1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a newly discovered illness caused by a virus, which belongs to the family of Coronaviridae [
1,
2]. It is a form of respiratory and systemic zoonosis that originated in Wuhan (China) and spread rapidly worldwide. The World Health Organization declared the coronavirus 2019 (COVID-19) a pandemic in May 2020 [
3] and as of 14
th February 2023, the global burden of disease was over 756 million cases with over 6.8 million deaths [
4].
The nature and mode of transmission of the disease drew the attention of the global scientific community to developing safe and effective vaccines against the virus, which is considered the appropriate means to curb disease spread and ensure the resumption of ordinary life. The COVID-19 vaccine types presently authorized were shown in trials to be highly effective in preventing the disease among adults, with an efficacy of 76.7% for the Ad26.COV2. S (Johnson & Johnson–Janssen, Beerse, Belgium) vaccine [
5]; an efficacy of 94.1% for the mRNA-1273 (Moderna, Cambridge, MA, USA) vaccine [
6] an efficacy of 95% for the BNT162b2 (Pfizer–BioNTech, Manhattan, NY, USA) vaccine [
7] and efficacy of 74-79% for AZD1222 (Oxford-AstraZeneca) COVID vaccine [
8,
9].
Globally, Health Authorities have endorsed herd community as a potential tool against the COVID -19 pandemic. As part of the worldwide strategy, efforts have been made to distribute vaccines with the help of the COVAX program backed by the World Health Organization (WHO) and other multilateral bodies. As of 14
th February 2023, a total of approximately 13.2 billion COVID-19 vaccine doses have been administered globally. In Africa, about 857.6 million vaccine doses have been administered with 45.6% of the population fully vaccinated (African CDC COVID-19 dashboard, 2023) and currently in Ghana, almost 22.4 million COVID-19 vaccines have been administered among the eligible population and with about 40% fully vaccinated [
10]
Despite these innovative scientific discoveries and vaccination campaigns against COVID-19 infection, skepticism, hesitancy, and a negative perception of the efficacy of vaccines are obstacles to halting the outbreak [
11]. Ghana continues to battle misinformation due to various cultural, religious and conspiracy theory on its effects on blacks which remains a constant challenge in ensuring public trust in vaccines [
12].
The reluctance to get vaccinated against COVID-19 poses a significant threat to the efforts to curb the infection. This becomes more alarming when the hesitancy is among the high-risk populace such as healthcare workers, which directly comes into contact with infected COVID-19 patients [
13,
14]. Studies have reported the unwillingness of healthcare workers to receive the COVID-19 vaccine. Studies conducted in Ghana on acceptance of the vaccine by healthcare workers indicated that 39.3% and 48% of the participants were willing to accept the vaccine. The low rate of acceptance may translate into the acceptance by the population since most of these groups rely on healthcare workers for credible medical information [
12,
15].
Vaccine hesitancy, which encompasses reluctance, delay, or refusal to receive a vaccine despite availability, has been a significant threat to the effectiveness of vaccination programs [
16,
17]. Against this backdrop, this study seeks to assess the prevalence and predictors of COVID-19 vaccine hesitancy among healthcare workers in infectious disease centres in Ghana, who serve as primary source of health information for the public and can influence the general public’s decision on uptake of the COVID-19 vaccine.
2. Materials and Methods
2.1. Study Setting
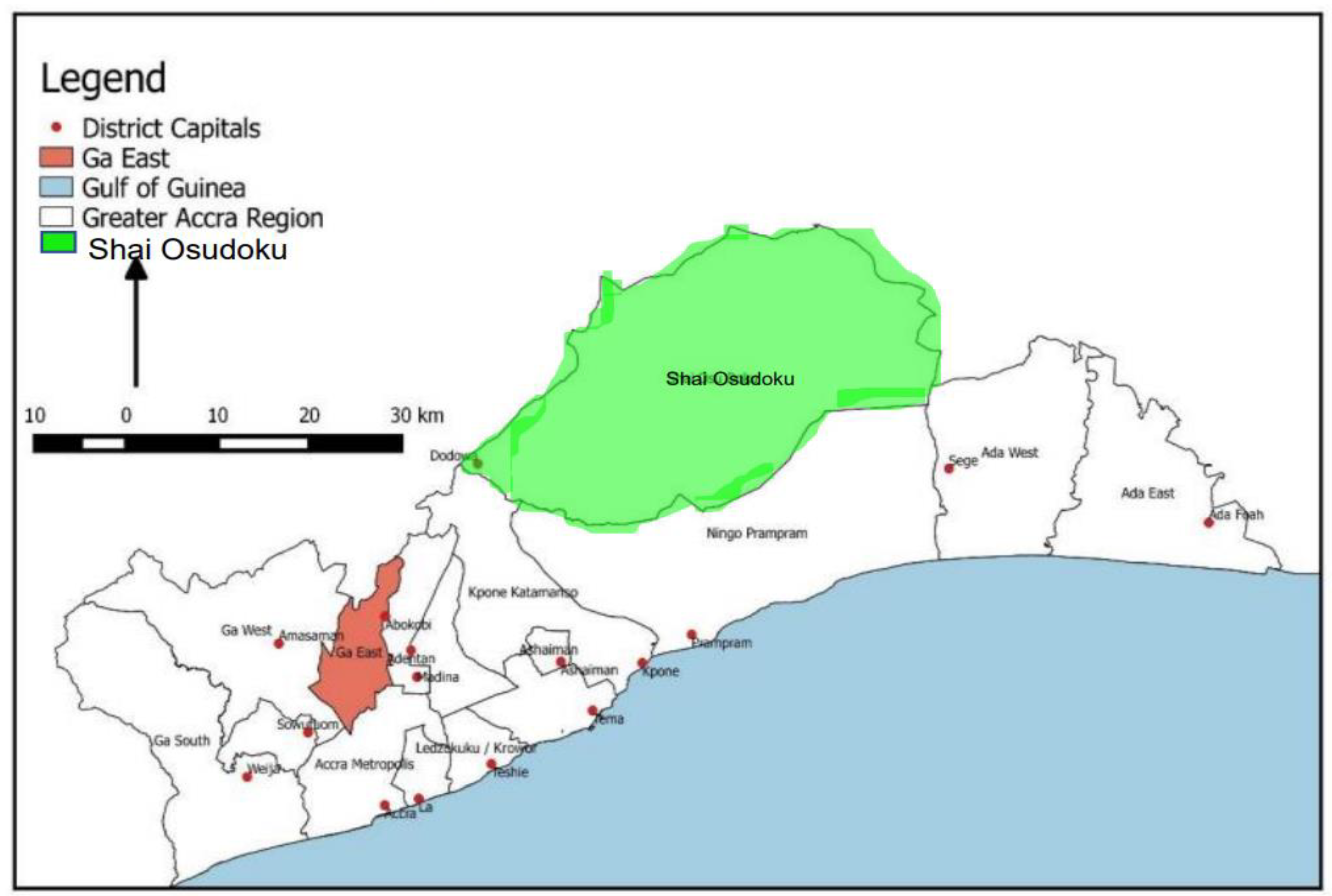
The study was conducted in four infectious disease institutions located in Accra, the capital city of Ghana. Accra is a major urban setting with a population of over 5 million people and has undergone significant development and growth in recent years. It is known as the city with high COVID-19 Infection rate.
