Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease is a progressive condition characterised by persistent airflow limitation and an increased chronic inflammatory response in the airways and lungs to noxious particles or gases [
1]. Respiratory infections, smoking, occupational exposures, genetic predisposition are considered as risk factors for COPD [
2]. It presents with both pulmonary and extra pulmonary symptoms that includes impairments such as peripheral muscle dysfunction and dyspnea that curb an individual’s ability to carry out the activities of daily living (ADLs) [
2,
3].
Arm activities, supported or unsupported, are common in all aspects of daily life. They play an important role in both simple and complex daily tasks such as grooming activities, washing the dishes, and putting groceries on shelves [
4]. Peripheral muscle dysfunction and dyspnea during routine ADLs involving unsupported upper limb activities is common and often leads to the avoidance of upper limb activities. This makes the patients progressively disabled as they can no longer cope with simple ADLs [
5,
6].
Peripheral muscle dysfunction may be attributable to systemic inflammation, oxidative stress, blood gas disturbances, corticosteroid use, reduction in muscle mass and inactivity-induced deconditioning [
7]. A reduced capacity for muscle aerobic metabolism may also contribute to this dysfunction. Increased lactic acidosis for a specific workload increases ventilatory requirements which impose an additional burden on the already overloaded respiratory muscles [
6].
Dyspnea during upper limb activities can be due to the mechanical effects of arm elevation. The accessory respiratory muscles assist with the postural support of the arm, diminishing their participation in ventilation and shifting the respiratory work to the diaphragm [
8,
9]. Arm elevation increases functional residual capacity, possible mechanisms are the passive stretching of the thoracic muscles and the expansion of the rib cage, imposing a greater burden that must be overcome by the diaphragm [
9,
10].The reduction in upper limb muscle strength may increase arm fatigue, thereby contributing to the impairments [
11].
Measuring and monitoring skeletal muscle function should be a part of the routine assessment of patients with COPD. In order to attain this aim, standardized and feasible static and dynamic measurement methods, along with reference values are required. Although isometric measurements have been recommended, dynamic measurements of skeletal muscle function should be considered as they are related to daily life functional tasks to a great extent [
12].
Various tests have been designed for assessing upper limb function, including the
, unsupported upper limb exercise test (UULEX) [
13], six-minute pegboard and ring test (6PBRT) [
14], the supported upper limb extremity test (SULEX) [
5] and grocery shelving task (GST) [
15,
16]. GST is one of the highly reproducible standard evaluation tests that assess upper extremity function by asking patients to place two grocery shopping bags on a high shelf as quickly as possible 15,16].
Reference values for the test are required to compare with the values derived from patients and accordingly assess the impairments. These values can also serve as the target point for the upper limb strength training regime as a part of the pulmonary rehabilitation protocol. Studies have hardly been conducted to attain reference values for GST. As there is a lack of retrievable data regarding these values, the main aim of this study was to find the reference values of GST in the population of the United Arab Emirates population, for it to be used as an effective tool to test the functional capacity of people with different pulmonary conditions and diseases.
Material and methods
Study design and population
We conducted a cross-sectional study with 220 healthy individuals of both genders from age groups 20 to 69 years. They were stratified into five groups (20-29, 30-39, 40-49, 50-59 and 60-69 years) based on their age.
Ethical considerations
The approval for this study was received from the Ethical committee of the University of Sharjah. The eligible participants were explained about the study procedure (Parameters that will be assessed, starting position, steps of the test, symptoms to stop performing the test) and written informed consent was taken from the eligible participants.
Recruitment of the participants
The recruitment of the healthy population for the study was initiated through an advertisement on social media stating- “a request to adults older than 20 years old to participate in a study on the GROCERY SHELVING TASK –a simple upper limb test”. Details regarding the test, investigators’ phone numbers and email addresses were also provided. Clinically healthy individuals were also recruited randomly from public places and through their families and friends for a period of 1 year (June 2021 to June 2022). Participants who expressed interest in the study were interviewed and assessed to screen them for eligibility. They were asked questions regarding their health status, daily medications, previous hospital admission, restrictions in performing ADLs and exercise routine. Screening assessments including measurement of height, weight, range of motion of upper limb were performed.
Eligibility criteria
Inclusion criteria:
- i)
Healthy adult between the age of 20-70 years; of either gender
- ii)
Body mass index (BMI) of 18.5 kg/ to 40 kg/
- iii)
No symptoms of cardiopulmonary disease
- iv)
Can accomplish his or her ADLs with no restrictions.
