1. Introduction:
In the Kyrgyz Republic, 2019 was declared the year of digitalization by the government. This initiative aimed to integrate innovative electronic technologies into various sectors, including healthcare. Despite significant progress in controlling tuberculosis (TB) globally, TB remains a major public health challenge in Kyrgyz Republic, where around 5,000 new cases are diagnosed annually [
1]. Effective and systematic anti-tuberculosis treatment is essential for those diagnosed with TB to ensure positive health outcomes. However, there is a need to develop and implement effective systems to track and monitor TB patients and their progress through the healthcare system.
Patient data is used to monitor different aspects of the management of national TB control programs, including identifying delays in treatment initiation. This information helps those responsible for managing the program to improve patient care, by addressing issues related to patient management such as the time between diagnosis and initiation of treatment. By tracking patient outcomes and comparing them to other national programs, program administrators can take the necessary steps to address issues related to patient management. By understanding the duration of treatment episodes and identifying delays in treatment, healthcare professionals can better manage patient treatment outcomes and ensure that the program's resources are used efficiently.
The World Health Organization (WHO) has been encouraging the adoption of digital technologies in the management of TB programs, including electronic registers, since 2015 [
2]. Digital technologies are critical components for creating sustainable health systems and achieving universal health coverage. There are four main areas where electronic technology can contribute to TB control: i) patient care and electronic directly observed therapy, ii) surveillance and monitoring, including health information system management, iii) measuring the burden of TB disease and death, iv) monitoring drug resistance and program management such as stock control, and v) electronic learning [
3].
To support the digitalization initiative in the Kyrgyz Republic, a medical information system (MIS) was developed for tuberculosis services. This system includes an electronic health record (EHR), Laboratory Information System (LIS), and an electronic TB register. The integration of these systems has eliminated the need for entering the same data into several systems, reducing errors and improving data quality. Additionally, this integration has contributed to the timely receipt of results, which could potentially minimize delays in treatment. In penitentiary facilities in Kyrgyz Republic, treatment delays have been reported in around 47% of cases [
4].
Studies have shown that using electronic register systems in low-income countries can have a positive impact on patient care quality, management and planning (Williams & Boren, 2008). Using an electronic TB register can improve the accuracy and completeness of the data recorded for each patient, potentially improving patient outcomes. While it may be expected that changing from a paper-based system to an electronic register system would improve data quality, experience elsewhere has shown that implementing the change can be challenging. The determinants of success (or failure) include ethical, financial, technical, organizational and training-related issues [
5]. Some studies have shown that the quality of the data improves [
6] and the time from diagnosis to treatment initiation of antiretroviral therapy is reduced [
7]. However, others have found that where both paper-based and electronic systems are used in parallel, neither system contains high-quality data [
8]. This further highlights the importance of avoiding duplication of data to ensure reliable information.
The electronic TB register was introduced in Kyrgyzstan in 2021 but has not yet been evaluated. This study aimed to assess the completeness and reliability of the data in both the paper-based records and electronic register and evaluate whether the quality of care indicators had improved since the introduction of the TB Medical Information System.
This study had two objectives.
1. To assess the concordance and completeness of data in both the paper-based and electronic records in patients with drug-sensitive pulmonary TB in two regions of the Kyrgyz Republic who were registered between June 2021 and May 2022.
2. To compare the time from diagnosis to initiation of TB treatment and programmatic TB treatment outcomes in patients with drug-sensitive pulmonary TB in two regions of the Kyrgyz Republic who were registered in the paper-based system between January and December 2019 and in the electronic register system between June 2021 and May 2022, respectively.
2. Materials and Methods
2.1. Study Design
This was a cohort study that utilized secondary data collected routinely by the national TB control program.