The four infectious disease centers included in the study were the Ghana Infectious Disease Centre, Pantang COVID-19/Infectious Disease Treatment and Isolation Centre, Ga East Municipal Hospital, and Shai Osudoku Municipal Hospital. The Ghana Infectious Disease Centre is the first infectious disease facility in Ghana and serves as a referral facility for severe and critical COVID-19 cases. It also has a BLS 3 molecular laboratory for testing infectious pathogens, including COVID-19 .
The Pantang COVID-19/Infectious Disease Treatment and Isolation Centre was established during the pandemic and was used to admit travelers who tested positive for COVID-19 at the Kotoka International Airport.
The Ga East Municipal Hospital was the first COVID-19 treatment center in Ghana before the establishment of the Ghana Infectious Disease Centre. The Shai Osudoku District Hospital is the only major government health facility with an infectious disease center in the district, with a 125-bed capacity.
Figure 1.
Ga East and Shai-Osudoku Municipalities in Regional Context depicting the Study Area.
Figure 1.
Ga East and Shai-Osudoku Municipalities in Regional Context depicting the Study Area.
2.2. Study Design and Sample Size
The study was an institution-based cross-sectional study, which employed a structured questionnaire to assess the prevalence and predictors of COVID-19 vaccine hesitancy among health care workers in infectious disease centres in Ghana. 170 healthcare workers at infectious disease treatment centers in Ghana were recruited in the study. Cochrane formula was used to determine the sample size. Using prevalence (12.2%) of COVID-19 vaccine hesitancy among healthcare workers in a previous study [
18]. The Study formular is given by
N = Z2 P(1-P)
d2
where:
N= sample size, Z= statistic for level of confidence, P= expected prevalence e= margin of error,
Z at a 95% confidence interval = 1.96
Margin of error e= 5% (0.05)
N = (1.96)2 0.122(1-0.122) = 164.59 approximately 165
(0.05)2
Thus, 165 participants were calculated to be sampled for this study. However, a response rate of 170 respondents was attained due to concurrent data collection.
2.3. Data Collection and Sampling Process
A Multistage sampling technique was employed to sample the healthcare workers (HCWs) from the four various Infectious Centers. The participants were stratified into clinical and non-clinical staffs who worked at the Ghana Infectious Disease Centre, Ga East Municipal Hospital, Pantang COVID-19/Infectious Diseases Treatment and Isolation Centre and Shai Osudoku Infectious Disease Isolation Center. Using the employment database from each infection center as a sample frame, a proportionate simple random sampling method was then used to select eligible participants after they consented to be included in the study. The structured questionnaire was then administered to the participant at the various selected hospitals. The questionnaire was in various sections, including information on sociodemographic and health-related information, personal history and experience with COVID-19, routine vaccination history, general attitudes towards vaccination and perception about COVID-19 severity and vaccine safety.
2.4. Data Analysis
After data collection, entry and collation, the data was exported to STATA version 17 for analysis. Descriptive statistics such as mean, standard deviation, frequencies and proportions were used to summarize continuous and categorical variables. Vaccine hesitancy as a variance was measured on the basis of not taking at least one dose of any of the COVID-19 approved vaccines in the country. Health workers who took at least a dose of vaccine were categorized as not vaccine hesitant) and those who did not take any dose of COVID-19 vaccines and with no intention of taking it were classified as vaccine hesitant.
Multivariate logistic regression was used to determine correlates of COVID-19 vaccine hesitancy among the participants. Based on this, a dichotomous variable was created “0” (Not vaccine hesitant) and “1” (vaccine hesitant) using a variable which reported on whether had taken at least one dose of any COVID-19 vaccine in Ghana. The outcome of interest was vaccine hesitancy. The strengths of association between independent variables and COVID-19 vaccine hesitancy were determined using crude odds ratio. Multilinear collinearity was used to address issues relating to confounders. The likelihood ratio test was used to test for the goodness of fit of Model II. A p-value less than 0.05 was considered statistically significant.
2.5. Ethical Considerations
The study obtained ethical clearance from the Ghana Health Services Ethics Review Committee, and written informed consent was obtained from all participants. Participants were informed that participation was voluntary and they could opt out at any time. Data collected was kept confidential, and participants were identified using codes and numbers instead of their actual names to ensure anonymity
3. Results
3.1. Sociodemographic Characteristics of Respondents
One hundred and seventy health workers were recruited for this study (
Table 1). More than half 104 (61.2%) were female. Exactly half 85 (50%) of the health workers were aged 30-39 years and few 9 (5.3%) were between 40-49 years. Regarding marital status, most 105 (61.8%) were single and almost all 169 (99.4%) were Ghanaian. Christianity was the dominant religion 148 (87.0%). The health workers in this study had varying levels of education ranging from basic education 6 (3.5%), certificate/diploma 28 (16.5%) to bachelor’s degree 107 (62.9%) with some having postgraduate qualifications 16 (9.4%). Respondents were sampled from four workplaces, Ghana Infectious Disease Centre 69 (40.6%), Shai Osudoku Isolation center 43 (25.3%), Ga East Municipal Hospital 42 (24.7%) and the Pantang Infectious Disease Centre 16 (9.4%). Majority of the health facilities were located in urban settings 124 (72.9%). A greater proportion 135 (79.4%) were in the clinical care cadre (Anesthesia, Nurses, physicians, Laboratory, Pharmacy and Radiology) while the remaining 35 (20.6%) formed part of administration, estate and security personnel. More 107(62.9%) had been working for less than five years and few have been working for more than ten years 11(6.5%). Majority 146 (85.9%) indicated they did not have any comorbidity.
α (Anesthesia, OPD, Ward, ICU, HDU, Laboratory, Pharmacy, Radiology); β(Administration, Estate, Records, Security); δ(Hypertension, Diabetes, Asthma, Sickle cell, Autoimmune disease).
3.2. Experiences and Perception about COVID-19 Severity and COVID-19 Vaccine Safety
In this study, 131 (77.1%) of the respondents reported being involved in direct care for COVID-19 patients. 88 (51.8%) of participants reported having been infected with COVID-19, and 10 out of 88 (11.4%) were admitted to hospital. 163 (95.9%) of the health workers perceived COVID-19 as a serious disease and 167 (98.2%) knew that it could result in serious complications. Additionally, 161 (94.7%) believed that health workers were more vulnerable to COVID-19 infection, and 155 (91.2%) reported that COVID-19 vaccines had side effects. Finally, 79 (46.5%) agreed that COVID-19 vaccines could prevent infection. Regarding self-perceived risk, 60 (35.3%) agreed they were at highly at risk of getting severe form of the disease and 11 (6.5%) strongly disagreed they were at risk as shown in
Table 2 below.
