Submitted:
25 May 2023
Posted:
26 May 2023
You are already at the latest version
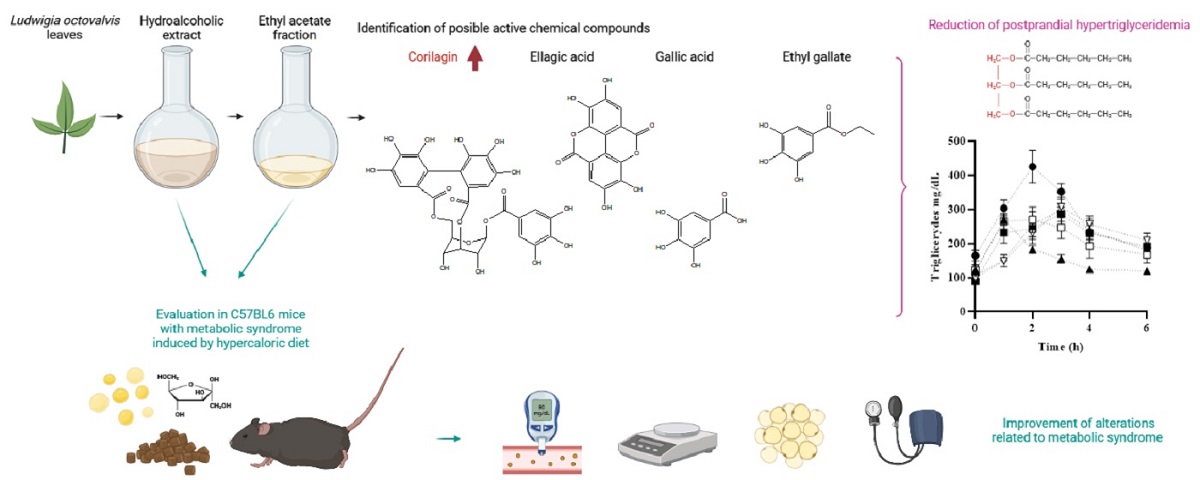
Abstract
Keywords:
1. Introduction
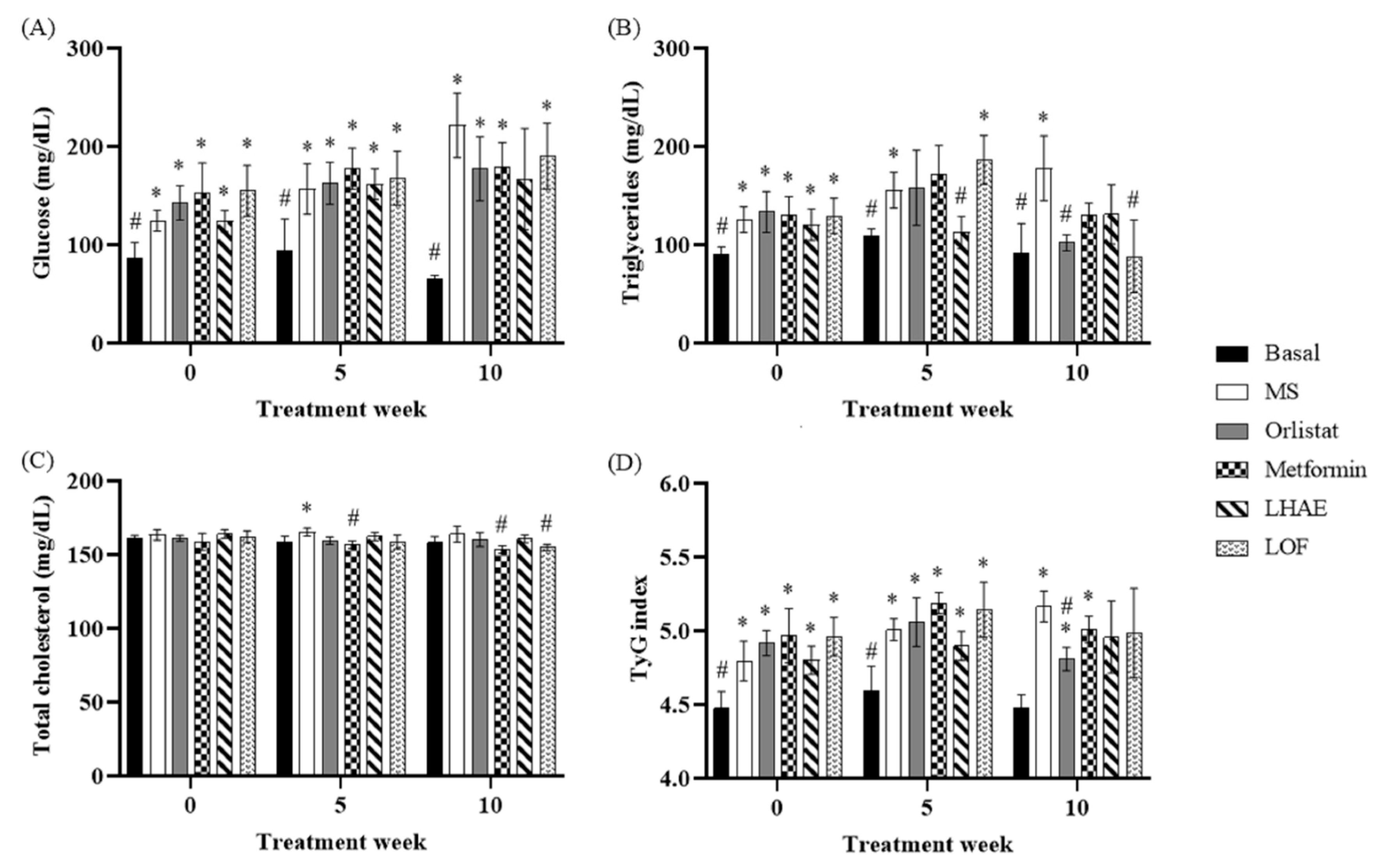
2. Results
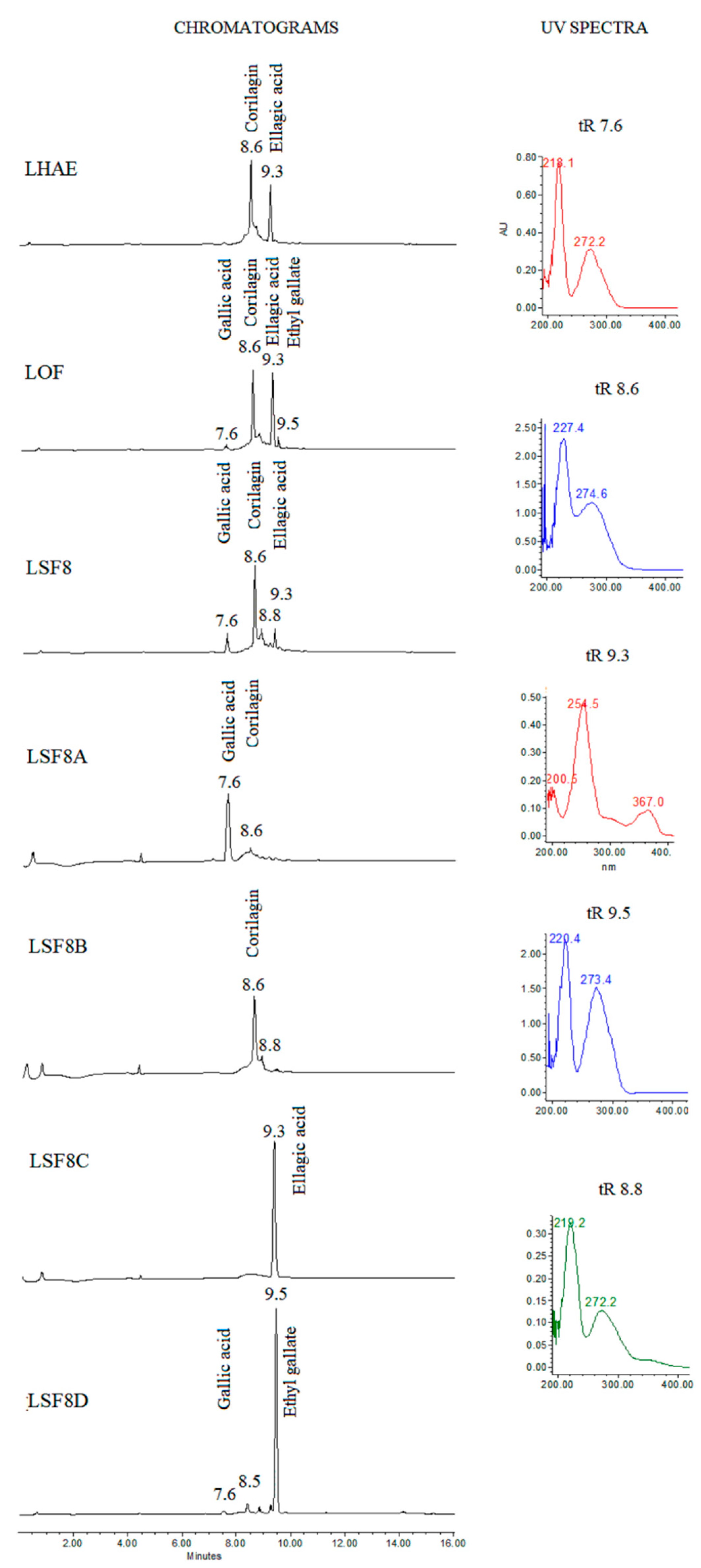
2.1. Phytochemistry
2.2. MS model
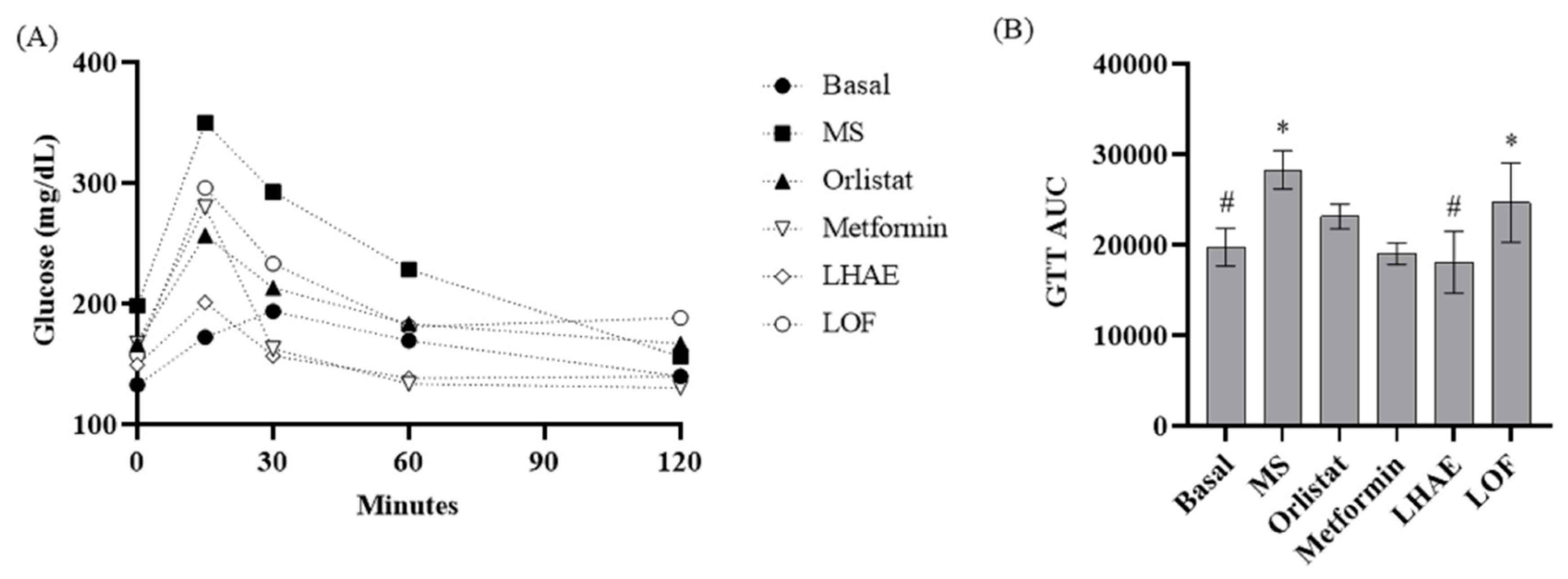
2.2.1. Insulin resistance and glucose metabolism
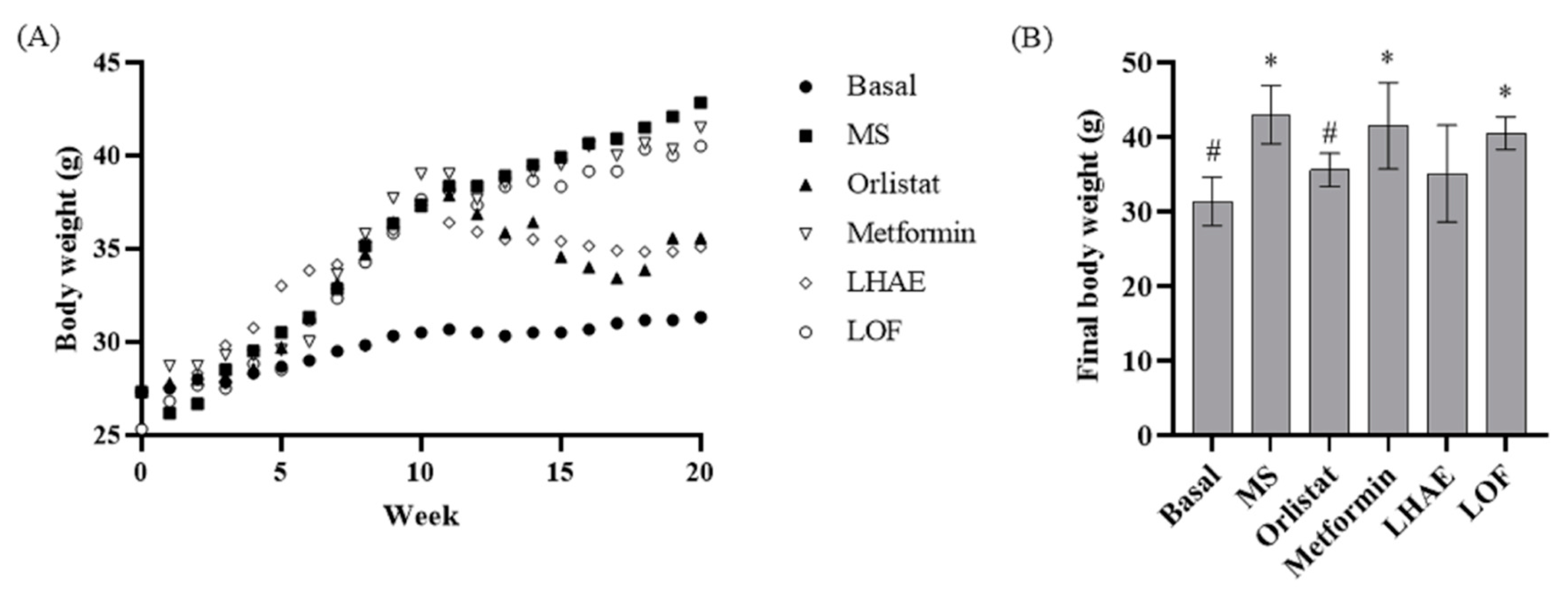
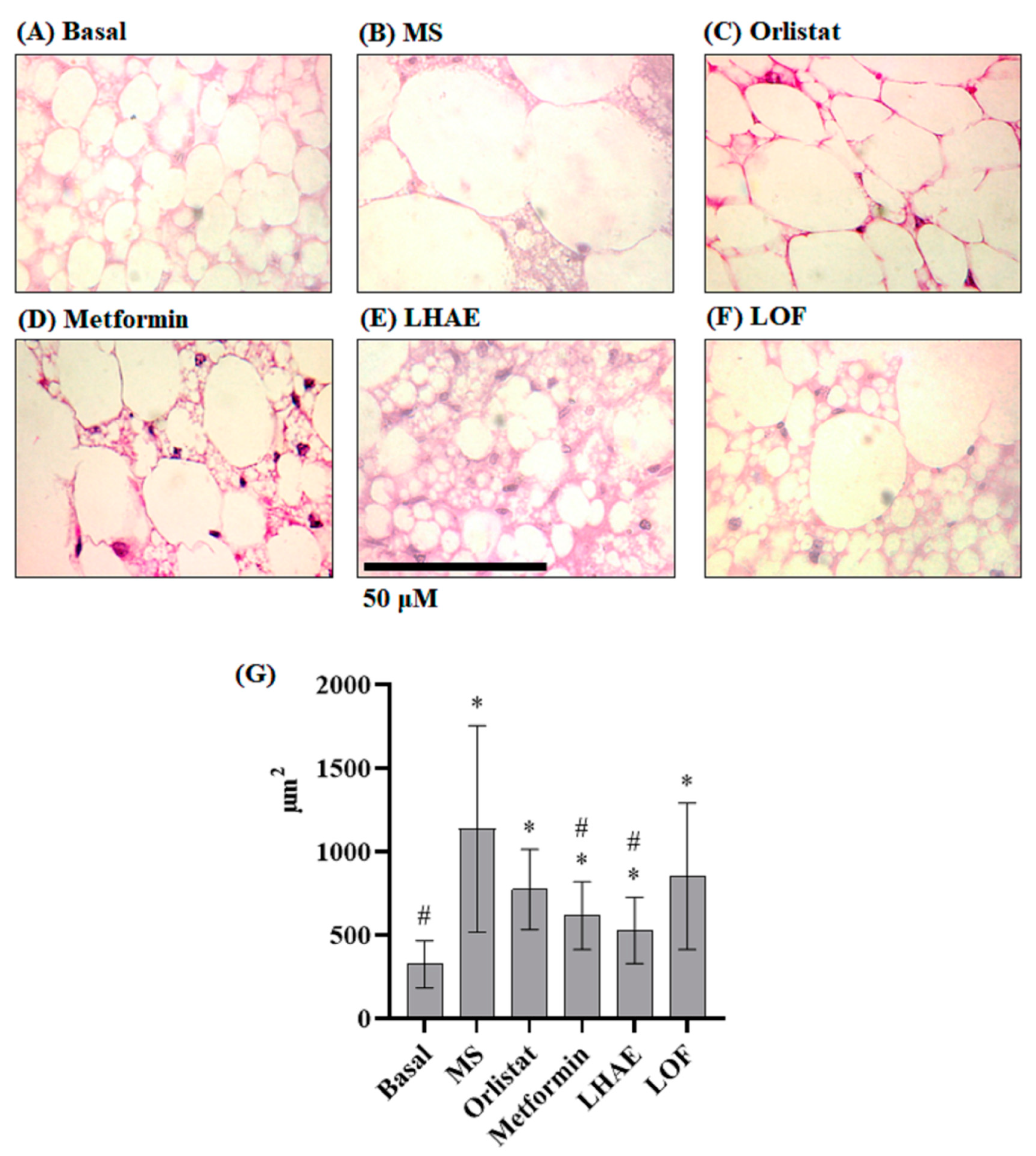
2.2.2. Obesity
2.2.3. Atherogenic dyslipidemia
2.2.4. Hypertension
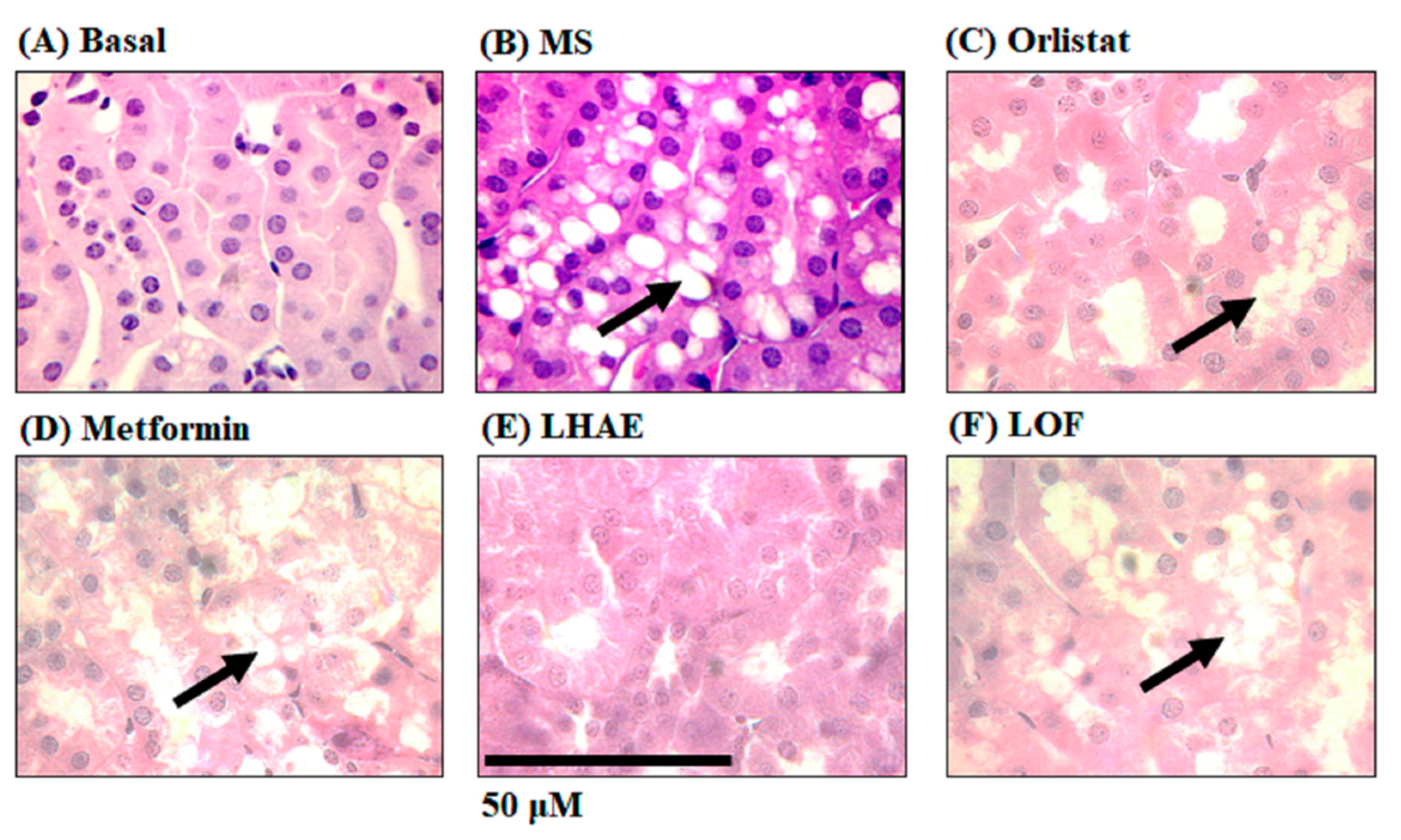
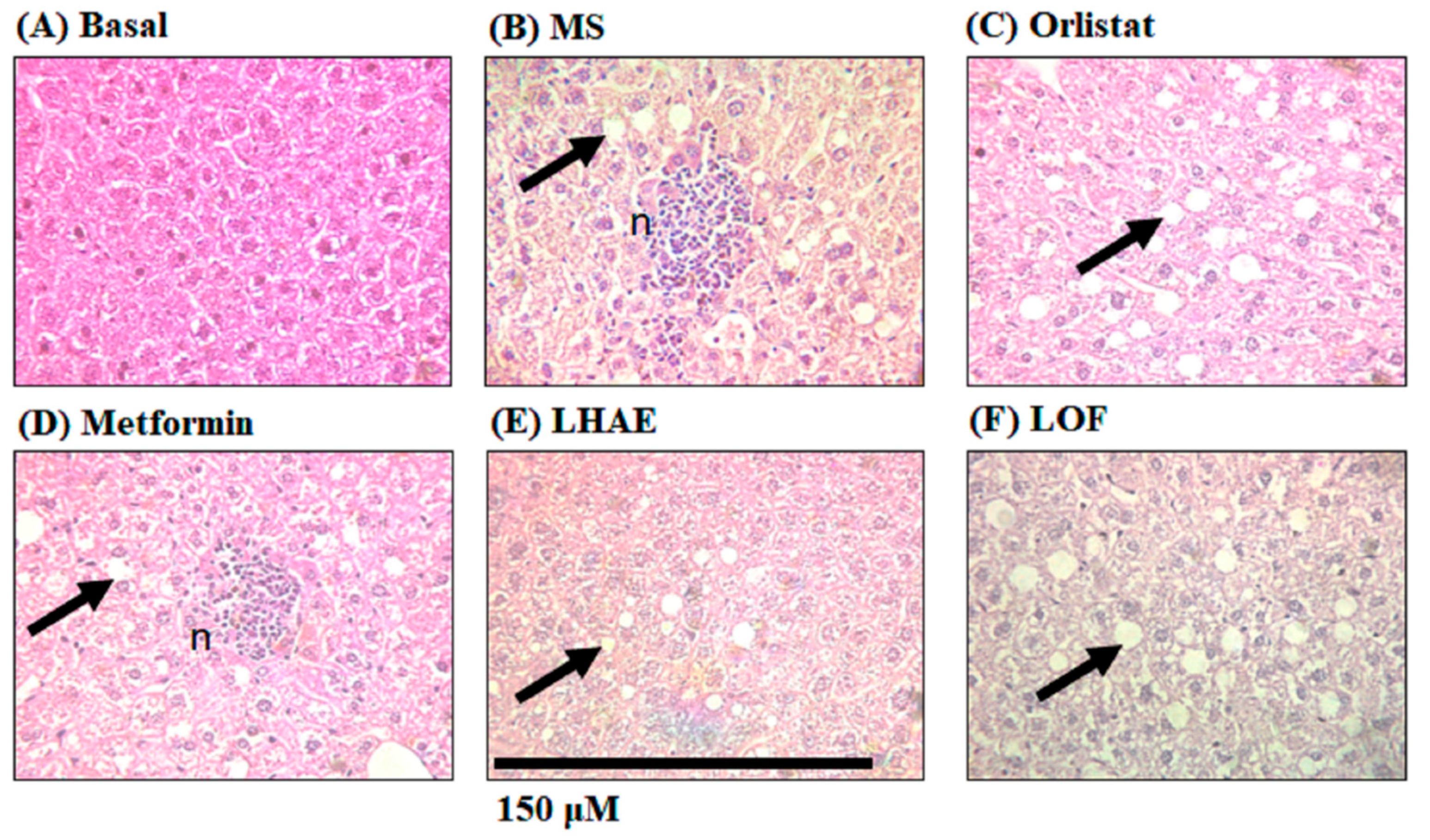
