1. Introduction
Today, using a conventional full arch for the treatment of edentulous patients has been a treatment approach used for several years. [
1] However, often, due to severe vertical and horizontal resorption of the alveolar ridge, complications such as lack of stability and reduced chewing function are often associated with lower full dentures. [
2] Thus, to improve and usable oral function, chewing ability and esthetic comfort, the use of mandibular full-arch restorations (fixed or removable) supported by conventional implants has been advanced in the interforaminal region, which have achieved a predictable mode with high success rates (87% to 100%) [
1,
2]. However, maxillary resorption due to periodontal disease and vertical and horizontal bone loss can reach a degree of severity that prevents or even limits conventional implant rehabilitation treatments.[
34] In addition, sovereign anatomical structures such as the inferior alveolar nerve can be irreparably damaged when using conventional length implants [
34]. To overcome these situations, the literature often proposes more invasive techniques to which the clinician must refer such as vertical bone augmentation [
4], osteogenic distraction [
4] and inferior alveolar nerve lateralization [
4]. However, limiting elements such as dental phobia, morbidity in the postoperative period, economic costs, and treatment difficulty may negatively influence the patient in wanting and being able to accept implant therapy[
5]. Recently, some systematic scientific reviews and clinical studies have shown that using short implants results in low failure and complication rates and, most importantly, have found very minimal marginal bone loss for single and partial restorations supported by short implants placed in the mandible. However, to date, we do not have enough evidence on the durability of full-arch prosthetic restorations supported by short implants (<8 mm) in completely edentulous and severely resorbed mandibles [
6,
7]. On the other hand, we have Group 1 of the 6th ITI Consensus Conference that analyzing the definition of ‘‘short’’ established “short dental implants” as all dental implants ≤6 mm in size. [
8] Today, scientific evidence from several clinical studies in the literature has either found no statistically significant differences in implant survival rates or observed no changes in marginal bone loss (MBL) of short dental implants compared to standard length dental implants. Often combining the use of short implants and bone regeneration techniques can result in less surgical complexity.[
