Submitted:
18 May 2023
Posted:
19 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion/Exclusion Criteria
2.3. Triple-Blind Study Design
2.4. Anaesthetic Protocol
2.5. Monitoring
2.6. Data Collection
2.7. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Haemodynamics Parameters
3.3. Adverse Reactions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Baetge, C.L.; Matthews, N.S. Anesthesia and analgesia for geriatric veterinary patients. Vet Clin North Am Small Anim Pract 2012, 42, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J. Anaesthesia for the geriatric dog and cat. Ir Vet J. 2008, 61, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Gaynor, J.; Dunlop, C.; Wagner, A.; Wertz, E.; Golden, A.; Demme, W. Complications and mortality associated with anesthesia in dogs and cats. J Am Anim Hosp Assoc 1999, 35, 13–17. [Google Scholar] [CrossRef]
- Mazzaferro, E.; Wagner, A.E. Hypotension During Anesthesia in Dogs and Cats: Recognition, Causes, and Treatment. Compendium 2005, 23, 728–737. [Google Scholar]
- Redondo, J.I.; Rubio, M.; Soler, G.; Serra, I.; Soler, C.; Gómez-Villamandos, R.J. Normal Values and Incidence of Cardiorespiratory Complications in Dogs During General Anaesthesia. A Review of 1281 Cases. J Vet Medicine Ser 2007, 54, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Hofmeister, E.H.; Keenan, K.; Egger, C.M. Dobutamine-induced bradycardia in a dog. Vet Anaesth Analg 2005, 32, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Tisdale, J.E.; Patel, R.V.; Webb, C.R.; Borzak, S.; Zarowitz, B.J. Proarrhythmic Effects of Intravenous Vasopressors. Ann Pharmacother 1995, 29, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Dyson, D.H.; Sinclair, M.D. Impact of dopamine or dobutamine infusions on cardiovascular variables after rapid blood loss and volume replacement during isoflurane-induced anesthesia in dogs. Am J Vet Res 2006, 67, 1121–1130. [Google Scholar] [CrossRef]
- Meel JCA van Diederen, W. Hemodynamic Profile of the Cardiotonic Agent Pimobendan. J Cardiovasc Pharm 1989, 14, S7. [Google Scholar] [CrossRef]
- Yokota, S.; Takizawa, M.; Katsumura, H.; Shukunobe, K.; Ishiguro, Y.; Kitagawa, H.; Ohara, N. Pharmacological studies of a novel cardiotonic agent, pimobendan (UD-CG 115 BS). Jpn Pharmacol Ther 1992, 20, 1143–1174. [Google Scholar]
- Boswood, A.; Häggström, J.; Gordon, S.G.; Wess, G.; Stepien, R.L.; Oyama, M.A.; Keene, B.W.; Bonagura, J.; MacDonald, K.A.; Patteson, M. Effect of Pimobendan in Dogs with Preclinical Myxomatous Mitral Valve Disease and Cardiomegaly: The EPIC Study—A Randomized Clinical Trial. J Vet Intern Med 2016, 30, 1765–1779. [Google Scholar] [CrossRef] [PubMed]
- Keene, B.W.; Atkins, C.E.; Bonagura, J.D.; Fox, P.R.; Häggström, J.; Fuentes, V.L.; Oyama, M.A.; Rush, J.E.; Stepien, R.; Uechi, M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J Vet Intern Med 2019, 33, 1127–1140. [Google Scholar] [CrossRef] [PubMed]
- Summerfield, N.; Boswood, A.; O’Grady, M.; Gordon, S.; Dukes-McEwan, J.; Oyama, M.; Smith, S.; Patteson, M.; French, A.; Culshaw, G. Efficacy of Pimobendan in the Prevention of Congestive Heart Failure or Sudden Death in Doberman Pinschers with Preclinical Dilated Cardiomyopathy (The PROTECT Study). J Vet Intern Med 2012, 26, 1337–1349. [Google Scholar] [CrossRef] [PubMed]