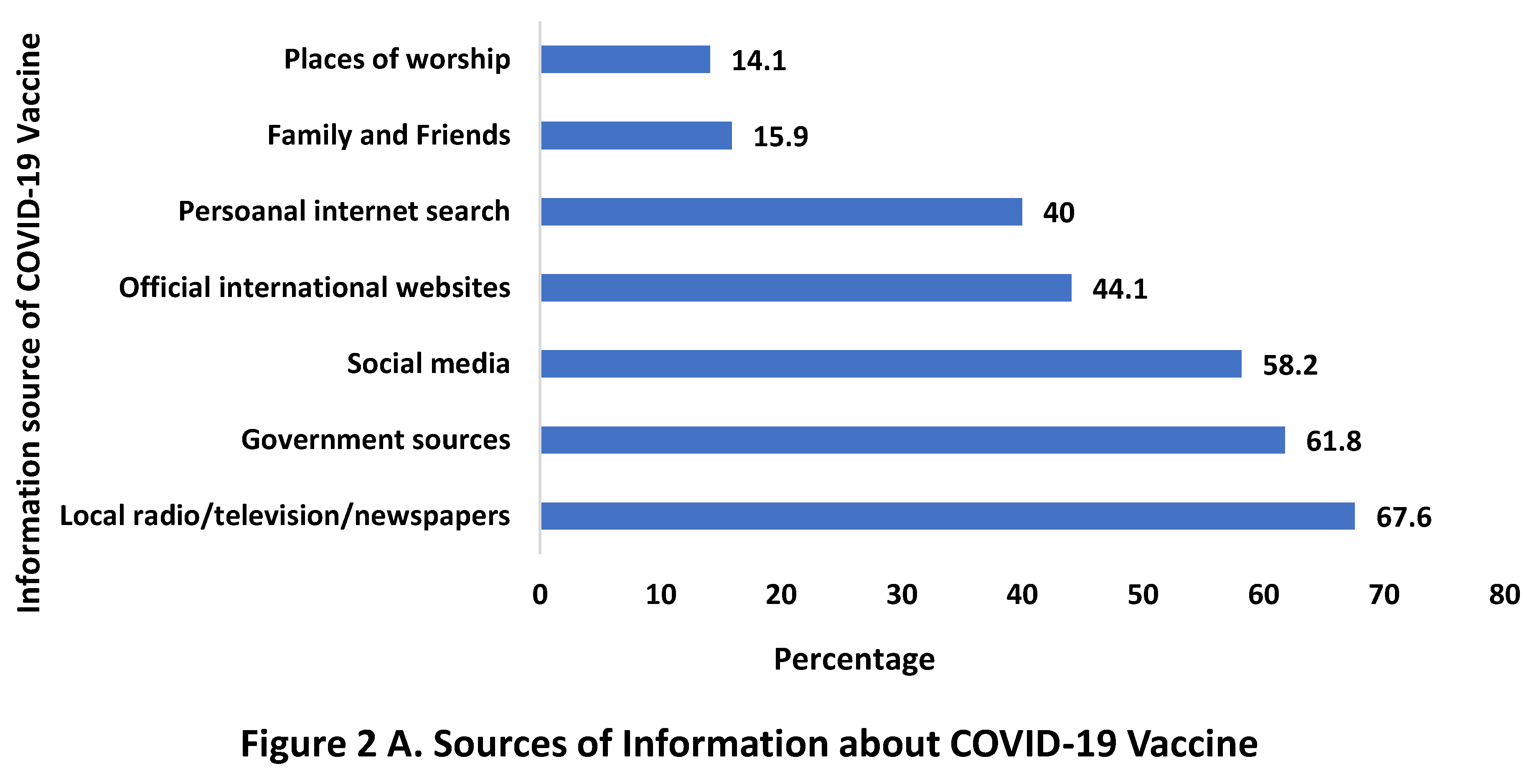
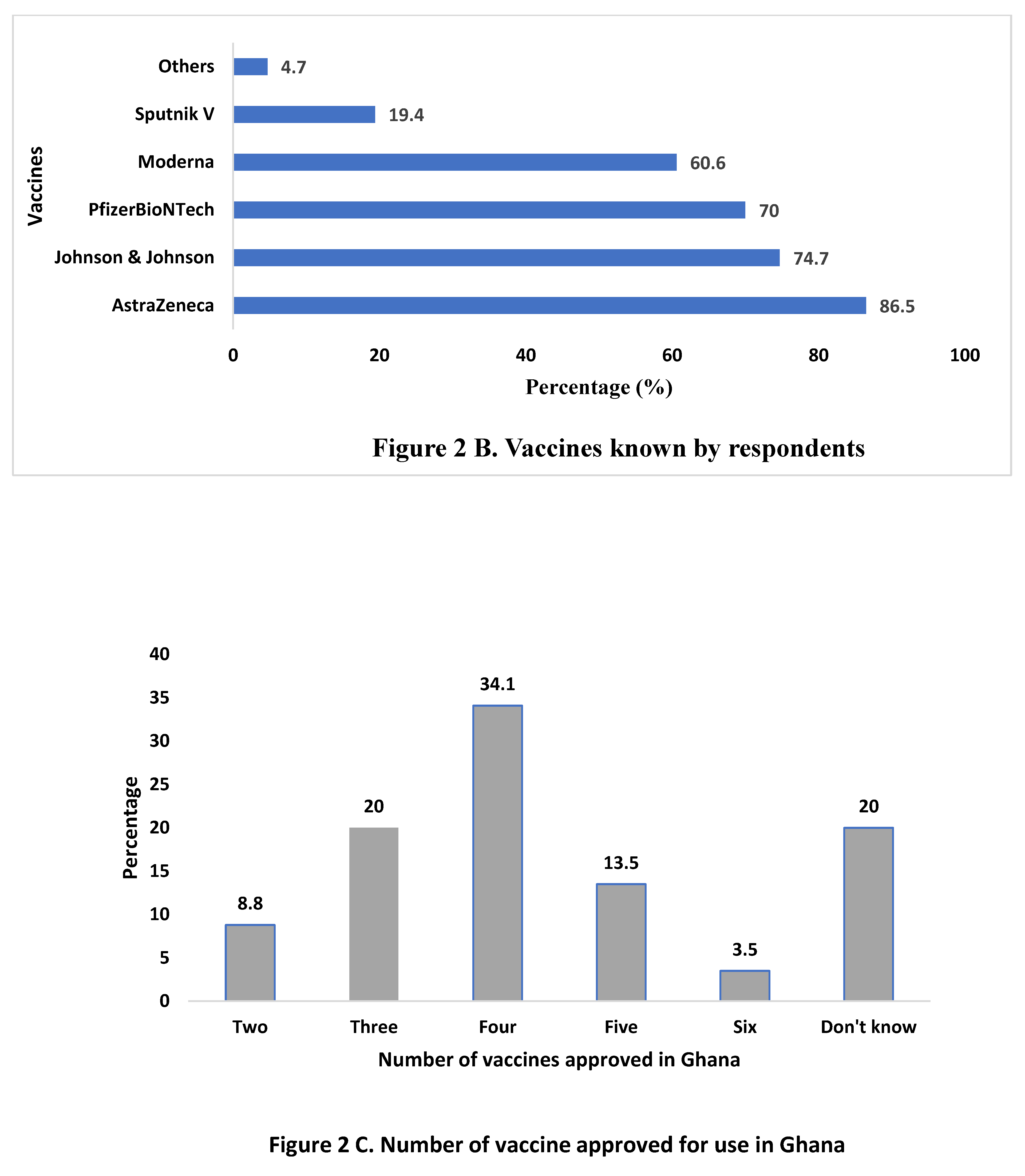
3.3. Vaccine Related Characteristics of Respondents
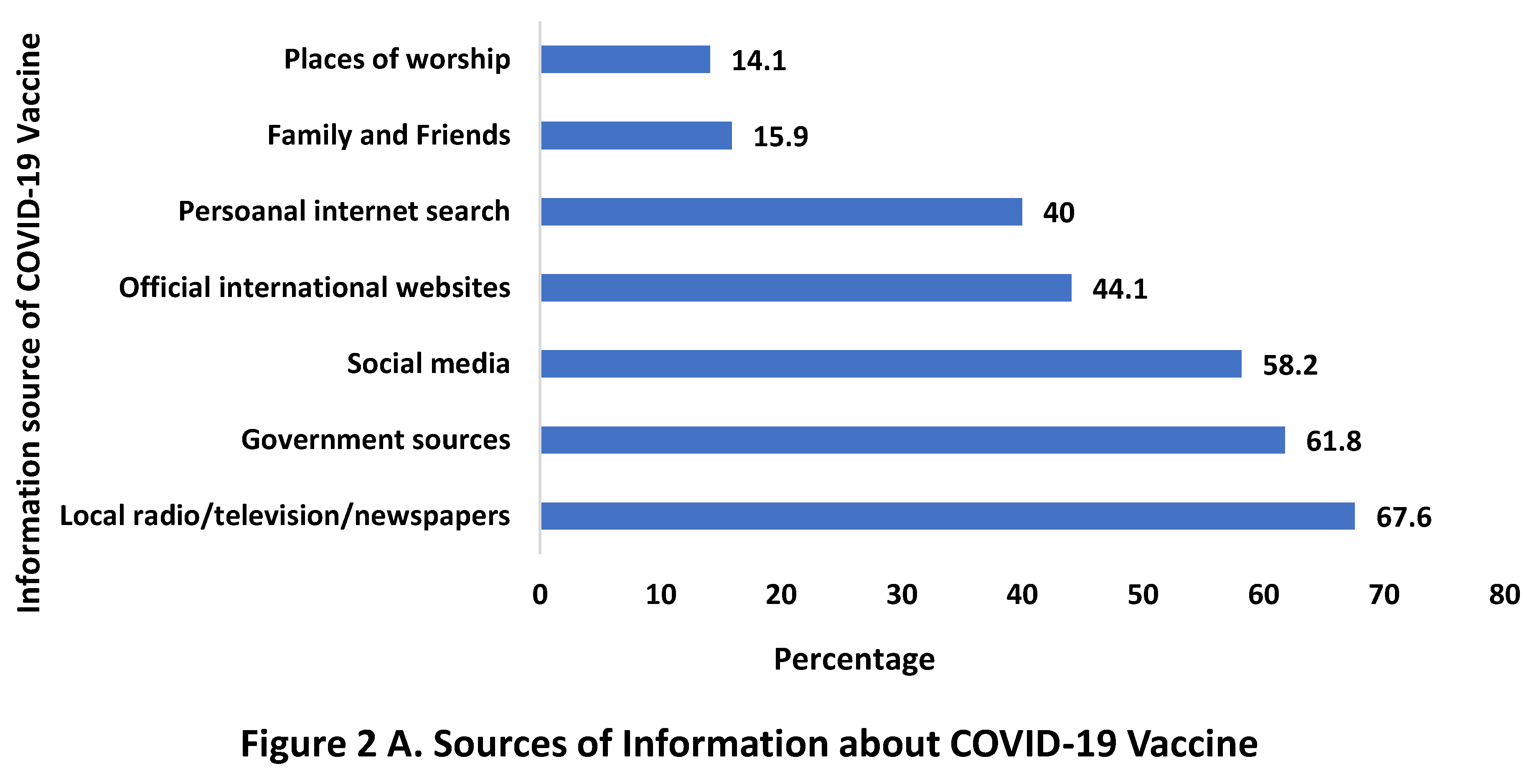
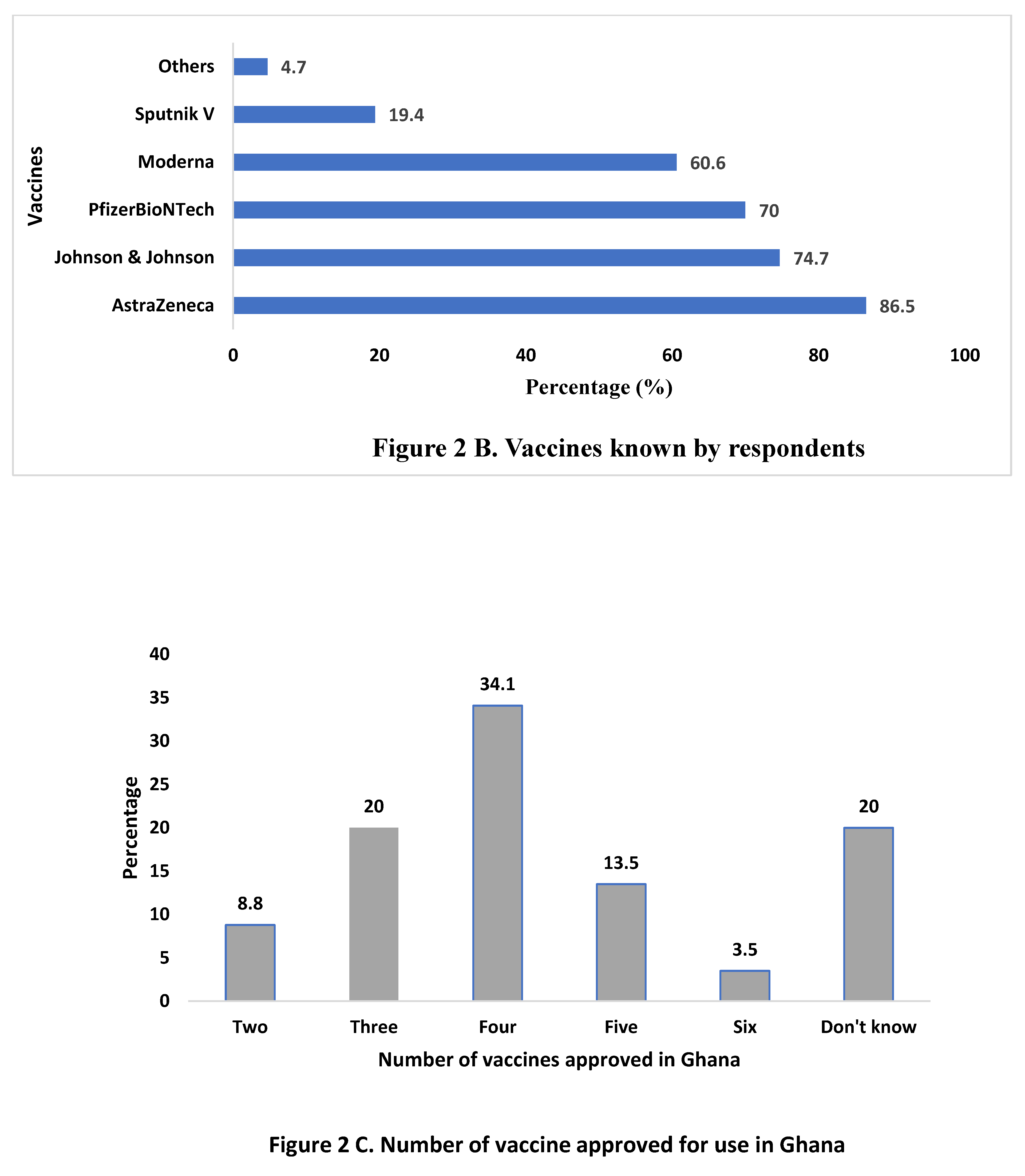
Figure 2 depicts the COVID-19 vaccine related characteristics. Figure 2 A, shows the various sources of information on COVID-19 vaccine among the health care workers. The most common sources of information about the vaccine were local media 115 (67.6%), government sources 105 (61.8%), social media 99 (58.2%) and official international websites 75 (44.1%). Other sources included places of worship 24 (14.1%) and personal internet search 68 (40.0%). In
Figure 1B, most respondent 147 (86.5%) and 127 (74.7%), indicated that AstraZeneca and Johnson and Johnson were the most known vaccine brand, and Sputnik V 33 (19.4%) was the least known vaccine brand. Health workers in this study reported on the number of approved vaccines in Ghana. 58 (34.1%) stated four vaccines were approved for use in Ghana, 34 (20.0%) indicated three and did not know the number of approved vaccines for use in the country and 15 (8.8%) revealed two vaccines were approved for use in Ghana (Figure 2C).