8] Other studies have shown the more discrepancy is present in the crown-to-implant ratio, the more the risk of mechanical problems increases, but has not increased the risk of peri-implant marginal bone loss. Another important aspect to evaluate and consider is the area of implant installation, because the likelihood of failure increases when implants are installed in low-density bone, such as in the maxilla in the posterior region.[
7,
8,
9,
10,
11,
12] However, there is no consensus on the short-term survival rate of implants in the maxilla and mandible posteriorly.[
9] Some authors have advanced limited success rates, while others have found high success rates for short implants placed in the maxillae.[
9,
10,
11]
The purpose of this study was to systematically review the literature regarding implant survival rates, marginal bone levels, and prosthetic success of full-arch short dental implants used for the rehabilitation of severe mandibular atrophy..
2. Materials and Methods
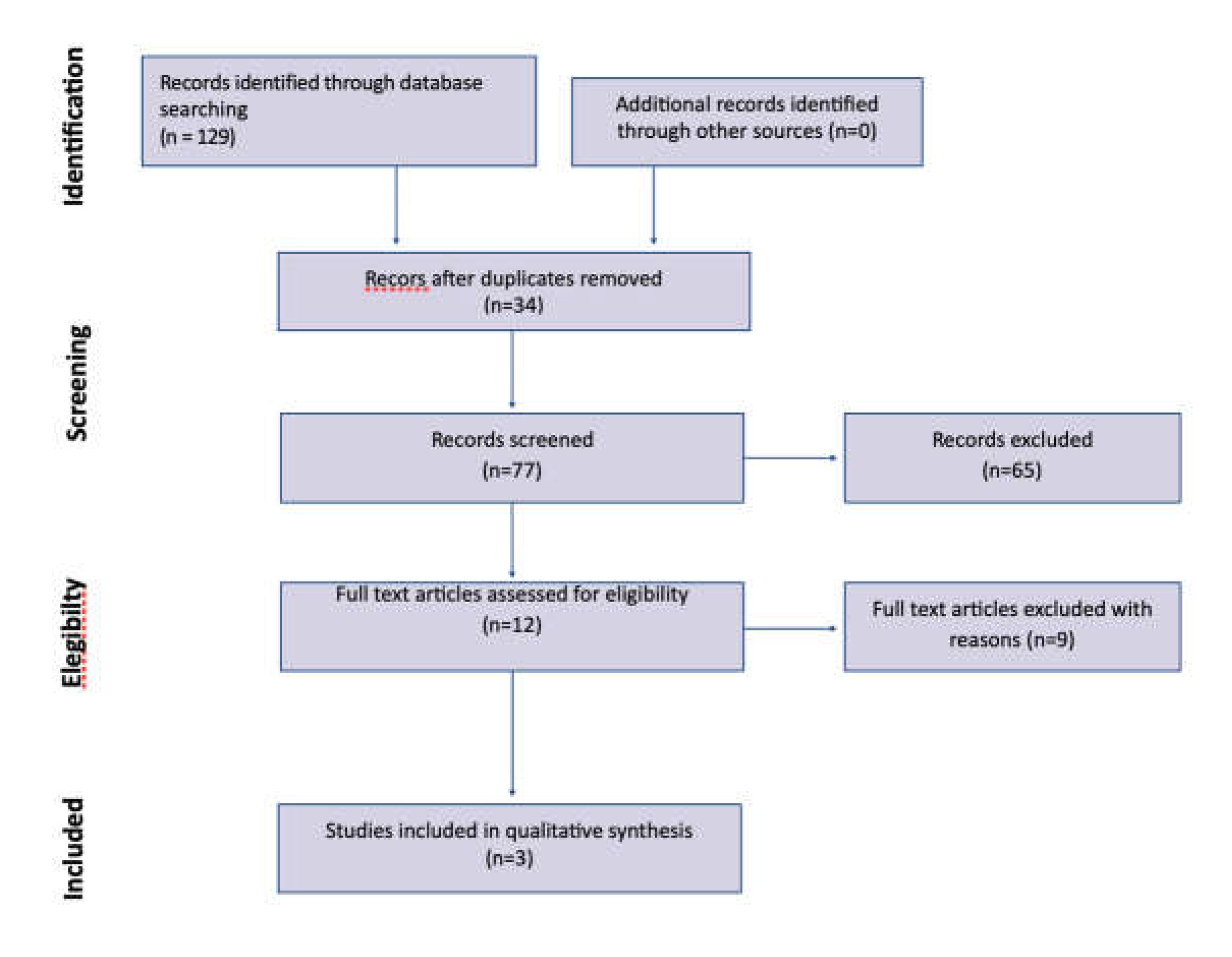
This study followed the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement. Therefore, the aim of this systematic review was to answer the focused question: “In patients with edentulous jaws, what is the performance of fixed and removable full-arch restorations supported by short (≤6 mm) implants with regards to marginal bone loss , the implant failure rate, prevalence of biological and prosthetic complications?”. The primary research question was captured in the PICO (Population, Intervention, Comparison, Outcomes) format: “Do shorts implants as full arch support (I) report the same clinical results (O) in randomized controlled trials (S) in total edentulism of the mandible (P) as a substitute for long implants (C)? The inclusion and exclusion criteria were defined by the authors before the start of the study. Inclusion criteria were all human-based randomized controlled trials (RCTs) with at least 10 patients and 1 year of follow-up after prosthesis delivery and published in English. All studies were designed to evaluate the clinical efficacy of short implants to rehabilitate severe posterior mandibular atrophy. All the studies analyzed were published between January 1, 2010 and February 28, 2023. The exclusion criteria were as follows: studies reporting the same data as subsequent publications by the same authors, systematic reviews, comments and letters to the editor , case reports, in vitro studies, animal model studies, and case series. Relevant systematic review papers, as well as reference lists of all included articles, were searched by hand to identify additional publications. Full-text screening, study selection, and data extraction were performed in duplicate, and disagreements were resolved by consensus.
Figure 1.
Search strategy flow chart.
Figure 1.
Search strategy flow chart.
