1. Introduction
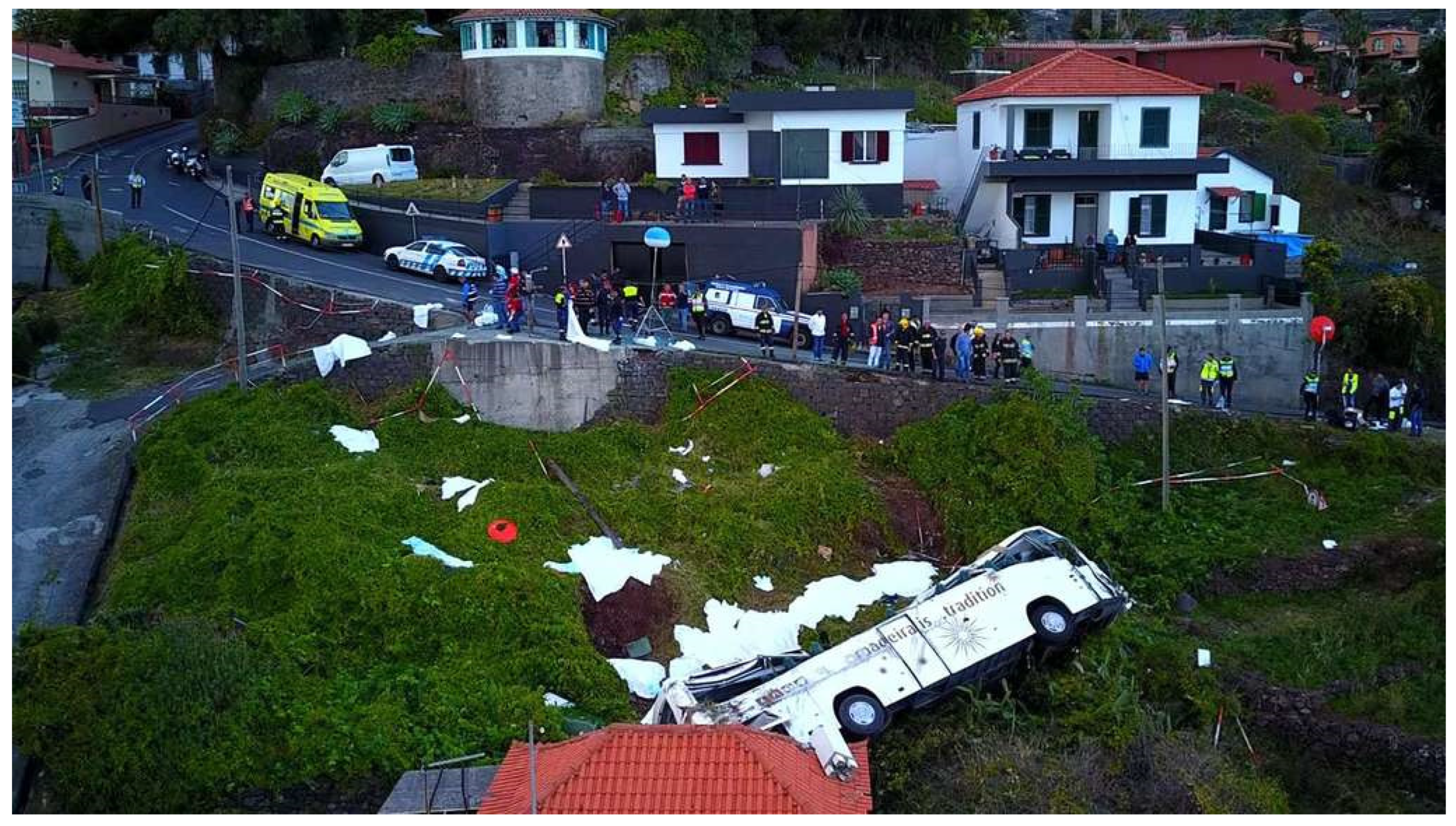
On April 17, 2019, a coach (Irizar type) carrying a German civilian tour group crashed in Caniço in the Portuguese island of Madeira. The bus crashed 200 m after the start on a steeply sloping road on a left-hand bend falling down a steep embankment. It overturned sideways and collided with the roof of a house before stopping (Picture 1). The roof of the bus was significantly deformed and partially ripped open. Only five passengers were found in the vehicle, the others were presumably ejected. Seat belts are compulsory in buses in Portugal. The cause of the accident is said to be excessive speed. A technical defect in the vehicle has been ruled out. Fatally injured were 28 of the 56 bus occupants. Subsequently, another patient died in hospital. All the deceased were German citizens. The injured bus driver and the tour guide were Portuguese.