Exclusion criteria:
- i)
Any history of cardiopulmonary problems
- ii)
Recent surgery that prevents them from participating in the study test
- iii)
Any musculoskeletal, neuromuscular, or metabolic diseases; and any deformities such as severe kyphosis, scoliosis that would interfere with protocol performance
- iv)
Those who are not able to understand commands and instructions.
Initial evaluation
Demographic data were collected prior to the commencement of the test session. Body mass and height were measured to calculate body mass index (BMI). Baseline measurements of oxygen saturation, blood pressure, heart rate, respiratory rate, fatigue and breathlessness using modified Borg scale were taken at rest just before initiating the test. All the measurements were performed in short sitting (on the chair) position.
Materials
- i)
1 Shelf
- ii)
1 High table
- iii)
20 objects of 420-g
- iv)
2 shopping bags
- v)
Stop watch
- vi)
Pulse oxymeter
- vii)
Sphygmomanometer
- viii)
Weighing machine
- ix)
Stadiometer
Procedure
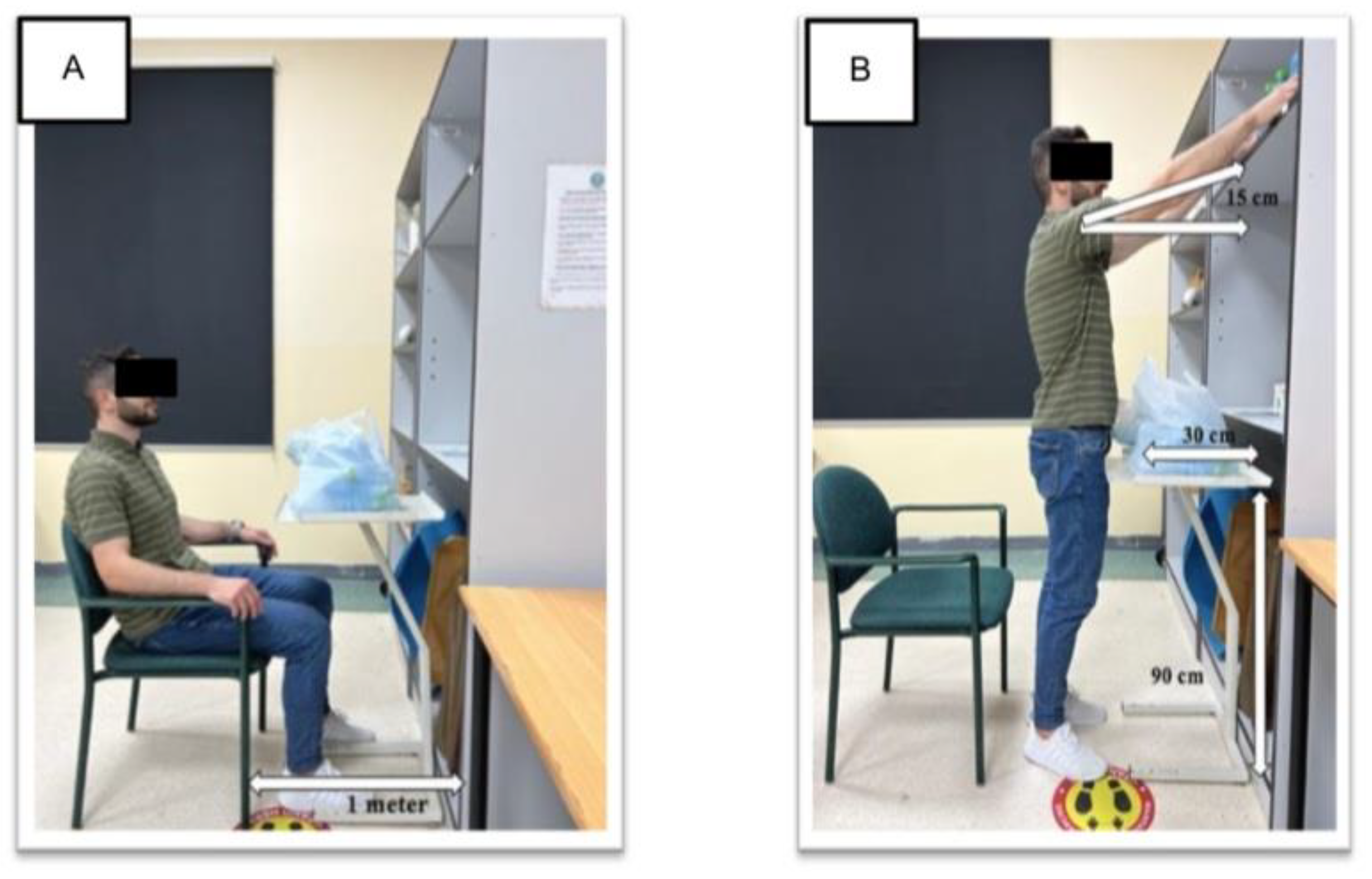
The standard procedure and instructions of the GST were explained to the participants [
15]. A shelf was placed 15 cm above the shoulder level while the participants were in a standing position. Then a 90 cm high table was placed 30 cm in front of the shelf. Twenty objects weighing 420-g were placed in 2 shopping bags on the floor on both sides of the table. The individual started the test from a sitting position in a chair, at a 1mtr distance from the table (
Figure 1).
