1. Introduction
Rotator cuff injury is a common diagnosis among patients with shoulder pain and dysfunction. Rotator cuff tendinopathy is characterized by pain and weakness, especially during elevation and external rotation [
1]. The supraspinatus muscle, the most important external rotator, is one of the key movers and stabilizers of the shoulder and is highly susceptible to overloading and tendinopathy. It accounts for more than half of all cases of chronic shoulder diseases [
2]. Increased disabilities of the arm, shoulder and hand and poor visual analogic scale have been found in patients with active external rotation restriction [
3].
Treatment includes nonsteroidal anti-inflammatory drugs, analgesics, corticosteroid injections and, eventually, in some patients, arthroscopic rotator cuff repair is necessary [
4], especially in the case of associated subacromial impingement syndrome. In addition, exercise and physical therapy have also been considered as non-pharmacological treatments. Indeed, exercise therapy is the mainstay of conservative management of tendinopathy and has focused largely on resistance training, and, in many instances, eccentric strengthening techniques [
5].
The rationale of exercise therapy is to improve load tolerance and possibly structural adaptation of the musculotendinous unit to restore function. In the early phase of rehabilitation, flexibility exercises are often initiated and incorporated into strengthening regimes to facilitate improvements in mobility.
Swinton et al [
5], in their recent review, report that tendon healing is a complex and lengthy process, with remodeling only beginning 1–2 months post-injury and extending beyond 1 year, suggesting that longer exercise interventions are required with guidelines recommending a minimum of 12 weeks. In clinical practice, the duration of over 90% of programs is 12 weeks or less, and exercise programs are thus frequently provided for patients to continue therapy at home due to the limited resources. In addition, the use of upper limb exoskeletons for individuals who have lost their range of motion (ROM) may allow them to perform motor training with multiple repetitions and minimal physical burden to therapists, with a view to allowing independent continuation of the training in a community setting in the future. Furthermore, the COVID-19 pandemic has highlighted the need for safe and effective home-based and tele-rehabilitation settings. Cost-effective automation devices, such as exoskeletons, are critical for the success of these interventions and rehabilitation programs. Physical therapy can be a demanding, lengthy, and costly process, which can lead to a loss of interest in individuals undergoing therapy. Reducing recovery time is a potential solution that may motivate individuals to participate and continue physical therapy. Rehabilitation with an exoskeleton can reach more patients while reducing physician interactions and overall rehabilitation costs [