All the injured patients were taken to the hospital Serviço Regional de Saúde da Região Autónoma da Madeira (SESARAM, EPRAM) in Funchal, the capital of Madeira, after receiving pre-hospital care.
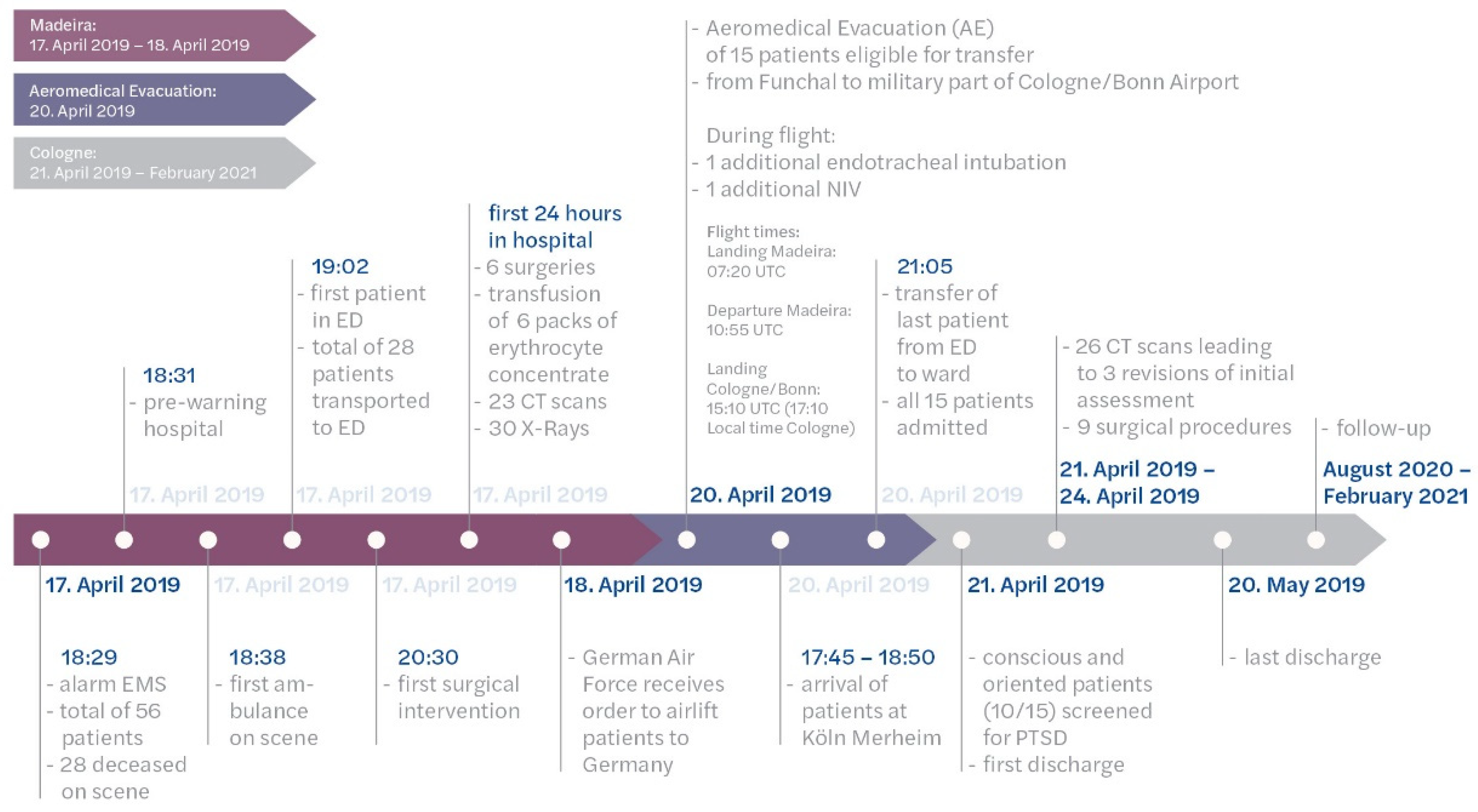
The German Air Force was assigned to repatriating the surviving patients following a visit by Germany's Foreign Minister, Heiko Mass, on April 18, 2019.
The repatriation of 15 transferable patients was done airborne using the Aeromedical Evacuation (AE) capability in the German Air Force Airbus A310-304 Multi-Role Transport Tanker (MRTT) to Cologne Bonn Airport in Germany on April 20, 2019 [
17]. This date was also a Germany-wide holiday as part of the Christian Easter celebration. For further inpatient care, the patients were transferred to the Cologne Merheim Hospital, a Level1trauma center 13 km away from the airport. The first inpatient admission was scheduled on 18:00 on the day of transfer.