- Hori, Y.; Taira, H.; Nakajima, Y.; Ishikawa, Y.; Yumoto, Y.; Maekawa, Y.; Oshiro, A. Inotropic effects of a single intravenous recommended dose of pimobendan in healthy dogs. J Vet Medical Sci 2019, 81, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Pichayapaiboon, P.; Tantisuwat, L.; Boonpala, P.; Saengklub, N.; Boonyarattanasoonthorn, T.; Khemawoot, P.; Kijtawornrat, A. Pharmacodynamics and Pharmacokinetics of Injectable Pimobendan and Its Metabolite, O-Desmethyl-Pimobendan, in Healthy Dogs. Frontiers Vet Sci 2021, 8, 656902. [Google Scholar] [CrossRef] [PubMed]
- Ichihara, K.; Abiko, Y. The Effect of Pimobendan on Myocardial Mechanical Function and Metabolism in Dogs: Comparison with Dobutamine. J Pharm Pharmacol 1991, 43, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Goto, Y.; Futaki, S.; Ohgoshi, Y.; Yaku, H.; Kawaguchi, O.; Takasago, T.; Saeki, A.; Taylor, T.W.; Nishioka, T. Mechanoenergetic effects of pimobendan in canine left ventricles. Comparison with dobutamine. Circulation 2018, 86, 1291–1301. [Google Scholar] [CrossRef]
- Pagel, P.S.; Hettrick, D.A.; Warltier, D.C. Influence of levosimendan, pimobendan, and milrinone on the regional distribution of cardiac output in anaesthetized dogs. Brit J Pharmacol 1996, 119, 609–615. [Google Scholar] [CrossRef]
- Canfrán, S.; Cediel, R.; Sández, I.; Caro-Vadillo, A.; de Segura, I.A.G. Evaluation of an oesophageal Doppler device for monitoring cardiac output in anaesthetised healthy normotensive dogs. J Small Anim Pract 2015, 56, 450–455. [Google Scholar] [CrossRef]
- Monnet, X.; Robert, J.M.; Jozwiak, M.; Richard, C.; Teboul, J.L. Assessment of changes in left ventricular systolic function with oesophageal Doppler. Br J Anaesth 2013, 111, 743–749. [Google Scholar] [CrossRef]
- Sohn, S.; Kim, H.S.; Han, J.J. Doppler Flow Velocity Measurement to Assess Changes in Inotropy and Afterload: A Study in Healthy Dogs. Echocardiogr 2002, 19, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Sández, I.; Soto, M.; Torralbo, D.; Rioja, E. Effect of different analgesic techniques on hemodynamic variables recorded with an esophageal Doppler monitor during ovariohysterectomy in dogs. Can Vet J La Revue Veterinaire Can 2018, 59, 419–424. [Google Scholar]
- Sández, I.; Verdier, N.; Redondo, J.I.; Tarragona, L.; Donati, P.A.; Serrano, S.; Otero, P.E. Agreement between transthoracic echocardiography and esophageal Doppler on aortic flow variables in anesthetised mechanically ventilated dogs. Can Vet J. 2022, 63, 722–726. [Google Scholar] [PubMed]
- Anonymous. Real Decreto 53/2013, de 1 de febrero, por el que se establecen las normas básicas aplicables para la protección de los animales utilizados en experimentación y otros fines científicos, incluyendo la docencia 2013. Available online: https://www.boe.es/eli/es/rd/2013/02/01/53 (accessed on 28 June 2022).
- R.Core.Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2022; https://www.R-project.org/. [Google Scholar]
- Mair, P.; Wilcox, R. Robust statistical methods in R using the WRS2 package. Behav Res Methods 2020, 52, 464–488. [Google Scholar] [CrossRef] [PubMed]
- Champely, S. pwr: Basic Functions for Power Analysis. R package Version 1.3-0. 2020. Available online: https://CRAN.R-project.org/package=pwr (accessed on 28 June 2022).