The instructions were as follows:
When instructed, get up as quickly as possible and place all these items as quickly as you can from the two shopping bags on the shelf in front of you. You may accomplish the task in any form you would like; you cannot hold more than one item at once or lift the bag directly to the shelf. Put your arms down when the task is over. The duration (in seconds) required to complete the task will be recorded. You can decrease your speed or pause if you need to.
A practice test was performed followed by one trial of GST after a gap of thirty minutes. No encouragement was provided during the task. If the participant took a pause in between the test, the time recording was continued. The variables oxygen saturation, blood pressure, heart rate, respiratory rate, fatigue and breathlessness were assessed at the baseline, immediately, 1 minute and 3 minutes after completing the task.
Statistical Analysis
Statistical analysis was performed using IBM SPSS statistics for Windows, version. 25.0 (IBM Corp., Armonk, NY, USA). The normality of data was checked using the Shapiro-Wilk test. Data were expressed as mean ± standard deviation. The correlation between the duration of the test and the age, height, and body mass of the participants were assessed using Pearson’s correlation test. A p value of less than 0.05 was considered significant.
Results
A total of 220 apparently healthy individuals from both genders and different age groups were included in this study, involving a total of 127 females and 93 males from the ages of 20-29, 30-39, 40-49, 50-59, 60-69 years. The participants’ demographic data are presented in
Table 1.
The duration, hemodynamic parameters, respiratory parameters, and fatigue pre- and post-GST are presented in
Table 2 and
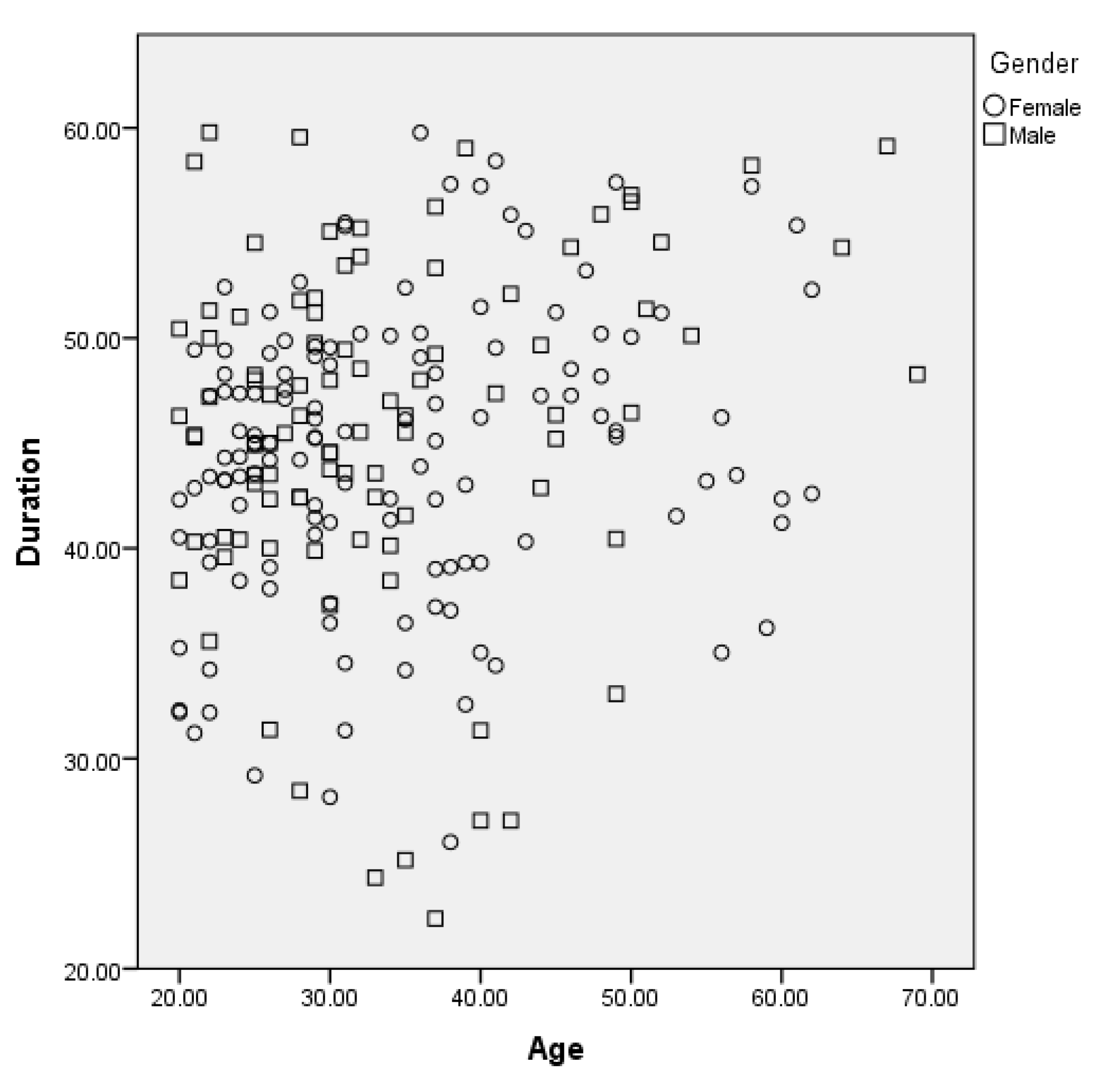
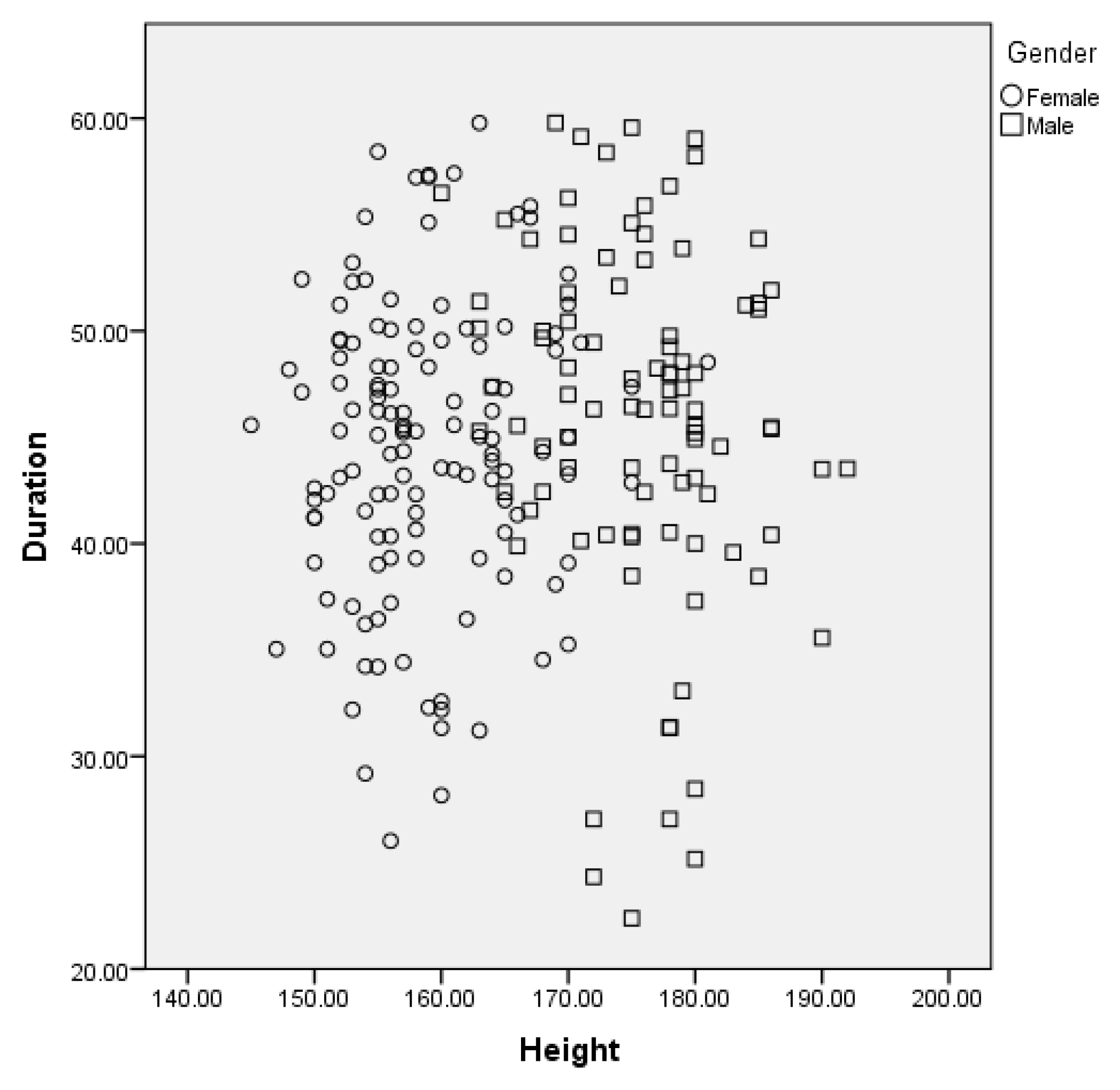
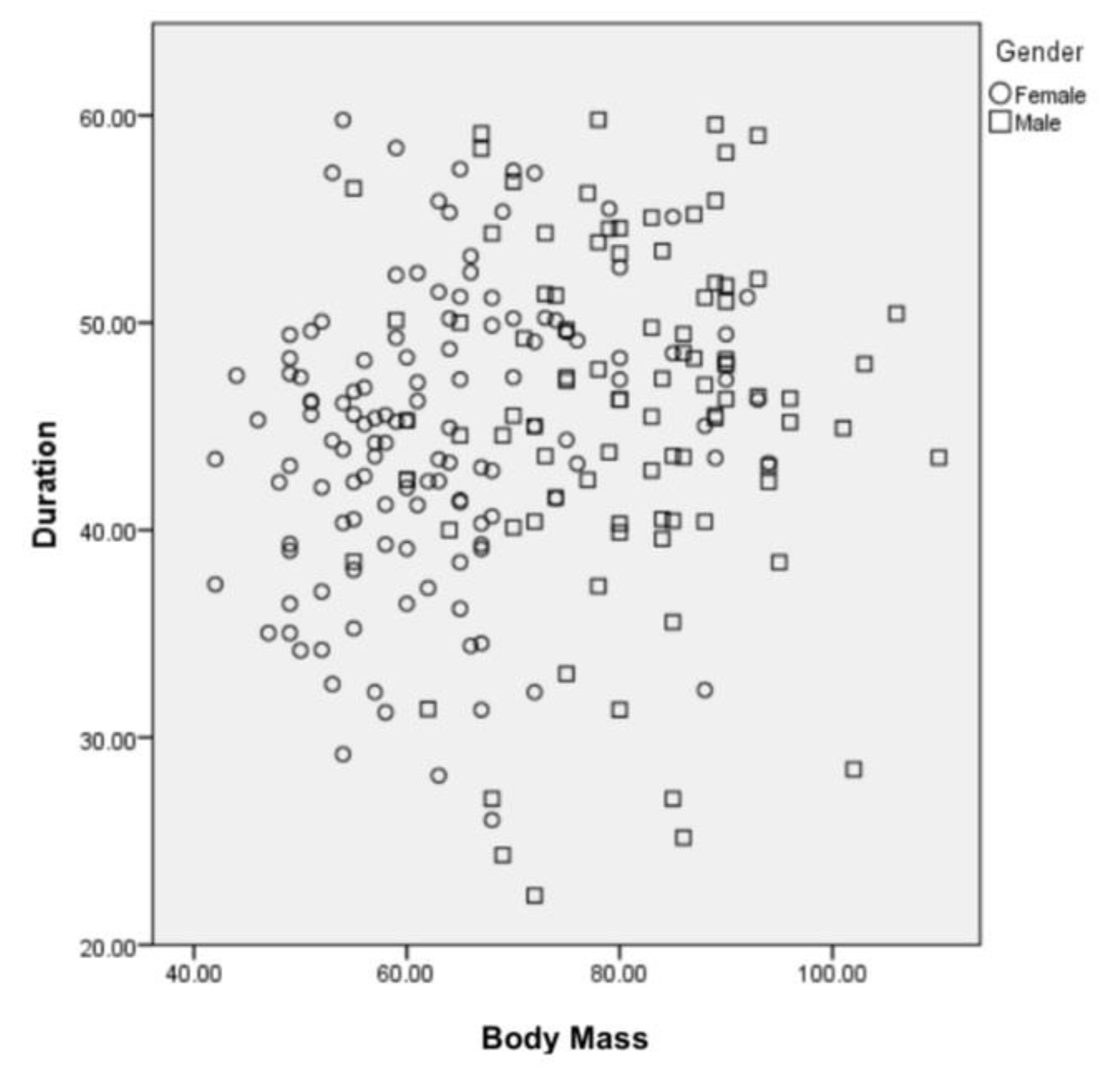
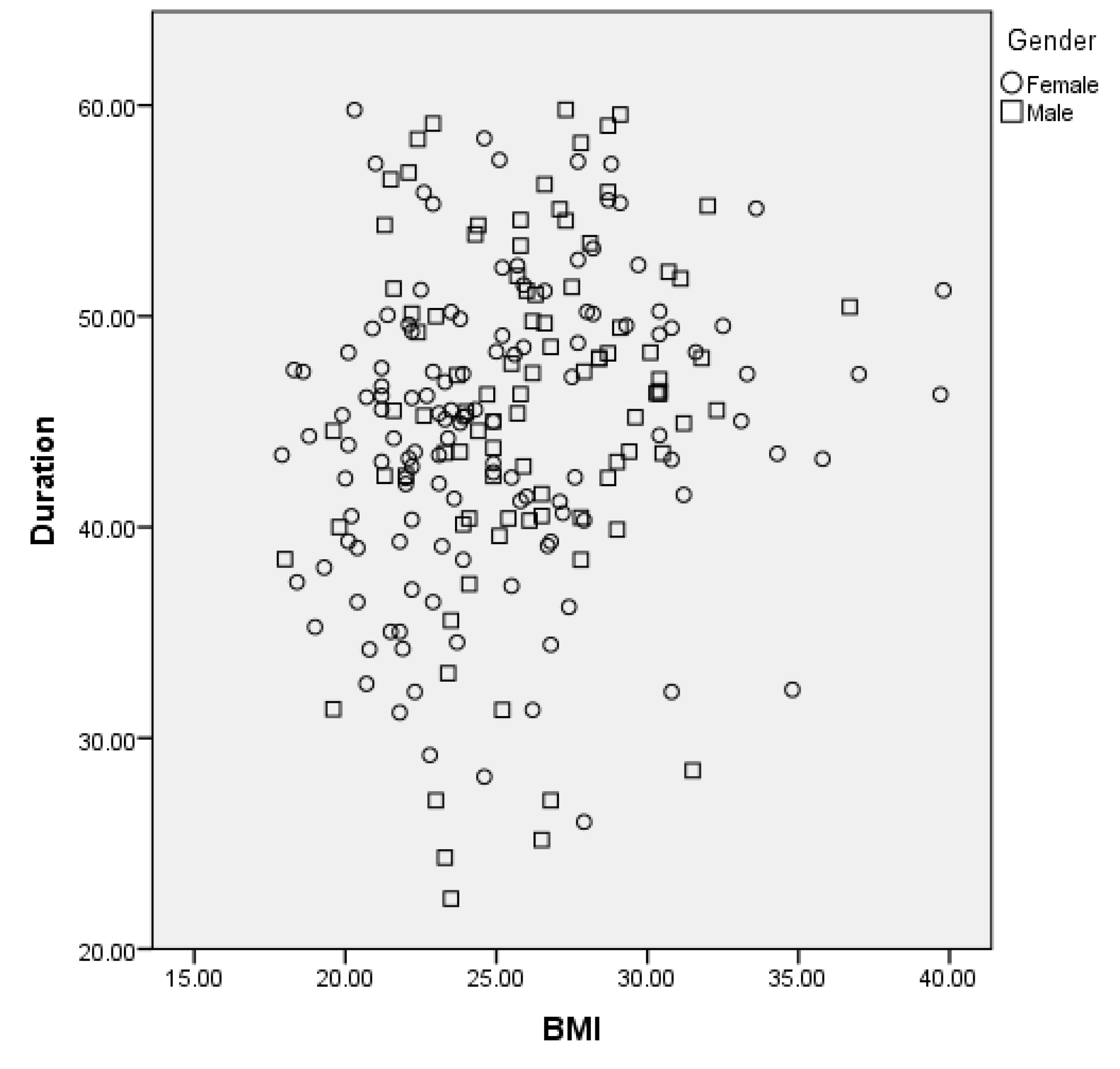
Table 3. In males, the mean duration in of task completion in seconds was 42.5±10.01 for 20-29 years, 44.8±8.9 for 30-39years, 45.7±6.7 for 40-49 years, 53.4±4.2 for 50-59 and 53.9±5.4 for 60-69 years. In females, the mean duration in seconds was 43.5±5.5 for 20-29 years, 43.1±8.08 for 30-39years, 48.1±6.7 for 40-49 years, 49.9±7.1for 50-59 years and 56.7±6.5 for 60-69 years. Heart rate, respiratory rate, peripheral oxygen saturation, and systolic blood pressure showed significant differences between the pre and post-test values in most of the age groups. Dyspnea and fatigue showed no significant difference in most age groups. The correlation analysis, as represented in
Table 4, showed a weak positive correlation between the duration of GST test and age, body mass, height, BMI, among both females and males (
Figure 2,
Figure 3,
Figure 4 and
Figure 5).