This study describes medical and logistical challenges in delivering ATLS-based management in a mass casualty event requiring repatriation and reports on quality of life outcomes two years after the accident.
Picture 1.
aerial view accident site (©Getty Images).
Picture 1.
aerial view accident site (©Getty Images).
2. Materials and Methods
Madeira
Prehospital deployment details (staff) and data from the initial clinical care (ATLS-compliance of care, injuries identified) in Madeira were collected through a structured interview with the medical directors of prehospital care and of the hospital. Also the required staff was documented.
Description Aeromedical Evacuation German Air Force
The analysis of the AE was based on an evaluation of the intensive care transport records used during flight (based on recommendations of the German Interdisciplinary Association for Intensive Care and Emergency Medicine [DIVI], version 1.1, including all vital signs, medical treatments). These records were started by the attending intensive care physician after the patient was handed over by the emergency service at the airport of embarkation until the patient was handed over to the emergency service at the airport of debarkation. Data were checked for plausibility and, if necessary, corrected in accordance with information in the form fields or in-flight data of the intensive care transport record. Potential channels of in-flight communication were critically appraised on data security and all-time availability. Staff requirements were documented.
Cologne
Patient charts, digital physician documentation, emergency department software, and the Madeira workgroup's lesson learned protocol were reviewed for data collection. Information of medical assessment and management, additional injuries identified and staffing involved were extracted.
The patients who were temporally and spatially oriented (10 of 15) were screened for psychological trauma sequelae on the day after admission using a standardized screening tool (Freiburg Screening Questionnaire, FSQ) in order to define the need of talk therapy [
1].
Follow-up
To assess health-related quality of life (HRQoL) and individual patient satisfaction, the patients were given a 12-item Short-Form Health Survey (SF-12) and five additional questions evaluating their satisfaction with treatment, work capacity, and trauma-related medical treatment. For the evaluation of the SF-12, the corresponding German reference collective was used. Thus, the HRQoL assessment concept of the TraumaRegister DGU® was implemented [
2].
Patients were contacted by mail for the first time 15 months after the accident. A reminder was sent after 18 and 21 months. In case of ambiguity, telephone contact was established after the patient gave written consent.
Statistical analysis
Statistical analysis was performed using SPSS statistical software (version 24; IBM Inc., Armonk, NY, USA). Data between groups were compared using the Mann-Whitney U test for continuous variables and Fisher's exact test for categorical variables, unless indicated otherwise.
A significance level of p < 0.05 was applied. Data were presented as medians with IQRs for continuous variables and as percentages for incidence rates.
3. Results
3.1. Patients
The median patient age was 69 years (interquartile range [IQR] 67–73), with nine female and six male patients. Ten (66%) had chronic pre-existing illnesses (four arterial hypertension; three, coronary artery disease; three insulin dependent diabetes mellitus; one hypothyroidism; one myocardial infarction; and one basilar artery stenosis). Five were on anticoagulant premedication (antiplatelet and oral anticoagulants). No patient had pre-diagnosed osteoporosis.
3.2. Madeira Perspective
The ambulance service was alerted at 18:29 local time. The first ambulance, with an emergency medical technician, arrived at 18:38. Later, 3 physicians and 21 ambulances transferred to the scene. Firefighters performed technical rescue. Transport time from the accident scene to the hospital was 10 min. In total, 28 patients were transported. Apart from four endotracheal airway securing measures, no invasive measures were carried out at the scene. At 18:31, mass casualty pre-warning was given to the only available hospital, the Serviço Regional de Saúde da Região Autónoma da Madeira (SESARAM, EPRAM). The hospital was a Level III Trauma Center with 18 intensive care unit (ICU) beds, 2 trauma bays, and 11 operating rooms.