6].
Most current robot-like rehabilitation equipment is based on exoskeletons [
7], or haptic devices [
8]. Exoskeletons typically cover the arm and forearm and are linked to the trunk using flexible components. Meanwhile, haptic devices are attached to the hand to guide upper-limb movement while exerting force.
This paper describes a one-degree-of-freedom haptic device applied to execute three different exercises for shoulder rehabilitation. This device implements force control behavior. This force control entails a resistance to the patient shoulder rotation that is customized according to patient status. Therefore, the same equipment can be adapted to the patient´s evolution and record all session activities for clinician studies. In addition, a compact piece of equipment was designed for a specific rehabilitation task.
2. Materials and Methods
2.1. Device
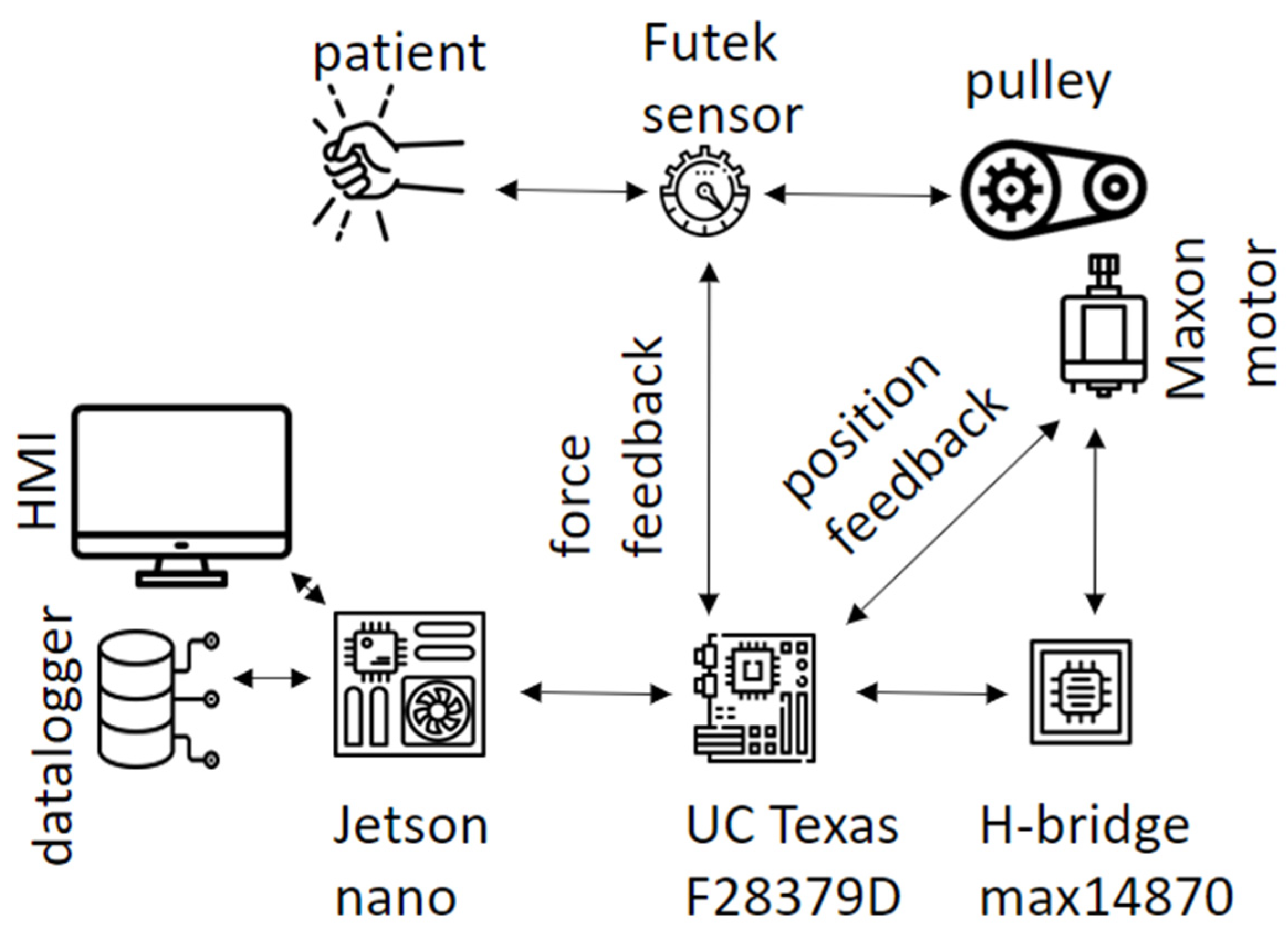
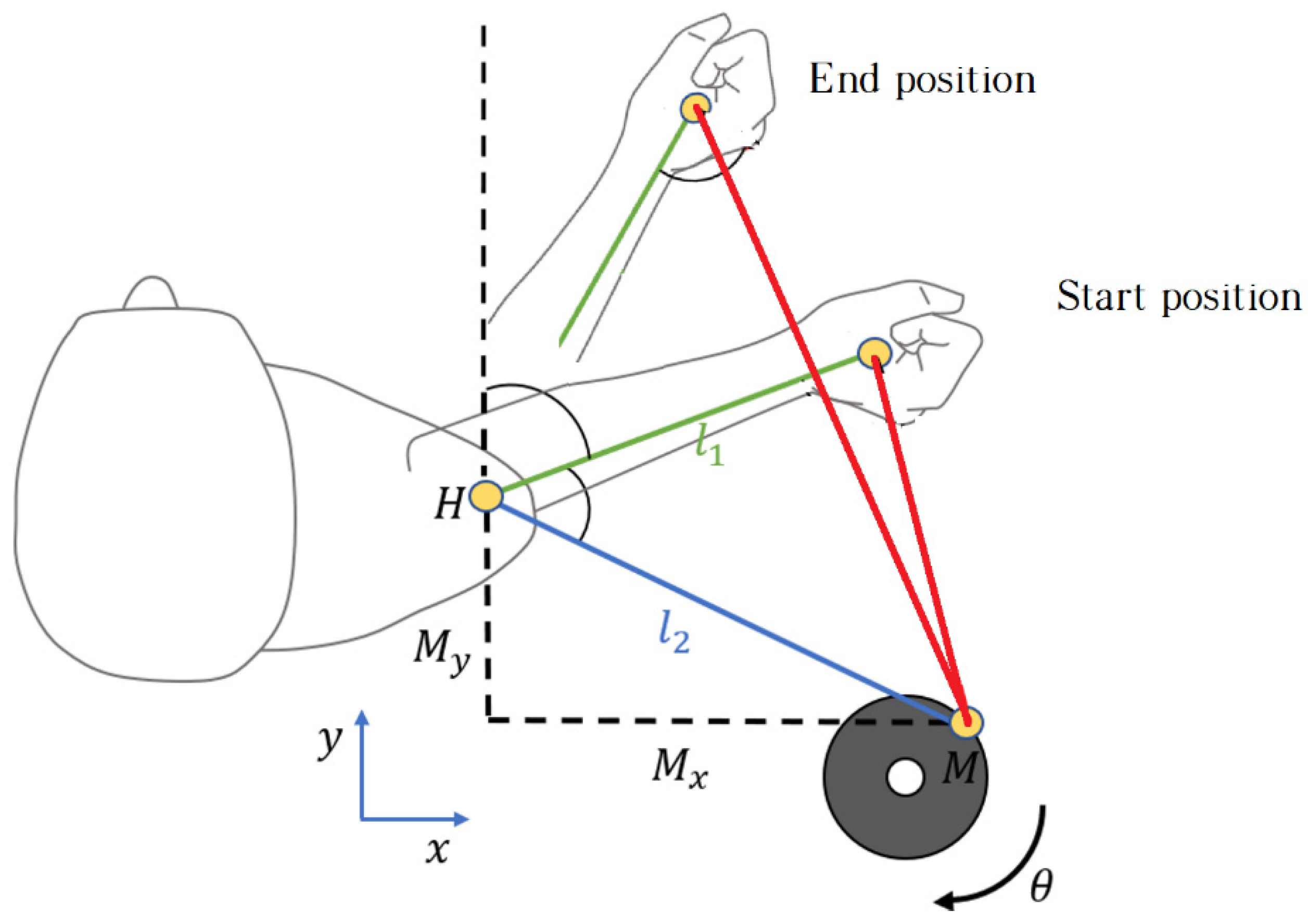
The rehabilitation device consists of the following components: the actuator, transmission components, force sensor, handle and controller. The architecture used is shown in the
Figure 1. The actuator is based on a DC motor; the Maxon DCX22S+GPX26HP+ENX16EASY was selected for this application. Its rated operation is at 38 VDC, 5.9 Nm, and 10.5 revolution per minute (RPM). This motor generates the required force applied to the patient. The controller calculates the reference value according to the desired force and information provided by sensors, then the driver (H-bridge max14870) set the power to the motor The controller is run on a Texas Instruments board, specifically, the LAUNCHXL-F28379D model. This board contains the 32-bit dual-core TMS320F2-8379D microcontroller, which runs at 200 MHz. The controller closes the force control loop at 1 kHz.The transmission is made up of a cable and a pulley that transmit the actuator torque to the patient, the ratio between motor and pulley is 100:1 millimeter A force sensor is located at the end of the cable and is also linked to the handle. The force sensor is implemented by a load cell manufactured by Futek, which is used for measuring the force reflected by the motor. The sensor model used in this work is LSB205 connected to the Analog Strain Gauge Signal Conditioner IAA100, it offers a load measurement range from 0 to 11 Kg corresponding to 0 to 5 DC volts.