- Enokizono, M.; Mandour, A.S.; Komeda, S.; Goya, S.; Takeuchi, A.; Katoh, K.; Yairo, A.; Yilmaz, Z.; Shimada, K.; Tanaka, R. Hemodynamic effect of pimobendan following intramuscular and intravenous administration in healthy dogs: A pilot study. Front Vet Sci. 2022, 9, 969304. [Google Scholar] [CrossRef] [PubMed]
- Singer, M. Oesophageal Doppler. Curr Opin Crit Care 2009, 15, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Bajorat, J.; Hofmockel, R.; Vagts, D.A.; Janda, M.; Pohl, B.; Beck, C.; NoeldgeSchomburg, G. Comparison of invasive and less-invasive techniques of cardiac output measurement under different haemodynamic conditions in a pig model. Eur J Anaesth 2006, 23, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Blanco, P. Rationale for using the velocity–time integral and the minute distance for assessing the stroke volume and cardiac output in point-of-care settings. Ultrasound J 2020, 12, 21. [Google Scholar] [CrossRef]
- Paranjape, V.V.; Henao-Guerrero, N.; Menciotti, G.; Saksena, S. Esophageal Doppler-derived indices and arterial load variables provide useful hemodynamic information during assessment of fluid responsiveness in anesthetized dogs undergoing acute changes in blood volume. Am J Vet Res. 2023, 84, ajvr.22.11.0198. [Google Scholar] [CrossRef]
- Cattai, A.; Rabozzi, R.; Ferasin, H.; Isola, M.; Franci, P. Haemodynamic changes during propofol induction in dogs: New findings and approach of monitoring. Bmc Vet Res 2018, 14, 282. [Google Scholar] [CrossRef]
- Bonagura, J.D.; Miller, M.W.; Darke, P.G.G. Doppler Echocardiography. I. Pulsed-Wave and Continuous-Wave Examinations. Vet Clin North Am Small Animal Pract 1998, 28, 1325–1359. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Fukushima, R.; Ishikawa, T.; Hamabe, L.; Aytemiz, D.; Huai-Che, H.; Nakao, S.; Machida, N.; Tanaka, R. The Effect of Pimobendan on Left Atrial Pressure in Dogs with Mitral Valve Regurgitation. J Vet Intern Med 2011, 25, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Koshman, Y.E.; Herzberg, B.R.; Seifert, T.R.; Polakowski, J.S.; Mittelstadt, S.W. The evaluation of drug-induced changes in left ventricular function in pentobarbital-anesthetized dogs. J Pharmacol Toxicol 2018, 91, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Kochie, S.L.; Schober, K.E.; Rhinehart, J.; Winter, R.L.; Bonagura, J.D.; Showers, A.; Yildez, V. Effects of pimobendan on left atrial transport function in cats. J Vet Intern Med 2021, 35, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Joho, S.; Asanoi, H.; Ishizaka, S.; Kameyama, T.; Inoue, H. Disparate force-frequency effects of pimobendan and dobutamine in conscious dogs with tachycardia-induced cardiomyopathy. J Card Fail 2002, 8, 423–430. [Google Scholar] [CrossRef]
- Saeian, K.; Wann, L.S.; Sagar, K.B. Doppler Echocardiographic Evaluation of Left Ventricular Function. Echocardiogr 1990, 7, 21–25. [Google Scholar] [CrossRef]
- Perez, J.E.T.; Ortiz-Urbina, J.; Heredia, C.P.; Pham, T.T.; Madala, S.; Hartley, C.J.; Entman, M.L.; Taffet, G.E.; Reddy, A.K. Aortic acceleration as a noninvasive index of left ventricular contractility in the mouse. Sci Rep-uk 2021, 11, 536. [Google Scholar] [CrossRef]
- Sagar, K.B.; Wann, L.S.; Boerboom, L.E.; Kalbfleisch, J.; Rhyne, T.L.; Olinger, G.N. Comparison of Peak and Modal Aortic Blood Flow Velocities With Invasive Measures of Left Ventricular Performance. J Am Soc Echocardiog 1988, 1, 194–200. [Google Scholar] [CrossRef]