2.2.5. Global damage parameters
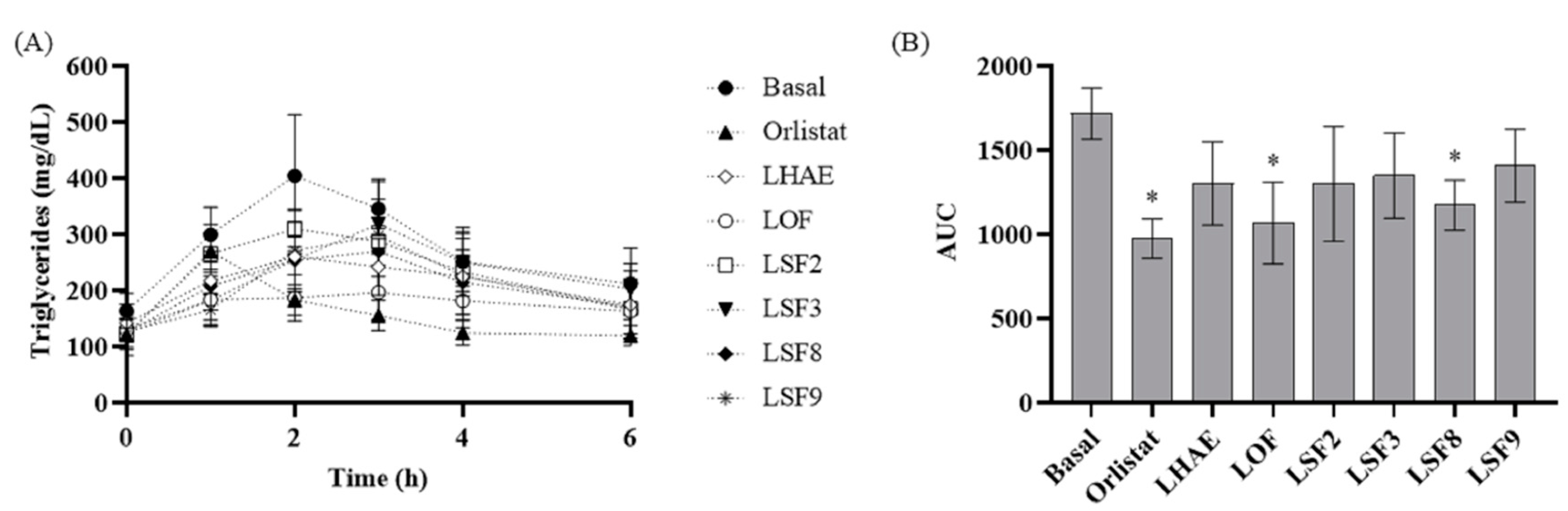
2.3. Postprandial triglyceridemia
3. Discussion
4. Materials and Methods
4.1. Plant material and phytochemical procedures
4.2. Experimental animals and MS induction
4.3. Evaluated parameters in MS model
4.4. Postprandial triglyceridemia
4.5. Data processing and statistical aspects
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Neill, S.; O’Driscoll, L. Metabolic Syndrome: A Closer Look at the Growing Epidemic and Its Associated Pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Barba Evia, J.R. México y El Reto de Las Enfermedades Crónicas No