3.4. Attitudes towards COVID-19 Vaccines
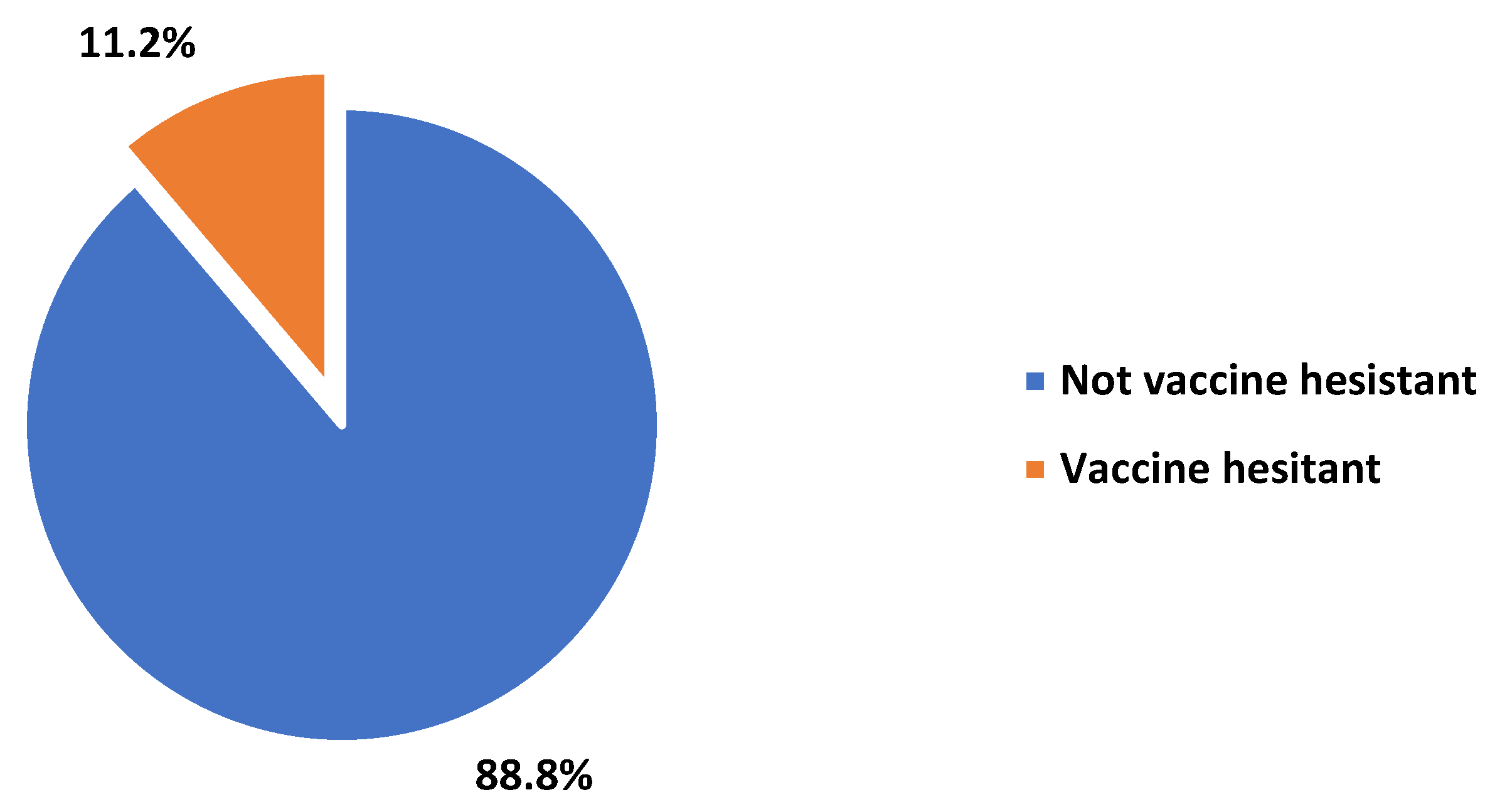
The study found that 148 (87.1%) of the respondents reported being vaccinated against COVID-19, with the AstraZeneca vaccine being the most common (72%). Among those who were not vaccinated, 19 (86.4%) stated they would not receive the vaccine, citing reasons such as lack of trust, painful administration, and already being infected with COVID-19. Only 32 (21.5%) of the vaccinated participants reported taking booster shots. Among those who did not take booster shots, 70 (60.3%) revealed they would eventually take them while 46 (39.7%) stated otherwise, with the main reasons for not receiving them being a lack of time, indecision, vaccine safety and side effects from previous shots. The majority of health workers 151 (88.25%) would recommend the COVID-19 vaccine to their family and friends, and 154 (90.6%) agreed that vaccinations reduce the risk of severe disease and death from infectious diseases.
Figure 3.
Prevalence of Vaccine Hesitancy among health workers.
Figure 3.
Prevalence of Vaccine Hesitancy among health workers.
3.5. Prevalence of COVID-19 Vaccine Hesitancy among Health Workers
Overall, 19 (11.2%) of health workers were hesitant in taking the COVID-19 vaccine while majority 151 (88.8%) were receptive to taking the COVID-19 vaccine
3.5. Association between Demographic Characteristics and Vaccine Hesitancy
Univariate logistic regression was used to predict sociodemographic characteristics that can influence COVID-19 vaccine hesitancy among the health workers. The regression model revealed workplace and location of workplace to significantly predict COVID-19 vaccine hesitancy. Health workers working in the Ghana Infectious Disease center were 77% less likely to be hesitant to COVID-19 vaccine compared to their counterparts working at the Shai Osudoku Isolation Center [COR= 0.23, 95% CI: 0.07-0.81, p-value = 0.022]. Similarly, respondents who work in urban settings were also 85% less likely to be hesitant to COVID-19 vaccine compared to their counterpart in rural settings [COR= 0.15, 95% CI: 0.02-0.97, p-value = 0.046].
3.6. Association between COVID-19 Experiences, Perception, Attitude towards COVID-19 and Vaccine Hesitancy among Health Workers
Univariate logistic regression was used to predict COVID-19 experience, perception and attitude towards COVID-19 which can influence COVID-19 vaccine hesitancy among health workers in this study. The univariate model predicted being infected with COVID-19, having an infected family member, perceiving COVID-19 as a serious disease, knowing COVID-19 can result in serious complication, regarding health workers as more vulnerable to COVID-19 infection, perceiving oneself at risk of severe form of COVID-19, recommending COVID-19 vaccine and associated severe disease and death as factors which could influence COVID-19 vaccine hesitancy among health workers in this study. Health workers who have ever been infected with COVID-19 were 69% less likely to be vaccine hesitant [COR= 0.31, 95% CI: 0.11-0.87, p-value = 0.027], those with an infected family member were also 78% less likely to be vaccine hesitant [COR= 0.22, 95% CI: 0.05-0.97, p-value = 0.045], perceived COVID-19 as a serious disease were 85% less likely to be vaccine hesitant [COR= 0.15, 95% CI: 0.03-0.70, p-value = 0.017], perceived health workers to be more vulnerable to COVID-19 infection were 78% less likely to be vaccine hesitant [COR= 0.22, 95% CI: 0.05-0.97, p-value = 0.045] and disagreed
they were at risk of getting the severe form of COVID-19 were 6.3 times more likely to be vaccine hesitant compared to those who agreed they were at risk [COR= 6.30, 95% CI: 1.51-26.23, p-value = 0.011]. Furthermore, health workers who stated they would recommend COVID-19 vaccine to their family and friends [COR= 0.05, 95% CI: 0.01-0.13, p-value <0.0001] and agreed vaccinations reduce the risk of severe disease and death associated with infectious diseases [COR= 0.15, 95% CI: 0.04-0.60, p-value = 0.007] were 95% and 85% less likely to be vaccine hesitant respectively.