The patient’s hand is inside the handle, which is made of a flexible textile for a comfortable grip.
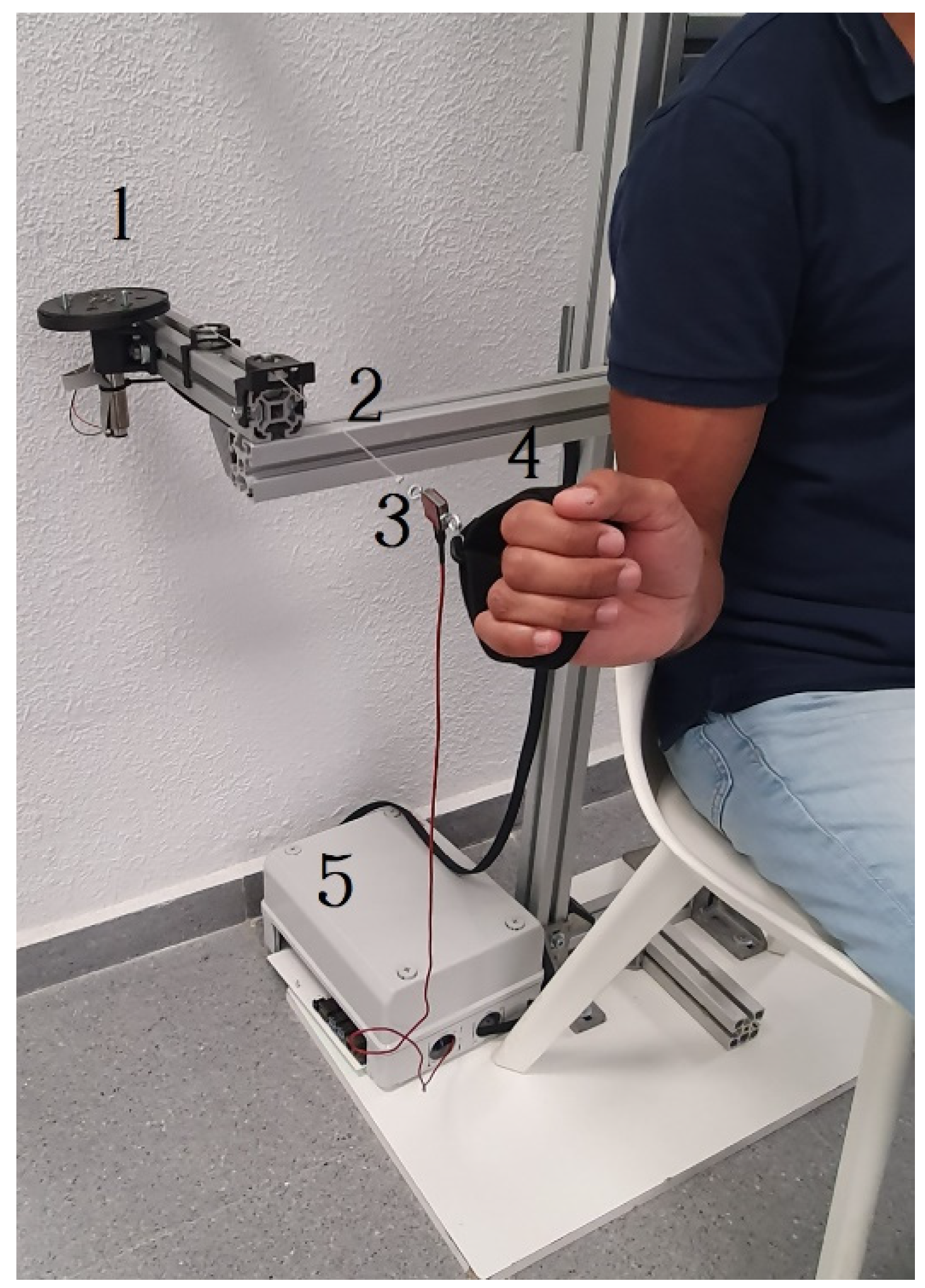
Figure 2 shows an image with all the components. Patients sit in a chair, and the components described are mounted in an aluminum structure that provides a comfortable workspace.