2.2. Setting- general and specific
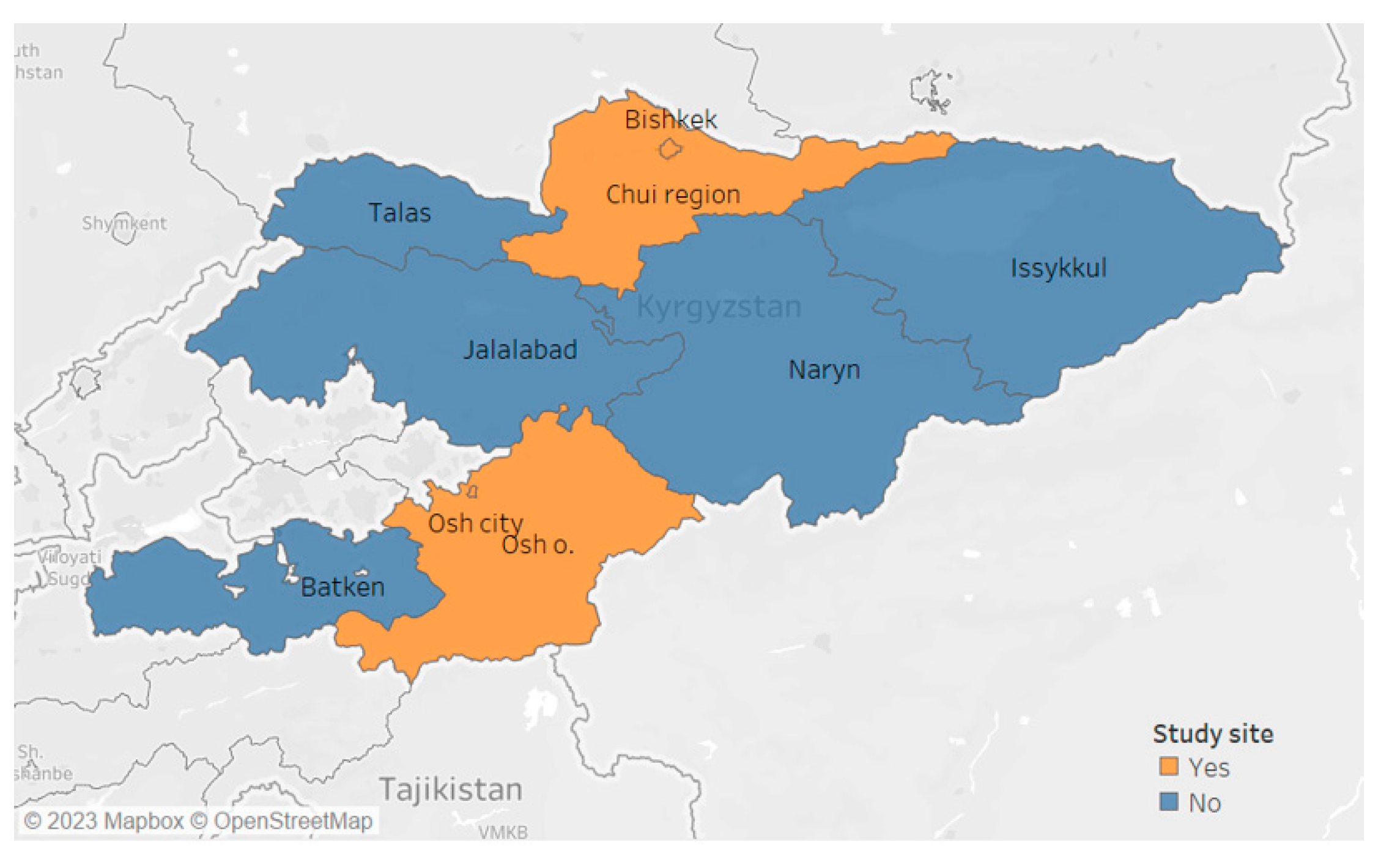
The study was conducted in the Kyrgyz Republic, a landlocked country in north-eastern Central Asia that was formerly part of the Soviet Union. The population is 7 million, with 1.1 million living in the capital city of Bishkek [
9]. The country is divided into seven administrative regions [
10], and its economy is mainly based on agriculture and mining.
The public health system in the Kyrgyz Republic is divided into three levels: central (tertiary) hospitals, regional hospitals, and polyclinics. Provincial and central hospitals are primarily referral centers for complex medical cases.
TB is a significant problem in the country. The number of newly diagnosed tuberculosis patients in the country had been falling for some years up to 2019 when 5,096 cases (78.9 per 100,000 population) were diagnosed. There was a sharp decline in 2020 during the COVID-19 pandemic with only 3,518 new cases registered. This increased slightly to 3,877 in 2021.
Private-for-profit facilities are authorized to provide initial TB diagnosis, but all patients identified with the disease are required to be referred to public facilities for treatment under the National TB program. Inpatient and outpatient TB clinics are also available in each of the seven regions for initial diagnosis.