3.7. Factors Associated with Vaccine Hesitancy among Health Workers
A multivariate logistic regression model was used to predict factors associated with COVID-19 vaccine hesitancy among health workers taking into consideration significant factors from
Table 4 and
Table 5. In the adjusted model, perceiving oneself to be at risk of severe disease from COVID-19, recommending COVID-19 vaccine to friends and family and agreeing vaccination against infectious diseases and reduces the risk of disease and death were the final predicted factors associated with COVID-19 vaccine hesitancy among the health workers. Health workers who disagreed they were at risk of getting the severe form of COVID-19 were 2.5 times more likely to be hesitant to COVID-19 vaccine compared to their counterparts who agreed [AOR= 2.53, 95% CI: 1.42-44.97, p-value = 0.028]. However, respondents who indicated they would recommend the vaccine to family and friends were 96% less likely to be vaccine hesitant compared to those who stated otherwise [AOR= 0.04, 95% CI: 0.06-0.19, p-value <0.0001]. Similarly, health workers who agreed vaccinations reduce the risk of severe disease and death associated with infectious diseases were also 94% less likely to be COVID-19 vaccine hesitant [AOR= 0.06, 95% CI: 0.01-0.56, p-value = 0.013].
4. Discussion
Vaccine hesitancy poses a significant threat to the efforts to curb infections. This becomes more disturbing when the hesitancy is among the high-risk populace such as healthcare workers, Healthcare workers play a vital role in rendering quality healthcare services, and their safety is central in the response of nations against pandemic[
15]. Hence to address the vaccine hesitancy, scientists and researchers need to investigate the determinants and predictors of vaccine hesitancy among the health workers, and develop tailored strategies to address the issue successful.
4.1. Attitude and Perception on COVID-19 Vaccine
The study found that over half (51.8%) of the health workers at various infectious disease treatment centers had been prior infected with COVID-19, which was higher than the infection rates reported among health workers in some studies conducted in New York, Atlanta, Qatar, and Iran [
19,
20,
21,
22,
23].The high infection rate may be due to the nature of their work and lack of resources in fighting the pandemic in a poor resource setting like Ghana. This high rate of COVID-19 infections among the health workers buttresses the World Health Organization's study that classified health workers as being more vulnerable to COVID-19 due to the nature of their work [
24]. Nonetheless, only 35.5% of the respondents perceived themselves as being at risk of getting a severe form of the infection.
While COVID-19 vaccination has been found to minimize the severity of the infection and prevent hospitalization, almost half (46.5%) of the health workers in this study thinks otherwise. They believe that being vaccinated prevents one from getting COVID-19 infection. This held perception of the participants is not the case and therefore education is needed in this regard, since they are seen as a prime source of health information. The majority of health workers (91.2%) acknowledged that the COVID-19 vaccines come with side effects, which is consistent with a study conducted among health workers in the Czech Republic [
18]. However, this perception did not influence hesitancy to the COVID-19 vaccine, which is consistent with a study that concluded that informing people of the limitations and side effects of vaccinations does not reduce their intentions to be vaccinated [
25].
Among the study participants, the AstraZeneca vaccine was the most well-known COVID-19 vaccine, followed by Pfizer-BioNTech and Johnson and Johnson. This may be due to AstraZeneca being the first vaccine to arrive in Ghana and its higher usage in the country. According to Ghana Health Service, as of February 15, 2023, out of the 23,466,480 COVID-19 vaccine doses administered in Ghana, 44.9% were AstraZeneca and 30.1% were Pfizer-BioNTech [
26] Also, only a small percentage (19.4%) of the participants knew about Sputnik V as a COVID-19 vaccine approved in Ghana, this is likely due to its low usage in the country.
Surprisingly, only 13.5% of health workers had knowledge about the number of COVID-19 vaccines approved for use in Ghana, which is concerning given that health workers are a trusted source of health information. The participants equally indicated that their primary source of information on COVID-19 vaccines was mainly through the local media outlets, social media and government of Ghana’s communiques. This finding is consistent with other studies which acknowledge the significant role of the both traditional and modern media in promoting vaccination and its positive impact on health-risk behaviours in the community [
27,
28]. Notwithstanding, the study highlights the need for regulation to prevent the spread of false information on the disease, since excess and uncontrolled information can lead to media fatigue, misinformation and fake news [
29].
The COVID-19 vaccine uptake among participants was high, with 87.05% having received at least one dose, exceeding the vaccination rate among some health workers in some other countries [
30]. Encouragingly, a higher proportion of health workers (76.5%) were fully vaccinated compared to the national figures. However, only 31.8% of participants had received their booster dose, despite its availability. This is a cause for concern as studies have shown that booster doses improve immunity and offer greater protection against new variants of the virus [
31,
32]. In contrast, health workers in Singapore had a much higher booster dose uptake rate of 73.8% [
33].
4.2. Prevalence of COVID-19 Vaccine Hesitancy
Based on the results of the present study, the COVID-19 vaccine hesitancy rate among participants was found to be 11.2%, which is lower than the rates reported in studies conducted in Ethiopia (60.3%), Egypt (41.9%), Uganda (13.3%), and Sub-Saharan Africa (50.5%) [
34,
35,
36]. This indicates an improvement compared to previous studies conducted among radiographers and health workers in Ghana, which reported vaccine hesitancy rates of 40.7% and 70%, respectively [
12,
37]. However, it is still concerning as these facilities treat patients with all severities of COVID-19, which put them more at risk. Evidence-based data from the Ghana Infectious Disease Centre suggests that unvaccinated patients with poor prognosis and those who end up in the Intensive Care Unit after contracting COVID-19 are in the majority, while those who had been vaccinated had milder symptoms and shorter hospital stays [
38]. Despite this data, some healthcare workers at these infectious disease centers remain hesitant to vaccinate, possibly due to cultural and psychological factors.
The hesitancy rate for booster doses in this study was found to be 31.1%, which is higher than the rates reported in studies conducted among health workers in the Czech Republic and Poland [
39,
40]. The study also found that health workers at the Ghana Infectious Disease Centre were 77% less likely to be hesitant than their colleagues at Shai Osudoku. Similarly, respondents who work in urban settings were 85% less likely to be hesitant than those in rural areas, which is consistent with earlier studies conducted in Ghana [
41]. This may be due to the low rate of COVID-19 infections in the rural areas as compared to the cities and also the misconceptions of the vaccine among the rural population in Ghana.
Although the prevalence of vaccine hesitancy in this study is lower than in other countries, it is still a concern given the crucial role of these facilities in treating COVID-19 patients. Efforts are needed to address the cultural and psychological factors that contribute to vaccine hesitancy among healthcare workers, particularly in rural areas, and to increase awareness of the benefits of vaccination.