2.2. Control algorithm design
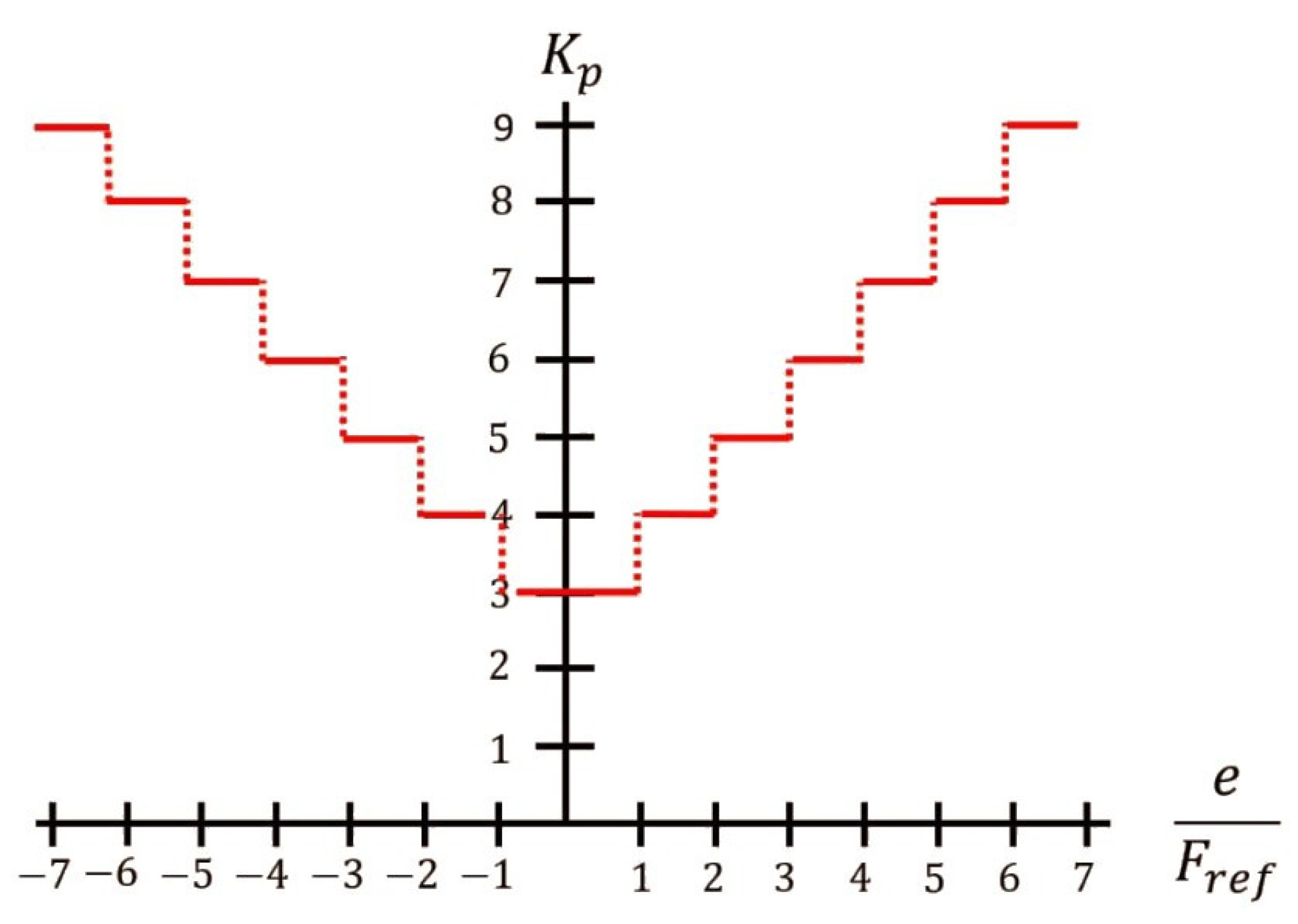
In this work a force controller is proposed, it is based on the cable tension exerted by the patient and an adaptive speed PI controller. The force sensor provides a range of detection from 0 N to 111 N, therefore the maximum configurable payload of the prototype is 11.32 Kg. The proportional gain K
p is modified as a function of the ratio between the force error and the reference, the proposed values are shown in
Figure 3. Whereas the integral gain K
i was set with a value of 2. The K
p and K
i were tuning experimentally.
2.3. Controller performance
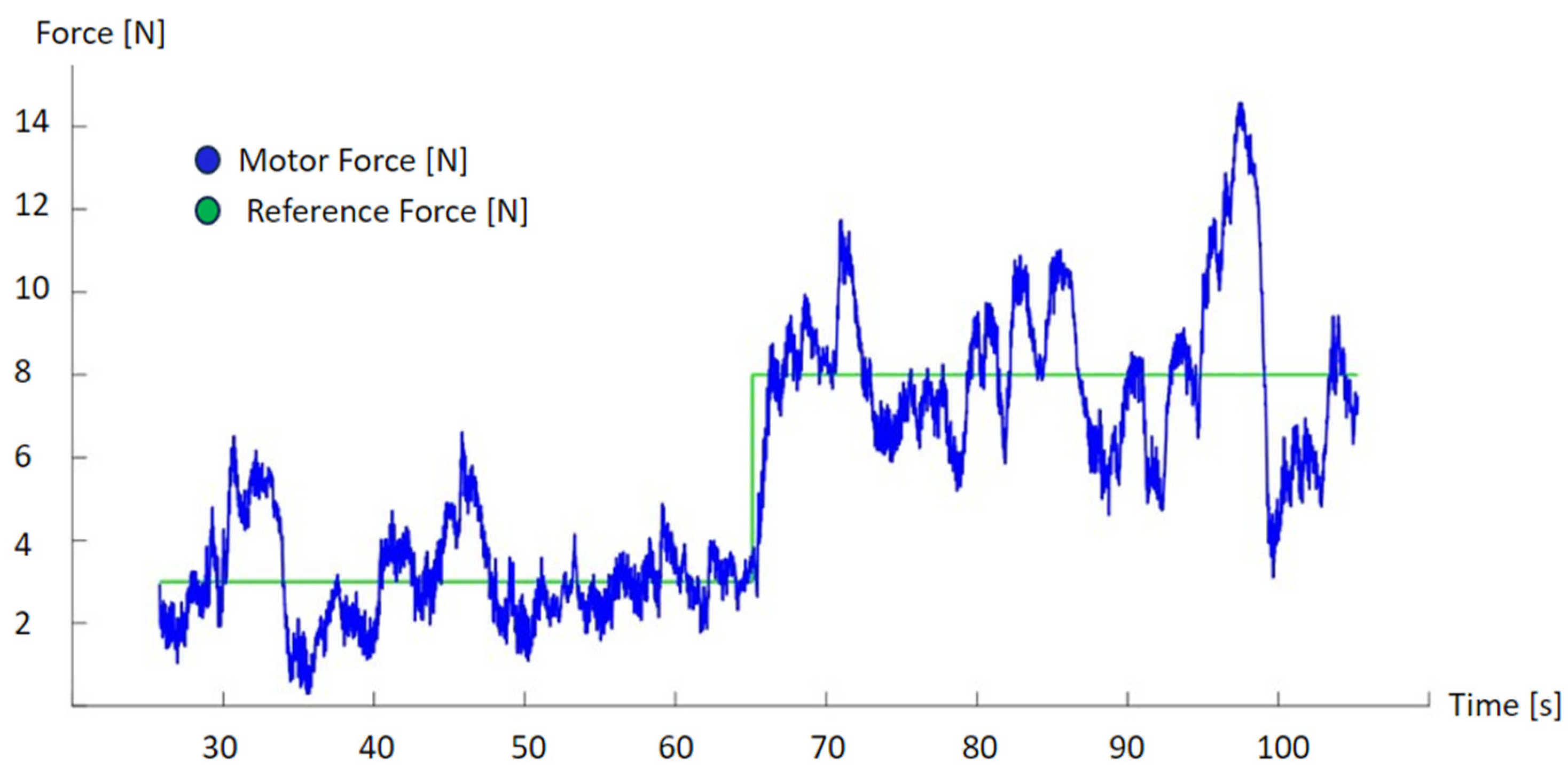
Some trials were performed in the laboratory to properly tunned the controllers.
Figure 4 shows the performance of the force exerted by the motor when is applied a step to the reference. As we can see, the information provided by the force sensor is oscillating on the reference. This oscillation is due to the interaction with the person, the different movement speed is directly transformed to an incremental variation of the reflected force. This is the usual behavior of a force control loop that maintain a reflected force.
2.4. Participants
The inclusion criteria established for the selection of patients were as follows: musculoskeletal injury of the upper limb, presenting no pathology for which rehabilitation treatment is contraindicated, and being over 18 years of age. Patients that presented any of the following exclusion criteria were not admitted to the study: cognitive impairment that prevented the understanding of simple commands, neurological lesion affecting the upper extremity, dermatological lesion of the upper extremity preventing the use of device material and any other type of injury impeding the use of the device.
This protocol was approved by the Research Ethics Committee of the Rey Juan Carlos University Institute. The ethical principles for medical research in humans from the Declaration of Helsinki were followed. All subjects signed the informed consent prior to participation. The trials were carried out at the Getafe Clinical Center (Madrid, Spain).
2.5. Intervention
The clinician adjusted the controller parameters for each patient according to the predefined exercise, in this case, the shoulder rotation movement. These parameters define the shoulder rotation range and the stress of the reflected force on the patient, which is in an interval of 5N to 15N. Additionally, it was verified that the pulley was in the same plane as the patient's forearm. This alignment makes movements more comfortable as the forces directly oppose shoulder rotation with no movement at the elbow.
Each session lasted 15 minutes and consisted of repeating a cycle of external rotation and internal rotation 30 times, returning to the starting position. These cycles were carried out with the patient sitting down, in a chair with a backrest and with their feet on the floor. Initially, the arm was positioned close to the body with a 90° elbow flexion, and from this position, the rotation movements were performed.