2.2.1. Specific setting
Patients suspected of having TB were diagnosed using sputum microscopy, GeneXpert MTB/RIF assay, and X-Ray. If a sputum test was positive, the result was recorded in an electronic register. At the inpatient or outpatient TB clinic, a nurse created a new electronic medical record (EMR) for the patient using the TB01 form. Prior to 2020, the information was only entered in the paper-based TB01 record, but since the introduction of the electronic register, the result and patient details are now entered in both the paper-based record and electronic database. Once the necessary information was entered, the nurse sent the patient's electronic database to the attending physician. All further TB follow-up was documented in both the paper-based and electronic registers. Patient registration is usually carried out in the outpatient department registry using an electronic medical information system. The registration is completed by a nurse using the patient's personal number, which is indicated in their passport. After the data is saved, a medical record is automatically generated with the fields previously filled in by the nurse. This card is then sent to the department where the patient will be treated.
2.3. Study population
The study population included patients with drug-sensitive pulmonary tuberculosis in the Chuy and Osh regions of the Kyrgyz Republic and Osh and Bishkek cities, who were registered in the paper-based system between January and December 2019 and in the electronic system between June 2021 and May 2022.
Figure 1.
Regions of Kyrgyz Republic.
Figure 1.
Regions of Kyrgyz Republic.
2.4. Definitions
Paper-based records – the form TB01 used for all outpatients with TB
Electronic TB register – National database using the TB01 form for all patients diagnosed with TB since early 2021
Completeness of the records was measured as the proportion of data fields that were completed out of the total number of data fields for each data variable, and the percentage of data fields completed was also calculated for each variable.
Concordance of records was assessed by comparing the number and percentage of fields with the same value in the two data sources (paper-based and electronic) for specified variables.
2.5. Study sites
Data from two regions and two cities were obtained. The storage site of paper records depended on where the patient had completed treatment. It could be either at the primary level (FMC - family medicine center) or the hospital level. These regions and cities were chosen based on their feasibility and convenience, as they had a high-density population that facilitated data collection. The study was able to collect a significant amount of data in a relatively short period of time.
2.6. Data variables collected for each objective
2.6.1. Data variables are shown in relation to study objectives.
Objective 1: In patients with drug-sensitive pulmonary tuberculosis in the Kyrgyz Republic registered between June 2021 and May 2022, to assess the completeness and concordance of the data. Variables included patient demographic and clinical characteristics and treatment outcomes.
Objective 2: To compare the time from diagnosis to treatment initiation and programmatic TB treatment outcomes among drug-sensitive pulmonary TB patients registered from January to December 2019 (paper-based) and during June 2021 and May 2022 (electronic registration). Variables included dates of diagnosis, and dates of treatment initiation.
2.6.2. Data collection and validation:
The main investigator extracted data for the study from both a sample of the paper records in the health organization archives and from the national electronic TB register.
2.7. Analysis and Statistics
2.7.1. Data analysis
The data from the paper-based TB-01 journal for the 2019 period and the paper-based register during the electronic registration period (2021-22) was entered into a separate structured Excel file using single-entry with data quality checks to minimize data entry errors. The data were analyzed using STATA® software (version 16.0, Copyright 1985-2019 StataCorp LLC). Completeness was analyzed as: the frequency and proportion of completed non-mandatory variables were presented among all individuals registered in the electronic record. Concordance was analyzed for each variable by assessing the frequency and proportion of patients with the same information in both the paper-based and electronic registers were calculated.
Baseline demographic and clinical characteristics of patients were summarized using frequencies and percentages, stratified by the pre- and post-electronic system period. The baseline demographic and clinical characteristics across the two time periods were compared using a chi-square test.
To compare the time taken from symptom onset to diagnosis and diagnosis to initiation of TB treatment across the two time periods, the study used either Student's t-test or the Mann-Whitney test, depending on the distribution of continuous data. TB treatment outcomes were categorized as either successful or unsuccessful. Patients with recorded outcomes of cure or treatment completion were classified as having a 'successful outcome', while patients who died, were lost to follow-up, experienced treatment failure, or were not evaluated were classified as having an 'unsuccessful outcome'. The study used the chi-square test to compare the proportions with successful outcomes across the two time periods, as well as to compare the proportion of 'not evaluated' cases in the two time periods.