Discussion
The current study aimed to identify reference values for GST in the population of the United Arab Emirates. A total of 220 participants were recruited in the age groups 20-29, 30-39, 40-49, 50-59 and 60-69. A smaller number of participants could be recruited in the older age groups because of difficulty in meeting the eligibility criteria.
Significant differences were seen in the pre and post-test heart rate, respiratory rate, peripheral oxygen saturation and systolic blood pressure in most of the age groups. The reason for these changes could be the increase in metabolic demand caused by the exercising muscles. This demand is achieved through numerous changes in the cardiovascular and respiratory systems mediated by the sympathetic nervous system [
10]. These changes include generalized peripheral vasoconstriction in non-exercising muscle causing increase in systolic blood pressure, increased frequency of sinoatrial node depolarization resulting increased heart rate and augmented myocardial contractility. Respiratory rate increases to attain the requirement of increased oxygen extraction and consumption by the exercising muscles. The amount of response depends on the muscle mass involved in the task [
17]. Similar increases in physiological parameters were seen in studies done on other upper limb functional tests [
9,
11].
Various factors could influence the duration required to perform the GST, therefore, we tried to find a correlation between the duration and demographic characteristics of the participants, such as age, height, body mass and BMI. All the variables had a weak correlation with the duration of the task. This is because the height of the shelf was adjusted according to the height of the participant. For example, the shelf was fixed at 15 cm above shoulder level for all the participants and did not have a fixed level from the ground which omits the height significance. The body mass factor did not interfere with the task results, as GST does not assess functional capacity through full body activities. As the BMI calculation is based on height and body mass, it was not significantly correlated to the duration of the task. These results are in accordance with the studies performed on other unsupported upper limb tests [
9,
14].
Although a weak correlation was found between age and duration was found, gradual increase in the duration required for completing the test was seen as the age increased. The factors that have been attributed to this result could be age related changes in cardiorespiratory endurance and muscle strength and endurance [
4,
5]. Reduction in muscle strength and endurance could be attributed to the loss of muscle mass due to decreased protein synthesis, reduction in cross-sectional area and lowered motor unit activation as the age progresses [
18].Variations in the cardiovascular endurance could be attributed to decrements in both central and peripheral cardiovascular function. This includes reduction in stroke volume, maximal heart rate, stiffening of ventricles and arteries and blunted functional sympatholysis [
18]. Reductions in proprioceptive abilities and memory as age progresses could also contribute to this result [
8]. A similar trend of decreasing performance is seen in studies conducted on other upper limb tests [
9,
14]. Lima et al.[
14] and Kulkarni et al.[
9] discovered that the number of rings moved in six minutes decreased as age increased in studies to determine the normative values of the six-minute peg board and ring test.
The limitations of the present study were that we also did not consider the motivation levels while the test was performed. We also did not study more objective parameters like pulmonary functions in relation to the duration of the test. Factors such as balance and peripheral muscle strength that could have influenced the duration of the test were not studied. Future studies can be conducted on patients with pulmonary and cardiovascular conditions to assess their performance and to compare the difference from the normative values.
Conclusion
This study determined the normative values for GST among the United Arab Emirates population from the age 20 to 69 years. Changes were observed in heart rate, respiratory rate, peripheral oxygen saturation, and systolic blood pressure between the pre and post-test values in most of the age groups. Dyspnea and fatigue showed no significant difference in most age groups. Weak correlations were found between the duration of the task and the age, height, body mass, and BMI of the participants.
Funding
This work was supported by the Fundação Carlos Chagas Filho de Apoio à Pesquisa do Estado do Rio de Janeiro (FAPERJ, No. E-26/211.104/2021) and Coordenação de Aperfeiçoamento de Pessoal (CAPES, Finance Code 001; No. 88881.708719/2022-01, and No. 88887.708718/2022-00).