4.3. Predictors to COVID-19 Vaccine Hesitancy
The study found that individuals who had previously been infected with COVID-19 or had relatives or acquaintances who had been infected were less likely to be hesitant towards COVID-19 vaccination. This aligns with findings from similar studies conducted in the United States and India among healthcare workers, where knowing someone who had been infected with COVID-19 significantly reduced vaccine hesitancy[
42,
43]. In contrast, healthcare workers in Atlanta and Lebanon who had previously been diagnosed with COVID-19 were more hesitant towards vaccination than those who had not been diagnosed [
44,
45]. Participants who perceived COVID-19 as a serious disease with the potential for severe complications were also less likely to be hesitant towards vaccination. Additionally, healthcare workers who believed they were more vulnerable to COVID-19 infection and could therefore develop a severe form of the disease were less likely to be hesitant towards vaccination. These factors were significant in informing a person's decision to get vaccinated. Having a good perception of the risk posed by COVID-19 was positively correlated with COVID-19 vaccine acceptance [
46,
47].
Multiple factors can influence people's attitudes towards vaccine hesitancy or refusal [
48]. Although most participants in this study adequately perceived the severity of COVID-19 and its prevention strategies, a small number were still hesitant to be vaccinated. Factors contributing to vaccine hesitancy included a preference for natural immunity, concerns about vaccine safety and unforeseen side effects. Major factors contributing to hesitancy towards the booster dose included side effects from previous doses, indecisiveness, and a lack of time to receive the vaccine. It is essential to evaluate the predictors of vaccine hesitancy among healthcare workers to inform policy development.
In this study, place of work (Ghana Infectious Disease Centre), urban settlement, knowing someone who had previously been infected with COVID-19, and perception of the severity of COVID-19 were significant predictive factors for hesitancy towards COVID-19 vaccines among the participants. Nonetheless, predictors varied for healthcare workers who participated in similar studies conducted in different parts of the world, including income, years of experience, individuals perceiving themselves to be at high risk, sex, and educational level [
35,
42,
49].
5. Conclusions
The study found that COVID-19 vaccine hesitancy among healthcare workers was generally low, as they had adequate perception of the severity of COVID-19. However, the hesitancy rate for the booster dose was high. The study identified past COVID-19 infection, knowing someone who had been infected, Vaccine safety, vaccine side effect and perception about COVID-19 severity as significant predictive factors for vaccine hesitancy. A multi-disciplinary approach is needed to address hesitancy among health workers.To bridge knowledge gaps on vaccination observed among some respondents in this study, the Institutional Care Division of the Ghana Health Service should organize training for health workers in various health institutions. Health promotion campaigns should also be conducted by the Ministry of Health and Ghana Health Service to encourage health workers to accept and receive the vaccines. Media sources were found to be a significant source of information on the vaccines among respondents, and this can be leveraged to enhance health promotion efforts.
Author Contributions
All authors substantively contributed to the work. Conceptualization G.D and S.A.B Investigation, G.D and S.A.B; resources, G.D, Data collection G.D Data analysis, G.D and S.A.B; Supervision of work, S.A.B; Original draft preparation; S.A.B and G.D; reviewing and editing, S.A.B and G.D; Project administration; S.A.B; Funding acquisition, G.D.
Funding
This research received no external funding, it was solely funded by the researchers.
Institutional Review Board Statement
Ethical clearance was sought and approved by Ghana Health Services Ethics Review Committee, with reference number: GHS-ERC: 040/12/22. Research was conducted under ethical standards.
Informed Consent Statement
All participant’s content was sought for the research and the publication of the research findings.
Acknowledgments
The authors would like to thank the Healthcare workers from the various Ghana Infectious Disease Centres and Ghana Health Service for their support that made this study possible. The technical and informational support is very much appreciated.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lippi, G.; Plebani, M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chim. Acta 2020, 505, 190–191. [Google Scholar] [CrossRef]
- Pal, R. COVID-19, hypothalamo-pituitary-adrenal axis and clinical implications. Endocrine 2020, 68, 251–252. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623–101623. [Google Scholar] [CrossRef] [PubMed]
- Syed, U.; Kapera, O.; Chandrasekhar, A.; Baylor, B.T.; Hassan, A.; Magalhães, M.; Meidany, F.; Schenker, I.; Messiah, S.E.; Bhatti, A. The Role of Faith-Based Organizations in Improving Vaccination Confidence & Addressing Vaccination Disparities to Help Improve Vaccine Uptake: A Systematic Review. Vaccines 2023, 11, 449. [Google Scholar] [CrossRef] [PubMed]
- Sadoff, J.; Gray, G.; Vandebosch, A.; Cárdenas, V.; Shukarev, G.; Grinsztejn, B.; Goepfert, P.A.; Truyers, C.; Fennema, H.; Spiessens, B.; et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against Covid-19. N. Engl. J. Med. 2021, 384, 2187–2201. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R. , et al., Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. New England journal of medicine, 2021. 384(5): p. 403-416. [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Mallapaty, S. and E. Callaway, What scientists do and don’t know about the Oxford-AstraZeneca COVID vaccine. Nature, 2021. 592(7852): p. 15-17.
- Chagla, Z. In adults, the Oxford/AstraZeneca vaccine had 70% efficacy against COVID-19 >14 d after the 2nd dose. Ann. Intern. Med. 2021, 174, JC29. [Google Scholar] [CrossRef]
- COVID-19-Dashboard, W.E., Ghana’s COVID-19 updates Ghana. Available online: https://covid19.who.int/region/afro/country/gh (accessed on 14 April 2023).
- Chou, W.-Y.S.; Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Heal. Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef]
- Alhassan, R.K.; Owusu-Agyei, S.; Ansah, E.K.; Gyapong, M. COVID-19 vaccine uptake among health care workers in Ghana: a case for targeted vaccine deployment campaigns in the global south. Hum. Resour. Heal. 2021, 19, 1–12. [Google Scholar] [CrossRef]
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef]
- Chou, R. , et al., Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Annals of internal medicine, 2020. 173(2): p. 120-136. [CrossRef]
- Agyekum, M.W.; Afrifa-Anane, G.F.; Kyei-Arthur, F.; Addo, B. Acceptability of COVID-19 Vaccination among Health Care Workers in Ghana. Adv. Public Heal. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Dhama, K.; Sharun, K.; Tiwari, R.; Dhawan, M.; Bin Emran, T.; Rabaan, A.A.; Alhumaid, S. COVID-19 vaccine hesitancy—reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum. Vaccines Immunother. 2021, 17, 3495–3499. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Pokorná, A.; Attia, S.; Klugarová, J.; Koščík, M.; Klugar, M. Prevalence of COVID-19 Vaccine Side Effects among Healthcare Workers in the Czech Republic. J. Clin. Med. 2021, 10, 1428. [Google Scholar] [CrossRef] [PubMed]
- Covid, C. , et al., Characteristics of health care personnel with COVID-19—United States, –April 9, 2020. Morbidity and Mortality Weekly Report, 2020. 69(15): p. 477. 12 February.