2.7.2. Sample size calculation
For objective 1: The sample size was determined using a 95% confidence interval with 80% power and assuming a relative 50% reduction in the proportion of patients with "not evaluated" in electronic (7%) compared to paper-based register (14%). At the ratio of 1:1 of unexposed to exposed, data needed to be extracted from 325 patients from both electronic and paper-based registers. Time constraints with running the study meant that the investigators could extract data of 302 patients to assess the completeness and concordance of paper-based and electronic data.
For objective 2: A sample size of 350 in each group was calculated to compare the change in the proportion of treatment outcomes between 2019 (paper-based) and 2021 (electronic registration period). The sample size was determined using a 95% confidence interval with 80% power and assuming a relative 40% reduction in the unsuccessful outcomes in electronic (12%) period compared to paper-based period (20%). Systematic random sampling with a sampling interval of four was used to select participants from the 2019 period and the required sample size was achieved.
3. Results
The study analyzed data from 302 individuals to assess the completeness and concordance of demographic and clinical details of TB patients between paper-based and electronic TB registers in 2021. Mandatory fields were complete in both registers, while non-mandatory fields had varying levels of completeness. The lowest completion rate was observed for the number of medication side effects reported (26.8%). The date fields (i.e., date of symptom onset, diagnosis, TB treatment initiation, and the first visit to a TB clinic) had the highest completeness rate (85.1%-93.0%) and concordance rate (83.2%-91.1%) between the two registers. Concordance was high for most variables, including sex, age, date of birth, case definition, treatment outcome, height, weight, and location of the disease. However, the number of medication side effects reported showed lower concordance between the two registers (see
Table 1).
In addition, the study analyzed the data of 350 individuals, equally distributed between the pre-implementation period (2019) and the post-implementation period (2021) of a digital recording system. The time taken from symptom onset to diagnosis was similar in both groups, with a median of 25 days in the paper-based system and 27 days in the electronic register system. The median time taken from symptom onset to treatment initiation was similar between the two groups, with a median of 29 days in the paper-based system and 30 days in the electronic register system. However, the percentage of patients who initiated treatment on the same day of diagnosis was significantly higher in the electronic register system (80.3%) compared to the paper-based system (57.1%) (p < 0.001)
(see
Table 2).
The study additionally compared the treatment outcomes of patients during the paper-based and electronic registration periods. The results showed that the proportion of successful outcomes (including cured and treatment-completed patients) was similar in the paper-based and electronic records groups (81.4% vs. 79.7%, p=0.284). There were some significant differences in the subcategories of unsuccessful outcomes. Specifically, the digital group had a higher proportion of patients who were lost to follow-up (5.7% vs. 2.0%, p<0.001), died (5.1% vs. 1.7%, p<0.001), and failed treatment (4.6% vs. 0.6%, p<0.001). Conversely, the electronic register system had a significantly lower proportion of patients with outcomes that were not evaluated or recorded (4.8% vs. 14.3%, p<0.001) (
Table 3).
4. Discussion
The study findings provide support for the implementation of electronic register systems in TB management, as these can lead to faster treatment initiation and improve data concordance. However, the study also highlights the importance of understanding the local context and potential limitations of the system, such as technical issues, data entry errors, and follow-up mechanisms. The study aimed to assess the concordance and completeness of demographic and clinical details of TB patients between paper-based and electronic TB registers in 2021. Our results showed high completeness and concordance for most variables, with some variations in non-mandatory fields. These findings are consistent with previous studies that have shown that the electronic system had higher completeness and concordance of data compared to paper records [
11]. The study's results provide important insights into the completeness and consistency of demographic and clinical data between the paper-based and electronic TB registers. These findings are applicable to health facilities providing services to patients with drug-sensitive pulmonary TB, as the study offers a comprehensive assessment of the data quality of both record-keeping systems.
The study found that medication side effects were reported in only a small proportion of cases in both the electronic TB register and paper-based records. We were unclear about what a blank field meant. This highlights the limitation of leaving the variable field blank instead of recording "0" when there are no side effects, which can result in incomplete and inaccurate data.
While there was no significant difference in the median time taken from symptom onset to diagnosis or treatment initiation between the paper-based and electronic registers, the electronic register system had a significantly higher proportion of patients who initiated treatment on the same day of diagnosis. This observation is in line with a previous study that showed a 22% increase in the initiation of HIV patients enrolled for ART after transitioning from a paper-based system [
12]. Initiating treatment on the same day of diagnosis is a crucial component of early and effective TB management, highlighting the potential benefit of electronic TB registers in improving patient outcomes.