2.1. Elegibility Criteria
Eligible studies must have the following characteristics: (1) randomized controlled trials, (2) prospective studies, (3) studies with at least ten edentulous patients receiving fixed or removable full-arch restorations supported by short implants in the mandible,(4) comparisons between short and standard implants
works in the same study, (6) published in English. In this study, the threshold to consider an implant short was a length of ≤8mm
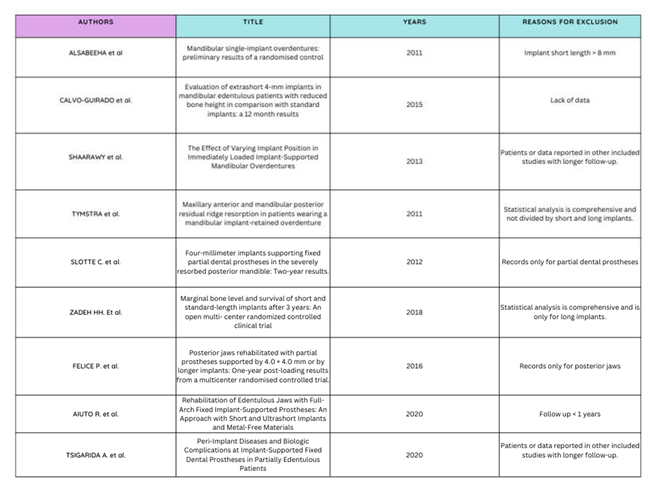
2.2. Exclusion Criteria
(1) Reviews, letters, case reports, conference abstracts; (2) retrospective studies; (3) In vitro studies; (4) preclinical studies; (5) Studies with fewer than 4 short implants; (6) Studies with a follow-up of less than 1 year after loading; (7) Studies describing short implants with a length greater than 8mm; (8) Other types of restorations (single crowns, fixed partial dentures); 9 - Short implants placed in the grafted areas; (10) Absence of data on implant length; and (12) Failure to attempt to contact the author for eligibility purposes.
2.3. Outcome Measures
The primary outcome examined by this systematic review was the survival rate of short dental implants supporting full arches. Secondary outcomes were marginal bone levels, biological complications, and prosthesis failure. All data collected and analyzed were measured preoperatively and at each annual recall, for at least 1 year of follow-up.
2.4. Search Strategy
The search involved electronic databases (MEDLINE, Embase and Cochrane Library). The following combination of words was used: “short implant OR short implants OR extra short implant OR extra shorts implants AND mandible AND full arch”. In addition, review bibliographies were analyzed and compared.
2.5. Selection Criteria and Data Extraction
Two independent reviewers (A.R.) and (A.P.) performed a three-step screening procedure of all selected studies. Any possible disagreements were resolved by further review. First, the titles were analyzed to eliminate studies that were inappropriate. Then, all abstracts were reviewed and only selected studies were involved in reading the full text.
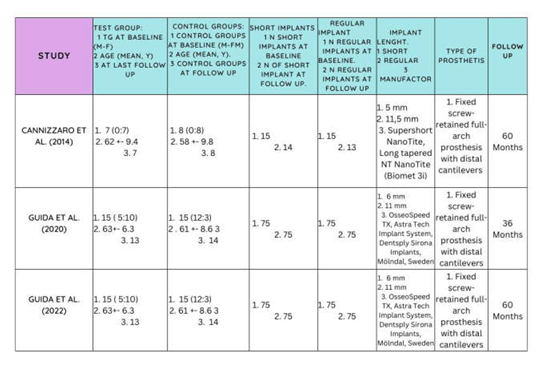
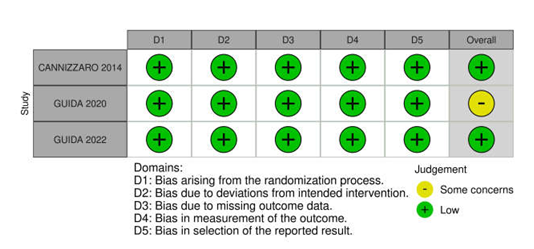
2.6. Risk of Bias
The quality of the studies included in the review was assessed by the reviewer (A.R.) and (A.P.) using the Cochrane Collaboration tool for assessing the risk of bias for randomized trials. The potential risk of bias was classified as low, high, or unclear. Any disagreements were discussed until resolved by consensus. (Table 3)
4. Discussion
This review considered whether full prosthetic arches supported by short (≤8 mm) implants confer success in the aesthetic/functional restoration of totally edentulous mandibles. The short implant concept itself has been described and evaluated in recent years, still not properly defined as to the specific length and diameter that are sufficient to have surgical and prosthetic predictability. In this review, implants with an “osseointegrable surface length” less than or equal to 8 mm were chosen to guide the search for articles in the literature.[
13]A mean marginal bone loss of approximately 0.13 mm was found to correlate with a randomized trial that studied 75 short implants and reported mean values between 0 and 2 mm for the same 3-5 year follow-up period Cannizzaro et al.[
16]. In contrast, a systematic review by Seeman and Bruggenkate et al.[
6,
7,
8,
9,
10,
11,
12,
13,
14,
15] found a significant effect of increased diameter on marginal bone loss of short implants supporting single crowns. The bone loss of short implants in the first year is significantly better than that of long implants. Thus, it can be argued that the type of prosthetic rehabilitation provided on a short implant plays a critical role on the outcome of bone loss. Blanes Rj et al. [
20] in a review showed that the disadvantageous ratio of implant length to superstructure height does not result in bone loss for both short and long implants. Of interest is the study by Tsigarida et al. [
30] who reported high survival rates for implants supporting fixed full-arch restorations in the mandible in a review. Immediate loading procedures have high survival rates for both fixed and removable prostheses. There are, however, differences in the number of implants, implant characteristics, complications, and costs between these two types of prostheses to consider. Rameh et al. [
32] in a review showed that survival rates of short implants to full arch support are high regardless of the length or position of the inserted implant. However, more biological complications were found in standard implants especially for splinted prostheses, which were associated with fewer technical complications. The results of this review demonstrated that, when used correctly, short implants achieve predictable long-term results and p, provided they are placed following a comprehensive surgical and prosthetic protocol based on the various biomechanical parameters essential for optimizing long-term prognosis.
