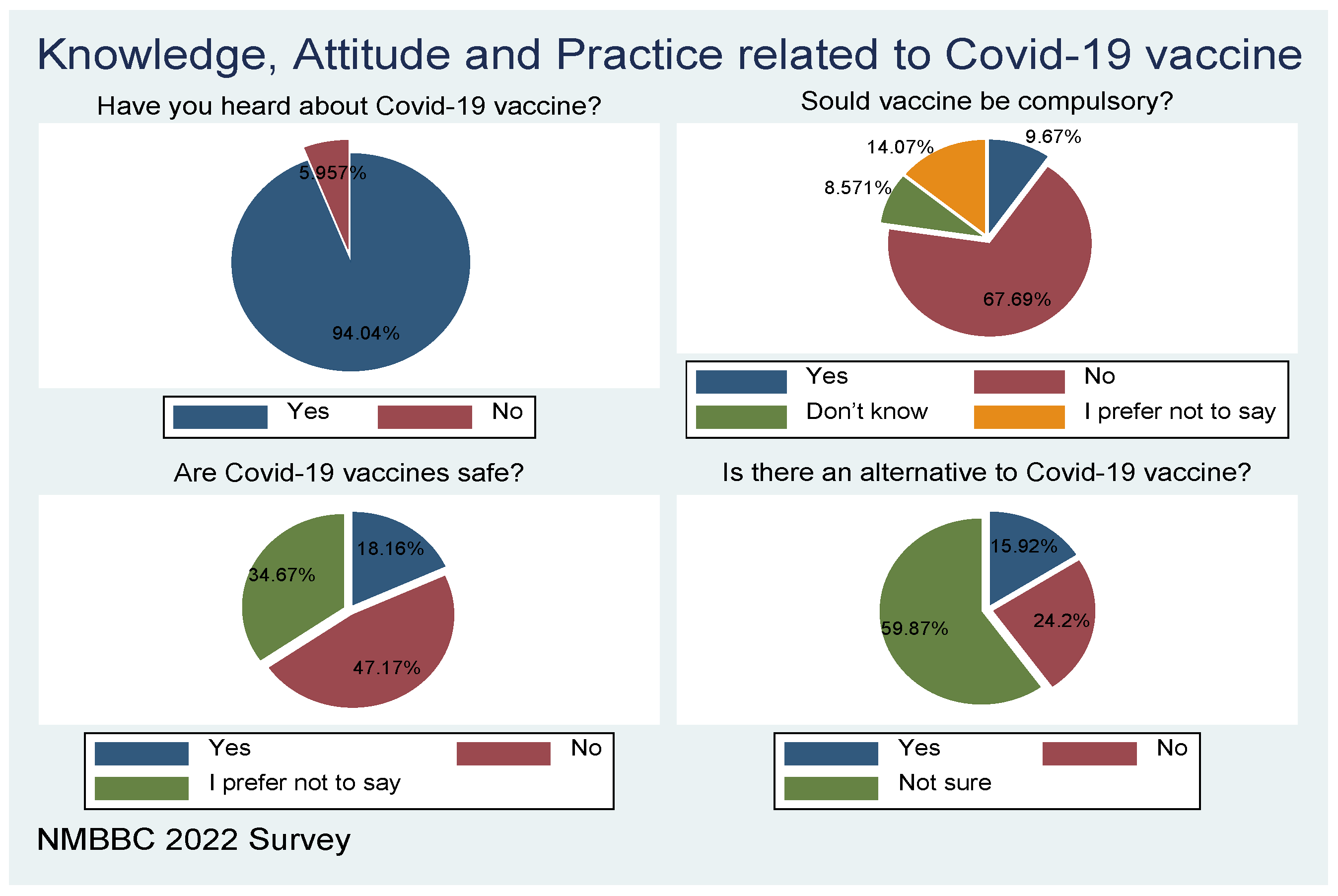
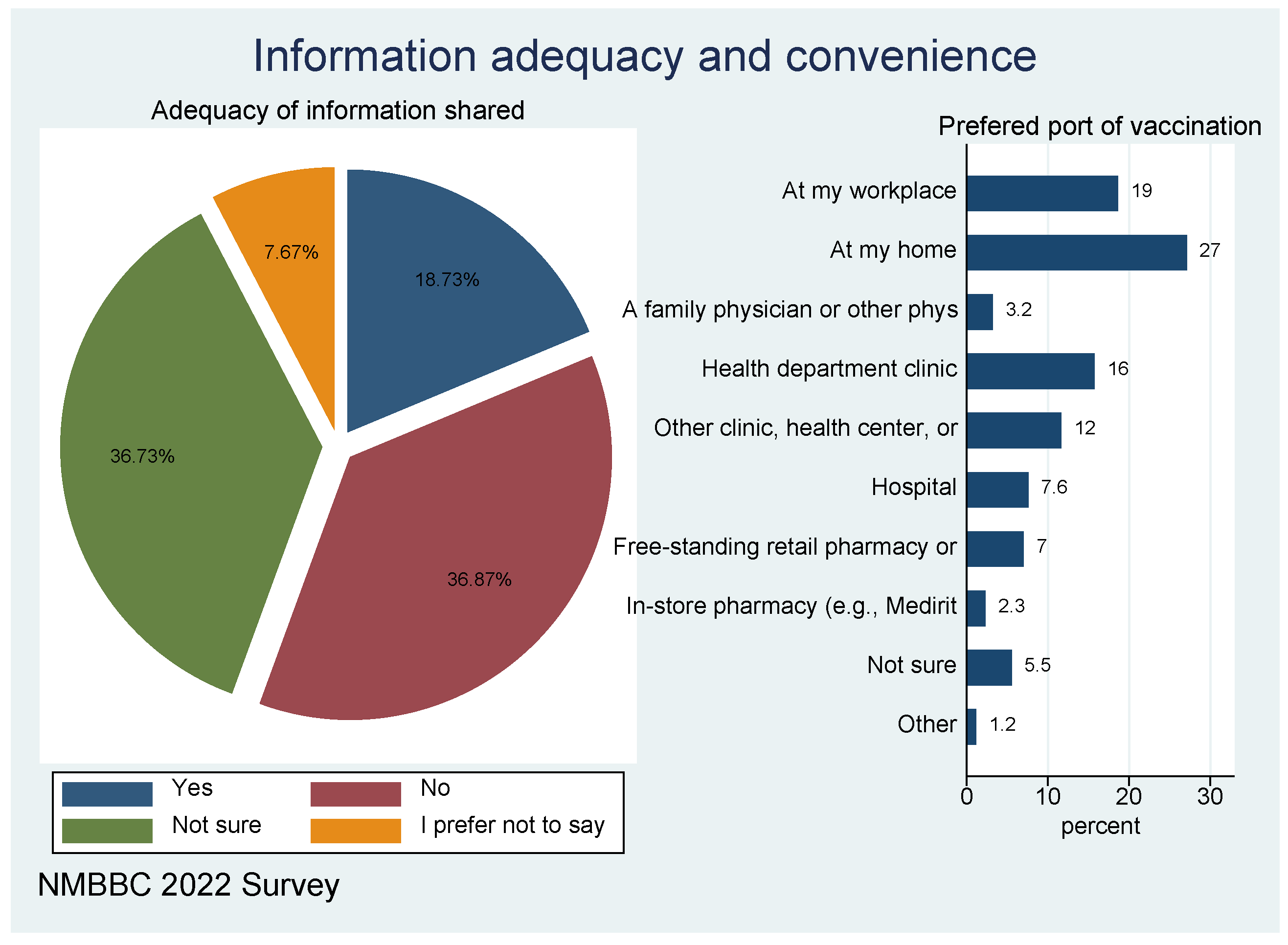
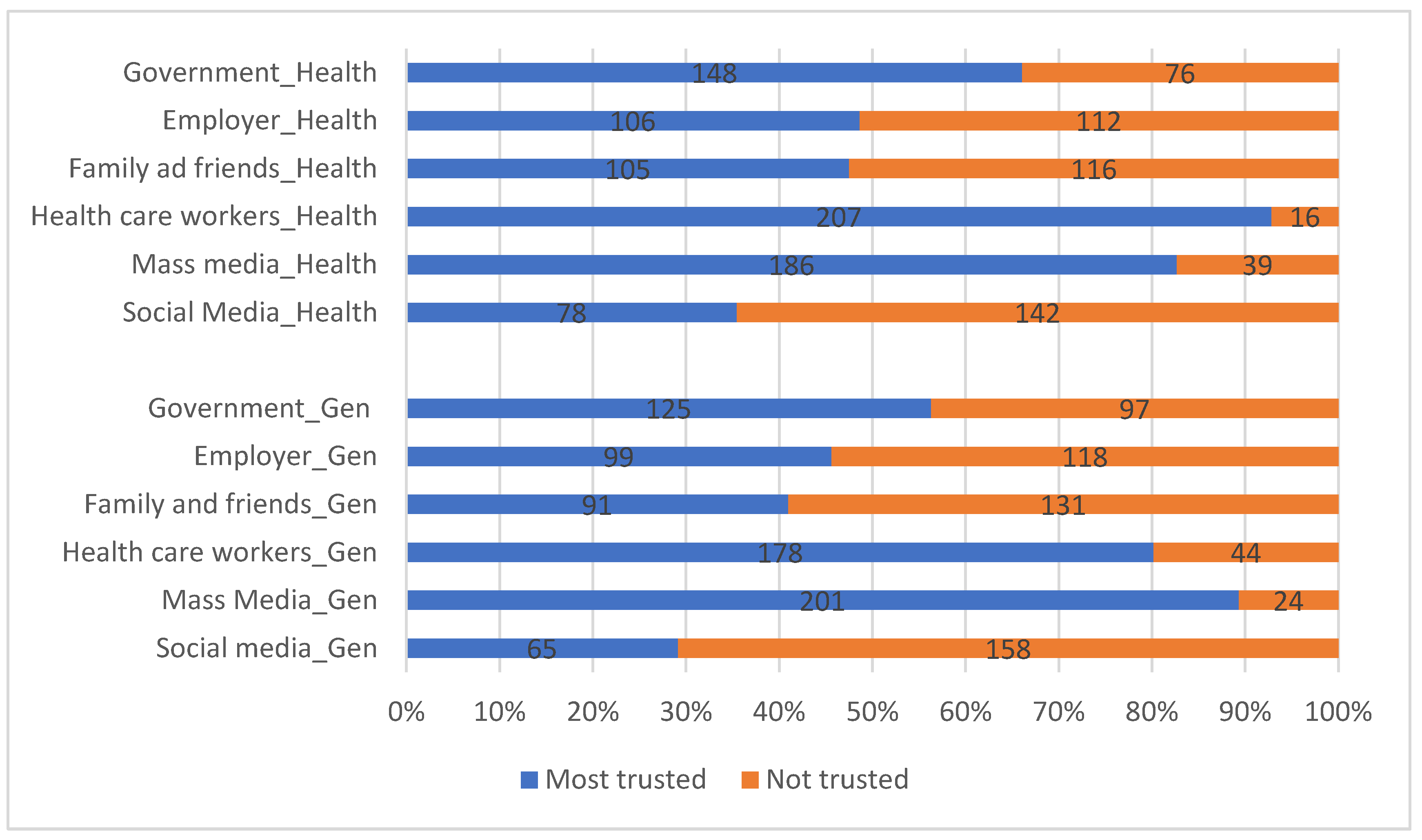
3. Results
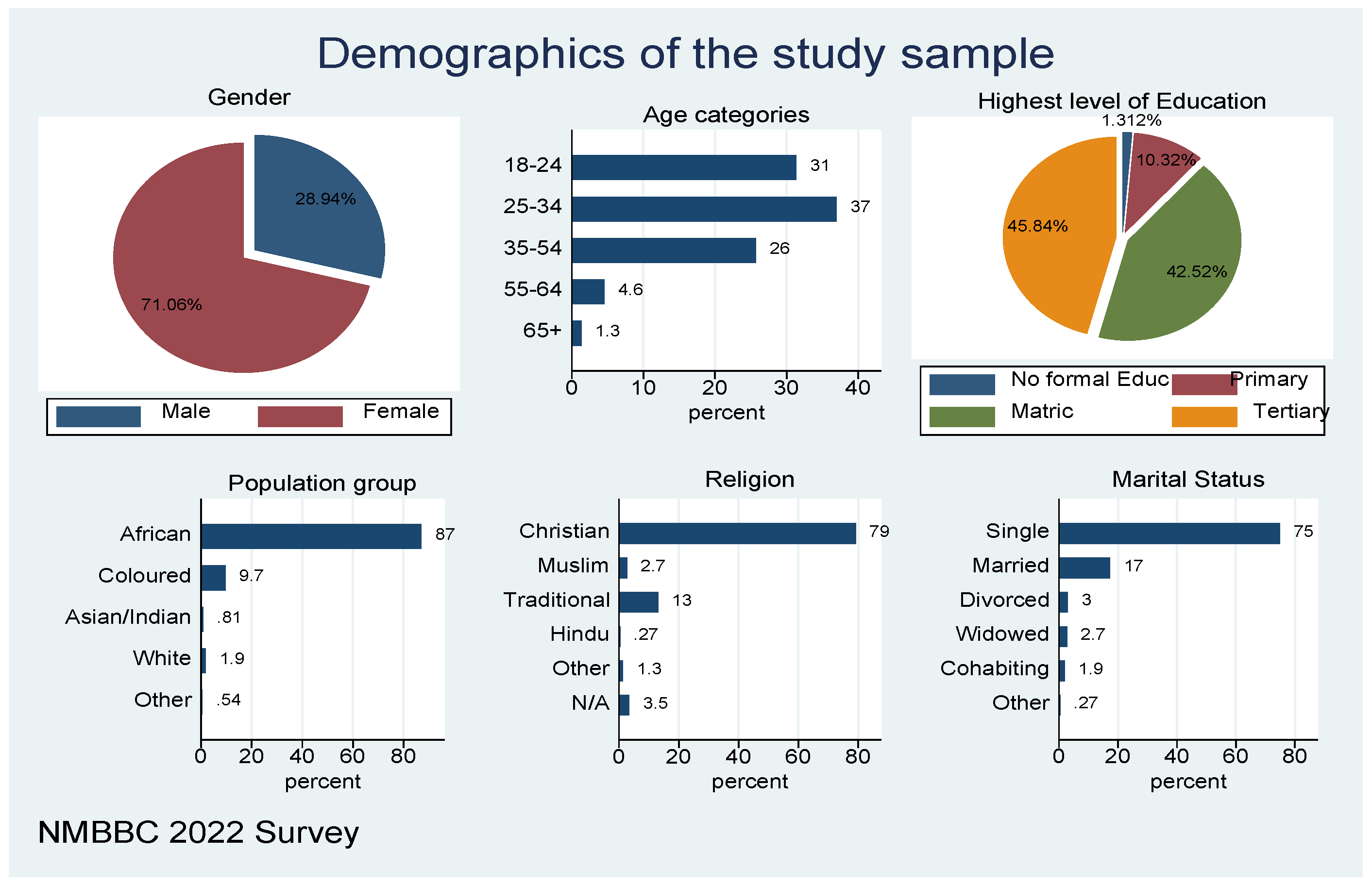
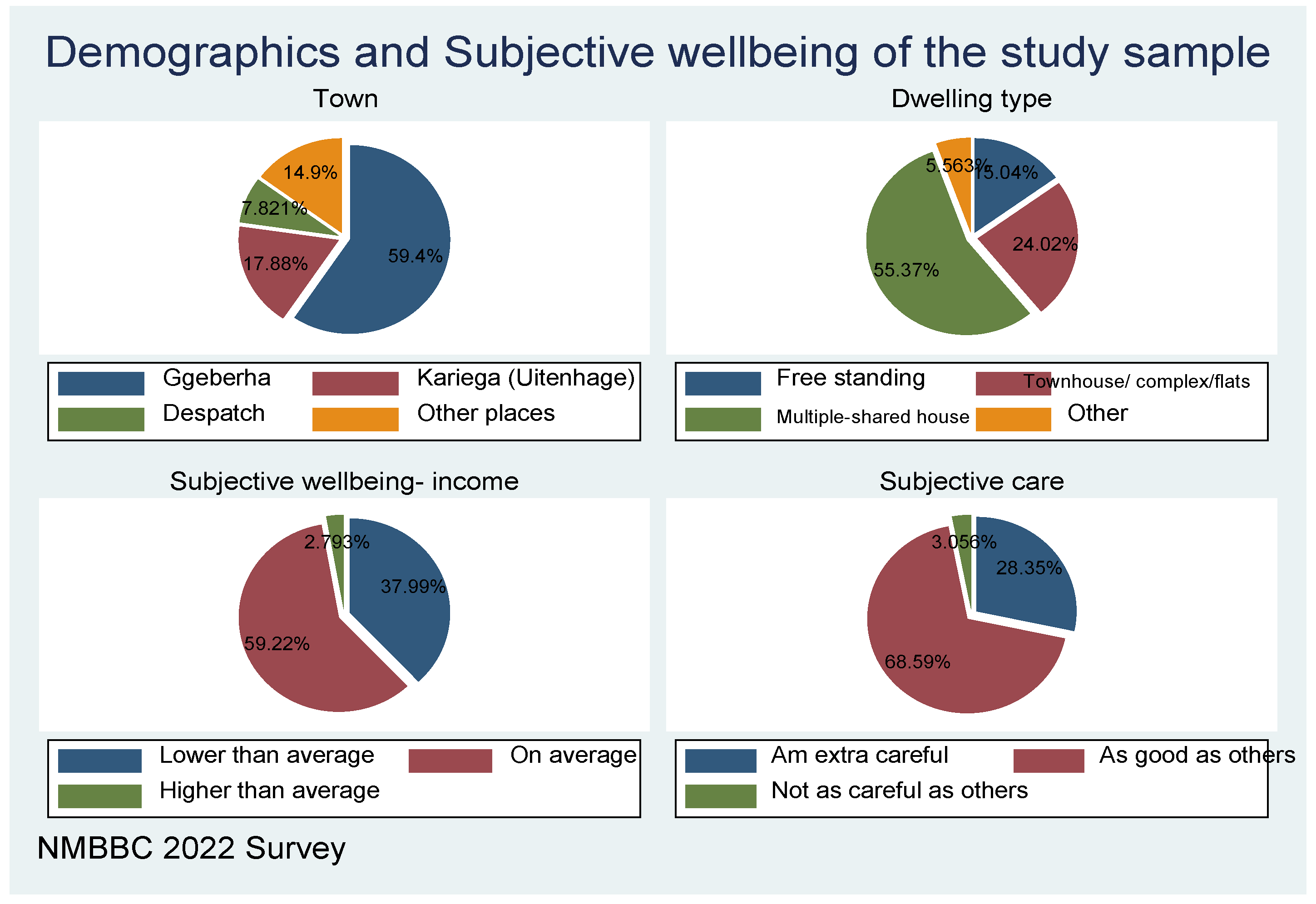
Demographics of the sample
4. Discussions
5. Conclusion and recommendations
6. Limitations
Author Contributions
Funding
Acknowledgement
Conflicts of Interest
References
- G. Anakpo and S. Mishi, “Hesitancy of COVID-19 vaccines: Rapid systematic review of the measurement, predictors, and preventive strategies,” Human Vaccines & Immunotherapeutics, 18(5), p. 2074716, 2022. [CrossRef]
- S. Cooper, H. van Rooyen and C. S. Wiysonge, “COVID-19 vaccine hesitancy in South Africa: how can we maximize uptake of COVID-19 vaccines?,” Expert review of vaccines, vol. 20, no. 8, pp. 921-933., 2021. [CrossRef]
- W. World Health Organization, “Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO Technical Advisory Group on Behavioural Insights and Sciences for Health, Meeting Report, 15 October 2020. 2020.,” 2020.