Figure 5 shows a patient during a session.
To carry out the rotation movements, the patient started the external rotation movement from the initial position up to the maximum rotation they were able to achieve. In this half cycle, the patient exerted a force greater than that generated by the motor. In the second half of the cycle, when the patient returned to the initial position, performing an internal rotation, the movement was in the opposite direction and the force applied by the motor was greater than that exerted by the patient.
Figure 6 shows the limits of the cyclical movement. The force reflected by the actuator was fixed throughout the cycle and was measured by the load cell. This load cell was located close to the patient's hand to obtain an accurate estimate of the force reflected to the patient; otherwise, the forces caused by friction might affect the information processed by the controller.
2.6. Outcome measures
The range of motion (ROM) of shoulder external rotation was measured using a double-armed 360° goniometer. The patients were in a supine position with the humerus abducted at 90° and elbow flexed at 90°. The measurements were performed twice and averaged for subsequent analysis [
9].
3. Results
3.1. SUS and statistical analysis
System Usability Scale (SUS): this questionnaire was developed by Brooke [
10] as a system usability tool and has been widely used in the evaluation of a variety of systems. The SUS provides a quick and reliable tool for measuring the usability of a device. It is a short questionnaire that is simple to answer; a final score is provided with an interpretation based on a well-established reference standard. It has excellent reliability (0.85). It consists of a 10-item questionnaire with five response options, from strongly agree (score of 5) to strongly disagree (score of 1). There are five positive and five negative statements, which are presented in alternation. The odd numbered questions (Q1 “I think I would use this device frequently”, Q3 “I think the device was easy to use”, Q5 “The functions of this device are well integrated”, Q7 “I imagine that most people would learn to use this device very quickly”, and Q9 “I feel safe using this device”) are positive questions, and the recorded scores are the original scores subtracted by 1. The even numbered questions (Q2 “I find this device unnecessarily complex”, Q4 “I think I would need help from a person with technical knowledge to be able to use this device”, Q6 “I think the device has a lack of consistency”, Q8 “I find the device very difficult to use”, and Q10 “I needed to learn many things before being able to use this device”) are negative questions with the recorded scores being subtracted from 5. Once the results for the ten questions are treated, the score of each question is added and the result is multiplied by a factor of 2.5. The score of the SUS, therefore, ranges from 0 to 100, where a higher score means better usability, with a threshold of 68 determining the usability of the device [
11].