The survival rate of implants placed in this study (97.7%) parallels the systematic review performed by Srinivasan et al.[
21], who observed high survival rates (98.6%) for short implants with the rough surface (6 mm) placed in the mandible under different prosthetic restorations. Carosi et al.[
7] in one study showed that out of 14 patients with a full mandibular arch, only five implants failed, resulting in an overall implant survival rate of 96.9%. No definitive prostheses have failed, with a prosthetic success rate of 100%. The failed implants were successfully and without final problems replaced before the final restorations were fabricated, with an overall treatment success rate of 100%.
Furthermore, it has been observed that approximately 75% of short implant failures are failures of the early type. The survival rate of the short implants in this study is comparable to the survival rate (96%) of the longer implants placed in heterologous bone with various surgical techniques. Another important study performed by Slotte et al. [
26] demonstrated that the 12-month survival rate of 100 short (4 mm) implants was 95.7%, 92.3% at 24 months, slightly lower than another study by Renouard et al. [
14] who reported a survival rate of short implants placed in the mandible and loaded of 94.6% at two years. As already mentioned above, the reasons for the good results with short implants can be related to the high initial primary stability and the effective use of residual bone volume with high primary bone-to-implant contact in dense bone structures. Also Renouard et al.[
14] in a recent review demonstrated how the failure rate with short implants was related to the learning curves of the surgical operator, osteotomy preparation (regardless of bone density), use of surface-machined implants, and placement in sites with low bone density.[
27]tine surgical preparation (regardless of bone density), use of surface-machined implants, and placement in sites with bone density scarce.[
27]
Compared to the prevalence of biological complications, this was not relevant for the type of prosthetic restoration. The most common biological event observed was the accumulation of residual plaque and the increase (> 4 mm) of the probing depth of the pocket at the various follow-ups. The relationship between plaque accumulation and gingivitis or periodontitis is well documented in the literature as a major late risk factor for implant failure. Already Linde et al. [
13] demonstrated that accumulations of plaque around implants induce local inflammation and progressive marginal bone loss over the years. In the studies considered for this review, none of them evaluated and found any risk factors that could lead to peri-implant pathology, nor signs of peri-implantitis.[
18,
19]. Carosi et al. [
2] in another study showed that a total of 160 implants were placed in 37 patients, while in 3 patients both arches were rehabilitated. 40 full arch rehabilitations were performed, of which only 14 were in the mandible. Of these, only 5 implants failed, with an overall implant survival rate of 96.9%. BoP was detected in approximately 6 implants (3.7%) and 16 implants had a superficial amount of plaque, resulting in a plaque score of 10%. Lian et al. [
33] in a systematic review with meta-analysis showed that for completely edentulous mandibles, short implants are a reliable therapeutic alternative, as survival and MBL were not different from those of long implants placed. However, further high-level studies are still needed to determine the long-term clinical outcomes of short implants in completely edentulous jaws.