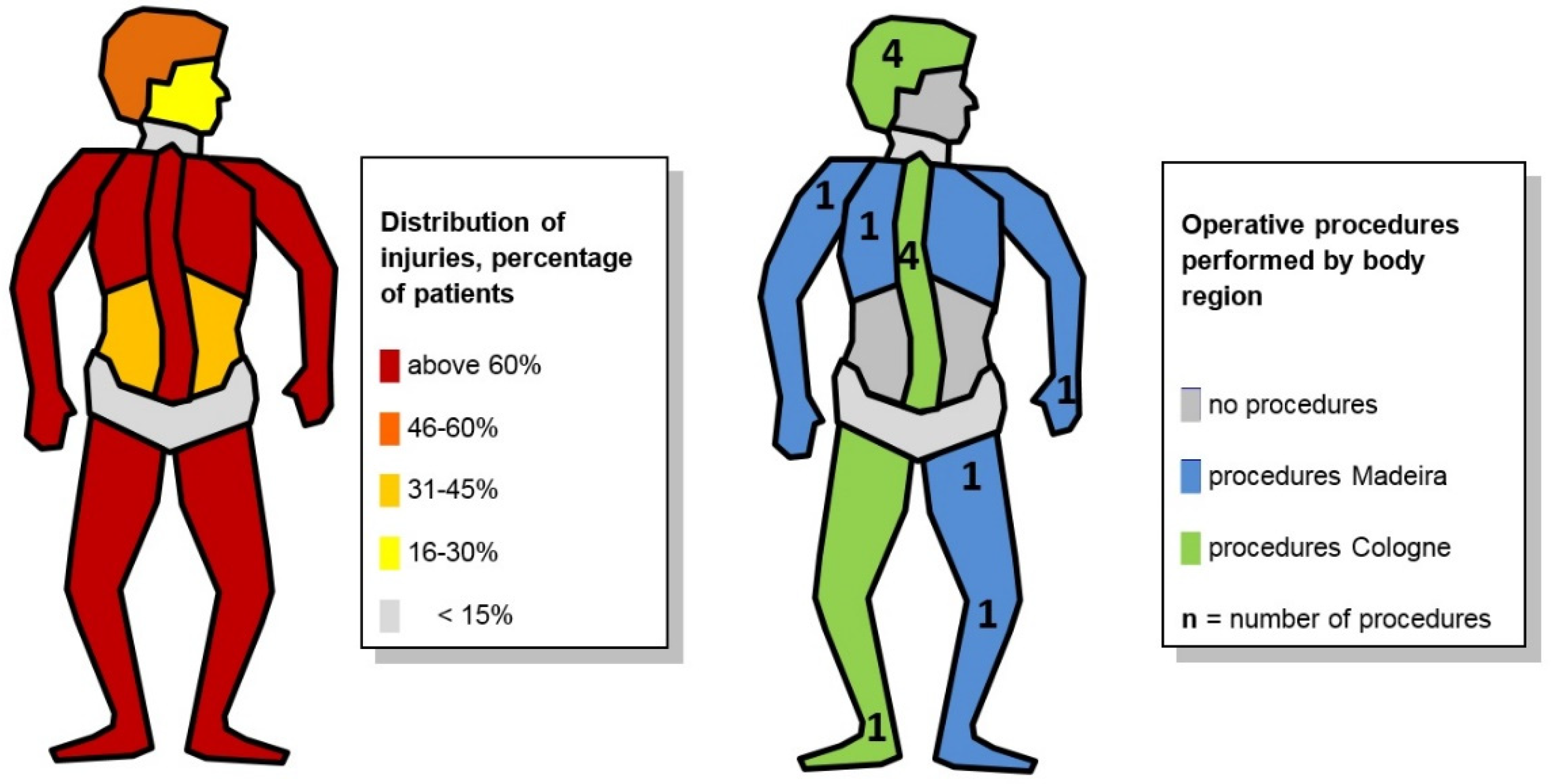
All 28 prehospital patients were transported to this hospital. At 19:02, the first patient reached the emergency department. At 19:25, the first ICU admission took place and at 20:30, the first surgery. At 23:30, the last patient was admitted to the ward. In the first 24 h, 6 surgeries, 6 red blood cell transfusions, 23 computed tomography (CT) scans, and 30 radiographs were performed. Cross-sectional imaging was available in the emergency department. The following injury patterns were identified:
- -
Orthopedic trauma to limbs and pelvis: multiple cases
- -
Head trauma: one patient with severe traumatic brain injury died in the ICU, and another had severe craniofacial trauma
- -
Thoracic trauma: two patients had pulmonary contusions and hemothorax
- -
Abdominal trauma: one patient with traumatic duodenal laceration was laparatomized
The initial staffing of 18 physicians, including 9 surgeons and 4 anesthesiologists, and 21 nurses was augmented during the course by 9 surgeons, 20 nurses, and other personnel, such as psychologists, social workers, and administrative staff. The surgical specialties represented were abdominal, orthopedic trauma, cardiothoracic, neurological (head and spine), vascular, and plastics. The staff were trained in the standard trauma course formats like ATLS.
All 28 patients received a full initial assessment consisting of primary and secondary survey with adjuncts within the first 24 hours after admission.