Our statistical analysis was performed using the SSPS statistical software system (SSPS Inc., Chicago, IL; version 27.0). A descriptive analysis of all the variables was performed. The results were expressed as average and standard deviation and median and interquartile range. The normal distribution of the variables was verified using the Shapiro-Wilk test. The hypothesis that the variables did not have a normal distribution was accepted, given the results of this test, the verification of each variable's histograms, and the sample size. We used the Wilcoxon test, a non-parametric test for related samples. The statistical analysis was performed with a confidence level of 95%, and so the significant values were those whose p was < 0.05.
3.2. Clinical tests
The sample consisted of 12 shoulder rehabilitation sessions with 11 patients (5 men and 6 women) with different shoulder pathologies that limited their range of shoulder mobility. In one of the patients, both shoulders were treated. One patient performed two sessions for the rehabilitation of both shoulders, while the rest performed only one rehabilitation session. The patients’ ages ranged from 35 to 66 years (54.92 ± 3.16 years).
Table 1 shows the data of the patients that participated in the testing of the device.
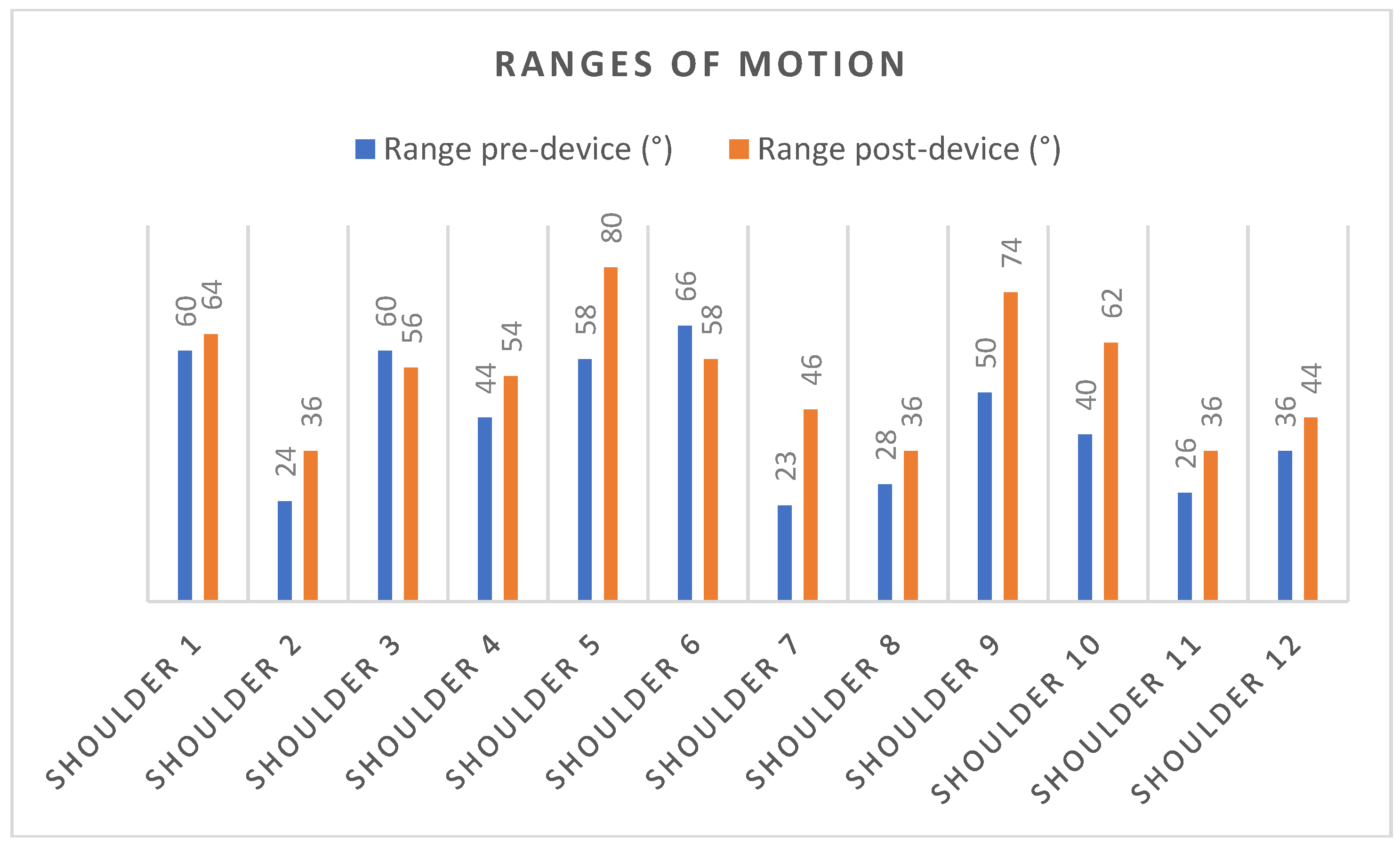
The analysis shows statistically significant changes for the ROM of shoulder external rotations. The mean and standard deviations of the ROM of shoulder external rotations were 42.91±4.53º for the pre-intervention measurements and were 53.88±4.26º for the post-intervention measurements.
Figure 7 and
Table 2 shows data and range of movement of the patient during the rehabilitation sessions.
The patients’ scores on the SUS questionnaire ranged from 65 to 97.5, with an average score of 82.70 ± 9.21, suggesting a high degree of acceptance. These scores are higher than 68, indicating that this device can be rated "excellent" in the acceptability range.