On the contrary, it was demonstrated in this study that the prevalence of prosthetic complications was widely different for both types of prostheses loaded on short implants (fixed or removable). In this review Guida et al.[
17,
18,
19,
20,
21,
22,
23] demonstrated that failures with fixed full-arch restorations were more frequent and common and reported that the prosthetic failure rate reached 62.5%, considering that they were installed 7 prostheses and there were 3 debondings of five restorations and 3 fractures of the prosthetic structure. This could be due to the presence of the distal cantilevers. The review by Morris et al. is very interesting. [
28] which demonstrates in a study in which 13 arches were treated with approximately 64 short implants that the minimum value of the implant insertion torque was 20 Ncm. After 12-18 months of operation (average 14 months), the implant and prosthetic survival rates were 100%. Eight patients were restored with permanent hybrid fixed prostheses in zirconia or acrylic resin. Two patients were restored with titanium rod frameworks and removable overdentures. No prosthetic complications were reported for the definitive prostheses. This demonstrates that this result should be interpreted with caution. Conversely Cannizzaro et al.[
16], who used fixed screw-retained full-arch restorations, found only one screw loosening during the 1-year follow-up. The author’s most reported restorative failures were unthreading, loss of retention, rod adjustment, rod tension, cantilevers, and relining. In an interesting systematic review performed by AlTarawneh et al. [
29] Satisfactory clinical and esthetic results have been found for full arch implant restoration with the use of monolithic zirconia, thereby increasing short-term success. The rate of technical complications associated with this type of restoration, to date, is still minimal and the survival rates are very high. Since the concept of short implants remains an ever-evolving abstract (less than or equal to 8 mm), two different calculations were performed in this review: 1) ≤ 9 mm; and 2) ≤ 5 mm as a threshold for short length implants. In fact it has been observed that the greater the length of the implants used, the lower the failure rate of these implants. Telleman et al. [
22] in his review, however, did not find this increase in survival rate using long implants alone.The question of a probable compensation of the reduction in implant length with an increase in the diameter of the implant remains controversial at present. In this review, no significant difference was found between implant diameter and outcomes of marginal bone loss and implant failure rate, once the majority of implants used were of regular diameter. Conversely, the least favorable results were found to be related to implants of larger diameter rather than regular for all lengths. The results suggest that short implants need not have a large diameter to resist masticatory forces if the prosthetic axes are respected. Due to the thickness and blood supply (cortical bone) characteristics of the buccal and lingual bone walls, short, regular diameter implants help to better dissipate masticatory forces over the crestal bone, reducing marginal bone loss. A study on finite element analysis by Himmlova et al. [
24] and Anitua et al.[
25] It demonstrated that implant length plays a minor role in force distribution. From this in vitro study, in order to reduce the loss of marginal bone, it was recommended to modify the design of the implant, favoring rough surfaces and increasing the thread to favor and improve osseointegration. de Oliveira Melo et al [
31] noted in a finite element study that it is suggested that all short (4 mm) implants studied are apparently viable alternatives for the rehabilitation of atrophic mandibles. However, the 6 and 8 mm implants showed more favorable mechanical behavior than the 4 mm implants.
The clinical recommendations obtained from this review with the associated limitations dictated by the sparse literature were as follows:
Short implants demonstrated the same survival rate as long implants
There are slight variations in marginal bone loss between short and long implants
Standard implants are associated with more biological complications when associated with GBR
Fixed prostheses with cantilevers are more prone to prosthetic complications
Limitations of this review include the limited number of articles found in the literature and selected and included with small sample sizes. The following limitation may be mainly due to the recent nature of the topic that the aforementioned review aims to address, as well as to the eligibility criteria applied during the study selection phase. Another limitation is that the studies included evaluated full-arch fixed restorations and no removable-type restorations. It is well documented that the two types of restorations exhibit different biomechanical behaviors and, therefore, a direct comparison should be made in detail.
5. Conclusion
Implant therapy has significantly developed over the years thanks to growing experience, technical development and procedures to enable treatment. This means that implant therapy has also become available for patients with reduced bone support due to. A 4mm implant can be used in special clinical situations, as shown in this study, and also in combination with longer implants. In terms of cost-effectiveness, placing a short implant in the available bone reduces treatment time by avoiding alternative procedures such as bone grafting or GBR. Furthermore, as shown in this study, the predictable result, even in challenging situations, is a major advantage over a sometimes unpredictable bone augmentation procedure. Designing a short implant for pre-existing available bone appears to be a good alternative to time-consuming, often painful and expensive supplementary methods. From a specialist point of view, there are still indications in which a short implant satisfies a requested need very well. However, before long-term studies are available, this implant should primarily be suitable for well-experienced clinicians/specialists in order not to compromise the treatment outcome in difficult cases. Despite the limitations, the present systematic review concluded that both fixed and full-arch restorations supported by short implants represent a viable short-term option for the treatment of mandibular atrophies, with minimal marginal bone loss and a low failure rate. implants. Evidence on this topic is lacking and larger, prospective clinical trials using short implants, particularly for full-arch restorations, should be conducted.