Declaration of interest
None
References
- Vestbo, J.; Hurd, S.S.; Agusti, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013, 187, 347–365. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Silverman, E.K.; Shapiro, S.D. Chronic Obstructive Pulmonary Disease. In Harrison’s Principles of Internal Medicine, 16th ed.; Kasper, D.L., Braunwald, E., Fauci, A.S., Hauser, S.L., Longo, D.L., Jameson, J.L., Eds.; United States McGraw-Hill: United States, 2004; pp. 1547–1551. [Google Scholar]
- Panka, G.F.; Oliveira, M.M.; França, D.C.; Parreira, V.F.; Britto, R.R.; Velloso, M. Ventilatory and muscular assessment in healthy subjects during an activity of daily living with unsupported arm elevation. Rev Bras Fisioter 2010, 14, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Hoogendam, Y.Y.; van der Lijn, F.; Vernooij, M.W.; Hofman, A.; Niessen, W.J.; van der Lugt, A.; et. al. Older age relates to worsening of fine motor skills: a population-based study of middleaged and elderly persons. Front Aging Neurosci. 2014, 6, 259–265. [Google Scholar] [CrossRef]
- Ingram, L.A.; Butler, A.A.; Walsh, L.D.; Brodie, M.A.; Lord, S.R.; Gandevia, S.C. The upper limb Physiological Profile Assessment: Description, reliability, normative values and criterionvalidity. PloS One 2019, 14, e0218553. [Google Scholar] [CrossRef] [PubMed]
- Nici, L.; Donner, C.; Wouters, E.; Zuwallack, R.; Ambrosino, N.; Bourbeau, J.; et al. American ThoracicSociety/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006, 173, 1390–1413. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society/European Respiratory Society. Skeletalmuscle dysfunction in chronic obstructive pulmonary disease: a statement of the American Thoracic Society and European Respiratory Society. Am J Respir Crit Care Med. 1999, 159, S1–S40. [Google Scholar]
- Adamo, D.E.; Alexander, N.B.; Brown, S.H. The influence of age and physical activity on upper limb proprioceptive ability. J Aging Phys Act. 2009, 17, 272–293. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, M.S.; Alaparthi, G.K.; Krishnan, S.; Ramakrishna, A.; Acharya, V. Reference value for the six-minute peg board and ring test. A cross sectional study. Multidiscip Respir Med. 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Thimmaraju, L.; Anandarao, S.B. Gender differences in cardiovascular response to upper limb isometric exercises. Int J Res Health Sci. 2014, 2, 454–461. [Google Scholar]
- Gulart, A.A.; Munari, A.B.; Tressoldi, C.; Dos Santos, K.; Karloh, M.; Mayer, A.F. Glittre-ADL multiple tasks induce similar dynamic hyperinflation with different metabolic and ventilatory demands in patients with COPD. J Cardiopulm Rehabil Prev. 2017, 37, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Marklund, S.; Bui, K.L.; Nyberg, A. Measuring and monitoring skeletal muscle function in COPD: current perspectives. Int J Chron Obstruct Pulmon Dis. 2019, 1825–1838. [Google Scholar] [CrossRef] [PubMed]
- Zhan, S.; Cerny, F.J.; Gibbons, W.J.; Mador, M.J.; Wu, Y.M. Development of an unsupported arm exercise test in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2006, 26, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Lima, V.P.; Almeida, F.D.; Janaudis-Ferreira, T.; Carmona, B.; Ribeiro-Samora, G.A.; Velloso, M. Reference values for the six minute peg board and ring test in healthy individuals in Brazil. J Bras Pneumol. 2018, 44, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.J.; Denehy, L.; Holland, A.E.; McDonald, C.F. Measurement of functional activity in chronic obstructive pulmonary disease: the grocery shelving task. J Cardiopulm Rehabil Prev. 2008, 28, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Janaudis-Ferreira, T.; Beauchamp, M.K.; Goldstein, R.S.; Brooks, D. How should we measure arm exercise capacity in patients with copd?: A systematic review. Chest 2012, 141, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Holtgrefe, K.; Glenn, T.M. Principles of Aerobic Exercise. In Therapeutic Exercise Foundations and Techniques, 5th ed.; Kisner, C., Colby, L.A. and Borstad, J., Eds.; F.A.Davis Company: Philadelphia, USA, 2002; pp. 235–236. [Google Scholar]
- Kenney, W.L.; Wilmore, J.H.; Costill, D.L. Aging in Sport and Exercise. In Physiology of Sport and Exercise, 5th ed.; Kenney, W.L., Wilmore, J.H., Costill, D.L., Eds.; United States of America: Human Kinematics: 2011; pp. 452–454.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).