3.3. AE Perspective
Three days after the accident patients were taken over at Madeira Airport by the crew of the A310-304 MRTT from the local ambulance service and prepared for air transport on the same day. Of the 15 patients, one was intubated and ventilated, while the remaining 14 were spontaneous breathing and conscious. Initially, median blood pressure was 136/75 mmHg, heart rate was 76 bpm (IQR 65-80), and peripheral oxygen saturation was 95.5% (IQR 92,0%-98,8%). Six of the patients had a peripheral venous cannula (PVC, venous access), and one had a central venous catheter (CVC). Another had an arterial line for measuring blood pressure (AA). Three other patients recieved a PVK and one an AA in-flight. Seven needed supplemental oxygen during the flight since their spontaneous breathing was maintained, and one received non-invasive Continuous Positive Airway Pressure (CPAP) support. Another had to be intubated and ventilated during the flight due to worsening pulmonary conditions and respiratory exhaustion. In Cologne, the median blood pressure was 135/80 mmHg and the heart rate was 80 bpm (IQR 70-85). There were no significant changes in vital signs during the flight (p > 0.05). The patients were under the care of the medical staff of the AE flight for a median of 5 h (min: 4 h, max. 7 h) from the takeover in Madeira until the handover to the local rescue service in Cologne.
Figure 1
3.4. Cologne perspective
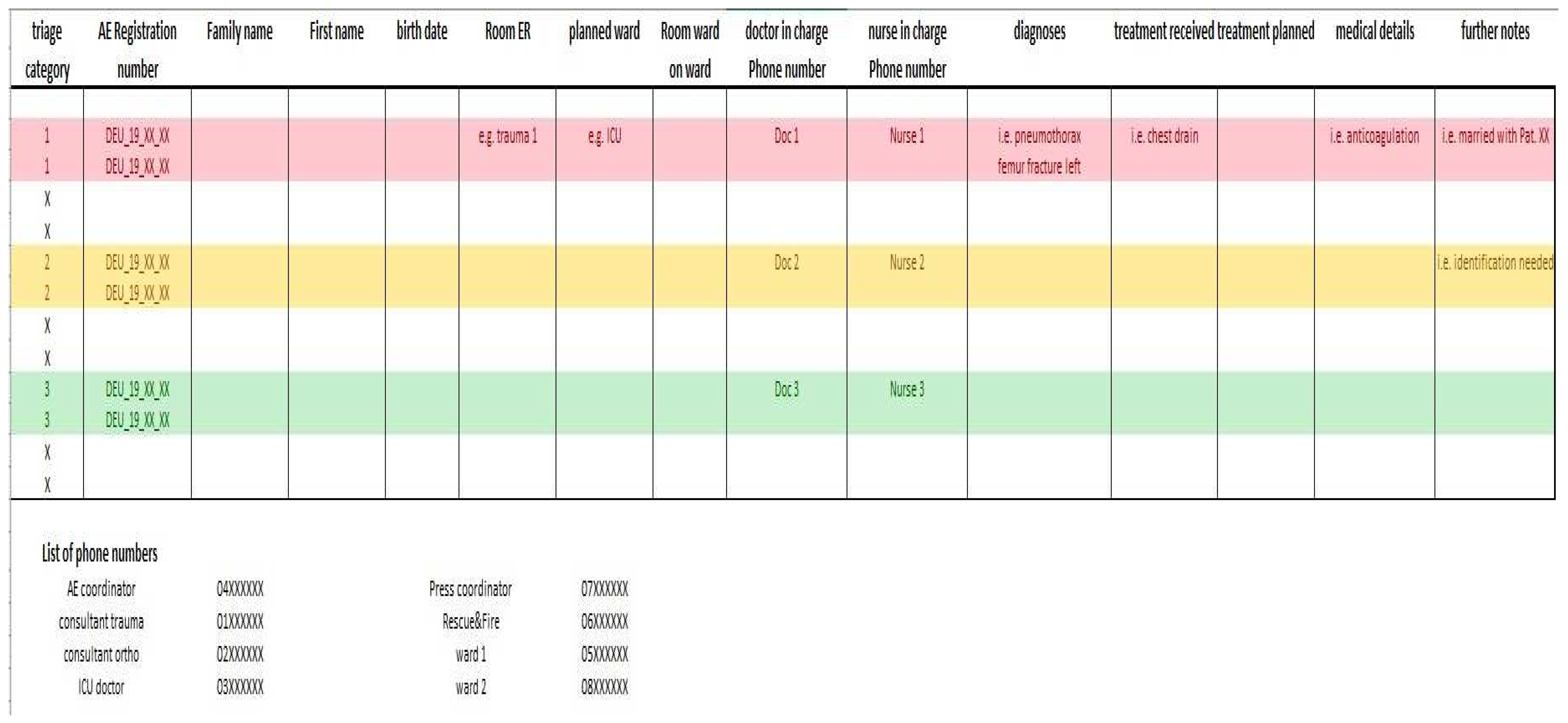
The receiving hospital received patient data (number, age, triage category, known injury pattern, and therapy given and ongoing) 24 h before AE. The team on call in the trauma department (one consultant, one fellow, and one resident) was augmented 2 h before pre-planned admission time by the night shift team. Together with the hospital management team, seven trauma doctors were present (one director, two consultants, two fellows, and two residents). For each patient, the responsible physician, nurse, admission location in the emergency department, and ward room were defined pre-arrival. Patients of the red (1) and yellow (3) triage categories were treated in the emergency department with one responsible physician per category. Patients in the green category were treated in the consultation area of the traumatology clinic (1 resident per 6 patients). This distribution was graphed with contact details and communicated in a briefing to the whole team 1.5 h before the first patient’s arrival.