The electronic register had a higher proportion of patients who were lost to follow-up, died, and failed treatment compared to the paper-based system, but a lower proportion where the outcome was not evaluated or recorded. One possible explanation for this finding could be that the electronic register system allowed for more accurate and comprehensive documentation of treatment. The finding supports the belief that the electronic register has improved the accuracy of TB treatment outcome documentation. These findings highlight the programmatic realities of managing drug-sensitive TB and the importance of accurate and complete documentation in tracking patient outcomes.
The strengths of this study include the use of routine data from the national TB program. The data was collected by a person with considerable experience in the program and data and who also understood the local context well. The number of records reviewed for the second objective met the requirement for the sample size. Finally, the conduct and reporting of the study were in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Limitations of the study included the following. Only 93% of the required sample size was achieved for the first objective. Only two regions of the country were sampled. These are thought to have better records than other regions, and so it is not clear how generalizable the results are to other parts of the country. Patient characteristics could also differ in separate cohorts as data was collected in 2019 and 2021.
Overall, this study highlights the potential benefits of implementing an electronic TB register system for TB patient care in the Kyrgyz Republic. The use of this system could be a reliable and effective alternative to paper-based records, providing accurate demographic and clinical data on TB patients. While the findings suggest that the electronic TB register is a valuable tool for TB care, mechanisms to regularly evaluate data quality and provide feedback to users should be put in place.
Author Contributions
“Conceptualization, D.S., O.P., M.G., E.W., E.M.K., P.K., K.I., O.G., B.K.; methodology, D.S., O.P., E.M.K., M.G., E.W., P.T., K.I., O.G., B.K.; software, D.S., O.P., P.T., E.M.K.; validation, D.S., O.P., E.M.K., M.G., E.W., P.T.; formal analysis, D.S., O.P., E.M.K., M.G., E.W., P.T.; investigation, D.S., O.P., E.M.K., M.G., E.W., P.T.; resources, D.S., O.G., B.K., K.I.; data curation, D.S., P.T., O.P.; writing— D.S., O.P., E.M.K., M.G., E.W.; original draft preparation, D.S., O.P, E.M.K., P.T.; writing—review and editing, D.S., O.P., E.M.K., P.T., E. W.; visualization, D.S., O.P., E.M.K., P.T..; supervision, E.M.K, E.W.; project administration, D.S., O.P., O.G.; funding acquisition, D.S.. All authors have read and agreed to the published version of the manuscript.”
Funding
This SORT IT program was funded by USAID and supported by TDR and implementing partners. TDR is able to conduct its work thanks to the commitment and support from a variety of funders. A full list of TDR donors is available at:
https://tdr.who.int/about-us/our-donors.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France (approval No EAG 16/2022 dated 26/01/2023) and by the Kyrgyzstan National Ethics Review Board (No 5/2023).
Informed Consent Statement
Since this study included data which is routinely collected as part of the National Tuberculosis Program of the Kyrgyz Republic, informed consent was not applicable.
Data Availability Statement
Requests to access these data should be sent to the corresponding author.
Acknowledgments
This research was conducted through Structured Operational Research and Training. Initiative (SORT IT), a global partnership coordinated by TDR, the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO). The specific SORT IT program that led to this publication included a partnership of TDR the European Tuberculosis Research Initiative (ERI-TB) at the WHO Regional Office for Europe the WHO Country Office in Kyrgyzstan and the National TB Control Programme of Kyrgyzstan. The SORT IT program was implemented along with the National TB Control Program of Kyrgyzstan, National Center of Phthisiology, Kyrgyz Republic; Tuberculosis Research and Prevention Center Non-Governmental Organization, Armenia; The International Union Against Tuberculosis and Lung Diseases, Paris and South East Asia offices; the American University of Armenia Turpanjian School of Public Health; The United Arab University of the Emirates; Damien Foundation, Belgium; University of Chester, United Kingdom; All India Institute of Medical Sciences, Nagpur, India Conflicts of Interest: No conflicts of interest.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Open Access Statement and Disclaimer
In accordance with WHO’s open-access publication policy for all work funded by WHO or authored / co-authored by WHO staff members, WHO retains the copyright of this publication through a Creative Commons Attribution IGO license (
http://creativecommons.org/licenses/by/4.0/igo/legalcode) which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited. There should be no suggestion that WHO endorses any specific organization, products or services. The views expressed in this article are those of the authors and do not necessarily reflect those of their affiliated institutions. The use of the WHO logo is not permitted. This notice should be preserved along with the article’s original URL.