Transmisibles. El Laboratorio También Juega Un Papel Importante. Rev. Latinoam. Patol. Clínica y Med. Lab. 2018, 65, 4–17. [Google Scholar]
- McCracken, E.; Monaghan, M.; Sreenivasan, S. Pathophysiology of the Metabolic Syndrome. Clin. Dermatol. 2018, 36, 14–20. [Google Scholar] [CrossRef]
- Dimitriadis, G.; Boutati, E.; Raptis, S.A. Pathogenesis: The Lipotoxicity and Glucotoxicity Hypothesis in the Metabolic Syndrome and Type 2 Diabetes. In The Metabolic Syndrome at the Beginning of the XXI Century: A Genetic and Molecular Approach; Serrano Ríos, M., Caro, J.F., Carraro, R., Gutiérrez Fuentes, J.A., Eds.; Elsevier, 2005; pp. 271–282. ISBN 8481748927. [Google Scholar]
- Cusi, K. Role of Insulin Resistance and Lipotoxicity in Nonalcoholic Steatohepatitis. Clin Liver Dis 2009, 13, 545–563. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, V.A.; Raghavan, V A Parthasarathy, S. Biochemical Basis and Clinical Consequences of Glucolipotoxicity: A Primer. Hear. Fail Clin 2012, 8, 501–511. [Google Scholar] [CrossRef]
- Laclaustra Gimeno, M.; Bergua Martínez, C.; Pascual Calleja, I.; Casasnovas Lenguas, J.A. Síndrome Metabólico. Concepto y Fisiopatología [Metabolic Syndrome. Concept and Pathophysiology]. Rev. Española Cardiol. 2006, 5, 3–10. [Google Scholar] [CrossRef]