Figure 2 The director and consultants were not scheduled in patient care, but had coordinating tasks (one triage on arrival and one planning further diagnostics and therapy after admission). At no time was the hospital de-registered as a Level 1 trauma center for regular patients.
The first patient arrived at 17:45 and the last patient at 18:50. The patients in the red and yellow categories arrived at the clinic between 18:00 and 18:40. The last patient was transferred from the admission rooms to the ward at 21:05. The patients were transferred to the wards only with a treatment plan approved by the consultant.
The one patient intubated during flight was triaged in the red category on admission being in the yellow category before. The median Injury Severity Score ISS was 10.0 (IQR 8.0–18.0), 5 patients ISS > 16).
In the second hospital phase in Germany in total 82 radiological images were prepared (56 x-rays, 26 CT scans). That adds up to around 5.5 images per patient transferred. Imaging can be divided into two phases. In the first 48h – the “diagnostic” phase- 57% of the CT scans (n = 15) and 48% of x-rays (n = 27) were taken in order to identify all relevant injuries. In the second phase - the re-assessment phase – imaging was used to control operative results and conservative healing processes (for example: 17 x-rays of the chest).
Additional CT diagnosis indicated stabilization of unstable spine fracture (AO B1 fractures, "Chance-like") in four patients. In three injuries, the primary assessment of fracture stability was revised, and one fracture were captured in the admission survey (third survey following ATLS) for the first time. Osteosynthesis was also performed on a distal fibula (AO C2), and a soft tissue injury to the head was treated by plastic surgery using vacuum-assisted closure therapy and swing flaps. No emergency surgeries were performed on the day of admission. Surgical treatment was performed in the first four days post-admission.
Figure 3.
Of the evaluated patients, 80% (8 out of 10) showed an increased risk for post-traumatic stress disorder (PTSD). Talk therapy based on the concept of somatic experience (SE) according to P. Levine was started in individual consultations with these patients. SE is reportedly suitable for the reduction of the development of PTSD after civilian trauma [3, 4]. Poor FSQ scores and the mental component of the SF-12 at the follow up showed no significant correlation (p = 0.121).
Four patients spend in median 5 days in the intensive care unit (IQR 1–21). In general, hospital stay lasted 11 days (median, IQR 10–18). All but one patient were discharged home.
The identification of one patient had to be revised since language barrier and delirium probably caused a wrong identification in Madeira.
3.5. Follow-up patients
Follow-up for 14 of 15 patients (93.3%) was done during a median follow-up period of 16 months (IQR 16–21). One patient died of a brain tumor unrelated to the accident. Compared with the German SF-12 reference, the median physical component score of the SF-12 was 49.7 (IQR 33.9–51.8, median difference -5.4 [IQR -17.1–0.33]) and the median mental component score, 50.7 (IQR 42.3–54.9), with a median difference of 0.7 (IQR -7.7–4.8). The patients expressed satisfaction with the treatment outcome. HRQoL was rated lower compared to pre-accident conditions. Of the patients, 53% (8/15) were still receiving medical treatment (6 by physiotherapist and 3 by psychologists, one receives both), and 47% (7/15) reported relevant accident-related limitations.
4. Discussion
The Advance Trauma Life Support (ATLS) concept developed by the American College of Surgeons for the systematic, priority-oriented primary care of serious injured patients, includes repeated surveys of a patient at different times. In the primary survey, life-threatening injuries are to be identified and remedied (Madeira). The secondary survey as a part of the initial assessment should identify additional threats to life or limb and is used to identify all injuries sustained (Madeira). While the third survey should monitor the course of injuries identified in the primary and secondary survey (Cologne) [
5,
6]. Resource-related transfer of patients should not be delayed by measures at any time. Following ATLS standards is able to reduce preventable mortality [
7].
From the compilation of the different perspectives of care and the temporal processing of the individual injury histories, six relevant key findings emerged that should be used in future AE missions.