References
- World Health Organization. Kyrgyzstan [Internet] (2021). Available from: https://www.who.int/countries/kgz/en/.
- World Health Organization & Society. Digital Health Technologies for TB Control: A Rapid Scan of Experience and Lessons Learned [Internet] (2015). Available from: https://www.who.int/tb/publications/digital-health-technologies-tb-control/en/.
- Lee, Y., Raviglione, M. C., & Flahault, A. (2020). Use of Digital Technology to Enhance Tuberculosis Control: Scoping Review. Journal of Medical Internet Research, 22(2), e15727. [CrossRef]
- Soltobekova, N., Kozukeev, T., Yiehdego, G., Labib, F., Hovhannesyan, A., & Rossi, R. (2022). Time to start of tuberculosis treatment in penitentiary system of Kyrgyz Republic: A retrospective cohort study. PLOS ONE, 17(3), e0264252. [CrossRef]
- Fritz, F., Tilahun, B., & Dugas, M. (2015). Success criteria for electronic medical record implementations in low-resource settings: A systematic review. Journal of the American Medical Informatics Association: JAMIA, 22(2), 479–488. [CrossRef]
- Abiy, R., Gashu, K., Asemaw, T., Mitiku, M., Fekadie, B., Abebaw, Z., Mamuye, A., Tazebew, A., Teklu, A., Nurhussien, F., Kebede, M., Fritz, F., & Tilahun, B. (2018). A Comparison of Electronic Medical Record Data to Paper Records in Antiretroviral Therapy Clinic in Ethiopia: What is affecting the Quality of the Data? Online Journal of Public Health Informatics, 10(2), e212. https://doi.org/10.5210/ojphi.v10i2.8309. [CrossRef]
- Oluoch, T., Katana, A., Ssempijja, V., Kwaro, D., Langat, P., Kimanga, D., Okeyo, N., Abu-Hanna, A., & de Keizer, N. (2014). Electronic medical record systems are associated with appropriate placement of HIV patients on antiretroviral therapy in rural health facilities in Kenya: A retrospective pre-post study. Journal of the American Medical Informatics Association, 21(6), 1009–1014. [CrossRef]
- Gadabu, O. J., Munthali, C. V., Zachariah, R., Gudmund-Hinderaker, S., Jahn, A., Twea, H., Gondwe, A., Mumba, S., Pulmonaryu, M., Malisita, K., Mhango, E., Makombe, S. D., Tenthani, L., Mwalwanda, L., Moyo, C., Douglas, G. P., Lewis, Z. L., and Chimbwandira, F. (2011) 'Is transcription of data on antiretroviral treatment from electronic to paper-based registers reliable in Malawi?', Public Health Action, 1(1), pp. 10-12. Available at. [CrossRef]
- National Statistical Committee of the Kyrgyz Republic [Internet]. (n.d.) . Available from: http://www.stat.kg/en/.
- The World Bank. (2022). Kyrgyz Republic Overview. Retrieved from https://www.worldbank.org/en/country/kyrgyzrepublic/overview.
- Thai, L. H., Nhat, L. M., Shah, N., Lyss, S., Ackers, M., Public Health Action, Electronic medical records and tuberculosis control in Vietnam: a stakeholder perspective. Public Health Action Volume 7, Number 4, 21 December 2017, pp. 294-298(5) International Union Against Tuberculosis and Lung Disease. [CrossRef]
- Abiy R, Gashu K, Asemaw T, Mitiku M, Fekadie B, Abebaw Z, Mamuye A, Tazebew A, Teklu A, Nurhussien F, Kebede M, Fritz F, Tilahun B. A Comparison of Electronic Medical Record Data to Paper Records in Antiretroviral Therapy Clinic in Ethiopia: What is affecting the Quality of the Data? Online J Public Health Inform. 2018 Sep 21;10(2):e212. PMID: 30349630; PMCID: PMC6194098. [CrossRef]
Table 1.
Completeness and Concordance of demographic and clinical details of TB patients between the paper-based TB register and electronic TB register in Kyrgyzstan during 2021.
Table 1.