- Mitra, S.; Karmakar, A.; Mukherjee, A.; Barik, A. The Role of Leaf Volatiles of Ludwigia Octovalvis (Jacq.) Raven in the Attraction of Altica Cyanea (Weber) (Coleoptera: Chrysomelidae). J. Chem. Ecol. 2017, 43, 679–692. [Google Scholar] [CrossRef]
- Khan, M.H.; Yadava, P.S. Antidiabetic Plants Used in Thoubal District of Manipur, Northeast India. Indian J. Tradit. Knowl. 2010, 9, 510–514. [Google Scholar]
- Ramírez, G.; Zavala, M.; Pérez, J.; Zamilpa, A. In Vitro Screening of Medicinal Plants Used in Mexico as Antidiabetics with Glucosidase and Lipase Inhibitory Activities. Evid. Based Complement. Alternat. Med. 2012, 2012, 1–6. [Google Scholar] [CrossRef]
- Ipor, I. Ludwigia Octovalvis (Jacq.) P.H. Raven; van Valkenburg, J.L.C.H., Bunyapraphatsara, N., Eds.; Backhuys: Leiden, Netherlands, 2001. [Google Scholar]
- Murugesan, T.; Sinha, S.; Pal, M.; Saha, B. Review on Phytochemical and Medicinal Aspects of Jussiaea Suferuticosa Linn. Anc. Sci. Life 2002, 21, 205–207. [Google Scholar]
- UNAM Atlas de Las Plantas de La Medicina Tradicional Mexicana Available online:. Available online: http://www.medicinatradicionalmexicana.unam.mx/atlas.php (accessed on 13 June 2019).