Pre-hospital and clinical care in Madeira showed a structured approach and clear communication. This was based on the high level of specific training, especially Advanced Trauma Life Support (ATLS) and Medical Response to Major Incidents & Disasters (MRMI) training, of the medical staff.
As enough trained personnel was available quickly in the emergency room, performing the primary surveys was unproblematic and secondary surveys were partially started but not fully finished (missing cross-sectional imaging in stable patients).
In Germany, ATLS was continued for every patient by a detailed tertiary survey. The task of this survey was to recognize transport-related deterioration of known injuries, to critically review treatment concepts and to identify all unknown injuries.
In the injured collective stability was reassessed in a relevant number of the spinal fractures (75%, 3/4) and one unstable spinal injury was newly identified. The other fractures had cross-sectional imaging before transfer. To avoid spinal cord injury, the correct assessment of the stability of a spinal fracture is of the highest priority, especially as the assessment has immediate implications for the transport section (EnBloc positioning, supine position). It is therefore recommended to use international valid fracture classification systems (AOSpine thoracolumbar spine injury classification system), as these have a high interobserver reliability even among inexperienced users [8, 9]. This is particularly required when advanced diagnostics for final stability assessment (CT imaging) have not yet been completed, or digital imaging and communications if images are not available for assessment [10-13]. The classification provides modifiers (M1) for these unclear situations [
9]. In case spinal stability can not been assessed in the primary or secondary survey patients should be treated like having unstable injuries. Therefore have spine immobilization for transfer. (
1st key finding)
Precise knowledge of the trauma mechanism (multiple rollovers of the vehicle with flexion-distraction and possible spinal rotation) and the individual risk of injury in the specific collective are also useful for the secondary care hospital [
14].
The stresses of flight (hypoxia, gravitational forces, barometric pressure changes, thermal changes, vibration, humidity, noise, and fatigue) can worsen the clinical condition of a patient during airborne AE transport [
15]. Therefore, invasive measures become necessary while the patient is still in flight or directly upon admission to the destination hospital. In particular, elderly patients with pre-existing conditions and thoracic trauma have an increased risk [
16]. As a
2nd key finding, it is recommended to maintain an ICU capacity (respirator) higher than announced and to have additional room options in the emergency department.
Therefore, it is recommended to establish a secure communication channel with destination hospital before the start of the transport which is maintained for the entire transport (3rd key finding).
The patients showed a high risk for PTSD. Early exploration of the patients is recommended. Somatic experience seems to be a valuable tool of early intervention to avoid PTSD at least until time of follow-up. The large number of patients usually exceeds the personnel resources of the receiving hospital, which is why the use of established military resources (PTSD teams) should be assessed (4th key finding).
In order to avoid incorrect identification of patients, it is recommended for each patient to perform a new self-identification after admission to the destination hospital in the patient's native language, if their mental orientation is present (5th key finding).
AE missions in the context of humanitarian aid missions or on behalf of the German government for the transport of German citizens receive relevant media attention and accompaniment. It is advisable to establish structures to manage external communication with relatives and the media. For undisturbed patient care, relatives and media representatives should be looked after in separate rooms by staff of the hospital (6th key finding).
The results need to be interpreted with respect to the retrospective study design. Due to pandemic restrictions a physical examination of participants was not possible hence a self-reporting survey design
5. Conclusions
Almost 2 years after the event, half of the patients still received some form of rehabilitation and almost 50% reported that their quality of life was impaired as a result of an accident. These consequences persist despite the consequent use of ATLS and the considerable use of resources in caring for the patients.
Author Contributions
Conceptualization, S.I. and A.D.; methodology, S.I., T.T., S.S.; software, S.I., S.S.; validation, S.I., S.S., B.B., T.T. and A.D.; formal analysis, T.P.; investigation, S.I., A.D., S.S., M.R., ; resources, B.B., T.T.; data curation, S.I., M.B.; writing—original draft preparation, S.I., S.S., A.D., S.M.; writing—review and editing, S.I.; visualization, S.I., A.D.; supervision, B.B.; project administration, S.I., A.D.; All authors have read and agreed to the published version of the manuscript.
Funding
“This research received no external funding”
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of the Faculty of Medicine, University of Witten/Herdecke, Germany (register number 03/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper if applicable.
Data Availability Statement
Data available on request due to restrictions e.g. privacy or ethical.
Acknowledgments
The authors acknowledge the time your patient spend while answering questions regarding the study. The authors are well aware of the trauma they suffered when losing partners and friends in the horrific accident.