Table 3 shows the means of the scores obtained in each question. Questions Q1, 3, 5, 7, and 9 were positive questions and the averages obtained in these questions were above 4. It is worth noting that Q1 "I think I would use this device frequently" presented an average score of 4.75±0.59 and Q9 "I feel safe using this device" showed an average score of 4.91 ± 0.27. Meanwhile, questions Q2, 4, 6, 8, and 10 were negative questions. The mean scores in these questions were 1, except in Q2 "I find this device unnecessarily complex" which had a mean score of 2.5±1.55 and Q4 "I think I would need help from a person with technical knowledge to be able to use this device" with a mean score of 2.91±1.49.
4. Discussion
The present study shows the use of an active device for shoulder rehabilitation based on a force control architecture. It aimed to rehabilitate, in a single treatment session, external rotation movements of the shoulder in patients in which this was limited by musculoskeletal injuries. It also describes the patients’ acceptance of the device, and results show a great approval by patients after the first trial.
Shoulder rotator cuff injuries include tendinopathies and partial or complete tendon ruptures, mostly related to the supraspinatus tendon [
12]. Exercise is a key component of rehabilitation for soft tissue injuries of the shoulder. Evidence recommends exercise-based interventions to reduce pain and increase shoulder function. The evidence also suggests that progressive shoulder strengthening and stretching are effective for the management of rotator cuff injuries [
13]. Exercises should be introduced as early as possible. However, in clinical practice, the actual referral rate to physiotherapists is low, due to the lack of access to publicly funded physiotherapy in health care systems [
14].
Waiting for outpatient physiotherapy services has shown to have mixed results on clinical and health system outcomes. The review by Deslauriers et al. [
15] suggests the possible detrimental effects of waiting on pain, disability, quality of life, and psychological symptoms in persons with shoulder disorders. There is also evidence of higher healthcare utilization and costs for patients who wait longer before physiotherapy services [
15]. The effects of waiting caused by lack of access to physiotherapy services might be mitigated by the implementation of exoskeletons with which more patients can be treated at the same time with a lower number of physiotherapists. Rehabilitation robots also can significantly reduce the burden of therapists by providing repetitive and precise therapy to people with upper limb impairment for a long duration of time [
16].
Most of the exoskeletons for the rehabilitation of the upper limb available on the market are designed to improve flexion and abduction, and not external rotation, which is a fundamental movement in the performance of activities of daily living. Rotation movements are fundamental for carrying out activities below the horizontal and for executing coordinated movements with the hand for an individual to locate themselves in space [
17]. Addition, most studies have been carried out in stroke [
18,
19].
With a single treatment session, this active device for shoulder rehabilitation based on force control, was found to significantly increase the external rotation movement of the shoulder in the patients that used it. The mean and standard deviations of the ROM of shoulder external rotations of the pre-intervention measurements were 42.91±4.53º, and 53.88±4.26º for the post-intervention measurements. In addition, the patients reported high levels of acceptance of the device; their scores on the SUS questionnaire ranged from 65 to 97.5, with an average score of 82.70 ± 9.21, indicating a high degree of acceptance. These very promising results were obtained with minimal hardware and a user-friendly interaction with the patient.
Robotics and haptic technologies, such as force control, and real-time signal processing, were found to have an effective contribution in upper-limb rehabilitation. There are many examples of complex exoskeletons [
20,
21], and robot-like equipment applied to upper-limb rehabilitation [
22]. This equipment can perform a great variety of movements but are specifically programmed for executing rehabilitation tasks. It is also required to design the proper patient interface in order to fix, or attach, the patient’s upper limb to the robot structure. This kind of solutions have the advantage of being able to adapt to different rehabilitation activities.
However, this device is in line with a new generation of compact and simple rehabilitation equipment that are portable and easy for use by the patient [
23], in contrast with the classical robotic solutions previously mentioned. The main advantage of this kind of solutions is the simplicity and cost-effective solution. Only one degree of freedom is enough for performing the shoulder rehabilitation, and this equipment can be adapted for horizontal and vertical rotations. Moreover, the reduce size of the device allows transporting it to the rehabilitation workspace, that can be located in the clinic, or at patient home.
This prototype is currently improved in order to provide more functionalities to clinicians for performing new rehabilitation exercises, and also developing software for a better characterization of the rehabilitation sessions.
5. Conclusions
A compact and cost-effective prototype for shoulder rehabilitation is described in this paper. The most important features are the simplicity of the hardware and its effectiveness in rehabilitation exercises. The equipment is designed for repeating a shoulder rotation while reflecting a force on the patient hand. This exercise allows for muscle activation, while also increasing the range of shoulder movement.
This device allows patients to perform exercises for rehabilitation sessions that are an ideal complement to clinician manipulation. The preliminary results suggest that use of this device and incorporation of such equipment into rehabilitation services could be of great help patients in their rehabilitation process and for physiotherapists in applying their therapies.