- Wu, S.J.; Ng, L.T.; Wang, G.H.; Huang, Y.J.; Chen, J.L.; Sun, F.M. Chlorophyll a, an Active Anti-Proliferative Compound of Ludwigia Octovalvis, Activates the CD95 (APO-1/CD95) System and AMPK Pathway in 3T3-L1 Cells. Food Chem. Toxicol. 2010, 48, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.S.; Lo, J.H.; Yang, J.H.; Wang, H.W.; Fan, S.Z.; Yen, J.H.; Wang, P.Y. Ludwigia Octovalvis Extract Improves Glycemic Control and Memory Performance in Diabetic Mice. J. Ethnopharmacol. 2017, 207, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.S.; Chen, J.Y.; Wang, J.C.; Chen, L.Y.; Lin, C.H.; Hsieh, T.R.; Wang, M.F.; Fu, T.F.; Wang, P.Y. The Anti-Aging Effects of Ludwigia Octovalvis on Drosophila Melanogaster and SAMP8 Mice. Am. Aging Assoc. 2014, 36, 689–703. [Google Scholar] [CrossRef]
- Morales, D.; Ramirez, G.; Herrera-Arellano, A.; Tortoriello, J.; Zavala, M.; Zamilpa, A. Identification of Digestive Enzyme Inhibitors from Ludwigia Octovalvis (Jacq.) P.H. Raven. Evid. Based Complement. Alternat. Med. 2018, 2018, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kadum Yakob, H.; Manaf Uyub, A.; Fariza Sulaiman, S. Toxicological Evaluation of 80% Methanol Extract of Ludwigia Octovalvis (Jacq.) P.H. Raven Leaves (Onagraceae) in BALB/c Mice. J. Ethnopharmacol. 2012, 142, 663–668. [Google Scholar] [CrossRef]
- Ghareeb, M.A.; Sobeh, M.; El-Maadawy, W.H.; Mohammed, H.S.; Khalil, H.; Botros, S.; Wink, M. Chemical Profiling of Polyphenolics in Eucalyptus Globulus and Evaluation of Its Hepato–Renal Protective Potential against Cyclophosphamide Induced Toxicity in Mice. Antioxidants 2019, 8, 4–7. [Google Scholar] [CrossRef]
- Li, X.; Deng, Y.; Zheng, Z.; Huang, W.; Chen, L.; Tong, Q.; Ming, Y. Corilagin, a Promising Medicinal Herbal Agent. Biomed. Pharmacother. 2018, 99, 43–50. [Google Scholar] [CrossRef]
- Im, S.H.; Wang, Z.; Lim, S.S.; Lee, O.H.; Kang, I.J. Bioactivity-Guided Isolation and Identification of Anti-Adipogenic Compounds from Sanguisorba Officinalis. Pharm. Biol. 2017, 55, 2057–2064. [Google Scholar] [CrossRef]
- Qing, W.; Li, W.; Xiaolin, Y.; Yuanming, S.; Yueming, J. Polyphenols from Longan Leaf and Their Radical-Scavenging Activity. Int. Proc. Chem. Biol. Environ. Eng. 2013, 50, 180–185. [Google Scholar] [CrossRef]
- Yan, J.; Yang, X.W. Studies on the Chemical Constituents in Herb of Ludwigia Octovalvis. China J. Chinese Mater. medica 2005, 30, 1923–1926. [Google Scholar]
- Morales, D.; Ramirez, G.; Herrera-Arellano, A.; Tortoriello, J.; Zavala, M.; Zamilpa, A. Identification of Digestive Enzyme Inhibitors from Ludwigia Octovalvis (Jacq.) P.H.Raven. Evid. Based Complement. Alternat. Med. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Murugesan, T.; Rao, B.; Sinha, S.; Biswas, S.; Pal, M.; Saha, B. . Anti-Diabetic Activity of Jussiaea Suffruticosa Extract in Rats. Pharm. Pharmacol. Commun 2000, 6, 451–453. [Google Scholar] [CrossRef]
- Nandini, H.S.; Naik, P.R. Action of Corilagin on Hyperglycemia, Hyperlipidemia and Oxidative Stress in Streptozotocin-Induced Diabetic Rats. Chem. Biol. Interact. 2019, 299, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Lv, B.; Li, X.; Wang, H. Corilagin Decreases Insulin Resistance in Polycystic Ovary Syndrome Rat Model through Regulating AMPK/GSK3β Pathway. Transl. Cancer Res. 2020, 9, 3242–3248. [Google Scholar] [CrossRef]
- Perera, A.; Ton, S.H.; Moorthy, M.; Palanisamy, U.D. The Insulin-Sensitising Properties of the Ellagitannin Geraniin and Its Metabolites from Nephelium Lappaceum Rind in 3T3-L1 Cells. Int. J. Food Sci. Nutr. 2020, 71, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, Y.; Nishii, S.; Zaima, N.; Moriyama, T.; Kawamura, Y. Ellagic Acid Improves Hepatic Steatosis and Serum Lipid Composition through Reduction of Serum Resistin Levels and Transcriptional Activation of Hepatic Ppara in Obese, Diabetic KK-Ay Mice. Biochem. Biophys. Res. Commun. 2013, 434, 486–491. [Google Scholar] [CrossRef]
- Amor, A.J.; Gómez-Guerrero, C.; Ortega, E.; Sala-Vila, A.; Lázaro, I. Ellagic Acid as a Tool to Limit the Diabetes Burden: Updated Evidence. Antioxidants 2020, 9, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S.; Goyal, R.K. Cardioprotective Effects of Gallic Acid in Diabetes-Induced Myocardial Dysfunction in Rats. Pharmacol. Res. 2011, 3, 239–245. [Google Scholar] [CrossRef]
- Montani, J.P.; Carroll, J.F.; Dwyer, T.M.; Antic, V.; Yang, Z.; Dulloo, A.G. Ectopic Fat Storage in Heart, Blood Vessels and Kidneys in the Pathogenesis of Cardiovascular Diseases. Int. J. Obes. 2004, 28, 58–65. [Google Scholar] [CrossRef]
- Ferrara, D.; Montecucco, F.; Dallegri, F.; Carbone, F. Impact of Different Ectopic Fat Depots on Cardiovascular and Metabolic Diseases. J. Cell. Physiol. 2019, 234, 21630–21641. [Google Scholar] [CrossRef]
- Henderson, G.C. Plasma Free Fatty Acid Concentration as a Modifiable Risk Factor for Metabolic Disease. Nutrients 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.L.; Yen, K.Y.; Kiso, Y.; Hikino, H. Antihepatotoxic Actions of Formosan Plant Drugs. J. Ethnopharmacol. 1987, 19, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; Haczeyni, F.; Chitturi, S. Pathogenesis of NASH: How Metabolic Complications of Overnutrition Favour Lipotoxicity and pro-Inflammatory Fatty Liver Disease. Adv. Exp. Med. Biol. 2018, 1061, 19–44. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G.; Langsted, A.; Freiberg, J.J. Nonfasting Hyperlipidemia and Cardiovascular Disease. 2009, 328–335.