- Stock, A.D.; Bader, E.R.; Cezayirli, P.; Inocencio, J.; Chalmers, S.A.; Yassari, R.; Yanamadala, V.; Eskandar, E. COVID-19 Infection Among Healthcare Workers: Serological Findings Supporting Routine Testing. Front. Med. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Alajmi, J.; Jeremijenko, A.M.; Abraham, J.C.; Alishaq, M.; Concepcion, E.G.; Butt, A.A.; Abou-Samra, A.-B. COVID-19 infection among healthcare workers in a national healthcare system: The Qatar experience. Int. J. Infect. Dis. 2020, 100, 386–389. [Google Scholar] [CrossRef]
- Sabetian, G.; Moghadami, M.; Haghighi, L.H.F.; Shahriarirad, R.; Fallahi, M.J.; Asmarian, N.; Moeini, Y.S. COVID-19 infection among healthcare workers: a cross-sectional study in southwest Iran. Virol. J. 2021, 18, 1–8. [Google Scholar] [CrossRef]
- Burrer, S.L. , de Perio, M. A., Hughes, M. M., Kuhar, D. T., Luckhaupt, S. E., McDaniel, C. J., Porter, R. M., Silk, B., Stuckey, M. J., & Walters, M, Characteristics of health care personnel with COVID-19—United States, –April 9, 2020. Morbidity and Mortality Weekly Report, 2020. 69(15): p. 477. 12 February.
- WorldHealthOrganization, Protecting health workers from COVID-19 infection. Retrieved from https://www.who.int/westernpacific/news-room/feature-stories/item/protecting-health-workers-from-covid-19. 2020.
- Kerr, J.R. , et al., Effect of information about COVID-19 vaccine effectiveness and side effects on behavioural intentions: two online experiments. Vaccines, 2021. 9(4): p. 379.
- GhanaHealthService, COVID-19 Vaccines doses administered. Retrieved on 16th March, 2023 from https://www.ghs.gov.gh/covid19/. 2023.
- Mohamed, N.A.; Solehan, H.M.; Rani, M.D.M.; Ithnin, M.; Isahak, C.I.C. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLOS ONE 2021, 16, e0256110. [Google Scholar] [CrossRef]
- Wakefield, M.A.; Loken, B.; Hornik, R.C. Use of mass media campaigns to change health behaviour. Lancet 2010, 376, 1261–1271. [Google Scholar] [CrossRef]
- Ho, K.K.W.; Chan, J.Y.; Chiu, D.K.W. Fake News and Misinformation During the Pandemic: What We Know and What We Do Not Know. It Prof. 2022, 24, 19–24. [Google Scholar] [CrossRef]
- Farah, W.; Breeher, L.; Shah, V.; Hainy, C.; Tommaso, C.P.; Swift, M.D. Disparities in COVID-19 vaccine uptake among health care workers. Vaccine 2022, 40, 2749–2754. [Google Scholar] [CrossRef] [PubMed]
- Canaday, D.H.; Oyebanji, O.A.; White, E.; Keresztesy, D.; Payne, M.; Wilk, D.; Carias, L.; Aung, H.; Denis, K.S.; Sheehan, M.L.; et al. COVID-19 vaccine booster dose needed to achieve Omicron-specific neutralisation in nursing home residents. EBioMedicine 2022, 80, 104066. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, R.K. , et al., Need of booster vaccine doses to counteract the emergence of SARS-CoV-2 variants in the context of the Omicron variant and increasing COVID-19 cases: an update. Human Vaccines & Immunotherapeutics, 2022. 18(5): p. 2065824.
- Koh, S.W.C.; Tan, H.M.; Lee, W.H.; Mathews, J.; Young, D. COVID-19 Vaccine Booster Hesitancy among Healthcare Workers: A Retrospective Observational Study in Singapore. Vaccines 2022, 10, 464. [Google Scholar] [CrossRef] [PubMed]
- Amuzie, C.I.; Odini, F.; Kalu, K.U.; Izuka, M.; Nwamoh, U.; Emma-Ukaegbu, U.; Onyike, G. COVID-19 vaccine hesitancy among healthcare workers and its socio-demographic determinants in Abia State, South-East Nigeria: a cross-sectional study. Pan Afr. Med J. 2021, 40. [Google Scholar] [CrossRef] [PubMed]
- El-Sokkary, R.H. , et al., Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: a cross-sectional study. BMC infectious diseases, 2021. 21: p. 1-9.
- Mohammed, R.; Nguse, T.M.; Habte, B.M.; Fentie, A.M.; Gebretekle, G.B. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PLOS ONE 2021, 16, e0261125. [Google Scholar] [CrossRef] [PubMed]
- Botwe, B.; Antwi, W.; Adusei, J.; Mayeden, R.N.; Akudjedu, T.; Sule, S. COVID-19 vaccine hesitancy concerns: Findings from a Ghana clinical radiography workforce survey. Radiography 2021, 28, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Owoo, C. , Our Covid-19 OPDs are filling up; Infection of health workers on the rise—GHS. Myjoy online.com. Retrieved from https://www.myjoyonline.com/our-covid-19-opds-are-filling-up-infection-of-health-workers-on-the-rise-ghs/. 2021.
- Klugar, M.; Riad, A.; Mohanan, L.; Pokorná, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines 2021, 9, 1437. [Google Scholar] [CrossRef] [PubMed]
- Rzymski, P.; Poniedziałek, B.; Fal, A. Willingness to Receive the Booster COVID-19 Vaccine Dose in Poland. Vaccines 2021, 9, 1286. [Google Scholar] [CrossRef]
- Sampene, A.K.; Li, C.; Agyeman, F.O.; Brenya, R. Socioeconomic and demographic characteristics influencing the hesitancy and refusal of COVID-19 vaccine in Ghana. Ther. Adv. Vaccines Immunother. 2023, 11. [Google Scholar] [CrossRef]
- Elliott, T.R.; Perrin, P.B.; Powers, M.B.; Jacobi, K.S.; Warren, A.M. Predictors of Vaccine Hesitancy among Health Care Workers during the COVID-19 Pandemic. Int. J. Environ. Res. Public Heal. 2022, 19, 7123. [Google Scholar] [CrossRef]
- Ashok, N. , et al., High COVID-19 vaccine hesitancy among healthcare workers: should such a trend require closer attention by policymakers? Cureus, 2021. 13(9).
- Kandiah, S.; Iheaku, O.; Farrque, M.; Hanna, J.; Johnson, K.B.; Wiley, Z.; Franks, N.M.; Carroll, K.; Shin, S.R.; Sims, K.M.; et al. COVID-19 Vaccine Hesitancy Among Health Care Workers in Four Health Care Systems in Atlanta. Open Forum Infect. Dis. 2022, 9, ofac224. [Google Scholar] [CrossRef] [PubMed]
- Youssef, N.J.; Tfaily, N.K.; Moumneh, M.B.M.; Boutros, C.F.; Elharake, J.A.; Malik, A.A.; McFadden, S.M.; Galal, B.; Yildirim, I.; Khoshnood, K.; et al. COVID-19 Vaccine Acceptance and Hesitancy Among Health Care Workers in Lebanon. J. Epidemiology Glob. Heal. 2023, 13, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Ganti, L.; Graham, E.W.; Shah, D.; Aleksandrovskiy, I.; Al-Bassam, M.; Fraunfelter, F.; Falgiani, M.; Leon, L.; Lopez-Ortiz, C. COVID-19 Vaccine Hesitancy Among Healthcare Providers. Heal. Psychol. Res. 2022, 10, 34218. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688–113688. [Google Scholar] [CrossRef]
- Hickler, B. , et al., Health communication and vaccine hesitancy. Vaccine, 2015. 33: p. 4180-90.
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiology 2020, 35, 775–779. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).