Conflicts of Interest
S.I., T.P. and B.B. are course directors of the ATLS program in Germany. The funders or the national ATLS-board had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- https://www.fr.de/panorama/busunglueck-madeira-fuenf-passagiere-waren-angeschnallt-trotz-gurtpflicht-12205015.html 1. Stieglitz R-D, Nyberg E, Albert M, Frommberger U, Berger M. Entwicklung eines Screeninginstrumentes zur Identifizierung von Risikopatienten für die Entwicklung einer Posttraumatischen Belastungsstörung (PTB) nach einem Verkehrsunfall. Zeitschrift für Klinische Psychologie und Psychotherapie. 2002;31(1):22-30.
- Kamp O, Pfeifer R, Ritschel M, Flohe S, Bieler D. Polytrauma outcome: implementation of health-related quality of life assessment into the German Trauma Registry. European Journal of Trauma and Emergency Surgery. 2019:1-6.
- Brom D, Stokar Y, Lawi C, Nuriel-Porat V, Ziv Y, Lerner K, et al. Somatic Experiencing for Posttraumatic Stress Disorder: A Randomized Controlled Outcome Study. Journal of Traumatic Stress. 2017;30(3):304-12. [CrossRef]
- Andersen TE, Lahav Y, Ellegaard H, Manniche C. A randomized controlled trial of brief Somatic Experiencing for chronic low back pain and comorbid post-traumatic stress disorder symptoms. European Journal of Psychotraumatology. 2017 2017/01/01;8(1):1331108.
- Münzberg M, Mutschler M, Paffrath T, Trentzsch H, Wafaisade A, Walcher F, et al. Level of Evidence Analysis for the Latest German National Guideline on Treatment of Patients with Severe and Multiple Injuries and ATLS. World journal of surgery. 2015 2015/08/01;39(8):2061-7. [CrossRef]
- Henry, S. ATLS 10th edition offers new insights into managing trauma patients. Bulletin of the American College of Surgeons [Internet][published 01 Jun. 2018.
- Navarro S, Montmany S, Rebasa P, Colilles C, Pallisera A. Impact of ATLS Training on Preventable and Potentially Preventable Deaths. World journal of surgery. 2014 2014/09/01;38(9):2273-8. [CrossRef]
- Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai L-Y, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. European Spine Journal. 2013;22(10):2184-201. [CrossRef]
- Kepler CK, Vaccaro AR, Koerner JD, Dvorak MF, Kandziora F, Rajasekaran S, et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. European Spine Journal. 2016 2016/04/01;25(4):1082-6.
- Banaste N, Caurier B, Bratan F, Bergerot J-F, Thomson V, Millet I. Whole-Body CT in Patients with Multiple Traumas: Factors Leading to Missed Injury. Radiology. 2018;289(2):374-83. [PubMed]
- Antevil JL, Sise MJ, Sack DI, Kidder B, Hopper A, Brown CVR. Spiral Computed Tomography for the Initial Evaluation of Spine Trauma: A New Standard of Care? Journal of Trauma and Acute Care Surgery. 2006;61(2):382-7. PubMed PMID: 00005373-200608000-00020.
- Eurin M, Haddad N, Zappa M, Lenoir T, Dauzac C, Vilgrain V, et al. Incidence and predictors of missed injuries in trauma patients in the initial hot report of whole-body CT scan. Injury. 2012 2012/01/01/;43(1):73-7. [CrossRef]
- Bernstein MP, Mirvis SE, Shanmuganathan K. Chance-Type Fractures of the Thoracolumbar Spine: Imaging Analysis in 53 Patients. American Journal of Roentgenology. 2006 2006/10/01;187(4):859-68.
- Chapman J, Bransford R. Geriatric Spine Fractures: an Emerging Healthcare Crisis. Journal of Trauma and Acute Care Surgery. 2007;62(6). [CrossRef]
- Sammito S, Post J, Ritter DM, Hossfeld B, Erley OM. Innereuropäische Aeromedical-Evacuation-Transporte im Rahmen von COVID-19. Der Notarzt. 2020 //12.10.2020;36(05):263-70. Epub 22.07.2020. De. [CrossRef]
- Van Vledder MG, Kwakernaak V, Hagenaars T, Van Lieshout EMM, Verhofstad MHJ, Boonstra O, et al. Patterns of injury and outcomes in the elderly patient with rib fractures: a multicenter observational study. European Journal of Trauma and Emergency Surgery. 2019 2019/08/01;45(4):575-83.
- Maegele M, Gregor S, Steinhausen E, Bouillon B, Heiss M, Perbix W, Wappler F, Rixen D, Geisen J, Berger-Schreck B, Schwarz R; The long-distance tertiary air transfer and care of tsunami victims: Injury pattern and microbiological and psychological aspects; Critical Care Medicine2005, 33(5):p 1136-1140.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).