- The Plant List Available online:. Available online: http://www.theplantlist.org/ (accessed on 14 December 2017).
- Ramirez, G.; Zamilpa, A.; Zavala, M.; Perez, J.; Morales, D.; Tortoriello, J. Chrysoeriol and Other Polyphenols from Tecoma Stans with Lipase Inhibitory Activity. J. Ethnopharmacol. 2016, 185, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Botello-Amaro, A.C.; González-Cortazar, M.; Herrera-Ruiz, M.; Román-Ramos, R.; Aguilar-Santamaría, L.; Tortoriello, J.; Jiménez-Ferrer, E. Hypoglycemic and Hypotensive Activity of a Root Extract of Smilax Aristolochiifolia, Standardized on N-Trans-Feruloyl-Tyramine. Molecules 2014, 19, 11366–11384. [Google Scholar] [CrossRef] [PubMed]
- Falholt, K.; Lund, B.; Falholt, W. An Easy Colorimetric Micromethod for Routine Determination of Free Fatty Acids in Plasma. Clin. Chim. Acta 1973, 46, 105–111. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Simental-Mendía, L.E.; González-Ortiz, M.; Martínez-Abundis, E.; Ramos-Zavala, M.G.; Hernández-González, S.O.; Jacques-Camarena, O.; Rodríguez-Morán, M. The Product of Triglycerides and Glucose, a Simple Measure of Insulin Sensitivity. Comparison with the Euglycemic-Hyperinsulinemic Clamp. J. Clin. Endocrinol. Metab. 2010, 95, 3347–3351. [Google Scholar] [CrossRef]
- Gamboa-Gómez, C.; Salgado, L.M.; González-Gallardo, A.; Ramos-Gómez, M.; Loarca-Piña, G.; Reynoso-Camacho, R. Consumption of Ocimum Sanctum L. and Citrus Paradisi Infusions Modulates Lipid Metabolism and Insulin Resistance in Obese Rats. Food Funct. 2014, 5, 927–935. [Google Scholar] [CrossRef]
- Murray, I.; Sniderman, A.D.; Cianflone, K. Mice Lacking Acylation Stimulating Protein (ASP) Have Delayed Postprandial Triglyceride Clearance. J. Lipid Res. 1999, 40, 1671–1676. [Google Scholar] [CrossRef]
| Parameter | Basal | MS | Orlistat | Metformin | LHAE | LOF |
|---|---|---|---|---|---|---|
| MAT (mg/g) | 2.7 ± 2.2# | 22.8 ± 8.2* | 10.2±3.5# | 20.0±7.9* | 11.0±5.6# | 17.1±5.3* |
| SAT (mg/g) | 14.5 ± 12.1# | 93.1 ± 17.1* | 38.5±14.3 | 71.0±16.4* | 64.4±19.4* | 67.5±12.5* |
| PAT (mg/g) | 10.9 ± 7.9# | 28.4 ± 8.2* | 19.9±3.9 | 23.2±2.4* | 22.2±5.9* | 23.3±3.6* |
| EAT (mg/g) | 26.2 ± 14.4# | 62.8 ± 9.5* | 42.9±3.8 | 51.2±7.8* | 52.7±12.2* | 51.8±11.4* |
| TAT (mg/g) | 54.3 ± 20.5# | 207.1±21.3* | 110.5±23.3 | 165.4±21.4* | 150.2±40.8*# | 159.7±20.2* |
| BAI | 2.61 ± 1.42# | 6.26±0.97* | 4.31±0.41*# | 5.12±0.79* | 5.25±1.21* | 5.18±1.14* |
| LTG (mg/g) | 396.5 ± 26.1# | 864.3±31.7* | 604.6±95.9 | 575.6±155.0 | 502.3±183.6 | 733.9±202.7 |
| HTG (mg/g) | 1488 ± 124# | 2820±542* | 1921±201# | 1795±95# | 901±434# | 976±393# |
| KTG (mg/g) | 1083 ± 670# | 2841±374* | 2249±909 | 2195±306 | 965±384# | 2681±471 |
| SBP (mmHg) | 89.9 ± 11.9# | 110.3±16.7* | 87.4±7.1# | 86.8±6.4# | 84.3±11.5# | 87.8±9.2# |
| DBP (mmHg) | 61.6 ± 7.9# | 73.7±8.5* | 53.0±5.0*# | 60.2±11.3# | 65.6±3.3 | 57.5±9.1# |
| FFA (μg/mL) | 26.6 ± 5.4# | 41.9 ± 5.1* | 32.1±3.8 | 41.3±6.0* | 28.1±2.8# | 33.9±6.1 |
| AST (U/L) | 91.7 ± 34.2# | 227.0 ± 84.4* | 73.1±37.7# | 207.9±113.6# | 74.2±23.4# | 68.3±50.6# |
| ALT (U/L) | 25.6 ± 19.9 | 39.2 ± 18.4 | 15.0±7.1 | 32.1±12.1 | 13.0±10.2 | 10.8±1.2 |
| Group | Diet | Treatment in 10 to 20 weeks |
|---|---|---|
| Basal | Standard | Vehicle (5% tween 20) |
| MS | Hypercaloric | Vehicle (5% tween 20) |
| Orlistat | Hypercaloric | Orlistat 40 mg/kg |
| Metformin | Hypercaloric | Metformin 100 mg/kg de peso |
| LHAE | Hypercaloric | L. octovalvis hydroalcoholic extract 25 mg/kg |
| LOF | Hypercaloric | L. octovalvis organic fraction 25 mg/kg |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