Author Contributions
Conceptualization, all authors; methodology, all authors; rehabilitation device design and development David Pont-Esteban, Juan Carrillo, Paul Espinosa, Manuel Ferre, and Miguel Ángel Sánchez-Urán; clinical validation, Alicia Cuesta-Gómez, Isabel M. Alguacil-Diego; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Universidad Rey Juan Carlos (N-20130081).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The Authors would like to thank all the patient and clinicians that participated in the validation test of the exoskeleton.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Notarnicola A; Covelli I; Macchiarola D; Bianchi FP; Cassano GD; Moretti B. The Efficacy of Temperature-Controlled High-Energy Polymodal Laser Therapy in Tendinopathy of the Shoulder. J Clin Med. 2023. 12(7):2583. [CrossRef]
- Chun Lung So B; Cheuk Ting Lau S; Yu Kwok W; Hon Ting Tse D; Shing Man S. Investigating The Association Between Supraspinatus Tendon Abnormality, Shoulder Pain and Isokinetic Strength in Elite Swimmers: A Cross-Sectional Study. J Sports Sci Med. 2023. 22(1); pp. 17-27. [CrossRef]
- Langer JS; Sueoka SS; Wang A. The importance of shoulder external rotation in activities of daily living: improving outcomes in traumatic brachial plexus palsy. J Hand Surg Am. 2012 Jul;37(7):1430-6. [CrossRef]
- Kim JH; Min YK; Kim DY; Park JH; Seo YC; Seo WS. Influence of joint volume on range of motion after arthroscopic rotator cuff repair. BMC Musculoskelet Disord. 2023. 24(1):201. [CrossRef]
- Swinton PA; Shim JSC; Vladimirovna Pavlova A; Moss R; Maclean C; Brandie D; Mitchell L; Greig L; Parkinson E; Tzortziou Brown V; Morrissey D; Alexander L: Cooper K. What are small, medium and large effect sizes for exercise treatments of tendinopathy? A systematic review and meta-analysis. BMJ Open Sport Exerc Med. 2023 Feb 27;9(1):e001389. [CrossRef]
- Delgado P; Yihun Y. Integration of Task-Based Exoskeleton with an Assist-as-Needed Algorithm for Patient-Centered Elbow Rehabilitation. Sensors. 2023. 23(5):2460. [CrossRef]
- T. Proietti, E. Ambrosini, A. Pedrocchi and S. Micera. Wearable Robotics for Impaired Upper-Limb Assistance and Rehabilitation: State of the Art and Future Perspectives. IEEE Access, 2022. 10, pp. 106117-106134. [CrossRef]
- J. Podobnik, M. Mihelj and M. Munih. Upper limb and grasp rehabilitation and evaluation of stroke patients using HenRiE device. 2009 Virtual Rehabilitation International Conference, 2009, pp. 173-178. [CrossRef]
- Norkin, C. & White, D.J. Manual de Goniometría. Evaluación de la movilidad articular. 5.a ed. Barcelona: 2019, Editorial Paidotribo.
- Brooke, J. SUS-A quick and dirty usability scale. Usability Eval. Ind. 1996. 189, pp. 4–7.
- Brooke, J. SUS: A retrospective. J. Usability Stud. 2013, 8, pp. 29–40.
- Rotator cuff injuries include tendinopathies and partial or complete tendon ruptures, most related to the supraspinatus tendon.
- Abdulla SY; Southerst D; Côté P; Shearer HM; Sutton D; Randhawa K; Varatharajan Y; Wong JJ; Yu H; Marchand AA; Chrobak K; Woitzik E; Shergill Y; FergusonB; Stupar M; Nordin M; Jacobs C; Mior S; CarrollLJ; van der Velde G; Taylor-Vaisey A. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man Ther. 2015 Oct;20(5):646-56. [CrossRef]
- Lowry V; LavigneP; Zidarov D; Perreault K; Roy JS; Desmeules F. Knowledge and appropriateness of care of family physicians and physiotherapists in the management of shoulder pain: a survey study in the province of Quebec, Canada. BMC Prim Care. 2023 Feb 16;24(1):49. [CrossRef]
- Deslauriers S; Déry J; Proulx K; Laliberté M; Desmeules F; Feldman DE; Perreault K. Effects of waiting for outpatient physiotherapy services in persons with musculoskeletal disorders: a systematic review. Disabil Rehabil. 2021 Mar;43(5):611-620. [CrossRef]
- Ahmed T; Islam Md R; Brahmi B; Habibur Rahman M. Robustness and Tracking Performance Evaluation of PID Motion Control of 7 DoF Anthropomorphic Exoskeleton Robot Assisted Upper Limb Rehabilitation. Sensors (Basel). 2022 May; 22(10): 3747. [CrossRef]
- Suárez Sanabria N; Osorio Patiño AM. Biomecánica del hombro y bases fisiológicas de los ejercicios de Codman. Rev CES Med. 2013; 27(2):205-217.
- Teasell R, McIntyre A, Viana R, Bateman EA, Murie-Fernandez M, Janzen S, Saikaley M. Developing a framework for utilizing adjunct rehabilitation therapies in motor recovery of upper extremity post stroke. Top Stroke Rehabil. 2023 Jul;30(5):493-500.
- Wu J, Cheng H, Zhang J, Yang S, Cai S. Robot-Assisted Therapy for Upper Extremity Motor Impairment After Stroke: A Systematic Review and Meta-Analysis. Phys Ther. 2021 Apr 4;101(4):pzab010. [CrossRef]
- Kadivar Z, Beck CE, Rovekamp RN, O'Malley MK. Single limb cable driven wearable robotic device for upper extremity movement support after traumatic brain injury. J Rehabil Assist Technol Eng. 2021. [CrossRef]
- Gupta S, Agrawal A, Singla E. Architectural design and development of an upper-limb rehabilitation device: a modular synthesis approach. Disabil Rehabil Assist Technol. 2022. [CrossRef]
- R. O. Hailey et al., "Impact of Gravity Compensation on Upper Extremity Movements in Harmony Exoskeleton," 2022 International Conference on Rehabilitation Robotics (ICORR), Rotterdam, Netherlands, 2022, pp. 1-6. [CrossRef]
- Garzo, J. H. Jung, J. Arcas-Ruiz-Ruano, J. C. Perry and T. Keller, ArmAssist: A Telerehabilitation Solution for Upper-Limb Rehabilitation at Home. IEEE Robotics & Automation Magazine, vol. 30, pp. 62-71, March 2023. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).