| PLACEBO (N=15) |
PIMOBENDAN (N=18) |
Overall (N=33) |
p-value | |
|---|---|---|---|---|
| AGE | 9.00 [7.00, 12.0] | 9.00 [7.00, 12.0] | 9.00 [7.00, 12.0] | 0.2 |
| WEIGHT | 9.50 [5.00, 25.0] | 11.5 [5.00, 25.0] | 11.0 [5.00, 25.0] | 0.8 |
| ASA | ||||
| 1 | 5 (33.3%) | 2 (11.1%) | 7 (21.2%) | 0.12 |
| 2 | 10 (66.7%) | 16 (88.9%) | 26 (78.8%) |
|
VARIABLE (units)(units) |
GROUP | TIME | p-value | |||
| T0 | T1 | T2 | T3 | |||
| HR (bpm) | PLACEBO | 74 [49, 138] | 72 [48, 132] | 72. [50, 133] | 63 [51, 128] | p=0.12 |
| PIMOBENDAN |
86 [45, 102] | 82 [43, 99] | 78 [48, 110] | 77 [48, 110] | ||
| MAP (mmHg) | PLACEBO | 86 [65, 138] | 90 [64, 133] | 88 [65, 141] | 80 [59, 137] | p=0.19 |
| PIMOBENDAN |
83 [65, 156] | 83 [60, 151] | 80 [62, 143] | 80 [74, 94] | ||
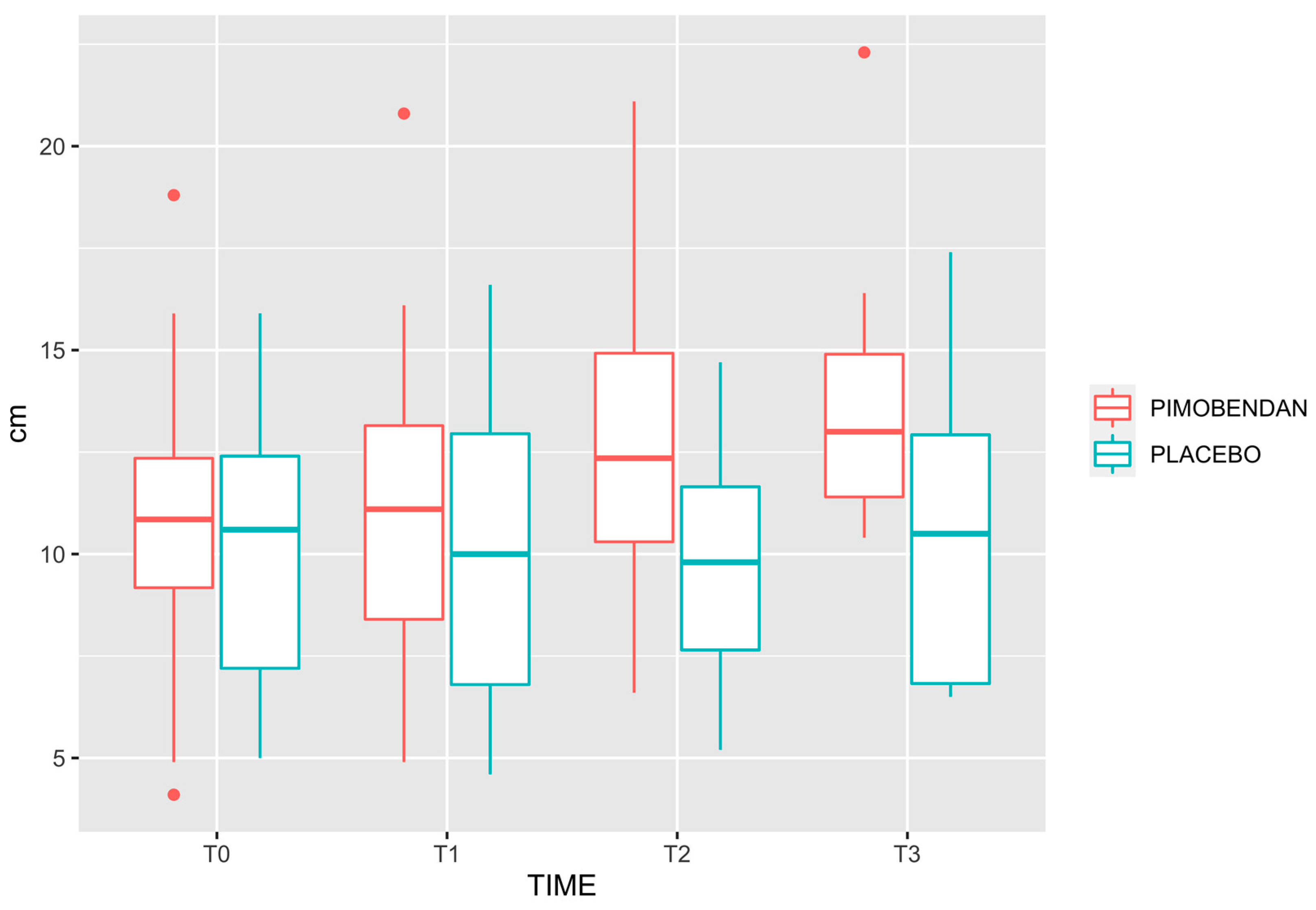
| VTI (cm) | PLACEBO | 10.6 [5.00, 15.9] | 10.0 [4.60, 16.6] | 9.80 [5.20, 14.7] | 10.5 [6.50, 17.4] | p=0.019 |
| PIMOBENDAN |