- S. L. Benoit and R. F. Mauldin, “The “anti-vax” movement: a quantitative report on vaccine beliefs and knowledge across social media,” BMC public health, vol. 2, no. 1, pp. 1-11, 2021. [CrossRef]
- K. Hayawi, S. Shahriar, M. A. Serhani, H. Alashwal and M. M. Masud, “Vaccine versus variants (3Vs): are the COVID-19 vaccines effective against the variants? A systematic review.,” Vaccines, vol. 9, no. 11, p. 1305, 2021. [CrossRef]
- F. Pandolfi, L. Franza, L. Todi, V. Carusi, M. Centrone, A. Buonomo, .. and E. Nucera, “The importance of complying with vaccination protocols in developed countries:“Anti-Vax” hysteria and the spread of severe preventable diseases. Current Me,” 2018.
- S. Mylan and C. Hardman, “COVID-19, cults, and the anti-vax movement,” The Lancet, vol. 397, no. 10280, p. 1181, 2021. [CrossRef]
- A. M. L. Amit, V. C. F. Pepito, L. Sumpaico-Tanchanco and M. M. Dayrit, “COVID-19 vaccine brand hesitancy and other challenges to vaccination in the Philippines,” PLOS Global Public Health, vol. 2, no. 1, p. e0000165., 2022. [CrossRef]
- B. Roberts, N. Bohler-Muller and J. Struwig, “South African Social Attitudes Survey (SASAS) (Round 17) Brief report. Summary findings: Attitudes towards vaccination.,” 2021.
- J. Khubchandani, S. Sharma, J. H. Price, M. J. Wiblishauser, M. Sharma and F. J. Webb, “COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment,” Journal of Community Health, vol. 46, no. 2, p. 270–277, 2021. [CrossRef]
- A. Campo-Arias and J. C. Pedrozo-Pupo, “Attitude towards COVID-19 vaccines in Colombian university students: Frequency and associated variables,” Acta Bio Medica: Atenei Parmensis, vol. 92, no. 6, 2022.
- S. Neumann-Böhme, N. E. Varghese, I. Sabat, P. P. Barros, W. Brouwer, J. van Exel, ... and T. Stargardt, “Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19,” The European Journal of Health Economics, vol. 21, pp. 977-982, 2020. [CrossRef]
- E. Paul, A. Steptoe and D. Fancourt, “Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications,” The Lancet Regional Health-Europe, vol. 100012, p. 1, 2021. [CrossRef]
- C. Runciman, K. Alexander and M. Bekker, “SA survey sheds some light on what lies behind coronavirus vaccine hesitancy. Daily Maverick [Internet].,” 2021.