Completeness and Concordance of demographic and clinical details of TB patients between the paper-based TB register and electronic TB register in Kyrgyzstan during 2021.
| Variable |
Completeness |
Concordance |
| |
Electronic |
Paper-based |
| |
n |
(%) |
n |
(%) |
Total |
n |
(%) |
| Total TB patients |
302 |
|
302 |
|
|
|
|
| Auto-calculated field |
|
|
|
|
|
|
|
| Sex |
302 |
(100) |
257 |
(85.1) |
257 |
254 |
(98.8) |
| Age |
302 |
(100) |
237 |
(78.5) |
237 |
225 |
(95.0) |
| Date of birth |
302 |
(100) |
281 |
(93.0) |
281 |
272 |
(96.8) |
| Mandatory field |
|
|
|
|
|
|
|
| Date of symptom onset |
302 |
(100) |
257 |
(85.1) |
257 |
234 |
(91.1) |
| Date of diagnosis |
302 |
(100) |
259 |
(85.8) |
259 |
217 |
(83.8) |
| Date of TB treatment initiation |
302 |
(100) |
281 |
(93.0) |
281 |
242 |
(86.1) |
| Date of the first visit to a TB clinic |
302 |
(100) |
270 |
(89.4) |
270 |
239 |
(88.5) |
| Case definition@
|
292 |
(96.7) |
261 |
(86.4) |
261 |
260 |
(99.9) |
| Date of treatment outcome |
302 |
(100) |
209 |
(69.2) |
209 |
174 |
(83.2) |
| Treatment outcome |
302 |
(100) |
229 |
(75.8) |
229 |
224 |
(97.8) |
| Non-mandatory fields |
|
|
|
|
|
|
|
| Height |
284 |
(94.0) |
263 |
(87.0) |
259 |
253 |
(97.6) |
| Weight |
289 |
(95.7) |
261 |
(86.4) |
259 |
255 |
(98.4) |
| Location of the disease |
290 |
(96.0) |
247 |
(81.8) |
247 |
247 |
(100) |
| Number of medication side effects reported |
81 |
(26.8) |
41 |
(13.6) |
41 |
35 |
(85.4) |
Table 2.
Comparison of time from symptoms to initiation of TB treatment among drug-sensitive TB patients initiated on anti-TB treatment in Bishkek pre (2019) and post (2021) implementation of an electronic register system in Kyrgyz republic.
Table 2.
Comparison of time from symptoms to initiation of TB treatment among drug-sensitive TB patients initiated on anti-TB treatment in Bishkek pre (2019) and post (2021) implementation of an electronic register system in Kyrgyz republic.
| Characteristics |
Paper-based |
Electronic |
p Value |
| |
Median |
(IQR) |
Median |
(IQR) |
|
| Total |
350 |
|
350 |
|
|
| Symptom onset to diagnosis in days |
25 |
(5-49) |
27 |
(13-45) |
0.210 |
| Diagnosis to treatment initiation in days |
0 |
(0-1) |
0 |
(0-0) |
<0.001 |
| Symptom onset to treatment initiation in days |
29 |
(13-48) |
30 |
(16-32) |
0.056 |
| Number (percentage) initiated on treatment on the same day of diagnosis* |
200 |
(57.1) |
281 |
(80.3) |
<0.001 |
Table 3.
Comparison of TB treatment outcomes among drug-sensitive TB patients initiated on anti-TB treatment in Bishkek pre (2019) and post (2021) implementation of an electronic register system in Kyrgyz Republic.
Table 3.
Comparison of TB treatment outcomes among drug-sensitive TB patients initiated on anti-TB treatment in Bishkek pre (2019) and post (2021) implementation of an electronic register system in Kyrgyz Republic.
| Treatment Outcomes* |
Paper-based |
Electronic |
p value$
|
| |
n |
(%)* |
n |
(%)* |
|
| Total |
350 |
|
350 |
|
|
| Successful Outcomes |
285 |
(81.4) |
279 |
(79.7) |
0.284 |
| Cured |
105 |
(30.0) |
88 |
(25.1) |
0.076 |
| Treatment Completed |
180 |
(51.4) |
191 |
(54.6) |
0.203 |
| Unsuccessful Outcomes |
|
|
|
|
|
| Loss-to-follow up |
7 |
(2.0) |
20 |
(5.7) |
<0.001 |
| Death#
|
6 |
(1.7) |
18 |
(5.1) |
<0.001 |
| Failure |
2 |
(0.6) |
16 |
(4.6) |
<0.001 |
| Not evaluated/recorded |
50 |
(14.3) |
17 |
(4.8) |
<0.001 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).