10.9 [4.10, 18.8] | 11.1 [4.90, 20.8] | 12.4 [6.60, 21.1] | 13.0 [10.4, 22.3] | ||
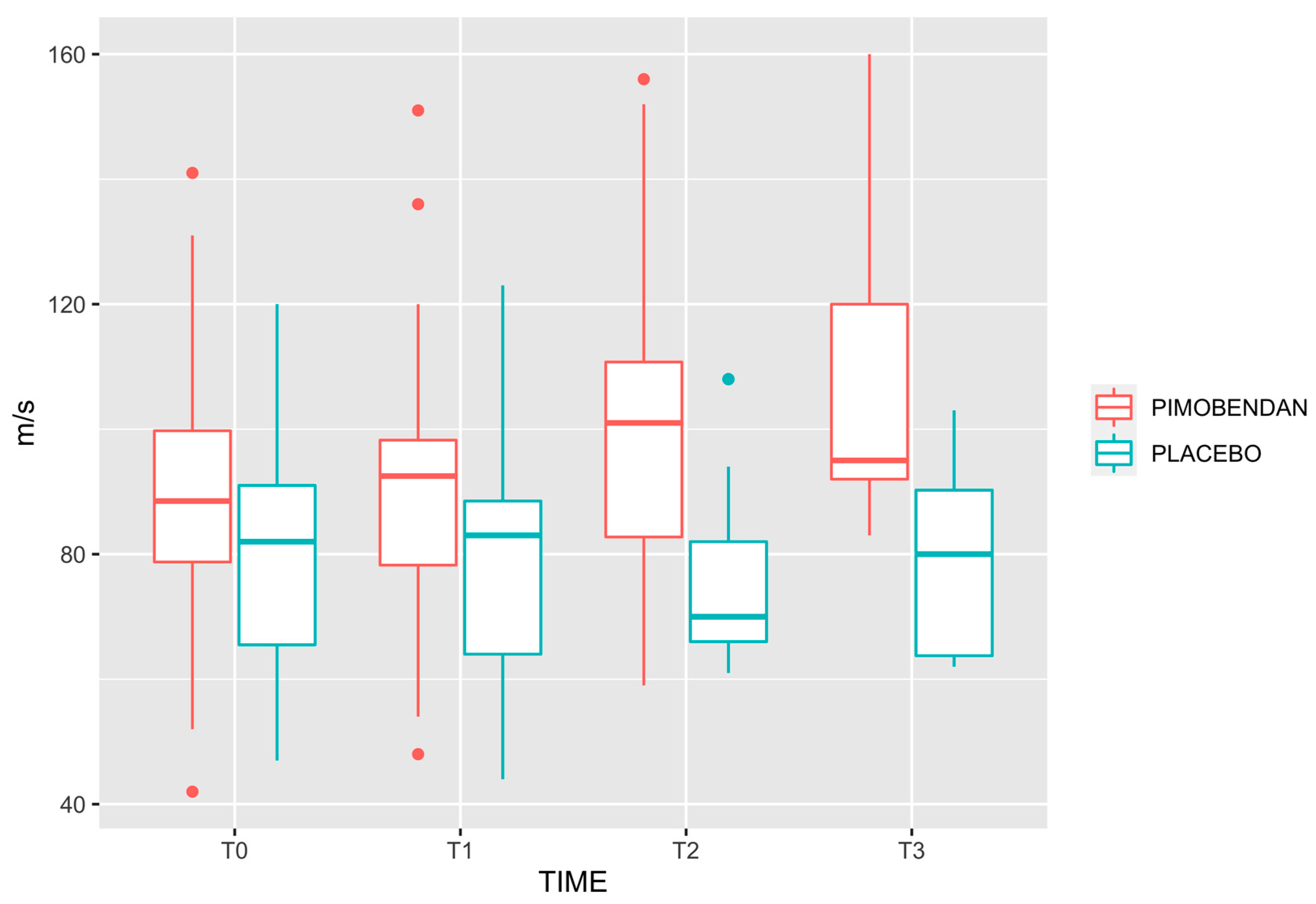
| PV (cm seg-1) | PLACEBO | 82 [47, 120] | 83 [44, 123] | 70 [61, 108] | 80 [62, 103] | p<0.0001 |
| PIMOBENDAN |
88 [42, 141] | 92 [48, 151] | 101 [59, 156] | 95 [83, 160] | ||
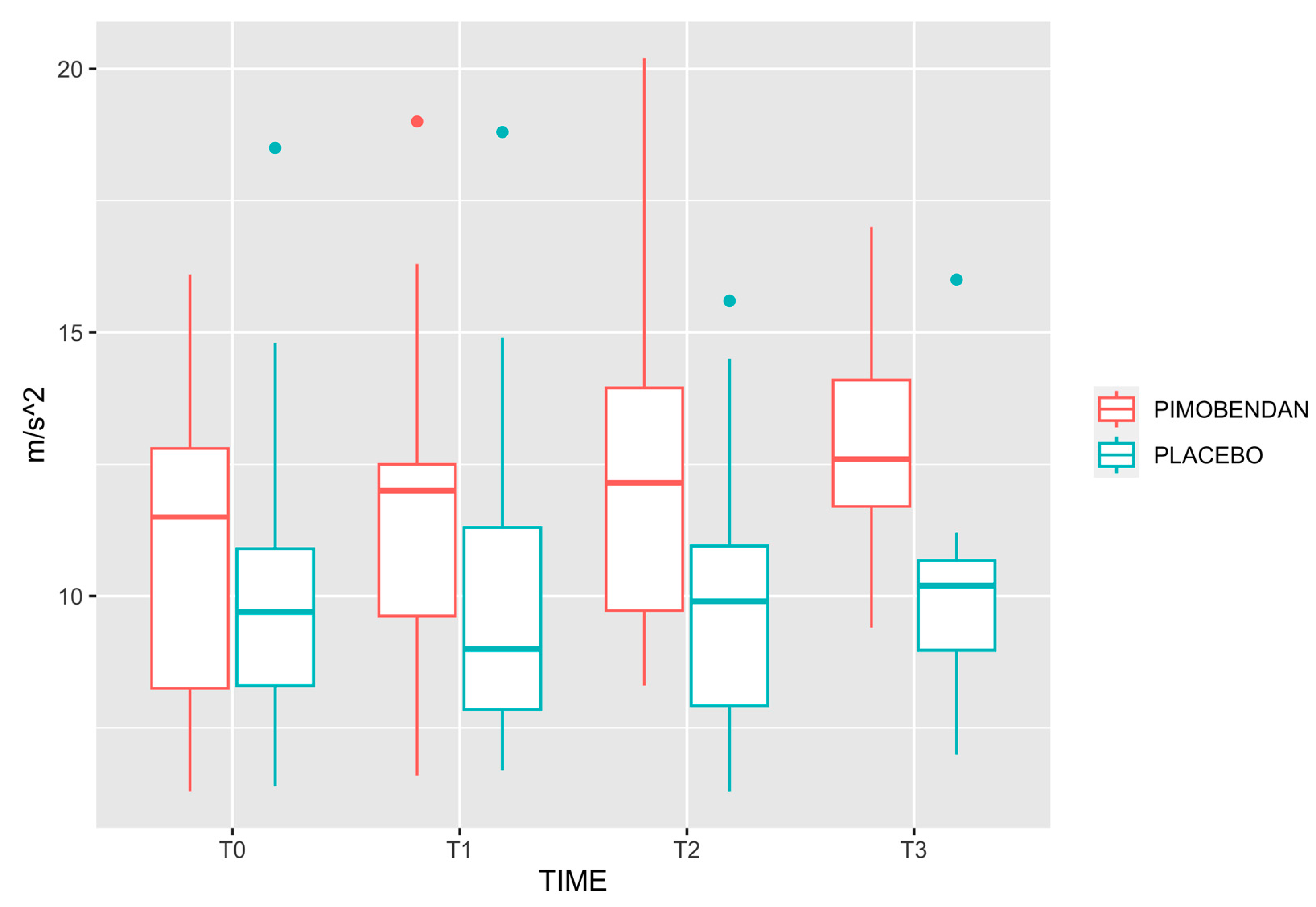
| MA (cm seg-2) | PLACEBO | 9.7 [6.4, 18.5] | 9.0 [6.7, 18.8] | 9.9 [6.3, 15.6] | 10.2 [7.0, 16.0] | p<0.0001 |
| PIMOBENDAN |
11.5 [6.3, 16.1] | 12.0 [6.6, 19.0] | 12.2 [8.3, 20.2] | 12.6 [9.4, 17.0] | ||
| MD (cm) | PLACEBO | 774 [285, 1150] | 792 [253, 1090] | 778 [286, 1120] | 831 [332, 1010] | p=0.65 |
| PIMOBENDAN |
823 [362, 1790] | 785 [357, 2000] | 969 [461, 1770] | 1030 [499, 1870] | ||
| PE´CO2 (mmHg) | PLACEBO | 39 [35, 41] | 39 [35, 44] | 39 [36, 43] | 40 [36, 42] | p=0.23 |
| PIMOBENDAN |
40 [35, 41] | 40 [35, 42] | 40 [35, 43] | 40 [35, 41] | ||
| FeISO (%) | PLACEBO | 1.1 [1.0, 1.4] | 1.1 [0.9, 1.4] | 1.1 [0.9, 1.8] | 1.1 [0.9, 1.4] | p=0.08 |
| PIMOBENDAN |
1.1 [0.7, 1.4] | 1.0 [0.7, 1.4] | 1.1 [0.7, 1.4] | 1.1 [1.0, 1.2] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