- J. Khubchandani, S. Sharma, J. H. Price, M. J. Wiblishauser, M. Sharma and F. J. Webb, “COVID-19 vaccination hesitancy in the United States: a rapid national assessment,” Journal of community health, vol. 46, pp. 270-277, 2021. [CrossRef]
- P. D. Katoto, S. Parker, N. Coulson, N. Pillay, S. Cooper, A. Jaca, ... and C. S. Wiysonge, “Predictors of COVID-19 vaccine hesitancy in South African local communities: The VaxScenes Study.,” Vaccines, vol. 10, no. 3, p. 353, 2022. [CrossRef]
- M. R. Biswas, M. S. Alzubaidi, U. Shah, A. A. Abd-Alrazaq and Z. Shah, “A scoping review to find out worldwide COVID-19 vaccine hesitancy and its underlying determinants,” Vaccines, vol. 9, no. 11, p. 1243, 2022. [CrossRef]
- G. Anakpo and S. Mishi, “Business response to COVID-19 impact: Effectiveness analysis in South Africa,” The Southern African Journal of Entrepreneurship and Small Business Management, vol. 13, no. 1, p. 7, 2021. [CrossRef]
- K. Jafta, G. Anakpo and M. Syden, “Income and poverty implications of Covid-19 pandemic and coping strategies: the case of South Africa,” Africagrowth Agenda., vol. 19, no. 3, pp. 4-7, 2022.
- G. Anakpo, Z. Nqwayibana and S. Mishi, “The Impact of Work-from-Home on Employee Performance and Productivity: A Systematic Review,” Sustainability, vol. 15, no. 5, p. 4529, 2023. [CrossRef]
- G. Anakpo, F. Hlungwane and S. Mishi, “The Impact of COVID-19 And Related Policy Measures on The Livelihood Strategies in Rural South Africa,” Africagrowth Agenda, 2023.
- E. Komanisi, G. Anakpo and M. Syden, “Vulnerability to COVID-19 impacts in South Africa: analysis of the socio-economic characteristics.,” Africagrowth Agenda, , vol. 19, no. 2, pp. 10-12, 2022.
- H. Gqoboka, G. Anakpo and S. Mishi, “Challenges Facing ICT Use during COVID-19 Pandemic: The Case of Small, Medium and Micro Enterprises in South Africa,” American Journal of Industrial and Business Management, vol. 12, no. 9, pp. 1395-1401, 2022. [CrossRef]
- S. Mish, N. Tshabalala, G. Anakpo and M. Weliswa, “COVID-19 experiences and Coping strategies: The case of dif-ferently sized businesses in South Africa,” Sustainability, 2023. [CrossRef]
- M. Pivetti, S. Di Battista, F. G. Paleari and E. Hakoköngäs, “Conspiracy beliefs and attitudes toward COVID-19 vaccinations: A conceptual replication study in Finland,” Journal of Pacific Rim Psychology, 15, 18344909211039893, 2021. [CrossRef]
- R. R. Marzo, W. Sami, M. Z. Alam, S. Acharya, K. Jermsittiparsert, K. Songwathana, ... and S. Yi, “Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asia,” Tropical medicine and health, vol. 50, pp. 1-10, 2022. [CrossRef]
| Have you heard about the COVID-19 vaccine | From which of the following towns do you reside? | |||
|---|---|---|---|---|
| Ggeberha | Kariega (Uitenhage) | Despatch | Total | |
| Yes | 277 | 42 | 11 | 330 |
| 84.0 | 12.7 | 3.3 | 100.0 | |
| 97.9 | 93.3 | 84.6 | 96.8 | |
| No | 6 | 3 | 2 | 11 |
| 54.6 | 27.2 | 18.2 | 100.0 | |
| 2.1 | 6.7 | 15.4 | 3.2 | |
| Total | 283 | 45 | 13 | 341 |
| 83 | 13.2 | 3.8 | 100.0 | |
| 100.0 | 100.0 | 100.0 | 100.0 | |
| 1 | Raosoft is a software company that primarily calculates or generates the sample size of a research or survey (Raosoft Inc., 2004).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




